ASCO 2018 Relapsed/Refractory Metastatic Solid Tumors ... · A Phase 1, First-in-Human, Open...
Transcript of ASCO 2018 Relapsed/Refractory Metastatic Solid Tumors ... · A Phase 1, First-in-Human, Open...

http://northernbiologics.com/wp-content/uploads/2018/12/ASCO_2018_Final_Poster.pdf
A Phase 1, First-in-Human, Open Label, Dose Escalation, Dose Expansion Study of MSC-1, A Humanized Anti-LIF Monoclonal Antibody, in Patients with
Relapsed/Refractory Metastatic Solid Tumors David M Hyman1, Irene Braña2, Anna Spreafico3, Alison M Schram1, Naimish B Pandya4, Kimberly Hoffman4, Robin Hallett4, Patricia Giblin4,
Judit Anido4, Isabel Huber Ruano4, Jeanne Magram4, Robert Wasserman4, Lillian L Siu3, Josep Tabernero2, Joan Seoane2, Jose Baselga1
1Memorial Sloan Kettering Cancer Center, New York, NY; 2Vall D’Hebron Institute of Oncology, Barcelona, Spain; 3Princess Margaret Cancer Center, Toronto, Canada; 4Northern Biologics, Inc., Toronto, Canada
Presented at the American Society of Clinical Oncology Annual Meeting, June 1–5, 2018, Chicago, IL
ASCO 2018Abstract 229677
ClinicalTrials.gov NCT03490669
BACKGROUND AND PRECLINICAL
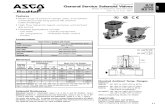
LEUKEMIA INHIBITORY FACTOR (LIF)■■ A multi-functional cytokine and part of the IL-6 family of cytokines■■ Binds to its specific receptor (LIFR) and recruits gp130 to form high affinity receptor complex■■ Activates downstream signaling pathways that regulate proliferation and survival
– Induces JAK/STAT3, PI3K/AKT and MAPK signaling pathways
■■ Complex role in tumor development and progression
– Increases the migration and invasion abilities of tumor cells and promotes metastasis – Described role in regulating multiple immune cell types found within TME, including T-eff, T-reg, Th17 cells, as well as Myeloid cells
■■ Promotes the activity of cancer initiating cells (CICs)■■ Increases resistance to anti-cancer therapy (chemotherapy and radiation therapy)
Scientific World Journal, 2013
Schema of the proposed LIF signaling pathway. LIF triggers activation of JAK/STAT and MAPK pathways independently, resulting in different cell-responses: increase of invasiveness and proliferation, respectively.3
MSC-1 — ANTI-LIF MONOCLONAL ANTIBODY ■■ First-in-class, humanized IgG1 monoclonal antibody■■ Binds to LIF with high affinity and specificity■■ Functions as a potent LIF antagonist■■ Inhibits downstream pSTAT3 in vitro and in vivo■■ Drives reprogramming of TME through modulation of immunosuppressive macrophages and of several immune cell types
Nor
mal
ized
MSD
Sig
nal 0.25
0.20 IC50 2.5 nm
0.15
0.10
0.05
0.00-2 -1 0 1 2 3
MSC-1 (log nM)
HCC1954 pSTAT3
Representative IC50 dose-inhibition curve of LIF-induced pSTAT3 with MSC-1 treatment in HCC1954 breast cancer cell line.
M2 Macrophages
T-regs
NK cells
CD4+ and CD8+ cells
MSC-1
Self-renewal(CIC)
TeffTregMyeloid/M2
LIF
LIF
ROLE IN MALIGNANCY■■ LIF is highly expressed in a sub-set of many solid tumors
GBM NSCLC
LIF
H-S
core
Ovarian CA
Low
LIF
Hig
h LI
F
CRC Pancreatic Ca
0
100
200
300
0
100
200
300
0
100
200
300
0
100
200
300
0
100
200
300
IHC with an anti-LIF polyclonal antibody evaluating different tumor types (Red bars represent mean +/- SEM). LIF was highly expressed in a subset of GBM, NSCLC, Ovarian, Colorectal and Pancreatic tumors.
■■ LIF over-expression correlates to poor prognosis
MonthsMonths Since Initial Diagnosis Local Recurrence-free Survival (years)00 20 40 60 80 100 120 50 100 150 200 250
50
60
70
80
90
100
0
20
40
60
80
100
HR=1.357 (0.96–1.92)p=0.041
p=0.016p=0.001
A.
C.
B.
100
50
00 50 100 150
Perc
ent
Surv
ival
Months
High LIFLow LIF
High LIFLow LIF
High LIFLow LIF
High LIFLow LIF
High LIFLow LIF100
50
0 0
0.25
0.50
0.75
1.00
0 20 40 60 80 100
Perc
ent
Surv
ival
Perc
ent
Surv
ival
Perc
ent
Surv
ival
Cum
ulat
ive
Surv
ival
Prob
abili
ty o
f Sur
viva
l
Months Breast Relapse-free Survival (years)
p<0.001p<0.001
0 20 40 60 80 100
p=0.0039
LIF negative stainingLIF positive staining
1.0
0.8
0.6
0.4
0.2
00 2 4 6 8
Colon
Lung Breast
NasopharyngealGBM
Head and Neck
High LIF expression correlates with poor prognosis. A. High LIF transcript levels are associated with poor outcome in GBM (Internal data) and Colon cancer (Yu 2014). B. High circulating serum LIF protein levels correlates with poor outcome in Nasopharyngeal cancer (Liu 2013). C. High intratumoral LIF protein expression correlates with poor outcome in Head and Neck, Lung and Breast cancers (Albrengues 2014, Li 2014).
MSC-1 IN SYNGENEIC MODELS■■ MSC-1 inhibited tumor growth in mutiple syngeneic models
Control rMSC-1
Control rMSC-1
Control rMSC-1
OvarianID8
NSCLCKLN205
ColonCT26
Vehicle rMSC-1 shLIF#1 shLIF#20
4x107
3x107
2x107
1x107
Tota
l Flu
x (p
/s)
0
8x106
6x106
4x106
2x106
Tota
l Flu
x (p
/s)
Abd
omin
al V
olum
e (m
m3 )
Abd
omin
al V
olum
e (m
m3 )
p=0.07
**(p=0.001)
****(p<0.0001)
****(p<0.0001)
Vehicle rMSC-10
500
1000
1500
2000
2500 ***
Tum
or V
olum
e (m
m3 )
Tum
or V
olum
e (m
m3 )
Vehicle rMSC-10
2000
4000
6000
8000
10000
5 10 15 20
ControlrMSC-1
Days after Inoculation
shLIF #1shLIF #2
ControlrMSC-1
ControlrMSC-1
30 35 40250
2000
4000
6000
8000
Days after Inoculation
Days after Inoculation10 15 20
0
500
1000
1500
Tumor growth in rMSC-1 and control treated mice in three syngeneic models: KLN205 NSCLC tumor (orthotopic), ID8 Ovarian tumor (peritoneum), and CT26 Colon cancer (SQ).
MSC-1 REPROGRAMS TUMOR MICROENVIRONMENT■■ MSC-1 increased frequency of intratumoral immune cells and activation status
Control (PBS) rMSC-10
1
2
3
4
Control (PBS) rMSC-1
% C
D45
+
*(p=0.02)
Vehicle rMSC-10.0
0.1
0.2
0.3
% C
D3+ C
D4+
**(p=0.008)
Vehicle rMSC-1
Control (PBS) rMSC-1 Vehicle rMSC-1 Vehicle rMSC-1
0.0
0.5
1.0
1.5
2.0
% C
D3+ C
D8+
**(p=0.008)
0.00
0.02
0.04
0.06
0.08
0.10
% C
D3– C
D49
b+
**(p=0.008)
0.000
0.005
0.010
0.015
0.020
% C
D4+ C
D69
+
**(p=0.008)
0.000
0.005
0.010
0.015
0.020
% C
D8+ C
D69
+
**(p=0.008)
N=5 N=5 N=5 N=5 N=5 N=5
N=5 N=5 N=5 N=5 N=5 N=5
Immune cell infiltrates in ID8 tumors from rMSC-1 or control treated mice. Tumors were harvested at d40 post implantation and analyzed by flow cytometry. Similar results were observed in the KL205 and CT26 models.
■■ LIF drives differentiation into immunosuppressive human macrophages
CD206CCL22
CCL1CTSK
Vehicle
****
rMSC-1% C
D20
6+ / IB
A1+ C
ells 100
80
60
40
20
0Vehicle
****
rMSC-1% C
CL22
+ / IB
A1+ C
ells 100
80
60
40
20
0
Cont
rol
rMSC
-1
Cont
rol
rMSC
-1
CD206 IBA-1 MERGE DAPI CCL22 IBA-1 MERGE DAPIPatient 1 Patient 1
M2 M1MSC-1
Pro-tumorEffect
Anti-TumorEffect
HumanMonocytes
72h CM ofU251 shLIF
Log
(p-v
alue
)
Log2 Fold Change
A.
B.
A. Evaluation of gene expression in monocytes isolated from human peripheral blood and treated with conditioned media from U251 cells and U251 cells with a knockdown of LIF expression by shRNA. The expression analysis is shown as a volcano plot highlighting differentially expressed M2 macrophage genes. B. Human GBM organotypic slices were incubated with rMSC-1 for 72 hrs. and stained using double immunofluorescence for (A) CD206 or (B) CCL22 with IBA-1. Representative images of the immunofluorescence are shown (scale bar, 50 µm). Similar results were observed with three patients
■■ MSC-1 treatment reprogramed macrophages towards a pro-inflammatory phenotype Control CD11b TAM
M1: CD206neg/MHCIIhigh M2: CD206high/MHCIIneg
MHCII
CD20
6
106
105
104
103
103 104 105 106 107
0-103
-104
106
105
104
103
103 104 105 106 107
0-103
-104
80
60
40
20
0
40
30
20
10
0
% in
CD
45
% in
CD
45
80
60
40
20
0
10
6
8
4
2
0
% in
TA
M
% in
TA
M
MSC-1Control
p=0.016 P=0.007
MSC-1 Control MSC-1
Control MSC-1 Control MSC-1
M2:9.2
M2:0.5
M1: 19.1
M1: 48.9
Tumor associated macrophages (TAMs) were harvested from tumors treated with MSC-1 (15 mg/kg, 2QW) on day 25 (endpoint). TAMs in treated tumors were polarized towards the M1 pro-inflammatory phenotype. Statistical significance determined by unpaired t-test.
STUDY RATIONALE■■ LIF is a pleotropic cytokine over-expressed in multiple solid tumors and hypothesized to play a role in tumor growth, progression and resistance to standard anti-cancer treatments■■ It is hypothesized that in patients with advanced solid tumors, treatment with MSC-1 will lead to effective blocking of LIF signaling and reprogramming of the tumor microenvironment causing increased immune-mediated anti-tumor effect■■ It is further hypothesized that administration of MSC-1 will be sufficiently well tolerated to enable further development subsequent to the completion of this Phase 1 study
KEY STUDY OBJECTIVESPRIMARY OBJECTIVE ■■ To evaluate the safety and tolerability of MSC-1 in patients with advanced solid tumors■■ To determine the recommended dose for MSC-1 monotherapy■■ To assess the preliminary anti-tumor activity, as measured by ORR, of MSC-1 according to RECIST 1.1 criteria
SECONDARY OBJECTIVES■■ To characterize the PK and immunogenicity of MSC-1■■ To assess efficacy parameters in patients with advanced solid tumors, including DCR & PFS by RECIST 1.1
KEY EXPLORATORY OBJECTIVES■■ To explore the relationships between PK, pharmacodynamics and MSC-1 exposure to patient safety and anti-tumor activity■■ To assess whether high tumor LIF expression correlates with anti-tumor activity of MSC-1■■ To characterize pharmacodynamic effects of MSC-1 in the periphery and in the tumor ■■ To characterize impact of MSC-1 treatment on exploratory biomarkers
STUDY DESIGN■■ Open-label, Phase 1 study enrolling advanced solid tumor patients ■■ The study will be conducted in an accelerated-titration 3 + 3 design ■■ Flat dose of MSC-1 administered intravenously once Q3W
DOSE ESCALATION(all comer solid tumors)
MTD / OBD
DOSE EXPANSION(LIF-High)
NSCLC BasketOvarianCancer
PancreaticCancer
RESPONSE ASSESSMENTS■■ Anti-tumor response will be assessed by Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 guidelines■■ Assessments to be performed at baseline and every 6 weeks for first 6 months and then every 12 weeks thereafter until confirmed progression disease or patient withdrawal
SAFETY ASSESSMENTS■■ Adverse events will be graded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 4.03■■ To be assessed continuously during the study and for 30 days after the last treatment
ENTRY CRITERIAKEY INCLUSION CRITERIA■■ Histologically proven relapsed / refractory advanced, unresectable solid tumor ■■ Measurable disease as per RECIST 1.1 criteria■■ Identification of archival tumor sample for LIF expression analysis■■ ECOG 0 or 1■■ Weight > 37.5 kg■■ Life expectancy ≥ 12 weeks■■ Men and women ≥ 18 years of age■■ Adequate organ function■■ Signed Informed Consent
KEY EXCLUSION CRITERIA■■ Symptomatic or unstable brain metastasis■■ Prior systemic therapy within 4 weeks of study entry■■ Prior radiation therapy or significant surgery within 21 days to study entry■■ Ascites or pleural effusion requiring large volume para- or pleurocentesis within 4 weeks of study entry ■■ Patients currently receiving immunosuppressive therapy, except inhaled corticosteroids ■■ Uncontrolled or clinically significant cardiovascular or pulmonary disease■■ Grade 3 or 4 peripheral neuropathy (NCI CTCAE v4.03)■■ Vaccination with live virus vaccine 4 weeks from initiation■■ Positive for hepatitis B or C or HIV ■■ Second primary malignancy not in remission > 2 years■■ Therapeutic anticoagulation for a thromboembolic event
REFERENCES1. Yue X et al. Cancer Cell Microenvironment 2015 PMID: 26807429. 2. Nicola NA et al. Cytokine Growth Factor Rev 2015 PMID: 26187859. 3. Morales-Prieto DM et al. The Scientific World Journal 2013 PMID: 24288470. 4. Yu H et al. Nature Communications 2014 PMID: 4203416. 5. Liu S et al. J of Clinical Investigations 2013 PMID: 24270418. 6. Albrengues J et al. Cell Reports 2014 PMID: 24857661. 7. Li X et al. Oncotarget 2014 PMID: 24553191.
Copies of this poster obtained through Quick Response (QR) Code are for personal use only and may not be reproduced without permission from ASCO® and the author of this poster.