ARRHYTHMIAS in ACS PATIENTS · 2019. 2. 14. · Trial design: Patients with an indication for oral...
Transcript of ARRHYTHMIAS in ACS PATIENTS · 2019. 2. 14. · Trial design: Patients with an indication for oral...
-
ARRHYTHMIAS in ACS PATIENTS
PRACTICAL ASPECTS
14 Feb 2562
Roj Rojjarekampai , MD
-
OUTLINES AF VAs
• Epidemiology and
consequences
• Management in acute
and long term phase
• - rate and rhythm
management
• - stroke prevention
• Epidemiology and
pathophysiology
• Acute Management in
Vas related ACS
• : Medications
• : Non-medications
-
STEMI with AF
-
INCIDENCE
-
AF & short-term Mortality in ACS
STEMI NSTEMI
HR = 1.65 HR = 2.30
-
AF & long-term Mortality in ACS
STEMI NSTEMI
HR=2.37 HR =1.67
-
Mortality in AF with MI
OR = 1.46 New AF ; OR =1.37
-
AF and ACS • AF occurred in ACS 10-20 %
[ more frequently in more
severe setting and advance
ages ]
• In pooled analysis of 120,566
pts of STEMI , NSTEMI show
in-hospital AF 8% and 6.4%
respectively
-
AF and ACS • Ass with increase of in-hospital
and long term mortality
• Both pre-existing and new onset
AF increase equivalent mortality rate in ACS patients
-
Management of AF complicating ACS
• Acute Phase
-
Management of AF complicating ACS
• Acute Phase
-
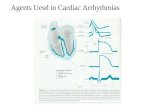
AF in ACS
Rate control
Amiodarone BB , Digitalis
DCCV
Amiodarone
Hemodynamic instability YES NO
-
Management of AF complicating ACS
• Long term phase : focus on stroke prevention
• Triple Therapy [ OAC +ASA+P2Y12inh] should be
considered in all ACS with AF whose CHA2DS2VASc ≥ 2
-
Triple Therapy
-
Triple Therapy vs DAT
-
Triple Therapy vs DAT
-
Trial design: Patients with an indication for oral anticoagulation (OAC) and undergoing DES PCI
were randomized to either 6 weeks or 6 months of triple therapy (aspirin + clopidogrel + OAC
initially, aspirin + OAC indefinitely). Patients were followed for 9 months.
9.8 8.8
0
10
20 Primary endpoint: Composite of death, MI, stent thrombosis, stroke, TIMI major bleeding at 9 months for 6 weeks vs. 6 months of triple therapy: 9.8% vs. 8.8%, HR 1.14, 95% CI 0.68-1.91, p = 0.63
Cardiac death, MI, stent thrombosis, ischemic stroke: 4.0% vs. 4.3%, p = 0.87; TIMI major bleeding: 5.3% vs. 4.0%, p = 0.44
Stent thrombosis: 0.7% vs. 0%
ISAR-TRIPLE trial
N.Sarafoff et al.TCT 2014
Primary endpoints at 9 months
-
Duration of triple therapy
-
PIONEER AF-PCI
ACS 50 % , high stroke risk90%
-
PIONEER AF-PCI:BLEEDING
-
PIONEER AF –PCI :MACE
-
ROW, rest of
world
RE-DUAL PCI: dual antithrombotic therapy with dabigatran after percutaneous coronary
intervention in patients with atrial fibrillation
Dabigatr
an 110
mg dual
therapy
(n=981)
Warfarin triple
therapy
(n=981)
Dabigatran 150
mg dual therapy
(n=763)
Corresponding
Warfarin triple
therapy (n=764)
Age, years, mean 71.5 71.7 68.6 68.8
≥80 (US, ROW), ≥70 (Japan),
%
22.9 22.9 1.0 1.0
-
Full analysis set presented. HRs and Wald CIs from Cox proportional-hazard model. For the dabigatran 110 mg vs warfarin comparison, the model is
stratified by age, non-elderly vs elderly
(
-
ACS c Stenting c AF (high stroke risk)
Strategies of antithrombotic therapy • : triple therapy [ OAC +ASA+P2Y12inh] [ Class I ] for
4-6 weeks [ class II b]then dual therapy [ P2Y12 inh
+ OAC ] until 1 year and OAC monotherapy lifelong
• : Dual therapy [ OAC + P2Y12 inh ] for 1 year [ II a ]
• - VKA + Clop [ or Tica ]
• - NOACS [ Riv 15 mg od or Dab 150 bid ] + Clop
-
VAs
-
VAs and ACS • In STEMI : incidence decrease
from 10 % in fibrinolytic era
[ GUSTO-1] to near 6 % in
primary PCI era [ APEX-AMI]
• 90% occurred in first 48 hrs
• Ass with increase mortality
-
Predictors for VAs
Should be considered at increased risk of
Ventricular Tachyarrhythmias
-
outcome
-
VT/VF in ischemia
1 2
3
-
Myocardial ischemia(1) • Net cellular K loss
• Net cellular Na gain
• Decrease intracellular ATP
content
• Increase intracellular proton
generation ( acidosis )
-
Mechanisms (2) 1)increase RMP [ -80 to -60 mv ]
2)Reduction in AP amplitude ,
velocity, duration
3)Early cellular uncoupling
-
Types of VAs • Acute : VT in ischemic zone [ re-entry]
• : PVC triggers
• : often irregular and degeneration to VF
• Reperfusion and subacute :recovering from brief
duration of ischemia
• : ↑ iCa lead to increase automatism & triggers activity [ DAD ]
• Chronic { > 1 MONTH } mostly from re-entry around scar tissue : stable anatomic circuit MMVT
-
Accerelated Idioventricular Rhythm
BENIGN
-
AIVR ; CAVEAT • AIVR is one of the reperfusion arrhythmias
• AIVR is not specific sign of successful reperfusion Rx
• Most AIVR does not need for specific Rx
• Clinical correlation of patients is essential
• Regular rhythm.
• Rate 50-110 bpm.
• Three or more ventricular complexes.
• QRS complexes >120ms.
• Fusion and capture beats.
https://lifeinthefastlane.com/ecg-library/basics/vt_vs_svt/
-
Treatment of VAs
in ACS
-
• prophylactic AADs not suitable
• optimal revascularization ,early Rx with BB
, balancing Elyte ,sedation, DCCV /
overdrive stimulation should be considered
first
• if AADs is needed ( recurrent VAs related-
ACS after failure available Rx) ,IV
Amiodarone and followed by IV Lidocaine
is reasonable
-
Management of VAs in STEMI
-
Amiodarone vs Lidocaine
-
Management of VAs in STEMI ( 2 )
-
Management of VAs in STEMI ( 3 )
-
Beta Blockers Which , How to start ?
-
Beta-Blocker Heart Attack Trial: impact of
propranolol therapy on ventricular
arrhythmias.
• Trial started in 1978 • Double blinded RCT compared propranolol
[ n=1,926]vs placebo [n=1,921]in pts of 5-21 days
after MI
• Propranolol started at 120 mg /day and titrated to
180-240 mg / day
• Average 25 months F/U
-
BHAT trial
-
BHAT : cause of death
-
IV BB • Limited availibilty of IV BB which recommended for
ACS patients [ IV Metoprolol , IV Propranolol ] in
Thailand
• Ultra-short acting BB ; Esmolol was shown as
effective treatment for refractory VF in OHCA, post
MI patients [ 500 ug/kg IV bolus then 50-100 ug/kg/min infusion IV ]
-
Esmolol in OHCA
-
Esmolol in MI • The first case is about a 47-year-old woman, who came to our attention for anterior myocardial
infarction (STEMI). A primary percutaneous coronary intervention on the left anterior descendant artery was performed in a single vassel disease. Circulation was supported by an intra-aortic balloon pump (IABP) and epinephrine infusion. The left ventricular function was depressed (LVEF 30% at echo). The patient was then stabilized; IABP was removed and epinephrine infusion was stopped. Eight days later, she suffered an episode of sustained monomorphic VT at 220/min perceived as simple palpitations; blood pressure was 73/49 mmHg (85/50 mmHg during sinus rhythm). Lidocaine 100 mg was administered unsuccessfully, so she was sedated and converted to sinus rhythm with 200J synchronized DC shock. From that moment on six other arrhythmic relapses occurred, for a total of seven DC shocks, despite the infusion of amiodaron (20 mcg/kg/min) and lidocaine (20 mcg/kg/min). After the last cardioversion an infusion of esmolol 50 mcg/kg/min was started and the patient stabilized, without any other relapse. There was no mechanical cause for the arrhythmia (Figure 1A) The second case is about a 71-year-old man with an idiopathic dilated cardiomyopathy (LVEF 28% at echo) and normal coronary arteries. He was admitted because of an appropriate ICD intervention. During the hospitalization he suffered another episode of VT refractory to antitachycardia pacing (ATP) and evolving into ventricular flutter treated with DC shock. In the following hours he had incessant episodes of haemodynamically well-tolerated VT, not responding to medical treatment with intravenous lidocaine (100 mg bolus and then infusion 20 mcg/kg/min), intravenous flecainide (1 mg/kg), amiodarone (150 mg plus 300 mg bolus), and several attempts of ATP. The patient was cardioverted eight times with external and internal DC shock. The arrhythmias stopped when esmolol therapy was instituted, with an initial bolus of 40 mg followed by an infusion of 50 mcg/kg/min for two hours. No relapse of ventricular arrhythmia was observed and in the following days (Figure 1B).
Emergency Care Journal 2016; volume 12:6097
-
REVASCULARIZATION
BB , SEDATION
RATE & RHYTHM CONTROL
-
Non – Medication Treatments
-
Overdrive Pacing
-
Cardiac sympathetic denervation
-
Bradyarrhythmias in MI • High grade AVB
• - in acute RCA occlusion : narrow complex ,
good prognosis
• - in acute LAD occlusion : wide complex [ CRBBB
with LAFB ], bad prognosis
• BBB had no longer associated with long term
mortality except in case with new LBBB within 60 minutes after admission
-
STEMI inf wall with CHB
-
STEMI ant wall with CHB
-
Rx of Bradyarrhythmias related ACS
-
CHB and STEMI
US database from 2003-2012 2,273,853 STEMI 2.2% CHB In hosp mortality 20.4 % vs 8.7% OR 2.47
-
In Hospital Moratlity rate In STEMI complicating CHB
-
Medications for AVB ass MI
-
Take Home Messages • 1) Both SVAs and VAs are not uncommon in ACS
patients despite aggressive revascularization
strategy widely used
• 2) DCCV not be delayed in case with arrhythmias
induced hemodynamic worsened
• 3) Beta Blockers must be prescribed in all patients
of ACS if no contraindication , esp in first 48
hours
• 4) Non Pharmacological treatments should be considered in patients who failed for medication