ANTTI SIIKI - Etusivu
Transcript of ANTTI SIIKI - Etusivu

ANTTI SIIKI
Endoscopic Management of Benign Biliary Strictures
Acta Universitatis Tamperensis 2079
AN
TTI SIIK
I Endoscopic M
anagement of B
enign Biliary S
trictures A
UT 2079

ANTTI SIIKI
Endoscopic Management of Benign Biliary Strictures
ACADEMIC DISSERTATIONTo be presented, with the permission of
the Board of the School of Medicine of the University of Tampere,for public discussion in the Small Auditorium of Building M,
Pirkanmaa Hospital District, Teiskontie 35, Tampere, on August 28th, 2015, at 12 o’clock.
UNIVERSITY OF TAMPERE

ANTTI SIIKI
Endoscopic Managementof Benign Biliary Strictures
Acta Universitatis Tamperensis 2079Tampere University Press
Tampere 2015

ACADEMIC DISSERTATIONUniversity of Tampere, School of MedicineTampere University Hospital, Department of Gastroenterology and Alimentary Tract Surgery Finland
Supervised by Reviewed byDocent Johanna Laukkarinen Docent Jorma HalttunenUniversity of Tampere University of HelsinkiFinland FinlandDocent Juhani Sand Docent Sari VenesmaaUniversity of Tampere University of Eastern FinlandFinland Finland
The originality of this thesis has been checked using the Turnitin OriginalityCheck service in accordance with the quality management system of the University of Tampere.
Copyright ©2015 Tampere University Press and the author
Cover design byMikko Reinikka
Layout bySirpa Randell
Distributor:[email protected]://verkkokauppa.juvenes.fi/
Acta Universitatis Tamperensis 2079 Acta Electronica Universitatis Tamperensis 1573ISBN 978-951-44-9869-5 (print) ISBN 978-951-44-9870-1 (pdf )ISSN-L 1455-1616 ISSN 1456-954XISSN 1455-1616 http://tampub.uta.fi
Suomen Yliopistopaino Oy – Juvenes PrintTampere 2015

CONTENTS
Abstract ...................................................................................................................................... 7
Tiivistelmä ................................................................................................................................. 9
List of original communications ........................................................................................ 11
Abbreviations ......................................................................................................................... 12
1 Introduction ................................................................................................................ 15
2 Review of the literature ............................................................................................ 182.1 Biliary anatomy ............................................................................................. 182.2 Benign biliary strictures .............................................................................. 18
2.2.1 Pathophysiology ................................................................................ 182.2.2 Incidence ............................................................................................. 222.2.3 Classification ...................................................................................... 26
2.3 Radiologic imaging of biliary strictures ................................................... 272.3.1 Magnetic resonance imaging .......................................................... 282.3.2 Other imaging modalities ............................................................... 29
2.4 Endoscopic retrograde cholangio-pancreatography (ERCP) ............... 302.4.1 Cannulation and cholangiography ............................................... 302.4.2 Endoscopic cholangioscopy ............................................................ 31
2.5 Complications of ERCP .............................................................................. 322.5.1 Incidence ............................................................................................. 342.5.2 Mortality ............................................................................................ 362.5.3 Risk factors ......................................................................................... 36
2.6 Obtaining and analysing samples from biliary strictures ..................... 392.6.1 Brush samples and cytologic analysis ............................................ 392.6.2 Flow cytometry, digital image analysis and FISH ..................... 402.6.3 Cholangiography and endoscopy guided biopsies ..................... 402.6.4 Visually guided biopsies .................................................................. 41
2.7 Serum diagnostics ......................................................................................... 422.8 Non-endoscopic treatment of benign biliary strictures ........................ 43
2.8.1 Percutaneous management ............................................................. 432.8.2 The role of surgery ............................................................................. 44

2.9 Endoscopic treatment and outcome of biliary strictures by aetiology 452.9.1 Post-cholecystectomy ....................................................................... 452.9.2 Post-liver transplantation ............................................................... 472.9.3 Chronic pancreatitis ......................................................................... 492.9.4 Primary sclerosing cholangitis ....................................................... 512.9.5 Autoimmune cholangitis ................................................................ 532.9.6 Other causes of BBS ......................................................................... 54
2.10 Treatment with endoscopic stents ............................................................. 542.10.1 Plastic stents ....................................................................................... 552.10.2 Covered self-expandable stents ...................................................... 562.10.3 Biodegradable stents ......................................................................... 59
3 Aims of the study ...................................................................................................... 62
4 Materials and methods ............................................................................................ 634.1 Study I: ERCP success rates and complications in a Finnish
central hospital ............................................................................................. 634.2 Study II: Initial experience of SpyGlass cholangioscopy in biliary
strictures secondary to sclerosing cholangitis ......................................... 634.3 Study III: Meta-analysis comparing covered self-expanding metal
stents and multiple plasic stents in benign biliary strictures ................ 644.4 Study IV: Protein expression in benign biliary strictures before
and after treatment with metal and biodegradable biliary stents ....... 674.5 Study V: Biodegradable biliary stent in the endoscopic treatment
of cystic duct leak after cholecystectomy. ................................................. 69
5 Statistics ...................................................................................................................... 72
6 Ethical aspects ........................................................................................................... 73
7 Results ......................................................................................................................... 747.1 Study I: ERCP success rates and complications in a Finnish
central hospital .............................................................................................. 747.2 Study II: Initial experience of SpyGlass cholangioscopy in biliary
strictures secondary to sclerosing cholangitis ......................................... 777.3 Study III: Meta-analysis comparing covered self-expanding metal
stents and multiple plasic stents in benign biliary stricture ................. 797.4 Study IV: Protein expression in benign biliary strictures before
and after treatment with metal and biodegradable biliary stents ....... 817.5 Study V: Biodegradable biliary stent in the endoscopic treatment
of cystic duct leak after cholecystectomy ................................................. 83

8 Discussion ................................................................................................................... 84
9 Summary and conclusions ...................................................................................... 89
10 Future perspectives ................................................................................................... 90
Acknowledgements .............................................................................................................. 92
References ............................................................................................................................... 94
Original communications ................................................................................................. 109


ABSTRACT
Benign biliary strictures (BBS) develop most commonly secondary to previous surgery or chronic pancreatitis (CP). The molecular level pathogenesis of BBS as well as the response to biliary stents is poorly understood. The role of endoscopy (endoscopic retrograde cholangio-pancreatography, ERCP) in the management of BBS is crucial not only in terms of diagnostic tissue sampling, but also as the first line of treatment. This thesis summarises the clinically most relevant aspects of the current endoscopic diagnostic and treatment methods of BBS in adults.
For the first time, the outcome of ERCP procedures in a Finnish central hospital was investigated. The study showed that acceptable success rate and complication frequency can be achieved even in a low-volume unit, when the procedures are all assigned to a few endoscopists, and the indication and treatment are carefully considered for each patient. In relatively infrequent BBS, the proper assessment of the risks and benefits of the endoscopic interventions is especially important.
In the evaluation of indeterminate biliary strictures, single-operator cholangioscopy (SOC) has proven helpful by facilitating biopsies under direct visual control. However, its role has been unclear in primary sclerosing cholangitis (PSC), which is a progressive stenosing autoimmune biliary disease carrying a risk for cholangiocarcinoma with challenging diagnostics. We investigated the feasibility and safety of Spyglass cholangioscopy (Boston Scientific, MA, USA) in PSC patients and obtained encouraging results on this novel reported experience in Finland.
Although covered self-expandable metal stents (CSEMS) are widely used in extrahepatic BBS with good clinical experience, no long-term results supporting their use have been available until recently. Therefore we performed a systematic review with a meta-analysis comparing these methods in various aetiologies of BBS. We found that CSEMS may be superior to multiple plastic stents in the treatment of BBS related to CP.
Biodegradable biliary stents (BDBS) could potentially overcome the drawbacks associated with plastic and metal stents, rendering numerous endoscopy sessions for stent removal or exchange unnecessary. We first evaluated the expression of healing-related proteins in an experimental BBS and found that the changes in the protein pattern occurring during stricture formation seem to return closer to the level of an

intact bile duct after treatment with BDBS than with CSEMS. With these promising results, we undertook a study on the clinical use of endoscopically inserted BDBS, for which a device for endoscopic insertion has not previously been available. An excellent clinical outcome was achieved with the first endoscopic insertion of BDBS that was initially tested in the setting of post-operative bile leak and is reported herein.
From these abovementioned studies we conclude that 1) ERCP performance and complication rate is at an acceptable level in a Finnish central hospital, 2) peroral cholangioscopy may contribute to the diagnostics of PSC, 3) CSEMS use is well justified in BBS secondary to CP, 4) protein expression pattern of BBS reflecting the stricture development is different after BDBS and CSEMS therapy and 5) in the future the drawbacks of conventional endoscopic stent therapy may be circumvented by BDBS. The endoscopic diagnostics and therapy of BBS are continuously developing, warranting critical examination of the novel methods in terms of effectiviness and patient safety.

9Endoscopic Management of Benign Biliary Strictures
TIIVISTELMÄ
Hyvänlaatuisten sappitieahtaumien yleisimmät syyt ovat leikkauksen jälkitila ja pitkäaikainen haimatulehdus. Suun kautta tähystimellä tehtävä endoskopia (endo-skooppinen retrogradinen kolangio-pankreatografia, ERCP) on nykyään ensisijainen tutkimus- ja hoitomenetelmä. Se mahdollistaa diagnostiikan näytteenotolla ahtau-masta ja hoitotoimenpiteet muovisten- tai itsestään laajenevien metalliverkkostenttien (CSEMS) avulla. Väitöskirja vetää yhteen hyvänlaatuisten sappitiehtaumien nykyai-kaisen diagnostiikan ja hoidon.
Tämän väitöskirjan ensimmäinen osatyö kuvasi ERCP-aineiston suomalaisessa kes-kussairaalassa. Sen tulosten perusteella pienessäkin yksikössä voidaan päästään kan-sainvälisestikin hyväksyttäviin onnistumis- ja komplikaatiolukuihin, kunhan ERCP toiminta keskitetään pienelle määrälle osaavia endoskopisteja. Vastaavaa komplikaatio-lukuja selvittävää työtä suomalaisesta keskussairaalasta ei ole aiemmin julkaistu.
Toisessa osatyössä selvitettiin uuden ERCP:n yhteydessä tehtävän sappitietähys-tyksen eli kolangioskopian (SOC) käyttöä sklerosoivaan kolangiittiin (PSC) liittyvis-sä ahtaumissa, joissa syövän esiastetasoisten muutosten varhaisella diagnostiikalla on suuri vaikutus ennusteeseen. Epäselvien sappitieahtaumien diagnostiikan on aiem-min todettu tarkentuvan SpyGlass –kolangioskopian (Boston Scientific, MA, USA) avulla, koska läpivalaisulla otettujen solunäytteiden lisäksi saadaan videokuvan avulla kohdennettuja koepaloja. Tutkimuksessa todettiin, että kolangioskopiassa otettavat näytteet saattavat tuoda lisäinformaatiota PSC-diagnostiikkaan. Tämän pienen poti-lasmateriaalin perusteella Spyglass -kolangioskopia ja kohdennettut koepalat vaikuttaa olevan turvallinen menetelmä PSC:ssa yhdistettynä jo käytössä oleviin kuvantamiseen, sappitien harjairtosolunäytteisiin, virtaussytometriaan ja verikokeisiin.
Kolmannessa osatyössä verrattiin muovi- ja metallistenttien paremmuutta sappitie-ahtaumissa kirjallisuuskatsauksen ja meta-analyysin avulla. Metallistenttejä käytetään potilaille hyvänlaatuisissa ahtaumissa, vaikka vertailevia tutkimuksia perinteisesti käy-tettyihin muovistentteihin on julkaistu vasta hiljattain. Tuloksemme puoltavat metal-listenttien käyttöä pitkäaikaiseen haimatulehdukseen liittyvissä sappitieahtaumissa, joissa niillä saadaan muovistentteihin verrattuna turvallisesti parempia onnistumislu-kuja vähemmällä endoskopioiden määrällä.

10 Antti Siiki
Uusilla biohajovilla sappitiestenteillä voitaisiin välttää perinteisiin stentteihin liit-tyvät toistuvat endoskopiat stenttien vaihtamiseksi ja poistamiseksi. Sappitieahtaumi-en kehittymisen ja biohajoavien stenttien aiheuttaman kudosvasteen tutkimiseksi neljännessä osatyössä koeläimille aiheutettiin sappitieahtauma, jota hoidetttiin joko metallistentillä tai biohajoavalla stentillä. Proteiinien, kuten galectin-2 ja annexin-A4 esiintyminen muuttui selvästi ahtaumassa verrattuna koskemattomaan sappitiehen. Toisaalta biohajoavat stentit vaikuttivat palauttavan proteiinien esiintymistasot lähem-mäs normaalia sappitietä ja ne saattaisivat siten olla parempi hoitomuoto hyvänlaatui-sissa sappitieahtaumissa. Viidennessä osatyössä raportoitiin ensimmäinen potilasta-paus, jossa asennettiin endoskooppisesti biohajova sappitiestentti sappirakon poiston jälkeisen sappivuodon hoidossa. Yhdessä aiempien tutkimusten kanssa tuloksemme uuden instrumentin käytettävyydestä ja potilasturvallisuudesta puoltavat jatkotutki-muksia biohajoavilla stenteillä hyvänlaatuisissa sappitieahtaumissa.
Väitöskirjan yhteenvetona todetaan, että 1) ERCP toimenpiteet aiheet ja komp-likaatioluvut ovat asianmukaisella tasolla suomalaisessa keskussairaalassa, 2) endo-skooppinen kolangioskopia on käyttökelpoinen, täydentävä menetelmä myös sklerosoi-vassa kolangiitissa, 3) pitkäaikaiseen haimatulehdukseen liittyviä ahtaumia kannattaa hoitaa päällystetyillä metallistenteillä, 4) proteiinien ilmeneminen muuttuu sappitie-ahtauman muodostuessa ja kudosreaktio voi jopa olla suotuisampi biohajoavilla kuin metallistenteillä sekä 5) ensimmäiset käytännön kokemukset biohajovien stenttien käytöstä ihmisen sappitiessä ovat lupaavia ja ne saattavat olla endoskooppisen ahtau-manhoidon tulevaisuutta. Diagnostiikan tarkentumisella ja turvallisimman menetel-män valinnalla on olennainen merkitys potilaiden hoidossa.

11Endoscopic Management of Benign Biliary Strictures
LIST OF ORIGINAL COMMUNICATIONS
1. ERCP procedures in a Finnish community hospital: a retrospective analysis of 1207 cases. A Siiki, A Tamminen, T Tomminen, P Kuusanmäki. Scand J Surg 2012;101:45–50.
2. Spyglass single operator peroral cholangioscopy seems promising in the evalua-tion of primary sclerosing cholangitis related biliary strictures: a case series and initial experience of a tertiary referral center. A Siiki, I Rinta-Kiikka, T Koivisto, K Vasama, J Sand, J Laukkarinen. Scand J Gastroenterol 2014;49:1385–90
3. Covered self-expanding metal stents may be preferable to plastic stents in the treatment of chronic pancreatitis related biliary strictures; a systematic review comparing two methods of stent therapy in benign biliary strictures. A Siiki, M Helminen, J Sand, J Laukkarinen. J Clin Gastroenterol. 2014;48:635–43.
4. Protein expression in benign biliary strictures before and after treatment with metal and biodegradable biliary stents. A Siiki, R Jesenofsky, M Löhr, I Nord-back, M Kellomäki, J Mikkonen, H Gröhn, J Sand, J Laukkarinen. Submitted.
5. Biodegradable biliary stent in the endoscopic treatment of cystic duct leak after cholecystectomy: the first case report and review of literature. A Siiki, I Rin-ta-Kiikka, J Sand, J Laukkarinen. Laparoendosc Adv Surg Tech. 2015; 25(5): 419–22.

12 Antti Siiki
ABBREVIATIONS
ASA American Society of AnesthesiologistsIAC immunoglogulin associated cholangitis IAH immunoglobulin associated hepatitisIAP immunoglobulin associated pancreatitisBBS benign biliary strictureBDBS biodegradable biliary stentCA19-9 carbohydrate antigen 19-9CBD common bile duct (ductus choledochus)CCA cholangiocarcinomaCCY cholecystectomyCEA carcino-embryonal antigenCHD common hepatic duct (ductus hepaticus communis)CP chronic pancreatitisCRP C-reactive proteinCSEMS covered self-expanding metal stentCT computed tomographyDIA digital image analysisERC endoscopic retrograde cholangiographyERCP endoscopic retrograde cholangio-pancreatographyEST endoscopic sphincterotomyEUS endoscopic ultrasoundFCSEMS fully covered self-expanding metal stentPET positron emission tomographyFISH Fluorescence in situ hybridisationFNA fine needle aspirateHJ hepatico-jejunostomy anastomosis, e.g. roux-en-yi.v. intravenouslyIgG4 immunoglobulin-4KHKS Kanta-Häme Central Hospital, Hämeenlinna, Finland

13Endoscopic Management of Benign Biliary Strictures
LC laparoscopic cholecystectomyLFT liver function tests (enzymes)LT orthotopic liver transplantationm-Amsterdam modified Amsterdam classification of PSCmPS multiple plastic stents (polyethylene)MRI magnetic resonance imagingMRCP magnetic resonance cholangiopancreatographyPLA polylactidePCSEMS partially covered self-expandable metal stentPD pancreatic ductPDX polydioxanonePEP post-ERCP pancreatitisPS plastic stent (polyethylene)PSC primary sclerosing cholangitisPSHP Pirkanmaa Hospital District, Tampere, FinlandPTD percutaneous transhepatic cholangiography and drainageRCT randomised controlled trialSEMS self-expanding metal stentSOC single-operator peroral cholangioscopySOD dysfunction of sphincter of OddiUCSEMS uncovered self-expanding metal stentWBC white blood cell count

14 Antti Siiki

15Endoscopic Management of Benign Biliary Strictures
1 INTRODUCTION
Benign biliary strictures (BBS) are a rare entity of biliary diseases having diverse aetiologies and natural courses requiring different management strategies, most of which include endoscopic retrograde cholangio-pancreatography (ERCP) (Figure 1A-B). Any biliary stricture eventually leading to biliary obstruction requires primarily endoscopic interventions both to diagnose the type of stricture and to prevent secondary biliary cirrhosis. At the time when biliary obstruction is observed, typically due to elevated liver function tests (LFT) or acute cholangitis, the aetiology of the stricture is often anything but clear. Strictures which are initially indeterminate turn out to be malignant far more frequently than benign (Enochsson et al 2010). Management of biliary strictures typically requires co-ordinated multi-disciplinary management by surgeons, endoscopists, gastroenterologists, radiologists as well as pathologists (Baron and Davee 2013; Chan and Telford 2012; Shimada et al. 2012).
The incidence of BBS in Finland is not known. In the literature, BBS is the indication for ERCP in 3–7% of cases (Testoni et al. 2010; Wang et al. 2009). However, endoscopic BBS management necessitates more than one procedure and frequencies vary between centres (Baron and Davee 2013; Enochsson et al. 2010). The most common aetiologies of BBS are post-operative strictures as well as chronic pancreatitis (CP) and primary sclerosing cholangitis (PSC); less frequent causes may include autoimmune disorders, chemotherapy, stone disease and infections (Chan and Telford 2012).
The risk for complications associated with ERCP makes it crucial to always weigh up the indications of the procedure against the diagnostic and therapeutic benefit. The incidence of post-ERCP pancreatitis (PEP) is 2–5% with an overall complication rate of 5–15% (Andriulli et al. 2007; Enochsson et al. 2010). While CP patients are not prone to acute PEP, in PSC the risk is doubled to up to 7–8% (Cotton et al. 2009; Ismail et al. 2012; von Seth et al. 2015). Research is required to assess the benefits and risks for informing the patients, quality control and for the evaluation of the effectiviness and safety of any novel methods (Baron and Davee 2013; Lorenzo-Zuniga et al. 2014; Rey et al. 2014). In addition to highly specialised tertiary centres in Finland, ERCPs are also performed in the low-volume non-academic central hospitals, whose ERCP practice has not so far been described.

16 Antti Siiki
The primary aim in the diagnostics of indeterminate strictures is to exclude malignancy. In addition to radiologic imaging, cytology samples are often needed to confirm a diagnosis of BBS. This is especially challenging in PSC, where disease progression often leads to ERCP in order to find dysplasia before the development of cholangiocarcinoma (CCA) (de Valle et al 2012). Endoscopic brush cytology, flow cytometry, cholangiography image and serum markers are used in combination to estimate the risk of CCA or to plan the timing of liver transplantation (LT) (Halme et al. 2012; Lindberg et al. 2002). The current methods are far from perfect and a promising new diagnostic method could be single-operator peroral cholangioscopy (SOC) with visually guided biopsies, which
Figure 1B. A drawing of a duodenoscope introduced in the descending part of the duodenum. The duodenal papilla and the bile duct are cannulated with a guide wire in the right hepatic duct. For clarity, the most of the stomach is removed to reveal common bile duct (CBD) and illustrate the pancreas and the pancreatic duct (PD). The human biliary tract converges from the intrahepatic biliary ducts into a common hepatic duct (CHD) and after joining with the cystic duct, into the common bile duct (CBD), draining downstream via the duodenal papilla into the duodenum.
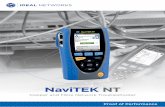
Figure 1A. A flexible duodenoscope (left) used in ERCP (endoscopic retrograde cholangio-pancreatography) with the Spyglass single-operator peroral cholangioscopy device (Boston Scientific, MA, USA) attached (right).

17Endoscopic Management of Benign Biliary Strictures
has been proven beneficial in indeterminate biliary strictures (Draganov et al. 2011; Kalaitzakis et al. 2012; Ramchandani et al. 2011; Rey et al. 2014; Woo et al. 2014). In PSC, data on SOC use is scarce, but it seems that visual image and guided biopsies may be helpful in diagnostics and in detecting changes in PSC related strictures (Awadallah et al. 2006; Tischendorf et al. 2007; Arnelo 2015). The molecular background of stricture pathophysiology, the natural course and response to stent therapy in BBS are little investigated issues that may offer answers for choosing the right type of stent, for the development of new diagnostic or prognostic markers of BBS or for finding target molecules for future drug-eluding biodegradable biliary stents (BDBS) (Lorenzo-Zuniga et al. 2014; Tokar et al. 2011).
Endoscopic treatment of BBS has evolved from dilation and plastic stents (PS) to the use of covered self-expanding metal stents (CSEMS) (Baron and Davee 2013; Deviere et al. 2014; Kaffes and Liu 2013; Perri et al. 2011; Van Boeckel et al. 2009). Strictures with various aetiologies, e.g. secondary to PSC, LT or CP require different treatment strategies (Baron and Davee 2013; Dumonceau et al. 2011; Kaffes and Liu 2013). While intrahepatic strictures often require balloon dilation followed by PS insertion, extrahepatic strictures may also be treated with CSEMSs (Baron and Davee 2013; Perri et al. 2011). The post-operative strictures at the biliary confluence especially are treated with single or preferably with increasing numbers of multiple plastic stents (mPS) with good results (Costamagna and Boškoski 2013). In short, while treatment with the inexpensive PS is technically challenging associated with numerous stent exchanges and stent clogging as a major disadvantage, CSEMSs are currently ten times costlier, need removal and are best suitable for strictures below the biliary confluence (Dumonceau et al. 2011). However, despite a large number of cohort studies, controlled trials comparing mPSs and CSEMSs have been presented only recently of strictures secondary to liver transplantation and chronic panreatitis (Haapamaki et al. 2015; Kaffes et al. 2014). The most recent promising alternative to CSEMSs are BDBSs, which do not necessitate removal, but of which no clinical experience in endoscopic use has so far been reported (Lorenzo-Zuniga et al. 2014).
This thesis summarises the clinically most relevant aspects of the current endoscopic diagnostic and treatment methods of BBS in adults. The aim was (1) to assess the complication and success rates of ERCPs in a Finnish central hospital, (2) to study the usefulness of SOC in PSC diagnostics, (3) to determine an optimal stent therapy for the treatment of BBS, (4) to investigate the protein expression in a surgically induced biliary stricture and in response to CSEMS and BDBS and (5) to report the feasibility and safety of a novel endoscopically inserted BDBS.

18 Antti Siiki
2 REVIEW OF THE LITERATURE
2.1 Biliary anatomyThe human biliary duct consists of an extrahepatic part and an intrahepatic part, which are lined with biliary epithelial cholangiocytes (Tietz and Larusso 2002). Intrahepatic biliary tree converges through the right and left main hepatic ducts through the hepatic confluence into the common hepatic duct (CHD). Further downstream the cystic duct from the gallbladder joins the CHD and continues as a common bile duct (CBD) to drain through the duodenal papilla (papilla Vateri) into the duodenum. In most cases, except in pancreas divisum, the pancreatic duct drains into the duodenum through the papilla (Figure 1B). This tiny structure functions as a natural access route to the biliary duct and to the pancreatic duct (PD) and plays a crucial role in the success rate and complications of ERCP (Halttunen et al. 2014). The boundary between the intra- and extrahepatic biliary ducts in the proximal part of the CHD below the biliary confluence is also clinically important because it determines the methods that may be used in surgical or endoscopic treatment (Costamagna and Boškoski 2013; Strasberg and Helton 2011).
2.2 Benign biliary strictures
2.2.1 Pathophysiology
The pathophysiologic changes occurring in the biliary epithelium in BBS are imperfectly understood in the majority of aetiologies (Tietz and Larusso 2002). There are few studies on the molecular and protein level development of strictures and also on their response to treatment methods. The most common aetiologies for BBS include post-operative strictures and strictures associated with chronic pancreatitis (CP) or autoimmune diseases.

19Endoscopic Management of Benign Biliary Strictures
Post-operative strictures
Post-operative strictures may appear either immediately after cholecystectomy (CCY) if a surgical clip or a suture is accidentally placed to compress the bile duct or up to years later by ischaemic injury and fibrosis (Strasberg and Helton 2011). In post-operative injury the underlying mechanism is typically a compromise in arterial supply e.g. after CCY, CBD exploration or anastomotic strictures after orthotopic liver transplantation (LT) (Akamatsu et al. 2011; Gunji et al. 2006; Strasberg and Helton 2011). While the liver parenchyma and the intrahepatic part of the biliary tree are supplied by the circulation of the portal vein and hepatic artery, the vascular supply of CHD and CBD is only arterial and mostly axial, running on both sides of the duct. About 60% of arterial perfusion of CBD comes from the gastroduodenal artery and only 30–40% downwards from the hepatic artery, making the preservation of circulation crucial in surgery (Gunji et al. 2006). On the other hand, cholangiocytes are vulnerable to ischaemia, resulting in ischaemic cholangiopathy and eventual stricture formation (Noack et al. 1993).
Strictures secondary to liver transplantation
The most common type of liver transplantation is the orthotopic deceased donor transplantation with duct-to-duct anastomosis (LT) (Aberg et al. 2011). The post-LT strictures are divided to two distinct categories with different aetiology and outcome; anastomotic and non-anastomotic strictures, the latter of which has shown a far less favourable response to treatment (Williams and Draganov 2009). Less used options are living donor transplantation and reconstruction with roux-en-Y hepatico-jejunal anastomosis (HJ), with which anastomotic strictures are associated more commonly than with LT with duct-to-duct anastomosis (Aberg, Isoniemi and Hockerstedt 2011; Akamatsu et al. 2011; Damrah et al. 2012; Tarantino et al. 2012a; Williams and Draganov 2009).
An anastomotic biliary stricture developing typically during the first year after LT is the most common complication (Akamatsu et al. 2011; Graziadei et al. 2006; Verdonk et al. 2006). Anastomotic strictures account for up to 80% of post-LT strictures and are typically short and located in the middle portion of the CBD (Baron and Davee 2013; Williams and Draganov 2009). A post-operative biliary leak is a risk factor for later anastomotic stricture, likewise small duct size (Akamatsu et al. 2011). Early anastomotic strictures resulting from oedema and inflammation respond best to endoscopic therapy within the first few months (Pasha et al. 2007; Verdonk et al. 2006). Late onset

20 Antti Siiki
anastomotic strictures presenting later than six months after LT result from fibrosis and scarring necessitate prolonged therapy (Pasha et al. 2007; Verdonk et al. 2006).
The risk factors for non-anastomotic strictures are devascularisation, prolonged ischaemia time, hepatic artery thrombosis, immunologic incompatibility, chronic and acute rejection episodes as well as advanced recipient age and profoundly impaired liver function (Akamatsu et al. 2011). Especially in PSC, disease recurrence may be the cause of a non-anastomotic stricture (Chan and Telford 2012). Non-anastomotic strictures typically occur earlier than anastomotic strictures, and may be diffusely located in the hilum, occasionally progressing to multiple sites intrahepatically but they may be concomitant to anastomotic strictures or be located in the CHD (Chan and Telford 2012; Verdonk et al. 2007). The multi-focality of strictures, associated sludge and recurrence of the underlying liver disorder are the reasons for the poor prognosis (Chan and Telford 2012).
Chronic pancreatitis
BBS may also result from external compression of the CBD as in CP, where fibrosis and calcifications in the head of pancreas compress the intrapancreatic biliary duct (Figure 1B). A tumour-like process associated with CP in the head of the pancreas may sometimes be indistinguishable from pancreatic cancer (Abdallah et al. 2007). Due to the increased risk of pancreatic cancer in CP related CBD strictures, an adequate radiologic diagnostic work-up and adeaquate sampling during ERCP should be performed before biliary stenting. This is particularly important in patients belonging to the high-risk groups: age over 50 years, female gender, presenting with jaundice, pancreatic exocrine insufficiency or hereditary pancreatic cancer or present without pancreatic calcifications (Dumonceau et al. 2012).
Primary sclerosing cholangitis
PSC is an autoimmune-mediated chronic, cholestatic progressive liver disease of unknown aetiology characterised by inflammation and fibrosis affecting both intra- and extrahepatic bile ducts with LT as the only curative treatment (Chapman et al. 2010; Eaton et al. 2013). The inflammation of the biliary epithelium causes gradual fibrotic and multi-focal stenosis, which is macroscopically hard to differentiate from malignancy (Awadallah et al. 2006; Chapman et al. 2010; Tischendorf et al. 2006). Small-duct PSC is a better prognosis variant occurring in 9% of all PSC patients and characterised by cholestatic and histologic features of PSC without the typical

21Endoscopic Management of Benign Biliary Strictures
cholangioraphy findings (Boonstra et al. 2013; Ehlken and Schramm 2013). About 4% of PSC patients have an overlap syndrome: diagnostic features from both PSC and immunoglobulin-4 (IgG4) associated autoimmune hepatitis (IAH) (Boonstra et al. 2013; Chapman et al. 2010; Eaton et al. 2013).
Immunoglogulin associated strictures
The pathogenesis of the autoimmune mediated and IgG4 related diseases such as IgG4 associated cholangitis (IAC) is unknown (Okazaki et al. 2014). The patients commonly have concomitant autoimmune pancreatitis (IgG4 -associated pancreatitis, IAP), which is another poorly understood IgG4-related systemic disorder frequently characterised by obstructive jaundice in intrapancreatic CBD with or without pancreatic mass (Okazaki et al. 2014). A biliary obstruction is caused by either direct involvement of the biliary duct epithelium or by external compression in IAP (Okazaki et al. 2014). The response to steroid treatment is a strong indicator of correct diagnosis; when the stricture does not resolve and the stent cannot be removed, and when LFT, serum IgG4 and CA19-9 do not decrease, the presence of malignancy should be reconsidered (Boonstra et al. 2014). Both IAC and IAP are easily confused with PSC or cancer and differential diagnosis may not be possible (Chan and Telford 2012).
Other causes
Less frequent causes of BBS (Table 1) include e.g. strictures secondary to transarterial chemoembolization and radiofrequency ablation, commonly used percutaneously in hepatocellular carcinoma (Baron and Davee 2013). A gallstone impacted in the gallbladder neck or in the cystic duct (Mirizzi syndrome) may induce an inflammatory stricture in the CHD sometimes associated with a biliary fistula (Chan and Telford 2012). Similarly, long-standing stones in the biliary duct may occasionally cause a

22 Antti Siiki
stricture in the CBD due to scarring; however, a malignant stricture may promote stone formation upstream (Chan and Telford 2012).
Table 1. Aetiology of benign biliary strictures
IatrogenicCholecystectomyOrthotopic liver transplantBiliary-enteric anastomosis, e.g. hepaticojejunostomyERCPPercutaneous transarterial chemoembolization and radiofrequency ablation for hepatocellular carcinomaPercutaneous ethanol injectionEndoscopic sclerotherapy of duodenal ulcerRadiation therapy Chemotherapy
IschaemicHypotensionHepatic artery thrombosis or stenosisProlonged transplant organ ischemiaPortal biliopathy
InfectiousRecurrent pyogenic cholangitis (oriental cholangiohe-patitis)ParasitosisGranulomatous: tuberculosis, histoplasmosisHuman immunodeficiency virus
InflammatoryMirizzi syndromeCholedocholithiasisChronic pancreatitisPrimary sclerosing cholangitisImmunoglobulin IgG4 associated cholangiopathyVasculitis
OtherAbdominal trauma
Strictures in surgically altered anatomy
The biliary strictures in surgically altered anatomy, e.g. in biliary-enteric roux-en-Y HJ anastomosis require special instrumentation and require a learning curve that is different from that of ERCP (Baron and Davee 2013). Balloon-assisted endoscopes allow access to the anastomosis with consequent cholangiography and interventions; success rates of up to 75–90% have been reported in balloon dilation or stent insertion via single-balloon or double-balloon endoscopes in surgically altered anatomy (Itokawa et al. 2014; Saleem et al. 2010).
2.2.2 Incidence
The most common and clinically most relevant causes of BBS are surgical injuries, particularly after open or laparoscopic cholecystectomy (LC), followed by CP related strictures (Baron and Davee 2013). The various aetiologies of BBS are presented in Table 1 as described in the literature (Baron and Davee 2013; Chan and Telford 2012; Costamagna and Boškoski 2013). Estimates of the incidence of BBS may be based on the numbers of ERCPs performed for BBS and the incidence of the most common aetiologies.

23Endoscopic Management of Benign Biliary Strictures
According to an Italian multicentre study, BBS was an indication in 3.5% (Testoni et al. 2010) while in a Chinese tertiary centre in 7.1% of ERCPs (Wang et al. 2009). In a Swedish national register study, the most common finding in ERCPs was CBD stone in 37% followed by biliary stricture in 30% of ERCPs, the aetiology of which was perioperatively considered malignant, benign and unclear in 47%, 15% and 38% of cases respectively (Enochsson et al. 2010). While 4000–4500 ERCPs are yearly performed in Finland (THL 2012), an estimate of the number of ERCPs for BBS may thus be 200–300 per year.
A bile duct injury occurs in about 0.5–1.5% of patients after CCY (Barbier et al. 2014; Tornqvist et al. 2012; Vitale et al. 2008). The majority of these injuries are recognised early post-operatively and consist mostly of bile leaks, isolated strictures being rare (Karvonen et al. 2011; Tornqvist et al. 2012; Vitale et al. 2008). CBD injury is accompanied by vascular injury in an estimated 25% of cases (Strasberg and Helton 2011). The most common type of injury immediately after surgery is a Strasberg A leak (Figure 2) from the cystic duct or the aberrant duct that is amenable to treatment with ERCP and stent insertion, often with a percutaneous drain (Karvonen et al. 2011; Strasberg and Helton 2011; Wu and Linehan 2010). The rationale in biliary leak management is to ensure the downstream flow of bile facilitating closure of the leak site (Karvonen et al. 2011).
When a complex biliary injury (Strasberg D-E) is excluded and reconstructive surgery is not necessary, the majority of simple injuries as well as later strictures may be treated endoscopically with ERCP, EST and stent insertion (Karvonen et al. 2011; Strasberg and Helton 2011; Wu and Linehan 2010). It has been suggested that even in complex lesions, ERCP may be attempted as the first-line effort to locate and classify the injury and, if successful, to avoid the problems associated to surgical repair (Wu and Linehan 2010).

24 Antti Siiki
A biliary stricture typically located in the CHD or proximal CBD is the most common late complication of CCY, presenting up to 15 years after surgery (Barbier et al. 2014; Shanbhogue et al. 2011). The incidence of surgically reconstructed post-CCY biliary strictures is 0.4% (Waage and Nilsson 2006). In Finland approximatelly 8,000 CCYs are performed annually with 88% of operations being laparoscopic (THL 2012). The number of strictures resulting from CCY treated or attempted to treat endoscopically is unknown. In suspected late post-CCY strictures, other benign causes such as CBD stones are encountered in over 20% and occult malignancy in up to 7% (Vitale et al. 2008).
The incidence of anastomotic and non-anastomotic strictures occurring after LT is 10–12% and 2–20% respectively (Akamatsu et al. 2011; Graziadei et al. 2006; Verdonk et al. 2006; Verdonk et al. 2007). ERCP is the first choice of treatment also offering diagostic yield in duct-to-duct anastomotic strictures (Akamatsu et al. 2011; Williams
Figure 2. Strasberg’s classification (A–D, E1–E5) of biliary injury after cholecystectomy. Type A bile leak (star) from the stump of a cystic duct or an aberrant cystic duct (duct of Luschka), B an occluded right posterior sectoral duct or an aberrant right sided hepatic duct, C a bile leak from right posterior sectoral duct or aberrant right sided hepatic duct, D a lateral injury to the main bile duct, E1 and E2 transection of the common hepatic duct more or less than 2 cm from the biliary confluence, E3 communication with right and left duct only intact, E4 confluence interrupted and E5 main duct injury associated with aberrant right sectoral hepatic duct involvement.

25Endoscopic Management of Benign Biliary Strictures
and Draganov 2009). In Finland 50-60 LTs are performed yearly (Aberg et al. 2011; THL 2012).
A biliary stricture develops secondary to an inflammatory process in the head of the pancreas in 10–30% of patients with CP, the incidence of which is at least 6-10/100,000 (Jakobs and Riemann 1999; Lankisch et al. 2002; Lohr et al. 2013). CP itself being a progressive inflammatory disease with pancreatic exocrine and endocrine insufficiency, malnutrition, pain, pancreatic duct stenosis or stones and pancreatic cyst formation as leading features, the majority of the CP related biliary stenoses are asymptomatic or intermittent. The clinical presentation of CP related biliary stricture fluctuates, with exacerbations and remissions as well as transient or asymptomatic cases being characteristic. Secondary biliary cirrhosis is rare and acute cholangitis occurs in only 10% of patients with varying degree of severity (Abdallah et al. 2007). While transient self-limiting jaundice due to acute pancreatitis or a pseudocyst in the head of the pancreas warrants primary conservative treatment or pseudocyst drainage, persistent biliary obstruction with elevated LFT, progression of a stricture, associated with cholangitis or CBD stones necessitates endoscopy as the first line of therapy (Abdallah et al. 2007; Dumonceau et al. 2012; Lohr et al. 2013).
The incidence of PSC is 1.2/100,000 and prevalence 16/100,000 (Lindkvist et al. 2010). It is increasingly common in the Nordic countries, accounting for 1–15% of ERCPs (Enochsson et al. 2010; Ismail et al. 2012). Patients with PSC are predominantly men, the median age at the time of diagnosis is 38-39 years, and there is an associated inflammatory bowel disease in two thirds of cases (Boonstra et al. 2013; Lindkvist et al. 2010). Eventual development of CCA and biliary cirrhosis with consequent liver failure are the most feared complications of PSC (Chapman et al. 2010) with respectively 30% and 7–14% of cases leading to LT or hepato-biliary cancer at 10-year follow-up (Burak et al. 2004; de Valle et al. 2012).
Up to 30–50% of PSC patients develop a dominant biliary stricture over the years and these are most commonly benign; in a series of 230 patients only 19% of strictures in PSC were caused by CCA (Charatcharoenwitthaya et al. 2008; Ehlken and Schramm 2013). However, PSC associated CCA tumours typically emerge in the dominant strictures of liver hilum. Up to 26% of these dominant strictures have been reported to eventually lead to CCA (Chapman et al. 2012; Tischendorf et al. 2006). The mean survival in patients with a dominant stricture is 13 years, compared to 23 years in those with diffuse intrahepatic disease (Chapman et al. 2012). However, the definition of a dominant stricture in PSC has not been established. Despite the strong association of dysplasia with development of CCA (dysplasia-carcinoma sequence) in PSC, the incidence of CCA does not correlate with the duration of the inflammation (Burak et al. 2004). The incidence of hepato-biliary cancer is 180-fold and CCA over 800-fold

26 Antti Siiki
in PSC patients compared to that in general population (de Valle et al. 2012) with a yearly incidence of 0.6–1.2% for CCA (Burak et al. 2004; Charatcharoenwitthaya et al. 2008). The estimated median survival of patients from diagnosis until LT or PSC -related death is 21 years (Boonstra et al. 2013). In Finland PSC is the most common indication for LT, with 10-year patient survival after transplantation being 84% (Aberg et al. 2011). The majority of CCAs arise within a few years after the diagnosis of PSC, making it critical to have a surveillance protocol and to exclude dyplasia or malignancy at the diagnosis of PSC for early potentially curative treatment with LT (Boberg et al. 2006; Boonstra et al. 2013; Boyd et al. 2014; Ehlken and Schramm 2013; Lindkvist et al. 2010). Differentiating biliary strictures secondary to PSC from malignancy and excluding dysplasia is one of the most challenging issues in hepato-biliary endoscopy. ERCP forms the cornerstone for obtaining samples and treating dominant strictures (Eaton et al. 2013).
2.2.3 Classification
The most commonly used Bismuth s classification (Bismuth and Majno 2001) of BBS is based on the level of stenosis and extent of reconstruction surgery required (Figure 3). It may also be used to describe acute biliary injuries (Bismuth and Majno 2001). The degree of post-CCY biliary injury is often graded with Strasberg’s classification (Strasberg et al. 1995), which involves both bile leaks and strictures according to similar principles as those in Bismuth’s classification (Figure 2). A more detailed classification system for post-CCY biliary injuries has been developed to also consider vascular involvement (Bektas et al. 2007).
Figure 3. Bismuth’s classification of BBS, graded I-V is based on the level of stricture and the extent of reconstructive surgery required: Type I stricture with a common hepatic duct stump longer than 2 cm, II with stump shorter than 2 cm, III with only the ceiling of the biliary confluence intact, IV with the biliary confluence interrupted and V with a stricture of common hepatic duct associated with a stricture of a separate aberrant right branch.

27Endoscopic Management of Benign Biliary Strictures
In PSC specifically, the radiological progression of biliary duct involvement is graded with the Amsterdam classification (Majoie et al. 1991) presented in Table 2. A modified Amsterdam (m-Amsterdam) classification may be used in PSC surveillance in determining the severity by summing the intra- and extrahepatic grades with the exception that intrahepatic grade I equals two points and slighter change in ductal irregularity and variation in calibre equals one point on the m-Amsterdam scale, which therefore ranges between 0 and 8 (Rajaram et al. 2001; Boyd et al. 2014).
The chances of successful ERCP and consequent endoscopic diagnosis and therapy depend on whether or not the stricture can be passed with guide wire; an impassable intra- or extrahepatic stricture or total discontinuity of the bile duct requires surgery (Baron and Davee 2013; Bismuth 2003).
Table 2. Radiologic grading of intrahepatic and extrahepatic changes in cholangiography image in PSC according to the Amsterdam classification (Majoie et al. 1991, Rajaram et al. 2001)
Type of duct involvement Cholangiographic abnormalitiesIntrahepatic0IIIIII
NormalMultiple strictures; normal calibre of bile ducts or minimal dilationMultiple strictures, saccular dilations, decreased arborizationOnly central branches filled despite adequate filling pressure, severe pruning
Extrahepatic0IIIIIIIV
NormalSlight irregularities of duct contour, no stenosisSegmental stenosisStenosis of almost entire length of ductExtremely irregular margin; diverticulum-like out-pouchings
2.3 Radiologic imaging of biliary stricturesWhen biliary obstruction is suspected from visible icterus and/or elevated liver LFT, the diagnosis of BBS is often initiated with radiologic imaging. In practice, the first imaging modality is often transabdominal ultrasound followed by magnetic resonance imaging (MRI) and magnetic resonance cholangiography (MRCP) or contrast enhanced computed tomography (CT). The long, irregular, asymmetric, abruptly ending strictures are traditionally considered more often malignant than the smooth, symmetric tapering strictures often present in benign disease. The findings from MRI or CT require cytologic or histologic confirmation and treatment by ERCP or surgery as a therapeutic intervention for a biliary stricture, except in cases where surgery is required for an evident malignant tumour (Shanbhogue et al. 2011).

28 Antti Siiki
2.3.1 Magnetic resonance imaging
MRCP is the current standard in the diagnostics of biliary strictures (Katabathina et al. 2014; Shanbhogue et al. 2011). Performed with heavily T2-weighted sequences, it offers the advantage of non-invasive cholangiography imaging of the bilary tract beyond a tight stricture enabling evaluation of the liver parenchyma and abdominal viscera as well as providing an assessment in the immediate post-operative phase and in cases of bilio-enteric anastomosis (Katabathina et al. 2014; Shanbhogue et al. 2011). The present day MRCP is excellent in the diagnostics of a biliary obstruction; however, the accuracy in differentiation between benign and malignant strictures varies widely, from 30 to 98% (Katabathina et al. 2014). In the evaluation of post-operative strictures, MRCP combined with contrast enhanced MRI of the liver is the definitive investigation method of choice, showing not only the level of obstruction, arterial stenosis or thrombosis, possible biliary leak but also excluding occult malignancy as well as revealing any recurrence of primary liver disease after LT (Shanbhogue et al. 2011). MRCP is also widely used in the diagnosis of PSC, where diagnostic sensitivity of 80–88% and specificity of 87–99% have been reported (Shanbhogue et al. 2011).
MRCP is currently considered to be the optimal non-invasive method for the evaluation of suspected post-LT complications, with an accuracy of 95% (Baron and Davee 2013; Chan and Telford 2012; Williams and Draganov 2009). The radiologic appearance of post-LT strictures differs in anastomotic or non-anastomotic cases and the type of anastomosis (Shanbhogue et al. 2011). While dilated donor bile ducts are an unreliable sign of a stricture in LT patients, the diagnosis of post-LT strictures is based on a combination of symptomatic or asymptomatic elevated LFT, contrast enhanced MRI as well as Doppler ultrasound to exclude arterial thrombosis (Chan and Telford 2012). In suspected post-CCY complication, a trans-abdominal ultrasound is often followed by MRCP to evaluate fluid collections, the location of surgical clips, CBD stones and site of the bile leak (Shanbhogue et al. 2011; Wu and Linehan 2010).
A typical radiologic finding seen in MRI in CP related biliary stricture is intra- and extrahepatic bile duct dilatation of varying degrees with a smooth tapering stricture in the intrapancreatic part of the CBD; evidence of chronic pancreatitis such as parenchymal atrophy, dilated main pancreatic duct or pseudocysts support the diagnosis (Shanbhogue et al. 2011).
The diagnosis of PSC is based on characteristic multi-focal “beaded” strictures with alternating segments of dilated or normal duct findings in MRCP or ERCP when secondary causes of sclerosing cholangitis have been excluded (Chapman et al. 2010; Ehlken and Schramm 2013; Shanbhogue et al. 2011). Although MRCP does not

29Endoscopic Management of Benign Biliary Strictures
reliably differentiate CCA from PSC, the sensitivity and specificity of MRCP in PSC diagnosis are well over 80% (Shanbhogue et al. 2011).
In IAP a characteristic bulky and sausage-like pancreas may be seen in MRI or abdominal CT (Chan and Telford 2012; Shanbhogue et al. 2011). The biliary stricture associated with IAC is typically located in the distal CBD but diffuse intra- and extrahepatic biliary strictures or perihilar strictures in isolation or combination may also be encountered (Shanbhogue et al. 2011).
In strictures associated with chemotherapy MRI may reveal a stricture reminiscent of PSC, typically affecting the CHD with little intrahepatic involvement; the distal CBD is also usually spared from stricture formation secondary to separate arterial supply (Shanbhogue et al. 2011). Radiologic diagnosis of Mirizzi’s syndrome with MRI and CT is usually straightforward, but as in any indeterminate biliary stricture, the possibility of occult malignancy has to be considered (Shanbhogue et al. 2011).
2.3.2 Other imaging modalities
Multiphase contrast enhanced CT scan is a standard imaging method in acute abdominal pain and trauma, in the evaluation of complications of surgery and in the assessment of tumour spread. In indeterminate biliary strictures CT scan is helpful in detecting the underlying cause of the obstruction, occult malignancy, complications such as cholangitis, fluid collections and arterial stenosis or thrombosis as well as in showing lymphadenopathy and lesions suspectible to metastasis (Shanbhogue et al. 2011). A contrast-enhanced CT scan is often used to complement and in combination with MRI in post-CCY and post-LT situations to evaluate liver ischaemia, vascular anatomy and arterial thrombosis (Shanbhogue et al. 2011; Wu and Linehan 2010). The CT scan is also a primary method in the evaluation of CP to assess parenchymal and morphological changes, such as calcifications and pseudocysts or tumour-like lesions, while MRI is used to show morphology of the pancreatic duct (Abdallah et al. 2007).
Endoscopic ultrasound (EUS) offers the advantage of guided fine needle aspirate (FNA) in the diagnosis of indeterminate strictures and CCA. When EUS and FNA may be used in combination with ERCP, improved accuracy may be achieved in the diagnosis of BBS (Shanbhogue et al. 2011). However, EUS is highly user-dependent in diagnosing malignancy (Shanbhogue et al. 2011). Although the benefits of EUS with FNA over ERCP and brush samples are the most apparent in pancreatic masses where a malignant biliary obstruction is suspected, it is also useful in other indeterminate biliary strictures and suspected CCA (Weilert et al. 2014).

30 Antti Siiki
FDG positron emission tomography (PET), the current disadvantages of which are price and availability, appears to be extremely accurate in differentiating between benign and malignant biliary strictures, with sensitivity and specificity of 92% (Shanbhogue et al. 2011). Inflammation in PSC may cause a false positive finding, and thus the role of PET is not established in PSC, despite the recent encouraging findings on its utility in excluding CCA (Eaton et al. 2013; Sangfelt et al. 2014).
2.4 Endoscopic retrograde cholangio-pancreatography (ERCP)The first reports on ERCP in humans appeared in literature in the 1970s (Cotton 1972). An experimental endoscopic cannulation or duodenal papilla with subsequent pancreatography was documented even earlier (McCune, Shorb and Moscovitz 1968). The first ERCP in Finland was performed in the University Hospital of Oulu in 1978, followed by the Surgical Hospital in Helsinki in 1979. The University Hospitals of Helsinki and Tampere set up the ERCP practice soon afterwards in the early 1980s. The first Finnish reports of ERCP concentrated on complications (Halme et al. 1999; Nordback and Airo 1988). The wider use of ERCP and understanding of the complications resulted in the avoidance of purely diagnostic procedures (Cotton et al. 1991; Freeman et al. 1996). Since then ERCP has established its position as a diagnostic and therapeutic procedure of the pancreato-biliary duct system. It is performed perorally with a flexible side-viewing duodenoscope, the tip of which includes an elevator to control instruments in the working channel and is steerable in vertical and horizontal directions. The cannulation, i.e. access through the papilla to the desired duct by a guide wire facilitating further interventions, continues to be the critical part of the procedure (Halttunen et al. 2014). In addition to the procedure itself, ERCP practice entails the interpretation of radiologic images beforehand and the analysis of tissue samples as well as subsequent decision-making, which are a good example of a multi-disciplinary approach. ERCP currently forms a well-established basis for the diagnosis and treatment of biliary strictures as well as selected cases of post-operative bile leaks (Shanbhogue et al. 2011; Karvonen et al. 2011; Baron and Davee 2013).
2.4.1 Cannulation and cholangiography
In a difficult cannulation, a variety of methods may be used to open the papillary orifice and access the biliary duct according to the endoscopist’s preference (Halttunen et al. 2014). Precut sphincterotomy with a needle-knife sphincterotome or fistulotomy (Gullichsen et al. 2005), pancreatic sphincterotomy (Halttunen et al. 2009) or double-

31Endoscopic Management of Benign Biliary Strictures
guide wire technique (Gyokeres et al. 2003; Huang et al. 2015) may be used separately or in combination (Halttunen et al. 2014). If cannulation fails, a second attempt is usually more succesful when the inflammation of papilla has subsided (Palm et al. 2007). A prophylactic pancreatic stent may be introduced over the guide wire in the PD to reduce the risk for PEP (Dumonceau et al. 2014). In urgent cases of failed ERCP, a PTD (percutaneous transhepatic cholangiography and drainage) is typically used in malignancy as a bridge to surgery or in other cases to facilitate the next ERCP attempt with rendezvous technique associated with a high success rate and low risk of complications (Swahn et al. 2013). Rendezvous ERCP may be used as an option to pass a tight stricture allowing balloon dilation and stent therapy (Costamagna et al. 2001).
A successful biliary cannulation is followed by the cholangio- or pancreatography image produced by a radioopaque contrast injection and x-ray. A diagnostic cholangiography image reveals the intrahepatic biliary tree and extrahepatic bile duct often crucial for the diagnosis of stricture or stones. The cholangiography itself is not adequate for the diagnosis of indeterminate biliary strictures (Chen et al. 2011). However, the morphology of the stricture in cholangiography may give clues to the aetiology; when a smooth and tapering, “birds-beak-like” or “hour-glass-like” narrowing in the CBD may indicate CP, a blunt-ended duct should lead to a suspicion of pancreatic cancer (Abdallah et al. 2007; Shanbhogue et al. 2011). Although the cholangiographic findings in ERCP are not reliable in differentiating PSC or CCA from IAC; IgG4 associated strictures may be longer and more segmental with a more frequent affision of the distal CBD than in PSC (Baron and Davee 2013; Kalaitzakis et al. 2011). After cholangiography, an endoscopic sphincterotomy (EST) and necessary interventions may be performed; tissue sampling with brush, sweeping and flushing of debris with extraction balloon, stone management, balloon dilation and insertion of stents. SOC instruments are also introduced through the working channel of the duodenoscope over the guide wire (Chen and Pleskow 2007).
2.4.2 Endoscopic cholangioscopy
The endoscopic cholangioscopy instruments have evolved from the prototypes of the early 1980s to mother-baby-scope double-operator procedures and eventually to present-day single-operator cholangioscopy (Urakami 1980). The currently widely used SOC with SpyGlass instruments (Boston Scientific Corp, MA, USA) offers a visual image inside the biliary duct and a controlled way to take biopsies for histologic analysis (Chen 2007). SOC includes a probe that is inserted through the working channel of a duodenoscope containing channels for the optical fibre transmitting video image,

32 Antti Siiki
irrigation and instruments such as mini-biopsy forceps or stone management. With the turning wheels of the instrument the tip of the probe can be adjusted in four directions. In addition to visually guided biopsies and stone management, SOC may be used for selective access through an otherwise impassable stricture e.g. in post-CCY strictures or PSC (Kuroda et al. 2010; Arnelo 2015).
The visual image showing smooth biliary mucosa without neovascularization and homogeneous granular mucosa is characteristic of benign disease. The presence of irregularly dilated tortuous “tumour vessels’’ at the strictures is indicative of malignancy (Kim et al. 2000). In a recent retrospective Chinese study, high sensitivity and negative predictive values have been proposed for visual assessment (Woo et al. 2014). In other studies, SOC image without tissue samples has been considered unreliable (Awadallah et al. 2006). In addition, the intraobserver agreement of visual image provided by SOC in indeterminate strictures in terms of hyperplasia and ulceration has also been questioned (Sethi et al. 2014). Especially in PSC, visual evaluation may be unreliable because of the multi-focality and inflammatory and fibrotic nature of the stricture, making predicting malignancy in PSC harder than in patients with non-PSC strictures that have an otherwise normal biliary epithelium (Awadallah et al. 2006; Arnelo 2015). Interestingly, indeterminate filling defects seen in previous ERCPs may occasionally turn out to be biliary stones without a stricture in SOC (Ramchandani et al. 2011). Biliary stones unseen in cholangiography may be encountered in SOC in up to 30% of PSC patients with symptom-relief after the stone management (Awadallah et al. 2006, Arnelo 2015).
2.5 Complications of ERCPLike any surgical or invasive procedure, ERCP and sphincterotomy carry a risk for severe and potentially fatal complications. Thus adequate pre-operative investigations, a careful consideration of procedure indications and alternative management options as well as keeping up procedure volume are always warranted (Freeman 2012; Silviera et al. 2009). The rate of complications and that of procedure success are connected; when cannulation is difficult and advanced attempts are needed to access the biliary duct, the complication rate is higher, especially for PEP (Halttunen et al. 2014). However, the term complication is sometimes used interchangeably in the literature for adverse event to underline that a successful procedure with a mild complication may sometimes be preferable to a failed procedure attempt without any obvious complication (Freeman 2012). A stent clogging, for instance, may be considered merely an adverse event than a complication during stent therapy. Although a critical analysis of own complications

33Endoscopic Management of Benign Biliary Strictures
is a part of quality management (Anderson et al. 2012), it is often neglected and only few studies are available from non-academic centres (Colton and Curran 2009; Garcia-Cano Lizcano et al. 2004).
The present day endoscopic techniques allow such complex procedures to be performed that major surgical or percutaneous interventions, both with considerable morbidity, mortality and costs, may often be avoided (Freeman 2012). The studies assessing typical ERCP related complications (PEP, haemorrhage, cholangitis, perforation) grade complications according to a well-established classification (Table 3) as mild, moderate or severe according to duration of hospitalisation and need for interventions (Cotton et al. 1991). Post ERCP pancreatitis is defined as a new-onset or increasing abdominal pain and elevation of serum amylase three times above normal at 24 hours after the procedure combined with pancreatitis-related hospitalisation (Cotton et al. 1991). Early ERCP related complications are recorded during the first 30 days after the procedure, with most events occurring within a few days, although cases of delayed bleeding, for example, may occur (Christensen et al. 2004; Silviera et al. 2009).
Table 3. Definitions of complications of ERCP used in research. An intensive care unit admission or a death after the ERCP grades the complication as severe. Any other complication is graded according to duration of hospitalisation. C: Celsius (Cotton et al. 1991)
Mild Moderate SeverePancreatitis Clinical pancreatitis, amylase
at least 3 times normal at more than 24 h after the pro-cedure, requiring admission or prolongation of planned admission to 2–3 d
Pancreatitis requiring hospi-talisation of 4–10 d
Hospitalisation for more than 10 d, pseudocyst, or intervention (percutaneous drainage or surgery)
Haemorrhage Clinical (i.e. not just endos-copic) evidence of bleeding, haemoglobin drop more <3g, no transfusion
Transfusion (4 units or less), no angiographic intervention or surgery
Transfusion 5 units or more, or intervention (angiographic or surgical)
Perforation Possible, or only slight leakage of fluid or contrast, treatable by i.v. fluids and suction <3 d
Any definite perforation treated medically 4–10 d
Medical treatment of more than 10 d, or intervention (percutaneous or surgical)
Infection (cholangitis)
Temperature >38 C for 24–48 h
Febrile or septic illness requiring more than 3 d of hospital treatment or percu-taneous intervention
Septic shock or surgery

34 Antti Siiki
2.5.1 Incidence
Two systematic reviews report the incidence of PEP to be 3–7% with cholangitis, haemorrhage and perforation occurring at rate of 1–3%, 1–2% and 0.5% respectively (Andriulli et al. 2007; Silviera et al. 2009). The reported incidence of other adverse events such as cardio-pulmonary and thromboembolic events varies between 0.5 and 10% (Christensen et al. 2004; Cotton et al. 2009; Wang et al. 2009). Cholecystitis may occur in 0.5% of cases (Silviera et al. 2009). Technical problems, e.g. trapping of a stone extraction basket are occasional curiosities (Wang et al. 2009). In the largest register study so far of nearly 38,000 ERCPs in Sweden, the incidence of pancreatitis was 5.6% and the overall complication rate was 12% (Enochsson et al. 2013).
In the literature it is usually assumed that in in-patient procedures the complications mainly emerge during the surveillance period of some 24 hours on the hospital ward and that patients with complications arising later or in outpatient procedures are eventually admitted to the same unit. There is, however, variation in the length and thoroughness of the follow-up; studies presenting the highest figures of overall complications often have a close 30-day follow-up protocol instead of relying on data gathered during primary hospital stay. Furthermore, the early studies may include diagnostic ERCPs and procedures performed with quite different equipment than that in present-day ERCPs in centres with varying expertise and procedure volume. Additionally, the studies on complications exclude procedures with already sphincterotomised papilla and thus repeated ERCPs for stent exchange, for example, which are characteristic of BBS management. The incidence of complications according to the key studies from the 2000s is summarised in Table 4.

35Endoscopic Management of Benign Biliary Strictures
Table 4. Key-studies of 30d-ERCP complications from the 2000s. Prosp: prospective. Retro: retrospective study. PEP: post-ERCP pancreatitis. Bleed: haemorrhage. Perf: perforation. Chol: cholangitis. Compl: overall complications. Mort: ERCP -related mortality rate. *The study reported only severe or fatal complication
Percentages (%)N Country Setting PEP Bleed Perf Chol Comp Mort
(Masci et al. 2001) 2462 Italy Prosp 1.8 1.2 0.6 0.6 4.9 0.1(Barthet et al. 2002) 1159 France Retro 3.5 1.2 1.8 1.2 7.7 0.9(Vandervoort et al. 2002) 1223 USA Prosp 7.2 0.8 0.1 0.7 11 0.002(Christensen et al. 2004) 1177 Denmark Prosp 3.8 0.9 1.1 5.0 16 1.0(Garcia-Cano Lizcano et al. 2004) 507 Spain Retro 5.5 1.6 1.6 1.6 11 0.8(Palm et al. 2007) 602 Finland Retro 4.8 0.6 0.8 0.5 7.3 0.5(Williams et al. 2007) 4561 UK Prosp 1.6 1.3 0.4 1.0 5.0 0.4(Salminen et al. 2008) 2788* Finland Retro 0.2 0.2 0.2 0.1 0.8 0.1(Colton and Curran 2009) 805 USA Prosp 3.2 0.6 0.1 0.8 5.0 0(Cotton et al. 2009) 11497 USA Prosp 2.6 0.3 0.1 0.3 4.0 0.06(Wang et al. 2009) 2597 China Prosp 4.3 1.7 0.2 1.4 7.9 0.3(Enochsson et al. 2010) 11074 Sweden Prosp 2.7 0.9 0.3 NA 5.9 NA(Kapral et al. 2012) 13513 Austria Prosp 4.2 3.6 0.6 1.4 10. 0.1
The effect of procedure volume on ERCP success rate has been discussed in several studies. While it is obvious that personnel’s experience improves ERCP outcomes, comparisons of complication rates between centres may be misleading due to different indications, case-mix and success rates; high-volume endoscopists generally attempt higher-risk and more challenging cases, but despite that have a higher success rate of cannulation (Freeman 2012). In a few multi-centre studies, high-volume tended to be associated with higher success rates of cannulation and slightly elevated complication rates (Freeman et al. 1996; Kapral et al. 2008; Loperfido et al. 1998). In the Swedish nationwide study, a tendency for more frequent haemorrhage and contrast extravasation was observed when low-volume was defined as less than 200 procedures a year (Enochsson et al. 2010). Interestingly, in the same study the rate of PEP was increased in high-volume centres, probably secondary to the frequency of more complex procedures involving e.g. manipulation of the PD in the high volume referral centres (Enochsson et al. 2010). In an Italian multi-centre study the PEP rate did not differ between low- and high-volume centres or between expert- and non-expert operators, even though the high-volume centres performed more complex procedures (Testoni et al. 2010). In a study from the United Kingdom no difference was found in the overall post-ERCP complications between endoscopists with differing case loads or hospital type, although a decrease in PEP rate in the university hospitals was observed (Williams et al. 2007).

36 Antti Siiki
While it is hard to define a minimum volume to maintain optimal proficiency, estimates of 50–100 cases for routine biliary therapy and 200–250 per year for advanced pancreatic techniques have been proposed (Freeman 2012). Concentrating procedures on a few endoscopists, referral of the most complex cases to specialised centres and optimising the risk and benefit for the individual patient according to endoscopist’s expertise are the ways to control the risks (Freeman 2012). No description of ERCP practice or complication figures has so far been published on Finnish low-volume hospitals.
2.5.2 Mortality
The majority of adverse events are self-containing and graded as mild or moderate in 87–99% of cases (Christensen et al. 2004; Cotton et al. 2009; Freeman et al. 2001; Testoni et al. 2010; Vandervoort et al. 2002; Wang et al. 2009). Mortality due to ERCP is rare (Table 4) being 0.3–0.5%. However, PEP and perforation may carry 3% and 9% risks of death respectively (Andriulli et al. 2007). Mortality due to severe PEP has reportedly been as high as 29% (Testoni et al. 2010). In a study of nearly 3,000 ERCPs at a Finnish university hospital, the incidence of severe complications was 0.8% with related mortality of 0.08% (Salminen et al. 2008). It has been previously noted that overall 30-day mortality (also other than ERCP-related) is predictably much lower when the indication is a CBD stone (1.5%) compared to a malignant stricture (15%) (Enochsson et al. 2010). Furthermore, the mortality rate is strongly associated with comorbidities (ASA classification, American Society of Anesthesiologists), being 0.2% and 5% in ASA1 and 4% and 21% in ASA3 with CBD stones and malignancy respectively (Enochsson et al. 2010). The overall all-cause mortality rate 30 d from ERCP is up to 1.4–6%, reflecting the frequency of co-morbidites in unselected patients undergoing ERCP (Christensen et al. 2004; Colton and Curran 2009; Williams et al. 2007).
2.5.3 Risk factors
The risk factors of ERCP complications have been investigated in several studies and it seems that the risk for pancreatitis especially is associated with the manipulation of the papilla or pancreatic duct in a difficult cannulation (Enochsson et al. 2010; Halttunen et al. 2014). In Freeman’s pioneering studies with PEP incidence 5–7%, the risk factors in multivariate analysis included young age, precut sphincterotomy, prior PEP, suspected dysfunction of Sphincter of Oddi (SOD) as ERCP indication, female gender, normal

37Endoscopic Management of Benign Biliary Strictures
bilirubin, absence of chronic pancreatitis, balloon dilation of the biliary sphincter and difficult cannulation (Freeman et al. 1996; Freeman et al. 2001). These results have been substantiated with small variations over the years, but difficult cannulation with several attempts and contrast injections to the PD seems to be the main procedure-related factor increasing the risk for PEP (Cotton et al. 2009; Kapral et al. 2012; Testoni et al. 2010; Vandervoort et al. 2002; Wang et al. 2009; Williams et al. 2007). A periampullary diverticulum has reportedly also been associated with an increased risk for PEP (Wang et al. 2009). Precut sphincterotomy, performed to facilitate cannulation in difficult situations, has been noted to be an independent risk factor for PEP (Freeman et al. 1996; Freeman et al. 2001; Testoni et al. 2010; Vandervoort et al. 2002). While young patients with SOD or a history of PEP seem to be prone to pancreatitis (Christensen et al. 2004; Cotton et al. 2009; Freeman et al. 1996; Freeman et al. 2001; Kapral et al. 2012; Testoni et al. 2010; Vandervoort et al. 2002; Williams et al. 2007), older patients with a history of CP and thus with less potential for pancreatic inflammation are at less risk (Cotton et al. 2009; Freeman et al. 2001; Vandervoort et al. 2002). The use of prophylactic pancreatic stents, pre-procedural rectal administration of non-steroidal anti-inflammatory drugs and the rendezvous cannulation technique have been shown to reduce the risk for PEP (Dumonceau et al. 2014; Swahn et al. 2013).
Predictably, haemorrhage seems to be related to visible bleeding during ERCP, sphincterotomy as well as comorbidities, haemodialysis or anticoagulation treatment and urgent procedures (Cotton et al. 2009; Enochsson et al. 2013; Kapral et al. 2012; Williams et al. 2007). It has been noted that the incidence of haemorrhage is nowadays lower than proposed by older series, perhaps due to the development of CBD stone therapy and diathermy equipment decreasing the risk of bleeding related to EST (Enochsson et al. 2010).
Perforations are associated with cases with sphincterotomy, difficult cannulation, precut sphincterotomy, previous surgery involving biliary diversions, or malignancy (Christensen et al. 2004; Cotton et al. 2009; Kapral et al. 2012; Williams and Draganov 2009). Cholangitis is more likely if biliary access failed or drainage was insufficient, and in men (Christensen et al. 2004; Freeman et al. 1996; Kapral et al. 2012). In the prevention of cholangitis, complete and successful biliary drainage is the most important issue; routine prophylactic antibiotics are recommended in patients with incomplete biliary drainage, in PSC and in LT patients (Anderson et al. 2012; Freeman 2012).
The role of patient’s age and co-morbidities in relation to complications other than PEP is contradictory: while background illnesses and age over 65 years have been related to increased cardio-pulmonary complications (Kapral et al. 2012) as well as severe or

38 Antti Siiki
fatal complications (Cotton et al. 2009) earlier, no such connection was substantiated in the large prospective Danish study with a close follow-up (Christensen et al. 2004).
As an indication for ERCP, BBS and PSC carry a 10% and 21% risk for PEP, which is high compared to the 4% risk in unselected ERCP patients (Testoni et al. 2010). Simple procedures like exchange of biliary stent (Cotton et al. 2009) and stone removal (Garcia-Cano Lizcano et al. 2004) are associated with fewer complications than complex procedures (Cotton et al. 2009; Enochsson et al. 2010; Testoni et al. 2010; Vandervoort et al. 2002). In a Finnish study of PSC related ERCP complications, the rate of PEP was 9.2% in patients with an intact papilla and 2.7% in patients with a previous EST (Ismail et al. 2012). In Sweden, the risk for PEP and cholangitis has been reported to have more than doubled in PSC patients compared to other ERCPs, any advese events occurring in 18% and 7% and PEP in 8% and 3% of the PSC and non-PSC patients respectively (von Seth et al. 2015). In PSC, acute cholangitis occurs in 1–7% and perforation in 0.6–0.7% of procedures, but incidences of mild perforations (contrast extravasation) as high as 6% have been reported (Etzel et al. 2008; Ismail et al. 2012; Navaneethan et al. 2015b; von Seth et al. 2015). A difficult cannulation and insertion of the guide wire more than twice into the PD also greatly increased the PEP risk in PSC (Ismail et al. 2012; Navaneethan et al. 2015b; von Seth et al. 2015). Much lower PEP risks of 1.2% and cholangitis of 2.4% in PSC patients have also been reported, possibly explained by the large proportion of previously sphincteromised papillas and liberal use of prophylactic pancreatic stents (Navaneethan et al. 2015b). The PEP rate has been 5–9% and the cholangitis rate 5% in studies specifically assessing the risks of stricture management in PSC (Kaya et al. 2001; Ponsioen et al. 1999).
According to studies on adverse events of SOC, complications occur in 3–19% of cases and are seldom severe and consist most commonly of cholangitis, PEP and post-sphincterotomy bleeding (Chen et al. 2011; Draganov et al. 2011; Kalaitzakis et al. 2012; Manta et al. 2013; Woo et al. 2014; Lubbe et al. 2015). The complications seen with SOC have been proposed to be associated with female sex, previous ERCP, and hilar or multifocal strictures, but to have no relation to patient’s age, sex, pre-existing cholangitis or duration of the procedure of over 30 minutes (Chen et al. 2011; Kalaitzakis et al. 2012). Interestingly, most of the adverse events involved acute cholangitis and no cases of PEP occurred (Kalaitzakis et al. 2012). This perhaps indicates a different complication pattern than in ERCP without SOC and may explain why previous EST appeared as a protecting factor. PSC is not a known risk factor for SOC related complications, but biliary cannulation may be more difficult in PSC (Halttunen et al. 2009; Kalaitzakis et al. 2012). In the most recent study of SOC use in PSC, a 15% of overall complication rate was reported with 9% incidence of PEP (Arnelo et al. 2015) Although SOC is used in cases where other diagnostic methods remain inconclusive and thus a increased risk

39Endoscopic Management of Benign Biliary Strictures
is acceptable to achieve the correct diagnosis, a careful consideration of the additional diagnostic yield of SOC is warranted (Lubbe et al. 2015).
2.6 Obtaining and analysing samples from biliary stricturesIn clinical practice, the diagnosis of BBS is in most cases primarily to exclude malignancy and secondly about a specific diagnosis. The diagnosis is based on a combination of all available information, patient’s history, previous ERCPs, radiologic imaging, results of blood samples including LFTs, immunoglobulins and tumour markers, cholangiography image and cytologic results of brush samples with DNA analysis (Chan and Telford 2012). The brush samples acquired in ERCP offer a fundamental diagnostic method in ERCP. However, they offer only cytologic and not histologic diagnosis with a poor sensitivity (Dumonceau 2012). Thus a stepwise approach is often needed in unclear cases, including further radiologic imaging and repeated ERCPs with or without SOC to aquire imaging and biopsies under direct visual guidance (Baron and Davee 2013; Chan and Telford 2012; Draganov et al. 2011; Shanbhogue et al. 2011).
2.6.1 Brush samples and cytologic analysis
Brush samples and subsequent cytologic analysis from the biliary tract have a poor sensitivity of less than 60%, but a high specificity (Burnett, Calvert and Chokshi 2013; Dumonceau 2012). While a preceding balloon dilation of a stricture does not affect the diagnostic yield of brush cytology, repeated sampling may improve the sensitivity of brush cytology (de Bellis et al. 2003). A minimum of five passes of the brush through the stricture is considered sufficient. However, flushing the brush catheter and including the transsected tip of the brush within the sample markedly increases the cytologic yield (Halme et al. 2012; Lindberg et al. 2002). Cytological examination of the aspirated bile juice itself gives only little further information in addition to brush cytology – the method is recommended as an adjunct to bare brushing to acquire more cells for analysis in a suspected malignacy (Dumonceau 2012). Although the role of diagnostic markers in bile juice is unclear in indeterminate strictures, improved accuracy when combining measurement of e.g. pyruvate kinase M2 from the bile juice to brush cytology and serum samples has been recently proposed (Navaneethan et al. 2015). In some studies, protein analysis of bile juice has identified variety of biomarkers that may be of potential benefit in stricture diagnostics, but the clinical significance of which is not yet known (Farina et al. 2014; Lukic et al. 2014)

40 Antti Siiki
Cytologic specimens acquired from brush samples are graded as malignant, suspected malignant, atypical, or benign using well-established criteria (Lemon and Byrnes 1949). In PSC, brush cytology has a high specificity but the sensitivity generally remains as low as 40–71% in detecting malignancy (Chapman et al. 2010). However, whenever high-grade dysplastia is detected in brush cytology, this is fairly successful in predicting (73% sensitivity and 95% specificity) a finding of high-grade dysplasia or adenocarcinoma in the following surgery (Boberg et al. 2006). The interpretation of a standard cytology specimen is subjective, and depends on the skills of the pathologist (Baron et al. 2004). The rate of false positives due to PSC-related inflammation can be reduced when the pathologist is provided with adequate background data (Dumonceau 2012).
2.6.2 Flow cytometry, digital image analysis and FISH
The cytology sample acquired by endoscopic brushing may also be used for advanced analyses to diagnose pre-malignant or malignant lesions. An abnormal nuclear DNA content of the cells, (aneuploidy, abnormal DNA index) as well as number of cells in the S-phase of the cell cycle with rapid duplication rate is assessed by the flow cytometry (Ryan and Baldauf 1994). Assesment of DNA index has been shown to increase sensitivity of brush cytology to 62–72%, making an aneuploidic DNA content a strong indicator of a developing dysplasia or malignancy (Lindberg et al. 2006; Halme et al. 2012). Similar analysis of DNA content may be performed with digital image analysis (DIA) or with fluorescence in situ hybridization (FISH) that have been shown to be a valuable adjunct to cytology in detecting malignancy of the biliary tract (Baron et al. 2004; Kipp et al. 2004).
The poor sensitivity of brush cytology in the diagnosis of biliary strictures may thus be improved by using flow cytometry, DIA or FISH as an adjunct. Although these are especially valuable in indeterminate strictures in PSC and strong predictors of malignancy when positive, the analysis of DNA content or cell morphology should not be used as a screening tool, but selectively in combination with cytology in patients with other signs indicating dysplasia or CCA, e.g. in dominant stricture (Bangarulingam et al. 2010).
2.6.3 Cholangiography and endoscopy guided biopsies
Adding a routine cholangiography guided forceps biopsy to brush cytology does not necessarily improve sensitivity, at least in extraluminal pancreatic cancer, but provides

41Endoscopic Management of Benign Biliary Strictures
nearly 100% specificity at the cost of a perforation risk (Dumonceau 2012; Pugliese et al. 1995). Given that the biopsy forceps are not wire guided, manoevering the forceps beyond the inferior margin of the CBD stricture and thus acquiring reliable samples is questionable (Baron et al. 2004). An endoscopically guided papillary biopsy is valuable in the diagnostics of malignancy and in IgG4-related diseases (Chan and Telford 2012; Dumonceau 2012). In IAP and IAC, the histologic features include plasma cell infiltration and fibrosis as well as presence of IgG4 stained cells (Boonstra et al. 2014; Okazaki et al. 2014).
2.6.4 Visually guided biopsies
Obviously the accuracy of biopsies depends on whether the biopsies are taken at the intended site. Thus SOC with visually controlled biopsy provides an attractive method to improve the diagnostics of BBS. Although the biopsy forceps of the currently most widely used Spyglass SOC are tiny, visually controlled biopsies still provide more tissue material for analysis than brush cytology samples, and thus potentially a more precise diagnosis (Rey et al. 2014). Accordingly, visually controlled biopsies with SOC have been able to provide an accurate definitive diagnosis in unclear bilary strictures in 82% of cases where previous ERCP guided samples were inconclusive (Ramchandani et al. 2011) and to provide additional information or affect clinical decision-making in 67% (Chen et al. 2011). SOC with biopsies has been proven to be technically feasible and safe in the case of an indeterminate biliary stricture. Procedural technical success rates of 90-100% and rates of 72–98% for acquiring biopsies eligible for diagnosis have been reported (Awadallah et al. 2006; Chen et al. 2011; Draganov et al. 2011; Kalaitzakis et al. 2012; Woo et al. 2014).
The diagnostic value of ERCP, visual impression on SOC and biopsies in the diagnostics of indeterminate biliary strictures are presented in Table 5 according to the largest prospective multi-centre study to date of 226 patients. SOC visual evaluation has been shown to have higher sensitivity while biopsies have high specificity (Chen et al. 2011).
Supporting results have been published on the high accuracy of SOC guided biopsies in confirming or excluding malignancy: the overall sensitivity in diagnosing malignant lesions is up to 95% for visual assessment and 82% for biopsies, with overall specificity of 78% and 82% respectively (Ramchandani et al. 2011). In addition, SOC biopsies have been proven more accurate in diagnosing biliary strictures than brush cytology and cholangiography guided biopsies with sensitivity, specificity and negative predictive value of 77, 100 and 69% respectively (Draganov et al. 2011).

42 Antti Siiki
Table 5. The diagnostic value of ERCP, SOC visual impression and biopsies in differentiating between malignant and benign biliary strictures in a study of single-operator peroral cholangioscopy (SOC) use in indeterminate biliary strictures. Expressed by sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accurancy according to a multi-centre study of SOC use (Chen et al. 2011)
Sensitivity Specificity PPV NPV AccuracyERCP impression 51% 54% 88% 77% 53%SOC impression 78% 82% 80% 80% 80%Biopsy histology 49% 98% 100% 72% 75%
The use of SOC in PSC diagnostics and surveillance has not been established due to the small number of studies available (Kalaitzakis et al. 2012; Ramchandani et al. 2011; Arnelo et al. 2015). However, a cholangioscopy has reportedly been helpful in distinguishing between malignant and benign dominant strictures in PSC compared to cholangiography or brush cytology; sensitivity of 92%, specificity of 93%, accuracy of 93%, positive predictive value of 79% and negative predictive value of 97% were achieved in 53 PSC patients in median follow-up of 47 months (Tischendorf et al. 2006). When malignancy is suspected in a macroscopically ulcerous mucosa but biopsies remain benign, repeating SOC in a few weeks or months is recommended (Tischendorf et al. 2006).
It has been suggested that the diagnostic value of SOC guided biopsies is best in difficult cases with inconclusive previous diagnostic modalities, and better for patients with hilar or proximal strictures than in distal CBD strictures (Draganov et al. 2011).
2.7 Serum diagnosticsCarbohydrate antigen 19-9 (CA19-9) is used in the diagnosis of tumours located in the head of the pancreas and CCA. This serum tumour marker should be interpreted with caution, especially in the presence of biliary obstruction; however, marked elevation to levels over 1000 U/ml are strongly suggestive of cancer (Pearce et al. 1994; Steinberg 1990). While the overall sensitivity of CA19-9 in the diagnostics of pancreatic cancer is 79% and specificity of 82%, a higher cut-off value (e.g. 300 U/ml instead of routine 37 U/ml) with obstruction increases the specificity to 87% (Goonetilleke and Siriwardena 2007). Being the least inaccurate of the markers available, the value of CA19-9 is in repeated measurement after relief of jaundice: a normalised level suggests that pancreatic cancer is unlikely in a patient with a normal CT (Goonetilleke and Siriwardena 2007).
Serum IgG4 is used in the diagnostics of autoimmune disorders IAC and IAP. While 15% of PSC patients have slightly elevated levels of serum IgG4, patients with

43Endoscopic Management of Benign Biliary Strictures
IAC usually have higher levels. When fourfold IgG4 (>5.6 g/L) was used as cut-off, sensitivity of 42% and specificity and positive predictive value of 100% were reached (Boonstra et al. 2014). In PSC, combining cytology, flow cytometry, CA19-9 with a cut-off value of 100 U/ml and CEA (carcino-embryonal antigen) provided sensitivity, specificity and NPV of 100, 85 and 100% respectively (Lindberg et al. 2002).
2.8 Non-endoscopic treatment of benign biliary stricturesWhile percutaneous technique is a secondary method in BBS treatment, surgery has a definitive role in providing treatment in unresponsive cases and confirming the diagnosis in unclear cases where malignancy is suspected (Abdallah et al. 2007; Larghi et al. 2008).
2.8.1 Percutaneous management
Percutaneous interventions via PTD are an alternative to endoscopy in relieving biliary obstruction and treating strictures. A therapeutic PTD is used when endoscopy fails as a bridge to surgery or continued percutaneous treatment and to facilitate a rendezvous ERCP (Swahn et al. 2013). In a post-CCY biliary injury, a percutaneous drain may be inserted to provide access to the biliary tract and to collect samples (Wu and Linehan 2010).
Percutaneous biliary drainage is associated with a success rate of up to 98% in biliary cannulation with 9% and 0.7% complication and mortality risk respectively (Weber et al. 2009). Patients with non-dilated ducts are at greater risk of up to 14% for complications, most commonly bleeding, cholangitis, sepsis and acute pancreatitis (Weber et al. 2009). The complication risk of PTD in malignant cases and a mortality rate of up to 2% are considered acceptable in palliative situations with patients unfit for surgery (Yee and Ho 1987).
A traditional method in the percutaneous treatment of BBS is to dilate with balloon or plastic bougies, followed by the exchange of PTD catheters with gradually increasing diameters of up to 18F across the stricture. In refractory or endoscopically inaccessible strictures success rates of 77–90% have been reported with this method (Janssen et al. 2014; Weber et al. 2009). The percutaneous insertion of retrievable covered self-expanding metal stents has been successfully used in strictures of the bilio-enteric HJ anastomosis in strictures secondary to LT, with 16%, 87% and 20% rates of migration, resolution and recurrence respectively (Gwon et al. 2013). In two case series of BBS secondary to HJ anastomosis and CP, the novel BDBS was used percutaneously with a

44 Antti Siiki
high success rate and predictable degradation pattern in six months (Mauri et al. 2013; Petrtyl et al. 2010).
2.8.2 The role of surgery
The well-established surgical treatment of BBS has long experience in use and good long-term results (Larghi et al. 2008). Surgical approach is preferred if endoscopy fails or is not possible due, for example to total obstruction or major duct leakage in the post-operative situation as well as in selected cases of CP and PSC. Despite the associated morbidity, burden on the patient and on the health care system, resection not only provides definite diagnosis but has also been associated with good long-term results (Ahrendt and Pitt 2001; Gourgiotis et al. 2007; Lillemoe et al. 2000). However, with successful endoscopy, surgery may be avoided, which is especially important in patients with co-morbidities or in difficult surgical circumstances, e.g. immediately after complicated biliary surgery, in CP or in stricture of a duct-to-duct anastomosis after LT (Ahrendt and Pitt 2001; Damrah et al. 2012; Gourgiotis et al. 2007).
In post-operative strictures, most commonly after LC or open CCY or CBD exploration, an initial success rate of up to 98% with late recurrence after surgical anastomosis in 9% was observed in five-year follow-up after Roux-en-Y HJ reconstruction (Lillemoe et al. 2000). Performing a surgical HJ anastomosis on lesions at less than two centimeters from the biliary confluence (Bismuth II–IV) becomes more complex (Bismuth and Majno 2001). Surgery due to CCY related late strictures is associated with morbidity and mortality rates of up to 19% and 3% respectively (Bektas et al. 2007). However, the complex injuries affecting or transecting the bile duct at the biliary confluence (Bimuth IV–V, Strasberg E) typically require surgery (Larghi et al. 2008; Lillemoe et al. 2000). In post-LT anastomotic strictures surgical revision and re-transplantation are the final options if all others fail (Akamatsu et al. 2011; Chan and Telford 2012; Williams and Draganov 2009).
In CP related biliary strictures the surgical approach is most commonly intended to not only bypass the stricture but also to manage intractable pain, involvement of the adjacent organs, e.g. duodenal obstruction and suspected malignancy. Surgical options include complete duodenal preserving resection of the head of the pancreas with end-to-end pancreato-jejunostomy (Beger) and currently more commonly its modification without division of pancreas (Berne) or a local resection of the pancreatic head with a longitudinal pancreato-jejunostomy (Frey). Radical pancreato-duodenectomy is a definite option when there is any concern about an underlying malignancy or duodenal obstruction (Abdallah et al. 2007; Dumonceau et al. 2012; Gourgiotis et al. 2007; Yin

45Endoscopic Management of Benign Biliary Strictures
et al. 2012). An isolated HJ may be performed with good long-term results in a minority of patients who are pain-free with CBD stricture (Abdallah et al. 2007).
In advanced PSC, a curative treatment is LT with preferably duct-to-duct anastomosis (Damrah et al. 2012) with indications similar to those of other chronic liver diseases: complications of portal hypertension, impaired quality of life and liver failure (Chapman et al. 2010). Extrahepatic resection in PSC is controversial, and there is no evidence of non-transplant surgery actually affecting the natural history or disease progression (Chapman et al. 2010). It is still debated if an LT with neo-adjuant therapy should be advocated for the therapy of early stage PSC associated CCA (Chapman et al. 2010).
While endoscopic diagnostics has improved hugely due to improvements in tissue analysis and the availability of visually controlled biopsies, it is still far from perfectly accurate. Even in combination with radiology and serum samples, predicting CCA in PSC patients, for example is still extremely difficult. The false positive results of the diagnostic tests may lead to unnecessary surgery, which offers an ultimate diagnostic and therapeutic option, the cost being the associated morbidity. Thus further research is needed to improve and simplify the diagnostics of BBS (Chan and Telford 2012; Baron and Davee 2013).
2.9 Endoscopic treatment and outcome of biliary strictures by aetiologyThe optimal endoscopic treatment method depends on stricture aetiology, location and timing of the intervention (Baron and Davee 2013). The strictures secondary to PSC require a quite different strategy than post-operative strictures, which respond well compared to strictures in distal CBD due to CP, which are relatively resistant to any endoscopic treatment method (Abdallah et al. 2007). The different types of strictures also have different outcomes, ranging from a good response in LT to a long-lasting stent therapy in patients with CP unfit for surgery (Baron and Davee 2013; Chan and Telford 2012).
2.9.1 Post-cholecystectomy
Treatment of post-CCY strictures with an increasing number of tri-monthly exchanged and added multiple PSs (mPS) has been successful with a low rate of adverse events. An Italian study of 45 patients with post-CCY strictures by Costamagna et al. evaluated the long-term results of aggressive therapy with increasing numbers of up to six plastic stents for 12 months. This achieved an excellent 89% success rate with no recurrences in

46 Antti Siiki
the follow-up of four years. In this retrospective study of mPS therapy where over half of the cases were Bismuth I–II, and one fourth were Bismuth III–IV, stent occlusion necessitating early exchange occurred in 18% and complications such as cholangitis or pancreatitis in 9% of patients (Costamagna et al. 2001). In smaller patient populations post-CCY strictures graded as Bismuth I-II and Bismuth III have been associated with respective success rates of 80% and 25% with mPS therapy (Draganov et al. 2002).
However, good results have also been achieved by inserting three or fewer PSs in Strasberg B and C lesions not mandating HJ; 78% of stricture resolution after 12 months with only 6% of patients requiring early stent exchange due to cholangitis or stent clogging (Vitale et al. 2008). In a similar protocol involving the insertion of 2-4 simultaneous PSs, long-term success rates of up to 67% and 82% have been presented in the follow-up of over six years in Bismuth II–III strictures with single and additional treatment periods respectively. However, a considerable rate of adverse events has been reported with 10% PEP and 2% perforation rate as well as an incidence of symptomatic stent clogging and migration of 7% and 2% respectively (Tuvignon et al. 2011). In two large multi-centre studies in France, recurrences after stent therapy became evident in the first 12–24 months of follow-up. Half of the recurrences responded to additional stenting with either PSs or CSEMSs and half underwent surgery (Tuvignon et al. 2011; Vitale et al. 2008). Over 80% long-term success rates and incidence of adverse events of up to 19% have been presented in other studies with mPS therapy of post-CCY strictures (De Palma et al. 2003; Draganov et al. 2002; Kuroda et al. 2010). The poorest results for mPSs have been associated with the complex hilar strictures of Bismuth III–IV (Costamagna et al. 2001; de Reuver et al. 2007).
The number of ERCPs required for mPS therapy usually ranges from four to up to seven during the treatment period of 12 months (Costamagna et al. 2001). The benefits of aggressively increasing mPS therapy have not been substantiated in all studies. Although mPS treatment may be the most obvious when the largest possible number of stents are inserted early in the course of therapy in CCY-related strictures, problems such as post-insertional pain in 28% and stent related problems in 42% were reported with a failure rate of 33% in a Dutch study of over 100 patients (de Reuver et al. 2007). While the main advantage of mPS therapy appears to be the gradual dilation effect with the ability also to treat the strictures affecting the biliary confluence, the main drawback is the laborious protocol of multiple ERCP sessions (Costamagna and Boškoski 2013).
Studies evaluating the use of fully covered self-expanding metal stents (FCSEMS) in post-CCY strictures include strictures below the biliary confluence where primary therapy with mPS has failed. A success rate of 90% with safe removal has been achieved in several studies with in dwelling times ranging from four to 11 months (Deviere

47Endoscopic Management of Benign Biliary Strictures
et al. 2014; Irani et al. 2014; Kahaleh et al. 2013; Tarantino et al. 2012b). Rate of adverse events during treatment have been up to 39%, most commonly cholangitis or fever as well as PEP (Deviere et al. 2014). The migration rate, apparently rising rapidly after an indwelling time exceeding six months, has ranged from 10% to over 50% in recent studies (Deviere et al. 2014; Tarantino et al. 2012b). The incidence of stricture recurrence in 18-month follow-up has been up to 17% (Deviere et al. 2014).
The use of FCSEMS seems to allow a short time and relatively simple treatment with potentially only two ERCP sessions, but is usually restricted to strictures below the biliary confluence.
2.9.2 Post-liver transplantation
In the treatment of post-LT strictures, balloon dilation with plastic stenting is considered superior to dilation only (Zoepf et al. 2006). The well-established endoscopic method with mPS has been successful in 80–90% of cases (Graziadei et al. 2006; Pasha et al. 2007). With maximal mPS therapy with 2–4 PSs for a shorter duration of 4-9 months, an immediate success rate of 88% was achieved with a 5% rate of mild complications (Pasha et al. 2007). Treatment with two PSs for 8–12 months resulted in a long-term success rate of 90% with a stent-related cholangitis rate as low as 4% (Morelli et al. 2003). The good clinical outcome with infrequent problems associated with mPS therapy was also sustantiated in a study by Tabibian et al, where mPS therapy of 38 anastomotic post-LT strictures led to a 94% success rate (Tabibian et al. 2010). However, an incidence of up to 37% for ERCP or stent-related adverse events has been reported, consisting mainly of cholangitis and PEP (Verdonk et al. 2006). The recurrences occurred after ERCP in 3-5% (Pasha et al. 2007; Tabibian et al. 2010; Verdonk et al. 2006). To overcome the main drawback of mPS therapy of multiple ERCPs and shorten the treatment, a rapid sequence mPS therapy with accelerated increase in the number of stents at two-week intervals with indwelling of maximum number of stents for 5–7 months resulted in an 87% success rate with low complications (Morelli et al. 2008). Although endoscopy is considered to be the primary management method, also in rare living donor anastomotic strictures, these respond less favourably to endoscopic therapy with dilation and mPS: Outcomes of 65–70% have been reported, which may be due to technical difficulties in traversing the stricture and multiple peripheral anastomoses (Tsujino et al. 2006; Williams and Draganov 2009).
The development of stents and the relative complexity of mPS therapy have led to a growing interest in and several studies on FCSEMS usage in post-LT anastomotic strictures. In the only randomised controlled trial (RCT) of the treatment of anastomotic

48 Antti Siiki
strictures in 20 patients, the 4-month FCSEMS therapy had an excellent outcome (80–90%), and was associated with fewer complications, fewer endoscopic interventions and lower costs than the 12-month mPS therapy with follow-up of 26 months (Kaffes et al. 2014). By using a special short stent with an anti-migration waist and long removal threads, neither severe complications nor cases of migration were encountered (Kaffes et al. 2014). Although a systematic review comparing mPS treatment and small series of FCSEMS or partially covered self-expanding metal stent (PCSEMS) studies from 2013 did not suggest a clear advantage of CSEMS over mPS, the indwelling time of over three months was associated with a very similar success rate of 80–90% compared to mPS, the disadvantage being the migration rate of 16% (Kao et al. 2013). Similarly, while immediate success rates of up to 86–5% with FCSEMS have been reported, the drawback has been the migration rate of 23% with recurrence rates up to 48% (Chaput et al. 2010; Garcia-Pajares et al. 2010). In a Finnish study, an outstanding success rate has been reported with 13% migration rate with a similar stent to that used in the RCT by Kaffes et al. which was kept in place for seven months (Haapamaki et al. 2012). However, the study of 54 patients by Tarantino et al. with success rates of 53–72% achieved by stent indwelling time as short as two months found an alarming migration rate of 33–47% with a standard FCSEMS and led to the conclusion that metal stents should be used only if conventional therapy with mPS fails (Tarantino et al. 2012a).
The most recent large studies of FCSEMS use have reported success rates of 61–88% with incidence of adverse events of 33%, consisting mostly of mild cholangitis and migration (Deviere et al. 2014; Kahaleh et al. 2013; Tarantino et al. 2012b). Although the removal has been unproblematic after the stent indwelling time of 4–6 months in post-LT anastomotic strictures, recurrences occurred in one out of four patients during the follow-up of 16–18 months (Deviere et al. 2014; Kahaleh et al. 2013; Tarantino et al. 2012b). Interestingly, a case report has suggested an effective treatment of post-LT and post-CCY strictures with FCSEMS even when stenosis necessitates stent placement over the biliary confluence by securing the contra-lateral duct with a single PS (Poley et al. 2011). FCSEMSs appear effective in treatment of post-LT anastomotic strictures, but migration remains an issue to be resolved.
The diagnostic and therapeutic approach to non-anastomotic strictures is similar to that for anastomotic strictures with endoscopic extraction of sludge, dilation of accessible strictures and stent placement. The response to endoscopic therapy is at best 50% with the rate of eventual re-transplantation up to 16–50% due to recurrent cholangitis or cirrhosis (Baron and Davee 2013; Chan and Telford 2012; Graziadei et al. 2006; Verdonk et al. 2007). Non-anastomotic strictures require more endoscopic interventions over prolonged periods of time with sludge extraction and stenting aimed to decrease or at least delay the need for re-transplantation; endoscopic therapy may

49Endoscopic Management of Benign Biliary Strictures
serve as a bridge to re-transplantation (Baron and Davee 2013; Graziadei et al. 2006; Verdonk et al. 2007).
2.9.3 Chronic pancreatitis
Chronic pancreatitis -related strictures are the most difficult BBSs to treat with endoscopic stenting, presumably due to the tight fibrotic calcificating tissue in the head of the pancreas (Kahl et al. 2003; Pozsár et al. 2004). The 2012 guideline for endoscopic therapy of CP-related CBD strictures recommended mPS therapy over a 12-month period (Dumonceau et al. 2012). Multiple PSs has been found superior to both single PSs and to UCSEMSs (uncovered self-expanding metal stent) in CP related strictures (Van Boeckel et al. 2009). Although the use of a short-term single PS may be adequate in biliary obstruction related to acute inflammation and concomitant acute pancreatitis, it has proved insufficient in a long-standing CP related stricture. With single PS treatment, all recurrences have been reported to occur during the first year (Cahen et al. 2005; Kahl et al. 2003).
The success rate with mPS therapy has been much poorer in CP than in post-operative strictures, although CP related strictures occur predominantly in the distal CBD (Abdallah et al. 2007). Chronic pancreatitis with calcifications especially is associated with a poor response: A failure rate of up to 83% has been reported while in strictures associated with non-calcifying CP therapy very seldom fails (Draganov et al. 2002). In calcifying and non-calcifying cases CP combined, other studies with mPS protocol have reported success rates as low as 31–44% (Eickhoff et al. 2001; Sakai et al. 2009). At best, the success rates of 50–60% have been achieved in patients with calcifying CP treated aggressively with mPS (Pozsár et al. 2004) . However, encouraging results of up to 92% success rate in four years of follow-up with mPS have been reported in a single study where half of the patients reportedly had calcifying CP (Catalano et al. 2004). Adverse events such as PEP have occurred in 2–5%, cholangitis in 3–10% and stent clogging in up to 34% when mPSs have been used in CP related strictures (Draganov et al. 2002; Pozsár et al. 2004; Sakai et al. 2009).
Poor compliance of patients with alcohol-related CP is often behind the complications, such as cholangitis due to stent clogging (Kiehne et al. 2000). It is noteworthy that in one study the lengthened interval of stent exchange, secondary to poor compliance, led to two deaths (7%), both of then related to a septic infection of biliary origin (Pozsár et al. 2004).
The most prominent disadvantages of mPS therapy in CP are the need for repeated ERCP sessions, high rate of stent dysfunction and poor long-term resolution rate.

50 Antti Siiki
The latter is possibly due to the inadequate dilation effect of PSs in a fibrotic stricture (Abdallah et al. 2007) .
The use of CSEMSs would be tempting in CP related strictures because of the stricture location in the distal CBD, the tight fibrotic nature of the stricture and the poor resolution rate even with increased number of mPSs in repeated ERCP sessions. In the early experiments, the treatment of BBS without intention to remove an UCSEMS was discarded due to eventual stent dysfuntion (Cantu et al. 2005). Next, PCSEMSs were tried in CP related strictures: In two reports of mPS resistant strictures, PCSEMSs indwelled for four to five months resulting in 80% clinical success (Behm et al. 2009; Kahaleh et al. 2004). Tissue ingrowth or secondary stricture at the uncovered part of the stent was predictably observed in 13% after PCSEMS therapy (Kahaleh et al. 2008). Tissue hyperplasia and embedding associated with PCSEMS often lead to difficult removal (Irani et al. 2014).
The first pioneering study showing that FCSEMSs are feasible in CP-related strictures was originally published as an abstract in 2005; it included six patients, in two of whom the stent could not be removed after indwelling of 4–6 months due to proximal migration, one ended up in HJ due to recurrence at six months and three were strictureless for three years of follow-up (Cahen et al. 2008). After this study several researchers concentrated mainly on determining the safety of removal in various FCSEMS designs: In a study with three months of FCSEMS indwelling, 58–65% success rate in four-month follow-up was achieved with a cost of non-severe adverse events occurring at placement in 11% and during stent therapy or removal in 16% of patients. While the anchoring fins of the early stents prevented migration, they caused ulceration and bleeding from the mucosa as the FCSEMS was extracted (Mahajan et al. 2009). In another stent design without fins, removal was unproblematic but migration occurred in nearly half of the patients (Park et al. 2011a). When a stent exchange at two months was then tried to ascertain the safe removal of FCSEMSs equipped with flared ends for anti-migration, it was noticed that CP-related strictures only achieved a success rate of 46% (Poley et al. 2012). This finding was substantiated in a recent series of 75 CP-related CBD strictures, one third of which were treated with PCSEMSs and two thirds with modern FCSEMSs for seven months: stricture resolution of only 48% with a recurrence rate of 10% in 20 months of follow-up was achieved, again a much poorer outcome than in other aetiologies. Although these findings supported the earlier findings of CP-related strictures being more resistant to treatment due to the fibrotic encasing process of CP, they did also speak for the usefulness of FCSEMSs in patients in whom prior PS therapy was unsuccessful (Irani et al. 2014).
In 2013, larger multi-centre studies with unvarying treatment protocols started to appear in the literature about FCSEMS usage in BBS (Deviere et al. 2014; Kahaleh et

51Endoscopic Management of Benign Biliary Strictures
al. 2013). In a study of 127 patients with long-standing CP-related biliary strictures, a 91% resolution rate after median indwelling period of 11 months was achieved. The recurrence rate was 10% during the 18-month follow-up, which was better than in the strictures secondary to CCY or LT. Interestingly, a 3% rate of moderate PEP was higher than in LT patients. Migration was less frequent than in other aetiologies, being only 5% in six months of follow-up (Deviere et al. 2014). Finally in 2015, a multi-center RCT directly comparing mPS to FCSEMS in CP-related biliary stricture was published. The Finnish researchers noticed that in 60 patients six-month treatment with mPS or FCSEMS provided similarly good clinical result of in two-year follow-up: 90% of the patients in mPS group and 92% of those in FCSEMS group were stricture-free at the end of the follow-up, without difference in rate of stent migration or stricture recurrence (Haapamaki et al. 2015).
The main conclusion of these largest studies to date was that even with long indwelling time, modern FCSEMSs could be safely removed. In addition, stricture resolution and migration outcome, achieved with a reduced number of ERCPs in CP, suggests a potential advantage over mPSs (Deviere et al. 2014; Haapamaki et al. 2015).
2.9.4 Primary sclerosing cholangitis
In the endoscopic treatment of biliary strictures secondary to PSC, balloon dilation with or without plastic stents is considered the mainstay of treatment intended to relieve symptoms, prevent recurrent cholangitis, improve quality of life and survival without LT (Eaton et al. 2013). On the other hand, endoscopy should not jeopardize timely LT (Chan and Telford 2012). Since ERCP in PSC setting is associated with complications far more commonly than ERCPs in the non-PSC population, careful patient selection is crucial (Ismail et al. 2012; von Seth et al. 2015).
PSC-related strictures usually respond well to dilation: the correct use of stents that offers optimal resolution with minimal complications has not yet been evaluated in prospective studies (Eaton et al. 2013). However, dilation followed by short-term plastic stenting of median nine days (ranging up to 23 days) is safe and effective, and relieved cholestatic symptoms and LFT in 83% of patients. This strategy has resulted in re-intervention-free follow-up of one and three years in 80% and 60% of patients respectively (Ponsioen et al. 1999). A later study of PSC patients who underwent interventions for dominant strictures reported that dilation alone provides outcomes similar to dilation with PS indwelling for three months. In this study the PSs were associated with more complications, but, on the other hand, all the stents were inserted

52 Antti Siiki
in patients in whom dilation alone was not believed to improve biliary drainage sufficiently (Kaya et al. 2001).
Stricture dilation with or without stent insertion resulted in perforation in 2–5% of cases (Kaya et al. 2001; Ponsioen et al. 1999). A recent large study reported the incidence of perforation to be up to 6% in any ERCP performed for PSC (von Seth et al. 2015). Consequently, after a fragile PSC-related stricture is balloon-dilated with a risk of contrast extravasation, a clinical practice of a short-term stent therapy may be reasonable to ensure bile flow downstream from the potential leak site. The rate of cholangitis is elevated after the dominant stricture is managed by intrabiliary interventions such as brushing, dilation and stent insertion to provide biliary drainage. In narrow strictures associated with PSC it is sometimes impossible to use stents larger than 7F. It has been noted that the lower the diameter of the PS, the higher the incidence of cholangitis. The infrequent use of multiple PSs in PSC-related dominant strictures was not associated with different complication profile than in the rest of the patients (Navaneethan et al. 2015b). The use of FCSEMSs is far from routine in PSC-related strictures due to the stent diameter and high radial force usually inappropriate to narrow bile ducts; FCSEMSs have occasionally been used in some studies, but no subgroup analysis of PSC has been published (Irani et al. 2014; Mahajan et al. 2009; Tarantino et al. 2012b).
Taken together, the optimal treatment strategy for PSC-related strictures is not evidence based (Eaton et al. 2013). It should include routine brush samples used for cytology and advanced analyses, followed by cautious balloon dilation and possibly a short-term (two weeks) PS therapy to ensure biliary drainage (Baron and Davee 2013). Forthcoming RCTs assessing the rationale of dilation and stent insertion in PSC will hopefully clarify optimal stent management in PSC. Prognostic models to predict the timing of LT during the life-long surveillance of PSC patients have been proposed, based on annual radiologic imaging with serum CA19-9 assessment and endoscopic sampling (cytology, FISH, DIA, flow cytometry). However, their use in individual patients has been questioned due to significant variation in disease course and lack of consensus and evidence of an optimal model (Chapman et al. 2010; Eaton et al. 2013; Ehlken and Schramm 2013). The protocol is aimed to detect dysplasia before the development of CCA to ensure a timely LT. The thoroughness of national surveillance is affected by the availability of liver transplants, which is generally good in the Nordic countries. The surveillance protocol of PSC developed in Helsinki University Hospital is presented in Figure 4 (Boyd et al. 2014).

53Endoscopic Management of Benign Biliary Strictures
2.9.5 Autoimmune cholangitis
There are no publications comparing different endoscopic treatment methods of IgG4-related biliary obstruction. Considering the indeterminate nature of a stricture at the time of ERCP, tissue sampling with a single plastic stent insertion is usually sufficient to provide biliary drainage during steroid therapy. In case of an early treatment failure, re-evaluating the diagnosis has to be contemplated, after which stent exchange - with or without increase in the number of PSs or exchange to FCSEMSs - remain as options. In IAC and IAP short-term endoscopic management is aimed to support the corticosteroid therapy by relieving the obstruction caused by primary biliary inflammation or external mass (Chan and Telford 2012).
Figure 4. Algorithm for diagnosis and surveillance of PSC (primary sclerosing cholangitis) developed by Färkkilä and co-workers in Helsinki University Hospital (Boyd et al. 2014). ERC: endoscopic retrograde cholangigraphy, m-Amsterdam: modified Amsterdam scale of intra- and extrahepatic severity of PSC, CT: computed tomography, MRI: magnetic resonance imaging, R: cytology grade, LT: liver transplantation. Presented with permission from Professor Färkkilä, University of Helsinki, Finland.

54 Antti Siiki
2.9.6 Other causes of BBS
Several other infrequent aetiologies of BBS have been described in the literature without studies evaluating the treatment methods (Table1). In most cases, endoscopy is the intervention of choice with similar general principles as in more common aetiologies. Selective biliary guide wire cannulation is the prequisite for safe procedures, followed by cholangiography, balloon dilation using 4–12 mm balloon advanced across the stricture under fluoroscopic guidance and inflated to facilitate the insertion of initially 1–2 PSs (Baron and Davee 2013). Adequate tissue sampling and radiologic imaging for the differential diagnosis of occult malignancy are warranted (Chan and Telford 2012). When the diagnosis becomes obvious, the initial PS may be followed by the insertion of tri-monthly exchanged and gradually increased number of PSs to reshape the stricture or insertion of FCSEMSs in selected cases (Baron and Davee 2013; Costamagna and Boškoski 2013).
2.10 Treatment with endoscopic stentsThe development of stents has led to situation in which FCSEMSs are replacing multiple PS therapy in CBD strictures in clinical work, despite the lack of strong evidence (Deviere et al. 2014). There are currently only two RCTs on this issue, one of post-LT strictures and another of CP -related strictures (Haapamaki et al. 2015; Kaffes et al. 2014). The plastic stents are used in cases where FCSEMSs are not practical, such as in strictures in the intrahepatic ducts or at the biliary confluence (Costamagna and Boškoski 2013; Dumonceau et al. 2011; Larghi et al. 2008). The dilation of a BBS is seldom enough for long-term treatment (Zoepf et al. 2006). In the early years of ERCP practice the dilation balloon may have been one of the few instruments to fit the narrow working channel of early duodenoscopes. However, it still has its place in facilitating PS insertion across a narrow stricture (Costamagna and Boškoski 2013).
BDBSs could potentially be the next generation of biliary stents that could overcome disadvantages related to traditional stents (Lorenzo-Zuniga et al. 2014). BDBSs have been successfully used percutaneously in BBS (Mauri et al. 2013). However, no endoscopic implantation device has been available for BDBS.

55Endoscopic Management of Benign Biliary Strictures
2.10.1 Plastic stents
Plastic stents are the most inexpensive and simplest types of endoscopically inserted stents, prototypes of which were introduced in the late 1970s (Soehendra and Reynders-Frederix 1980). Currently several different designs of polyethylene stents are commercially available. They usually have anchoring flaps at both ends, and most commonly have a calibre of 7, 8.5 or 10 F and length of 5–15 cm. A single PS may be used to treat a BBS, as a bridge to definitive treatment in an icteric patient and in post-CCY bile leaks (Perri et al. 2011). Multiple plastic stents have been shown to be superior to single plastic stents or UCSEMSs in the long-term treatment of BBS (Van Boeckel et al. 2009). Single, small bore (diameter 7–8.5 F) PSs especially have a very limited dilation effect and failures in the treatment with episodes of acute cholangitis occur in up to 30–50% of patients (Perri et al. 2011; Van Boeckel et al. 2009). According to a Swedish nationwide ERCP study, the stents used are plastic in 79%, and single in 87% of cases (Enochsson et al. 2010).
BBS therapy with tri-monthly ERCPs where increasing numbers of mPSs are placed side-by-side across the stricture facilitated by balloon dilation has been supported as a treatment of choice especially in post-operative cases (Baron and Davee 2013; Costamagna et al. 2001). Most of the study protocols have all the stents removed at 12–14 months (Costamagna et al. 2001; Draganov et al. 2002). Short stent exchange interval of two weeks (Morelli et al. 2008) and extended indwelling up to six months (Lawrence et al. 2010) have been successfully tried out to shorten treatment duration
Figure 5. Three types of biliary stents. Left: 10 F x 7 cm polyethylene plastic stent (Advanix, Boston Sci, MA, USA). Centre: Nitinol braided silicone covered self-expanding 10 mm x 60 mm FCSEMS (SX-Ella, Nitinol Plus, Ella, Czech Republic). Right: Braided self-expanding polydixanone biodegradable 8 mm x 60 mm BDBS (Ella, Czech Rep)

56 Antti Siiki
and to reduce the number of ERCPs required. The major advantages of mPS therapy are the gradually increasing continuous dilation effect and the possibility to treat even strictures at the biliary confluence with insertion of PSs going up to the intrahepatic branches (Costamagna et al. 2001; Dumonceau et al. 2011). In addition, stent displacement, migration or poor response can be managed at the time of any stent exchange (Costamagna and Boškoski 2013). The main disadvantage is the number of ERCP sessions needed; typically a minimum of four per patient (Costamagna et al. 2010; Tabibian et al. 2010). The mPS therapy is demanding for both endoscopist and patient compliance. Such a BBS treatment method is a fairly infrequent procedure, and only few centres or endoscopists have extensive experience of it (Costamagna and Boškoski 2013; Enochsson et al. 2010).
While the adverse events related to mPS insertion are usually mild, occurring at a rate of 1–9%, stent occlusion and cholangitis necessitate early stent exchange in 7–18% (Costamagna et al. 2001; Draganov et al. 2002; Sakai et al. 2009). Stent clogging is thought to result from the accumulation of bacterial biofilm and sludge inside the stent (Donelli et al. 2007). While in all BBSs the clinical success rate is up to 80%, the poorest outcomes are associated with complex post-operative hilar strictures and strictures secondary to calcifying CP, which are associated with success rates of 25% and 8–44% respectively (Draganov et al. 2002; Sakai et al. 2009). Thus the main problems of mPS therapy are failure to achieve stricture resolution or a relapse of the stricture soon after treatment (Perri et al. 2011).
2.10.2 Covered self-expandable stents
Self-expanding metal stents (SEMS) were first used in the 1980s in malignant CBD strictures to provide adequate radial strength and patency in tight strictures secondary to tumours in e.g. the head of the pancreas (Neuhaus, Hagenmuller, Classen 1989). At that time UCSEMSs were the only option available. For benign indications, UCSEMSs were first used in chronic pancreatitis related tight strictures in patients unfit for surgery (van Berkel et al. 2004). With stent development, interest has since turned to CSEMSs, in which the covering prevents tissue ingrowth and allows eventual removal (Cahen et al. 2008; Vakil 2011).
Today FCSEMSs are entirely silicone covered nitinol stents, with 10 mm post-deployment diameter, allowing flexion during implantation, patency and later removal (Baron TH and Davee 2013; Dumonceau et al. 2011; Vakil 2011). FCSEMS are best suited to CBD strictures or post-LT anastomotic strictures. If a FCSEMS is placed in the proximal CHD or over the biliary confluence, the plastic cover obstructs the

57Endoscopic Management of Benign Biliary Strictures
contralateral main intrahepatic branch (Dumonceau et al. 2011). In most cases, a FCSEMS is implanted so that the lower end remains visible from the duodenum to facilitate removal. Another option is to implant a special design FCSEMS up in the bile duct with only removal threads dangling visible in the duodenal lumen. This technique is used to avoid too long stents, e.g. in CHD or post-LT strictures (Haapamaki et al. 2012; Kaffes et al. 2014; Poley et al. 2012). The potential of the uncovered part of the stent to embed and integrate into the biliary wall and consequent problematic removal inhibits the use of PCSEMSs in the treatment of BBS (Kawakubo et al. 2012; Vakil 2011).
Several large studies on the usage of FCSEMSs in BBS have been published during the last few years (Deviere et al. 2014; Irani et al. 2014; Kahaleh et al. 2013; Perri et al. 2012; Tarantino et al. 2012b; Wagh et al. 2013). The current evidence on FCSEMS use in BBS is based on these, and on a few earlier cohort studies (Cahen et al. 2008; Garcia-Pajares et al. 2010; Hu et al. 2011; Mahajan et al. 2009; Traina et al. 2009). The first RCT on endoscopic treatment of BBS to compare FCSEMSs with multiple PSs in patients with post-LT strictures showed similar treatment success with a reduced number of ERCPs and fewer adverse events in the FCSEMS group (Kaffes et al. 2014). Another recent RCT addressing treatment of strictures secondary to CP reported that six-month treatment with either mPS or single FCSEMS resulted in similar 90% clinical success rate in two-year follow-up (Haapamaki et al. 2015)
The main advantage of FCSEMSs is the good bile flow because of a large, 10 mm post-deployment diameter with a radial force to press the stricture open (Baron TH and Davee 2013). In addition, stent insertion devices function quite smoothly and usually no previous balloon dilation is necessary (Deviere et al. 2014). Clinical experience has supported the encouraging results gained from FCSEMS studies; up to 10–12 months of indwelling time has been unproblematic with a good, 76–90% stricture resolution when stent therapy has ranged from 6-12 months (Deviere et al. 2014; Kahaleh et al. 2013; Tarantino et al. 2012b; Wagh et al. 2013). Even though a single FCSEMS is currently ten times more expensive than a single PS, FCSEMS therapy was still cost-effective due to fewer endoscopy sessions and shorter hospital stay in the only study so far to include a cost-analysis (Kaffes et al. 2014).
The possible drawbacks of FCSEMS include migration and difficult removal as well as complications such as acute cholangitis. The rate of overall adverse events has been up to 25–27% during the course of treatment with FCSEMSs (Deviere et al. 2014; Kahaleh et al. 2013). Biliary cannulation and EST, with associated risk of haemorrhage and pancreatitis, are usually required for diagnostic procedures before stent implantation, even if the FCSEMS itself can be placed endoscopically without EST (Deviere et al. 2014; Haapamaki et al. 2012). Cholangitis has been reportedly

58 Antti Siiki
associated with FCSEMS in 10-14% and pancreatitis in 3% (Deviere et al. 2014; Irani et al. 2014). Although not supported in all studies, it has been postulated that FCSEMSs placed in the distal CBD could potentially predispose to PEP by obstructing the pancreatic duct orifice due to covering membrane or the high radial force during stent expansion (Kahaleh et al. 2013).
One of the largest recent studies with FCSEMSs reported migration rates as high as 24–29% (Deviere et al. 2014), while a low risk of migration of 2–10% has also been presented (Haapamaki et al. 2015; Irani et al. 2014; Kahaleh et al. 2013). Regardless of the type of stent, migration is associated with a lower rate of stricture resolution (Deviere et al. 2014; Kahaleh et al. 2013). However, not all migrations result in treatment failure or necessitate additional procedures (Deviere et al. 2014; Irani et al. 2014; Tarantino et al. 2012b). In most cases, migration occurs distally or downwards and may potentially lead to treatment failure, obstruction of the bile duct or bowel or perforation (Baron and Davee 2013; Deviere et al. 2014; Kaffes and Liu 2013). Proximal migration, on the other hand, results in difficult removal (Baron and Davee 2013; Deviere et al. 2014; Kaffes and Liu 2013). To overcome migration, stents with convex shape and anchoring flaps or flares at the ends have been tested (Moon et al. 2012; Park et al. 2011a; Perri et al. 2012).
In recent studies with modern FCSEMSs without specific anti-migration features and with indwelling time of up to 12 months, eventual endoscopic stent removal has been achievable in all cases with only occasional use of e.g. stent-in-stent technique in difficult proximal migration (Deviere et al. 2014). The cases of impossible removal have occurred in patients with CP-related strictures with poor compliance to participate in the follow-up and consequent inadvertently long indwelling (Irani et al. 2014). However, the optimal stent indwelling time is still debated because shorter indwelling of only six months seems to provide over 90% stricture resolution rate in CP (Haapamaki et al. 2015).
Acute cholecystitis, thought to result from obstruction of the cystic duct, may occur in nil to 3% of all cases (Deviere et al. 2014). A higher incidence of up to 33% has been associated with narrow CBD with intact gallbladder and CSEMS inserted above the level of the cystic duct junction (Irani et al. 2014). Post-deployment pain occuring in 2–6% of cases is presumably caused by stent expansion to the maximum diameter in 24–48 hours, and seldom requires hospitalisation or stent removal (Deviere et al. 2014; Irani et al. 2014; Kahaleh et al. 2013).
An alarming tendency of late de-novo strictures, which were not secondary to the disease progression or recurrence, was observed in some of the early studies evaluating FCSEMSs. The incidence of these secondary strictures has ranged 2–8% (Irani et al. 2014; Kasher et al. 2011; Sauer et al. 2012) to up to 35% (Phillips et al. 2011). The

59Endoscopic Management of Benign Biliary Strictures
highest incidence of strictures occuring at the proximal end of the stent was observed in post-LT strictures with stents with exceptional radial force, suggesting that ischaemic factors and atypical stent design were the principal causes (Phillips et al. 2011). A similar observation was made more recently when 2% of patients, none of whom had a post-LT stricture, treated with CSEMSs developed a new stricture requiring endoscopic treatment. It was hypothesized that the discrepancy between stent diameter and bile duct diameter could lead to a pressure necrosis, circumferential ischaemia and ulceration causing a de-novo stricture. Thus the authors recommended avoiding CSEMSs with diameter greater than the bile duct where the proximal end of the stent would reside (Irani et al. 2014). It is interesting that the molecular level changes in response to modern FCSEMSs that may be associated with stricture resolution, late re-stricturing or difficult removal have not been extensively researched (Vakil 2011). In a single study, FCSEMSs appeared to induce only mild inflammation, fibrosis or epithelial injury in histologic examination after indwelling of only three months in an animal model (Bakhru et al. 2011). In a second animal study an incidental de-novo stricture was present in 42% of autopsies after FCSEMS therapy (Lee et al. 2014). While the most severe epithelial hyperplasia was noted when the silicone covering of a FCSEMS was damaged and strictures most commonly occurred when a stent had been in place for more than six months, the authors hypothesised that the small calibre of bile duct comparing to stent diameter may predispose to de-novo stricture formation. The role of tissue response towards stents and covering materials is unclear in the development of de-novo strictures and warrants further attention in future studies (Lee et al. 2014).
The use of FCSEMS in biliary strictures below the biliary confluence is both technically feasible and has been associated with a good resolution rate. The current evidence supporting their use is based on several cohort studies, and only recently in terms of the post-LT strictures and CP on two RCTs (Haapamaki et al. 2015; Kaffes et al. 2014).
2.10.3 Biodegradable stents
In BBS therapy, BDBSs could potentially offer a radial expansion force and patency similar to FCSEMSs without the costs and morbidity associated with repeat ERCP procedures (Lorenzo-Zuniga et al. 2014). BDBSs could also overcome other limitations of current stents, such as difficult removal. In addition, they would not require removal even if they migrated (Tokar et al. 2011). The most promising biodegradable materials in stent design are synthetic polymers such as polylactid acid (PLA) and polydioxanone (PDX), the degradation and behaviour of which in the human body are

60 Antti Siiki
well documented (Freudenberg et al. 2004). PDX has been widely used in absorbable PDS surgical sutures from 1980s (Ray et al. 1981) and has been proven to be a durable material in the environment of the human biliary duct (Freudenberg et al. 2004). The degradation characteristics of PLA resemble material used in Vicryl (Ethicon Endo-Surgery, Ohio, US) sutures (Freudenberg et al. 2004). A single experiment has been published on the endoscopic implantation of a non-radiopaque poly-capro-lactone BDBS, a material close to that used in Monocryl (Ethicon) sutures (Itoi et al. 2011). PDX is the only biodegradale material from which BDBSs are currently manufactured and commercially available.
The first experimental PLA biodegradable stents were inserted into rabbit ureters in Finland (Kemppainen et al. 1993). This was followed by a variety of studies on their use in human pancreato-biliary tract surgery and in animal models (Ginsberg et al. 2003; Laukkarinen et al. 2007a; Laukkarinen et al. 2008; Nordback et al. 2008; Nordback et al. 2012) . The endoscopically inserted Finnish designed, braided, self-reinforcing PLA stents with 10 mm diameter and 50 mm length showed encouraging characteristics of expansion and patency in the CBDs of pigs (Ginsberg et al. 2003). Further studies on experimental pig models have confirmed their predictable degradation in three to six months of a PLA BDBS in securing a HJ anastomosis (Laukkarinen et al. 2007b) and in the CBD for the treatment of a cystic duct leak (Laukkarinen et al. 2007a).
Subsequent studies have concentrated on the percutaneous insertion of BDBSs made of PDX in the absence of an endoscopic insertion device (Petrtyl et al. 2010). In percutaneous use in humans PDX stents have reportedly been associated with immediate radial expansion, good patency and complete degradation in six months (Mauri et al. 2013; Petrtyl et al. 2010). These findings have been substantiated by a recent study on PDX biliary stents inserted in an animal model (Grolich et al. 2015). In the largest human study so far, 10 patients were treated for post-operative and CP-related BBS with percutaneosly inserted BDBSs. The 16-month follow-up witnessed no relapses or re-stricturing, indicating adequate radial expansion strength to treat the BBS, but a 30% incidence of transient episodes of cholangitis (Mauri et al. 2013). It has been postulated that PDX has a higher flexibility, degrades more slowly by hydrolysis and potentially retains its mechanical properties longer than other biodegradable polymers such as polyglycolide or PLA (Sabino, Márquez, Feijoo 2000). Although PLA and PDX stents have not been compared, as a suture material PDX appears to have an optimal degeneration pattern in human bile environment (Freudenberg et al. 2004). PDX is expected to degrade by hydrolysis in 3-6 months (Sabino, Márquez and Feijoo 2000), which finding concurs with clinical results on the radiologic disappearance of braided PDX stents and absence of re-stricture in six months (Mauri et al. 2013) as well as with the results from an animal study of PDX biliary stents (Grolich et al. 2015).

61Endoscopic Management of Benign Biliary Strictures
One concern about BDBSs has been the possible epithelial hyperplasia which may develop after stent therapy, occasionally observed after the use of oesophageal PDX stents (Hair and Devonshire 2010; Lorenzo-Zuniga et al. 2014). In biliary PLA stent studies on animals there have been no changes similar to those associated with SEMSs, i.e. no epithelial hyperplasia, inflammation or proliferation after stent therapy; (Ginsberg et al. 2003; Laukkarinen et al. 2007a). In the study on pigs with an experimental cystic duct leak a blinded histologic analysis excluded any signs of residual stent material, scar formation and granulation after BDBS therapy of six months (Laukkarinen et al. 2007a). It has been suggested that the unexpected finding of neglible tissue reaction is not solely attributable to the lower radial expansion force than in SEMS, but to the material itself (Ginsberg et al. 2003). These findings were supported by the results from an animal experiment where the intensity of inflammatory foreign-body reaction to PDX stents decreased over the duration of stent therapy and was considered temporary with no clinical consequences (Grolich et al. 2015). The potential problems arising in the endoscopic use of biliary PDX stents are yet to be discovered; the feasibility of implantation in more widespread use, the predictability of stent expansion, sufficient radial force for stricture remodelling and possible migration risk remain uncharted. Before BDBS insertion, EST is often necessary but correspondingly to FCSEMSs, pre-implantation dilation of a stricture is not (Mauri et al. 2013).
Consequently, there is a clear need for more studies comparing mPSs and CSEMSs as well as evaluating the emerging role of endoscopically inserted BDBSs in the management of BBS. Although some animal studies and experiences from percutaneous use are encouraging, the lack of an endoscopic implantation device for BDBSs has so far prevented their clinical use (Mauri et al. 2013; Grolich et al. 2015). Furthermore, molecular level pathogenesis and tissue response to biliary stents remains largely unstudied (Bakhru et al. 2011; Lee et al. 2014).

62 Antti Siiki
3 AIMS OF THE STUDY
The aim of this thesis was to review the current endoscopic diagnostics and treatment of relatively infrequent benign biliary strictures.
The detailed aims of the studies were as follows:
I) To describe the rate of complications and success rate of ERCP in a Finnish central hospital.
II) To evaluate the usefulness of single operator peroral SpyGlass cholangioscopy in the diagnostics of BBS, especially in PSC, which is still one of the most difficult and least published entities in BBS.
III) To compare the two methods of endoscopic BBS treatment currently in use in terms of clinical success and complication rate: a traditional method with insertion of mPSs and increasingly used therapy with CSEMSs.
IV) To examine the differences in protein expression in an experimental animal model between: a) intact bile duct and an ischaemic biliary stricture and b) between strictures treated with FCSEMSs or BDBSs.
V) To assess the feasibility of a novel endosopically inserted biodegradable stent and its implantation device in post-operative biliary leak.

63Endoscopic Management of Benign Biliary Strictures
4 MATERIALS AND METHODS
4.1 Study I: ERCP success rates and complications in a Finnish central hospital
The database of Kanta-Häme Central Hospital (KHKS) was searched for all ERCPs performed from 2002 to 2009 as specified by the procedure codes. A retrospective chart review was continued for up to 30 days after the procedure or to the end of longer hospitalisation at KHKS or local district hospitals. The primary method of cannulation was to use a sphincterotome or to cannulate over a guide wire. In the early years, contrast medium injection was sometimes used to facilitate cannulation. When necessary, a needle-knife precut sphincterotomy was performed. In the last few years of the period in question the double-guide-wire technique or pancreatic sphincterotomy were used selectively.
During the last two to three years of the study period a routine antibiotic prophylaxis was administered. Before this, antibiotics were given if a stent insertion was planned or if a patient had a bile duct obstruction or an acute infection. Pre-ERCP rectal diclofenac was not routinely administered. In the last few years of the study period ERCPs were performed under general anaesthesia supervised by an anaesthesist. In the earlier years, the endoscopy team managed and monitored sedation. Routine serum WBC count, haemoglobin, CRP and amylase were measured after 6–10 hours. Each patient was followed up in the hospital for at least 24 hours after ERCP.
Complications were classified using the standardised criteria presented in Table 3 (Cotton et al. 1991).
4.2 Study II: Initial experience of SpyGlass cholangioscopy in biliary strictures secondary to sclerosing cholangitis
The first 11 consecutive patients undergoing ERC and SOC for intrahepatic or combined PSC from March to August 2012 in Tampere University Hospital were included. The diagnosis of PSC was based on the typical cholangiographic findings in

64 Antti Siiki
MRI and in nine cases (82%) also on earlier ERC. MRI was performed using standard imaging protocols including heavily T2-weighted 2D thin-section and thick sequences in coronal plane to visualise all biliary ductal structures. Additionally, gadolinium enhanced sequences were routinely used to estimate inflammatory and neoplastic changes. An experienced endoscopist performed all the endoscopies with standard ERC and Spyglass SOC instrumentation (Boston Scientific) with air insufflation. Tissue samples were harvested by endoscopic brushing for cytology and flow cytometry as well as by visually controlled Spybite (Boston Scientific) biopsy forceps for histology. The number of histological biopsies ranged from four to six for each patient. A routine single-dose prophylactic intravenous cefuroxime and diclofenac suppository was administered to all patients before ERC. The endoscopy team managed the patient’s sedation. Duodenal peristalsis was reduced by giving, i.v. hyoscine butylbromide or i.v. glugacon.
ERC- and cholangioscopy-related findings were recorded prospectively. Patient history, serum LFT and tumour marker CA19-9, brush cytology and flow cytometric analysis as well as pathological analysis of the biopsies were recorded. Post-ERC complications were graded and prospectively recorded for 30 days after the procedure according to their severity and length of the associated hospital stay as in Study I (Table 3).
An experienced abdominal radiologist re-analysed the patients’ MRI and cholangiography images. The intra- and extrahepatic PSC findings were graded according to the Amsterdam classification (Majoie et al. 1991) presented in Table 2. Data on patients’ later treatment and follow-up, including the need for any further procedures, was recorded.
The endpoints were technical success and complication rate of ERC with SOC and the adequacy of biopsies obtained. The effect on clinical decision-making was also subjectively assessed in terms of additional benefit obtained by the direct stricture visualisation and biopsies. Moreover, to assess the need for repeated endoscopy procedures or later events, e.g. disease progression, a prospective follow-up was carried out from the hospital records until March 2014.
4.3 Study III: Meta-analysis comparing covered self-expanding metal stents and multiple plasic stents in benign biliary strictures
A literature search of the Medline and Embase and Scopus databases was conducted for studies published in English and completed by a manual search of the reference lists of key studies. The titles and abstracts of the studies identified were screened and the full texts

65Endoscopic Management of Benign Biliary Strictures
of potentially relevant publications were obtained. Studies on endoscopic treatment of BBS with PSs or CSEMSs and with adequate data about stent type, stricture aetiology, complications and outcome were considered to meet the inclusion criteria. The search strategy, resulting in 13 PS studies and 10 CSEMS studies, is presented in Figure 6. Data extracted from the selected studies included: study details, characteristics of study population and strictures treated, technical success, complications related to stent insertion and removal, complications and other adverse events such as stent migration in follow-up, duration of stent therapy and clinical success at stent removal after six and 12 months and at the end of follow-up. The definitions are presented in Table 6.
To assess the outcome of the stent therapy, three aetiology groups were formed: chronic pancreatitis (CP), post-liver transplantation (LT) and others (Other Strictures). The aetiology-specific outcome was available from most of the studies. Five CSEMS studies reported the results of single stricture aetiology and seven studies of multiple stricture aetiologies. Eleven PS studies addressed single stricture aetiology and two studies multiple stricture aetiologies. When it was only possible to extract data on the majority of the study population, and not aetiology-specific data; these results were grouped according to the majority. In the strictures related e.g. to CCY or bile duct stones, case numbers were insufficient for subgroup analysis. Therefore all strictures except those due to chronic pancreatitis and liver transplant were combined into a single group of other aetiologies for outcome. Case numbers in the aetiology groups were as follows: CP: 128 CSEMS and 90 PS, LT: 118 CSEMS and 190 PS, and other aetiologies: 130 CSEMS and 290 PS.
The primary outcome was sustained clinical success defined as stricture resolution without unscheduled endoscopic interventions or treatment failure during follow-up. Secondary outcome parameters were technical success rate and complications.

66 Antti Siiki
Figure 6. Flow chart of the search strategy for meta-analysis and systematic review
Full text articles assessed for eligibility (n=79)
Records identified through Medlinedatabase search (n=3558)
Records identified through Cochranedatabase search (n=420)
Records excluded after review of title and abstracts (n=3899)
Additional articles after handsearching of reference lists (n=20)
Studies of potential relevance (n=99)
Included in meta-analysis (n=23)Plastic stent n=13, cSEMSn n=10
Excluded with reasons (n=76)
Insufficient dataor otherwise not relevant n=30
Single plastic stent n=28Uncovered or unremoved stent n=7
Percutaneous treatment n=3Abstract only n=3Case report n=3Dilation only n=2
Post sphincterotomy stricture n=1

67Endoscopic Management of Benign Biliary Strictures
Table 6. Definitions of BBS, treatment methods, outcome measures, complications and follow-up in Study III
Expression DefinitionBenign biliary stricture A non-malignant stricture of common bile duct secondary to chronic pan-
creatitis, orthotopic-liver transplantation, cholecystectomy or other cause.Multiple plastic stents A treatment strategy of tri-monthly plastic stent exchange with insertion
of a gradually increasing number of plastic stents across the stricture and eventual stent removal at 12 months
CSEMS A BBS treatment with PCSEMSs or FCSEMSs covered self-expandable metal stent with eventual stent removal
Clinical success A successful clinical stricture resolution at a given time point without unscheduled interventions or a change of treatment strategy.
Procedure related complications ERCP or stent exchange related complications, such as pancreatitis, cholangitis, haemorrhage, perforation and post-insertion pain requiring hospital admission.
Other adverse events Infections, stent migration or stent occlusion in the follow-up periodEarly complications Occurring during the first 30 days from initial stent insertionLate complications Occurring during follow-up until stent removalFollow-up The data on treatment success was collected at one or more time points;
at stent removal, at 6 and 12 months and at the end of follow-up.
4.4 Study IV: Protein expression in benign biliary strictures before and after treatment with metal and biodegradable biliary stents
BBS was induced surgically in 14 pigs in laparotomy by subtotal ligation of the CBD with absorbable sutures causing controlled ischaemia. Two months after induction of BBS, the CBD was cannulated under duodenoscopy. In ERC a tight BBS, estimated length of median 10 mm (range 9–11 mm) was confirmed in all animals.
The groups compared are shown in Figure 7. Five animals had no treatment of the stricture (untreated). From these animals, BBS samples were harvested at two months after the induction of BBS. Nine animals received endoscopic treatment of BBS; in the BDBS group four with a braided self-expandable polylactide BDBS (diameter 7 mm, length 50 mm; custom-made at the Institute of Biomaterials, Tampere University of Technology, Finland) and in the CSEMS group five with an FCSEMS (diameter 10 mm, length 80 mm; Wallstent, Boston Sci, USA). Control samples were harvested from the intact part of the bile duct. During follow-up, stent patency, function and location were confirmed by repeated serum liver function tests and native x-ray. At six months tissue samples were harvested from the stent-treated BBSs and the animals were exsanguinated. All procedures were performed in at the University of Kuopio,

68 Antti Siiki
Finland (now part of the University of Eastern Finland) under general anaesthesia with intubation. The animals received antibiotics for infection profylaxis i.v. cefuroxim before operations and peroral cefalexin for three days afterwards. The animals were fed with standard pig chow and were allowed free access to water and free movement in their pens. Adequate intra- and postoperative analgesia was provided.
The management of protein samples and identification of expression patterns took place entirely in the University of Heidelberg, Mannheim, Germany. The proteins were subjected to a fractionated extraction protocol as described previously (Lohr et al. 2010). After protein labelling for 2-dimensional gel electrophoresis (DIGE), the separated proteins in DIGE gels were visualised using image analysis software. Gel staining, digestion, protein extraction and identification of protein sequences were performed according to earlier published methods (Hellman et al. 1995; Mortz et al. 2001).
Figure 7. Protocol of Study IV. In 14 Yorkshire pigs, an ischaemic stricture was induced by subtotal ligation of the CBD. Five animals formed a control group (Intact BD) and five were left untreated (BBS). At two months ERC was performed and polylactide BDBS or FCSEMS was implanted across the stricture in four (BDBS) and five pigs (CSEMS) respectively. The drawing is from the archives of Docent Johanna Laukkarinen, and presented with her permission.

69Endoscopic Management of Benign Biliary Strictures
4.5 Study V: Biodegradable biliary stent in the endoscopic treatment of cystic duct leak after cholecystectomy.
The first patient enrolled in the prospective study of endoscopic BDBS use in cystic duct leak was a previously healthy 64 year-old male admitted two days after an elective open CCY with elevated temperature and CRP and upper abdominal pain. Trans-abdominal ultrasound and CT scan revealed a 6 cm fluid accumulation in the gallbladder bed without signs of biliary obstruction or concomitant vascular injury. The MRCP did not show any CBD stones, but failed to accurately identify the site of the bile leak. A radiologist inserted a percutaneous 8F pigtail drain under ultrasonic guidance into the fluid accumulation, from which elevated bilirubin confirmed a post-operative bile leak.
As the bile flow into the drain continued for eight days after surgery, ERCP was performed under conscious sedation. An anti-inflammatory suppository of diclofenac was given an hour before ERC. Duodenal peristalsis was reduced with buscopan i.v. The patient was receiving i.v. meropenem treatment. A standard duodenoscope with air insufflation was used. The cholangiography revealed a slight leakage of contrast in the vicinity of the cystic duct stump (Figure 8).
Before stent implantation, a long stiff guidewire was replaced. A custom made braided non-covered self-expandable biodegradable PDX stent with golden radiopaque markers at both ends and 40 mm in length with a post-deployment diameter of 8 mm (Ella CS, Czech Republic) was then inserted (Figure 8 and 9).

70 Antti Siiki
Figure 8. BDBS insertion. A. Cholangiography image from ERCP showing a suspected leak of bile from the stump of the cystic duct just below the surgical clips (arrow). A percutaneous pigtail drain is visible on the left and the implantation device on the right side of the duodenoscope. B. Insertion of BDBS. The arrows indicate the radiopaque markers at both ends of the stent. C. Endoscopy image of insertion of BDBS. D. Endoscope image of the implanted BDBS. The distal end of the stent is visible from the duodenum and the guidewire is still inside the stent. Re-printed with permission of the copyright holder, published in J Laparoendosc Adv Surg Tech 2015; 25(5): 419–22, Siiki et al.

71Endoscopic Management of Benign Biliary Strictures
Figure 9. The braided self-expandable biodegradable polydioxanone (PDX) non-covered biliary stent with golden radiopaque markers at both ends with a post-deployment diameter of 8 mm and the endoscopic implantation device with the compression tool for stent loading (Ella CS, Czech Republic). Re-printed with permission of the copyright holder, published in J Laparoendosc Adv Surg Tech 2015; 25(5): 419–22, Siiki et al.

72 Antti Siiki
5 STATISTICS
In Study I statistical analysis was performed using IBM SPSS Statistics 19.0 (IBM Computer Software, USA). Categorial variables were compared using Chi-square test and calculating odds ratios and their 95% confidence intervals. In Study IV, variables were compared using 2-tailed Student’s t-test. In both of these, a probability of <0.05 was regarded as significant. In Studies II and V no statistical analyses were performed due to the nature of the study settings (small cohort in Study II, case report in Study V)). In Study III an analysis of the systematic review and a meta-analysis were performed by a statistician. The statistical analysis of the review comparing two methods was performed using metaprop function in Meta Package for R (Software environment for statistical computing and graphics, version 2.13.0, The R Foundation for Statistical Computing, Austria). Arcsine transformation was applied for comparisons where either of the groups (CSEMS or PS) contained at least one study with a proportion of 100%, otherwise untransformed proportions were used. Using the proportion estimates and confidence intervals obtained from the systematic review, the statistical significances for the differences between the groups were evaluated using unpaired, 2-tailed Student’s t-test, and an association was considered significant when the exact significance level of the test was p < 0.05.

73Endoscopic Management of Benign Biliary Strictures
6 ETHICAL ASPECTS
All studies were carried out in accordance with the Helsinki Declaration. In Study I the protocol was approved by the Ethics Committee of KHKS and in Study V by the Regional Ethics Committee of Pirkanmaa Hospital District. For Study V informed consent was acquired from the patient for the research use of a biodegradable stent. In Study IV the protocol was reviewed and approved by the Provincial Government of Eastern Finland and the Animal Ethics Committee of the University of Kuopio, Finland (now part of University of Eastern Finland). Studies II and III involved no ethical issues because the use of SOC in Study II was part of regular patient care and Study III consisted of a literature review only.

74 Antti Siiki
7 RESULTS
7.1 Study I: ERCP success rates and complications in a Finnish central hospital
Demographics, indications and success rate
A total of 1,207 consecutive ERCPs were performed on 809 patients. Of all procedures, 79% were planned electively and 21% were acute cases where ERCP was perfomed less than 72 hours after admission. Of the procedures 8.7% were planned second attempt procedures, taking place 2–14 days after either a failed or intentionally aborted initial ERCP, The most common initial working diagnosis or indication for ERCPs was CBD stone in 28%, unspecified icterus in 24%, suspected malignancy in 19%, acute pancreatitis in 6%, chronic pancreatitis in 5% and benign pancreto-biliary disease in 6% of the cases. A biliary stent exchange was performed in 7.6%. Any kind of biliary stent was inserted in 14% of the cases: for malignant stricture in 11% and for other reasons in 3.3% of these 1,207 ERCPs.
The papilla was intact i.e. no earlier sphincterotomy had been performed in 68% of the procedures (n=825, 61% females, median age 70 years). Data on cases with intact papilla was considered the most relevant in terms of the success rate of cannulation and incidence of complications. In the cases with the papilla intact, CBD stone was the most common working diagnosis or indication at the time of ERCP (32%), followed by malignant biliary obstruction (21%) and icterus with unspecific diagnosis at the time of the procedure (21%). Benign pancreato-biliary indications accounted for 5% of the cases (Table 7).
Cannulation of the desired duct was achieved in 89% of the procedures. With intact papilla complete stone extraction was successful in 91% and bile duct obstruction was relieved completely in 80% of procedures with an intact papilla.

75Endoscopic Management of Benign Biliary Strictures
Table 7. Indications or working diagnoses of the 825 ERCPs with intact papilla, amounting to 68% of all cases. Re-printed with permission of copyright holder, Siiki et al. Scand J Surg 2012;101:45–50
Indication or work-up diagnosis n %CBD stone 266 32 %Malignancy 173 21 %Bile duct obstruction or jaundice without accurate diagnosis 172 21 %Acute biliary pancreatitis 64 7.8%Acute cholangitis 59 7.2%Chronic pancreatitis 35 4.2%Dysfunction of sphincter of Oddi 10 1.2%Bile leak after cholecystectomy 7 0.8%Other benign pancreato-biliary disease 39 4.7%Total 825 100%
Complications
Overall complication rate was 11% in ERCPs with intact papilla (Table 8). The majority of the complications (77 %) were mild or moderate, i.e. they were managed conservatively and necessitated less than ten days of hospitalisation. Two of the 16 (1.9%) cases of PEP were severe and required surgery, but the patients recovered. Haemorrhage occurred after 16 (1.9%) of the procedures. Perforations caused by EST or guidewire were observed in eight (1.0%) patients, three of whom required surgery. Most of the cases were retroperitoneal and were noticed during the same endoscopy. Seventeen (2.1%) patients developed cholangitis, none of which was related to mortality. One of the cholangitis patients was laparotomised for suspected duodenal perforation after referral to another hospital.
Other adverse events occurred in 4.2% of ERCPs with intact papilla. The most common cases were pneumonia, infection of unknown origin, cerebral infarction, cardiac event and urinary retention or urinary tract infection. Additionally two patients (0.2%) with cholecystitis were operated on. The overall complication rate was 9.8% in the entire study population of 1,207 procedures.
Risk factors of complications
Precut sphincterotomy was a risk factor for moderate or severe PEP (OR 3.8, 95 % CI 1.1–12.8, p 0.022). Age over 60 years was a risk factor for other complications (e.g. cardiac event, pneumonia) graded moderate or severe (OR 3.6, 95% CI 1.1–12.0,

76 Antti Siiki
p 0.027). There was a slight trend towards increased incidence of PEP, haemorrhage and perforation after precut as well as towards more frequent PEP in patients less than 50 years of age, but the differences were not statistically significant.
Table 8. Complications, adverse events and ERCP-related mortality in 825 ERCPs with intact papilla and their severity grades based on the need for interventions and the length of associated hospitalisation. Age: median (interquartile range); PEP: post-ERCP pancreatitis (Re-printed with permission of copyright holder, Siiki et al. Scand J Surg 2012;101:45–50)
Complication Severity Age (years) n (%) ERCP related mortality
Pancreatitis MildModerateSevere
Total 63 (44–74)
4 (0.5%)10 (1.2%)2 (0.2%)
16 (1.9%)
0000
Haemorrhage MildModerateSevere
Total 74 (53–83)
1 (0.1%)9 (1.1%)6 (0.7%)
16 (1.9%)
0022
Cholangitis MildModerateSevere
Total 77 (58–83)
3 (0.3%)12 (1.5%)2 (0.2%)
17 (2.1%)
0000
Perforation MildModerateSevere
Total 72 (68–81)
5 (0.6%)–
3 (0.4%)8 (1.0%)
0000
Other MildModerateSevere
Total 79 (68–88)
5 (0.6%)20 (2.4%)10 (1.2%)
35 (4.2%)
0000
Overall complications 75 (63–83) 91 (11%) 2 (0.2%)
Mortality
In the procedures with the papilla intact, the ERCP related mortality was 0.2% (n=2). Both of these cases resulted from haemorrhage in patients with severe co-morbidities. Overall mortality in 30 days was 3.3% (n=27). Eighteen (2.2%) of these were caused by cancer and seven (0.8%) by other, non-ERCP-related events, such as pneumonia or cardiac disease.
In all 1,207 procedures ERCP related mortality was was 0.4% (n=5). The details of these cases are presented in Table 9. In addition to the abovementioned two cases of haemorrhage, two patients died after perforation and the death of a one patient nine days after biliary stent insertion was considered ERCP-related.

77Endoscopic Management of Benign Biliary Strictures
Table 9. ERCP -related 30-day mortality after 1,207 procedures. Details of the five patients who died of complications are presented. The two uppermost cases had an intact papilla i.e. had not undergone previous ESTCause of death
Age/Sex
Co-morbidities Intact papilla
ERCP indication ERCP procedure Comment
Haemorrhage, acute myocar-dial infarction
83/F Hypertension, coro-nary heart disease, acute myocardial infarction
Yes CBD stones in percuta-neous cholangiography (T-tube)
EST, stone extraction
Severe bleeding at 7 days
Haemorrhage 88/F Dementia, hyper-tension, congestive heart disease, atrial fibrillation, sick sinus syndrome
Yes Inoperable pancreatic carcinoma, bile duct obstruction, PTD removed by patient
ERCP and precut sphincterotomy, no access to biliary duct
Severe early bleeding
Perforation 76/F None No Inoperable pancreatic carcinoma, bile duct obstruction
EST, dilation of CBD stricture, stent insertion
Laparotomy for duodenal perforation
Perforation 82/F None No Inoperable pancreatic carcinoma, bile duct obstruction
Replacement of obstructed biliary duct stent
Managed non-operatively
Multi-organ fail-ure of unknown origin
68/M Atrial fibrillation, chronic pancreatitis, congestive heart disease, mechanical aortic valve, anticoag-ulation therapy
No Unclear biliary duct obstruction
EST, biliary stent insertion
Intensive care for multi-organ failure for 9 days
7.2 Study II: Initial experience of SpyGlass cholangioscopy in biliary strictures secondary to sclerosing cholangitis
Eleven patients (5 female, median age 45, range 24–66) underwent ERC with SOC for PSC. The baseline characteristics of the study population are presented in Table 10. The median time from the diagnosis of PSC was eight years (range 1–28 years). All but one patient were on ursodeoxycholic acid treatment for PSC and all patients had ulcerative colitis. In nine patients (82%) a previous ERC, and in six (55%) a previous sphincterotomy had been performed. One patient had had an earlier temporary biliary stent therapy for CBD stricture years before the current endoscopy. Another patient had undergone conservative treatment for a mild post-ERC perforation years earlier. Serum tumour markers CA19-9 and CEA were within normal range in all patients. The progression of PSC was classified according to Amsterdam criteria (Table 2, Table 10). Both intra- and extrahepatic changes were present in eight (73%) patients; the rest had intrahepatic disease.

78 Antti Siiki
Table 10. Details of ERC and results of tissue analysis in patients of Study II. PSC; primary sclerosing cholangitis, MRI; magnetic resonance cholagiopancreatography, LFT; liver function tests. ERC; endoscopic retrograde cholangiography, Stricture classification: intra and extrahepatic disease according to Amsterdam classification; Cytology: cytology class. Inadeq: Sample inadequate. Re-printed with permission of copyright holder, published in Scand J Gastroenterol 2014; 49:1385–90, Siiki et al.
Stricture classificationNo Age/sex Indication Intrahep Extrahep Cytology DNA
indexS-phase Histology
1 43/M Progression in MRI III IV 2 1 1.8 Inadequate2 28/M Progression in MRI,
elevated LFTI Normal 2 1.2 7.2 Inflammation
3 44/F “ II II 2 1 2.1 Normal4 41/M “ III II 1 1 NA Inflammation5 45/F Elevated LFT, no
previous ERCII I 2 1 1.2 Inflammaton
6 54/F Elevated LFT II II Inadeq. Inadeq NA Regenerative atypia
7 51/M More than 5 year from ERC
I IV 2 1 NA Fibrosis
8 50/F Progression in MRI III I 2 1 0 Fibrosis9 49/F “ III II 2 1 6.8 Inlammation
10 66/M “ I Normal Inadeq. Inadeq NA Fibrosis11 24/M Over 5 years from
ERCI Normal 1 1 0 Fibrosis
Under ERCP, EST was performed in 90% of patients. Both brush samples for cytology and flow-cytometry were successfully obtained from desired locations in all patients as well as direct visualisation of the epithelium by SOC and guided biopsy. The stricture could be completely traversed with a cholangioscope in six cases (55%). In others, a tight impassable dominant stricture was located intrahepatically, except in one patient, with a narrow class IV extrahepatic stenosis. Bile duct stones, initially unidentified in MRCP and cholangiography, were detected in SOC in one patient and removed by extraction balloon.
Out of nine patients (82%) with adequate brush samples for cytologic analysis, the result was Amsterdam class 2 in seven and class 1 in two. The flow-cytometric analysis showed normal diploidic DNA content in all but one patient, who had an elevated DNA index of 1.21 and normal S-phase of 7.2%, which were considered suspicious for malignancy. The biopsy specimens were adequate for successful histological analysis in ten (91%) patients; one normal bile duct epithelium and seven regenerative, fibrotic or chronic inflammatory changes (Table 10). Most of the histologic specimens consisted of stromal cells and only a small amount of epithelial tissue.

79Endoscopic Management of Benign Biliary Strictures
Two patients developed immediate complications from which they all recovered uneventfully; one 28 year-old male and one 43 year-old male developed a moderate PEP within three days after ERC. In addition, one 41 year-old male was observed for mild post-ERC pain without pancreatitis.
The follow-up of PSC patients was planned individually in accordance with the guideline of our institution, which is essentially similar to that used in the Endoscopy Unit of Helsinki University Hospital and is presented in Figure 4 (Boyd et al. 2014). The median length of follow-up at the time of analysing the data was 22 months (range 16–24 months). Patient #1 with severe cholangiography changes and rapid PSC progression was referred to the liver-transplantation unit of Helsinki University Hospital after the SOC-ERCP procedure, but LT has not so far been necessary. He has later undergone endoscopic stenting and stent removal. Patient #2 with initially aneuploidic flow cytometry was scheduled for re-ERC at six months with normalised results. Other patients were scheduled for outpatient follow-up, during which none of them had progression of PSC or episodes of acute cholangitis. The patient with CBD stones removed has been asymptomatic ever since.
7.3 Study III: Meta-analysis comparing covered self-expanding metal stents and multiple plasic stents in benign biliary stricture
Twenty-five studies met the final inclusion criteria for the review: 13 studies on mPSs with 570 patients and 12 studies on CSEMSs with 376 patients. The CSEMS and PS groups were comparable in terms of age and sex.
All 13 PS studies reported an endoscopic technique with gradually increasing number of polyethylene 7-10 F plastic stents inserted and exchanged tri-monthly for up to 12 months. Three of the CSEMS studies used partially covered stents (Behm et al. 2009; Chaput et al. 2010; Kahaleh et al. 2008). The median duration of stent therapy was shorter in the CSEMS (4.5 months) than in the PS group (11 months) (p=0.001). Fewer ERCP sessions were needed in the CSEMS than in the PS group (median 1.5 and 3.9, p=0.002). When cases of CP were analysed separately, the difference in the duration of stent therapy (median 4.8 vs. 16 months, p=0.1) or in the number of ERCPs (2.0 vs. 4.2, p=1.0) was statistically insignificant. The primary stent insertion and the eventual stent removal were equally successful in the CSEMS and PS groups.
In 83% of CSEMS studies and 100% of PS studies adequate data at 12 months of follow-up was obtained, and was used in the final analysis. The results at the end of the total follow-up time were not comparable, as the length of follow-up was shorter in the CSEMS group (14 vs. 49 months, p=0.003).

80 Antti Siiki
There was no difference in the early complications (pancreatitis, cholangitis, perforation and haemorrhage) between the CSEMS and PS groups in all stricture aetiologies. However, late complications or any adverse events (pain, infection, stent occlusion and stent migration) occurred less often with CSEMS than in PS (5% vs 14%, p=0.006) when all aetiologies were combined (95% CI 2–7% and 9–19% respectively). There were fewer late complications in the CSEMS (3 vs. 67%) than in the PS group in CP aetiology (95% CI 0–13% vs. 17–99%, p=0.02). No statistical difference was found in the complication figures of other aetiology groups.
The clinical success of treatment according to stricture aetiology at the end of the stent therapy and at six and 12 months after stent removal is presented in Figure 10. In CP strictures there was tendency for better clinical success in CSEMS treatment at 12 months after stent removal: 77% vs. 33% (95% CI 61–94% vs. 4–63%, p=0.06) in CSEMS and PS respectively. At other time points of follow-up the difference was also observable: at stent removal 80% vs. 38% (95% CI 62–93% vs. 12–68%, p=0.02) and at six months 74% vs. 33% (61–86% vs. 4–63%, p=0.02). In other aetiologies except CP there was no difference in the success rate. The overall clinical success of CSEMS and PS in all aetiologies at stent removal was 87% vs. 85% (p=0.8) and at 12 months 79% vs. 77% (p=0.9).

81Endoscopic Management of Benign Biliary Strictures
7.4 Study IV: Protein expression in benign biliary strictures before and after treatment with metal and biodegradable biliary stents
Proteins potentially associated with tissue damage and healing, apolipoprotein-A1, annexin-A4, galectin-2, transgelin, myosin light polypeptide-6 (MLP-6), albumin, superoxide dismutase-1, heat-shock protein beta-6, peroxiredoxin-5 and muscle creatine kinase were screened for. Expression pattern of annexin-A4, galectin-2, transgelin and MLP-6 from an intact BD, untreated BBS and after treatment with BDBS or CSEMS is presented in Figure 11. For other proteins no differences were found.
Tissue samples were analysed from pigs with intact bile duct (intact BD, n=5), untreated BBS (n=5) and after six months of therapy with BDBS (n=4) or CSEMS (n=5). In BBS, expression of annexin-A4 was reduced to 37% and expression of galectin-2 was reduced to 14% (p=0.03) compared to the intact BD. Fragmented transgelin expression was increased by 190% compared to the intact BD. No difference in myosin light polypeptide-6 (MLP-6) expression was observed (Figure 11).
Figure 10. Success rate of CSEMS and PS therapy in strictures by aetiology (A) chronic pancreatitis (CP), (B) post-liver transplant (LT), and (C) other aetiologies immediately after primary stent insertion and after 6 and 12 months (mo) in Study III. *p<0.05, overlapping confidence intervals, see text for details on statistical significance. Re-printed with permission of copyright holder, published in J Clin Gastroenterology 2014; 48:653–453, Siiki et al.
A. Chronic pancreatitis B. Post-liver transplantation
C. Other aetiology
%
%
%
80 74 7791 85 85
92
86
88 85
84 85
38 33 33
8876 72
Immediate
Immediate
Immediate6 mo 12 mo 6 mo 12 mo
6 mo 12 mo
100 100
50
0
50
0
100
50
0

82 Antti Siiki
After BDBS and CSEMS treatment the expression of annexin A4 remained at the level seen in BBS. After BDBS treatment the expression of galectin-2 returned to the level of intact BD, whereas after CSEMS treatment the expression remained at the low level seen in the BBS (p=0.02). Transgelin expression, being zero in intact BD, was increased to 450% in CSEMS-treated animals compared to BDBS. Expression of fragmented transgelin remained at the elevated level of untreated BBS after both BDBS (p=0.03) and CSEMS treatment. MLP-6 expression was increased to 300% after BDBS treatment, but remained unchanged after CSEMS treatment (Figure 11).
Figure 11. Expression of annexin A4 (A), galectin-2 (B), transgelin (C) and myosin light polypeptide-6 (D) proteins based on immunohistochemical analysis. Four samples (columns from left to right) were compared: intact bile duct (BD), BBS at two months (BBS 2 mo) from stricture induction and after six months treatment with either BDBS or CSEMS. In figure B p<0.05 in BBS 2 mo compared to intact duct, CSEMS compared to intact duct and CSEMS compared to BBS 2 mo. In figure C, p<0.05 in BDBS compared to intact duct. Re-printed with permission of copyright holder, under review in BMC Gastroenterolgy 2015, Siiki et al.

83Endoscopic Management of Benign Biliary Strictures
7.5 Study V: Biodegradable biliary stent in the endoscopic treatment of cystic duct leak after cholecystectomy
Endoscopic insertion of the BDBS was successful for the treatment of the post-CCY biliary leak. The stent was adjusted to the proper location in the CBD with its distal end visible inside the duodenum (Figure 7). The external drain was removed on day 7 after ERC at an outpatient visit. Although complications related to ERCP or stent did not occur during the first 30 days, the patient had been treated with peroral antibiotics for an episode of acute infection, presumably acute cholangitis, at 1.5 months from ERC. At three-month follow-up MRI the stent was patent and in the right location (Figure 12), whereas at six months it was no longer visible.
Figure 12. MRI image at three months after BDBS insertion. BDBS is visible fully expanded in the distal CBD (arrow). Re-printed with permission of the copyright holder, published in J Laparoendosc Adv Surg Tech 2015; 25(5): 419–22, Siiki et al.

84 Antti Siiki
8 DISCUSSION
This thesis summarises current endoscopic BBS management based on a literature review and five original publications. In indeterminate biliary strictures, the primary goal is to exclude malignancy and set at least a temporary diagnosis. While patient history, serum samples, radiologic imaging and ERCP with brush samples are often sufficient in the primary evaluation of indeterminate strictures, repeated ERCP or advanced endoscopic methods such as cholangioscopy with guided biopsies may be necessary in unclear cases. After a diagnosis of BBS, an appropriate treatment strategy may be selected; this may include insertion of a single plastic or multiple plastic stents, which is often the case in post-operative strictures affecting the biliary confluence, or FCSEMSs that are most appropriate for strictures in the CBD and CHD. Biodegradable stents are a convincing alternative of which clinical experience is needed before embarking on widespread clinical use.
The impact of this thesis on the literature is in providing data on ERCP practice in a Finnish central hospital as well as substantiating and complementing the findings of earlier studies on SOC diagnostics in PSC patients. In addition, the thesis clarifies the issue of the optimal stent therapy in benign CBD strictures. Furthermore, it introduces possibilities of proteomic research that could perhaps lead to better comprehension of BBS pathogenesis and improved stent development and stent therapy. Lastly, a pioneering endoscopic therapy with BDBS is reported, which may have further applications as more experience accumulates.
The first publication evaluating ERCP practice in a Finnish central hospital showed that even in a low-volume centre it is possible to achieve an appropriate success rate in cannulations (Colton and Curran 2009; Enochsson et al. 2010; Kapral et al. 2008) and an acceptable incidence of post-ERCP complications (Andriulli et al. 2007; Christensen et al. 2004; Colton and Curran 2009; Testoni et al. 2010). The case-mix reported in our study was close to what has been reported from other non-university hospitals (Colton and Curran 2009; Garcia-Cano Lizcano et al. 2004), and, as expected, differed considerably from that of academic centres in terms of numbers of complex procedures (Enochsson et al. 2010). Basic ERCP such as CBD stone removal, carrying the lowest risks is more common in low-volume centres than in specialised units (Enochsson et al. 2010; Garcia-Cano Lizcano et al. 2004; Testoni et al. 2010). This needs to be kept

85Endoscopic Management of Benign Biliary Strictures
in mind when complication figures are compared. The risk factors for PEP are known to be cumulative (Freeman 2012), including e.g. female sex, young age and challenging cannulation (Cotton et al. 2009; Halttunen et al. 2014; Testoni et al. 2010; Williams et al. 2007). The trend seen in our paper is consistent with earlier findings.
Reviewing own complications is crucial in the process of continous improvement of quality and education, and is also needed in balancing the risk for future complications (Anderson et al. 2012). The value of a nationwide register in quality control and acquiring the “big picture” of ERCP practice, indications, complication rate and differences in patient mix between centres and adequate referral pattern of complex cases has been demonstrated in the large Swedish Gallriks -studies (Enochsson et al. 2010; Enochsson et al. 2013). Unfortunately no such national registry so far exists in Finland. This makes it even more important to run investigations like that reported in Study 1, where the advantages were the careful inclusion of over 1,000 consecutive ERCPs in a single domestic central hospital in a quality control setting, and a separate analysis of the procedures with intact papilla. A retrospective study may obviously include errors in terms of data collection and interpretation. The study concluded that ERCP quality is at an appropriate level in a Finnish non-university centre, at least when the procedures are assigned to a few endoscopists and the standards of practice are critically monitored, as was the case here.
According to the second study, Spyglass cholangioscopy is safe and feasible in the evaluation of PSC with an acceptable rate of successful biopsies. The findings confirm the usefulness of SOC in indeterminate biliary strictures and the diagnostics of BBS as well as in PSC (Awadallah et al. 2006; Chen and Pleskow 2007; Draganov et al. 2011; Kalaitzakis et al. 2012; Manta et al. 2013; Rey et al. 2014; Tischendorf et al. 2006). A similar finding was recently published from Sweden, encouraging SOC use in selected cases of PSC (Arnelo et al. 2015). In our study the rate of PEP was 18%, which, being partly attributable to the learning curve with SOC in our institution, is consistent with rates reported in other studies (Awadallah et al. 2006; Tischendorf et al. 2006; Arnelo et al. 2015). Because the complication risk is elevated both in PSC (Ismail et al. 2012; von Seth et al. 2015) and for performing SOC (Draganov et al. 2011; Lubbe et al. 2015, Arnelo et al. 2015), the indications and true role of SOC in the surveillance of PSC have to be carefully analysed. Study II was the first report from Finland on SOC use in PSC, and one of the first papers on SOC safety in PSC in general. Rare PSC cases were deliberately collected into this consecutive series. It can be argued that the number of patients is insufficient to demonstrate the true rate of complications and the follow-up is short for the diagnostic yield. A large multicentre study with long follow-up is called having as its end-points the influence of SOC on surveillance as well as diagnosing dysplasia and exlusion of CCA. As a conclusion from Study II, the complication risk

86 Antti Siiki
of SOC is tolerable and provides additional diagnostic information in PSC patients. We suggest that SOC should be a second-line option in conjunction with MRI, cytology and flow cytometry as a part of the multi-disciplinary surveillance of PSC in experienced centres, e.g. in cases with suspicious cytologic findings or aneuploidy. The next generation of SOC instruments will without doubt change our thinking on SOC possibilities as the quality of the image and thus diagnostics improve (Parsi et al. 2014).
The third study showed that treatment with CSEMSs is more successful with comparable complications and smaller numbers of ERCP sessions than multiple PS in CP related CBD strictures. The findings were compatible with the clinical expectations and the recently published pioneering Finnish RCT (Haapamaki et al. 2015). The results were also in accordance with other recent studies reporting long-term success rates of 80–90% with FCSEMS in CP (Deviere et al. 2014; Kahaleh et al. 2013). In the studies included in the meta-analysis, a very short stent indwelling time of 4–6 months was used; however, modern FCSEMSs may be safely kept in place much longer in CP-related strictures, presumably further improving the stricture remodelling and long-term effect (Deviere et al. 2014). The migration rate remains a problem even with the current FCSEMSs, although it does not automatically lead to treatment failure (Deviere et al. 2014). In LT or other post-operative strictures, where later studies have shown encouraging results (Deviere et al. 2014; Kaffes et al. 2014; Kahaleh et al. 2013) the meta-analysis was inconclusive. Further studies with adequate follow-up are needed to ascertain the long-term recurrence rate of FCSEMS-treated strictures, as well as the cost-efectiveness in comparison to mPSs or surgery. It can be summarised, however, that up to 12 months indwelling time with modern FCSEMSs is feasible and yields impressive clinical results in selected BBS. Particularly strictures secondary to CP, which are typically treatment resistant and located in the distal CBD, as well as LT-related anastomotic strictures are best suited for FCSEMS therapy (Deviere et al. 2014; Kaffes et al. 2014; Haapamäki et al. 2015). A single PS has and will continue to have a role as a bridge to surgery and e.g. in PSC related dominant strictures. The strategy of gradual stricture remodelling with mPS therapy remains relevant in hilar strictures or multifocal strictures arising from previous surgery, which are different entities than calcifying CP affecting the distal CBD. The main drawback of mPS therapy in post-operative strictures is the need for repeated ERCP sessions with associated burden on the patient and costs (Costamagna and Boškoski 2013). To give a perspective in the Finnish health care system, the cost of an ERCP procedure varies between 800 and 1200 euros, a FCSEMS costs approximately 800 euros and a PS around 80 euros. Thus a year’s treatment with mPSs consisting of at least four ERCPs with progressive insertion of up to seven PSs is over twice as expensive as therapy with a single FCSEMS necessitating ERCP procedures only twice: for insertion and removal.

87Endoscopic Management of Benign Biliary Strictures
The strength of Study III was a meticulous literature search and careful selection of studies for inclusion. The meta-analysis was designed with and performed with the help of a statistician. However, all the studies included were uncontrolled low-quality studies, with confounding factors due to heterogenity, making it hard to draw solid conclusions on comparison of treatment groups even after meta-analysis. Furthermore, the number of cases was relatively small in aetiology-specific subgroups. In addition, the variation in the definition of clinical success and relatively short follow-up times were the major limitations. At the time of the preparation of Study III, no high-quality papers on FCSEMS with a long follow-up had been published. Thus our results, already updated by a recent multi-centre RCT, lend support to the clinical use of FCSEMS in CP related CBD strictures.
The fourth paper concluded that the expression of proteins related to tissue healing, such as galectin-2 and annexin-A4, have a different expression pattern in ischaemic BBS than in intact bile duct. Furthermore, a difference was noted after treatment with either BDBSs or FCSEMSs. The proteomic response to BDBS resembling intact bile duct may suggest a beneficial effect of BDBSs over FCSEMSs in BBS. However, in the absence of similar research of BBS proteomics, it remains unknown which benefits BBS healing most, change towards intact bile duct or no such change. The potentially more beneficial effect does not contradict with earlier findings, where BDBS stents did not cause scar formation or histologic changes that could potentially precede re-stricturing or damaging biliary epithelium (Ginsberg et al. 2003; Laukkarinen et al. 2007a). The physiology and potential clinical applications of variation in tissue response and lack of epithelial hyperplasia warrant additional studies. When FCSEMSs are increasingly used in BBS with long indwelling times, our findings constitute an interesting point of comparison to recent reports of de-novo strictures after FCSEMSs due to late epithelial response, which has been thought to result from the forceful radial expansion of metal stents and at least partly from covering materials (Ginsberg et al. 2003; Irani et al. 2014; Phillips et al. 2011). The differences in protein expression imply that the optimal result of endoscopic therapy also depends on the molecular level mechanisms of stricture pathogenesis, scar formation and response to stent of the biliary epithelium. Study IV was the first to investigate the pathogenesis of BBS and to compare the tissue response to CSEMSs and BDBSs in terms of protein expression pattern in a carefully performed and documented experimental ischaemic large animal model. The BDBS was made of PLA, which is a slightly different co-polymer from PDX used in the BDBSs currently commercially available. The future prospects in the endoscopic management of BBS include diagnostic and prognostic biomarkers, possible target molecules for therapy and improved stent design to reduce tissue damage. Furthermore, the biodegradable

88 Antti Siiki
polymers used for drug release are presumably among the next technological advances in stent design (Lorenzo-Zuniga et al. 2014; Tokar et al. 2011).
The fifth study demonstrated the feasibility of the novel endoscopic implantation device of BDBSs in the treatment of post-operative bile leak as an alternative to traditional PS therapy. The degradation and predictable behaviour of PDX BDBS is also well documented in human BBS (Freudenberg et al. 2004; Lorenzo-Zuniga et al. 2014; Mauri et al. 2013). The lack of an endoscopic insertion device has prevented endoscopic use until this experience. It is reasonable to conclude that an 8mm diameter BDBS provides better bile flow than a smaller diameter PS (Laukkarinen et al. 2007a). The usefulness of BDBSs in the leak of a cystic duct may be extrapolated to BBS of the CBD, since the implantation device may be easier to introduce into a dilated duct above the stenosis. It is still unknown whether the radial expansion effect of the current BDBS, reportedly up to 30% less than in CSEMS in the early PLA stent experiments (Ginsberg et al. 2003) and 10% less in 8mm bore BDBS made of PDX (Grolich et al. 2015) is sufficient for successful stricture remodelling, prevention of migration and long-term success. In this sense, the results from its percutaneous use are encouraging, but the numbers are small, consisting mostly of post-operative strictures (Mauri et al. 2013). The cost of BDBSs may be justified by rendering unnecessary repeated endoscopy either for CSEMS removal or multiple PS insertion. This may be particularly important in patients with alcohol-related CP, often associated with poor compliance (Kiehne, Folsch, Nitsche 2000), which may lead to difficult removal or septic cholangitis if the stents are inadvertently left in situ (Irani et al. 2014). The episodes of acute cholangitis during the stent therapy, noted in our case report and in up to 30% of the cases during percutaneous BDBS therapy warrant attention in future studies (Mauri et al. 2013). Study V was the first report of a successful endoscopic insertion of PDX BDBS in a single patient with thorough follow-up. The feasibility of BDBS implantation and the excellent results during six-month follow-up encourage us to continue with the prospective cohort trial of endoscopic BDBS use in BBS and in bile leaks.
During the past decade extensive research has been conducted on endoscopic BBS management and the medical technology has rapidly developed. Earlier studies have shown that the diagnosis of BBS is often complex and the treatment strategy of BBS has to be chosen according to the stricture aetiology. The diagnostics of biliary strictures may be safely improved by selective use of SOC even in PSC patients. In addition, the clinical use of CSEMSs is encouraged in benign CBD strictures, especially in CP. This thesis also supports the usefulness of BDBSs, based both on our results from the animal model and on the feasibility demonstrated in the first case report of endoscopic use in humans. As in any invasive procedure, the indications for ERCP and the endoscopic approach to BBS management need to be weighed up against the complication risks.

89Endoscopic Management of Benign Biliary Strictures
9 SUMMARY AND CONCLUSIONS
The present thesis provides data to support the following conclusions and summary:
1) ERCP success rates and complications were for the first time evaluated in a Fin-nish central hospital, showing that high quality level can be achieved in a low-volume ERCP unit.
2) SpyGlass single-operator peroral cholangioscopy is a safe and useful method in diagnostics and surveillance of primary sclerosing cholangitis, and it s role is still evolving.
3) Covered self-expanding metal stents may well be used in selected cases of benign biliary strictures, especially in strictures secondary to chronic pancreatitis. Alt-hough cases of stent migration and cholangitis do occur, the main advantages are the good stricture resolution rate with fewer procedures.
4) The novel biodegradable biliary stents has a different and potentially beneficial effect on biliary epithelium compared to covered self-expanding metal stents ac-cording to the analysis of protein expression in a pig model. Additionally, an ischaemic biliary stricture has a different protein expression pattern than an intact bile duct, and this information may also be beneficial for future clinical applications.
5) Endoscopic insertion of biodegradable biliary stent was successful and without significant complications during the six-month follow-up in the first published case report on the treatment of a post-cholecystectomy bile leak. Even though more experience and more research on the endoscopic use of biodegradable bilia-ry stents are needed, they appear to be promising option for the future treatment of benign biliary strictures.

90 Antti Siiki
10 FUTURE PERSPECTIVES
The future of endoscopic diagnostics of indeterminate biliary strictures may develop in the direction of combining advanced samples such as FISH, DIA or flow-cytometry with standard ERCP with cytologic samples (Barr Fritcher et al. 2014; Halme et al. 2012). Additionally, the analysis of bile juice for diagnostic markers such as pyruvate kinase may offer interesting prospects in evaluation of indeterminate strictures (Navaneethan et al. 2015a). The stepwise approach with additional radiologic modalities, such as contrast enhanced MRI and FDG PET in selected cases will hopefully be of help in unclear cases (Katabathina et al. 2014; Sangfelt et al. 2014). Potential further investigations when standard procedures are non-diagnostic, includes peroral cholangioscopy, preferably with high-definition digital image quality, which enables an impressive view of the ductal lumen and mucosa as well as superior accuracy (Parsi et al. 2014). Additional techniques such as staining could augment the visual diagnostics of SOC (Chen et al. 2011). In SOC the adequacy of biopsies continues to be an issue; the diagnostic accuracy is improved if more biopsies with more tissue are available for analysis (Kalaitzakis et al. 2012). While in recent studies the range of median number of biopsies has been from three to four (Chen et al. 2011; Kalaitzakis et al. 2012), perhaps even more and up to ten biopsies per lesion should be taken (Draganov et al. 2011). The true diagnostic yield of SOC, optimal timing and relation to radiologic imaging in different clinical scenarios require further studies despite the present promising results. Interesting prospects of immediate cytopathologic staining and interpretation in the endocopy suite may provide more accurate diagnosis and help in intraprocedural decisions (Wright et al. 2011).
Future research may eventually show the true diagnostic predictive value and accuracy of SOC-cholangioscopy and targeted biopsies, also in the evaluation of PSC progression and in the exclusion of CCA that remains one of the most difficult problems in BBS management (Eaton et al. 2013). In PSC, narrow-band imaging, also aimed to better visualize mucosal surface abnormalities such as dysplasia by filtering light in the green and blue spectra has already been used experimentally in conjunction with cholangioscopy. Although the first use of this promising method enabled definition of tumour margins in patients with CCA and increased number of biopsies, it did not in a single report increase the detection of dysplasia (Azeem et al. 2014). FDG PET may

91Endoscopic Management of Benign Biliary Strictures
also serve as a more accurate tool than cytologic samples in the exclusion of malignancy in PSC (Sangfelt et al. 2014).
In addition, further research on the molecular basis of stricture formation and response to stents to possibly verify our findings, is eagerly anticipated (Bakhru et al. 2011; Lee et al. 2014).
In the treatment of BBS, recently published randomised studies and others already ongoing studies may modify our thinking on optimal stent selection and perhaps confirm the ideas on the superiority of FCSEMSs over plastic stents in selected cases of BBS (Deviere et al. 2014; Kaffes et al. 2014; Haapamaki et al. 2015). The optimal and safe indwelling time is yet to be defined; it probably varies between six and 12 months (Deviere et al. 2014; Haapamaki et al. 2015). The issue of optimal dilation with or without PS in the dominant strictures associated with PSC will hopefully be clarified in future studies (Ehlken and Schramm 2013). Furthermore, possible benefits of early surgery in CP to manage not only biliary obstruction but also pain and pancreatic insufficiency are currently being investigated (Ahmed Ali et al. 2013). Finally, clinical studies on the endoscopic use of BDBSs in BBS have already been undertaken to gain experience of this promising technology.
While the ever-evolving technology and instrumentation will provide even more advanced diagnostic and therapeutic methods, the risk of complications and patient safety has to be critically considered in all future studies.

92 Antti Siiki
ACKNOWLEDGEMENTS
This thesis was carried out at the Department of Gastroenterology and Alimentary Tract Surgery, Tampere University Hospital, at the Department of Surgery, Kanta-Häme Central Hospital and at the School of Medicine, University of Tampere, during the years 2010–2015.
I warmly thank Head of Department of Surgery, Professor Teuvo Tammela for supporting me to finish my work.
I owe my deepest gratitude both to supervisor, Chief of Alimentary Tract Surgery, Docent Johanna Laukkarinen, and co-supervisor Head of Division, Docent Juhani Sand, for the opportunity to work under their expert guidance in Tampere Pancreas Group. I wish especially to thank Johanna for endless support and optimism throughout the process and Juhani for encouraging feedback and constructive revision of manuscripts. Despite of all your duties, both of you always had time and energy for me and this work.
I would also like to express my thanks to Chief of Surgery Pekka Kuusanmäki, MD, PhD for convincing me to begin scientific research on ERCP in Kanta-Häme Central Hospital and for mentoring the first original publication. I am also grateful to Head of Gastroenterology, Professor Pekka Collin and Head of Radiology, Docent Irina Rinta-Kiikka, the follow-up members of this work, for their excellent collaboration and helpful comment on the manuscripts and the thesis. I am also indebted to other co-authors, especially Heidi Gröhn, MSc, Mika Helminen, MSc, Ralf Jesenofsky, MSc, Professor Minna Kellomäki, Tarmo Koivisto, MD, Professor Matthias Löhr, Joonas Mikkonen, MSc, Docent Isto Nordback, Antti Tamminen, MD, Timo Tomminen, MD and Kaija Vasama, MD for their highly proficient contribution to the publications. I am thankful to research coordinator Mrs. Taina Ahlgren and research nurse Mrs. Satu Järvinen for all their help. I owe special thanks to Chief of Alimentary Tract Surgery, Docent Petri Aitola, who together with the supervisors and Professor Collin, facilitated the completion of the thesis beside my clinical work at the Department of Gastroenterology and Alimentary Tract Surgery.
I wish to sincerely thank Docent Jorma Halttunen and Docent Sari Venesmaa, the official reviewers of the thesis, for providing with excellent comments and criticism to improve the manuscript. I also thank Virginia Mattila, MA, for her expertise in revising the English language.

93Endoscopic Management of Benign Biliary Strictures
I would like to acknowledge all colleagues I have had priviledge to work with and learn from during the years of surgical training. I am particularly grateful to Head of Endoscopic Surgery, Docent Urban Arnelo, for the ERCP fellowship in 2013 in the Karolinska University Hospital, Stockholm, Sweden. Special thanks go to the participants and mentors of the sixth course of international Pancreas 2000 -program as well as the members of Tampere Pancreas Group.
This study was financially supported by Competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital, The Pirkanmaa regional Fund of the Finnish Cultural Foundation, The Finnish Medical Foundation, Mary and Georg Ehrnrooth Foundation, The Finnish-Norwegian Medical Foundation and The City of Tampere.
I express my warmest gratitude to my parents Ritva and Pertti for their kind support. I also wish to thank my brother Johannes, my aunt Marja and my grandparents for believing in me. I am thankful to my friends, especially Ilkka Kivekäs, MD, PhD and Kari Ranta, MD, and all the others that cannot be thanked by name here: friendship with you is extremely valuable in reminding me that there is life outside. Finally, I want to dedicate this thesis to my beloved wife Piia, MD, PhD. Together with our wonderful daughter, you are the best fan club I can ever wish for.
Tampereella 18.5.2015

94 Antti Siiki
REFERENCES
Abdallah AA, Krige JEJ, Bornman PC. 2007. Biliary tract obstruction in chronic pancreatitis. HPB 9(6):421–8.
Aberg F, Isoniemi H, Hockerstedt K. 2011. Long-term results of liver transplantation. Scand J Surg 100(1):14–21.
Ahmed Ali U, Issa Y, Bruno MJ, van Goor H, van Santvoort H, Busch OR, Dejong CH, Nieuwenhuijs VB, van Eijck CH, van Dullemen HM, et al. 2013. Early surgery versus optimal current step-up practice for chronic pancreatitis (ESCAPE): Design and rationale of a randomized trial. BMC Gastroenterol 13:49,230X-13-49.
Ahrendt SA and Pitt HA. 2001. Surgical therapy of iatrogenic lesions of biliary tract. World J Surg 25(10):1360–5.
Akamatsu N, Sugawara Y, Hashimoto D. 2011. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: A systematic review of the incidence, risk factors and outcome. Transplant Int 24(4):379–92.
Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, Cash BD, Decker GA, Early DS, Fanelli RD, et al. 2012. Complications of ERCP. Gastrointest Endosc 75(3):467–73.
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. 2007. Incidence rates of post-ERCP complications: A systematic survey of prospective studies. Am J Gastroenterol 102(8):1781–8.
Arnelo U, von Seth E, Bergquist A. 2015. A prospective evaluation of the clinical utility of single-operator peroral cholangioscopy in patients with primary sclerosing cholangitis. Endoscopy Mar 2015 (e-pub)
Awadallah NS, Chen YK, Piraka C, Antillon MR, Shah RJ. 2006. Is there a role for cholangioscopy in patients with primary sclerosing cholangitis? Am J Gastroenterol 101(2):284–91.
Azeem N, Gostout CJ, Knipschield M, Baron TH. 2014. Cholangioscopy with narrow-band imaging in patients with primary sclerosing cholangitis undergoing ERCP. Gastrointest Endosc 79(5):773,779.e2.
Bakhru MR, Foley PL, Gatesman J, Schmitt T, Moskaluk CA, Kahaleh M. 2011. Fully covered self-expanding metal stents placed temporarily in the bile duct: Safety profile and histologic classification in a porcine model. BMC Gastroenterology 11:76–82.
Bangarulingam SY, Bjornsson E, Enders F, Barr Fritcher EG, Gores G, Halling KC, Lindor KD. 2010. Long-term outcomes of positive fluorescence in situ hybridization tests in primary sclerosing cholangitis. Hepatology 51(1):174–80.
Barbier L, Souche R, Slim K, Ah-Soune P. 2014. Long-term consequences of bile duct injury after cholecystectomy. J Visc Surg 151(4):269–79.
Baron TH S and Davee T. 2013. Endoscopic management of benign bile duct strictures. Gastrointest Endosc Clin N Am 23(2):295–311.

95Endoscopic Management of Benign Biliary Strictures
Baron TH, Harewood GC, Rumalla A, Pochron NL, Stadheim LM, Gores GJ, Therneau TM, De Groen PC, Sebo TJ, Salomao DR, et al. 2004. A prospective comparison of digital image analysis and routine cytology for the identification of malignancy in biliary tract strictures. Clin Gastroenterol Hepatol 2(3):214–9.
Barr Fritcher EG, Kipp BR, Halling KC, Clayton AC. 2014. FISHing for pancreatobiliary tract malignancy in endoscopic brushings enhances the sensitivity of routine cytology. Cytopathology 25(5):288–301.
Barthet M, Lesavre N, Desjeux A, Gasmi M, Berthezene P, Berdah S, Viviand X, Grimaud JC. 2002. Complications of endoscopic sphincterotomy: Results from a single tertiary referral center. Endoscopy 34(12):991–7.
Behm B, Brock A, Clarke BW, Ellen K, Northup PG, Dumonceau JM, Kahaleh M. 2009. Partially covered self-expandable metallic stents for benign biliary strictures due to chronic pancreatitis. Endoscopy 41(6):547–51.
Bektas H, Schrem H, Winny M, Klempnauer J. 2007. Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br J Surg 94(9):1119–27.
Bergquist A, Tribukait B, Glaumann H, Broome U. 2000. Can DNA cytometry be used for evaluation of malignancy and premalignancy in bile duct strictures in primary sclerosing cholangitis? J Hepatol 33(6):873–7.
Bismuth H. 2003. Surgical management of bile duct stricture following laparoscopic cholecystectomy. Acta Chir Belg 103(2):140–2.
Bismuth H and Majno PE. 2001. Biliary strictures: Classification based on the principles of surgical treatment. World J Surg 25(10):1241–4.
Boberg KM, Jebsen P, Clausen OP, Foss A, Aabakken L, Schrumpf E. 2006. Diagnostic benefit of biliary brush cytology in cholangiocarcinoma in primary sclerosing cholangitis. J Hepatol 45(4):568–74.
Boonstra K, Culver EL, de Buy Wenniger LM, van Heerde MJ, van Erpecum KJ, Poen AC, van Nieuwkerk KM, Spanier BW, Witteman BJ, Tuynman HA, et al. 2014. Serum immunoglobulin G4 and immunoglobulin G1 for distinguishing immunoglobulin G4-associated cholangitis from primary sclerosing cholangitis. Hepatology 59(5):1954–63.
Boonstra K, Weersma RK, van Erpecum KJ, Rauws EA, Spanier BW, Poen AC, van Nieuwkerk KM, Drenth JP, Witteman BJ, Tuynman HA, et al. 2013. Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Hepatology 58(6):2045–55.
Boyd S, Arola J, Mäkisalo H, Färkkilä M. 2014. Cytology is in pivotal role at screening and surveillance of PSC (in FInnish). Duodecim 134(22-23):2397–404.
Burak K, Angulo P, Pasha TM, Egan K, Petz J, Lindor KD. 2004. Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol 99(3):523–6.
Burnett AS, Calvert TJ, Chokshi RJ. 2013. Sensitivity of endoscopic retrograde cholangiopancreatography standard cytology: 10-y review of the literature. J Surg Res 184(1):304–11.
Cahen DL, Rauws EA, Gouma DJ, Fockens P, Bruno MJ. 2008. Removable fully covered self-expandable metal stents in the treatment of common bile duct strictures due to chronic pancreatitis: A case series. Endoscopy 40(8):697–700.
Cahen DL, Van Berkel A-M, Oskam D, Rauws EAJ, Weverling GJ, Huibregtse K, Bruno MJ. 2005. Long-term results of endoscopic drainage of common bile duct strictures in chronic pancreatitis. European Journal of Gastroenterology and Hepatology 17(1):103–8.

96 Antti Siiki
Cantu P, Hookey LC, Morales A, Le Moine O, Deviere J. 2005. The treatment of patients with symptomatic common bile duct stenosis secondary to chronic pancreatitis using partially covered metal stents: A pilot study. Endoscopy 37(8):735–9.
Catalano MF, Linder JD, George S, Alcocer E, Geenen JE. 2004. Treatment of symptomatic distal common bile duct stenosis secondary to chronic pancreatitis: Comparison of single vs. multiple simultaneous stents. Gastrointest Endosc 60(6):945–52.
Chan CHY and Telford JJ. 2012. Endoscopic management of benign biliary strictures. Gastrointest Endosc Clin N Am 22(3):511–37.
Chapman MH, Webster GJ, Bannoo S, Johnson GJ, Wittmann J, Pereira SP. 2012. Cholangiocarcinoma and dominant strictures in patients with primary sclerosing cholangitis: A 25-year single-centre experience. Eur J Gastroenterol Hepatol 24(9):1051–8.
Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, Gores GJ, American Association for the Study of Liver Diseases. 2010. Diagnosis and management of primary sclerosing cholangitis. Hepatology 51(2):660–78.
Chaput U, Scatton O, Bichard P, Ponchon T, Chryssostalis A, Gaudric M, Mangialavori L, Duchmann J-, Massault P-, Conti F, et al. 2010. Temporary placement of partially covered self-expandable metal stents for anastomotic biliary strictures after liver transplantation: A prospective, multicenter study. Gastrointest Endosc 72(6):1167–74.
Charatcharoenwitthaya P, Enders FB, Halling KC, Lindor KD. 2008. Utility of serum tumor markers, imaging, and biliary cytology for detecting cholangiocarcinoma in primary sclerosing cholangitis. Hepatology 48(4):1106–17.
Chen YK. 2007. Preclinical characterization of the spyglass peroral cholangiopancreatoscopy system for direct access, visualization, and biopsy. Gastrointest Endosc 65(2):303–11.
Chen YK and Pleskow DK. 2007. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: A clinical feasibility study (with video). Gastrointest Endosc 65(6):832–41.
Chen YK, Parsi MA, Binmoeller KF, Hawes RH, Pleskow DK, Slivka A, Haluszka O, Petersen BT, Sherman S, Deviere J, et al. 2011. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc 74(4):805–14.
Christensen M, Matzen P, Schulze S, Rosenberg J. 2004. Complications of ERCP: A prospective study. Gastrointest Endosc 60(5):721–31.
Colton JB and Curran CC. 2009. Quality indicators, including complications, of ERCP in a community setting: A prospective study. Gastrointest Endosc 70(3):457–67.
Costamagna G and Boškoski I. 2013. Current treatment of benign biliary strictures. Annals of Gastroenterology 26(1):37–40.
Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. 2001. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc 54(2):162–8.
Costamagna G, Tringali A, Mutignani M, Perri V, Spada C, Pandolfi M, Galasso D. 2010. Endotherapy of postoperative biliary strictures with multiple stents: Results after more than 10 years of follow-up. Gastrointest Endosc 72(3):551–7.
Cotton PB. 1972. Cannulation of the papilla of vater by endoscopy and retrograde cholangiopancreatography (ERCP). Gut 13(12):1014–25.
Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. 2009. Risk factors for complications after ERCP: A multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 70(1):80–8.

97Endoscopic Management of Benign Biliary Strictures
Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. 1991. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest Endosc 37(3):383–93.
Damrah O, Sharma D, Burroughs A, Rolando N, Fernando B, Davidson B, Rolles K. 2012. Duct-to-duct biliary reconstruction in orthotopic liver transplantation for primary sclerosing cholangitis: A viable and safe alternative. Transpl Int 25(1):64–8.
de Bellis M, Fogel EL, Sherman S, Watkins JL, Chappo J, Younger C, Cramer H, Lehman GA. 2003. Influence of stricture dilation and repeat brushing on the cancer detection rate of brush cytology in the evaluation of malignant biliary obstruction. Gastrointest Endosc 58(2):176–82.
De Palma GD, Galloro G, Romano G, Sottile R, Puzziello A, Persico F, Masone S, Labianca O, Persico G. 2003. Long-term follow-up after endoscopic biliary stent placement for bile duct strictures from laparoscopic cholecystectomy. Hepatogastroenterology 50(53):1229–31.
de Reuver PR, Rauws EA, Vermeulen M, Dijkgraaf MG, Gouma DJ, Bruno MJ. 2007. Endoscopic treatment of post-surgical bile duct injuries: Long term outcome and predictors of success. Gut 56(11):1599–605.
de Valle MB, Bjornsson E, Lindkvist B. 2012. Mortality and cancer risk related to primary sclerosing cholangitis in a swedish population-based cohort. Liver Int 32(3):441–8.
Deviere J, Nageshwar Reddy D, Puspok A, Ponchon T, Bruno MJ, Bourke MJ, Neuhaus H, Roy A, Gonzalez-Huix Llado F, Barkun AN, et al. 2014. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology 147(2):385,95.
Donelli G, Guaglianone E, Di Rosa R, Fiocca F, Basoli A. 2007. Plastic biliary stent occlusion: Factors involved and possible preventive approaches. Clinical Medicine and Research 5(1):53–60.
Draganov P, Hoffman B, Marsh W, Cotton P, Cunningham J. 2002. Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents. Gastrointest Endosc 55(6):680–6.
Draganov PV, Lin T, Chauhan S, Wagh MS, Hou W, Forsmark CE. 2011. Prospective evaluation of the clinical utility of ERCP-guided cholangiopancreatoscopy with a new direct visualization system. Gastrointest Endosc 73(5):971–9.
Dumonceau JM. 2012. Sampling at ERCP for cyto- and histopathologicical examination. Gastrointest Endosc Clin N Am 22(3):461–77.
Dumonceau J-, Heresbach D, Devière J, Costamagna G, Beilenhoff U, Riphaus A. 2011. Biliary stents: Models and methods for endoscopic stenting: European society of gastrointestinal endoscopy (ESGE) technology review. Endoscopy 43(7):617–26.
Dumonceau JM, Andriulli A, Elmunzer BJ, Mariani A, Meister T, Deviere J, Marek T, Baron TH, Hassan C, Testoni PA, et al. 2014. Prophylaxis of post-ERCP pancreatitis: European society of gastrointestinal endoscopy (ESGE) guideline - updated june 2014. Endoscopy 46(9):799–815.
Dumonceau JM, Delhaye M, Tringali A, Dominguez-Munoz JE, Poley JW, Arvanitaki M, Costamagna G, Costea F, Deviere J, Eisendrath P, et al. 2012. Endoscopic treatment of chronic pancreatitis: European society of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy 44(8):784–800.
Eaton JE, Talwalkar JA, Lazaridis KN, Gores GJ, Lindor KD. 2013. Pathogenesis of primary sclerosing cholangitis and advances in diagnosis and management. Gastroenterology 145(3):521–36.
Ehlken H and Schramm C. 2013. Primary sclerosing cholangitis and cholangiocarcinoma: Pathogenesis and modes of diagnostics. Dig Dis 31(1):118–25.

98 Antti Siiki
Eickhoff A, Jakobs R, Leonhardt A, Eickhoff JC, Riemann JF. 2001. Endoscopic stenting for common bile duct stenoses in chronic pancreatitis: Results and impact on long-term outcome. European Journal of Gastroenterology and Hepatology 13(10):1161–7.
Enochsson L, Thulin A, Osterberg J, Sandblom G, Persson G. 2013. The swedish registry of gallstone surgery and endoscopic retrograde cholangiopancreatography (GallRiks): A nationwide registry for quality assurance of gallstone surgery. JAMA Surg :1–8.
Enochsson L, Swahn F, Arnelo U, Nilsson M, Lohr M, Persson G. 2010. Nationwide, population-based data from 11,074 ERCP procedures from the swedish registry for gallstone surgery and ERCP. Gastrointest Endosc 72(6):1175,84, 1184.e1-3.
Etzel JP, Eng SC, Ko CW, Lee SD, Saunders MD, Tung BY, Kimmey MB, Kowdley KV. 2008. Complications after ERCP in patients with primary sclerosing cholangitis. Gastrointest Endosc 67(4):643–8.
Farina A, Dumonceau JM, Antinori P, Annessi-Ramseyer I, Frossard JL, Hochstrasser DF, Delhaye M, Lescuyer P. Bile carcinoembryonic cell adhesion molecule 6 (CEAM6) as a biomarker of malignant biliary stenoses. Biochim Biophys Acta. 1844(5):1018–25.
Freeman ML. 2012. Complications of endoscopic retrograde cholangiopancreatography: Avoidance and management. Gastrointest Endosc Clin N Am 22(3):567-86.
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. 1996. Complications of endoscopic biliary sphincterotomy. N Engl J Med 335(13):909–18.
Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS, et al. 2001. Risk factors for post-ERCP pancreatitis: A prospective, multicenter study. Gastrointest Endosc 54(4):425–34.
Freudenberg S, Rewerk S, Kaess M, Weiss C, Dorn-Beinecke A, Post S. 2004. Biodegradation of absorbable sutures in body fluids and pH buffers. Eur Surg Res 36(6):376–85.
Fritcher EG, Kipp BR, Halling KC, Oberg TN, Bryant SC, Tarrell RF, Gores GJ, Levy MJ, Clayton AC, Sebo TJ, et al. 2009. A multivariable model using advanced cytologic methods for the evaluation of indeterminate pancreatobiliary strictures. Gastroenterology 136(7):2180–6.
Garcia-Cano Lizcano J, Gonzalez Martin JA, Morillas Arino J, Perez Sola A. 2004. Complications of endoscopic retrograde cholangiopancreatography. A study in a small ERCP unit. Rev Esp Enferm Dig 96(3):163–73.
Garcia-Pajares F, Sánchez-Antolín G, Pelayo SL, Gómez De La Cuesta S, Herranz Bachiller MT, Pérez-Miranda M, De La Serna C, Vallecillo Sande MA, Alcaide N, Llames RV, et al. 2010. Covered metal stents for the treatment of biliary complications after orthotopic liver transplantation. Transplant Proc 42(8):2966–9.
Ginsberg G, Cope C, Shah J, Martin T, Carty A, Habecker P, Kaufmann C, Clerc C, Nuutinen J-, Törmälä P. 2003. In vivo evaluation of a new bioabsorbable self-expanding biliary stent. Gastrointest Endosc 58(5):777–84.
Goonetilleke KS and Siriwardena AK. 2007. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol 33(3):266–70.
Gourgiotis S, Germanos S, Ridolfini MP. 2007. Surgical management of chronic pancreatitis. Hepatobiliary Pancreat Dis Int 6(2):121–33.
Graziadei IW, Schwaighofer H, Koch R, Nachbaur K, Koenigsrainer A, Margreiter R, Vogel W. 2006. Long-term outcome of endoscopic treatment of biliary strictures after liver transplantation. Liver Transplantation 12(5):718–25.
Grolich T, Crha M, Novotny L, Kala Z, Hep A, Necas A, Hlavsa J, Mitas L, Misik J. 2015. Self-expandable biodegradable biliary stents in porcine model. J Surg Res 193(2):606–12.

99Endoscopic Management of Benign Biliary Strictures
Gullichsen R, Lavonius M, Laine S, Gronroos J. 2005. Needle-knife assisted ERCP. Surg Endosc 19(9):1243–5.
Gunji H, Cho A, Tohma T, Okazumi S, Makino H, Shuto K, Mochizuki R, Matsubara K, Hayano K, Mori C, et al. 2006. The blood supply of the hilar bile duct and its relationship to the communicating arcade located between the right and left hepatic arteries. Am J Surg 192(3):276–80.
Gwon DI, Ko GY, Ko HK, Yoon HK, Sung KB. 2013. Percutaneous transhepatic treatment using retrievable covered stents in patients with benign biliary strictures: Mid-term outcomes in 68 patients. Dig Dis Sci 58(11):3270–9.
Gyokeres T, Duhl J, Varsanyi M, Schwab R, Burai M, Pap A. 2003. Double guide wire placement for endoscopic pancreaticobiliary procedures. Endoscopy 35(1):95–6.
Haapamaki C, Udd M, Halttunen J, Lindstrom O, Makisalo H, Kylanpaa L. 2012. Endoscopic treatment of anastomotic biliary complications after liver transplantation using removable, covered, self-expandable metallic stents. Scand J Gastroenterol 47(1):116–21.
Haapamaki C, Kylanpaa L, Udd M, Lindstrom O, Gronroos J, Saarela A, Mustonen H, Halttunen J. 2015. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy Jan 2015 (e-pub).
Hair CS and Devonshire DA. 2010. Severe hyperplastic tissue stenosis of a novel biodegradable esophageal stent and subsequent successful management with high-pressure balloon dilation. Endoscopy 42 Suppl 2:E132-3.
Halme L, Doepel M, von Numers H, Edgren J, Ahonen J. 1999. Complications of diagnostic and therapeutic ERCP. Ann Chir Gynaecol 88(2):127–31.
Halme L, Arola J, Numminen K, Krogerus L, Makisalo H, Farkkila M. 2012. Biliary dysplasia in patients with primary sclerosing cholangitis: Additional value of DNA ploidity. Liver Int 32(5):783–9.
Halttunen J, Keranen I, Udd M, Kylanpaa L. 2009. Pancreatic sphincterotomy versus needle knife precut in difficult biliary cannulation. Surg Endosc 23(4):745–9.
Halttunen J, Meisner S, Aabakken L, Arnelo U, Gronroos J, Hauge T, Kleveland PM, Nordblad Schmidt P, Saarela A, Swahn F, et al. 2014. Difficult cannulation as defined by a prospective study of the scandinavian association for digestive endoscopy (SADE) in 907 ERCPs. Scand J Gastroenterol 49(6):752–8.
Hellman U, Wernstedt C, Gonez J, Heldin CH. 1995. Improvement of an “in-gel” digestion procedure for the micropreparation of internal protein fragments for amino acid sequencing. Anal Biochem 224(1):451–5.
Hu B, Gao D, Yu F, Wang T, Pan Y, Yang X. 2011. Endoscopic stenting for post-transplant biliary stricture: Usefulness of a novel removable covered metal stent. Journal of Hepato-Biliary-Pancreatic Sciences 18(5):640–5.
Huang L, Yu QS, Zhang Q, Liu JD, Wang Z. 2015. Comparison between double-guide wire technique and transpancreatic sphincterotomy technique for difficult biliary cannulation. Dig Endosc 27(3);381–7.
Irani S, Baron TH, Akbar A, Lin OS, Gluck M, Gan I, Ross AS, Petersen BT, Topazian M, Kozarek RA. 2014. Endoscopic treatment of benign biliary strictures using covered self-expandable metal stents (CSEMS). Dig Dis Sci 59(1):152–60.
Ismail S, Kylanpaa L, Mustonen H, Halttunen J, Lindstrom O, Jokelainen K, Udd M, Farkkila M. 2012. Risk factors for complications of ERCP in primary sclerosing cholangitis. Endoscopy 44(12):1133–8.

100 Antti Siiki
Itoi T, Kasuya K, Abe Y, Isayama H. 2011. Endoscopic placement of a new short-term biodegradable pancreatic and biliary stent in an animal model: A preliminary feasibility study (with videos). J Hepatobiliary Pancreat Sci 18(3):463–7.
Itokawa F, Itoi T, Ishii K, Sofuni A, Moriyasu F. 2014. Single- and double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with roux-en-Y plus hepaticojejunostomy anastomosis and whipple resection. Dig Endosc 26 Suppl 2:136–43.
Jakobs R and Riemann JF. 1999. The role of endoscopy in acute recurrent and chronic pancreatitis and pancreatic cancer. Gastroenterol Clin North Am 28(3):783,800, xii.
Janssen JJ, van Delden OM, van Lienden KP, Rauws EA, Busch OR, van Gulik TM, Gouma DJ, Lameris JS. 2014. Percutaneous balloon dilatation and long-term drainage as treatment of anastomotic and nonanastomotic benign biliary strictures. Cardiovasc Intervent Radiol 37(6):1559–67.
Kaffes A, Griffin S, Vaughan R, James M, Chua T, Tee H, Dinesen L, Corte C, Gill R. 2014. A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol 7(2):64–71.
Kaffes AJ and Liu K. 2013. Fully covered self-expandable metal stents for treatment of benign biliary strictures. Gastrointest Endosc 78(1):13–21.
Kahaleh M, Tokar J, Le T, Yeaton P. 2004. Removal of self-expandable metallic wallstents. Gastrointest Endosc 60(4):640–4.
Kahaleh M, Behm B, Clarke BW, Brock A, Shami VM, De La Rue SA, Sundaram V, Tokar J, Adams RB, Yeaton P. 2008. Temporary placement of covered self-expandable metal stents in benign biliary strictures: A new paradigm? (with video). Gastrointest Endosc 67(3):446–54.
Kahaleh M, Brijbassie A, Sethi A, Degaetani M, Poneros JM, Loren DE, Kowalski TE, Sejpal DV, Patel S, Rosenkranz L, et al. 2013. Multicenter trial evaluating the use of covered self-expanding metal stents in benign biliary strictures: Time to revisit our therapeutic options? J Clin Gastroenterol 47(8):695–9.
Kahl S, Zimmermann S, Genz I, Glasbrenner B, Pross M, Schulz H-, Mc Namara D, Schmidt U, Malfertheiner P. 2003. Risk factors for failure of endoscopic stenting of biliary strictures in chronic pancreatitis: A prospective follow-up study. Am J Gastroenterol 98(11):2448–53.
Kalaitzakis E, Webster GJ, Oppong KW, Kallis Y, Vlavianos P, Huggett M, Dawwas MF, Lekharaju V, Hatfield A, Westaby D, et al. 2012. Diagnostic and therapeutic utility of single-operator peroral cholangioscopy for indeterminate biliary lesions and bile duct stones. European Journal of Gastroenterology and Hepatology 24(6):656–64.
Kalaitzakis E, Levy M, Kamisawa T, Johnson GJ, Baron TH, Topazian MD, Takahashi N, Kanno A, Okazaki K, Egawa N, et al. 2011. Endoscopic retrograde cholangiography does not reliably distinguish IgG4-associated cholangitis from primary sclerosing cholangitis or cholangiocarcinoma. Clin Gastroenterol Hepatol 9(9):800,803.e2.
Kao D, Zepeda-Gomez S, Tandon P, Bain VG. 2013. Managing the post-liver transplantation anastomotic biliary stricture: Multiple plastic versus metal stents: A systematic review. Gastrointest Endosc 77(5):679–91.
Kapral C, Duller C, Wewalka F, Kerstan E, Vogel W, Schreiber F. 2008. Case volume and outcome of endoscopic retrograde cholangiopancreatography: Results of a nationwide austrian benchmarking project. Endoscopy 40(8):625–30.
Kapral C, Muhlberger A, Wewalka F, Duller C, Knoflach P, Schreiber F, Working Groups Quality Assurance and Endoscopy of Austrian Society of Gastroenterology and Hepatology (OeGGH). 2012. Quality assessment of endoscopic retrograde cholangiopancreatography: Results of a running nationwide austrian benchmarking project after 5 years of implementation. Eur J Gastroenterol Hepatol 24(12):1447–54.

101Endoscopic Management of Benign Biliary Strictures
Karvonen J, Salminen P, Gronroos JM. 2011. Bile duct injuries during open and laparoscopic cholecystectomy in the laparoscopic era: Alarming trends. Surg Endosc 25(9):2906–10.
Kasher JA, Corasanti JG, Tarnasky PR, McHenry L, Fogel E, Cunningham J. 2011. A multicenter analysis of safety and outcome of removal of a fully covered self-expandable metal stent during ERCP. Gastrointest Endosc 73(6):1292–7.
Katabathina VS, Dasyam AK, Dasyam N, Hosseinzadeh K. 2014. Adult bile duct strictures: Role of MR imaging and MR cholangiopancreatography in characterization. Radiographics 34(3):565–86.
Kawakubo K, Isayama H, Sasahira N, Kogure H, Miyabayashi K, Hirano K, Tada M, Koike K. 2012. Mucosal hyperplasia in an uncovered portion of partially covered metal stent. World J Gastrointest Endosc 4(9):432–3.
Kaya M, Petersen BT, Angulo P, Baron TH, Andrews JC, Gostout CJ, Lindor KD. 2001. Balloon dilation compared to stenting of dominant strictures in primary sclerosing cholangitis. Am J Gastroenterol 96(4):1059–66.
Kemppainen E, Talja M, Riihela M, Pohjonen T, Tormala P, Alfthan O. 1993. A bioresorbable urethral stent. an experimental study. Urol Res 21(3):235–8.
Kiehne K, Folsch UR, Nitsche R. 2000. High complication rate of bile duct stents in patients with chronic alcoholic pancreatitis due to noncompliance. Endoscopy 32(5):377–80.
Kim HJ, Kim MH, Lee SK, Yoo KS, Seo DW, Min YI. 2000. Tumor vessel: A valuable cholangioscopic clue of malignant biliary stricture. Gastrointest Endosc 52(5):635–8.
Kipp BR, Stadheim LM, Halling SA, Pochron NL, Harmsen S, Nagorney DM, Sebo TJ, Therneau TM, Gores GJ, de Groen PC, et al. 2004. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. Am J Gastroenterol 99(9):1675–81.
Kuroda Y, Tsuyuguchi T, Sakai Y, Sudhamshu KC, Ishihara T, Yamaguchi T, Saisho H, Yokosuka O. 2010. Long-term follow-up evaluation for more than 10 years after endoscopic treatment for postoperative bile duct strictures. Surgical Endoscopy and Other Interventional Techniques 24(4):834–40.
Lankisch PG, Assmus C, Maisonneuve P, Lowenfels AB. 2002. Epidemiology of pancreatic diseases in luneburg county. A study in a defined german population. Pancreatology 2(5):469–77.
Larghi A, Tringali A, Lecca PG, Giordano M, Costamagna G. 2008. Management of hilar biliary strictures. Am J Gastroenterol 103(2):458–73.
Laukkarinen J, Lamsa T, Nordback I, Mikkonen J, Sand J. 2008. A novel biodegradable pancreatic stent for human pancreatic applications: A preclinical safety study in a large animal model. Gastrointest Endosc 67(7):1106–12.
Laukkarinen J, Nordback I, Mikkonen J, Karkkainen P, Sand J. 2007a. A novel biodegradable biliary stent in the endoscopic treatment of cystic-duct leakage after cholecystectomy. Gastrointest Endosc 65(7):1063–8.
Laukkarinen JM, Sand JA, Chow P, Juuti H, Kellomaki M, Karkkainen P, Isola J, Yu S, Somanesan S, Kee I, et al. 2007b. A novel biodegradable biliary stent in the normal duct hepaticojejunal anastomosis: An 18-month follow-up in a large animal model. J Gastrointest Surg 11(6):750–7.
Lawrence C, Romagnuolo J, Payne KM, Hawes RH, Cotton PB. 2010. Low symptomatic premature stent occlusion of multiple plastic stents for benign biliary strictures: Comparing standard and prolonged stent change intervals. Gastrointest Endosc 72(3):558–63.
Lee S, Song T, Joo M, Park do H, Seo D, Lee S, Kim M. 2014. Histological changes in the bile duct after long-term placement of a fully covered self-expandable metal stent within a common bile duct: A canine study. Clin Endosc. 47(1):84–93.

102 Antti Siiki
Lemon HM and Byrnes WW. 1949. Cancer of the biliary tract and pancreas; diagnosis from cytology of duodenal aspirations. J Am Med Assoc 141(4):254–7.
Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Talamini MA, Sauter PA, Coleman J, Yeo CJ. 2000. Postoperative bile duct strictures: Management and outcome in the 1990s. Ann Surg 232(3):430–41.
Lindberg B, Enochsson L, Tribukait B, Arnelo U, Bergquist A. 2006. Diagnostic and prognostic implications of DNA ploidy and S-phase evaluation in the assessment of malignancy in biliary strictures. Endoscopy 38(6):561–5.
Lindberg B, Arnelo U, Bergquist A, Thorne A, Hjerpe A, Granqvist S, Hansson LO, Tribukait B, Persson B, Broome U. 2002. Diagnosis of biliary strictures in conjunction with endoscopic retrograde cholangiopancreaticography, with special reference to patients with primary sclerosing cholangitis. Endoscopy 34(11):909–16.
Lindkvist B, Benito de Valle M, Gullberg B, Bjornsson E. 2010. Incidence and prevalence of primary sclerosing cholangitis in a defined adult population in sweden. Hepatology 52(2):571–7.
Lohr JM, Haas SL, Lindgren F, Enochsson L, Hedstrom A, Swahn F, Segersvard R, Arnelo U. 2013. Conservative treatment of chronic pancreatitis. Dig Dis 31(1):43–50.
Lohr JM, Faissner R, Koczan D, Bewerunge P, Bassi C, Brors B, Eils R, Frulloni L, Funk A, Halangk W, et al. 2010. Autoantibodies against the exocrine pancreas in autoimmune pancreatitis: Gene and protein expression profiling and immunoassays identify pancreatic enzymes as a major target of the inflammatory process. Am J Gastroenterol 105(9):2060–71.
Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. 1998. Major early complications from diagnostic and therapeutic ERCP: A prospective multicenter study. Gastrointest Endosc 48(1):1–10.
Lorenzo-Zuniga V, Moreno-de-Vega V, Marin I, Boix J. 2014. Biodegradable stents in gastrointestinal endoscopy. World J Gastroenterol 20(9):2212–7.
Lukic N, Visentin R, Delhaye M, Frossard JL, Lescuyer P, Dumonceau JM, Farina A 2014. An integrated approach for comparative proteomic analysis of human bile reveals overexpressed cancer-associated proteins in malignant biliary stenosis. Biochim Biophys Acta 1844(5):1026–33.
Lübbe J, Arnelo U, Lundell L, Swahn F, Törnqvist B, Jonas E, Löhr JM, Enochsson L. 2015. ERCP- guided cholangioscopy using a single-use system: nationwide register-based study of its use in clinical practice. Endoscopy Apr 2015. (e-pub)
Mahajan A, Ho H, Sauer B, Phillips MS, Shami VM, Ellen K, Rehan M, Schmitt TM, Kahaleh M. 2009. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: Midterm evaluation (with video). Gastrointest Endosc 70(2):303–9.
Majoie CB, Reeders JW, Sanders JB, Huibregtse K, Jansen PL. 1991. Primary sclerosing cholangitis: A modified classification of cholangiographic findings. AJR Am J Roentgenol 157(3):495–7.
Manta R, Frazzoni M, Conigliaro R, Maccio L, Melotti G, Dabizzi E, Bertani H, Manno M, Castellani D, Villanacci V, et al. 2013. SpyGlass((R)) single-operator peroral cholangioscopy in the evaluation of indeterminate biliary lesions: A single-center, prospective, cohort study. Surg Endosc 27(5):1569–72.
Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, et al. 2001. Complications of diagnostic and therapeutic ERCP: A prospective multicenter study. Am J Gastroenterol 96(2):417–23.
Mauri G, Michelozzi C, Melchiorre F, Poretti D, Tramarin M, Pedicini V, Solbiati L, Cornalba G, Sconfienza LM. 2013. Biodegradable biliary stent implantation in the treatment of benign bilioplastic-refractory biliary strictures: Preliminary experience. Eur Radiol 23(12):3304–10.

103Endoscopic Management of Benign Biliary Strictures
McCune WS, Shorb PE, Moscovitz H. 1968. Endoscopic cannulation of the ampulla of vater: A preliminary report. Ann Surg 167(5):752–6.
Moon JH, Choi HJ, Koo HC, Han SH, Lee TH, Cho YD, Park S-, Kim S-. 2012. Feasibility of placing a modified fully covered self-expandable metal stent above the papilla to minimize stent-induced bile duct injury in patients with refractory benign biliary strictures (with videos). Gastrointest Endosc 75(5):1080–5.
Morelli G, Fazel A, Judah J, Pan JJ, Forsmark C, Draganov P. 2008. Rapid-sequence endoscopic management of posttransplant anastomotic biliary strictures. Gastrointest Endosc 67(6):879–85.
Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P. 2003. Long-term outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc 58(3):374-9.
Mortz E, Krogh TN, Vorum H, Gorg A. 2001. Improved silver staining protocols for high sensitivity protein identification using matrix-assisted laser desorption/ionization-time of flight analysis. Proteomics 1(11):1359–63.
Navaneethan U, Lourdusamy V, Poptic E, Hammel JP, Sanaka MR, Parsi MA. 2015a. Comparative effectiveness of pyruvate kinase M2 in bile, serum carbohydrate antigen 19-9, and biliary brushings in diagnosing malignant biliary strictures. Dig Dis Sci 60(4);903–9.
Navaneethan U, Jegadeesan R, Nayak S, Lourdusamy V, Sanaka MR, Vargo JJ, Parsi MA. 2015b. ERCP-related adverse events in patients with primary sclerosing cholangitis. Gastrointest Endosc 81(2):410–9.
Neuhaus H, Hagenmuller F, Classen M. 1989. Self-expanding biliary stents: Preliminary clinical experience. Endoscopy 21(5):225–8.
Noack K, Bronk SF, Kato A, Gores GJ. 1993. The greater vulnerability of bile duct cells to reoxygenation injury than to anoxia. implications for the pathogenesis of biliary strictures after liver transplantation. Transplantation 56(3):495–500.
Nordback I and Airo I. 1988. Post-ERCP acute necrotizing pancreatitis. Ann Chir Gynaecol 77(1):15–20.
Nordback I, Lamsa T, Laukkarinen J, Leppiniemi J, Kellomaki M, Sand J. 2008. Pancreatico-jejunostomy with a biodegradable pancreatic stent and without stitches through the pancreas. Hepatogastroenterology 55(82–83):319–22.
Nordback I, Raty S, Laukkarinen J, Jarvinen S, Piironen A, Leppiniemi J, Kellomaki M, Sand J. 2012. A novel radiopaque biodegradable stent for pancreatobiliary applications--the first human phase I trial in the pancreas. Pancreatology 12(3):264–71.
Okazaki K, Yanagawa M, Mitsuyama T, Uchida K. 2014. Recent advances in the concept and pathogenesis of IgG4-related disease in the hepato-bilio-pancreatic system. Gut Liver 8(5):462–70.
Palm J, Saarela A, Makela J. 2007. Safety of erlangen precut papillotomy: An analysis of 1044 consecutive ERCP examinations in a single institution. J Clin Gastroenterol 41(5):528–33.
Park DH, Lee SS, Lee TH, Ryu CH, Kim HJ, Seo D-, Park S-, Lee S-, Kim M-, Kim S-. 2011a. Anchoring flap versus flared end, fully covered self-expandable metal stents to prevent migration in patients with benign biliary strictures: A multicenter, prospective, comparative pilot study (with videos). Gastrointest Endosc 73(1):64–70.
Park JK, Moon JH, Choi HJ, Min SK, Lee TH, Cheon GJ, Cheon YK, Cho YD, Park S-, Kim S-. 2011b. Anchoring of a fully covered self-expandable metal stent with a 5F double-pigtail plastic stent to prevent migration in the management of benign biliary strictures. Am J Gastroenterol 106(10):1761–5.

104 Antti Siiki
Parsi MA, Jang S, Sanaka M, Stevens T, Vargo JJ. 2014. Diagnostic and therapeutic cholangiopancreatoscopy: Performance of a new digital cholangioscope. Gastrointest Endosc 79(6):936–42.
Pasha SF, Harrison ME, Das A, Nguyen CC, Vargas HE, Balan V, Byrne TJ, Douglas DD, Mulligan DC. 2007. Endoscopic treatment of anastomotic biliary strictures after deceased donor liver transplantation: Outcomes after maximal stent therapy. Gastrointest Endosc 66(1):44–51.
Pearce S, Thornes H, Carr D, Tanner A. 1994. Diagnostic pitfall; interpretation of CA 19-9 concentrations in the presence of hepatic dysfunction. Gut 35(5):707–8.
Perri V, Familiari P, Tringali A, Boskoski I, Costamagna G. 2011. Plastic biliary stents for benign biliary diseases. Gastrointest Endosc Clin N Am 21(3):405–33.
Perri V, Boškoski I, Tringali A, Familiari P, Mutignani M, Marmo R, Costamagna G. 2012. Fully covered self-expandable metal stents in biliary strictures caused by chronic pancreatitis not responding to plastic stenting: A prospective study with 2 years of follow-up. Gastrointest Endosc 75(6):1271–7.
Petrtyl J, Bruha R, Horak L, Zadorova Z, Dosedel J, Laasch HU. 2010. Management of benign intrahepatic bile duct strictures: Initial experience with polydioxanone biodegradable stents. Endoscopy 42 Suppl 2:E89–90.
Phillips MS, Bonatti H, Sauer BG, Smith L, Javaid M, Kahaleh M, Schmitt T. 2011. Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Endoscopy 43(6):512–7.
Poley J-, Van Tilburg AJP, Kuipers EJ, Bruno MJ. 2011. Breaking the barrier: Using extractable fully covered metal stents to treat benign biliary hilar strictures. Gastrointest Endosc 74(4):916–20.
Poley J-, Cahen DL, Metselaar HJ, Van Buuren HR, Kazemier G, Van Eijck CHJ, Haringsma J, Kuipers EJ, Bruno MJ. 2012. A prospective group sequential study evaluating a new type of fully covered self-expandable metal stent for the treatment of benign biliary strictures (with video). Gastrointest Endosc 75(4):783–9.
Ponsioen CY, Lam K, van Milligen de Wit AW, Huibregtse K, Tytgat GN. 1999. Four years experience with short term stenting in primary sclerosing cholangitis. Am J Gastroenterol 94(9):2403–7.
Pozsár J, Sahin P, László F, Forró G, Topa L. 2004. Medium-term results of endoscopic treatment of common bile duct strictures in chronic calcifying pancreatitis with increasing numbers of stents. J Clin Gastroenterol 38(2):118–23.
Pugliese V, Conio M, Nicolo G, Saccomanno S, Gatteschi B. 1995. Endoscopic retrograde forceps biopsy and brush cytology of biliary strictures: A prospective study. Gastrointest Endosc 42(6):520–6.
Rajaram R, Ponsioen C, Majoie C, Reeders W, Lameris J. 2001. Evaluation of a modified cholangiographic classification system for primary sclerosing cholangitis. Abdom Imaging 26:43–47.
Ramchandani M, Reddy DN, Gupta R, Lakhtakia S, Tandan M, Darisetty S, Sekaran A, Rao GV. 2011. Role of single-operator peroral cholangioscopy in the diagnosis of indeterminate biliary lesions: A single-center, prospective study. Gastrointest Endosc 74(3):511–9.
Ray JA, Doddi N, Regula D, Williams JA, Melveger A. 1981. Polydioxanone (PDS), a novel monofilament synthetic absorbable suture. Surg Gynecol Obstet 153(4):497–507.
Rey JW, Hansen T, Dumcke S, Tresch A, Kramer K, Galle PR, Goetz M, Schuchmann M, Kiesslich R, Hoffman A. 2014. Efficacy of SpyGlass(TM)-directed biopsy compared to brush cytology in obtaining adequate tissue for diagnosis in patients with biliary strictures. World J Gastrointest Endosc 6(4):137–43.

105Endoscopic Management of Benign Biliary Strictures
Ryan ME and Baldauf MC. 1994. Comparison of flow cytometry for DNA content and brush cytology for detection of malignancy in pancreaticobiliary strictures. Gastrointest Endosc 40(2 Pt 1):133–9.
Sabino M, Márquez L, Feijoo J. 2000. Study of the hydrolytic degradation of polydioxanone PPDX. Polymer Degradation and Stability 69(2):209–16.
Sakai Y, Tsuyuguchi T, Ishihara T, Yukisawa S, Sugiyama H, Miyakawa K, Kuroda Y, Yamaguchi T, Ozawa S, Yokosuka O. 2009. Long-term prognosis of patients with endoscopically treated postoperative bile duct stricture and bile duct stricture due to chronic pancreatitis. J Gastroenterol Hepatol 24(7):1191–7.
Saleem A, Baron TH, Gostout CJ, Topazian MD, Levy MJ, Petersen BT, Wong Kee Song LM. 2010. Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered roux-en-Y anatomy. Endoscopy 42(8):656–60.
Salminen P, Laine S, Gullichsen R. 2008. Severe and fatal complications after ERCP: Analysis of 2555 procedures in a single experienced center. Surgical Endoscopy and Other Interventional Techniques 22(9):1965–70.
Sangfelt P, Sundin A, Wanders A, Rasmussen I, Karlson BM, Bergquist A, Rorsman F. 2014. Monitoring dominant strictures in primary sclerosing cholangitis with brush cytology and FDG-PET. J Hepatol 61(6):1352–7.
Sauer P, Chahoud F, Gotthardt D, Stremmel W, Weiss K-, Büchler M, Schemmer P, Weitz J, Schaible A. 2012. Temporary placement of fully covered self-expandable metal stents in biliary complications after liver transplantation. Endoscopy 44(5):536–8.
Sebo TJ. 1995. Digital image analysis. Mayo Clin Proc 70(1):81–2.Sethi A, Widmer J, Shah NL, Pleskow DK, Edmundowicz SA, Sejpal DV, Gress FG, Pop GH,
Gaidhane M, Sauer BG, et al. 2014. Interobserver agreement for evaluation of imaging with single operator choledochoscopy: What are we looking at? Dig Liver Dis 46(6):518–22.
Shanbhogue AKP, Tirumani SH, Prasad SR, Fasih N, McInnes M. 2011. Benign biliary strictures: A current comprehensive clinical and imaging review. Am J Roentgenol 197(2):W295–306.
Shimada H, Endo I, Shimada K, Matsuyama R, Kobayashi N, Kubota K. 2012. The current diagnosis and treatment of benign biliary stricture. Surg Today:1–11.
Silviera ML, Seamon MJ, Porshinsky B, Prosciak MP, Doraiswamy VA, Wang CF, Lorenzo M, Truitt M, Biboa J, Jarvis AM, et al. 2009. Complications related to endoscopic retrograde cholangiopancreatography: A comprehensive clinical review. J Gastrointestin Liver Dis 18(1):73–82.
Soehendra N and Reynders-Frederix V. 1980. Palliative bile duct drainage – a new endoscopic method of introducing a transpapillary drain. Endoscopy 12(1):8–11.
Steinberg W. 1990. The clinical utility of the CA 19-9 tumor-associated antigen. Am J Gastroenterol 85(4):350–5.
Strasberg SM and Helton WS. 2011. An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB (Oxford) 13(1):1–14.
Strasberg SM, Hertl M, Soper NJ. 1995. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1):101–25.
Swahn F, Nilsson M, Arnelo U, Lohr M, Persson G, Enochsson L. 2013. Rendezvous cannulation technique reduces post-ERCP pancreatitis: A prospective nationwide study of 12,718 ERCP procedures. Am J Gastroenterol 108(4):552–9.
Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, Busuttil RW, Durazo FA. 2010. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video). Gastrointest Endosc 71(3):505–12.

106 Antti Siiki
Tarantino I, Traina M, Mocciaro F, Barresi L, Curcio G, Di Pisa M, Granata A, Volpes R, Gridelli B. 2012a. Fully covered metallic stents in biliary stenosis after orthotopic liver transplantation. Endoscopy 44(3):246–50.
Tarantino I, Mangiavillano B, Di Mitri R, Barresi L, Mocciaro F, Granata A, Masci E, Curcio G, Di Pisa M, Marino A, et al. 2012b. Fully covered self-expandable metallic stents in benign biliary strictures: A multicenter study on efficacy and safety. Endoscopy 44(10):923–7.
Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N, Mutignani M, et al. 2010. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: A prospective multicenter study. Am J Gastroenterol 105(8):1753–61.
THL. 2012. Statistics in somatic specialist medical care.National Institute for Health and Welfare, Finland.
Tietz P and Larusso NF. 2002. Cholangiocyte biology. Curr Opin Gastroenterol 18(3):360–5.Tischendorf JJ, Hecker H, Kruger M, Manns MP, Meier PN. 2007. Characterization, outcome,
and prognosis in 273 patients with primary sclerosing cholangitis: A single center study. Am J Gastroenterol 102(1):107–14.
Tischendorf JJ, Kruger M, Trautwein C, Duckstein N, Schneider A, Manns MP, Meier PN. 2006. Cholangioscopic characterization of dominant bile duct stenoses in patients with primary sclerosing cholangitis. Endoscopy 38(7):665–9.
Tokar JL, Banerjee S, Barth BA, Desilets DJ, Kaul V, Kethi SR, Pedrosa MC, Pfau PR, Pleskow DK, Varadarajulu S, et al. 2011. Drug-eluting/biodegradable stents. Gastrointest Endosc 74(5):954–8.
Tornqvist B, Stromberg C, Persson G, Nilsson M. 2012. Effect of intended intraoperative cholangiography and early detection of bile duct injury on survival after cholecystectomy: Population based cohort study. BMJ 345:e6457.
Traina M, Tarantino I, Barresi L, Volpes R, Gruttadauria S, Petridis I, Gridelli B. 2009. Efficacy and safety of fully covered self-expandable metallic stents in biliary complications after liver transplantation: A preliminary study. Liver Transplantation 15(11):1493–8.
Tsujino T, Isayama H, Sugawara Y, Sasaki T, Kogure H, Nakai Y, Yamamoto N, Sasahira N, Yamashiki N, Tada M, et al. 2006. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol 101(10):2230–6.
Tuvignon N, Liguory C, Ponchon T, Meduri B, Fritsch J, Sahel J, Boyer J, Legoux JL, Escourrou J, Boustiere C, et al. 2011. Long-term follow-up after biliary stent placement for postcholecystectomy bile duct strictures: A multicenter study. Endoscopy 43(3):208–16.
Urakami Y. 1980. Peroral cholangiopancreatoscopy (PCPS) and peroral direct cholangioscopy (PDCS). Endoscopy 12(1):30–7.
Vakil N. 2011. Expandable metal stents: Principles and tissue responses. Gastrointest Endosc Clin N Am 21(3):351,7, vii.
Van Berkel AM, Cahen DL, van Westerloo DJ, Rauws EAJ, Huibregtse K, Bruno MJ. 2004. Self-expanding metal stents in benign biliary strictures due to chronic pancreatitis. Endoscopy 36(5):381–4.
Van Boeckel PGA, Vleggaar FP, Siersema PD. 2009. Plastic or metal stents for benign extrahepatic biliary strictures: A systematic review. BMC Gastroenterology 17;9:96.
Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP,Jr, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW, et al. 2002. Risk factors for complications after performance of ERCP. Gastrointest Endosc 56(5):652–6.

107Endoscopic Management of Benign Biliary Strictures
Verdonk RC, Buis CI, van der Jagt EJ, Gouw AS, Limburg AJ, Slooff MJ, Kleibeuker JH, Porte RJ, Haagsma EB. 2007. Nonanastomotic biliary strictures after liver transplantation, part 2: Management, outcome, and risk factors for disease progression. Liver Transpl 13(5):725–32.
Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, Slooff MJ, Peeters PM, de Jong KP, Kleibeuker JH, et al. 2006. Anastomotic biliary strictures after liver transplantation: Causes and consequences. Liver Transpl 12(5):726–35.
Vitale GC, Tran TC, Davis BR, Vitale M, Vitale D, Larson G. 2008. Endoscopic management of postcholecystectomy bile duct strictures. J Am Coll Surg 206(5):918,23.
von Seth E, Arnelo U, Enochsson L, Bergquist A. 2015. Primary sclerosing cholangitis increases the risk for pancreatitis after endoscopic retrograde cholangiopancreatography. Liver Int 351(4):254–62.
Waage A and Nilsson M. 2006. Iatrogenic bile duct injury: A population-based study of 152 776 cholecystectomies in the swedish inpatient registry. Arch Surg 141(12):1207–13.
Wagh MS, Chavalitdhamrong D, Moezardalan K, Chauhan SS, Gupte AR, Nosler MJ, Forsmark CE, Draganov PV. 2013. Effectiveness and safety of endoscopic treatment of benign biliary strictures using a new fully covered self expandable metal stent. Diagn Ther Endosc 2013:183513.
Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, Huang Q, Zhang X, He LP, Sun WS, et al. 2009. Risk factors for ERCP-related complications: A prospective multicenter study. Am J Gastroenterol 104(1):31–40.
Weber A, Gaa J, Rosca B, Born P, Neu B, Schmid RM, Prinz C. 2009. Complications of percutaneous transhepatic biliary drainage in patients with dilated and nondilated intrahepatic bile ducts. Eur J Radiol 72(3):412–7.
Weilert F, Bhat YM, Binmoeller KF, Kane S, Jaffee IM, Shaw RE, Cameron R, Hashimoto Y, Shah JN. 2014. EUS-FNA is superior to ERCP-based tissue sampling in suspected malignant biliary obstruction: Results of a prospective, single-blind, comparative study. Gastrointest Endosc 80(1):97–104.
Williams ED and Draganov PV. 2009. Endoscopic management of biliary strictures after liver transplantation. World Journal of Gastroenterology 15(30):3725–33.
Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson ML, Williamson PR, et al. 2007. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy 39(9):793–801.
Woo YS, Lee JK, Oh SH, Kim MJ, Jung JG, Lee KH, Lee KT. 2014. Role of SpyGlass peroral cholangioscopy in the evaluation of indeterminate biliary lesions. Dig Dis Sci 59(10):2565–70.
Wright ER, Bakis G, Srinivasan R, Raju R, Vittal H, Sanders MK, Bernadino K, Stefan A, Blaszyk H, Howell DA. 2011. Intraprocedural tissue diagnosis during ERCP employing a new cytology preparation of forceps biopsy (smash protocol). Am J Gastroenterol 106(2):294–9.
Wu YV and Linehan DC. 2010. Bile duct injuries in the era of laparoscopic cholecystectomies. Surg Clin North Am 90(4):787–802.
Yee AC and Ho CS. 1987. Complications of percutaneous biliary drainage: Benign vs malignant diseases. AJR Am J Roentgenol 148(6):1207–9.
Yin Z, Sun J, Yin D, Wang J. 2012. Surgical treatment strategies in chronic pancreatitis: A meta-analysis. Arch Surg 147(10):961–8.
Zoepf T, Maldonado-Lopez EJ, Malago M, Broelsch CE, Treichel U, Gerken G. 2006. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transplantation 12(1):88–94.

108 Antti Siiki

109Endoscopic Management of Benign Biliary Strictures
ORIGINAL COMMUNICATIONS

110 Antti Siiki

Scandinavian Journal of Surgery 101: 1–6, 2012
ERCP PROCEDURES IN A FINNISH COMMUNITY HOSPITAL: A RETROSPECTIVE ANALYSIS OF 1207 CASES
A. Siiki, A. Tamminen, T. Tomminen, P. Kuusanmäki
Department of Surgery, Kanta-Häme Central Hospital, Hämeenlinna, Finland
ABSTRACT
Background and Aims: Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure with a risk of serious and life-threatening complications. The most common complications are pancreatitis, haemorrhage, perforation and cholangitis. The aim of this study was to determine indications, success rates and complications in a low-volume ERCP unit in Kanta-Häme Central Hospital (KHCH).
Material and Methods: Data on 1207 consecutive ERCPs performed in KHCH between 2002 and 2009 was collected retrospectively from patient histories. Complications were classified according to need for intervention and length of hospitalisation.
Results: Cannulation of the desired duct was successful in 89.2% of 825 ERCPs with no earlier sphincterotomy. Complete stone removal was achieved in 91.3% of procedures. Standard biliary sphincterotomy was performed in 73.8% and precut sphincterotomy in 12.0 % of cases. Cholangitis developed in 2.1%, bleeding in 1.9%, pancreatitis in 1.9%, perforation in 1.0% and cardio-pulmonary or miscellaneous complications in 4.2% of cases. The majority of complications could be managed conservatively. In procedures with no earlier sphincterotomy ERCP-related 30-day mortality was 0.2% (n = 2) and over-all 30-day mortality was 3.3% (n = 27).
Conclusions: ERCP indications and success rates, as well as morbidity and mortality were comparable to those reported earlier. Although the success rate of cannulation and thereby ERCP procedures seem to be somewhat lower than in tertiary referral centres, ERCP procedures can be safely performed in a low-volume ERCP unit by concentrating procedures on a few experienced endoscopists. The success rates may be further im-proved with the latest cannulation techniques, used selectively in the last years of the study period.Key words: ERCP; complications; sphincterotomy; precut sphincterotomy; pancreatitis; cholangitis; perforation; haemorrhage
Correspondence:Antti Siiki, M.D.Kanta-Häme Central HospitalAhvenistontie 10, FI - 13530 Hämeenlinna, FinlandEmail: [email protected]
ing procedure with a long learning curve and a risk of serious and life-threatening complications. The most common indications of ERCP are removal of common bile duct (CBD) stones and relieving bile duct obstruction by stent insertion. Diagnostic proce-dures should be avoided, because they can be mostly replaced by non-invasive magnetic resonance imag-ing (MRI) or endoscopic ultrasound. The main com-plications are pancreatitis, haemorrhage, cholangitis and perforation of the CBD or duodenum (1, 2). Sev-eral studies, most from large academic centres have reported a low incidence of complications (3–17). In
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is used in the treatment of benign and malig-nant pancreatic and biliary diseases. It is a demand-

2 A. Siiki, A. Tamminen, T. Tomminen, P. Kuusanmäki
Finland ERCPs are also widely performed in low-volume community hospitals. The quality indicators of ERCP practice include adequate indications and low complication figures as well as success rate of cannulation (18). The cannulation of the desired duct should be successful in over 85% of ERCPs (18), but success rates as high as 98% have been reported (19, 20, 21). In this study, our aim was to retrospectively investigate indications, success rates and complica-tions of ERCPs in a low-volume community hospi-tal.
MATERIAL AND METHODS
The hospital database was searched for ERCPs performed between 1 January 2002 and 31 December 2009 in the en-doscopy unit of Kanta-Häme Central Hospital (KHCH) in Hämeenlinna. KHCH is a medium-sized community hos-pital in southern Finland serving a population of 173.000. All procedures were performed by two experienced endos-copists. All complications were managed in our hospital except one patient with cholangitis and suspected duode-nal perforation. Thirty-three procedures were excluded because papilla Vateri could not be reached (for reasons related e.g. to duodenal obstruction or inadequate seda-tion). Retrospective chart review was continued for up to 30 days after the procedure or to the end of longer hospi-talisation. Patient status after 30 days could be confirmed in 91.5% of ERCPs. Olympus duodenoscopes were used in all ERCPs. The cannulation techniques evolved during the study period. A primary method of entering the bile duct was to use sphincterotome or to cannulate over guide wire inserted in the CBD. In the early years of the study period, the guide wire cannulation was not routinely used and some cannulations had to be done with a little contrast medium injection to the pancreatic duct as access to CBD was attempted. When necessary, a precut sphincterotomy was performed with a needle knife towards 11–12 o´clock
to expose the CBD. Selectively, in the last few years a pan-creatic sphincterotomy technique was used in which precut was directed towards pancreatic duct. Some of the CBD cannulations were performed with a double-guide-wire technique (i.e. an another guide wire inside the pancreatic duct). CBD stones were extracted by balloon catheter or basket.
During the last two years of the study period, a routine antibiotic prophylaxis (i.v. cefuroxime 1.5 g) was admin-istered. Before this, antibiotics were given selectively if a stent insertion was planned or if a patient had a bile duct obstruction or an acute infection. The patients were given i.v. sedation (midatsolame or propofol) in the last three years of the study period administered mainly by an anaes-thetist. In the earlier years, sedation and monitoring were managed by the endoscopy team and only i.v. midatsolame was used. Duodenal peristalsis was reduced by i.v. hyos-cine butylbromide or i.v. glucagon. Procedures were clas-sified as therapeutic when sphincterotomy, stone removal, stent insertion or removal, brush cytology or dilatation was performed. Routine serum blood samples after 6–10 hours included WBC count, haemoglobin, CRP and amylase. Each patient was followed up in our hospital for at least 24 hours after ERCP.
Complications were classified using the standardised criteria proposed by Cotton et al. (22). A complication was defined as any adverse event occurring during the 30-day period after ERCP requiring more than one night of hos-pitalisation. Severe complications required more than ten days of hospitalisation, necessitated surgical or invasive radiologic intervention, required admission to the intensive care unit (ICU) or caused patient’s death. We compared the age, sex, history of diabetes, use of anticoagulation treatment, long-term corticosteroid use and the procedure related factors (e.g. precut) to mortality and morbidity to find significant risk factors. The grade of procedure diffi-culty and complexity was defined by the criteria published earlier (23).
Statistical analysis was performed using IBM SPSS Sta-tistics 19.0. Categorial variables were compared using Chi-square test and calculating odds ratios and their 95 % confidence intervals. A probability of < 0.05 was regarded as significant. The study protocol was approved by ethics committee of KHCH.
RESULTS
A total of 1207 consecutive ERCPs were performed to 809 patients. Papilla was intact i.e. no earlier sphinc-terotomy had been performed in 68.4% (n = 825) of procedures. In these procedures 61.1% of patients were females and the median age was 70 years (range 17–101). The cannulation of the desired duct was achieved in 89.2% (n = 736) of the procedures with intact papilla in the first ERCP session of the study period. Complete stone extraction was successful in 91.3% and bile duct obstruction could be relieved completely in 80.1% of procedures with intact papilla. Of all 1207 ERCPs performed, 80.9% were therapeu-tic, 11.7% diagnostic or without therapeutic interven-tions and in 7.4% cannulation was unsuccessful.
The most common indications were CBD stones or bile duct obstruction caused by malignancy (Table 1). Of ERCPs with intact papilla, precut was performed in 12%, standard sphincterotomy in 73.8%, CBD stone removal in 33.7%, brush cytology in 11.8% and stric-ture dilation in 8.1% of procedures. A biliary stent
TABLE 1
Indications or work-up diagnosis of 825 ERCPs with intact papilla
Indication or work-up diagnosis n %
CBD stone 266 32.2%
Malignancy1 173 20.9%
Bile duct obstruction or jaundice without accurate diagnosis 172 20.8%
Acute biliary pancreatitis 64 7.8%
Acute cholangitis 59 7.2%
Chronic pancreatitis 35 4.2%
Dysfunction of sphincter of Oddi 10 1.2%
Bile leak after cholecystectomy 7 0.8%
Other benign biliary disease2 39 4.7%
Total 825 100.0%1 Pancreatic cancer or papillary cancer 114 (13.8%), liver metastasis
or hepatocellular cancer 32 (3.9%), cancer of biliary tract or gall-bladder 18 (2.2%), other (e.g. lymphoma or malignancy of un-known origin) 9 (1.1%)
2 Cases of benign stricture of CBD, primary sclerosing cholangitis, papillary tumor or polyp, bile duct obstruction after cholecystec-tomy, primary biliary cirrhosis, cyst of CBD and pancreatic duct stone or stricture.

3ERCP procedures in a Finnish community hospital: a retrospective analysis of 1207 cases
was inserted for malignant stricture in 11.4% and for other reasons in 3.3% of ERCPs. A pancreatic stent was inserted in 0.6% and pancreatic stone was ex-tracted in 0.5% of primary procedures. Pancreatogra-phy was performed or contrast medium was observed in the pancreatic duct in 47.8% of ERCPs with intact papilla and in 38.8% of all procedures. Of all 1207 procedures a biliary stent exchange was performed in 7.6% of ERCPs.
The complexity and difficulty level of completed ERCP procedures were graded by a three-step clas-sification. ERCPs with intact papilla fell into catego-ries I, II and III respectively as 79%, 19% and 2%. No connection between the level of difficulty and com-plications was found.
Of all ERCPs, 8.7% were planned second attempt procedures 2–14 days after an incomplete or failed procedure. These included cases where an earlier at-tempted ERCP had failed or had been intentionally aborted after performing precut sphincterotomy in a difficult cannulation.
Overall complication rate was 11.1% in procedures with intact papilla (Table 2) and 9.8% in all ERCPs. The majority of the complications (77 %) were mild or moderate i.e. they were managed conservatively and necessitated less than ten days of hospitalisation. No statistically significant risk factors for overall complications were found.
PANCREATITIS
Pancreatitis occurred after 16 (1.9%) of procedures with intact papilla. Two of these were severe and re-quired operation. Both were caused by a therapeutic procedure. None of the patients died of pancreatitis.
After precut sphincterotomy, pancreatitis of any de-gree was noted in six (5.6%) cases and after standard sphincterotomy in 11 (1.8%) cases, but the difference was not statistically significant (NS). Precut was a risk factor of moderate or severe pancreatitis (OR 3.8, 95% CI 1.1–12.8, p 0.022). Patient´s sex, diabetes, medication or contrast injection to pancreatic duct during ERCP did not affect the risk of pancreatitis. In patients under 50 years of age pancreatitis developed in five cases (3.4%) and in 11 cases (1.6%) in older patients (NS).
HAEMORRHAGE
Haemorrhage was present after 16 (1.9%) ERCPs with intact papilla. Half of these (50%) were treated with re-duodenoscopy to achieve haemostasis. Two pa-tients died of ERCP-related haemorrhage. Bleeding resulted after four (4.0%) procedures with precut sphincterotomy and after 13 (2.1%) of those with standard sphincterotomy (NS). All ERCPs that caused moderate or severe bleeding were therapeutic. None of the patient or procedure related factors (e.g. age, use of anticoagulation treatment, sphincterotomy, precut) were related to the incidence of hemor-rhage.
CHOLANGITIS
Seventeen (2.1%) patients developed cholangitis after ERCPs with intact papilla. One patient was treated surgically for a suspected duodenal perforation. Both cases of severe cholangitis developed after therapeu-tic procedures. No risk factors for cholangitis were found.
TABLE 2
Complications and ERCP related mortality in 825 ERCPs with intact papilla (i.e. no earlier sphincterotomy). Age: median (interquartile range)
Complication Difficulty grade Age (years) n (%) ERCP-related death n (%)
Pancreatitis Mild 04 (0.5%) 0 Moderate 10 (1.2%) 0 Severe 02 (0.2%) 0 Total 63 (44–74) 16 (1.9%) 0
Haemorrhage Mild 01 (0.1%) 0 Moderate 09 (1.1%) 0 Severe 06 (0.7%) 2 Total 74 (53–83) 16 (1.9%) 2
Cholangitis Mild 03 (0.3%) 0 Moderate 12 (1.5%) 0 Severe 02 (0.2%) 0 Total 77 (58–83) 17 (2.1%) 0
Perforation Mild 05 (0.6%) 0 Moderate 0– 0 Severe 03 (0.4%) 0 Total 72 (68–81) 08 (1.0%) 0
Other Mild 05 (0.6%) 0 Moderate 20 (2.4%) 0 Severe 10 (1.2%) 0 Total 79 (68–88) 35 (4.2%) 0
All complications 75 (63–83) 91 (11.1%) 2 (0.2%)

4 A. Siiki, A. Tamminen, T. Tomminen, P. Kuusanmäki
PERFORATION
Perforation was observed in eight (1.0%) patients. Most of the perforations (75%) were retroperitoneal and were noticed during the endoscopy (75%). None of the cases were caused by a duodenoscope. Three patients required surgery. All cases of moderate or severe perforations were preceded by a therapeutic ERCP. Perforation occurred in two (2.0%) procedures with precut sphincterotomy and in four procedures (0.7%) with standard sphincterotomy (NS). Patient or procedure related factors were not related to risk of perforation. Two patients of all of the 1207 ERCPs died after perforation.
OTHER COMPLICATIONS
Other morbidity or complications developed in 35 (4.2%) of ERCPs with intact papilla. These included seven (0.8%) patients with pneumonia, seven (0.8%) infections of unknown origin, six (0.7%) cerebral in-farctions, four (0.5%) cardiac events and four (0.5%) cases with urinary retention or urinary tract infection. Two (0.2%) patients with cholecystitis were operated on. In addition, one case (0.1%) of each of the follow-ing events occurred: acute colitis, gastroenteritis, deep venous thrombosis, suspected pulmonary em-bolism, and haemorrhage from oesophageal varices. Age over 60 years was a risk factor of other complica-tions graded moderate or severe (OR 3.6, 95% CI 1.1–12.0, p 0.027).
MORTALITY
The ERCP-related mortality in procedures with intact papilla was 0.2% (n = 2). Both cases resulted from hemorrhage. Overall mortality in 30 days was 3.3% (n = 27). Eighteen (2.2%) of these were caused by can-cer and seven (0.8%) by other, non-ERCP-related ad-verse events. These seven deaths consisted of two cases of pneumonia, three cardiac events, a septic infection after insertion of a percutaneous transhe-patic biliary drain and a haemorrhage from esopha-geal varices in a patient with severe liver cirrhosis. Age over 60 years was a risk factor of overall 30-day mortality (OR 11.8, 95% CI 1.6–87.4, p 0.002).
In all of the 1207 procedures, ERCP-related mortal-ity was 0.4% (n = 5). Two patients died after perfora-tion. In addition, the death of a 68-year old male in the ICU nine days after biliary stent insertion was considered ERCP-related. In autopsy, the cause of death was multi-organ failure of unknown origin.
DISCUSSION
Given that ERCP is a technically demanding invasive procedure with a risk of complications, ERCP prac-tice should be critically evaluated in terms of indica-tions, success rates and complications (18). Most of the earlier studies come from university clinics, whereas there are only few reports of complications in low-volume centres (10). Our objective was to de-scribe ERCP-practice in a community hospital and to
report success rates and complication figures that could be compared to earlier studies.
In our material 80.9% of all ERCPs were therapeu-tic and 11.7% were diagnostic or without need for intervention. In the earlier studies, the proportion of therapeutic ERCPs has ranged from 54.7% to 97.7% (7, 8, 10, 12, 13). Both the indications of ERCPs and the proportions of different biliary procedures were essentially similar to those described in earlier re-ports (6, 8–12). The number of pancreatographies seems high, because it was defined as any amount of contrast medium in the pancreatic duct and not only as an intentional diagnostic filling of the duct. In the early years of the study period, as CBD was cannu-lated without a guide wire, a careful injection of con-trast medium to pancreatic duct was sometimes un-avoidable. In our study a pancreatic stent was in-serted in 1.8% of all procedures and in 0.6% of ERCPs with intact papilla. No complications occurred after pancreatic procedures. In the earlier studies the pro-portion of pancreatic procedures varied widely, which may indicate differences in patient mix between cen-tres. In the study by Williams et al. (9) pancreatic procedures accounted for 1.6% of ERCPs. In other reports, the proportion of pancreatic stent insertions has ranged from 5.5 to 9.2% of procedures (10, 11).
A three-step classification of procedure complexity has been used in a few earlier studies to control the effect of patient mix to complications (10, 11). More complex and more difficult procedures (grade III) have resulted more often in severe complications or mortality (11). The proportion of the most complex procedures was expectedly slightly lower than in larger centres (10, 11). In a retrospective setting, de-fining ERCP complexity may be unreliable. In our material, five patients were referred to the endoscopy unit of Helsinki University Hospital (HUS) because demanding pancreatic interventions were needed and in our unit even repeated attempts had not been successful.
We used precut sphincterotomy in 12% of ERCPs with intact papilla. This is slightly more than 8.5–10.0% in earlier studies (5, 6, 19, 21). In our material precut was a significant risk factor for moderate or severe pancreatitis. This concurs with findings show-ing both difficult cannulation and precut sphinctero-tomy to be risk factors of ERCP-related complications (5, 7, 8, 9, 12). On the other hand, properly timed precut sphincterotomy performed by an expert en-doscopist makes it possible to complete the procedure endoscopically without risk of operative or percuta-neous interventions (3, 4, 19, 20, 21). It has been sug-gested, that precut sphincterotomy should be used early enough in a difficult cannulation to avoid nu-merous cannulation attempts and unnecessary injury to the papilla or to the pancreatic duct. Early use of precut sphincterotomy may reduce the risk of pan-creatitis (24, 25). The second cannulation attempt a few days after precut is usually easier (13, 19, 20).
In the last two years of the study period, we selec-tively used pancreatic sphincterotomy in difficult bile duct cannulation (21, 26, 27). This technique has been shown to enable bile duct cannulation relatively safely in up to 98.1% of cases (20). We did not use

5ERCP procedures in a Finnish community hospital: a retrospective analysis of 1207 cases
temporary pancreatic stenting to prevent ERCP-re-lated pancreatitis (12, 27, 28, 29).
The success rate of cannulation and complication figures are usually reported from ERCPs with no ear-lier sphincterotomy. The cannulation of the papilla is easier and less risky if a sphincterotomy has already been done. In the present study the success rate of cannulation was 89.2% of ERCPs in which the papilla was intact and 92.6% of all ERCPs. Studies from aca-demic centres have reported successful bile duct can-nulation in 85.6–98.1% of cases (8, 9, 10, 12, 13, 19, 20, 21). However, in our study the proportion of planned second attempt ERCPs 2–14 days after aborted or failed procedure was 8.7% of all procedures. As far as we know, this figure has seldom been reported in other studies; in the study by Palm et al., the propor-tion of second attempt ERCPs was 3.0% (20). We have tried to avoid complications by converting a difficult cannulation attempt early enough into a precut sphincterotomy, followed by a planned second at-tempt ERCP a few days later. As our figures are per procedure, the definitive success rate per patient after repeated ERCPs remains unknown. In the other stud-ies, repeat ERCP after precut sphincterotomy has been shown to enable successful cannulation ulti-mately in up to 96.0–98.2% of cases (19, 20). The suc-cess rates for extraction of CBD stone or relieving bile duct obstruction were similar to the results of Colton et al. in a community setting and to the published guideline (10, 18).
In our study the incidence of pancreatitis (1.9%) was lower than 2.6–7.2% reported earlier (3, 4, 6–12, 21). According to the prospective studies, younger patients and patients under 60 years of age have been in increased risk of pancreatitis (4, 9, 12). In the ear-lier studies, the incidence of haemorrhage and cho-langitis has been 0.3–2.0% and 0.3–1.4%, respectively (3, 4, 6–12). The highest incidence of cholangitis has reportedly been up to 5% (8). Our results substantiate this. Some cases of haemorrhage could have been avoided, as some of the procedures were performed to extremely high risk patients as a palliative attempt to relieve e.g. malignant biliary obstruction. Perfora-tion has occured in 0.1–1.1% of cases (3, 4, 6–12). Our incidence was 1.0%. Other, e.g. cardio-pulmonary complications were slightly more frequent than 0.2–1.5% in recent reports (7–12). On the other hand, in a large prospective Danish study with a thorough fol-low-up, the incidence of other complications was 5.1% with an overall complication rate of 15.9% (8). As noted in the earlier studies (7–12), the majority of the complications was mild or moderate and could be managed non-operatively with a short hospitalisa-tion.
The most of the mortality was caused by cancer or non-ERCP-related diseases. ERCP-related mortality in procedures with intact papilla (0.2%) was similar to figures of 0–1.0% of the earlier studies (8, 10, 11). In the reports from Finnish academic centres, ERCP-related mortality has been 0.1–0.3% (13, 14, 20). Over-all mortality usually ranges from 1.4% to 5.8% (8, 10, 11), but this figure, as well as rate of overall morbid-ity, may be influenced to some extent by differences in patient follow-up and study design. Both non-ER-
CP-related complications and overall mortality were expectedly related to patient´s age of over 60 years.
This study describes ERCP practice in a low-vol-ume community hospital. The indications and suc-cess rates as well as morbidity and mortality are ac-ceptable compared to those in earlier reports and published guidelines. Although the success rate of cannulation and thereby ERCP procedures seem to be somewhat lower than in tertiary referral centres, our results confirm that ERCP procedures can be safely performed in a low-volume ERCP unit. Adequate in-dications of ERCP and good procedure routine can be maintained, at least when procedures are concen-trated on a few experienced endoscopists. Cannula-tion success rates reported from academic centers may be achieved using techniques, such as pancreatic sphincterotomy and cannulation with the double guide wire technique, that were used only in the last years of the study period.
REFERENCES
01. Silviera ML, Seamon MJ, Porshinsky B et al: Complications related to endoscopic retrograde cholangiopancreaticography: a comprehensive clinical review. J Gastrointestin Liver Dis 2009:18(1);73–82
02. Andriulli A, Loperfido S, Napolitano G et al: Incidence rates of post-ERCP complications. A systematic survey of prospec-tive studies. Am J Gastroenterol 2007;102:1781–1788
03. Freeman ML, Nelson DB, Sherman S et al: Complications of endoscopic biliary sphincterotomy. N Engl J Med 1996;335:909–918
04. Loperfido S, Angelini G, Benedetti G et al: Major early compli-cations from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 1998:48(1);1–10
05. Freeman ML, DiSario JA, Nelson DB et al: Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Gastroin-test Endosc 2001: 54(4);425–434
06. Masci E, Toti A, Mariani A et al: Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol 2001:96(2);417–423
07. Vandervoort J, Soetikno RM, Tham TC et al: Risk factors for complications after performance of ERCP. Gastrointest Endosc 2002:56 (5);652–656
08. Christensen M, Matzen P, Schulze S et al: Complications of ERCP: a prospective study. Gastrointest Endosc 2004:60:721–731
09. Williams EJ, Taylor S, Fairclough P et al: Risk factors for com-plication following ERCP; results of a large−scale, prospective multicenter study. Endoscopy 2007:39;793–801
10. Colton J, Colleen C, Curran MS: Quality indicators, including complications, of ERCP in a community setting: a prospective study. Gastrointest Endosc 2009:70;457–467
11. Cotton PB, Garrow DA, Gallagher J et al: Risk factors of com-plications after ERCP: a multivariate analysis of 11497 proce-dures over 12 years. Gastrointest Endosc 2009:70(1);80–889
12. Wang P, Li ZS, Liu F et al: Risk factors for ERCP-related com-plications: a prospective multicenter study. Am J Gastroen-terol 2009:104;31–40
13. Salminen P, Laine S, Gullichsen R: Severe and fatal complica-tions after ERCP: analysis of 2555 procedures in a single expe-rienced center. Surg Endosc 2008:22;1965–1970
14. Halme L, Doepel M, von Numers H et al: Complications of diagnostic and therapeutic ERCP. Ann Chir Gynaecol 1999:88; 127–131
15. Rabenstein T , Schneider HT, Bulling D et al: Analysis of the risk factors associated with endoscopic sphincterotomy tech-niques: preliminary results of a prospective study, with em-phasis on the reduced risk of acute pancreatitis with low dose anticoagulation treatment. Endoscopy 2000:32;10–19
16. Räty S, Sand J, Pulkkinen M et al: Post-ERCP pancreatitis: re-duction by routine antibiotics. J Gastrointest Surg 2001:5(4);339–345

6 A. Siiki, A. Tamminen, T. Tomminen, P. Kuusanmäki
17. Sand J, Uusimäki J, Räty S et al: Sappi ja haimatiehyen tähys-tystoimenpiteet onnistuvat myös polikliinisesti (in Finnish) Duodecim 2005:121(7);763–767
18. Baron TH, Petersen BT, Mergener K et al: Quality Indicators for endoscopic retrograde cholangiopancreatography. Am J Gastroenterol 2006:101;892–897
19. Gullichsen R, Lavonius M, Laine S et al: Needle knife assisted ERCP. Surg Endosc 2005:19(9);1243–1245
20. Palm J, Saarela A, Mäkelä J: Safety of Erlangen papillotomy: An analysis of 1044 consecutive ERCP examinations in a single institution. J Clin Gastroenterol 2007:41(5);528–533
21. Halttunen J, Keränen I, Udd M et al: Pancreatic sphincterotomy versus needle knife precut in difficult biliary cannulation. Surg Endosc 2009:23;745–749
22. Cotton PB, Lehman G, Vennes AJ et al: Endoscopic sphincter-otomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991:37;383–393
23. Madhotra R, Cotton PB, Vaughn J et al: Analyzing ERCP prac-tice by a modified degree of difficulty scale: A multicenter database analysis. Am J Gastroenterol 2000;95:2480–2481
24. Gong B, Hao L, Bie L et al: Does precut technique improve selective bile duct cannulation or increase post-ERCP pancrea-
titis rate? A meta-analysis of randomized controlled trials. Surg Endosc 2010:24;2670–2680
25. Cennamo V, Fuccio L, Zagari RM et al: Can early precut imple-mentation reduce ERCP-related complication risk? Meta-anal-ysis of randomized controlled trials. Endoscopy 2010:42;381–388
26. Goff J: Common bile duct pre-cut sphincterotomy: transpan-creatic sphincter approach. Gastrointest Endosc 1995:41;502–505
27. Kylänpää L, Halttunen J: ERCP uudet tekniikat (in Finnish). Duodecim 2008:124(12);1419–1424
28. Tarnasky P, Palesch Y, Cunningham J et al: Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology 1998:115;1518–1524
29. Mazaki T, Masuda H, Takayama T: Prophylactic pancreatic stent placement and post-ERCP pancreatitis: a systematic re-view and meta-analysis. Endoscopy 2010:42;842–852
Received: February 25, 2011Accepted: June 18, 2011

Scandinavian Journal of Gastroenterology. 2014; 49: 1385–1390
ORIGINAL ARTICLE
Spyglass single-operator peroral cholangioscopy seems promising in theevaluation of primary sclerosing cholangitis-related biliary strictures
ANTTI SIIKI1, IRINA RINTA-KIIKKA2, TARMO KOIVISTO1, KAIJA VASAMA3,JUHANI SAND1 & JOHANNA LAUKKARINEN1
1Department of Gastroenterology and Alimentary Tract Surgery, Tampere University Hospital, Tampere, Finland,2Department of Clinical Radiology, Tampere University Hospital, Tampere, Finland, and 3Department of Pathology,Fimlab Laboratories, Tampere University Hospital, Tampere, Finland
AbstractEarly diagnosis of dysplastic changes and exclusion of cholangiocarcinoma (CCA) in patients with primary sclerosingcholangitis (PSC) remain a major clinical challenge. Although SpyGlass single-operator cholangioscopy (SOC) appearseffective in diagnostics of indeterminate biliary strictures, there are only few studies on its safety in PSC-related strictures.Objective. The aim of this study was to assess the clinical feasibility of SOC and directed biopsies, flow cytometry, and brushcytology in PSC patients.Materials andmethods. Eleven consecutive patients (median age 45 years, 5 females) undergoingSOC for progression of PSC in a single tertiary center were included in a prospective observational study. Results. Brushsample and directed biopsies were successfully acquired from strictures in all cases. Samples were adequate for cytological andhistological diagnosis in 9 (82%) and 10 patients (91%), respectively. There were two cases of pancreatitis. In one patient, flowcytometry showed aneuploidy, which resulted in closer follow-up. Conclusions. SpyGlass SOC and directed biopsies seem tooffer a feasible and promising method in evaluation of PSC-related strictures. However, the long-term prognostic value it addsto cytology and flow cytometry remains to be assessed in future trials.
Key Words: Benign biliary strictures, cholangioscopy, endoscopic retrograde cholangio-pancretography, primary sclerosingcholangitis
Introduction
Early diagnosis of dysplastic changes and exclusionof cholangiocarcinoma (CCA) in patients withprimary sclerosing cholangitis (PSC) remain a majorclinical challenge. Although single operator peroralcholangioscopy (SOC) appears effective in diagnos-tics of indeterminate biliary strictures, there are onlyfew studies of its safety and feasibility on PSC-relatedstrictures [1–9]. Combination of cholangiography,brush cytology, analysis of serum tumor markers(CA19-9, CEA) and flow cytometry (DNA ploidity)provide only relatively accurate differentiationbetween benign and malignant strictures in PSC[9,10].
The objective was to characterize the initial expe-rience and clinical feasibility of SOC in PSC patientsin a tertiary endoscopy unit and to evaluate thecombined diagnostic yield of SOC and directedbiopsies, flow cytometry and brush cytology.
Methods
All consecutive patients who underwent endoscopicretrograde cholangiopancreatography (ERC) andSOC between March and August 2012 for progres-sion of PSC in a single tertiary center (TampereUniversity Hospital, Finland) were included. Thecase series was carried out in accordance withDeclaration of Helsinki.
Correspondence: Johanna Laukkarinen, MD PhD, Department of Gastroenterology and Alimentary Tract Surgery, Tampere University Hospital, Teiskontie 35,P.O. Box 2000, 33521 Tampere, Finland. Tel: +358 3 311 64314, + 358 50 358 6556. Fax: + 358 3 311 64358. E-mail: [email protected]
(Received 4 February 2014; revised 5 April 2014; accepted 24 June 2014)
ISSN 0036-5521 print/ISSN 1502-7708 online � 2014 Informa HealthcareDOI: 10.3109/00365521.2014.940376
Scan
d J
Gas
troe
nter
ol D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y T
ampe
re U
nive
rsity
on
12/0
8/14
For
pers
onal
use
onl
y.

The diagnosis of PSC was based on the typicalfindings in MRCP (magnetic resonance cholangio-pancreatography) and previous ERC. MRCP wasperformed using standard imaging protocols includ-ing heavily T2-weighted two-dimensional thin-section and thick sequences in coronal plane tovisualize all biliary ductal structures. Additionally,gadolinium-enhanced sequences were routinelyused to estimate inflammatory and possible neoplasticchanges.SOC procedures were performed by SpyGlass
Direct Visualization Equipment (Boston ScientificCorp, USA) according to the methods described indetail by Chen et al. [1]. The number of directedbiopsies (Figures 1, 2 and 3) ranged from four to sixand they were obtained with SpyBite biopsy forceps(Boston Scientific Corp). For both cytology [11] andflow cytometric analysis [10], brush sampling (RX
Cytology Brush, Boston Scientific Corp) wasperformed. A single dose of intravenous antibiotics(i.v. cefuroxime 1.5 g) and anti-inflammatory sup-pository (diclofenac 100 mg) was given to all patientsbefore ERC. Patient sedation (i.v. midatsolame andoxycodone) was administered and monitored by anendoscopy team. To reduce duodenal peristalsis, i.v.hyoscine butylbromide (20–40 mg) or i.v. glugacon(0.3 mg) was given. Patients�MRCP and cholangiog-raphy images were carefully reanalyzed by an experi-enced abdominal radiologist to classify the PSCfindings according to the well-established methodof Majoie et al. [12] presented in Table I. Procedureswere performed in outpatient setting, except in 4 caseswith 24 hours of in-patient observation for deep
A B
Figure 1A-B. Cholangiography image of a 49-year-old female (patient no 9) with PSC duration of 23 years. Intrahepatic findings (*) andSpyGlass cholangioscope (**) in the common hepatic duct.
Figure 2. A hematoxylin-eosin–stained specimen taken by aSpyBite biopsy forceps from bile duct of a 49-year-old patient(no 9) presenting active chronic inflammation, regenerative atypia,and no dysplasia.
Figure 3. Typical appearance of primary sclerosing cholangitis inextrahepatic bile duct of a 51-year-old male (no 7). Images acquiredby SpyGlass single-operator peroral cholangioscopy; note SpyBitebiopsy forceps in the lower right-hand image.
1386 A. Siiki et al.
Scan
d J
Gas
troe
nter
ol D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y T
ampe
re U
nive
rsity
on
12/0
8/14
For
pers
onal
use
onl
y.

sedation or patient logistics. ERC complicationswere classified according to Cotton et al. [13], andwere prospectively recorded for 30 days after theprocedure.Study endpoints were technical success, frequency
of adequate biopsies obtained and complication rate.For PSC progression, prospective follow-up fromhospital records was carried out until March 2014.
Results
A total of 11 patients (5 female) underwent ERC withSOC. The baseline characteristics of the study
population are presented in Table II. The medianage was 45 years (range 24–66). The median timefrom the diagnosis of PSC was 8 years (range 1–28years).In nine patients (82%) a previous ERC, and in
six (55%) a previous sphincterotomy had beenperformed. None of the patients had previous post-ERC pancreatitis. Pre-procedural serum tumormarkers (CA19-9 and CEA) were within normalrange in all patients.After successful wire-guided biliary cannulation,
endoscopic sphincterotomy was performed on allbut one patient (90%), for whom earlier sphincter-otomy was adequate.The radiologic grade of PSC changes is presented
in Table I. Both intra- and extrahepatic changes werepresent in eight (73%) patients; the other three hadintrahepatic disease.Brush samples for cytology and flow cytometry
were successfully obtained from extrahepatic and/orintrahepatic dominating strictures in all cases. Directvisualization of the epithelium at the site of thedominant stricture as well as acquiring SOC-guidedbiopsies was successful in all cases (Figure 3). Thestricture could be completely traversed with a cho-langiosope in six cases (55%). In others, a tightimpassable dominant stricture was located intrahepa-tically, except in one patient, with a narrow class IVextrahepatic stenosis. Bile duct stones were unexpect-edly detected in cholangioscopy in one patient (9%)and successfully removed by balloon. Stricture
Table I. Classification of cholangiographic findings in primarysclerosing cholangitis [12].
Type of ductinvolvement/classification Cholangiographic abnormalities
IntrahepaticI Multiple strictures; normal caliber of
bile ducts or minimal dilationII Multiple strictures, saccular dilations,
decreased arborizationIII Only central branches filled despite
adequate filling pressure, severepruning
ExtrahepaticI Slight irregularities of duct contour, no
stenosisII Segmental stenosisIII Stenosis of almost entire length of ductIV Extremely irregular margin;
diverticulum-like out-pouchings
Table II. Patient demographics, indication for and findings of ERC, results of cytological and flow cytometric analysis, and histologicalfindings of SpyGlass biopsies.
Classification (Majoie)
N Age Sex Indication (PSC) Intrahepatic Extrahepatic Cytology DNA index S-phase Histology
1 43 M Progression in MRI III IV 2 1 1,8 Inadequate2 28 M Progression in MRI,
elevated LFTI Normal 2 1.21 7.2 Inflammation
3 44 F Progression in MRI,elevated LFT
II II 2 1 2.1 Normal
4 41 M Progression in MRI,elevated LFT
III II 1 1 NA Inflammation
5 45 F Elevated LFT,no previous ERC
II I 2 1 1.2 Inflammation
6 54 F Elevated LFT II II Inadeq. Inadeq. NA Regenerativeatypia
7 51 M More than 5 yearsrom ERC
I IV 2 1 NA Fibrosis
8 50 F Progression in MRI III I 2 1 0 Fibrosis9 49 F Progression in MRI III II 2 1 6.8 Inflammation10 66 M Progression in MRI I Normal Inadeq. Inadeq. NA Fibrosis11 24 M Over 5 years from
ERCI Normal 1 1 0 Fibrosis
Abbreviations: Age (years); PSC = primary sclerosing cholangitis; MRI = magnetic resonance cholagiopancreatography; LFT = liver functiontests; ERC = Endoscopic retrograde cholangiography; Stricture classification = Majoie; Cytology = Papa classification. Inadeq = Sampleinadequate for diagnosis.
Spyglass cholangioscopy in sclerosing cholangitis 1387
Scan
d J
Gas
troe
nter
ol D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y T
ampe
re U
nive
rsity
on
12/0
8/14
For
pers
onal
use
onl
y.

dilatation or stenting was not necessary in any ofthe procedures.Out of nine patients (82%) with adequate brush
sample for cytological analysis, the result wasclass 2 in seven and class 1 in two. The flow cyto-metric analysis showed normal diploidic DNA in allbut one patient, who had a marginally elevated DNAindex of 1.21 and normal S-phase of 7.2%. Thespecimens were adequate for successful histologicalanalysis in 10 (91%) patients; one normal bile ductepithelium and seven regenerative, fibrotic or chronicinflammatory changes (Table II).Two patients developed immediate post-ERC com-
plications from which they recovered uneventfullywithout need for interventions or intensive care; a28-year-old male and a 43-year-old male both devel-oped a moderate pancreatitis within a few days afterERC.The follow-up of PSC patients was planned accord-
ing to guidelines of our institution. Themedian lengthof follow-up was 22 months (range 16–24 months).Patient 1 with severe cholangiography changes andrapid PSC progression at first referred to the liver-transplantation unit of Helsinki University Hospital,Finland, has undergone endoscopic stenting and stentremoval. Without episodes of acute cholangitis ordisease progression, liver transplantation has not yetbeen performed. Patient 2 with initially aneuploidicflow cytometry was scheduled for re-ERC at 6 monthswith normalized results. Next surveillance ERCP isgoing to take place at 18 months. Other patients werescheduled for outpatient follow-up (liver enzymes,CA19-9, MRCP, colonoscopy for ulcerative colitis)and for re-ERC at 12 months (patients 3, 4, 6, 7 and8) or at 36–48 months (patients 5, 9, 10 and 11).None of the patients have unexpected diseaseprogression or episodes of acute cholangitis. Patient8 with a common bile duct stone has been asymp-tomatic ever since the stone removal.
Discussion
SOC has been reported to increase the sensitivity andspecificity in the detection of malignant biliary stric-tures [1–5]. It may also be beneficial in PSC patients[6,7], where cholangiography (ERC) andMRCP havetraditionally been the foundation of diagnostics. Tothe best of our knowledge, no reports on the results ofcombined diagnostic yield of SOC, directed biopsies,flow cytometry and brush cytology in PSC have beenpresented. We found that direct visualization SOCseems feasible and it, thus, may be promising in termsof even better stricture evaluation and diagnosticswhen compared to methods such as cholangiography,flow cytometry and brush cytology. The true safety,
diagnostic value of SOC and guided biopsies in thelong term remain to be assessed in future trials.The most important clinical problem with PSC-
related stricture is the prompt diagnosis of biliarydysplasia and exclusion or early detection of cholan-giocarcinoma, potentially associated with poorprognosis [8].In PSC, the combination of brush cytology, flow
cytometry and serum tumor markers (CEA, CA19-9)has been found to yield the most accurate results inpredicting malignancy; sensitivity of 100% and spec-ificity of 85%, positive predictive value of 78% andnegative predictive value of 100% were reported byLindberg et al. in 24 months of follow-up [9]. Com-bining flow cytometry and cytology in predicting livertransplantation or a diagnosis of CCA or dysplasia inPSC has produced sensitivity and specificity of 72%and 82%, respectively [10]. Brush cytology has a highspecificity but sensitivity is low, which is similar toflow cytometry with sensitivity of 29% and specificityof up to 100% [9].In the earlier studies, direct SOC visualization
without biopsies has been found misleading andunreliable in PSC setting due to the inflammatoryand fibrotic appearance of the stricture [6]. Predictionof malignancy in PSC with multiple strictures may bemore challenging than in patients with non-PSCstenosis, who usually have otherwise normal morphol-ogy of the biliary tree [7].In unselected biliary strictures, the suspicious
findings can usually be confirmed by SOC-directedbiopsies [1]. In indeterminate strictures the accuracyof biopsies was 87% in distinguishing malignant frombenign stricture [4]. In a multicenter study byChen et al., SOC was found to be decidedly moreaccurate than cholangiography in the diagnostics ofmalignancy; sensitivity and specificity were 78% and82% to 51% and 54%, respectively [2]. SOC anddirected biopsies have been found to alter clinicalmanagement in 64% of patients in indeterminatestrictures [2]. Although the sensitivity, accuracy andnegative predictive value of mini-forceps biopsies havereportedly been superior to those of brush cytology orcholangiography-guided biopsies, the negative predic-tive value being of mini-forceps biopsy has been as lowas 69% [3]. It has been suggested that in patients withsuspected malignancy but benign tissue samples,a repeated cholangioscopy with biopsies should becarried out [7].In the present study, all procedures were technically
successful. The cannulation of the papilla has report-edly been more difficult in PSC patients than inunselected patients with an indeterminate biliarystricture [4]. Very narrow intrahepatic or hilar stric-ture may sometimes prevent safe passing with a
1388 A. Siiki et al.
Scan
d J
Gas
troe
nter
ol D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y T
ampe
re U
nive
rsity
on
12/0
8/14
For
pers
onal
use
onl
y.

cholangioscope [6]. In these cases, tissue samplescould still be obtained from the stricture area bySOC-directed biopsies, which is clinically moreimportant than completely traversing an intrahepaticstricture with a cholangioscope.Our findings support the excellent rate (91%) of
obtaining adequate biopsies for histological analysis.In the literature the rate of sufficient biopsies acquiredhas been up to 98% in PSC [6]. However, determin-ing epithelial dysplasia from tiny amount of tissueobtained by mini-forceps for histologic samples maybe unreliable, since the biopsy bites seem to consist ofmostly stroma and only small amount of epithelialtissue. We thus recommend acquiring more than fourto six directed biopsies per stricture. Moreover, thecytology, flow cytometry and histology samples fromeach case should all be analyzed simultaneously andcomplementary to each other by experienced andhighly specialized pathologists.SOC was considered useful in evaluation of PSC.
There was no discrepancy between information fromSOC image, cytology, flow cytometry and histology.However, our sample size is small for any conclusionof additional clinical value provided by SOC. In thestudy by Tischendorf et al. on 53 PSC patients, SOCwas found to significantly increase the ability to dis-tinguish malignant from benign strictures comparedto cholangiography or brush cytology [7]. An SOCsensitivity of 92%, specificity of 93%, accuracy of93%, positive predictive value of 79% and negativepredictive value of 97% in the evaluation of dominantPSC strictures were reportedly achieved in themedian follow-up of 47 months [7].There was one case of biliary stones undiagnosed in
MRCP or cholangiography, but found and removedby SOC. In the study of Awadallah et al., cholangio-scopy revealed in 30% of PSC patients bile ductstones missed in cholangiography, the removal ofwhich resulted in clinical improvement in up to77% [6].Two complications occurred, neither with severe
clinical consequences. These patients were among thefirst four SOCs performed for PSC in our institution,which may be attributable to learning curve. The rateof post-ERC pancreatitis has reportedly been 7% inPSC patients when SOC is not performed, withfemale sex and difficult cannulation increasing andearlier sphincterotomy decreasing the risk [14], Themost common complications related to SOC areepisodes of cholangitis and pancreatitis [1,4,5,15].Total overall ERC complications have been reportedto be twice, and cholangitis nearly five times asfrequent when concomitant SOC is performed [15].In conclusion, SOC and directed biopsies seem
to offer a feasible and promising method in evaluation
of PSC-related strictures, especially in extrahepaticdisease. The additional information SOC provideswhen combined with flow cytometry, brush cytologyand serum tumor markers is a subject for future trials.Moreover, further studies on PSC patients are neededto assess the predictive value and long-term effect onclinical decision-making of this novel technology.
Acknowledgments
This work was financially supported by the SigridJusélius Foundation, Finland, and the competitiveresearch found of Pirkanmaa Hospital District,Finland.
Declaration of interest: The authors report noconflicts of interest. The authors alone are responsiblefor the content and writing of the paper.
References
[1] Chen Y, Pleskow D. SpyGlass single-operator peroralcholangiopancreatoscopy system for the diagnosis and ther-apy of bile-duct disorders: a clinical feasibility study (withvideo). Gastrointest Endosc 2007;65:832–41.
[2] Chen Y, Parsi M, Binmoeller K, Hawes R, Pleskow D,Slivka A, et al. Single-operator cholangioscopy in patientsrequiring evaluation of bile duct disease or therapy of biliarystones (with videos). Gastrointest Endosc 2011;74:805–14.
[3] Draganov P, Chauhan S, Wagh M, Gupte A, Lin T,Hou W, et al. Diagnostic accuracy of conventional andcholangioscopy-guided sampling of indeterminate biliarylesions at the time of ERCP: a prospective, long-termfollow-up study. Gastrointest Endosc 2012;75:347–53.
[4] Kalaitzakis E, Webster G, Oppong K, Kallis Y, Vlavianos P,Huggett M, et al. Diagnostic and therapeutic utility of single-operator peroral cholangioscopy for indeterminate biliarylesions and bile duct stones. Eur J Gastroenterol Hepatol2012;24:656–64.
[5] Ramchandani M, Reddy N, Gupta R, Lakhtakia S,Tandan S, Darisetty S, et al. Role of single-operator peroralcholangioscopy in the diagnosis of indeterminate biliarylesions: a single-center, prospective study. GastrointestEndosc 2011;74:511–19.
[6] Awadallah N, Chen Y, Piraka C, AntillonM, Shah R. Is therea role for cholangioscopy in patients with primary sclerosingcholangitis. Am J Gastroenterol 2006;101:284–91.
[7] Tischendorf J, Krüger M, Trautwein C, Duckstein N,Schneider A, Manns M, et al. Cholangioscopic characteri-zation of dominant bile duct stenosis in patients with primarysclerosing cholangitis. Endoscopy 2006;38:665–9.
[8] Chapman R, Fevery J, Kalloo A, Nagorney D, Boberg K,Schneider BM, et al. Diagnosis and management of primarysclerosing cholangitis. Hepatology 2010;51:660–78.
[9] Lindberg B, Arnelo U, Bergquist A, Thörne A, Hjerpe A,Grandqvist S, et al. Diagnosis of biliary strictures inconjunction with endoscopic retrograde cholangiopancreati-cography,with special reference to patients with primarysclerosing cholangitis. Endoscopy 2002;34:909–16.
Spyglass cholangioscopy in sclerosing cholangitis 1389
Scan
d J
Gas
troe
nter
ol D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y T
ampe
re U
nive
rsity
on
12/0
8/14
For
pers
onal
use
onl
y.

[10] Halme L, Arola J, Numminen K, Krogerus L, Mäkisalo H,Färkkilä M. Biliary dysplasia in patients with primary scle-rosing cholangitis: additional value of DNA ploidity. LiverInt 2012;32:783–9.
[11] Boberg K, Jebsen P, Clausen O, Foss A, Aabakken L,Scrumpf E. Diagnostic benefit of biliary cytology in cholan-giocarcinoma in primary sclerosing cholangitis. J Hepatol2006;45:568–74.
[12] Majoie C, Reeders J, Sanders J, Huibregtse K, Jansen P.Primary sclerosing cholangitis: a modified classification ofcholangiographic findings. AJR Am J Roentgenol 1991;157:495–7.
[13] Cotton P, Lehman G, Vennes A, Geenen J, Russell L,Meyers W, et al. Endoscopic sphincterotomy omplicationsand their management: an attempt at consensus. GastrointestEndosc 1991;37:383–93.
[14] Ismail S, Kylänpää L, Mustonen H, Halttunen J,Lindström O, Jokelainen K, et al. Risk factors for complica-tions of ERCP in primary sclerosing cholangitis. Endoscopy2012;44:1133–8.
[15] SethiA,ChenY,AustinG,BrownW,BrauerB,FukamiN,etal.ERCP with cholangiopancreatoscopy may be associatedwith higher rates of complications than ERCP alone: a singlecenter experience. Gastrointest Endosc 2011;73:251–6.
1390 A. Siiki et al.
Scan
d J
Gas
troe
nter
ol D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y T
ampe
re U
nive
rsity
on
12/0
8/14
For
pers
onal
use
onl
y.

Covered Self-expanding Metal Stents May be Preferableto Plastic Stents in the Treatment of Chronic
Pancreatitis-related Biliary Strictures
A Systematic Review Comparing 2 Methods of Stent Therapyin Benign Biliary Strictures
Antti Siiki, MD,* Mika Helminen, MSc,wz Juhani Sand, MD, PhD,*and Johanna Laukkarinen, MD, PhD*
Background: Covered self-expanding metal stents (CSEMS) arebeing increasingly used in the endoscopic treatment of benignbiliary strictures (BBS). There is no solid evidence yet to supporttheir routine use.
Goals: To evaluate feasibility, success rate, and complications ofCSEMS compared with multiple plastic stents (PS) in BBS in asystematic review.
Study: A systematic search of electronic databases (Medline,Scopus, and Embase) for studies published from 2000 to 2012combined to hand-search of reference lists resulted 4977 articles.Out of 99 potentially relevant studies selected for full-text review,12 CSEMS (376 patients) and 13 PS studies (570 patients) met thefinal inclusion criteria. A systematic review comparing the 2methods was made using proportion meta-analysis.
Results: A tendency to successful use of CSEMS in stricturesrelated to chronic pancreatitis (CP) was shown: clinical success of77% and 33% [95% confidence interval (CI), 61%-94% vs. 4%-63%, P=0.06] was achieved with CSEMS and PS at 12 monthsfollow-up, respectively. There were no differences in the successrates of other etiologies except CP or in the early complications. InCSEMS, incidence of late adverse events was lower in CP-relatedstrictures (3% vs. 67%, 95% CI, 0%-13% vs. 17%-99%,P=0.02). The median number of endoscopic retrograde chol-angiopancreatographies was lower with CSEMSs: 1.5 versus 3.9(P=0.002).
Conclusions: Improved clinical success with fewer endoscopic ses-sions and corresponding complication rate may be achieved withCSEMS treatment compared with PS in BBS secondary to CP. Inother BBS etiologies, this systematic review remains inconclusive.
Key Words: endoscopy, benign biliary strictures, stents, chronic
pancreatitis, postoperative biliary stricture
(J Clin Gastroenterol 2014;48:635–643)
In the endoscopic treatment of benign biliary strictures(BBS), the use of multiple plastic stents (PS) has a widely
recognized role as a primary therapy.1–4 Relatively highstricture recurrence rate and a tendency to stent cloggingnecessitating frequent stent exchanges in PSs has generateda growing interest of use of covered self-expanding metalstents (CSEMS) in BBS.1,2,5–8 Although a single random-ized controlled trial (RCT) comparing PS and CSEMS inpostoperative strictures supports,9 as well as several recentnon-comparative studies show promising results, strongevidence justifying their routine use is limited.
BACKGROUNDThe etiology of BBS ranges from postoperative
[postorthotopic liver transplant (LT) or postchole-cystectomy] to stenosis caused by chronic pancreatitis (CP),common bile duct (CBD) stones, sclerosing cholangitis,previous endoscopic sphincterotomy, and abdominaltrauma.1,6 The optimal treatment strategy and expectedoutcome depend on stricture etiology.3 Percutaneoustranshepatic and surgical methods are associated with sig-nificant morbidity and a considerable recurrence rate.10–12
If endoscopy fails, the long-term results of operativeapproach in refractory BBS are relatively good.12,13 How-ever, surgical hepaticojejunal anastomosis makes laterendoscopic treatment challenging if restricturing of anas-tomosis occurs. Especially in CP, patient comorbiditiesand hostile conditions due to chronic inflammation maycomplicate the surgical approach.
The well-established endoscopic treatment method ofPS includes tri-monthly insertion of increasing number of10F PS across the stricture for 12 months.2,14 PS therapyhas produced good long-term results in BBS,14–17 especiallyin postcholecystectomy BBS14,17–20 and duct-to-duct anas-tomotic strictures after LT.16,21–24 Strictures secondary toCP respond least well to PS treatment25–29 because of thefibrotic nature of the strictures in calcifying CP. The maindrawbacks of PS therapy are the need for frequent endo-scopic stent exchanges, either scheduled tri-monthly orunscheduled for stent obstruction, and relatively challeng-ing insertion of multiple stents side-by-side across thestricture.6
CSEMS offer potential advantages over PS: fewerendoscopic sessions and improved patency with fewer stentocclusions due to postdeployment diameter equivalent ofthree 10F PS.1,6 Possible drawbacks include complicated
Received for publication March 25, 2013; accepted October 8, 2013.From the *Department of Gastroenterology and Alimentary Tract
Surgery, Tampere University Hospital; wScience Center, PirkanmaaHospital District; and zSchool of Health Sciences, University ofTampere, Tampere, Finland.
Supported by Sigrid Juselius Foundation, Finland and the competitiveresearch fund of Pirkanmaa Hospital District, Finland.
The authors declare that they have nothing to disclose.Reprints: Johanna Laukkarinen, MD, PhD, Tampere Pancreas Labo-
ratory, Department of Gastroenterology and Alimentary TractSurgery, Tampere University Hospital, Teiskontie 35, FIN-33521Tampere, Finland (e-mail: [email protected]).
Copyright r 2013 by Lippincott Williams & Wilkins
ORIGINAL ARTICLE
J Clin Gastroenterol � Volume 48, Number 7, August 2014 www.jcge.com | 635

removal secondary to tissue embedding or proximalmigration,30–32 cholecystitis due to occlusion of the cysticduct,33 de novo strictures after stent removal,34–36 stentmigration,8,34,37,38 postdeployment pain possibly due tostent,8,32 limited usefulness in hilar strictures,39 and insuf-ficient evidence of optimal stent design and of adequatestent indwelling time. One single study has reported a cost-analysis of stent therapy in BBS, supporting the use ofCSEMS in CP-related strictures.40 Studies on CSEMSreport promising results in postoperative strictures9,30,41–47
and in CP.8,32,37,48–52 The only RCT available up to datereported feasibility and better long-term patency ofCSEMS compared with multiple PS in 31 cases of post-operative strictures, with success rates up to 82% withCSEMS during 5 to 6 years of follow-up.9 However,because of heterogeneity of studies and relative lack ofRCTs, CSEMS use, at least as a first-line treatment, cannotyet be universally recommended in BBS.5,6
OBJECTIVESThe aim of this systematic review was to compare
the outcomes of CSEMS and PS in the endoscopic treat-ment of BBS.
METHODS
Search StrategyA literature search of the Medline and Embase and
Scopus databases was conducted for studies assessingendoscopic treatment of BBS. To perform a highly sensitivedatabase query, an information specialist with expertise onmedical search strategy was involved (Mervi Ahola ofDepartment of Health Sciences of Tampere UniversityLibrary). The query was limited to studies on adults pub-lished in English between January 1, 2000 and December31, 2012. The search was performed with the followingkeywords combined with appropriate Medical SubjectHeadings terms: “biliary stricture, stenosis or constriction,bile duct diseases, cholestasis, jaundice, chronic pan-creatitis, postoperative complications of liver trans-plantation and cholecystectomy or sclerosing cholangitis”and “endoscopy, cholangiopancreatography, or stents.”The analysis was based on published results, and no addi-tional data were obtained from any original authors.
The titles and abstracts of studies identified werescreened and the full texts of potentially relevant pub-lications were obtained. Studies on endoscopic treatment ofBBS with PS or CSEMS and with reported adequate dataabout stent type, stricture etiology, complications, andoutcome were considered to meet the inclusion criteria. Theselection process was carried out by 2 independentreviewers (A.S., J.L.). In addition, the reference lists of keystudies were hand searched to identify further relevantstudies.
Case reports, publications about percutaneous, oper-ative, or vascular approaches, intestinal stenting, malignantstrictures, pancreatic duct strictures and bile leaks, as wellas strictures treated with only balloon dilatation orsphincterotomy were excluded. Whenever it was notpossible to exclude cases with neoplasm, biliary fistula(leakage) or combined operative and percutaneous treat-ment, the entire study was excluded.
Data extracted from the selected studies included:primary author, year of publication, country of origin,
characteristics of study population (age, sex, stricture eti-ology, previous treatment), study design, number ofpatients, technical success, complications related to stentinsertion and removal, complications and other adverseevents (such as stent migration) in the follow-up, durationof stent therapy, and clinical success at stent removal, after6 and 12 months and at the end of follow-up. Complica-tions were divided to early [related to stent insertion andpost–endoscopic retrograde cholangiopancreatography(ERCP) period of 30 d] and late (during the follow-up untilstent removal).
DefinitionsBBS: It is a nonmalignant stricture of CBD. Multiple
PS: It is a treatment strategy of tri-monthly plastic stentexchange with insertion of a gradually increasing number ofPS across the stricture and an eventual stent removal at12 months.18,20–24,26,29,53–57 CSEMS: It is used in BBStreatment with a partially or fully (FCSEMS) coveredself-expandable metal stent with eventual stentremoval30,37,41,46–48,50,51,58–60 or exchange of FCSEMSevery 2 months32 until removal. Clinical success: It isdefined as a successful clinical stricture resolution at a giventime point without unscheduled interventions or a changeof treatment strategy. Complications: ERCP-related or stentexchange–related complications, such as pancreatitis,cholangitis, hemorrhage, perforation, and postinsertionpain, requiring hospital admission (Figs. 2A, B, procedure-related) as well as other adverse events like infections, stentmigration, or stent occlusion in the follow-up period(Figs. 2A , B, other adverse events). Complications weredefined as early, when they occurred during the first 30 daysfrom initial stent insertion. Follow-up: The data on treat-ment success was collected at one or more time points; atstent removal, at 6 and 12 months, and at the end of follow-up.
Outcome MeasuresThe primary outcome was sustained clinical success
defined as stricture resolution without unscheduled endo-scopic interventions or treatment failure during follow-up.Secondary outcome parameters were technical success rateand complications.
Study QualityThe review consisted of 9 retrospective and 16 pro-
spective studies. No controlled studies comparing plasticand CSEMS treatment could be included. As the quality ofthe included studies was assessed using the Newcastle-Ottawa scale (NOS),61 all 25 studies received 4 or 5 in theclassifications of maximum 9 points.
Statistical AnalysisAs controlled studies were unavailable, a systematic
review was made by means of proportion meta-analysis.Statistical analysis of the review comparing the 2 methodswas performed using metaprop function in meta packagefor R (Software environment for statistical computing andgraphics, version 2.13.0, The R Foundation for StatisticalComputing). Arcsine transformation was applied for com-parisons where either of the groups (CSEMS or PS)contained at least one study with a proportion of 100%,otherwise untransformed proportions were used. Using theproportion estimates and confidence intervals obtainedfrom the systematic review, the statistical significances for
Siiki et al J Clin Gastroenterol � Volume 48, Number 7, August 2014
636 | www.jcge.com r 2013 Lippincott Williams & Wilkins

the differences between CSEMS and PS groups were eval-uated using the unpaired, 2-tailed Student t test, and anassociation was considered significant when the exact sig-nificance level of the test was P<0.05.
RESULTS
Selected StudiesThe search retrieved 99 studies of possible relevance. A
flowchart of the search strategy is presented in Figure 1.Twenty-five studies met the final inclusion criteria for
the review: 13 studies on multiple PS18,20–24,26,29,53–57 and 12studies on CSEMS30,32,37,41,46–51,58–60 (Table 1). The qualityassessment provided relatively low NOS scores in allselected studies, mainly because of lack of control groupsand also for the length of follow-up that may have been tooshort for outcomes, for example, treatment failure to occur.
The most of the excluded studies reported othertreatment modalities than those to be addressed in thisreview (eg, single PS or unremoved or uncovered SEMS),or included cases with biliary fistulas, or provided insuffi-cient data on follow-up or complications. To produceresults as valid and as clinically generalizable as possible,several otherwise excellent studies, among them 11 studies
of CSEMS,8,9,34,36,38,42–45,49,61 were excluded from theanalysis because of data that were noncomparable withother articles in terms of study end-points.
In the excluded CSEMS studies, the results weremainly in line with the included studies. A better long-termpatency of CSEMS in postoperative strictures comparedwith PS has been proposed.9 In cohort studies of widevariety of benign biliary conditions, including fistulas andrefractory strictures, the clinical success of CSEMS therapyhas been 70% to 100%8,45,49,61 with migrations occurring in9% to 10%8,45 and secondary strictures or relapses in 13%to 18%.36,61 A recent multicenter study showed strictureresolution rate at stent removal of up to 81% in CP com-pared with 92% in postsurgical strictures.8 In treatment ofpostorthotopic liver transplantation complications,CSEMS success rate has reportedly been up to 61% to95%8,34,38,43 with 14% to 31% of migrations.8,41
Patient CharacteristicsOf the 25 studies, a total of 946 patients were included
in the review: 376 underwent treatment with CSEMS and570 with multiple PS. The summary of study characteristicsand patient demographics is presented in Table 1. Thegroups were well comparable for age and sex. Mean age
FIGURE 1. Search strategy for systematic review.CSEMS indicates covered self-expanding metal stents.
J Clin Gastroenterol � Volume 48, Number 7, August 2014 CSEMS in the Treatment of Biliary Strictures
r 2013 Lippincott Williams & Wilkins www.jcge.com | 637

TA
BLE
1.
Stu
dy
Ch
ara
cterist
ics,
Patien
tD
em
og
rap
hic
s,C
ase
Num
bers
inD
iffe
ren
tStr
ictu
reEtiolo
gie
s,Le
ng
thof
Follo
w-u
p,
an
dC
linic
alSucc
ess
Rate
Age(M
ean)
Sex
Patients
Follow-up(M
ean)
Successrate
(%)
References
Group
Stent
Design
NOS
Country
(y)
(Male
%)
All
CP
OLT
Other
(mo)
Rem
oval(StentRem
oval)
12mo*
Tabibianet
al21
PS
Plastic
R4
USA
52.5w
65.2
69
069
011
94.2
92.8
Sakaiet
al18
PS
Plastic
R5
Japan
58.9
78.8
33
13
020
100.7
57.6
57.6
Kulaksizet
al22
PS
Plastic
P4
Germany
52.8
73.3
15
015
016.8
73.3
73.3
Holtet
al24
PS
Plastic
P5
UK
48.5
39.6
53
053
018
71.7
69.8
DeR
euver
etal53
PS
Plastic
R5
NL
49
28.2
110
00
110
91.2
73.6
73.6
Pashaet
al23
PS
Plastic
R5
USA
46.7
80
25
025
021.5
100
81.8
Kuzela
etal20
PS
Plastic
P4
SlovakRep
50.4
90
43
00
43
16
100
100
Pozsar5
4PS
Plastic
P5
Hungary
61.3
10
20
00
20
14.5
100
95
Pozsaret
al29
PS
Plastic
R5
Hungary
50.8
72.4
29
29
00
12.9
62.1
62.1
Morelliet
al55
PS
Plastic
R5
USA
48
64
25
025
054
95.7
95.7
DeP
alm
aet
al56
PS
Plastic
R5
Italy
46
22.5
80
00
80
70.8
68.6
61.4
Dragonovet
al26
PS
Plastic
R5
USA
51.4
55.2
29
93
16
48
93.1
69
Eickhoffet
al57
PS
Plastic
R5
Germany
54.7
82.1
39
39
00
58
46.2
30.8
Perriet
al51
CSEMS
Niti-S
P5
Italy
52
94
17
17
00
24
70.5
64.7
Tarantinoet
al46
CSEMS
Niti-S-C
omVi
P5
Italy
57
65
62
438
20
15.9
90.3
87.0
Poleyet
al32
CSEMS
Hanaro
P5
NL
57
52.2
23
13
010
15
65.2
65.2
Tarantinoet
al58
CSEMS
Niti-S-C
omvi
P5
Italy
59.1
66.7
15
015
014.4
100
46.7
Moonet
al41
CSEMS
Bonastent
P5
Korea
61.7
61.9
21
63
12
13.8
95.2
95.2
Huet
al47
CSEMS
MicroTech
P5
China
51.2
76.9
13
013
012.1
92.3
92.3
Park
J59
CSEMS
S&G
Biotech
P5
Korea
69
58.8
17
10
07
15
70.6
70.6
Park
etal60
CSEMS
MITech/Std
ST
P4
Korea
61.5
53.5
43
11
230
490.7
83.7
Chaputet
al29
CSEMSz
Wallstent
P5
France
49.7
81.8
22
022
012
86.4
45.5
Mahajanet
al50
CSEMS
Viabil
P4
USA
53.5w
63.6
44
19
916
3.8
82.9
82.9
Behm
etal48
CSEMSz
Wallstent
P5
USA
51
90
20
20
00
22
95
90
Kahalehet
al37
CSEMSz
Wallstent
P4
USA
55
68.4
79
32
16
31
12
91.1
87.3
*Follow-up:at12moorattheendofshorter
follow-up.
wMedianvalues.
zPartiallycovered.
CPindicateschronic
pancreatitis;CSEMS,covered
self-expandingmetalstents;NOS,New
castle-O
ttawaScale
(range1-9);OLT,orthotopic
liver
transplantation;Other,postcholecystectomy,other
postoperative,
bileduct
stone,
trauma,sphincterotomystricture,other;P,prospective;
R,retrospective.
Siiki et al J Clin Gastroenterol � Volume 48, Number 7, August 2014
638 | www.jcge.com r 2013 Lippincott Williams & Wilkins

was 57 years in the CSEMS group and 51 years in the PSgroup (P=0.06). There were 67% men in the CSEMSgroup and 55% in the PS group (P=0.5). The frequency ofprevious endoscopic treatment attempts was reported in8 studies30,32,41,46,48,51,59 in the CSEMS group and in 1 PSstudy.53
Stricture EtiologyFive CSEMS studies30,47,48,51,58 reported the results of
single stricture etiology and 7 studies32,37,41,46,50,59,60 ofmultiple stricture etiologies. Eleven PS studies20–24,29,53–57
were on single stricture etiology and 2 studies18,26 on mul-tiple stricture etiologies.
Case numbers of different stricture etiologies are pre-sented in Table 1. To assess the outcome, 3 groups wereformed: CP, post–liver transplantation (LT), and otherstrictures (OS). The etiology-specific data of outcome wasavailable from most of the studies. In few studies, it wasonly possible to pull out data that presented the majority ofthe study population, and these studies were groupedaccording to this majority etiology. In strictures related topostcholecystectomy or bile duct stones, case numbers wereinsufficient for subgroup analysis. Therefore, all stricturesexcept CP and liver transplant were combined into a singlegroup (OS) for etiological outcome analysis. Case numbersin the etiology groups were as follows: CP, 128 CSEMS and90 PS; LT, 118 CSEMS and 190 PS; and other etiologies,130 CSEMS and 290 PS.
Stent DesignThere were slight differences in CSEMS stent designs,
the trademarks and types of which are presented in Table 1.The populations of the studies by Park et al60 and Perriet al51 comparing stents with and without anchoring finswere pooled for analysis. All 13 PS studies had comparableendoscopic technique with a gradually increasing numberof polyethylene PS inserted and exchanged at tri-monthlyintervals up to 12 months. Three of the CSEMSstudies30,37,48 used partially covered stents and932,41,46,47,50,51,58–60 used fully covered stents.
Technical Success and Stent Indwelling TimeTechnical success of primary stent insertion was sim-
ilar in the study groups: 100% in CSEMS and 98% in PS(P=0.8). The median duration of stent therapy wasshorter in the CSEMS (4.5mo) than in the PS group(11mo) (P=0.001). Significantly fewer ERCP sessionswere required in the CSEMS group than in the PS group(median 1.5 and 3.9, P=0.002). When cases of CP wereanalyzed separately, neither duration of stent therapy(median 4.8 vs. 16mo, P=0.1) nor number of ERCPs (2.0vs. 4.2, P=1.0) were statistically different between CSEMSand PSs. Stent removal was equally successful in CSEMSand PS groups, respectively (99.8% and 100% of cases;P=0.8).
Follow-upIn 83% of CSEMS studies and 100% of PS studies,
adequate data at 12 months of follow-up were obtained andwere used in the final analysis (Table 1). In two CSEMSstudies,50,60 the mean follow-up time was <6 months. Theresults at the end of the total follow-up time were notcomparable, as the length of follow-up was shorter in theCSEMS group (14 vs. 49mo, P=0.003).
ComplicationsThere was no difference in the early complications
(pancreatitis, cholangitis, perforation, hemorrhage)between the CSEMS and PS groups [13% vs. 14%, 95%confidence interval (CI), 7%-19% vs. 8.1%-19%, P=0.9)in all stricture etiologies. However, late complications orany adverse events (pain, infection, stent occlusion andstent migration) occurred less often in CSEMS than in PS(4.6% vs. 14%, P=0.006) when all etiologies were com-bined (95% CI, 2%-7% and 9%-19%, respectively)(Figs. 2A, B). The complication figures according to treat-ment group and stricture etiology are presented in Figures2A and B; there were less late complications in the CSEMSgroup (3% vs. 67%) than in the PS group in CP etiology(95% CI, 0%-13% vs. 17%-99%, P=0.02). No statisticaldifference in complication figures of other etiology groupswas found (P=0.06-0.9). Severity grade of complicationswas not systematically reported in the studies.
Clinical SuccessIn CP strictures, there was tendency to better clinical
success in CSEMS treatment at 12 months after stentremoval: 77% versus 33% (95% CI, 61%-94% vs. 4%-63%, P=0.06) in CSEMS and PS, respectively. In othertime points of follow-up, the difference was also observable:at stent removal, 80% versus 38% (95% CI, 62%-93% vs.12%-68%, P=0.02) and at 6 months, 74% versus 33%(61%-86% vs. 4%-63%, P=0.02); however, the P-valuesmight not be reliable because of the small numbers ofstudies in comparisons. In other etiologies except CP therewas no difference (P=0.08-0.9) in the success rate. Theoverall clinical success of CSEMS and PS in all etiologies atstent removal was 87% versus 85% (P=0.8) and at 12months 79% versus 77% (P=0.9). Clinical successaccording to stricture etiology is presented in Figures 3A–Cat the end of the stent therapy and at 6 and 12 months afterstent removal.
DISCUSSIONBesides PS, CSEMS are today widely used in the
endoscopic treatment of BBS. However, there is only onesingle RCT on the subject comparing CSEMS to PS inpostoperative strictures.9 Present systematic review ofstudies published in the 2000s sheds light on the con-troversial issue about the decision between these treatmentmodalities. CSEMS seemed to be a more effective and safetreatment method in strictures caused by CP. In otherstricture etiologies, such as LT, no difference between the 2methods was found.
Treatment of BBS with multiple PS has been consid-ered to be a relatively safe method with few complica-tions.14 The review by VanBoeckel et al suggested thatmultiple PS treatment was safer than single plastic stent oruncovered SEMS.4 In the postoperative series by Cos-tamagna et al,14 the early complication rate was 9% anddistal displacement occurred in 11% of cases. In the treat-ment of CP, the rate of acute pancreatitis has been up to3.4% to 5.0%,18,26 the rate of cholangitis up to 7%,26 andthe rate of stent migration up to 2.5% to 9%.27,57 In PStherapy, frequent stent exchange and stent clogging seem tobe the major drawbacks, truly complicated cases beingmerely occasional and with mild clinical consequences.
The clinical success of multiple plastic stent treatmenthas been shown to be superior to single plastic stent
J Clin Gastroenterol � Volume 48, Number 7, August 2014 CSEMS in the Treatment of Biliary Strictures
r 2013 Lippincott Williams & Wilkins www.jcge.com | 639

treatment in BBS.4,27 The use of a single PS may be seen asa “bridge to decision” in newly diagnosed cases and inindeterminate strictures.2,51 Treatment with multiple PS hasbeen feasible in postcholecystectomy strictures, with asuccess rate of 70% to 90%14,15,17,19,26,53–56 and with 14%stent clogging and up to 33% pain after simultaneousinsertion of multiple PS.53 In post-LT anastomotic stric-tures, the reported success rate has been 69% to 91% inmultiple PS.16,21–24 However, in CP, the results of PStherapy have been mostly disappointing; success rates aslow as 24% to 38% in median follow-up of 45 months25
and treatment failure rate of up to 83% in follow-up of 48months26 have been reported. In contrast, in the study byCatalano et al,27 the prognosis was better with the insertionof up to 5 simultaneous PS; only 8% failure rate in follow-up of 3.9 years was reported. The presence of calcificationsin the pancreatic head secondary to CP is related to pooreroutcome with PS therapy, probably due to the fibroticnature of the strictures.25,27,28,51 Temporary biliaryobstruction due to acute pancreatic inflammation is asso-ciated to success rate of up to 92% in PS.25
In CSEMS, complications such as cholangitis, pan-creatitis, and cholecystitis occur at the rate of about14%37,50 and stent migrations at the rate of 5%37 to 10%8
to up to 38%38 with wide variation in their clinical con-sequences. The difference in migration rate may reflect thevariation stent indwelling time and in the CSEMS design;fully covered stents with or without anchoring fins, stentswith different coating materials, and partially covered stentswith uncovered ends have been used. It is logical to assumethat the fully covered stents may be more prone to migra-tion but less problematic to remove than the partiallycovered ones. However, these stent designs are yet to becompared in clinical study and also our material provedinadequate to reliably assess the difference. The optimalduration of CSEMS therapy allowing safe removal andstricture resolution remains unknown. As the presentstudies report results after 2 to 6 months of stent indwelling,the recent multicenter study of Kahaleh et al8 usingCSEMS with anchoring fins proposed that the stentindwelling time of >90 days was associated with increasedlikelihood of stricture resolution at stent removal. The
FIGURE 2. Early (A) and late (B) complications and other adverse events after stricture treatment with covered self-expanding metalstents (CSEMS) or plastic stents (PS). By etiology, complications include chronic pancreatitis (CP), post–liver transplant (LT), and otheretiologies (Other). Procedure-related complications include pancreatitis, cholangitis, perforation, and hemorrhage. Other adverseevents include pain, infection, stent occlusion, and stent migration. *P < 0.05.
FIGURE 3. Success rate of covered self-expanding metal stents (CSEMS) and plastic stents (PS) in strictures with different etiologies: (A)chronic pancreatitis (CP), (B) post–liver transplant (LT), and (C) other etiologies (other). *P < 0.05.
Siiki et al J Clin Gastroenterol � Volume 48, Number 7, August 2014
640 | www.jcge.com r 2013 Lippincott Williams & Wilkins

forceful radial expansion of CSEMS is likely to cause somediscomfort immediately after stent insertion: Poley et al32
reported transient abdominal pain in up to 56% of casesafter stent insertion, only a few cases resulting in admis-sion.8 The clinical significance of de novo strictures occa-sionally associated with CSEMS in a few recent stud-ies,34–36 remains a subject for further research.
Our study showed that CSEMS treatment was at leastas safe as PS in terms of complication rate, both in all casesand in the etiological subgroup analyses. The tendency toslightly higher prevalence of late adverse events in PS canbe explained by the high frequency of late stent clogging, aknown problem of multiple PS therapy. The postinsertionalpain, a complication typical of CSEMS and presumablyactively reported in first pilot studies, seems to cause aremarkable part of CSEMS early complications. Althoughinfrequent, clinically significant proximal migrations andproblems with removal of CSEMS should be considered asa potential and serious risk of CSEMS therapy. If endo-scopic removal fails, surgical operation may be inevitable.
Previous results with CSEMS have been encouragingin BBS.8,37,41,45,47,48,50 Long-term success rates range from53%30 to 96% to 100%34,42,43,46,47 in postorthotopic livertransplantation strictures. In strictures secondary to post-endoscopic sphincterotomy, a resolution rate of 90% at14.5-month follow-up has been achieved.54 The studies byMahajan et al50 and Moon et al41 with FCSEMS havereported treatment success rates of 83% to 95% on follow-up of 3.8 to 13.8 months in populations with a variety ofstricture etiologies including postoperative and CP cases.Similar promising outcomes were reported by Kahalehet al37 and Park et al60 in studies including multiple etiol-ogies, as well as in studies of Tarantino et al46 andMangiavillano et al49 with FCSEMS at 1 year of follow-up.The long-term resolution rate with FCSEMS, solely in CP-related strictures, has been around 66%.31 In the recentstudy of Perri et al,51 the 2-year treatment success ofFCSEMS in CP was 47%, with most of the failures causedby migrations of unflared-end stents used in the beginningof the study. In contrast, the success rate with FCSEMS onfollow-up of 15 months has been 80% for all patients butonly 46% for patients with CP.32 The fibrotic stricturessecondary to CP appear the most difficult to treat effectivelyin the long term, irrespective of the type of stent. Achievingnecessary dilatation and stricture remodeling effect14,27,31,53
with fewer endoscopic interventions compared with anincreasing number of PS appear the main benefits ofCSEMS therapy.
The only study up to date directly comparing PS toCSEMS by Artifon et al9 of 15 patients managed withmultiple PS and 16 cases treated with CSEMS, proposedfeasibility and safety of FCSEMS use in postoperativestrictures with clinical success in 5-year follow-up of 82%and 72% in FCSEMS and multiple PS, respectively.
Present study proposes a better success rate of CSEMStreatment in strictures secondary to CP: the success ratedefined as resolution without unscheduled reinterventionswas 77% with CSEMS compared with 33% in the PS groupat 12 month after stent removal. Parallel results at stentremoval and after 6 months seem to support this finding inCP. The results may reflect better dilating force of CSEMSthan PS treatment in strictures secondary to calcifying CP.However, this review did not find any difference betweenthe 2 treatment methods in other BBS etiologies, such aspostoperative, CBD stone or postsphincterotomy-related
biliary strictures. This is explained by heterogeneity and thesmall number of studies, making it difficult to prove anydifference significant. Although the unit cost of CSEMSstent is 10 times as high as that of PS, the number ofendoscopic interventions to produce equivalent clinicaleffect is considerably less in CSEMS therapy. This is con-sistent with the reported cost-effectiveness of CSEMStherapy in strictures secondary to CP.40
The strength of this systematic review was a metic-ulous literature search to include all relevant articles and acareful selection process to pick out studies with com-parable data. However, the lack of RCTs weakens thesystematic review. The definition of success rate differedslightly between studies and in some papers comparablesuccess rates needed to be deduced from the data presented.Several studies on postoperative strictures had to beexcluded as fistula-free data was not provided; evaluatingthe outcome of strictures with biliary fistulas was consid-ered noncomparable with pure biliary strictures. The onlyRCT of postoperative strictures had to be omitted becauseof inadequate follow-up data. The most important draw-backs of the studies included are the short follow-up ofCSEMS studies, insufficient data on previous unsuccessfultreatment, and often-unknown prevalence of calcifyingpancreatitis. In most of CSEMS studies (72%), a previouslyfailed treatment attempt with PS had been made. A pre-vious treatment attempt with PS may be associated withinferior resolution rate with subsequent CSEMS treat-ment.8 As studies on CP did not systematically report theprevalence of calcifying pancreatitis, it remains unknownwhether the strictures of CSEMS and PS groups are trulycomparable in CP.
According to earlier studies with PS, an optimal fol-low-up time would be 12 to 24 months after stent removal,by which time most restrictures appear.14,17,25,26,53,56 Whensuccessful endoscopic outcome is not achieved within 12months, surgical treatment of CP-related stricture shouldbe considered.25 As the number of CSEMS studies is lowand some of them report follow-up of <12 months, theresults of long-term stricture patency have to be interpretedwith caution until more trials with longer follow-up times.Whether CSEMS therapy actually prevents, or merelydelays the need for definitive surgical treatment in unre-sponsive cases of CP strictures remains unknown. Furtherstudies with a clear definition of complications, treatmentsuccess, and follow-up of at least 12 to 24 months arerecommended to compare CSEMS with PS.
In conclusion, this systematic review of the treatmentof BBS demonstrates a better success rate with an equiv-alent complication rate for CSEMS compared with PSwhen the BBS is caused by CP. With regard to other BBSetiologies, this systematic review remains inconclusive. Arandomized, controlled trial comparing CSEMS and PS inthe treatment of different BBSs is warranted: not only tostudy stricture resolution and treatment-associated com-plications but also to clarify indications and optimal stentdesign.
REFERENCES
1. Chan C, Telford J. Endoscopic management of benign biliarystrictures. Gastrointest Endosc N Am. 2012;22:511–537.
2. Dumonceau JM, Triangali A, Blero D, et al. Biliary stenting:indications, choice of stents and results: European Society ofGastrointestinal Endoscopy (ESGE) clinical guideline. Endo-scopy. 2012;44:277–298.
J Clin Gastroenterol � Volume 48, Number 7, August 2014 CSEMS in the Treatment of Biliary Strictures
r 2013 Lippincott Williams & Wilkins www.jcge.com | 641

3. Perri. V, Familiari P, Triangali A, et al. Plastic biliary stents forbenign biliary diseases. Gastrointest Endosc Clin N Am.2011;21:405–433.
4. vanBoeckel P, Vleggaar F, Siersema P. Plastic or metal stentsfor benign extrahepatic biliary strictures: a systematic review.BMC Gastroenterol. 2009;9:96–101.
5. Bakhru M, Kahaleh M. Expandable metal stents for benignbiliary disease. Gastrointest Endosc Clin N Am. 2011;21:447–462.
6. Baron TH. Covered self-expandable metal stents for benignbiliary tract diseases. Curr Opin Gastroenterol. 2011;27:262–267.
7. Siriwardana HP, Siriwardana AK. A systematic appraisal ofthe role of metallic endobiliary stents in the treatment ofbenign bile duct stricture. Ann Surg. 2005;242:10–19.
8. Kahaleh M, Brijbassie A, Sethi A, et al. Multicenter trialevaluating the use of covered self-expanding metal stents inbenign biliary strictures: time to revisit our therapeuticoptions? J Clin Gastroenterol. 2013;47:695–699.
9. Artifon E, Coelho F, Frazao M, et al. A prospectiverandomized study comparing partially covered metal stentversus plastic multistent in the endoscopic management ofpatients with postoperative benign bile duct strictures: afollow-up above 5 years. Rev Gastroenterol. Peru.2012;32:26–31.
10. Laasch HU, Martin DU. Management of benign biliarystrictures. Cardiovasc Intervent Radiol. 2002;25:457–466.
11. DePalma G, Persico G, Sottile R, et al. Surgery or endoscopyfor treatment of postcholecystectomy bile duct strictures. Am JSurg. 2003;185:532–535.
12. Lillemoe K, Melton G, Cameron J, et al. Postoperative bileduct strictures: management and outcome in the 1990s. AnnSurg. 2000;232:430–441.
13. Nealon W, Urrutia F. Long-term follow-up after bilioentericanastomosis for benign bile duct stricture. Ann Surg.1996;6:639–648.
14. Costamagna G, Pandolfi M, Mutignani M, et al. Long-termresults of endoscopic management of postoperative bile ductstrictures with increasing number of stents. GastrointestEndosc. 2001;54:162–168.
15. Kassab C, Prat F, Ligoury C, et al. Endoscopic management ofpost-laparoscopic cholecystectomy biliary strictures. Long-term multicentre study. Gastroenterol Clin Biol. 2006;30:124–129.
16. Graziadei I, Schwaighofer H, Koch R, et al. Long-termoutcome of endoscopic treatment of biliary strictures after livertransplantation. Liver Transpl. 2006;12:718–725.
17. Kuroda Y, Tsuyuguchi T, Sakai Y, et al. Long-term follow-upevaluation for more than 10 years after endoscopic treatmentfor postoperative bile duct strictures. Surg Endosc.2010;24:834–840.
18. Sakai Y, Tsuyuguchi T, Ishihara T, et al. Long-term prognosisof patients with endoscopically treated postoperative bile ductstricture and bile duct stricture due to chronic pancreatitis. JGastroenterol Hepatol. 2009;24:1191–1197.
19. Tuvignon N, Ligoury C, Ponchon T, et al. Long-term follow-up after biliary stent placement for postcholecystectomy bileduct strictures. Endoscopy. 2011;43:208–216.
20. Kuzela L, Oltman M, Sutka J, et al. Prospective follow up ofpatients with bile duct strictures secondary to laparoscopiccholecystectomy, treated endscopically with multiple stents.Hepatogastroenterology. 2005;52:1357–1361.
21. Tabibian J, Asham E, Han S, et al. Endoscopic treatment ofpost-orthotopic liver transplantation anastomotic biliary stric-tures with maximal stent therapy. Gastrointest Endosc.2010;71:505–512.
22. Kulaksiz H, Weiss K, Gotthard D, et al. Is stenting necessaryafter balloon dilatation of post-transplantation biliary stric-tures? Results of a prospective comparative study. Endoscopy.2008;40:746–751.
23. Pasha S, Harrison E, Das A, et al. Endoscopic treatment ofanastomotic biliary strictures after deceased donor liver
transplantation: outcomes after maximal stent therapy. Gastro-intest Endosc. 2007;66:44–51.
24. Holt A, Thorburn D, Muirza D, et al. A prospective study ofstandardized nonsurgical therapy in the management of biliaryanastomotic strictures complicating liver transplantation.Transplant. 2007;84:857–863.
25. Cahen D, vanBerkel AM, Oskam D, et al. Long-term results ofendoscopic drainage of common bile duct strictures in chronicpancreatitis. Eur J Gastroenterol Hepatol. 2005;17:103–108.
26. Draganov P, Hoffman B, Cotton P, et al. Long term outcomein patients with benign biliary strictures treated endoscopicallywith multiple stents. Gastrointest Endosc. 2002;55:680–686.
27. Catalano M, Lindeer J, George S, et al. Treatment ofsymptomatic distal common bile duct stenosis secondary tochronic pancreatitis: comparison of single vs multiple plasticstents. Gastrointest Endosc. 2004;60:945–952.
28. Kahl S, Zimmerman S, Genz I, et al. Risk factors for failure ofendoscopic stenting of biliary strictures in chronic pancreatitis:a prospective follow-up study. Am J Gastroenterol.2003;11:2448–2453.
29. Potzar J, Sahin P, Laszlo F, et al. Medium-term results ofendoscopic treatment of common bile duct strictures in chroniccalcifying pancreatitis with increasing number of stents. J ClinGastroenterol. 2004;38:118–123.
30. Chaput U, Scatton O, Bichard P, et al. Temporary placementof partially covered self-expandable metal stents for anasto-motic biliary strictures after liver transplantation: a prospectivemulticentre study. Gastrointest Endosc. 2010;72:1167–1174.
31. Cahen D, Rauws E, Gouma D, et al. Removable full-coveredself-expandable metal stents in the treatment of common bileduct strictures due to chronic pancreatitis: a case series.Endoscopy. 2008;40:697–700.
32. Poley JW, Cahen D, Metselar H, et al. A prospective groupsequential study evaluating a new type of fully covered self-expandable metal stent for the treatment of benign biliarystrictures. Gastrointest Endosc. 2012;75:783–789.
33. Ho H, Mahajan A, Gosain S. Management of complicationsassociated with partially covered biliary metal stents. Dig DisSci. 2010;55:516–522.
34. Sauer P, Chahod F, Gorrhard D, et al. Temporary placementof fully covered self-expandable metal stents in biliarycomplications after liver transplantation. Endoscopy.2012;44:536–538.
35. Phillips M, Bonatti H, Sauer B, et al. Elevated stricture ratefollowing the use of fully covered self-expandable metal stentsfor biliary leaks following liver transplantation. Endoscopy.2011;43:512–517.
36. Kasher J, Corasanti J, Tarnasky P, et al. A multicentre analysisof safety and outcome of removal of a fully covered self-expandable metals stent during ERCP. Gastrointest Endosc.2011;73:1292–1297.
37. Kahaleh M, Behm B, Clarke B, et al. Temporary placementof covered self-expandable metal stents in benign biliarystrictures: a new paradigm? Gastrointest Endosc. 2008;67:446–454.
38. Traina M, Tarantino I, Barresi L, et al. Efficacy and safety offully covered self-expanding metallic stents in biliary compli-cations after liver transplantation: a preliminary study. LiverTranspl. 2009;12:1493–1498.
39. Larghi A, Triangali A, Lecca P, et al. Management of hilarbiliary strictures. Am J Gastroenterol. 2008;103:458–473.
40. Behm B, Brock A, Clarke B, et al. Cost analysis of temporarilyplaced covered self expandable metallic stents versus plasticstents in biliary strictures related to chronic pancreatitis.Gastrointest Endosc. 2007;5:AB211. (Abstract).
41. Moon J, Choi H, Koo H, et al. Feasibility of placing amodified fully covered self-expandable metal stent above thepapilla to minimize stent-induced bile duct injury in patientswith refractory biliary strictures. Gastroint Endosc.2012;75:1080–1085.
42. Haapamaki C, Udd M, Halttunen J, et al. Endoscopictreatment of anastomotic biliary complications after liver
Siiki et al J Clin Gastroenterol � Volume 48, Number 7, August 2014
642 | www.jcge.com r 2013 Lippincott Williams & Wilkins

transplantation using removable covered self-expandablemetallic stents. Scand J Gastroenterol. 2012;47:116–121.
43. Garcia-Pajares F, Sanchez-Antolin G, Pelayo S, et al. Coveredmetal stents for treatment of biliary complications after orthotopicliver transplantation. Transplant Proc. 2010;42:2966–2969.
44. Marin-Gomez L, Sobrino-Rodriguez S, Alamo-Martines J,et al. Use of fully covered self-expandable stent in biliarycomplications after liver transplantation: a case series. Trans-plant Proc. 2010;42:2975–2977.
45. Garcia-Cano J, Taberna-Arana L, Jimeno-Ayllon C, et al. Useof fully covered metal stents for the management of benignbiliary conditions. Rev Esp Enferm Dig. 2009;102:526–532.
46. Tarantino I, Mangiovillano B, Mitri R, et al. Fully coveredself-expandable metallic stents in benign biliary strictures: amulticenter study on efficacy and safety. Endoscopy.2012;44:923–927.
47. Hu B, Gao D, Yu F, et al. Endsocopic stenting for post-transplantbiliary stricture: usefulness of a novel removable coveredmetal stent. J Hepatobiliary Pancreat Sci. 2011;18:640–645.
48. Behm B, Brock A, Clarke B, et al. Partially covered self-expandable metallic stents for benign biliary strictures due tochronic pancreatitis. Endoscopy. 2009;41:547–551.
49. Mangiavillano B, Luigian C, Viaggi P, et al. Coveredremovable self-expandable metal stents for the treatment ofrefractory benign biliary disease. J Dig Dis. 2012;13:486–490.
50. Mahajan A, Ho H, Sauer B, et al. Temporary placement of fullycovered self-expandable metal stents in benign biliary strictures:midterm evaluation. Gastrointest Endosc. 2009;70:303–309.
51. Perri V, Boskoski I, Triangali A, et al. Fully covered self-expandable metal stents in biliary strictures caused by chronicpancreatitis not responding to plastic stenting: a prospectivestudy with 2 years of follow-up. Gastrointest Endosc.2012;6:1271–1277.
52. Cantu P, Hookey LC, Morales A, et al. The treatment ofpatients with symptomatic common bile duct stenosis secon-dary to chronic pancreatitis using partially covered metalstents: a pilot study. Endoscopy. 2005;37:735–739.
53. DeReuver P, Rauws E, Vermeulen M, et al. Endoscopictreatment of post surgical bile duct injuries: long term outcomeand predictors of success. Gut. 2007;56:1599–1605.
54. Pozsar J, Sahin P, Laszlo F, et al. Endoscopic treatment ofsphincterotomy-associated distal common bile duct stricturesby using sequential insertion of multiple plastic stents. Gastro-intest Endosc. 2005;62:85–91.
55. Morelli J, Mulcachy H, Willner I, et al. Long-term outcomesfor patients with post-liver transplant anastomotic biliarystrictures treated by endoscopic stent placement. GastrointestEndosc. 2003;58:374–379.
56. DePalma G, Gallaro G, Romano G, et al. Long-term follow-up after endoscopic biliary stent placement for bile ductstrictures from laparoscopic cholecystectomy. Hepatogastroen-terology. 2003;50:1229–1231.
57. Eickhoff A, Jakobs R, Leonhardt A, et al. Endsocopic stentingfor common bile duct stenosis in chronic pancreatitis: resultand impact on long term outcome. Eur J Gasroenterol Hepatol.2001;13:1161–1167.
58. Tarantino I, Traina M, Barresi L, et al. Fully covered metalstents in biliary stenosis after orthotopic liver transplantation.Endoscopy. 2012;44:246–250.
59. Park JK, Moon J, Choi H, et al. Anchoring of a fully coveredself-expandable metal stent with a 5F double-pigtail plasticstent to prevent migration in the management of benign biliarystrictures. Am J Gastroenterol. 2011;106:1761–1765.
60. Park DH, Lee S, Lee T, et al. Anchoring flap versus flaredend fully covered self-expandable metals tents to preventmigration in patients with biliary strictures: a multicentreprospective comparative pilot study. Gastrointest Endosc. 2011;73:64–70.
61. Wells GA, Shea B, O’Connell D, et al. The Newcastle–OttawaScale (NOS) for Assessing The Quality of Non-RandomisedStudies in Meta-Analyses. 3rd Symposium on SystematicReviews: Beyond The Basics. Improving Quality And Impact.Oxford, UK; 2000. Available at: www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
J Clin Gastroenterol � Volume 48, Number 7, August 2014 CSEMS in the Treatment of Biliary Strictures
r 2013 Lippincott Williams & Wilkins www.jcge.com | 643

1
Biodegradable biliary stents have a different effect than covered metal stents on the expression
of proteins associated with tissue healing in benign biliary strictures
Antti Siiki1, Ralf Jesenofsky2, Matthias Löhr3, Isto Nordback1, Minna Kellomäki4, Heidi Gröhn5, Joonas
Mikkonen4, Juhani Sand1, Johanna Laukkarinen1
1Dept. of Gastroenterology and Alimentary Tract Surgery, Tampere University Hospital, Tampere,
Finland 2Dept. of Medicine II, University of Heidelberg, Mannheim, Germany 3Gastrocentrum, Karolinska University Hospital, Huddinge, Sweden 4Biomaterials and Tissue Engineering Group, BioMediTech and Department of Electronics and
Communications Engineering, Tampere University of Technology, Tampere, Finland
5Department of Clinical Physiology and Nuclear Medicine, Kuopio University Hospital, Kuopio, Finland
Background: Benign biliary strictures (BBS) are primarily treated endoscopically, increasingly with
covered self-‐expandable metal stents (CSEMS). Biodegradable biliary stents (BDBS) have shown
promising results in animal models and may be the future of endoscopic therapy of BBS. Tissue
response in BBS to different stents is largely unknown. The aim was to assess the expression of
proteins related to tissue healing in BBS compared to the intact bile duct (BD), and to study the protein
expression after therapy with CSEMS or BDBS.
Methods: Swine with ischemic BBS were endoscopically treated either with BDBS or CSEMS. Tissue
samples were harvested from swine with intact BD (n=5), untreated BBS (n=5) and after six months of
therapy with BDBS (n=4) or CSEMS (n=5). Two-‐dimensional electrophoresis with protein
identification was performed to evaluate protein expression patterns at these stages.
Results: Compared to the intact BD, in BBS the expression of proteins Galectin-‐2 and Annexin-‐A4
decreased. BDBS treatment normalized Galectin-‐2 level, but with CSEMS therapy it remained low.
Annexin-‐A4 expression remained low after both treatments. Transgelin expression, which was low in
intact BD and in the BBS, remained low after BDBS treatment but increased after CSEMS therapy.
Conclusion: The expression of proteins related to tissue healing in BBS is different after treatment
with BDBS and CSEMS. Treatment with BDBS may bring the protein expression towards what is seen
in the intact BD. These findings suggest future therapeutic implications and warrant further research.
Key words: biliary, stricture, stent, biodegradable, bioabsorbable, ERCP (endoscopic retrograde
cholangio-‐pancreatography)

2
Background
Endoscopic stent insertion has a well-‐established role as a primary therapy for benign biliary
strictures (BBS) [1]. The traditional use of plastic stents (PS) [2-‐4] has been challenged due to the
need of frequent endoscopic stent exchanges and relatively high rate of stricture recurrence with
consequent burden to patient. Increasingly used covered self-‐expandable metal stents (CSEMS) may
offer potential advantages over PS: fewer endoscopic sessions and improved patency with fewer stent
occlusions due to larger post-‐deployment diameter [5, 6]. However, only few studies comparing
plastic stents to CSEMS in benign strictures exist and the optimal duration of CSEMS therapy to ensure
stricture resolution with safe stent removal is yet to be determined [1].
A biodegradable self-‐expanding, large-‐bore stent (BDBS) with no need for stent removal offers a
seemingly ideal solution to overcome the drawbacks of previous methods [7-‐9]. As the device for
endoscopic application of these stents has been only recently available, those few clinical studies
published on human biliary strictures are from percutaneous use [10].
The protein-‐level mechanism of development of BBS as well as the details of tissue response caused by
CSEMS or BDBS are largely unknown. Understanding pathogenesis of a BBS and tissue response to
CSEMS and BDBS are factors that may prove critical in determining the optimal strategy of stent
therapy in BBS. In the present study we analyzed proteins, which according to the previous findings
may play a role in the gastrointestinal stricture formation [11-‐17].
The aim of this study was 1) to determine protein expression pattern of BBS and 2) to specify the
proteomic response to BDBS and CSEMS in biliary duct in the swine.
Methods
BBS was induced as previously described [18] in 14 Yorkshire swine (weight median 50 kg, range 48-‐
52 kg). BBS was induced in laparotomy by subtotal ligation of the common bile duct (CBD) with
absorbable sutures resulting in controlled ischemia. Two months after induction of BBS, CBD was
cannulated under duodenoscopy (Olympus 145 series, Tokyo, Japan). In endoscopic retrograde
cholangiography (ERC) with iohexol contrast medium (Omnipaque 180 mg I/ml; Amersham Health AS,
Oslo, Norway) a tight BBS, median length of 10 mm (range 9-‐11 mm) was confirmed in all of the
animals.

3
Five animals had no treatment of the stricture (BBS group). From these animals, samples were
harvested at two months after the induction of BBS and the animals were sacrificed. Nine animals
received an endoscopic treatment of BBS; in BDBS group four with a braided self-‐expandable poly-‐
lactide BDBS (diameter 7 mm, length 50 mm; custom-‐made at the Institute of Biomaterials, Tampere
University of Technology, Tampere, Finland) and in CSEMS group, five with a fully covered self-‐
expandable metal stent (diameter 10 mm, length 80 mm; Wallstent, Olympus PBD-‐3Z; Tokyo, Japan).
During the follow-‐up stent patency and location were confirmed by repeated serum liver function
tests, x-‐ray. At six months, tissue samples were harvested from the CSEMS and BDBS treated BBSs and
the animals were sacrificed. The control samples were harvested from intact bile duct (Intact BD).
For all the animal experiments and operations, anaesthesia was induced after 24 hour fasting by
propofol (Propofol Alpharma 10 mg/ml, Alpharma AS, Oslo, Norway) 5 mg/kg i.v. bolus after atropin
(Atropin 1mg/ml, OY Leiras Finland AB, Turku, Finland) 0.05 mg/kg i.m. plus azaperone (Stresnil
40mg/ml, Janssen Animal Health BVBA, Beerse, Belgium) 4 mg/kg i.m. premedication. The anaesthesia
was maintained with propofol 15 mg/kg/h and analgesia with fentanyl citrate (Fentanyl; 50 μg/ml;
Janssen Pharmaceutica, Beerse, Belgium) 5 μg/kg/h after intubation with a cuffed endotracheal tube.
Prior to extubation, buprenorfine (Temgesic; 0.3 mg/ml; Reckitt&Colman Products Ltd, Hull, UK)
0.009 mg/kg i.m. was given for postoperative pain medication; the dose was repeated in 8 hours and
continued twice daily for the three following days or longer if needed. The animals received cefuroxim
(Zinacef; GlaxoSmithKline, London, U.K.) 30 mg /kg i.v. for infection profylaxis before operations and
cefalexin (Kefexin, Orion, Espoo, Finland) 750 mg p.o. daily for three days after endoscopy to prevent
cholangitis. Omepratzole (Losec mups, AstraZeneca, Södertälje, Sweden) 20 mg p.o. was given daily for
the entire follow-‐up period to prevent duodenal ulcers. The animals were fed with standard pig chow
and were allowed free access to water and free movement in their cages. A histopathologic analysis
was performed to ascertain the histologic similarity of samples. The statistical significance was
assessed by Student´s two-‐tailed T-‐test, where p value of < 0.05 was considered significant.
2D Gel Electrophoresis (DIGE)
Proteins were subjected to a fractionated extraction protocol as described previously [19] Protein labeling for DIGE was conducted as described in the Ettan DIGE user manual. 50 µg of each protein
sample were labelled with 400 pmol CyDye DIGE fluor minimal dyes Cy2, Cy3, and Cy5 (Amersham
Biosciences, Freiburg, Germany). Isoelectric focusing was performed for a total of 125 kVh after
loading 50 µg of total protein/strip onto linear immobilised pH gradient (IPG) strips (Immobiline
DryStrips pH 3–11; Amersham Biosciences). After that, proteins were reduced by dithiothreitol,
alkylated by iodoacetamide, and second dimension separation was performed on 12.5%
polyacrylamide gels. Each sample was run at least three times.

4
The separated proteins in DIGE gels were visualised by Typhoon 9400 variable mode imager
(Amersham Biosciences) using the wavelengths of the respective CyDyes. DeCyder image anyalysis
software (Amersham Biosciences) was used to analyze the DIGE images as described in the Ettan DIGE
user manual. Experimental Mw and pI values were calculated internally.
Protein identification by MALDI-TOF-MS
Conventional SDS-‐Page gels were stained by modified silver staining compatible with MALDI-‐TOF-‐MS
[20]. Proteins of interest were manually excised from the corresponding preparative gel and subjected
to in-‐gel tyrptic digestion (Promega, Mannheim, Germany) as described [21]. Digested protein
samples were analysed using MALDI-‐MS in the positive ion mode (Autoflex II time-‐of-‐flight
instrument, Bruker Daltonics, Massachusetts, US). The resulting tryptic, monoisotopic peptide masses
were searched against the NCBInr or SwissProt nonredundant protein sequence database (Mascot;
Matrix Science Ltd., London, UK) using the Peptide Mass Fingerprint (PMF) method. Identification was
based on a significant Mascot score (p < 0.05) and on matching peptides with a protein sequence
coverage of > 20%. The experimental Mw and pI values determined from the protein pattern had to be
in agreement with the theoretical value of the identified proteins.
Ethical aspects
The animal study protocol was reviewed and approved by the Provincial Government of Eastern
Finland and the Animal Ethics Committee of the University of Kuopio, Finland.
Results
Tissue samples were analyzed from swine with intact bile duct (intact BD, n=5), untreated BBS (n=5)
and after six months of therapy with BDBS (n=4) or CSEMS (n=5). Proteins indentified in the screening
were Apolipoprotein-‐A1, Annexin-‐A4, Galectin-‐2, Transgelin, Myosin light polypeptide-‐6, Albumin,
Superoxide dismutase,-‐1, Heat-‐shock protein beta-‐6, Peroxiredoxin-‐5 and Muscle creatine kinase, all
potentially associated to tissue injury and healing. Protein expression pattern from an intact BD,
untreated BBS and after treatment with either BDBS or CSEMS is shown in Figure 2.
Housekeeping protein Apolipoprotein-‐1 expression was stable in all samples. In BBS, the, expression
of Annexin-‐A4 was reduced to 37% and expression of Galectin-‐2 was reduced to 14% (p=0.03)
compared to the intact BD. Fragmented Transgelin expression was increased to 290% compared to the
intact BD. No difference in Myosin light polypeptide-‐6 (MLP-‐6) expression was observed. (Fig 2A-‐D).

5
After BDBS and CSEMS treatment, the expression of Annexin A4 remained at the level seen in BBS.
After BDBS treatment the expression of Galectin-‐2 returned to the level of intact BD, whereas after
CSEMS treatment the expression remained at the low level seen in the BBS (p=0.02). Transgelin
expression, being undetectable in intact BD, was increased to 450% in CSEMS treated animals
compared to BDBS. Expression of fragmented Transgelin remained at the increased level of untreated
BBS after both BDBS (p=0.04) and CSEMS treatment. MLP-‐6 expression was increased to 300% after
BDBS treatment, but remained unchanged after CSEMS treatment (Fig. 2A-‐D).
Single gels of each sample showed similar results to pooled samples. For other screened proteins no
major differences were found.
Discussion
To the best of our knowledge, this is the first study to evaluate patterns of protein expression in BBS
and after treatment period of six months with either with BDBS or CSEMS. Protein analysis of BBS
treated with stents not only provides additional knowledge in attempting to understand the
pathogenesis of BBS but also contributes to our understanding of tissue response to different types of
stents.
The current treatment of BBS is based mainly on the dilation of a stricture followed by an insertion of
either plastic or CSEMS. The treatment of BBS with multiple plastic stents is associated in nearly 90%
clinical success [22], but up to 38% rate of stricture recurrences in long-‐term follow-‐up have been
reported [3]. The results have been much worse in strictures secondary to calcifying chronic
pancreatitis and when only one stent has been used instead of multiple plastic stents [4, 23]. The best
results are achieved in post-‐operative strictures by trimonthly stent exchange and aggressive increase
in the number of stents [2], with repeated demanding endoscopic procedures. CSEMS are increasingly
used in BBS, the most important benefit being the requirement of fewer endoscopic sessions and
possibly fewer adverse events and lower overall costs [1, 6]. The weaknesses of CSEMS include
difficult removal due to tissue embedding and overgrowth [24, 25] and risk of development of de-‐
novo strictures after stent removal [26, 27]. The tissue response of biliary epithelium to CSEMS is not
widely studied [28, 29], and no data on the changes on protein expression has been published.
Literature of braided, self-‐expanding, biodegradable stents in BBS is promising but scarce. Endoscopic
insertion has been shown feasible and poly-‐lactide stent therapy has been shown not to cause scar
formation, granulation or hyper-‐epithelisation in animal models [7, 8]. Besides, BDBS have been safe
and effective in the conventional type of hepatico-‐jejunostomy performed in swine, where it improves

6
biliary drainage during an 18-‐month follow-‐up [30]. They also appear better in management of a
cystic duct leakage than a plastic stent in an animal model [8]. In humans, they have been successfully
used for securing a hepatico-‐jejunal [9] and pancreato-‐jejunal anastomosis [31]. Commercially
available BDBS are made of polydioxanone, a co-‐polymer of poly-‐lactide, the degradation pattern of
which is similar to PDS surgical sutures [32]. The endoscopic implantation device is not yet in clinical
use. Published results with percutaneously inserted BDBS have been excellent in 16 months follow-‐up
[10]. Similarly to poly-‐lactide stents, a predictable degradation in three months as well as good
histologic biocompatibility has been reported in an animal model [33].
We discovered remarkable changes in a few proteins that have been previously associated to tissue
injury and healing on other tissues. Galectin-‐2 expression has reportedly been related to acute and
chronic inflammatory responses as well as in production of cytokines and inflammatory mediators,
cell adhesion, migration, and apoptosis [17]. Galectin expression may also be related to intestinal
wound healing [16] and apparently play a role in mucosal inflammation and stricture and fistula
formation in inflammatory bowel disease related strictures [15]. Annexins are related to cellular
functions such as endo-‐ and exocytosis, actin configuration, signaling, and plasma membrane repair
[11]. Transgelin levels have been linked to smooth muscle differentation [14] and in mesangial cell
migratory and proliferative response to injury [12]. Myosin light polypeptide expression is connected
to intestinal tight-‐junctions essential for epithelial function [13].
The ischemic model of BBS induced a statistically significantly decrease in galectin-‐2 expression and
an increase in transgelin expression. Additionally, a decrease was observed in Annexin -‐A4 and Myosin
light polypeptide-‐6. In the light of these findings it could be hypothetized, that Annexin-‐A4, Transgelin
and Galectin-‐2 play a role also in the reaction to ischemia in the biliary duct.
We also compared the effects of BDBS and CSEMS on the protein expression in the stricture. We found
that the protein expression appears to differ considerably depending on the type of biliary stent
Interestingly, BDBS treatment seemed to normalize Galectin-‐2 level, but with CSEMS therapy it
resembled untreated BBS. Moreover, Transgelin expression, which was low in intact BD and in the
BBS, was elevated as a reaction to CSEMS but not to BDBS. In contrast, Myosin light polypeptide-‐6
being normal in BBS was increasingly elevated in strictures treated with BDBS compared to intact bile
duct or CSEMS. Besides, reduced Annexin-‐A4 levels of BBS were not normalized after therapy with
either BDBS or CSEMS stents. However, it´s expression was less decreased in BDBS than in CSEMS
treatment group.

7
Conclusions
This study reports protein expression in an untreated BBS and after six months of treatment with
BDBS or CSEMS in an experimental ischemic stricture model. Significant differences in the expression
of proteins related to inflammatory response, apoptosis and smooth muscle differentiation between
intact BD and ischemic BBS were found. Furthermore, the response appears different depending
whether the stricture is treated with CSEMS or BDBS, possibly attributed to different healing response.
In the light of previous findings on BDBS and on the role of Annexins, Galectins and Transgelin, it may
be hypothesized that BDBS compared to CSEMS better reverses the changes in protein expression
induced by BBS. The result may pave the road for future therapeutic implications such as selecting the
optimal stent therapy in BBS or developing drug-‐eluding stents. However, this study does not answer
the question whether the observed changes were of benefit. Further research is thus warranted to
confirm the results from the relatively small sample since it is currently not known what would be the
optimal protein expression for stricture healing.
Figure 1: 2-‐Dimensional Electrophoresis image of biliary stricture from swine ischemic stricture after
6 months of stenting.
transgelin
muscle creatine kinase
annexin A4
trypsin precursor
heat-shock protein beta-6
peroxiredoxin 5 [fragm.] superoxide dismutase 1
albumin [fragm.]
pH 3 pH 11
mol. weight
myosin light polypeptide 6
apolipoprotein A-I
transgelin [fragm.]
galectin-2

8
Figure 2A-‐D Expression of Annexin-‐A4 (A), Galectin-‐2 (B), Transgelin (C) and MLP-‐6 (D) in swein:
intact bile duct (Intact BD), BBS at two months (BBS 2 mo) and after six months of therapy with BDBS
or CSEMS. In all groups, samples from five animals were analyzed, except in the BDBS group, where
samples from four animals were analyzed. In figure p<0.05 in BBS 2 mo compared to intact duct,
CSEMS compared to intact duct and CSEMS compared to BBS 2 mo. In figure C, p<0.05 in BDBS
compared to intact duct.
0"
500"
1000"
1500"
2000"
2500"
3000"
3500"
Intact"BD" BBS"2"mo" BDBS" CSEMS"
A.#Annexin#A4#
0"
500"
1000"
1500"
2000"
2500"
3000"
3500"
Intact"BD" BBS"2"mo" BDBS" CSEMS"
B.#Galec.n/2#
*"*"
0"
500"
1000"
1500"
2000"
2500"
3000"
3500"
4000"
4500"
Intact"BD" BBS"2"mo" BDBS" CSEMS"
C.#Transgelin#
transgelin"[fragm]"
transgelin"
*"
0"500"1000"1500"2000"2500"3000"3500"4000"4500"5000"
Intact"BD" BBS"2"mo" BDBS" CSEMS"
D.#MLP/6#
myosin"light"polypepBde"6"E"Spot"1"myosin"light"polypepBde"6"E"Spot"2"

9
Competing interests
The authors report no competing interest nor disclosures.
Acknowledgements
The authors wish to thank the staff of the National Laboratory Animal Center, Kuopio University,
Finland, for their competent technical assistance and for the use of laboratory facilities. We are
grateful to Dr Martina Schnölzer (German Cancer Research Center, Heidelberg, Germany) for
assistance and access to DIGE Typhoon Imager and DeCyder image analysis software and Prof.
Neumaier (Institute for Clinical Chemistry, Mannheim, Germany) for access to MALDI-‐TOF mass
spectrometer. This study was financially supported by the National Technology Agency of Finland (TEKES) and the Competitive State Research Financing of the Expert Responsibility Area of Tampere
University Hospital, Finland.
References
1. Baron TH S, Davee T: Endoscopic management of benign bile duct strictures. Gastrointest Endosc Clin N Am 2013, 23(2):295-311.
2. Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V: Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc 2001, 54(2):162-168.
3. Draganov P, Hoffman B, Marsh W, Cotton P, Cunningham J: Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents. Gastrointest Endosc 2002, 55(6):680-686.
4. Perri V, Familiari P, Tringali A, Boskoski I, Costamagna G: Plastic biliary stents for benign biliary diseases. Gastrointest Endosc Clin N Am 2011, 21(3):405-433.
5. Kahaleh M, Brijbassie A, Sethi A, Degaetani M, Poneros JM, Loren DE, Kowalski TE, Sejpal DV, Patel S, Rosenkranz L, McNamara KN, Raijman I, Talreja JP, Gaidhane M, Sauer BG, Stevens PD: Multicenter Trial Evaluating the Use of Covered Self-expanding Metal Stents in Benign Biliary Strictures: Time to Revisit Our Therapeutic Options? J Clin Gastroenterol 2013, 47(8):695-699.
6. Kaffes AJ, Liu K: Fully covered self-expandable metal stents for treatment of benign biliary strictures. Gastrointest Endosc 2013, 78(1):13-21.

10
7. Ginsberg G, Cope C, Shah J, Martin T, Carty A, Habecker P, Kaufmann C, Clerc C, Nuutinen J-, Törmälä P: In vivo evaluation of a new bioabsorbable self-expanding biliary stent. Gastrointest Endosc 2003, 58(5):777-784.
8. Laukkarinen J, Nordback I, Mikkonen J, Karkkainen P, Sand J: A novel biodegradable biliary stent in the endoscopic treatment of cystic-duct leakage after cholecystectomy. Gastrointest Endosc 2007, 65(7):1063-1068.
9. Laukkarinen J, Sand J, Leppiniemi J, Kellomaki M, Nordback I: A novel technique for hepaticojejunostomy for nondilated bile ducts: a purse-string anastomosis with an intra-anastomotic biodegradable biliary stent. Am J Surg 2010, 200(1):124-130.
10. Mauri G, Michelozzi C, Melchiorre F, Poretti D, Tramarin M, Pedicini V, Solbiati L, Cornalba G, Sconfienza LM: Biodegradable biliary stent implantation in the treatment of benign bilioplastic-refractory biliary strictures: preliminary experience. Eur Radiol 2013, 23(12):3304-3310.
11. Crosby KC, Postma M, Hink MA, Zeelenberg CH, Adjobo-Hermans MJ, Gadella TW: Quantitative analysis of self-association and mobility of annexin A4 at the plasma membrane. Biophys J 2013, 104(9):1875-1885.
12. Assinder SJ, Stanton JA, Prasad PD: Transgelin: an actin-binding protein and tumour suppressor. Int J Biochem Cell Biol 2009, 41(3):482-486.
13. Cunningham KE, Turner JR: Myosin light chain kinase: pulling the strings of epithelial tight junction function. Ann N Y Acad Sci 2012, 1258:34-42.
14. Daniel C, Ludke A, Wagner A, Todorov VT, Hohenstein B, Hugo C: Transgelin is a marker of repopulating mesangial cells after injury and promotes their proliferation and migration. Lab Invest 2012, 92(6):812-826.
15. Lippert E, Gunckel M, Brenmoehl J, Bataille F, Falk W, Scholmerich J, Obermeier F, Rogler G: Regulation of galectin-3 function in mucosal fibroblasts: potential role in mucosal inflammation. Clin Exp Immunol 2008, 152(2):285-297.
16. Paclik D, Lohse K, Wiedenmann B, Dignass AU, Sturm A: Galectin-2 and -4, but not galectin-1, promote intestinal epithelial wound healing in vitro through a TGF-beta-independent mechanism. Inflamm Bowel Dis 2008, 14(10):1366-1372.
17. Liu FT, Yang RY, Hsu DK: Galectins in acute and chronic inflammation. Ann N Y Acad Sci 2012, 1253:80-91.
18. Laukkarinen J, Chow P, Sand J, Yu S, Somanesan S, Kee I, Song IC, Ng T, Nordback I: Swine benign biliary stricture model. Gastroenterolology 2004, 126(Supplement 2):775.
19. Lohr JM, Faissner R, Koczan D, Bewerunge P, Bassi C, Brors B, Eils R, Frulloni L, Funk A, Halangk W, Jesenofsky R, Kaderali L, Kleeff J, Kruger B, Lerch MM, Losel R, Magnani M, Neumaier M, Nittka S, Sahin-Toth M, Sanger J, Serafini S, Schnolzer M, Thierse HJ, Wandschneider S, Zamboni G, Kloppel G: Autoantibodies against the exocrine pancreas in autoimmune pancreatitis: gene and protein expression profiling and immunoassays identify pancreatic enzymes as a major target of the inflammatory process. Am J Gastroenterol 2010, 105(9):2060-2071.

11
20. Mortz E, Krogh TN, Vorum H, Gorg A: Improved silver staining protocols for high sensitivity protein identification using matrix-assisted laser desorption/ionization-time of flight analysis. Proteomics 2001, 1(11):1359-1363.
21. Hellman U, Wernstedt C, Gonez J, Heldin CH: Improvement of an "In-Gel" digestion procedure for the micropreparation of internal protein fragments for amino acid sequencing. Anal Biochem 1995, 224(1):451-455.
22. Van Boeckel PGA, Vleggaar FP, Siersema PD: Plastic or metal stents for benign extrahepatic biliary strictures: A systematic review. BMC Gastroenterology 2009, 9.
23. Cahen DL, Van Berkel A-M, Oskam D, Rauws EAJ, Weverling GJ, Huibregtse K, Bruno MJ: Long-term results of endoscopic drainage of common bile duct strictures in chronic pancreatitis. European Journal of Gastroenterology and Hepatology 2005, 17(1):103-108.
24. Chaput U, Scatton O, Bichard P, Ponchon T, Chryssostalis A, Gaudric M, Mangialavori L, Duchmann J-, Massault P-, Conti F, Calmus Y, Chaussade S, Soubrane O, Prat F: Temporary placement of partially covered self-expandable metal stents for anastomotic biliary strictures after liver transplantation: A prospective, multicenter study. Gastrointest Endosc 2010, 72(6):1167-1174.
25. Cahen DL, Rauws EA, Gouma DJ, Fockens P, Bruno MJ: Removable fully covered self-expandable metal stents in the treatment of common bile duct strictures due to chronic pancreatitis: a case series. Endoscopy 2008, 40(8):697-700.
26. Kasher JA, Corasanti JG, Tarnasky PR, McHenry L, Fogel E, Cunningham J: A multicenter analysis of safety and outcome of removal of a fully covered self-expandable metal stent during ERCP. Gastrointest Endosc 2011, 73(6):1292-1297.
27. Phillips MS, Bonatti H, Sauer BG, Smith L, Javaid M, Kahaleh M, Schmitt T: Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Endoscopy 2011, 43(6):512-517.
28. Vakil N: Expandable metal stents: principles and tissue responses. Gastrointest Endosc Clin N Am 2011, 21(3):351-7, vii.
29. Bakhru MR, Foley PL, Gatesman J, Schmitt T, Moskaluk CA, Kahaleh M: Fully covered self-expanding metal stents placed temporarily in the bile duct: Safety profile and histologic classification in a porcine model. BMC Gastroenterology 2011, 11. 76.
30. Laukkarinen JM, Sand JA, Chow P, Juuti H, Kellomaki M, Karkkainen P, Isola J, Yu S, Somanesan S, Kee I, Song IC, Ng TH, Nordback IH: A novel biodegradable biliary stent in the normal duct hepaticojejunal anastomosis: an 18-month follow-up in a large animal model. J Gastrointest Surg 2007, 11(6):750-757.
31. Laukkarinen J, Lamsa T, Nordback I, Mikkonen J, Sand J: A novel biodegradable pancreatic stent for human pancreatic applications: a preclinical safety study in a large animal model. Gastrointest Endosc 2008, 67(7):1106-1112.
32. Lorenzo-Zuniga V, Moreno-de-Vega V, Marin I, Boix J: Biodegradable stents in gastrointestinal endoscopy. World J Gastroenterol 2014, 20(9):2212-2217.
33. Grolich T, Crha M, Novotny L, Kala Z, Hep A, Necas A, Hlavsa J, Mitas L, Misik J: Self-expandable biodegradable biliary stents in porcine model. J Surg Res 2015, 193(2):606-612.

12

Case Report
Biodegradable Biliary Stent in the EndoscopicTreatment of Cystic Duct Leak After Cholecystectomy:
The First Case Report and Review of Literature
Antti Siiki, MD,1 Irina Rinta-Kiikka, MD, PhD,2 Juhani Sand, MD, PhD,1 and Johanna Laukkarinen, MD, PhD1
Abstract
Background: The preferred therapy for simple postcholecystectomy biliary leak consists of percutaneousdrainage and biliary stent insertion under endoscopic retrograde cholangiopancreatography (ERCP). With anovel endoscopic insertion device, a biodegradable biliary stent (BDBS) may be used in the treatment of acystic duct leak without repeated endoscopy for stent removal. The objective of this article was to report the firstcase of endoscopic insertion of BDBS for postoperative bile leak and assess its feasibility and safety.Patient and Methods: A 64-year-old man with a postoperative leak from the cystic duct stump was treated withERCP, biliary sphincterotomy, and insertion of a self-expandable 40- · 8-mm polydixanone BDBS (Ella CS,Hradec Kralove, Czech Republic) after insertion of a percutaneous drain.Results: Endoscopic insertion of BDBS was successful and uncomplicated. On Day 7 after ERCP, the patientwas in good condition, no signs of bile leak or inflammation were observed, and the percutaneous drain wasremoved. At 3 months, magnetic resonance imaging showed that the BDBS was patent and in the right location.At 6 months, the stent had expectedly degraded.Conclusions: A novel endoscopic insertion device with a polydixanone BDBS appears feasible in treatingdisorders of the human biliary duct. BDBS now offers an encouraging option for endoscopic therapy of bile leaks.
Introduction
Being one of the most common complications of cho-lecystectomy,1 a bile leak either from the stump of the
cystic duct or from an aberrant biliary duct (Strasberg gradeA–C) may be treated endoscopically.2–4 The well-establishedtherapy consists of percutaneous drainage followed by en-doscopic retrograde cholangiopancreatography (ERCP), en-doscopic sphincterotomy, and insertion of an inexpensive 7–10 French plastic stent to ensure the bile flow downstreamthrough the papilla. In the biliary duct, a biodegradable biliarystent (BDBS) has been successfully used in animal models inendoscopic treatment of iatrogenic bile leak.5 The obviousadvantages of a self-expandable BDBS, with a postdeploy-ment diameter of 8 mm, include no need for removal in re-peated endoscopy and improved bile flow due to larger stentdiameter. Although the feasibility and long-term degradationpattern of polydixanone BDBS have been proven in percu-taneous use in humans,6 so far no endoscopic implantationdevice has been available for use in clinical studies.
Patient and Methods
A previously healthy 64-year-old man was admitted 2 daysafter an elective open cholecystectomy with elevated tem-perature and upper abdominal pain to the tertiary referralcenter of Tampere University Hospital, Tampere, Finland.The serum C-reactive protein concentration was elevated(93 mg/L), and the bilirubin level was within normal limits(17 lmol/L). Transabdominal ultrasound, magnetic reso-nance imaging (MRI), and computed tomography scan re-vealed a 5- · 6-cm fluid accumulation in the gallbladder bedwithout common bile duct stones or signs of biliary ob-struction or concomitant vascular injury. A radiologist in-serted a percutaneous 8-French pigtail drain under ultrasonicguidance to drain the fluid accumulation, which proved to bebile juice (fluid bilirubin level = 231 lmol/L).
As bile flow into the drain continued for 8 days after sur-gery, ERCP was performed with the patient under conscioussedation (7 mg of oxycodone [Oxynorm�; Takeda GmbH, Linz,Austria] and 7 mg of midazolam [Hameln Pharmaceuticals
Departments of 1Gastroenterology and Alimentary Tract Surgery and 2Clinical Radiology, Tampere University Hospital, Tampere,Finland.
This study is registered with Clinicaltrials.gov with clinical trial registration number NCT02353286.
JOURNAL OF LAPAROENDOSCOPIC & ADVANCED SURGICAL TECHNIQUESVolume 25, Number 5, 2015ª Mary Ann Liebert, Inc.DOI: 10.1089/lap.2015.0068
419

GmbH, Hameln, Germany]) administered intravenously andmonitored by the endoscopy team. An anti-inflammatorysuppository (100 mg of diclofenac [Novartis, Espoo, Finland])was given approximately 60 minutes before ERCP. Duodenalperistalsis was reduced with 40 mg of hyoscine butylbromide(Buscopan�; Delpharm Reims, Reims, France) intravenously.A standard duodenoscope (model TJF-Q180V; Olympus,Hamburg, Germany) with air insufflation was used. Afteruneventful cannulation with a standard short guidewire, a fullbiliary sphincterotomy was performed (Dreamtome� RX44;Boston Scientific Corp., Natick, MA) with pure-cut elec-trocautery (Erbe ViO� 200D electrosurgical system; ErbeElektromedizin GmbH, Tubingen, Germany). Cholangio-graphy (Philips BV Endura; Philips Medical Systems, Best,The Netherlands) using 240 mg/mL of iohexol (Omnipaque�;GE Healthcare, Little Chalfont, United Kingdom) with abiliary balloon (9/12 mm; Extractor� Pro RX; Boston Sci-entific Corp.) revealed a slight leakage of contrast outside thebiliary duct in the vicinity of the cystic duct stump (Fig. 1).
This study received approval (protocol number R12021)from the Ethical Committee of Pirkanmaa Hospital District,
Tampere. The research use of BDBS was previously ap-proved by the Regional Ethics Committee of PirkanmaaHospital District. Informed consent to the use of BDBS wasobtained from the patient.
Results
Before stent implantation, a stiff long guidewire (0.035inch; 450 cm; Dreamwire�; Boston Scientific Corp.) waspositioned. A custom-made braided self-expandable bio-degradable polydixanone noncovered biliary stent withgolden radiopaque markers at both ends and 40 mm inlength with a postdeployment diameter of 8 mm (Ella CS,Hradec Kralove, Czech Republic) was then successfullyinserted (Fig. 2). The stent was adjusted to the proper lo-cation with its distal end clearly visible inside the duodenum(Fig. 3). After discharge, the output of the percutaneousdrain diminished to less than 10 mL/day, indicating that theBDBS had successfully treated the postcholecystectomybiliary leak. The drain was removed on Day 7 after ERCP atan outpatient visit when the inflammatory markers werenormalized, with no signs of icterus, and the patient wasfeeling well. No ERCP- or stent-related complications oc-curred during the first 30 days. At the follow-up MRI at 3months, the stent was patent and in the right location inside
FIG. 1. A cholangiography image at the beginning of thebiodegradable stent implantation. *A faint contrast leakclose to the stump of the cystic duct is seen just below thesurgical clips. **Percutanous 8-French pigtail drain. ***Thetip of the stent implantation device is inserted over a stiffguidewire into the distal common bile duct.
FIG. 2. A custom-made braided self-expandablebiodegradable polydixanone noncovered biliarystent with golden radiopaque markers at both endswith a postdeployment diameter of 8 mm (Ella CS)and an endoscopic insertion device.
FIG. 3. An endoscopy view of the biodegradable stent infinal position with a guidewire still in place.
420 SIIKI ET AL.

the common bile duct (Fig. 4). At 6 months the stent was nolonger visible in MRI.
Discussion
Endoscopic stent treatment is the preferred treatment insimple bile duct injury and leakage from the cystic duct aftercholecystectomy.2–4 Although minor bile duct injury aftercholecystectomy (Strasberg grade A–C) is relatively un-common with an incidence of less than 1%,1,4 the largenumbers of cholecystectomies performed make this compli-cation an important clinical issue in tertiary-care centers forboth surgeons and endoscopists. Efficient therapy with aplastic stent necessitates repeated endoscopy for stent re-moval, usually 1–2 months after insertion. To overcome theburden of multiple endoscopies to patients and the healthcaresystem, a BDBS appears to offer a perfect solution. However,until recently, only transhepatic and no endoscopic insertiondevices have been available from stent manufacturers forbiliary use in biodegradable biliary stenting. We report thefirst case of successful endoscopic insertion of a BDBS with acommercial insertion device for postcholecystectomy cysticduct leak with 6 months of follow-up.
Earlier studies have shown that the biodegradable stentsmay be safely used in the hepatobiliary duct.7–9 An endo-scopically inserted BDBS also offered a safely and fastertreatment of bile leakage than a plastic stent in an animalmodel of iatrogenic cystic duct leak.5 Polylactide stents ap-pear to remain patent for at least 3 months and disintegrate at6 months with no residual changes in the histology of thebiliary epithelium.5 The polydixanone BDBS used in thiscase has been proven to be safe and fully degradable in 6months in percutanous biliary use in humans and in theanimal model.6,8 Its molecular structure and degradationprofile are comparable to those of polylactide.6 Further-more, there is accumulating clinical experience of the use ofpolydixanone biodegradable stents in, for example, esoph-ageal strictures.10
In this case, a prototype model of an endoscopic inser-tion device was successfully used with a custom-made self-expandable radiopaque braided polydixanone biliary stent40 mm long and 8 mm in diameter. Although the stent wasintroduced over a stiff guidewire, we found it challenging topush the stent insertion device into the common bile duct asthe prototype instrument appeared inflexible; during im-plantation, only careful manipulation of the tip of the duo-denoscope and limited use of an elevator were possible as theinsertion device was easily bent by axial force.
In our experience the most important issue for the suc-cessful use of the BDBS was good endoscopy technique witha stable position in the duodenum to be able to proceedstraight down the duodenoscope and to avoid excessive useof the elevator as the insertion device passes the tip of thescope. The gold radiography markers at both ends of the stentprovided adequate visibility in radiography. However, thestent itself is x-ray negative, and endoscopic visualization ofthe stent as it moves inside the insertion device may bechallenging.
The endoscopic implantation of a polydixanone BDBSwas successful with excellent clinical outcome in this case.At 3 months MRI showed that BDBS was still patent and hadnot migrated. Although the degradation profile has alreadybeen proven in clinical studies and now most issues associ-ated with the implantation device seem to have been solved,BDBS offers a fascinating option for endoscopists treatingpostoperative bile leaks. The main advantages—no needfor removal and large diameter—are obvious. However, re-sults from larger prospective studies are needed to confirmthe feasibility of the insertion device, as well as its cost-effectiveness and safety compared with plastic stents.
Acknowledgments
This study was financially supported by the CompetitiveState Research Financing of the Expert Responsibility area ofTampere University Hospital, Tampere, Finland.
Disclosure Statement
No competing financial interests exist.
References
1. Karvonen J, Salminen P, Gronroos JM. Bile duct injuriesduring open and laparoscopic cholecystectomy in the lap-aroscopic era: Alarming trends. Surg Endosc 2011;25:2906–2910.
FIG. 4. (A) T2-weighted, fat-suppressed magnetic reso-nance axial image shows the fluid-filled distal part of thecommon bile duct and the biodegradable stent inside it(white arrow). (B) T1-weighted magnetic resonance axialimage shows the distal part of the common bile duct and thebiodegradable stent inside it (white arrow).
ENDOSCOPIC BIODEGRADABLE BILIARY STENT IN BILE LEAK 421

2. Nordin A, Gronroos JM, Makisalo H. Treatment of biliarycomplications after laparoscopic cholecystectomy. Scand JSurg 2011;100:42–48.
3. Baillie J. Endoscopic approach to the patient with bile ductinjury. Gastrointest Endosc Clin N Am 2013;23:461–472.
4. Strasberg SM, Hertl M, Soper NJ. An analysis of theproblem of biliary injury during laparoscopic cholecystec-tomy. J Am Coll Surg 1995;180:101–125.
5. Laukkarinen J, Nordback I, Mikkonen J, et al. A novelbiodegradable biliary stent in the endoscopic treatment ofcystic-duct leakage after cholecystectomy. GastrointestEndosc 2007;65:1063–1068.
6. Mauri G, Michelozzi C, Melchiorre F, et al. Biodegradablebiliary stent implantation in the treatment of benign bilio-plastic-refractory biliary strictures: Preliminary experience.Eur Radiol 2013;23:3304–3310.
7. Itoi T, Kasuya K, Abe Y, et al. Endoscopic placement ofa new short-term biodegradable pancreatic and biliarystent in an animal model: A preliminary feasibility study(with videos). J Hepatobiliary Pancreat Sci 2011;18:463–467.
8. Grolich T, Crha M, Novotny L, et al. Self-expandablebiodegradable biliary stents in porcine model. J Surg Res2015;193:606–612.
9. Nordback I, Raty S, Laukkarinen J, et al. A novel radiopaquebiodegradable stent for pancreatobiliary applications—Thefirst human phase I trial in the pancreas. Pancreatology2012;12:264–271.
10. Lorenzo-Zuniga V, Moreno-de-Vega V, Marin I, et al.Biodegradable stents in gastrointestinal endoscopy. World JGastroenterol 2014;20:2212–2217.
Address correspondence to:Johanna Laukkarinen, MD, PhDDepartment of Gastroenterology
and Alimentary Tract SurgeryTampere University Hospital
Teiskontie 35FIN-33521 Tampere
Finland
E-mail: [email protected]
422 SIIKI ET AL.

![Antti Kiviluoto [email protected]](https://static.fdocuments.in/doc/165x107/61fc8a868d33c02b785e5fd1/antti-kiviluoto-emailprotected.jpg)