Antimycobacterial drugs. Famous Affected Europeans F Lesja Ukrainka F Anton Tchekhov F John Keats F...
-
Upload
anissa-pitts -
Category
Documents
-
view
220 -
download
4
Transcript of Antimycobacterial drugs. Famous Affected Europeans F Lesja Ukrainka F Anton Tchekhov F John Keats F...
Famous AffFamous Affeected Europeanscted Europeans
Lesja Ukrainka Lesja Ukrainka
Anton TchekhovAnton Tchekhov
John KeatsJohn Keats
Frédéric ChopinFrédéric Chopin
Charlotte, Emily, and Anne Brontë Charlotte, Emily, and Anne Brontë
Franz KafkaFranz Kafka
George OrwellGeorge Orwell
Increased Risk for TBIncreased Risk for TB: : People with HIVPeople with HIV
People who smoke 20+ cigarettes People who smoke 20+ cigarettes dailydaily
Man at an increased risk for TBMan at an increased risk for TB
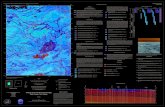
UkraineUkraine MorbidityMorbidity 10 1000/10000/1000000
populationpopulation 48,000 new cases 48,000 new cases
annuallyannually Mortality Mortality 15/100000 15/100000 Every hour 1 person Every hour 1 person
dies from tuberculosisdies from tuberculosis 8.3% of TB cases that 8.3% of TB cases that
are HIV +are HIV + 10 % of new cases are 10 % of new cases are
MDR-TBMDR-TB
2005 2006
Ukrainian PrisonsUkrainian PrisonsHigher risk for developing active TB due Higher risk for developing active TB due
to the following problems:to the following problems:
-Poor infection controlPoor infection control -Delays in diagnosis-Delays in diagnosis -Inadequate treatment-Inadequate treatment -High prevalence of HIV-High prevalence of HIV -Overcrowding and poor -Overcrowding and poor
nutritionnutrition TB is not unavoidable in prisons!TB is not unavoidable in prisons!
1993 – WHO1993 – WHO
Epidemy of tuberculosis has Epidemy of tuberculosis has started in the world, in the started in the world, in the
most countries it has spread most countries it has spread far beyond control borders far beyond control borders
and now it is a global danger and now it is a global danger for humanityfor humanity
Treatment of patients with tuberculosisTreatment of patients with tuberculosis
Chemotherapy with tuberculostaticsChemotherapy with tuberculostatics Hygiene regime Hygiene regime
DietDiet Fito therapyFito therapy
Sanatorium treatment Sanatorium treatment Collapse therapyCollapse therapy Surgical methodsSurgical methods
Other drugsOther drugs
Antimycobacterial drugs Derivatives of HINA: isoniazid, ftivazid etc. Antibiotics: rifampicin, rifabutin, strepromycin,
kanamycin, florimycin, capreomycin, cycloserine Derivatives of pyrazin-carbonic acid: pyrazinamide Ethambutol Tiourens: tioacetazone (tibon), salutizone Derivatives of tiamide-α-ethylizonicotinic acid:
ethionamide, protionamide Salts of PASA: PASA-Na etc. Combinated tuberculostatics: inabutol (isoniazid + ethambutol) infiricine (rifampicine + isoniazide) rifater (isoniazide + rifampicine + pyrazinamide)
Classification of International Union of tuberculosis treatment
Antimyco-bacterial activity
Drug Moderate daily dose
High IsoniazidRifampicinRifabutin
0,450,6
0,45
Moderate StreptomycinAmikacinKanamycinPirazynamidEtambutolOfloxacinPefloxacinCiprofloxacinetc.
1,01,01,0
1,5–2,01,2–1,60,6–0,80,4–0,8
1,0
Low ТіоаcetazonPAS-Na
0,1512,0
1st row: Isoniazid, Rifampicin, Ethambutol, Isoniazid, Rifampicin, Ethambutol,
Pirazynamid, Pirazynamid, Streptomycine Streptomycine
22ndnd row rowothers others
IsoniazideIsoniazide
Inhibits synthesis of phospholipids and Inhibits synthesis of phospholipids and damages membranes of MBT, hurts damages membranes of MBT, hurts mycolyc acidsmycolyc acids
Forms Forms compositions with two-valent ionscompositions with two-valent ions Hurts formation of RNA and DNAHurts formation of RNA and DNA Inhibits oxidative processes Inhibits oxidative processes Acts on MBT which is in state of active Acts on MBT which is in state of active
developmentdevelopment, situated int, situated intrra- and a- and extracellularly extracellularly
PPenetrates through all organs and tissuesenetrates through all organs and tissues
Metabolism in liver (acetylation)Metabolism in liver (acetylation) HINAHINA inactivators (acetylators)inactivators (acetylators)
(genetics) (genetics)SlowSlow FastFast
Since Since 6 6 h hafter test-dose after test-dose 44 mg mg//kgkg concentration in blood isconcentration in blood ismore than more than 0,8 0,8 mcg/mlmcg/ml
Intermittent administration is Intermittent administration is possiblepossible
Since Since 6 6 h hafter test-dose after test-dose 44 mg mg//kgkg concentration in blood isconcentration in blood isless than less than 0,0,22 mcg/mlmcg/ml
Hepatotoxicity increases Hepatotoxicity increases ((monoacetylhydrazine monoacetylhydrazine formationformation),),Intermittent administration Intermittent administration cannot be usedcannot be used
Side effects of isoniazide (derivatives of HINA) (5-18% of patients)
CNS – headache, euforia, insomnia, dizzyness
peripheral neuritis (derivatives of HINA – antivitamins В6), prophylaxis – 50 mg Vit В6 daily
allergy (treatment – antihistamine) heart – tachycardia, arrhythmia dyspeptic disorders, stomatitis hepatitis
Rifampicine Bactericide action, wide Bactericide action, wide spectrum of actionspectrum of action
damages synthesis of damages synthesis of proteins of MBTproteins of MBT
influences on intra- and influences on intra- and extracellular MBTextracellular MBT
penetrates through all penetrates through all organs and damaged areas organs and damaged areas (molecule in not ionized)(molecule in not ionized)
concentration concentration iin organs is n organs is 3-4 times 3-4 times highhigher than in er than in blood serumblood serum
Side effects of rifampicine (8-22%)
hepatotoxicity immune-allergic complications
– pseudo-flue syndrome- decreasing of platelets aggregation– haemolysis– acute hepato-renal insufficiency
induction of microsomal enzymes→ decreasing of effectiveness of oral contraceptives etc.
dyspeptic manifestations, stomatitis changes of urine, feaces, sweat, tears etc. color
into orange-red
Streptomycin
wide spectrum of action influences only on MBT situated
extracellularly is not absorbed in GIT concentration in tissues is 25-40 times
lower than in blood does not penetrate in caverns,
through BBB
Ethambutol
Influences on atypical mycobacteriumOn intra- and extracellular MBT,
which rapidly reproduce Gets accumulated in erythrocytesPenetrates into all organs and tissues,
into caverns
Side effects of ethambutol(1-2 %)
Retro bulbar neuritis of optic nerve (disorders of color vision – green, red, inaccuracy) – shouldn’t be administered for children under the age of 12
Bronchial spasm
Pyrasinamid
Acts on MBT, which are in condition of metabolic restmetabolic rest
On intra- and extracellular MBT Penetrates into all organs and tissues Activity grows in acid medium of caseous
masses
Side effects of pyrasinamid
hepatotoxicity– early – 7th day– late – after 6-8 months
dyspeptic disorders arthralgia (retains uric acid in the
organism – pyrasine-carbon acid is its antagonist)
Photosensitization
Standard regimes of anti-tuberculosis treatment according to WHO
Category of patients Treatment scheme Basic duration of treatment (months)
Primarily diagnosed tuberculosis (МBT+), heavy spread forms (MBT–)
2-3 months – 4 drugs, 4-5 months – 2 drugs
6–8
Patients with relapse of tuberculosis and non-effectively treated primarily diagnosed patients (MBT + in sputum smear)
2 months – 5 drugs3 months – 4 drugs4-5 months – 3 drugs
6–8
Primarily diagnosed tuberculosis (MBT–)
At first – 3,after – 2 drugs
6
Chronic forms of tuberculosis Individual regimes (depending on sensitivity of MBT) of 5-6 drugs
12
3 main schemes of administration of anti-tuberculosis drugs
І. Traditional long lasting (brakeless) treatment ІІ. Intermitting chemotherapy
3 times a week 1 time a week (HINA in slow acetylators) mixed chemotherapy (interchange of one drug in a
certain combination - 3-4 drugs daily from 5-6 of the administered) – 1-3 times a week the combination is changed , at nowadays – 5-6 drugs simultaneously
ІІІ. Short lasting courses of brakeless treatment
Classificatoin of fluoroquinolones
І generation
Ciprofloxacin * Ofloxacin * Norfloxacin * Pefloxacin * Lomefloxacin * Fleroxacin
ІІ generation
Grepafloxacin Sparfloxacin* Gatifloxacin Clinafloxacin Moxifloxacin* Trovafloxacin Levofloxacin *
Indications for fluoroquinilones administrationIndications for fluoroquinilones administration
Drugs of І choiceDrugs of І choice
Acute attack of chronic Acute attack of chronic bronchitis bronchitis
Acute and chronic sinusitis Acute and chronic sinusitis MMaalignant otitislignant otitis Hospital pneumoniaHospital pneumonia Pneumonia and bronchitis in Pneumonia and bronchitis in
patients with tuberculosispatients with tuberculosis Pneumonia in patients with Pneumonia in patients with
mucoviscidosismucoviscidosis Cholecystitis/ cholangitisCholecystitis/ cholangitis Chronic pielonephritisChronic pielonephritis Chronic prostatitisChronic prostatitis Bacterial diarrheaBacterial diarrhea Diarrhea of travellersDiarrhea of travellers
Alternative drugs
Acute medial otitisAcute medial otitis Community-acquiredCommunity-acquired
pneumoniapneumonia SepsisSepsis Intraabdominal infectionIntraabdominal infectionss OsteomOsteomyyelitiselitis Postoperative arthritisPostoperative arthritis Gynecological infectionGynecological infectionss
MeningitisMeningitis
Side effectsSide effects of of fluoroquinilonesfluoroquinilones
– photosensitization– seizures (if combined with
metronidazole, NSAIDs)– dyspeptic disorders– changes of mood, insomnia,
depression– allergic reactions– ulcerations of cartilages in children
and teenagers
Fluoroquinolones are contraindicated:
- for pregnant women- in lactation period - for children and
teenagers
Classification of sulfonamides(according to level of absorbtion in gastro-intestinal
tract and systemic action)
Drugs of resorbtive action: most of sulfonamides
Drugs which act in intestinal cavity:
phthalazole, sulgin, phthazin
Drugs for local administration:
sulfacyl-sodium, silver sulfazine, mafenide
Classification of sulfonamides(accordingly to duration of action)
Short action: streptocid, sulfadimezine, aethazole, norsulfazole, urosulfan, sulfizoxazole, sulfacyl-sodium
Medium duration of action: sulfamethoxazole (is a part of co-trimoxazole)
Longlasting action: sulfadimethoxyn, sulfapirydazin, sulfamonomethoxyn
Super longlasting action: sulfalen, sulfadoxyn (is a part of fansidar)
Indication for sulfonamides administration
Local 1. eye infections – trachoma, blennorrhea (sulfacyl-Na) 2. burns, wounds (silver salts, mafenide)
Orally 1. intestinal contamination (ftalazole 8-15g/daily 4-6 days) 2. chronic inflammatory diseases of intestines (salazo-substances) 3. nocardiosis (pneumonia, brain abscess), malaria (fansidar) 4. infections of urinary tracts – their primary treatment, chlamidia
infections 5. rarely – infections of respiratory tracts, LOR-infections, dysentery 6. herpetiform dermatitis of During (sulfapyridine)
Parenteral Sulfacyl-Na i.v.
Indications for co-trimoxazole administration
Pneumcystic pneumonia (children, patients with AIDS)
Pneumonia caused by Н. Influenzae, S. pneumoniae, Legionella pneumophila
Gonococcal urethritis, prostatitis, oropharyngeal gonorrhea
Urological and genital infections caused by sensitive E. coli, Proteus mirabilis, Salmonella typhi, Shigella
Gastro-intestinal infections (shigellosis, salmonellosis, hostage of Salmonella typhi)
Co-trimoxazole
480 - for adults 960 - for adults 120 – for children 240 – for children
Orally 2 times daily
Side effects of sulfonamidesSide effects of sulfonamides
Allergic reactions (rash, sometimes - Allergic reactions (rash, sometimes - multiform erythema)multiform erythema)
CrystalCrystallluriauria ( (kidney colic, anuriakidney colic, anuria)) Leukopenia, agranulocytosis, aplastic Leukopenia, agranulocytosis, aplastic
anemia, hemolytic anemia (in case of anemia, hemolytic anemia (in case of glucose-6-phosphate insufficiency of glucose-6-phosphate insufficiency of erythrocytes)erythrocytes)
Dysbacteriosis, superinfectionDysbacteriosis, superinfection
SlightSlight diuretic and hypoglycemic effects diuretic and hypoglycemic effects