Association of Cardiovascular Risk Factors With Cardiac ......We identified baseline diabetes,...
Transcript of Association of Cardiovascular Risk Factors With Cardiac ......We identified baseline diabetes,...

JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Association of Cardiovascular Risk Factors With CardiacEvents and Survival Outcomes Among Patients With BreastCancer Enrolled in SWOG Clinical TrialsDawn L. Hershman, Cathee Till, Sherry Shen, Jason D. Wright, Scott D. Ramsey, William E. Barlow, andJoseph M. Unger
A B S T R A C T
BackgroundCardiovascular disease is the primary cause of death among patients with breast cancer. However,the association of cardiovascular-disease risk factors (CVD-RFs) with long-term survival and cardiacevents is not well studied.
MethodsWe examined SWOG (formerly the Southwest Oncology Group) breast cancer trials from 1999 to2011. We identified baseline diabetes, hypertension, hypercholesterolemia, and coronary arterydisease by linking trial records to Medicare claims. The primary outcome was overall survival.Patients with both baseline and follow-up claims were examined for cardiac events. Cox regressionwas used to assess the association between CVD-RFs and outcomes.
ResultsWe identified 1,460 participants older than 66 years of age from five trials; 842 were eligible forsurvival outcomes analysis. At baseline, median age was 70 years, and median follow-up was6 years. Hypertension (73%) and hypercholesterolemia (57%) were the most prevalent conditions;87% of patients had one or more CVD-RF. There was no association between any of the individualCVD-RFs and overall survival except for hypercholesterolemia, which was associated with improvedoverall survival (hazard ratio [HR], 0.73; 95% CI, 0.57 to 0.93; P = .01). With each additional CVD-RF,there was an increased risk of death (HR, 1.23; 95% CI, 1.08 to 1.40; P = .002), worse progression-free survival (HR, 1.12; 95%CI, 1.00 to 1.25; P = .05), andmarginally worse cancer-free survival (HR,1.15; 95% CI, 0.99 to 1.34; P = .07). The relationship between baseline CVD-RFs and cardiac eventswas analyzed in 736 patients. A strong linear association between the number of CVD-RFs andcardiac event was observed (HR per CVD-RF, 1.41; 95% CI, 1.17 to 1.69; P , .001).
ConclusionAmong participants in clinical trials, each additional baseline CVD-RFwas associatedwith an increasedrisk of cardiac events and death. Efforts to improve control of modifiable CVD-RFs are needed, es-pecially among those with multiple risk factors.
J Clin Oncol 36:2710-2717. © 2018 by American Society of Clinical Oncology
INTRODUCTION
During the past two decades, improvements inscreening and treatment options in women withbreast cancer (BC) have led to longer life spansand decreased rates of cancer-specific mortality;as a result, the risk of noncancer mortality hasbeen increasing.1 Cardiovascular disease increasesthe risk of noncancer mortality and is now theprimary cause of death among patients withBC.2,3 Various risk factors are common to thedevelopment of both BC and cardiovascular disease,
including diabetes, hypertension, hypercholes-terolemia, and obesity.4-6 Many of these comor-bidities are also risk factors for worse survivalamong those diagnosed with BC.7,8 Patients withBC are at additional risk of developing incidentcardiac conditions due to the cardiotoxic effects ofvarious anticancer therapies, such as radiation,anthracycline chemotherapies, and trastuzumab,and the secondary effects of treatment such asincreased frailty and deconditioning.9-12 How-ever, the relationship between cardiovascular riskfactors and long-term cardiac events among pa-tients with BC is not well studied.
Author affiliations and support information
(if applicable) appear at the end of this
article.
Published at jco.org on March 27, 2018.
Correspondence: Dawn L. Hershman, MD,
Columbia University Medical Center, 161
Fort Washington Ave, 10-1068, New York,
NY 10032; e-mail: [email protected].
© 2018 by American Society of Clinical
Oncology
0732-183X/18/3626w-2710w/$20.00
ASSOCIATED CONTENT
Appendix
DOI: https://doi.org/10.1200/JCO.
2017.77.4414
DOI: https://doi.org/10.1200/JCO.2017.
77.4414
2710 © 2018 by American Society of Clinical Oncology
VOLUME 36 • NUMBER 26 • SEPTEMBER 10, 2018
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

The risk of incident BC and BC mortality increases with age,and although the relative hazard rates of BC mortality are de-creasing overall, the decrease is less among elderly patients.1,13,14
In addition, elderly women may experience significantly higherrates of cardiotoxic adverse effects from treatment than youngerpatients.15 Data on mortality due to cardiovascular disease andrates of cardiac events among elderly patients are limited, however,especially because of under-representation of older patients inclinical trials.16,17
In this study, we assessed the relationship between cardiovascular-disease risk factors (CVD-RFs) and survival, as well as incidenceof cardiac events among patients older than 66 years of age en-rolled in a series of National Cancer Institute–sponsored adjuvantand advanced BC clinical treatment trials. CVD-RFs were iden-tified using a novel linkage between the clinical trial records andMedicare claims data.
METHODS
We obtained data from SWOG, a member of the National Cancer Institute’sClinical Trials Network and Community Oncology Research Program. Weexamined the SWOG database to identify patients registered in phase II/IIIBC trials between 1999 and 2011, the period during whichMedicare claimsdata were available for linkage to clinical records. We identified five eligibletrials: S0012, S0221, S0226, S0307, and S0500 (Appendix Table A1, onlineonly).18-21 Clinical records from these studies were linked to Medicareclaims data according to Social Security number, sex, and date of birth. Tobe included in the analyses of whether baseline cardiovascular conditionswere prognostic for survival outcomes, patients had to be at least 66 yearsof age at baseline and have at least 12 months of Medicare Parts A and Bcoverage immediately before baseline. To be included in the analyses ofcardiac event outcomes, patients also needed at least 12 months ofMedicare coverage at any point after registration to identify cardiac eventsafter treatment initiation. In both cases, because health maintenance or-ganization providers do not submit claims records to Centers for Medicareand Medicaid Services, patients must simultaneously have had no healthmaintenance organization coverage. Seventeen participants took part inmore than one included trial; the trial with the earlier registration date wasretained.
Various patient demographics, including age, sex, self-reported raceand ethnicity, and baseline body mass index (BMI) were obtained fromquestionnaires administered at the time of enrollment. Comorbid con-ditions at baseline were identified using International Classification ofDiseases (9th revision, clinical modification [ICD9]) codes from Medicareclaims data and included diabetes (with and without chronic complica-tions), hypertension, hypercholesterolemia, and coronary artery disease orischemic heart disease (CAD; Appendix Table A2, online only). Obesity, asa CVD-RF, was defined as BMI. 30 kg.m2 using trial records. Postbaselinecardiac event outcomes were identified by ICD9, Healthcare CommonProcedure Coding System, and Current Procedural Terminology surgicalcodes (Appendix Table A3, online only). Conditions and events wereidentified as any hospital claim or two or more physician or outpatientclaims at least 30 days apart. Survival outcomes data were obtained fromSWOG clinical records. Medicare also provides dates of death, which wereused to supplement SWOG data on death as a competing risk.
Statistical MethodsWe used multivariable Cox regression to assess the impact of various
baseline CVD-RFs on survival. The primary outcome was overall survival;secondary outcomes were progression-free survival and cancer-free sur-vival. We defined overall survival as time from study registration to deathdue to any cause, progression-free survival as time from study registration
to the development of progressive disease or death due to any cause, andcancer-free survival as time from study registration to death after in-studydisease progression or any death that occurred within 180 days of reg-istration. Analyses were stratified by study and treatment arm and adjustedfor baseline age (66 to 70 v $ 70), race (black v nonblack), and baselineprognostic risk scores for cancer outcomes on the basis of prespecifiedstudy-specific stratification variables to account for prognostic risk acrossa panel of different studies (Appendix Table A4, online only). Cox re-gression was performed separately for each cardiovascular condition, andan additional analysis was performed to assess the potential impact ofhaving multiple concurrent cardiovascular risks. Secondary analyses wereperformed separately by study type (adjuvant [S0012, S0221, S0307] vadvanced [S0226, S0500]).
We also investigated the impact of baseline CVD-RFs on the in-cidence of postbaseline cardiac events. We defined a cardiac event as anacute ischemic event or acute heart failure (Appendix Table A3). Cu-mulative incidence estimates were derived to account for competing risk ofdeath. To compare differences in incidence by CVD-RFs, Cox regressionwas used to calculate time to event, from registration to cardiac event orcensor (death or date of last contact), stratified by study and adjusted forbaseline age, race, and prognostic risk score. Some patients experiencedgaps in observation whenMedicare coverage was discontinued temporarily(n = 35 with gaps of $ 3 months; gaps , 3 months were ignored to allowfor administrative switching between plans). Participant time at risk in Coxmodels for cardiac event outcomes included only time under Medicareobservation. As stated previously, Cox regression was performed separatelyfor each CVD-RF. Additional analyses were performed to assess the impactof having multiple concurrent risk factors, and secondary analyses wereperformed separately by study type (adjuvant v advanced). In all analyses, Pvalues were two-sided and were based on a Wald test statistic. P , .05 wasconsidered significant. All tests were performed in SAS, Version 9.4 (SASInstitute, Cary, NC).
RESULTS
Of a total of 1,460 participants $ 66 years of age in the includedtrials, 842 participants were eligible for analyses of baseline car-diovascular conditions and survival outcomes and 736 patientswere eligible for analyses of baseline cardiovascular conditions andcardiac event outcomes (Appendix Fig A1, online only). Patientcharacteristics are listed in Table 1. Among patients in both an-alyses, the median age was 70 years, and the median follow-up was6 years. The majority of patients were non-Hispanic white. Hy-pertension was the most prevalent condition (73% in both co-horts), followed by hypercholesterolemia (57% in the survivalcohort, 58% in the cardiac event cohort), and 87% of patients ineach cohort had at least one CVD-RF.
Baseline Cardiovascular Risk Factors as Predictors ofSurvival
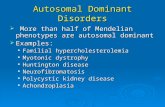
We observed no statistically significant association betweenany of the individual cardiovascular conditions and overall sur-vival, except for hypercholesterolemia, which was associated withimproved overall survival (hazard ratio [HR], 0.73; 95% CI, 0.57 to0.93; P = .01), progression-free survival (HR, 0.80; 95% CI, 0.65to 0.99; P = .04), and cancer-free survival (HR, 0.76; 95% CI, 0.57to 1.00; P = .05; Table 2; Fig 1). The association between hyper-cholesterolemia and better survival was stronger in advanced BCstudies, with considerably improved overall survival (HR, 0.65;95% CI, 0.48 to 0.88; P = .006), progression-free survival (HR,
jco.org © 2018 by American Society of Clinical Oncology 2711
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

0.68; 95% CI, 0.52 to 0.89; P = .005), and cancer-free survival (HR,0.62; 95% CI, 0.45 to 0.85; P = .003). Among participants inadjuvant studies only, the presence of CAD was marginally as-sociated with worse overall survival (HR, 1.53; 95% CI, 0.97 to2.41; P = .07) and progression-free survival (HR, 1.46; 95% CI,0.97 to 2.21; P = .07). We calculated the number of adverse CVD-RFs on the basis of Cox regression results for overall survival acrossall studies. Adverse risk was defined as having diabetes, hyper-tension, CAD, obesity, or the absence of hypercholesterolemia.Because so few patients had fewer than four conditions, we com-bined four and five concurrent conditions into one category. Witheach additional risk factor, there was a trend of increased riskof death (HR, 1.23; 95% CI, 1.08 to 1.40; P = .002), worseprogression-free survival (HR, 1.12; 95% CI, 1.00 to 1.25; P = .05),and marginally worse cancer-free survival (HR, 1.15; 95% CI, 0.99to 1.34; P = .07). A sensitivity analysis was performed with hy-percholesterolemia excluded as a risk factor, given its univariableassociation with better rather than worse survival; the results wereof similar direction and magnitude, although not statisticallysignificant (results not shown). There was no difference in overall
survival between patients with versus without a Medicare linkage(HR, 0.94; 95% CI, 0.79 to 1.11; P = .45; Appendix Fig A2, onlineonly).
Baseline Cardiovascular Risk Factors as Predictors ofCardiac Events
The proportion of patients who experienced cardiac eventswas much higher among patients with baseline CVD-RFs thanamong those without. The presence of CAD was associated witha more than two-fold increased risk of eventual cardiac event (HR,2.65; 95% CI, 1.70 to 4.13; P , .001), and diabetes was associatedwith a two-fold increased risk of a cardiac event (HR, 2.00; 95% CI,1.30 to 3.07; P = .002; Table 3). We stratified the analyses by studytype and found that in adjuvant studies, there was a more thanthree-fold increased risk of cardiac events among participants withhypertension (HR, 3.20; 95% CI, 1.39 to 7.39; P = .006) or CAD(HR, 3.44; 95% CI, 2.04 to 5.80; P , .001). Hypercholesterolemiaand obesity were not associated with increased risk of a cardiacevent. There were no statistically significant associations between
Table 1. Patient Characteristics
Characteristic
Survival Outcomes Cardiac Event OutcomesAll Trial Patients (linkedand unlinked; age $ 66)
(n = 842) (n = 736) (N = 1,460)
Median age, years (range) 70 66-91 70 66-91 70 66-92Median years of follow-up (range) 6 0-12 6 1-12 6 0-12RaceAsian/Pacific Islander 13 2 12 2 28 2Black 40 5 35 5 83 6Native 3 , 1 2 , 1 10 , 1Unknown 7 , 1 6 1 16 1White 779 93 681 93 1,323 91
EthnicityNot Hispanic 825 98 721 98 1,420 97Hispanic 17 2 15 2 40 3
Time of initial registrationBefore 2004 14 2 13 2 16 12004 or later 828 98 723 98 1,444 99
Baseline prognostic risk score*Low 592 72 530 74 1,006 70High 231 28 187 26 429 30
Study typeAdjuvant (S0012, S0221, S0307) 572 68 521 71 1,003 69Advanced (S0226, S0500) 270 32 215 29 457 31
Cardiovascular conditionsDiabetes with or without complications 206 24 179 24Hypertension 616 73 540 73Hypercholesterolemia 482 57 429 58CAD 156 18 134 18Obesity† 262 31 237 32
No. of cardiovascular conditionsNone 110 13 95 131 195 23 169 232 224 27 195 263 192 23 166 234 102 12 93 135 19 2 18 2
NOTE. Values are No. (%) unless otherwise indicated.Abbreviations: CAD, coronary artery disease or ischemic heart disease.*Baseline prognostic risk score is explained in Appendix Table A4.†Obesity at baseline is based on study questionnaires and at postbaseline is based on International Classification of Diseases (9th revision, clinical modification) codes inAppendix Table A2.
2712 © 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

any of the risk factors and cardiac events among participants inadvanced studies only, except diabetes (HR, 2.37; 95% CI, 1.09 to5.18; P = .03). We calculated the number of CVD-RFs on the basisof having diabetes, hypertension, CAD, obesity, or hypercholes-terolemia. Because so few patients had fewer than four condi-tions, we combined four and five concurrent conditions into onecategory. A linear association between the number of concurrentrisk factors and eventual cardiac event was observed (HR for eachadditional risk factor, 1.41; 95% CI, 1.17 to 1.69; P # .001;Table 3). The cumulative incidence of cardiac events by statis-tically significant baseline CVD-RFs for both adjuvant and ad-vanced studies is shown in Figure 2. A simple adverse risk modelwas derived by summing the number of statistically significantadverse cardiac factors from among the statistically significantfactors in univariable analysis (diabetes, hypertension, and CAD),grouped by 0 to 1 versus 2 versus 3. The association between fac-tor levels and development of cardiac events was even stronger forall patients (Table 3; Fig 2). This linear relationship was also evi-dent in the subset of adjuvant and advanced studies, respectively(Table 3; Fig 3).
Although trends were similar, the number of adverse riskfactors for cardiac events was not a statistically significant predictorof survival patterns (Table 2). For both the analyses of survivaloutcomes and cardiac events outcomes, there was no associationbetween number of CVD-RFs and treatment discontinuation(P = .63 and P = .70, respectively).
DISCUSSION
In this study of patients enrolled in five BC clinical trials,the presence of each additional CVD-RF was associated withworse overall and progression-free survival. CAD was inde-pendently associated with marginally worse overall survival andprogression-free survival among participants in adjuvant stud-ies, whereas hypercholesterolemia was actually associated withimproved overall survival, particularly among patients withadvanced disease. Similarly, the presence of each additional sig-nificant CVD-RF (diabetes, CAD, and hypertension) was associ-ated with an increased risk of a subsequent cardiac event in allpatients and when separately analyzed by adjuvant and advancedstudies.
The proportion of death due to cardiovascular disease hasbeen increasing among older women with BC. In a recent study oflong-term survivors of adult-onset cancer, 28.8% of the studyparticipants who had BC had a significantly higher risk of de-veloping cardiovascular disease than their noncancer counterparts,and overall survival was significantly worse among patients withcancer with cardiovascular disease.22 A large study of women olderthan 66 years of age with BC identified in the SEER databaseshowed that cardiovascular disease, which was defined as con-gestive heart failure, myocardial infarction, peripheral vasculardisease, or cerebrovascular disease, was the leading cause of death
Table 2. Survival by Baseline Cardiovascular Comorbidity Status
Comorbid Disease Predictors
Overall Survival Progression-Free Survival Cancer-Free Survival*
HR (95% CI)† P† HR (95% CI)† P† HR (95% CI)† P†
All studies combinedDiabetes 1.22 (0.94 to 1.58) .13 1.12 (0.89 to 1.42) .34 1.23 (0.91 to 1.65) .17Hypertension 1.17 (0.88 to 1.56) .28 1.05 (0.82 to 1.35) .67 1.03 (0.75 to 1.41) .87Hypercholesterolemia 0.73 (0.57 to 0.93) .01 0.80 (0.65 to 0.99) .04 0.76 (0.57 to 1.00) .05CAD 1.16 (0.88 to 1.54) .29 1.02 (0.79 to 1.31) .89 1.06 (0.76 to 1.48) .73Obesity 1.06 (0.77 to 1.46) .72 1.07 (0.80 to 1.43) .64 0.94 (0.62 to 1.42) .76No. of baseline cardiovascular risk factors‡ 1.23 (1.08 to 1.40) .002 1.12 (1.00 to 1.25) .05 1.15 (0.99 to 1.34) .07No. of significant risk factors 1.17 (0.98 to 1.39) .08 1.07 (0.92 to 1.26) .39 1.14 (0.93 to 1.39) .22
Adjuvant studies (S0012, S0221, S0307)Diabetes 1.09 (0.70 to 1.70) .71 1.07 (0.72 to 1.59) .74 1.16 (0.60 to 2.26) .65Hypertension 1.42 (0.86 to 2.34) .17 1.21 (0.80 to 1.83) .36 0.90 (0.47 to 1.72) .74Hypercholesterolemia 0.85 (0.57 to 1.28) .44 0.99 (0.69 to 1.42) .95 1.44 (0.75 to 2.76) .27CAD 1.53 (0.97 to 2.41) .07 1.46 (0.97 to 2.21) .07 1.59 (0.80 to 3.17) .19Obesity 1.10 (0.75 to 1.62) .63 1.10 (0.79 to 1.55) .57 0.91 (0.51 to 1.63) .75No. of baseline cardiovascular risk factors‡ 1.22 (1.01 to 1.47) .04 1.14 (0.96 to 1.35) .13 0.98 (0.74 to 1.31) .91Number of significant risk factors 1.23 (0.91 to 1.65) .18 1.20 (0.92 to 1.56) .17 1.25 (0.81 to 1.94) .31
Advanced studies (S0226, S0500)Diabetes 1.30 (0.95 to 1.80) .11 1.16 (0.86 to 1.55) .33 1.29 (0.92 to 1.80) .14Hypertension 1.02 (0.72 to 1.45) .92 0.92 (0.67 to 1.27) .62 1.04 (0.72 to 1.51) .83Hypercholesterolemia 0.65 (0.48 to 0.88) .006 0.68 (0.52 to 0.89) .005 0.62 (0.45 to 0.85) .003CAD 0.99 (0.69 to 1.42) .97 0.83 (0.60 to 1.14) .25 0.94 (0.64 to 1.38) .75Obesity 0.93 (0.51 to 1.67) .80 0.95 (0.55 to 1.65) .85 0.95 (0.53 to 1.73) .88No of baseline cardiovascular risk factors‡ 1.23 (1.03 to 1.47) .02 1.09 (0.94 to 1.27) .24 1.24 (1.03 to 1.48) .02No of significant risk factors§ 1.14 (0.91 to 1.42) .25 1.00 (0.82 to 1.22) .99 1.10 (0.88 to 1.39) .40
Abbreviations: CAD, coronary artery disease or ischemic heart disease; HR, hazard ratio.*Cancer-specific death was defined as any death that occurred either within 180 days of registration or after disease progression.†HRs and P values are stratified by study identification and treatment arm, and adjusted for age (66 to 70/$ 70 years), race (black/other), and baseline prognostic risk(low/high). P values are two-sided and are based on a Wald test statistic.‡Number of baseline cardiovascular risk factors is defined based on Cox regression results, for overall survival among all studies, as the number of concurrent factors:diabetes, hypertension, no hypercholesterolemia, CAD, or obesity.§On the basis of the adverse risk model including the three factors that were statistically significantly associated with cardiac events (diabetes, hypertension, and CADonly).
jco.org © 2018 by American Society of Clinical Oncology 2713
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

in the study population and was the primary cause of death amongolder women with stage I and II cancers.2 We also found that thenumber of baseline CVD-RFs was associated with worse overallsurvival, consistent with the current literature.
The association of CAD with worse overall survival and in-creased risk of cardiac events may have only been seen in adjuvant
and not advanced studies for several reasons. First, patients withadvanced cancer have a poor overall prognosis and short life
No. of significant BL CVD-RF
No. of BL CVD-RF
Obesity
CAD
Hypercholesterolemia
Hypertension
Diabetes
P = .04Adju
vant
Stu
dies
0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5
No. of significant BL CVD-RF
No. of BL CVD-RF
Obesity
CAD
Hypercholesterolemia
Hypertension
Diabetes
P = .006
P = .02
Hazard Ratio0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5
P = .005
0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5
P = .003
P = .02Adva
nced
Stu
dies
No. of significant BL CVD-RF
No. of BL CVD-RF
Obesity
CAD
Hypercholesterolemia
Hypertension
Diabetes
P = .01
P = .002
Overall Survival
All S
tudi
es C
ombi
ned
Progression-Free Survival
P = .04
P = .05
Cancer-Free Survival
P = .05
P = .07
Fig 1. Forest plot of survival by baseline comorbidity status. BL, baseline; CAD, coronary artery disease or ischemic heart disease; CVD-RF, cardiovascular-disease risk factor.
Table 3. Time to Cardiac Events for Participants With Baseline Cardiovascular Risk Factors
Baseline Risk Factor
All Studies Adjuvant Studies Advanced Studies
HR (95% CI)* P* HR (95% CI)* P* HR (95% CI)* P*
Diabetes 2.00 (1.30 to 3.07) .002 1.83 (1.09 to 3.09) .02 2.37 (1.09 to 5.18) .03Hypertension 2.00 (1.08 to 3.70) .03 3.20 (1.39 to 7.39) .006 0.96 (0.38 to 2.47) .94Hypercholesterolemia 1.50 (0.93 to 2.40) .09 1.63 (0.92 to 2.89) .09 1.42 (0.56 to 3.62) .46CAD 2.65 (1.70 to 4.13) , .001 3.44 (2.04 to 5.80) , .001 1.60 (0.69 to 3.69) .27Obesity 0.92 (0.56 to 1.50) 0.73 0.92 (0.55 to 1.55) .75 0.77 (0.14 to 4.42) .77No. of concurrent risk factors, per additional risk factor† 1.41 (1.17 to 1.69) , .001 1.47 (1.19 to 1.81) .001 1.31 (0.89 to 1.94) .17No. of concurrent significant risk factors, per additional riskfactor‡
2.11 (1.59 to 2.80) , .001 2.35 (1.65 to 3.34) , .001 1.79 (1.10 to 2.93) .02
Abbreviations: CAD, coronary artery disease or ischemic heart disease; HR, hazard ratio.*HRs and P values are stratified by study identification and treatment arm, and adjusted for age (66 to 70/$ 70), race (black/other), and baseline prognostic risk(low/high). P values are two-sided and are based on a Wald test statistic.†Includes diabetes, hypertension, hypercholesterolemia, CAD, and obesity. Because of small numbers of patients with many concurrent risk factors, patients with fouror five factors are combined.‡Includes only the risk factors that had a statistically significant association with cardiac events among the whole population of studies: diabetes, hypertension, andCAD. Patients with zero or one risk factor are combined.
2714 © 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

expectancy and thus may be at greater risk for cancer-specific deaththan death due to cardiac events, which usually results from long-term cumulative risk related to comorbidities. Second, elderlypatients are less adherent to their medications for chronic diseasesafter BC treatment, and decreased adherence to heart failureregimens can lead to cardiac events and mortality over time, whichagain may not have been captured in advanced studies.23 Third,two of the five studies included in this study, both adjuvant studies,included doxorubicin in the treatment regimens. Patients whoreceive doxorubicin have a significantly increased risk of developingcardiomyopathy, congestive heart failure, and heart disease; elderly
patients seem to be at greater risk for developing anthracycline-related cardiotoxicity, particularly incident congestive heart failure,than their younger counterparts.9,24 As such, elderly patients arealso at higher risk for experiencing cardiac events after receivinganthracycline-based chemotherapy, particularly if they had preexistingCVD-RFs.25 Neither of the two advanced studies examined in thecurrent study used anthracycline-based treatment regimens as theprimary treatment.
Diabetes has been consistently associated with poorer over-all survival among patients with BC, but the association withcancer-specific survival is less clear, with conflicting results in
0 1 2 3 4 5 6 7
Time Since Registration (years)
Cum
ulat
ive
Inci
denc
e of
Car
diac
Eve
nts
(%)
Diabetes
No diabetes
0
10
20
30
40
50
60
0 1 2 3 4 5 6 7
Time Since Registration (years)
Cum
ulat
ive
Inci
denc
e of
Car
diac
Eve
nts
(%)
0
10
20
30
40
50
60
Hypertension
No hypertension
0 1 2 3 4 5 6 7
Time Since Registration (years)
Cum
ulat
ive
Inci
denc
e of
Car
diac
Eve
nts
(%)
0
10
20
30
40
50
60
CAD
No CAD
0 1 2 3 4 5 6 7
Time Since Registration (years)
Cum
ulat
ive
Inci
denc
e of
Car
diac
Eve
nts
(%)
0
10
20
30
40
50
60
0 or 1
2
3
BA
C DFig 2. Cumulative incidenceof cardiac events
by statistically significant baseline cardiovascu-lar (CV) disease risk factors. CAD, coronary ar-tery disease or ischemic heart disease.
0 1 2 3 4 5 6 7
Time Since Registration (years)
Cum
ulat
ive
Inci
denc
e of
Car
diac
Eve
nts
(%)
0
10
20
30
40
50
60
0 or 1
2
3
0 1 2 3 4 5 6 7
Time Since Registration (years)
Cum
ulat
ive
Inci
denc
e of
Car
diac
Eve
nts
(%)
0
10
20
30
40
50
60
0 or 1
2
3
A B
Fig 3. Cumulative incidence of cardiacevents by number of cardiovascular dis-ease risk factors: (A) adjuvant studies and(B) advanced studies.
jco.org © 2018 by American Society of Clinical Oncology 2715
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

various studies.26-28 The increased mortality seen in patients withdiabetes has largely been attributed to an increased risk of car-diovascular events. Patients with diabetes present with later-stagedisease at the time of BC diagnosis, may receive altered treatmentregimens because of poorer baseline health, and may be at greaterrisk for experiencing treatment-related adverse effects.27 However,the use of metformin in patients with diabetes may improve overalland cancer-specific survival, possibly by inhibiting cancer cell pro-liferation or contributing to improved chemotherapy response.29 Inour study, diabetes was not significantly associated withworse overallsurvival, but did contribute to increased risk of all-cause mortalityin conjunction with other CVD-RFs and was associated with in-creased risk of cardiac events, suggesting that any association withincreased mortality seen in the literature may indeed be largely dueto increased risk of cardiovascular events.
The finding that hypercholesterolemia was actually associatedwith improved overall survival, particularly among patients withadvanced BC, is interesting; there are various possible explanationsfor this finding. Statins are considered first-line therapy in theprevention of cardiovascular mortality in patients with hypercho-lesterolemia and have been associated with improved disease-freesurvival in patients with BC.30 This association has also been seen inother cancers; a recent study of postdiagnosis statin use in patientswith prostate cancer showed an association with decreased cancer-specific and all-cause mortality.31 We were unable to assess whichpatients were receiving statin therapy in this analysis. Obesity isa significant risk factor for the development of BC, presentation ata later stage, and overall mortality among patients with BC, butcontrary to this, the obesity paradox has been seen in various othercancers where increased BMImay actually be protective in later-stagedisease against the wasting and cachexia effects of cancer.32-34 Al-though no significant association was seen in our study betweenobesity and overall survival in advanced studies, a recent study ofpostmenopausal women with BC in endocrine therapy trials foundthat a mean increase in BMI of 0.3 kg/m2 was associated withimproved survival after 1 year.35 A similar mechanismmay be at playamong late-stage patients with hypercholesterolemia in protectionagainst sarcopenia, frailty, and wasting; obese women often haveelevated levels of LDL cholesterol. The effect of hypercholesterolemiaspecifically in advanced BC has not been well studied; additionalstudies are warranted to clarify the relationship observed in ourstudy.
There are several strengths to our study. Participants wererequired to adhere to uniform protocol-specific therapy, andthe data were collected prospectively, enabling assessment ofprogression-free and cancer-free survival in addition to overallsurvival. These end points are rarely available in tumor registryanalyses. Uniform access to protocol therapy also limits the con-founding influence of access to cancer care. We were also able to
examine the association of multiple important CVD-RFs withsurvival and cardiac events. We also acknowledge several limi-tations. Patients were required to be enrolled in Medicare to beincluded in this study; therefore, all analyzed patients were olderthan 66 years of age; given that elderly patients are often under-represented in clinical trials, selection bias may limit the gen-eralizability of the results. Importantly, however, older patientsare those most at risk for cardiovascular events. We used ICD9codes to identify patients with CVD-RFs, but there are circum-stances in which patients’ conditions may not be properlycodified and thus subject to misclassification bias. All five SWOGstudies mandated a Zubrod score of 0 to 2, specifying that pa-tients needed to be at least ambulatory and capable of self-care aspart of the inclusion criteria; therefore, patients with severecomplications from their comorbidities and who may have been athigher cardiovascular event risk may not have been captured, alsopotentially limiting the generalizability of our results. Finally,specific cause-of-death data were not available, necessitating theuse of documented progression as an indicator of cancer-specificdeaths.
In conclusion, our study demonstrates significantly increasedrisk of all-cause mortality among patients with breast cancer andCAD, and shows aworsening of overall and progression-free survivalwith each additional cardiovascular risk factor. In addition, we showthat even among women with advanced cancer, the number of sig-nificant cardiovascular risk factors is associated with overall survivaland risk of a cardiac event. Because both early-stage patients and thosewith metastatic breast cancer live longer, care needs to be taken inmonitoring cardiovascular risk factors, especially among those withmultiple concurrent risk factors, to reduce the burden of death due tononcancer causes.
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTSOF INTEREST
Disclosures provided by the authors are available with this article atjco.org.
AUTHOR CONTRIBUTIONS
Conception and design: Dawn L. Hershman, Jason D. Wright, Scott D.Ramsey, Joseph M. UngerFinancial support: Dawn L. Hershman, Joseph M. UngerCollection and assembly of data: Dawn L. Hershman, Joseph M. UngerData analysis and interpretation: All authorsManuscript writing: All authorsFinal approval of manuscript: All authorsAccountable for all aspects of the work: All authors
REFERENCES
1. Jatoi I, Chen BE, Anderson WF, et al: Breastcancer mortality trends in the United Statesaccording to estrogen receptor status and age atdiagnosis. J Clin Oncol 25:1683-1690, 2007
2. Patnaik JL, Byers T, DiGuiseppi C, et al: Car-diovascular disease competes with breast cancer asthe leading cause of death for older females di-agnosed with breast cancer: A retrospective cohortstudy. Breast Cancer Res 13:R64, 2011
3. Chapman JA, Meng D, Shepherd L, et al:Competing causes of death from a randomized trial of
extended adjuvant endocrine therapy for breastcancer. J Natl Cancer Inst 100:252-260, 2008
4. Larsson SC, Mantzoros CS, Wolk A: Diabetesmellitus and risk of breast cancer: A meta-analysis.Int J Cancer 121:856-862, 2007
5. Rosato V, Bosetti C, Talamini R, et al: Meta-bolic syndrome and the risk of breast cancer in
2716 © 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

postmenopausal women. Ann Oncol 22:2687-2692,2011
6. Mozaffarian D, Benjamin EJ, Go AS, et al:Heart disease and stroke statistics-2016 update: Areport from the American Heart Association. Circu-lation 133:e38-e360, 2016
7. Protani M, Coory M, Martin JH: Effect ofobesity on survival of women with breast cancer:Systematic review and meta-analysis. Breast CancerRes Treat 123:627-635, 2010
8. Calip GS,Malone KE, Gralow JR, et al: Metabolicsyndrome and outcomes following early-stage breastcancer. Breast Cancer Res Treat 148:363-377, 2014
9. Doyle JJ, Neugut AI, Jacobson JS, et al:Chemotherapy and cardiotoxicity in older breastcancer patients: A population-based study. J ClinOncol 23:8597-8605, 2005
10. Perez EA, Suman VJ, Davidson NE, et al:Cardiac safety analysis of doxorubicin and cyclo-phosphamide followed by paclitaxel with or withouttrastuzumab in the North Central Cancer TreatmentGroup N9831 adjuvant breast cancer trial. J ClinOncol 26:1231-1238, 2008
11. Thavendiranathan P, Abdel-Qadir H, FischerHD, et al: Breast cancer therapy-related cardiacdysfunction in adult women treated in routine clinicalpractice: A population-based cohort study. J ClinOncol 34:2239-2246, 2016
12. Hooning MJ, Botma A, Aleman BM, et al:Long-term risk of cardiovascular disease in 10-yearsurvivors of breast cancer. J Natl Cancer Inst 99:365-375, 2007
13. Siegel RL, Miller KD, Jemal A: Cancer statis-tics, 2016. CA Cancer J Clin 66:7-30, 2016
14. Extermann M, Balducci L, Lyman GH:What threshold for adjuvant therapy in olderbreast cancer patients? J Clin Oncol 18:1709-1717,2000
15. Pinder MC, Duan Z, Goodwin JS, et al: Con-gestive heart failure in older women treated withadjuvant anthracycline chemotherapy for breastcancer. J Clin Oncol 25:3808-3815, 2007
16. Hutchins LF, Unger JM, Crowley JJ, et al:Underrepresentation of patients 65 years of age orolder in cancer-treatment trials. N Engl J Med 341:2061-2067, 1999
17. Lewis JH, Kilgore ML, Goldman DP, et al:Participation of patients 65 years of age or older incancer clinical trials. J Clin Oncol 21:1383-1389,2003
18. Ellis GK, BarlowWE, Gralow JR, et al: Phase IIIcomparison of standard doxorubicin and cyclophos-phamide versus weekly doxorubicin and daily oralcyclophosphamide plus granulocyte colony-stimulatingfactor as neoadjuvant therapy for inflammatory andlocally advanced breast cancer: SWOG 0012. J ClinOncol 29:1014-1021, 2011
19. Budd GT, BarlowWE,Moore HC, et al: SWOGS0221: A phase III trial comparing chemotherapyschedules in high-risk early-stage breast cancer.J Clin Oncol 33:58-64, 2015
20. Mehta RS, Barlow WE, Albain KS, et al:Combination anastrozole and fulvestrant in meta-static breast cancer. N Engl JMed 367:435-444, 2012
21. Smerage JB, BarlowWE, Hortobagyi GN, et al:Circulating tumor cells and response to chemother-apy in metastatic breast cancer: SWOG S0500. J ClinOncol 32:3483-3489, 2014
22. Armenian SH, Xu L, Ky B, et al: Cardiovasculardisease among survivors of adult-onset cancer: Acommunity-based retrospective cohort study. J ClinOncol 34:1122-1130, 2016
23. Yang J, Neugut AI, Wright JD, et al: Non-adherence to oral medications for chronic condi-tions in breast cancer survivors. J Oncol Pract 12:e800-e809, 2016
24. Swain SM, Whaley FS, Ewer MS: Congestiveheart failure in patients treated with doxorubicin: Aretrospective analysis of three trials. Cancer 97:2869-2879, 2003
25. Wang L, Tan TC, Halpern EF, et al: Majorcardiac events and the value of echocardiographicevaluation in patients receiving anthracycline-basedchemotherapy. Am J Cardiol 116:442-446, 2015
26. Srokowski TP, Fang S, Hortobagyi GN, et al:Impact of diabetes mellitus on complications andoutcomes of adjuvant chemotherapy in older pa-tients with breast cancer. J Clin Oncol 27:2170-2176,2009
27. Peairs KS, Barone BB, Snyder CF, et al: Di-abetes mellitus and breast cancer outcomes: Asystematic review and meta-analysis. J Clin Oncol29:40-46, 2011
28. Fleming ST, Rastogi A, Dmitrienko A, et al: Acomprehensive prognostic index to predict survivalbased on multiple comorbidities: A focus on breastcancer. Med Care 37:601-614, 1999
29. Xu H, Chen K, Jia X, et al: Metformin use isassociated with better survival of breast cancer pa-tients with diabetes: A meta-analysis. Oncologist 20:1236-1244, 2015
30. Borgquist S, Giobbie-Hurder A, Ahern TP, et al:Cholesterol, cholesterol-lowering medication use,and breast cancer outcome in the BIG 1-98 study.J Clin Oncol 35:1179-1188, 2017
31. Larsen SB, Dehlendorff C, Skriver C, et al:Postdiagnosis statin use and mortality in Danishpatients with prostate cancer. J Clin Oncol 35:3290-3297, 2017
32. Neuhouser ML, Aragaki AK, Prentice RL, et al:Overweight, obesity, and postmenopausal invasivebreast cancer risk: A secondary analysis of theWomen’s Health Initiative randomized clinical trials.JAMA Oncol 1:611-621, 2015
33. Kwan ML, Chen WY, Kroenke CH, et al: Pre-diagnosis body mass index and survival afterbreast cancer in the After Breast Cancer PoolingProject. Breast Cancer Res Treat 132:729-739,2012
34. Gonzalez MC, Pastore CA, Orlandi SP, et al:Obesity paradox in cancer: New insights provided bybody composition. Am J Clin Nutr 99:999-1005, 2014
35. Yerushalmi R, Dong B, Chapman JW, et al:Impact of baseline BMI and weight change inCCTG adjuvant breast cancer trials. Ann Oncol 28:1560-1568, 2017
AffiliationsDawn L. Hershman, Sherry Shen, and Jason D. Wright, Columbia University Medical Center, New York, NY; Cathee Till, Scott D.
Ramsey, William E. Barlow, and Joseph M. Unger, Fred Hutchinson Cancer Research Center, Seattle, WA.
SupportD.L.H. (National Cancer Institute [NCI] R01CA134964) and J.D.W. (NCI R01CA169121-01A1) are recipients of grants from the NCI,
Division of Cancer Prevention, Network and Community Oncology Research Program Research Base Grant No. 1UG1CA189974-01.D.L.H. is the recipient of grants from the Conquer Cancer Foundation, Breast Cancer Research Foundation, and Susan G. Komen ResearchFoundation (Grant No. SAC160066).
n n n
jco.org © 2018 by American Society of Clinical Oncology 2717
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Association of Cardiovascular Risk Factors With Cardiac Events and Survival Outcomes Among Patients With Breast Cancer Enrolled in SWOGClinical Trials
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships areself-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For moreinformation about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Dawn L. HershmanNo relationship to disclose
Cathee TillResearch Funding: Roche/Genentech (I)Patents, Royalties, Other Intellectual Property: Provisional patentapplication for CD20-targeted CAR T cells (I)
Sherry ShenNo relationship to disclose
Jason D. WrightConsulting or Advisory Role: Clovis Oncology, Tesaro
Scott D. RamseyConsulting or Advisory Role: BayerResearch Funding: Roche/GenentechTravel, Accommodations, Expenses: BMS
William E. BarlowResearch Funding: AstraZeneca (Inst), Merck (Inst)
Joseph M. UngerNo relationship to disclose
© 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

Appendix
No match to Medicare(n = 483)
Age ≥ 66 years with a DOBmatch to Medicare
(n = 977)
Total age ≥ 66 years(N = 1,460)
Survival analysis
Analyzable sample size(n = 842)
Inadequate Medicarecoverage to identify
baseline comorbiditiesand follow-up cardiac
events(n = 241)
Cardiac events analysis
Analyzable sample size(n = 736)
Inadequate Medicarecoverage to identify
baseline comorbidities(n = 135)
Fig A1. Flow diagram showing sample sizes and exclusions. DOB, date of birth.
jco.org © 2018 by American Society of Clinical Oncology
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

P = .460.25
0.50
0.75
1.00
0 2 4 6 8 10 12
Time Since Registration (years)
Time Since Registration (years)
Over
all S
urvi
val (
prob
abili
ty)
618 502 419 319 99 21 1
842 713 604 455 156 36 6
No. at risk
Not linked to Medicare database
Linked to Medicare database
Fig A2. Overall survival for patients with versus without a Medicare linkageamong patients with $ 12 months of continuous baseline Medicare coverage and$ 66 years old: (A) diabetes, (B) hypertension, (C) coronary artery disease orischemic heart disease (CAD), and (D) number of cardiovascular risk factors.
© 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

TableA1
.Sum
maryof
Includ
edStudies
Study
IDStudy
Nam
eTrea
tmen
tsEligibility
Yea
rsof
Enrollm
ent
Total
No.
No.
Age
$66
Yea
rs
No.
Eligible
forCurrent
Study
Surviva
lOutco
me
Ana
lysis*
Cardiac
Eve
ntOutco
meAna
lysis†
S00
12Breas
t,loca
llyad
vanc
ed/
inflam
matory,
AC
+G
vAC
Con
tinuo
usAC
+G-CSFthen
TStand
ardAC
35then
TLo
cally
advanc
edor
inflam
matory,
stag
eIIB
,IIIA,or
IIIB
2001
-200
539
930
2322
S02
21Breas
t,ad
juva
nt,N+,AC
vAC
+G/T
everywkvev
ery2wk
AC
+G
35wkthen
every2wk
T+PEG-G
36
AC
+G
315
wkthen
wee
kly
T3
12AC
+PEG-G
34then
every
2wkT+PEG-G
36
AC
+PEG-G
34then
wee
kly
T3
12AC
+PEG-G
36then
every2
wkT+PEG-G
36
AC
+PEG-G
36then
wee
kly
T3
12
Ope
rablestag
eI,II,
orIII
invasive
high
-risk
brea
stcarcinom
a20
03-201
23,29
123
713
597
S02
26Breas
t,ad
vanc
ed,
anastrozole6
Fulves
tran
t
Ana
strozole
Ana
strozole
andfulves
tran
tMetastatic
brea
stcanc
eror
multip
lesites
ofane
wdise
asethat
isclinically
obviou
smetastatic
dise
ase
2004
-200
970
732
720
317
6
S03
07Breas
t,ad
juva
nt,
bisp
hosp
hona
tes
Clodron
ate
Iban
dron
ate
Zoledron
icacid
Inva
sive
aden
ocarcino
maof
thebrea
st(stage
I,II,
III)with
noev
iden
ceof
metastatic
dise
ase
2006
-201
05,91
873
641
440
2
S05
00Breas
t,ad
vanc
ed,
CTC
,maintainv
chan
getrea
tmen
t
,5CTC
,arm
A(lo
wris
k)$
5CTC
,reregistratio
nrequ
ired
Initial
screen
ingbloo
ddraw
Maintaincu
rren
ttherap
ySwitc
htherap
y
Stage
IVdise
ase
2006
-201
260
113
067
39
Total
10,916
1,46
084
273
6
NOTE
.Sev
enteen
participan
tstook
partin
morethan
onetrial;forthes
epa
rticipan
ts,thetrialw
ithan
earlier
date
ofregistratio
nwas
retained
.Abb
reviations
:AC,d
oxorub
icinan
dcy
clop
hosp
hamide;
CTC
,circ
ulatingtumor
cells;G
,filgrastim
;G-CSF,
gran
uloc
yte-co
lony
stim
ulatingfactor;ID,ide
ntifica
tion;
N+,n
odepo
sitiv
e;PEG-G,p
egfilgrastim
;T,p
aclitaxel.
*Age
$66
yearsat
base
line,
with
$12
mon
thsMed
icareParts
Aan
dBco
verage
(nohe
alth
mainten
ance
orga
nizatio
n[HMO])be
fore
base
line.
†Age
$66
yearsat
base
line,
with
$12
mon
thsMed
icareParts
Aan
dBco
verage
(noHMO)be
fore
base
line,
and$
12mon
thsMed
icareParts
Aan
dB
cove
rage
(noHMO)at
anypo
intafterregistratio
n.
jco.org © 2018 by American Society of Clinical Oncology
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

Table A2. ICD9 Codes for Comorbidities
ICD9 Diagnosis Code Condition
Diabetes24900 Secondary diabetes mellitus without mention of complication, not stated as uncontrolled, or unspecified24901 Secondary diabetes mellitus without mention of complication, uncontrolled25000 Diabetes mellitus without mention of complication, type II or unspecified type, not stated as uncontrolled25001 Diabetes mellitus without mention of complication, type I [juvenile type], not stated as uncontrolled25002 Diabetes mellitus without mention of complication, type II or unspecified type, uncontrolled25003 Diabetes mellitus without mention of complication, type I [juvenile type], uncontrolled25010 Diabetes with ketoacidosis, type II or unspecified type, not stated as uncontrolled25011 Diabetes with ketoacidosis, type I [juvenile type], not stated as uncontrolled25012 Diabetes with ketoacidosis, type II or unspecified type, uncontrolled25013 Diabetes with ketoacidosis, type I [juvenile type], uncontrolled25020 Diabetes with hyperosmolarity, type II or unspecified type, not stated as uncontrolled25021 Diabetes with hyperosmolarity, type I [juvenile type], not stated as uncontrolled25022 Diabetes with hyperosmolarity, type II or unspecified type, uncontrolled25023 Diabetes with hyperosmolarity, type I [juvenile type], uncontrolled25030 Diabetes with other coma, type II or unspecified type, not stated as uncontrolled25031 Diabetes with other coma, type I [juvenile type], not stated as uncontrolled25032 Diabetes with other coma, type II or unspecified type, uncontrolled25033 Diabetes with other coma, type I [juvenile type], uncontrolled25080 Diabetes with other specified manifestations, type II or unspecified type, not stated as uncontrolled25081 Diabetes with other specified manifestations, type I [juvenile type], not stated as uncontrolled25082 Diabetes with other specified manifestations, type II or unspecified type, uncontrolled25083 Diabetes with other specified manifestations, type I [juvenile type], uncontrolled25090 Diabetes with unspecified complication, type II or unspecified type, not stated as uncontrolled25091 Diabetes with unspecified complication, type I [juvenile type], not stated as uncontrolled25092 Diabetes with unspecified complication, type II or unspecified type, uncontrolled25093 Diabetes with unspecified complication, type I [juvenile type], uncontrolled
Diabetes with complications25040 Diabetes with renal manifestations, type II or unspecified type, not stated as uncontrolled25041 Diabetes with renal manifestations, type I [juvenile type], not stated as uncontrolled25042 Diabetes with renal manifestations, type II or unspecified type, uncontrolled25043 Diabetes with renal manifestations, type I [juvenile type], uncontrolled25050 Diabetes with ophthalmic manifestations, type II or unspecified type, not stated as uncontrolled25051 Diabetes with ophthalmic manifestations, type I [juvenile type], not stated as uncontrolled25052 Diabetes with ophthalmic manifestations, type II or unspecified type, uncontrolled25053 Diabetes with ophthalmic manifestations, type I [juvenile type], uncontrolled25060 Diabetes with neurologic manifestations, type II or unspecified type, not stated as uncontrolled25061 Diabetes with neurologic manifestations, type I [juvenile type], not stated as uncontrolled25062 Diabetes with neurologic manifestations, type II or unspecified type, uncontrolled25063 Diabetes with neurologic manifestations, type I [juvenile type], uncontrolled25070 Diabetes with peripheral circulatory disorders, type II or unspecified type, not stated as uncontrolled25071 Diabetes with peripheral circulatory disorders, type I [juvenile type], not stated as uncontrolled25072 Diabetes with peripheral circulatory disorders, type II or unspecified type, uncontrolled25073 Diabetes with peripheral circulatory disorders, type I [juvenile type], uncontrolled25090 Diabetes with unspecified complication, type II or unspecified type, not stated as uncontrolled25091 Diabetes with unspecified complication, type I [juvenile type], not stated as uncontrolled25092 Diabetes with unspecified complication, type II or unspecified type, uncontrolled25093 Diabetes with unspecified complication, type I [juvenile type], uncontrolled
Hypertension4010 Malignant essential hypertension4011 Benign essential hypertension4019 Unspecified essential hypertension40200 Malignant hypertensive heart disease without heart failure40201 Malignant hypertensive heart disease with heart failure40210 Benign hypertensive heart disease without heart failure40211 Benign hypertensive heart disease with heart failure40290 Unspecified hypertensive heart disease without heart failure40291 Unspecified hypertensive heart disease with heart failure40300 Hypertensive chronic kidney disease, malignant, with chronic kidney disease stage I through stage IV, or unspecified40301 Hypertensive chronic kidney disease, malignant, with chronic kidney disease stage V or end stage renal disease40310 Hypertensive chronic kidney disease, benign, with chronic kidney disease stage I through stage IV, or unspecified40311 Hypertensive chronic kidney disease, benign, with chronic kidney disease stage V or end stage renal disease40390 Hypertensive chronic kidney disease, unspecified, with chronic kidney disease stage I through stage IV, or unspecified40391 Hypertensive chronic kidney disease, unspecified, with chronic kidney disease stage V or end stage renal disease40400 Hypertensive heart and chronic kidney disease, malignant, without heart failure and with chronic kidney disease stage I through stage IV,
or unspecified(continued on following page)
© 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

Table A2. ICD9 Codes for Comorbidities (continued)
ICD9 Diagnosis Code Condition
40401 Hypertensive heart and chronic kidney disease, malignant, with heart failure and with chronic kidney disease stage I through stage IV, orunspecified
40402 Hypertensive heart and chronic kidney disease, malignant, without heart failure and with chronic kidney disease stage V or end stagerenal disease
40403 Hypertensive heart and chronic kidney disease, malignant, with heart failure and with chronic kidney disease stage V or end stage renaldisease
40410 Hypertensive heart and chronic kidney disease, benign, without heart failure and with chronic kidney disease stage I through stage IV, orunspecified
40411 Hypertensive heart and chronic kidney disease, benign, with heart failure and with chronic kidney disease stage I through stage IV, orunspecified
40412 Hypertensive heart and chronic kidney disease, benign, without heart failure and with chronic kidney disease stage V or end stage renaldisease
40413 Hypertensive heart and chronic kidney disease, benign, with heart failure and chronic kidney disease stage V or end stage renal disease40490 Hypertensive heart and chronic kidney disease, unspecified, without heart failure and with chronic kidney disease stage I through stage
IV, or unspecified40491 Hypertensive heart and chronic kidney disease, unspecified, with heart failure andwith chronic kidney disease stage I through stage IV, or
unspecified40492 Hypertensive heart and chronic kidney disease, unspecified, without heart failure and with chronic kidney disease stage V or end stage
renal disease40493 Hypertensive heart and chronic kidney disease, unspecified, with heart failure and chronic kidney disease stage V or end stage renal disease40501 Malignant renovascular hypertension40509 Other malignant secondary hypertension40511 Benign renovascular hypertension40519 Other benign secondary hypertension40591 Unspecified renovascular hypertension40599 Other unspecified secondary hypertension45930 Chronic venous hypertension without complications45931 Chronic venous hypertension with ulcer45932 Chronic venous hypertension with inflammation45933 Chronic venous hypertension with ulcer and inflammation45939 Chronic venous hypertension with other complication7962 Elevated blood pressure reading without diagnosis of hypertension99791 Complications affecting other specified body systems, not elsewhere classified, hypertension
Hypercholesterolemia2722 Mixed hyperlipidemia2724 Other and unspecified hyperlipidemia
Coronary artery disease41400 Coronary atherosclerosis of unspecified type of vessel, native or graft41401 Coronary atherosclerosis of native coronary artery41402 Coronary atherosclerosis of autologous vein bypass graft41403 Coronary atherosclerosis of nonautologous biologic bypass graft41404 Coronary atherosclerosis of artery bypass graft41405 Coronary atherosclerosis of unspecified bypass graft41406 Coronary atherosclerosis of native coronary artery of transplanted heart41407 Coronary atherosclerosis of bypass graft (artery) (vein) of transplanted heartV4582 Percutaneous transluminal coronary angioplasty status43300 Occlusion and stenosis of basilar artery without mention of cerebral infarction43301 Occlusion and stenosis of basilar artery with cerebral infarction43310 Occlusion and stenosis of carotid artery without mention of cerebral infarction43311 Occlusion and stenosis of carotid artery with cerebral infarction43320 Occlusion and stenosis of vertebral artery without mention of cerebral infarction43321 Occlusion and stenosis of vertebral artery with cerebral infarction43330 Occlusion and stenosis of multiple and bilateral precerebral arteries without mention of cerebral infarction43331 Occlusion and stenosis of multiple and bilateral precerebral arteries with cerebral infarction43380 Occlusion and stenosis of other specified precerebral artery without mention of cerebral infarction43381 Occlusion and stenosis of other specified precerebral artery with cerebral infarction43390 Occlusion and stenosis of unspecified precerebral artery without mention of cerebral infarction43391 Occlusion and stenosis of unspecified precerebral artery with cerebral infarction4292 Cardiovascular disease, unspecified
Ischemic heart disease4110 Postmyocardial infarction syndrome4111 Intermediate coronary syndrome41181 Acute coronary occlusion without myocardial infarction41189 Other acute and subacute forms of ischemic heart disease other
Obesity27800 Obesity unspecified27801 Morbid obesity
Abbreviation: ICD9, International Classification of Diseases (9th revision, clinical modification).
jco.org © 2018 by American Society of Clinical Oncology
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

Table A3. ICD9, HCPCS, and Surgical Codes for Cardiac Event Outcomes
ICD9 Diagnosis Code HCPCS/CPT Code ICD9 Procedure Codes Description
41000 Acute myocardial infarction of anterolateral wall, episode of care unspecified41001 Acute myocardial infarction of anterolateral wall, initial episode of care41002 Acute myocardial infarction of anterolateral wall, subsequent episode of care41010 Acute myocardial infarction of other anterior wall, episode of care unspecified41011 Acute myocardial infarction of other anterior wall, initial episode of care41012 Acute myocardial infarction of other anterior wall, subsequent episode of care41020 Acute myocardial infarction of inferolateral wall, episode of care unspecified41021 Acute myocardial infarction of inferolateral wall, initial episode of care41022 Acute myocardial infarction of inferolateral wall, subsequent episode of care41030 Acute myocardial infarction of inferoposterior wall, episode of care unspecified41031 Acute myocardial infarction of inferoposterior wall, initial episode of care41032 Acute myocardial infarction of inferoposterior wall, subsequent episode of care41040 Acute myocardial infarction of other inferior wall, episode of care unspecified41041 Acute myocardial infarction of other inferior wall, initial episode of care41042 Acute myocardial infarction of other inferior wall, subsequent episode of care41050 Acute myocardial infarction of other lateral wall, episode of care unspecified41051 Acute myocardial infarction of other lateral wall, initial episode of care41052 Acute myocardial infarction of other lateral wall, subsequent episode of care41060 True posterior wall infarction, episode of care unspecified41061 True posterior wall infarction, initial episode of care41062 True posterior wall infarction, subsequent episode of care41070 Subendocardial infarction, episode of care unspecified41071 Subendocardial infarction, initial episode of care41072 Subendocardial infarction, subsequent episode of care41080 Acute myocardial infarction of other specified sites, episode of care unspecified41081 Acute myocardial infarction of other specified sites, initial episode of care41082 Acute myocardial infarction of other specified sites, subsequent episode of care41090 Acute myocardial infarction of unspecified site, episode of care unspecified41091 Acute myocardial infarction of unspecified site, initial episode of care41092 Acute myocardial infarction of unspecified site, subsequent episode of care4110 Postmyocardial infarction syndrome4111 Intermediate coronary syndrome41181 Acute coronary occlusion without myocardial infarction41189 Other acute and subacute forms of ischemic heart disease, other4275 Cardiac arrest4280 Congestive heart failure, unspecified4281 Left heart failure42820 Systolic heart failure, unspecified42821 Acute systolic heart failure42822 Chronic systolic heart failure42823 Acute on chronic systolic heart failure42830 Diastolic heart failure, unspecified42831 Acute diastolic heart failure42832 Chronic diastolic heart failure42833 Acute on chronic diastolic heart failure42840 Combined systolic and diastolic heart failure, unspecified42841 Acute combined systolic and diastolic heart failure42842 Chronic combined systolic and diastolic heart failure42843 Acute on chronic combined systolic and diastolic heart failure4289 Heart failure, unspecified42971 Acquired cardiac septal defect42979 Certain sequelae of myocardial infarction, not elsewhere classified, other
33510-3353333510 Coronary artery bypass, vein only; single coronary venous graft33511 Coronary artery bypass, vein only; 2 coronary venous grafts33512 Coronary artery bypass, vein only; 3 coronary venous grafts33513 Coronary artery bypass, vein only; 4 coronary venous grafts33514 Coronary artery bypass, vein only; 5 coronary venous grafts33516 Coronary artery bypass, vein only; 6 or more coronary venous grafts33517 Coronary artery bypass, using venous graft(s) and arterial graft(s); single vein graft (List
separately in addition to code for primary procedure)33518 Coronary artery bypass, using venous graft(s) and arterial graft(s); 2 venous grafts (List
separately in addition to code for primary procedure)33519 Coronary artery bypass, using venous graft(s) and arterial graft(s); 3 venous grafts (List
separately in addition to code for primary procedure)33521 Coronary artery bypass, using venous graft(s) and arterial graft(s); 4 venous grafts (List
separately in addition to code for primary procedure)(continued on following page)
© 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

Table A3. ICD9, HCPCS, and Surgical Codes for Cardiac Event Outcomes (continued)
ICD9 Diagnosis Code HCPCS/CPT Code ICD9 Procedure Codes Description
33522 Coronary artery bypass, using venous graft(s) and arterial graft(s); 5 venous grafts (Listseparately in addition to code for primary procedure)
33523 Coronary artery bypass, using venous graft(s) and arterial graft(s); 6 or more venous grafts(List separately in addition to code for primary procedure)
33530 Reoperation, coronary artery bypass procedure or valve procedure, more than 1 monthafter original operation (List separately in addition to code for primary procedure)
33533 Coronary artery bypass, using arterial graft(s); single arterial graft33960-33983
33962 Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)provided by physician; reposition peripheral (arterial and/or venous) cannula(e), open, 6years and older (includes fluoroscopic guidance, when performed)
33963 Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)provided by physician; reposition of central cannula(e) by sternotomy or thoracotomy,birth through 5 years of age (includes fluoroscopic guidance, when performed)
33964 Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)provided by physician; reposition central cannula(e) by sternotomy or thoracotomy, 6years and older (includes fluoroscopic guidance, when performed)
33965 Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)provided by physician; removal of peripheral (arterial and/or venous) cannula(e),percutaneous, birth through 5 years of age
33966 Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)provided by physician; removal of peripheral (arterial and/or venous) cannula(e),percutaneous, 6 years and older
33967 Insertion of intra-aortic balloon assist device, percutaneous33968 Removal of intra-aortic balloon assist device, percutaneous33969 Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)
provided by physician; removal of peripheral (arterial and/or venous) cannula(e), open,birth through 5 years of age
33970 Insertion of intra-aortic balloon assist device through the femoral artery, open approach33971 Removal of intra-aortic balloon assist device including repair of femoral artery, with or
without graft33973 Insertion of intra-aortic balloon assist device through the ascending aorta33974 Removal of intra-aortic balloon assist device from the ascending aorta, including repair of
the ascending aorta, with or without graft33975 Insertion of ventricular assist device; extracorporeal, single ventricle33976 Insertion of ventricular assist device; extracorporeal, biventricular33977 Removal of ventricular assist device; extracorporeal, single ventricle33978 Removal of ventricular assist device; extracorporeal, biventricular33979 Insertion of ventricular assist device, implantable intracorporeal, single ventricle33980 Removal of ventricular assist device, implantable intracorporeal, single ventricle33981 Replacement of extracorporeal ventricular assist device, single or biventricular, pump(s),
single or each pump33982 Replacement of ventricular assist device pump(s); implantable intracorporeal, single
ventricle, without cardiopulmonary bypass33983 Replacement of ventricular assist device pump(s); implantable intracorporeal, single
ventricle, with cardiopulmonary bypass33572 Coronary endarterectomy, open, any method, of left anterior descending, circumflex, or
right coronary artery performed in conjunction with coronary artery bypass graftprocedure, each vessel (List separately in addition to primary procedure)
3794 Implantation or replacement of automatic cardioverter/defibrillator, total system [AICD]3795 Implantation of automatic cardioverter/defibrillator lead(s) only3796 Implantation of automatic cardioverter/defibrillator pulse generator only3797 Replacement of automatic cardioverter/defibrillator lead(s) only3798 Replacement of automatic cardioverter/defibrillator pulse generator only3961 Extracorporeal circulation auxiliary to open heart surgery3962 Hypothermia (systemic) incidental to open heart surgery3963 Cardioplegia3965 Extracorporeal membrane oxygenation [ECMO]3966 Percutaneous cardiopulmonary bypass3603 Open chest coronary artery angioplasty3604 Intracoronary artery thrombolytic infusion3606 Insertion of non-drug-eluting coronary artery stent(s)3607 Insertion of drug-eluting coronary artery stent(s)3609 Other removal of coronary artery obstruction3760 Implantation or insertion of biventricular external heart assist system3761 Implant of pulsation balloon3762 Insertion of temporary nonimplantable extracorporeal circulatory assist device3763 Repair of heart assist system3764 Removal of external heart assist system(s) or device(s)3765 Implant of single ventricular (extracorporeal) external heart assist system
(continued on following page)
jco.org © 2018 by American Society of Clinical Oncology
Cardiovascular Risk Factors and Patients With Breast Cancer
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.

Table A3. ICD9, HCPCS, and Surgical Codes for Cardiac Event Outcomes (continued)
ICD9 Diagnosis Code HCPCS/CPT Code ICD9 Procedure Codes Description
3766 Insertion of implantable heart assist system3767 Implantation of cardiomyostimulation system3768 Insertion of percutaneous external heart assist device
Abbreviations: CPT, Current Procedural Terminology; HCPCS, Healthcare Common Procedure Coding System; ICD9, International Classification of Diseases (9threvision, clinical modification).
Table A4. Calculation of Baseline Prognostic Scores
Study ID Study-Specific Prognostic Factors Risk Score High Risk Sum
High Risk in SurvivalOutcome Analysis
No. (%)
High-Risk in CardiacOutcome Analysis
No. (%)
S0012 Inflammatory disease: no 0 1 13 (57) 12 (55)Inflammatory disease: yes 1
S0221 Nodal status: 0-3 0 $ 2 33 (27) 23 (27)Nodal status: $ 4 1HER2-negative and ER-positive and/or PR-positive 0HER2-positive and ER- and PR- either positive or negative 1HER2-negative and ER- and PR-negative 2
S0226 Prior adjuvant tamoxifen therapy: yes 1 1 76 (38) 66 (39)Prior adjuvant tamoxifen therapy: no 0
S0307 Nodal status: 0-3 0 $ 1 61 (15) 59 (15)Nodal status: $ 4 1Tumor size: # 5 cm 0Tumor size: . 5 cm 1
S0500 HER2-negative 1 2 48 (72) 27 (69)HER2-positive 0Measurable disease with or without nonmeasurable disease 1Nonmeasurable disease only including bone metastasis 0
NOTE. Our goal was to adjust for prognostic risk across a diverse pool of studies using a consistent approach. The variables defining risk scores were those identifiedprospectively for each trial as sufficiently meaningful with respect to prognosis as to be included as prespecified stratification variables to balance the treatmentrandomization assignment. For each study, we defined risk as follows. First, we identified the adverse risk categories from the stratification variables for each patient, andsummed the number of adverse risk categories, creating a score. Each study-specific risk scorewas split at the level thatmost closely approximated themedian, creatinga single binary indicator variable for low vs. high risk.Abbreviations: ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; ID, identification; PR, progesterone receptor.
© 2018 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Hershman et al
Downloaded from ascopubs.org by Journals Press Access on September 30, 2018 from 162.234.150.177Copyright © 2018 American Society of Clinical Oncology. All rights reserved.