ARTICLE IN PRESS · Daniel Gallego, Nicholas Ferrell, ... to eventually overcome some of the...
Transcript of ARTICLE IN PRESS · Daniel Gallego, Nicholas Ferrell, ... to eventually overcome some of the...

ng C xx (2007) xxx–xxx
+ MODEL
MSC-02085; No of Pages 6
www.elsevier.com/locate/msec
ARTICLE IN PRESS
Materials Science and Engineeri
Multilayer micromolding of degradable polymer tissue engineering scaffolds
Daniel Gallego, Nicholas Ferrell, Yang Sun, Derek J. Hansford ⁎
Biomedical Engineering Department, The Ohio State University, 1080 Carmack Road, 270 Bevis Hall, Columbus (OH), 43210, United States
Abstract
Precise surface geometrical morphologies have been shown to improve cellular proliferation, adhesion, and functionality. It has been found thatcells respond strongly to feature dimensions a fraction of their size. In this paper, soft lithography techniques were applied to microfabricatepolydimethylsiloxane molds with precisely controlled micro-scale patterns. Three-dimensional polycaprolactone (PCL) scaffolds were fabricatedusing a multilayer micromolding (MMM) method. Proper heating and stamping parameters were developed for micromolding PCL. This processallowed control of the size, shape, and spacing of support structures within the scaffold. The micromolding of multiple layers with independentfeatures allowed for alignment between layers. The high porosity, abundant interconnections, and sharp features were inherent advantages of thescaffolds. Human osteosarcoma cells were seeded in the 3-D scaffolds for cell growth testing. Fluorescent microscopy and scanning electronmicrographs showed that cells responded well to the 3-D scaffolds and the scaffolds regulated cell morphology and adhesion.© 2007 Elsevier B.V. All rights reserved.
Keywords: Polycaprolactone; Scaffold; Tissue engineering; Microfabrication; Soft lithography; Multilayer micromolding
1. Introduction
Tissue and organ failure have traditionally been treated by theimplementation of autografts or allografts. Such options still presentseveral limitations mainly due to the lack of donors, potential ofimmune rejection, pathogen infection, and high morbidity of donorsite [1]. Tissue engineering is an alternative option to restore lost ordamaged tissue through therapies based on a combination of threefactors: scaffolds, cells, and growth factors [2]. Scaffolds are eithertemporary or permanent matrices responsible for supporting and, inmost cases, regulating the growth of new tissue [3,4].
The fabrication of highly porous structures with synthetic ornaturally occurring biomaterials has been the most commonapproach for producing tissue engineering scaffolds. Severaltechniques, including particulate leaching, foaming, sponge tem-plating, phase separation, and freeze-drying [5–7] have been studiedfor this purpose. However, the lack of control of the scaffoldsmicrofeatures (pore size, shape, interconnection, distribution, etc.) isstill an issue related to the limited success of these structures inassisting the processes of tissue regeneration/formation [8].
Traditional porous scaffolds present a random geometry thatdoes not allow uniform nutrient exchange, therefore limiting cell
⁎ Corresponding author.E-mail address: [email protected] (D.J. Hansford).
0928-4931/$ - see front matter © 2007 Elsevier B.V. All rights reserved.doi:10.1016/j.msec.2007.04.021
Please cite this article as: D. Gallego et al., Mater. Sci. Eng. C (2007), doi:10.10
growth and differentiation. Recent advances in the field ofmicrotechnology show promising results in the fabrication oftissue engineering scaffolds with controlled chemistry andmorphology at themicro-scale. Such characteristics are expectedto eventually overcome some of the disadvantages presented bytraditional scaffold fabrication methods for tissue engineeringapplications due to production of random architectures [9,10].
This paper describes a soft lithography-basedmethod [11,12] forthe fabrication of three-dimensional tissue engineering scaffoldsfrom degradable polymers, with precisely controlled morphology atthe micro-scale. A multilayer micromolding (MMM) technique ispresented to obtain interconnected highly porous polycaprolactone(PCL) scaffolds with pre-defined pore size and shape. Scanningelectron microscopy (SEM) was used to evaluate the scaffoldmorphology. The cytocompatibility of the scaffolds was tested via24 and 48 h human osteosarcoma (HOS) cell cultures. Cellresponses were characterized by SEM and confocal microscopy.
2. Materials and methods
2.1. Scaffold fabrication and characterization
2.1.1. Microfabrication of master by photolithographyStandard photolithography [13,14] using a negative SU-
8 photoresist (MicroChem Corp., USA) was used to obtain a
16/j.msec.2007.04.021

Table 1Pressures and times used for multiple layer scaffold fabrication
Layer Pressure (psi) Time (min)
2 32 33 30 54 28 105 26 156 24 207 22 258 20 309 18 3010 18 30
2 D. Gallego et al. / Materials Science and Engineering C xx (2007) xxx–xxx
ARTICLE IN PRESS
master with raised features forming a grid pattern of lines at 90°to each other. The fabrication parameters (spin speed, exposuredose, and baking times) were set up to acquire 5 μm wide and10 μm thick ridges, with 45 μm spacing between parallel lines.SEM and light microscopy were used to characterize the mastermold.
2.1.2. Fabrication of PDMS mold by soft lithographySoft lithography techniques were used to fabricate a poly-
dimethylsiloxane (PDMS) mold from the master. PDMS (SilasticT-2, Dow Corning, USA) was uniformly mixed with curing agent
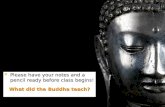
Fig. 1. Schematic diagram of the MMMmethod. A. PDMSmold B. PDMS mold spinsurface material D. PCL removed from the surface during the first stamping E. PDMSheat and pressure to remove the PCL from themoldG.Mold is removed leaving the PCrepeating step F I. Mold is removed and a two layer scaffold remains J. Process is rep
Please cite this article as: D. Gallego et al., Mater. Sci. Eng. C (2007), doi:10.10
at a 10:1 (w/w) ratio. Themixturewas poured onto themastermoldand subsequently degassed in a vacuum desiccator for approxi-mately 20 min. PDMS was allowed to cure at room temperature.After 48 h, the PDMS negative mold was peeled off of the mastermold and cut into smaller (0.5×0.5 in2) square molds that wereused to fabricate the scaffolds. The negative molds were examinedunder SEM and light microscopy.
2.1.3. Scaffold microfabrication using the multilayermicromolding (MMM) approach
A MMM approach was used to fabricate three-dimensionalscaffolds from polycaprolactone. For this purpose, polycapro-lactone (Aldrich, USA), with an average molecular weight of80,000 was dissolved in tetrahydrofuran (THF, Mallinckrodt,USA) and dimethylsulfoxide (DMSO, Fisher, USA) at a 1:3:6(w/w/w) ratio. The solution was spin coated on the PDMSmoldsat 4000 rpm for 1 min. The polymer that accumulated on theraised features was removed by using a preheated glass slide at65 °C. For the first layer, the PDMS mold was initially heated to90 °C for 15min on a hotplate. The PCL inside the microfeatureswas stamped out onto a glass slide by pressing the glassagainst the mold (facing the microfeatures) using 52 psi for2 min. Stamping of subsequent layers was done using the same
coated with PCL C. PCL is brought into contact with heated glass to remove themold with PCL remaining in the features F. Mold is applied to the substrate underL pattern on the substrateH. StepsA–E are repeated and themold is rotated beforeeated until the desired scaffold thickness is achieved (four layer scaffold shown).
16/j.msec.2007.04.021

Fig. 3. A. Portion of PCL from raised portions of mold stamped onto a glassslide. B. and C. PDMS mold after removing the excess of PCL accumulated onthe raised features (images illustrate the exposed PDMS and the PCL in therecessed microfeatures).
Fig. 2. A. and B. SEM images of PCL spun onto the PDMS mold exhibiting aporous configuration (lower and higher magnification, respectively).
3D. Gallego et al. / Materials Science and Engineering C xx (2007) xxx–xxx
ARTICLE IN PRESS
protocol, lowering the pressure values and increasing the contacttimes to prevent the scaffolding structure from collapsing.Table 1 shows the pressure and time used for fabrication of eachscaffold layer up to ten layers. A schematic of the MMMprocedure is illustrated in Fig. 1.
2.2. Cell culture experiments
Human osteosarcoma cells — HOS (ATCC, USA) wereseeded on top of the previously sterilized (24 h UV lightexposure) scaffolds at a density of 1×104 cells/ml, and culturedfor 24 and 48 h using Minimum Essential Medium (ATCC,USA) supplemented with 10% fetal bovine serum (ATCC,USA) and 1% antibiotics (ATCC, USA), in a humidifiedincubator (5% CO2, and 37 °C).
For confocal microscopy characterization, the cells werefixed 70% ethanol at −20 °C for 30 min. Postmortem staining ofcell nuclei was carried out with propidium iodine-RNase(Molecular Probes, USA) for 10 min at 4 °C. For SEMevaluation, the scaffolds that were not used for confocalmicroscopy were dehydrated in graded ethanol solutions (70,80, 90, and 100%) and hexamethyldisilazane (Ted Pella, USA)according to the procedure described by Braet et al. [15].
Please cite this article as: D. Gallego et al., Mater. Sci. Eng. C (2007), doi:10.10
3. Results
3.1. Scaffold fabrication
3.1.1. Fabrication of master and PDMS moldSEM characterization showed that the ridges were approx-
imately 10 μm thick and 5 μm wide, with a separation between
16/j.msec.2007.04.021

Fig. 4. SEM micrographs of the single layer pattern (A and B), and multilayer scaffolds (C–F).
4 D. Gallego et al. / Materials Science and Engineering C xx (2007) xxx–xxx
ARTICLE IN PRESS
lines of 45 μm. In general, the master mold exhibited a uniformphotoresist pattern on the surface of the silicon wafer.
The pattern of the master mold was successfully transferredto PDMS stamps. SEM and light microscopy evaluationrevealed a consistent grid pattern of 5 μm wide, 10 μm deepgrooves. The surface topography of the PDMS mold yielded anegative pattern of the master mold.
3.1.2. Scaffold fabricationMulti-layered grid scaffolds with uniform and precise features
were fabricated successfully using the MMM method. The PCLspun onto the PDMSmold formed a uniform coating with porousmicrostructure as shown in Fig. 2. A temperature of 65 °C allowedentire removal of the polymer excess outside the recessedmicrofeatures. Fig. 3A shows the PCL removed from the surface
Fig. 5. SEM images of HOS cells growing in the PCL sca
Please cite this article as: D. Gallego et al., Mater. Sci. Eng. C (2007), doi:10.10
of the mold, and Fig. 3B and C shows the remaining PCL in therecessed portions of the mold. For the first layer, the PCL insidethe microfeatures was effectively transferred onto a glass slideusing the parameters described above. The polymer conserved aconsistent grid pattern on the glass surface. The fabricationparameters (pressure and times)weremodified to stamp up to ninesubsequent layers on top of the first one, forming scaffoldswith upto ten layers of criss‑crossed lines. The mold was rotated approx-imately 30° between each layer. Fig. 4 shows SEM micrographsof the single layer pattern (A and B) and the multilayer scaffolds(C, D, E, and F). The heat introduced during scaffold fabricationpermitted PCL welding where the layers contacted each other(Fig. 4E and F).Overall, the PCL in the scaffolds exhibited a semi-porous texture, with sharp features of about 5 μm wide, 10 μmthick, and 45 μm spacing in between lines.
ffolds. Cell ingrowth is observed after 24 h of culture.
16/j.msec.2007.04.021

Fig. 6. Confocalmicroscopy images ofHOS cells (cell nuclei stainedwith PI-RNase)colonizing 5 (A) and 10 (B) layer scaffolds.
Fig. 7. A. HOS cell growing on patterned PCL. B. HOS cells growing on a flatglass surface. Cell morphology is affected by the substrate.
5D. Gallego et al. / Materials Science and Engineering C xx (2007) xxx–xxx
ARTICLE IN PRESS
3.2. Cell culture experiments
HOS cells were able to adhere and proliferate on the multi-layered scaffolds. Cell ingrowth was observed after 24 h ofincubation (Fig. 5). The confocal microscopy images shown inFig. 6 revealed that HOS cells penetrated several tens ofmicrons down into the scaffold after 48 h of culture. Cellaggregation was noticed in scaffolds with a lower number oflayers (b7 layers). Cells adhered preferentially to the corners ofthe microfeatures. Cell morphology was observed to bedifferent in the scaffolds, comparing with flat PCL or glasssurfaces (Fig. 7).
4. Discussion
The MMM method allowed the fabrication of three-dimensional tissue engineering scaffolds with controlledmicrofeatures at the micro-scale. The fabrication parameters(pressure, time, and temperature) that were selected permit thestamping of multiple layers, conserving the micro-architectureof each individual layer, and avoiding collapsing of thestructure. The layers fused together at the contact points,preventing the scaffold from delaminating. Lower pressurevalues were required as the number of layers in the structureincreased to maintain the structural integrity of the scaffolds.Fig. 8 shows distorted scaffolds fabricated using higher pressureto transfer the second layer. For this reason, the stamping timewas increased to guarantee complete PCL transfer.
Please cite this article as: D. Gallego et al., Mater. Sci. Eng. C (2007), doi:10.10
The porous configuration of the PCL after spin coating canbe attributed to rapid solvent evaporation [16]. The porositydecreases due to thermal processing, but a semi-porous textureis still maintained. The semi-porous PCL can have greatsignificance for tissue engineering applications, since previousresearch has reported that this configuration could be useful forthe loading of different components (e.g. drugs, growth factors,etc.) to influence cell behavior [17].
The scaffolds presented a fully interconnected structure withcontrolled pore size and shape. Pore interconnection facilitatedcell ingrowth [18]. Ten layer scaffolds were less likely topresent cell clumping because they provided higher surface areafor the cells to expand. The consistent architecture of thescaffold (as opposed to the random geometry of traditionalporous scaffolds) is crucial for allowing uniform nutrient–wasteexchange, without limiting cell growth and differentiation [9].Cell morphology in the scaffolds differed from cell morphologyon flat surfaces due to preferential adhesion of the cells to tipsand corners in the microfeatures throughout the scaffold, likelycaused by increased surface energy at these sites [19,20].
The fabrication parameters can be easily modified to obtainscaffolds with different architectures through the MMM method.Pore size, shape, and interconnection degree can be adjusted tosatisfy themorphological requirements of specific tissues [21–23].
16/j.msec.2007.04.021

Fig. 8. SEM images illustrating structure collapsing when higher pressure was used to stamp superior layers.
6 D. Gallego et al. / Materials Science and Engineering C xx (2007) xxx–xxx
ARTICLE IN PRESS
This paper describes the fabrication of multi-layeredscaffolds, where the chemistry and morphology of each layerare maintained throughout the entire structure. The versatility ofthe MMM method could potentially allow the fabrication ofstratified scaffolds, where layers with different chemistry and/orgeometry can be stamped in each step. Such structures mayinduce different cell responses (morphology, metabolic andsynthetic activity, etc) depending on the chemical and physicalproperties of the layer the cells interact with [24–26].
5. Conclusion
Multilayer micromolding was used to fabricate three-dimensional tissue engineering scaffolds from PCL. Thescaffolds presented high porosity, abundant interconnections,and precisely controlled features at the micro-scale. HOS cellsresponded well to the scaffolds. Cell adhesion, proliferation andingrowth were observed. The MMM method could potentiallybe used in the fabrication of scaffolds for a variety of tissueengineering applications.
Acknowledgments
The authors would like to thank Natalia Higuita (Grupo deInvestigación en Ingeniería Biomédica EIA-CES, The OhioMicroMD Laboratory, The Ohio State University) for assistancewith cell culture procedures, and Orin Hemminger (ChemicalEngineering, The Ohio State University) for assisting withconfocal microscopy.
References
[1] F.R. Rose, R.O. Oreffo, Biochem. Biophys. Res. Commun. 292 (2002) 1.
Please cite this article as: D. Gallego et al., Mater. Sci. Eng. C (2007), doi:10.10
[2] D.W. Hutmacher, Biomaterials 21 (2000) 2529.[3] J. Riesle, A.P. Hollander, R. Langer, L.E. Freed, G. Vunjak-Novakovic,
J. Cell. Biochem. 71 (1998) 313.[4] L.E. Freed, A.P. Hollander, I. Matin, J.R. Barry, G. Vunjak-Novakovid,
Exp. Cell Res. 240 (1998) 58.[5] H.W. Kim, S.Y. Lee, C.J. Bae, Y.J. Noh, H.E. Kim, H.M. Kim, J.S. Ko,
Biomaterials 24 (2003) 3277.[6] M. Navarro, S. del Valle, S. Martínez, S. Zeppetelli, L. Ambrosio, J.A.
Planell, M.P. Ginebra, Biomaterials 25 (2004) 4233.[7] Y.C. Kuo, C.Y. Chung, Biotechnol. Prog. 21 (2005) 1708.[8] C.S. Choong, D.W. Hutmacher, J.T. Triffitt, Tissue Eng. 9 (2006) 2521.[9] E. Leclerc, B. David, L. Griscom, B. Lepioufle, T. Fujii, P. Layrolle,
C. Legallaisa, Biomaterials 27 (2006) 586.[10] S.N. Bhatia, C.S. Chen, Biomedical Microdevices 2 (1999) 131.[11] Y. Xia, G.M. Whitesides, Annu. Rev. Mater. Sci. 28 (1998) 153.[12] J. Guan, N. Ferrell, L.J. Lee, D.J. Hansford, Biomaterials 27 (2006) 4034.[13] M.S. Jung, S.O. Jung, D.H. Jung, Y.K. Ko, Y.W. Jin, J. Kim, H.T. Jung,
J. Phys. Chem., B Condens. Mater. Surf. Interfaces Biophys. 109 (2005)10584.
[14] M. Madou, Fundumentals of Microfabrication, CRC Press, Boca Raton,1997.
[15] F. Braet, R. De Zanger, E. Wisse, J. Microsc. 186 (1997) 84.[16] B. Zhao, J. Zhang, X. Wang, C. Li, J. Mater. Chem. 16 (2006) 509.[17] Y. Cao, T.I. Croll, A.J. Oconnor, G.W. Stevens, J.J. Cooper-White,
J. Biomater. Sci., Polym. Ed. 17 (2006) 369.[18] M.K. Moore, E. Jabbari, E.L. Ritman, L. Lu, B.L. Currier, A.J.
Windebank, M.J. Yaszemski, J. Biomed. Mater. Res. A 71 (2004) 258.[19] Y.M. Zhang, P. Bataillon-Linez, P. Huang, Y.M. Zhao, Y. Han, M. Traisnel,
K.W. Xu, H.F. Hildebrand, J. Biomed. Mater. Res. A 2 (2004) 383.[20] J. Deutsch, D. Motlagh, B. Russell, T.A. Desai, J. Biomed. Mater. Res.
53 (2000) 267.[21] V. Karageorgiou, D. Kaplan, Biomaterials 27 (2005) 5474.[22] E. Sachlos, J.T. Czernuszka, Eur. Cell. Mater. 5 (2003) 29.[23] D.W. Hutmacher, J. Biomater. Sci., Polym. Ed. 12 (2001) 107.[24] J.J. Norman, T.A. Desai, Ann. Biomed. Eng. 34 (2006) 89.[25] J. Shim, T.F. Bersano-Begey, X. Zhu, A.H. Tkaczyk, J.J. Linderman, S.
Takayama, Curr. Top. Med. Chem. 3 (2003) 687.[26] R.S. Kane, S. Takayama, E. Ostuni, D.E. Ingber, G.M. Whitesides,
Biomaterials 20 (1999) 2363.
16/j.msec.2007.04.021