ANTIBIOTICOTERAPIA -...
Transcript of ANTIBIOTICOTERAPIA -...
ANTIBIOTICOTERAPIA
Pierluigi Viale Clinica di Malattie Infettive Policlinico S. Orsola – Malpighi
SEPSI ed INFEZIONI in GRAVIDANZA Bologna, 17-18 ottobre 2014
1846 Ignazio Filippo Semmelweiss descrive la
catena epidemiologica della sepsi puerperale
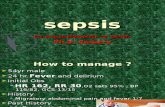
sepsis is a clinical event not a microbiologically defined disease
the term sepsis is not a synonymous of bacteremia or septicemia
From a clinical point of view the term sepsis represents an attempt to graduate the clinical severity of an infection in a single patient
Sepsis is the systemic maladaptive response of the host organism to the invasion of normally sterile tissue, fluid or body cavity by pathogenic or potentially pathogenic microorganisms. The culmination of complex interactions between the infecting microorganism and the host immune, inflammatory and coagulation responses influences the outcome in sepsis. Until recently, sepsis was regarded as a condition of hyper-inflammation and hyper-coagulation resulting in cellular damage and macrocirculation/ microcirculation derangement. Cinel I and Dellinger RP Curr Op Infect Dis 2007, 20:345–352
WHAT IS SEPSIS ?
The principles followed in elaborating the definitions were that: 1.infectious (and some non-infectious) processes, whatever their
cause, elicit a common systemic response which, although of variable intensity, is the expression of common patho-physiologic pathways resulting from the expression and interaction of various humoral and cellular mediators and cytokines;
2.There is a continuum between the various stages of this response
to infection sepsis severe sepsis septic shock MOF with an increased risk of mortality.
The SIRS concept SCCM/ACCP 1992
WHAT IS SEPSIS ?
SEVERE SEPSIS
SEPSIS
T° > 38.3 / < 36°C
pulse rate > 90 beats/minute
respiratory rate > 20 breaths/min
WBC > 12.000 / < 4.000/mmc
glycemia > 120 mg/dL
lactemia > 2 mmol/L
plasma C-reactive protein >2 SD above the normal value
plasma procalcitonin > 2 SD above the normal value
refilling > 2 seconds
altered mental status
hypotension (systolic < 90 mmHg)
lactemia > 4 mmol/L
organ disfunction/s
hypotension despite 20-40 ml/kg 1^h
SEPSIS DEFINITION
SEPTIC SHOCK
SIRS + infection
Identifying Acute Organ Dysfunction as a Marker of Severe Sepsis
Tachycardia Hypotension
CVP
Jaundice Enzymes Albumin
PT
Altered Consciousness Confusion Psychosis
Tachypnea PaO2 <70 mm Hg
SaO2 <90% PaO2/FiO2 300
Oliguria Anuria
Creatinine
Platelets PT/APTT D-dimer
Metabolic acidosis
Angus DC et al. Crit Care Med. 2001
organ dysfunction /s
Laboratories that will suggest organ dysfunction include …
PaO2 (mm Hg)/FiO2 <300,
Creatinine >2.0 mg/dL or Creatinine increase >0.5 mg/dL,
INR> 1.5,
PTT> 60 seconds,
Platelets < 100,000/mL,
Total bilirubin> 4 mg/dL,
Glasgow Coma Scale score < 13,
Serum lactate as a predictor of mortality in patients with infection TrzeciaK S et al, Intensive Care Med, 2007
A post-hoc analysis of a prospectively compiled registry in an urban academic hospital in patients with a primary or secondary diagnosis of infection
Acute-phase deaths and in-hospital deaths in infected patients stratified by initial lactate value.
Nationwide trends of severe sepsis in the twenty first century (2000-2007) Kumar G et al, Chest, 2011
from 143 in 2000 to 343 in 2007
Infective risk
Infection
Infection + SIRS
Severe sepsis
Septic shock
MANAGEMENT of THE SEPTIC SYNDROME
Prophylaxis
Immunostimulation
Antibiotics
Elimination of infective focus
TNF - IL1 - IL8
IL 6 - IL10 Antioxidants
Coagulation Inibithors
Etiological therapy
Etiological therapy
“Supportive” therapy
Pathogenetical therapy
Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department Gaieski DF et al, Crit Care Med 2010; 38:1045–1053
The epidemiology of adults with severe sepsis and septic shock in Scottish emergency departments. Gray A et al, Emerg Med J 2012 Jun 29
The epidemiology of adults with severe sepsis and septic shock in Scottish emergency departments. Gray A et al, Emerg Med J 2012 Jun 29
Sepsis resuscitation bundle compliance
55
29
66
48
%
LACTATE MEASUREMENT
BLOOD CULTURE TAKEN
ATB WITHIN 3 H
FLUID RESUSCITATION WHEN SBP < 90 mmHg
MORTALITY 28.3%
SEPSIS TEAM for patients admitted to ED with a diagnosis > severe sepsis
obsevational phase: The first 200 cases
Sepsis resuscitation bundle compliance
55
29
66
48
%
LACTATE MEASUREMENT
BLOOD CULTURE TAKEN
ATB WITHIN 3 H
FLUID RESUSCITATION WHEN SBP < 90 mmHg
MORTALITY 28.3%
MORTALITY 31.3%
The results demonstrate relatively low mortality rates among ICU patients with severe sepsis/septic shock, as compared to reports from outside Scandinavia. Early adequate antibiotic treatment and the low incidence of resistant isolates may partly explain these findings.
The day 28, hospital, and 1-year mortality rates were 19, 29, and 34%, respectively. 93% of the patients received adequate antibiotics from the beginning. Multi-resistant bacteria were only found in three cases (out of 101 patients). Among the 43 patients admitted to the ICU through the ED, the median time to antibiotics was 86 min (interquartile range 52–165), and overall 77% received appropriate antibiotics within 2 h.
Short- and long-term mortality in severe sepsis/septic shock in a setting with low antibiotic resistance: a prospective observational study in a Swedish university hospital. Linnér A, et al, Front Public Health. 2013;1:51.
On logistic regression, the OR for mortality in all patients with severe sepsis was 0.49 (95% CI, 0.46-0.52) in 2012 using 2000 as reference
Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012.Kaukonen KM et al, JAMA 2014;311:1308-16.
THE EQUATION OF THE INFECTIOUS RISK
BACTERIAL LOAD x VIRULENCE
HOST IMMUNITY
= INFECTIOUS RISK
+ DRUG RESISTANCE
HOST IMMUNITY
= INFECTIOUS RISK
DEATHS
COSTS
SUPERBUGS
Addressing the continued emergence of antibiotic resistance through the discovery of new drugs is not a sustainable strategy, particularly as antibiotics are increasingly more difficult and costly to develop. Thus, it is essential that we preserve the utility of existing antibiotics.
THE HISTORY OF MEDICINE
2000 BC Here, eat this root
1000 AD That root is heathen. Here, say this prayer
1850 AD That prayer is superstition. Here, drink this potion
1920 AD That potion is snake oil. Here, swallow this pill
1945 AD That pill is ineffective. Here, take this penicillin
1955 AD Oops, bugs mutated. Here take this tetracycline
1960-99 AD 39 more “oops”-
Here take this more powerful antibiotic
2000s AD We ran out of antibiotics! Here, eat this root
The ESKAPE trust
Bacterial clones that:
• retain a notable propensity for cross-transmission and spreading (low impact of resistance on fitness)
• play a relevant role in infections and in the dissemination of resistant determinants (high epidemiological risk)
• have acquired multiple resistance determinants (MDR/XDR phenotypes)
• are associated to significant morbidity and mortality (high clinical risk)
Woodford et al - FEMS Microbiol Rev 2011
The ESKAPE & company era : MAIN CHALLENGES
THE PERSISTENT CHALLENGE OF ENTEROCOCCUS SPP
THE VANCO MIC CREEP OF STAPHYLOCOCCUS AUREUS
THE OMINOUS SPREAD OF KPC KLEBISELLA PNEUMONIAE
THE MDR ACINETOBACTER REBUS
THE INCREASING INCIDENCE of MDR PSEUDOMONAS AERUGINOSA
THE EXPLOSION OF ESBL ENTEROBACTERIACEAE
THE CHALLENGING EPIDEMIOLOGY OF CLOSTRIDIUM DIFFICILE
THE GROWING EPIDEMIOLOGICAL BURDEN of CANDIDA spp.
Antibiotic start 1
• Empirical antibiotics should be started immediately following the diagnosis of SBP (Level A1).
Drug 2
• Since the most common causative organisms of SBP are Gram-negative aerobic bacteria, such as E. coli, the first line antibiotic treatment are third-generation cephalosporins . Alternative options include amoxycillin/clavulanic acid and quinolones such as ciprofloxacin or ofloxacin. However, the use of quinolones should not be considered in patients who are taking these drugs for prophylaxis against SBP, in areas where there is a high prevalence of quinolone-R bacteria or in nosocomial SBP (Level B1).
Management 3
SBP resolves with antibitic therapy in approximately 90% of patients. Resolution of SBP should be proven by demonstrating a decrease of ascitic neutrophil count to <250/mm3 and sterile cultures of ascitic fluid, if positive at diagnosis (Level A1). A second paracentesis after 48 h of start of treatment may help guide the effect of antibiotic therapy
EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis
0
10
20
30
40
50
60
EB SA EC Candida GNR
Pre
vale
nce (
%)
7%
34%
44%
15%
pan S
ESBL
Q-R
KPC
Etiology distribution and Prevalence of Sensitive Strains
Epidemiology and Outcomes of Bloodstream Infection In Patients with Cirrhosis Bartoletti M et al, J Hepatol 2014, Mar 26
Adjusted HR 0.37 (0.20-0.70)
P =0.002
Adequate antibiotic therapy
within 24 hours (n=100)
Inadequate antibiotic therapy
within 24 hours (n=62)
0.00
0.10
0.20
0.30
0.40
0.50
0.60
0.70
0.80
0.90
1.00 S
urv
iva
l P
rob
ab
ility
0 5 10 15 20 25 30
Days after positive blood culture
Impact of inadequate antimicrobial therapy in the first 24 hours on survival
Epidemiology and Outcomes of Bloodstream Infection In Patients with Cirrhosis Bartoletti M et al, J Hepatol 2014 , March 26
The ESKAPE & company era : MAIN CHALLENGES
THE PERSISTENT CHALLENGE OF ENTEROCOCCUS SPP
THE VANCO MIC CREEP OF STAPHYLOCOCCUS AUREUS
THE OMINOUS SPREAD OF KPC KLEBISELLA PNEUMONIAE
THE MDR ACINETOBACTER REBUS
THE INCREASING INCIDENCE of MDR PSEUDOMONAS AERUGINOSA
THE EXPLOSION OF ESBL ENTEROBACTERIACEAE
THE CHALLENGING EPIDEMIOLOGY OF CLOSTRIDIUM DIFFICILE
THE GROWING EPIDEMIOLOGICAL BURDEN of CANDIDA spp.
The MULTIFACETED concept of APPROPRIATENESS
- RIGHT INDICATION (epidemiologically, microbiologically and PK/PD driven)
- RIGHT DAILY DOSE
- RIGHT MODALITY OF ADMINISTRATION, PREPARATION, STORAGE
- RIGHT PRESCRIBER
- SHARED CRITERIA FOR DE-ESCALATION / INTERRUPTION
- IMPROVEMENT OF MICROBIOLOGICAL WORK UP
PRINCIPALI DETERMINANTI DI EFFICACIA ANTIBIOTICA IN VIVO
AUC
• t > MIC
t > MIC
Concentrazione antibiotico (µg/mL)
Intervallo di dosaggio (ore)
Cmax
• Cmax / MIC
MIC (µg/mL)
1000 mg BID 500 mg QID Con
cent
razione
ant
ibiotico
(µg/
mL)
0 12 24 36 48
30
25
20
15
10
5
0
35 2000 mg IC
Cmin
ANTIBIOTICO TEMPO DIPENDENTE IN UN SOGGETTO CON FUNZIONE RENALE CONSERVATA
Bacterial stasis
Maximal bactericidal effect
Mutant prevention
30%
50%
100%
Concept of clinical impact of T>MIC: beta-lactams
1000 mg OD 500 mg BID Con
cent
razione
ant
ibiotico
(µg/
mL)
0 24 48 72 96
30
25
20
15
10
5
0
35
Cmax
MIC
GENTAMICINA IN UN SOGGETTO GIOVANE CON FUNZIONE RENALE CONSERVATA
LD = Vd x CTARGET
Il concetto di “DOSE da CARICO”
Quanto più lunga è l’emivita di un farmaco tanto più importante è la dose da carico !
> 3 L > 3 L > Vd = 3 % > Vd = 25 %
12 L
100 L
ANTIBIOTICI IDROFILI
ANTIBIOTICI LIPOFILI
VD E CONDIZIONI FISIOPATOLOGICHE
VARIATIONS OF EXTRACELLULAR FLUID
VARIATIONS OF RENAL CLEARANCE
Dilution or loss of antibiotic
Consider
DOSAGE INCREASE
Enhanced antibiotic renal excretion
Consider
DOSAGE INCREASE
RENAL IMPAIRMENT
AGING DYALISIS
Decreased if
Reduced antibiotic renal excretion
Consider
DOSAGE DECREASE
DRUG ABUSE
HAEMODYNIMICALLY ACTIVE DRUGS
BURNS
LEUKEMIA
HYPERDYNAMICS
Increased if
HYPOALBUMINAEMIA
PLEURAL EFFUSION
FLUID THERAPY
ASCITES
OEDEMA
MEDIASTINITIS
DRAINAGES
Increased if
HYPOALBUMINAEMIA
Critically ill patients
Antimicrobial therapy in the critically ill patients: a review of those pathophysiological conditions responsible for huge pk variability Pea F, Viale P, Clin Pharmacokinet 2005;44:1009-34
Impact of Antimicrobial Stewardship Intervention on Coagulase- Negative Staphylococcus Blood Cultures in Conjunction with Rapid Diagnostic Testing.
Nagel JL et al, J. Clin. Microbiol. 2014, 52:2849
Impact of Antimicrobial Stewardship Intervention on Coagulase- Negative Staphylococcus Blood Cultures in Conjunction with Rapid Diagnostic Testing.
Nagel JL et al, J. Clin. Microbiol. 2014, 52:2849
single-center, quasi-experimental study. Adult patients with a CoNS blood culture identified via MALDI-TOF over a 3-month period were compared to a historical control group with CoNS identified by conventional methods . Patients were divided into 4 categories: Pts with CoNS BSI before/after implementation of MADLI-TOF plus AST intervention Pts with CoNS contamination before/after MADLI-TOF plus AST intervention During the preintervention study period, prescribers were immediately notified of positive Gram stain results from blood cultures. The AST did not intervene for positive bacterial cultures in real time but AST reviewed daily reports from Monday through Friday for all patients receiving restricted antimicrobials and recommended therapy changes on the basis of institutional guidelines and clinical judgment. Between the patients for whom changes were recommended may have included patients with blood cultures positive for CoNS. All stewardship activities, except for the addition of real-time alerts for positive blood cultures during the intervention period, remained unchanged during the study time frame.
Impact of Antimicrobial Stewardship Intervention on Coagulase- Negative Staphylococcus Blood Cultures in Conjunction with Rapid Diagnostic Testing.
Nagel JL et al, J. Clin. Microbiol. 2014, 52:2849
OUTCOMES – CoNS bacteremia
Impact of Antimicrobial Stewardship Intervention on Coagulase- Negative Staphylococcus Blood Cultures in Conjunction with Rapid Diagnostic Testing.
Nagel JL et al, J. Clin. Microbiol. 2014, 52:2849
OUTCOMES – CoNS contamination
Frequency of different ESKAPE pathogens in VAP in different geographical locations
Curr Opin Pulm Med 2012, 18:187–193
late 2008
KPC-producing K. pneumoniae of Clonal Complex 11
early 2011 late 2012
The first reported cases
of KPC-Kp
ST258
ST258, ST512 ST512
ST258
Clinical epidemiology of the global expansion of K.pneumoniae carbapenemases Munoz-Price LS et al Lancet Infect Dis 2013;13:785–96
ITALIAN STUDY GROUP on KPC-producing Klebsiella pneumoniae infections
Catholic University of the Sacred Heart,
A. Gemelli Hospital - ROME
Mario Tumbarello, Enrico Maria Trecarichi, Teresa Spanu
Angela Raffaella Losito, Francesca Raffaelli, Roberto Cauda
University of Bologna
S. Orsola-Malpighi Hospital - BOLOGNA
Pierluigi Viale, Fabio Tumietto
Francesco Cristini, Maddalena Giannella
Michele Bartoletti, Sara Tedeschi
Simone Ambretti
University of Genoa and
IRCCS San Martino-IST – GENOA
Claudio Viscoli, Valerio Del Bono
Carolina Saffioti, Anna Marchese
University of Turin
Amedeo di Savoia Hospital - TURIN
Francesco Giuseppe De Rosa, Silvia Corcione, Nicole Pagani, Chiara Simona Cardellino
Santa Maria Misericordia University Hospital - UDINE
Matteo Bassetti
Analysis to December 2013 (661 patients)
• Patients with KPC Kp infections had an overall in-hospital mortality rate of 41.1% [273/661]
• 14 day mortality was 34.1 (225/661)
• Peak rates occurred in the subgroup with KPC Kp BSIs (173/447, 38.7% vs. 52/214, 24.3%, of those with other types of infection).
ITALIAN STUDY GROUP on KPC-producing Klebsiella pneumoniae infections
In-hospital mortality of 447 patients with KPC Kp BSIs
51.3% (80 of 156 patients) for monotherapy
32.0% (93 of 291 patients) for combo regimens
(P < 0.001)
ITALIAN STUDY GROUP on KPC-producing Klebsiella pneumoniae infections
Infection control measures for Gram neg colonized patients
- Hand hygiene
- Physical separation of patients
- Education
- Detection/surveillance
- Environmental cleaning
- Cohort patients’ and staff
- Antimicrobial stewardship
- Multifaceted approaches
ESCMID/SHEA guidelines Clin Microbiol Infect 2014;20 suppl 1: 1-55
La Gestione del rischio infettivo in Emilia-Romagna il nuovo assetto organizzativo
Nucleo Strategico
Nucleo Operativo per il controllo
delle ICA
Nucleo Operativo per l’uso
responsabile di antibiotici
DELIBERAZIONE DELLA GIUNTA REGIONALE 25 MARZO 2013, N. 318 Linee di indirizzo alle Aziende per la gestione del rischio infettivo: infezioni correlate
all’assistenza e uso responsabile di antibiotici
Comitato Infezioni Ospedaliere
Donskey CJ and Eckstein BC New England Journal of Medicine January 15, 2009
After visiting an MRSA carrier After cleaning with alcohol foam
Clinical epidemiology of carbapenem-intermediate or –resistant Enterobacteriaceae Patel N et al, J Antimicrob Chemother 2011; 66: 1600–1608
Methods: A case–control study. Cases were adults with a culture-confirmed infection with reduced susceptibility to meropenem or ertapenem. The cases were matched 1:1 to patients from two different control series: (i) those with carbapenem-susceptible Enterobacteriaceae (CSE) infections; and (ii) inpatients residing on the same ward within 30 days of CIRE culture date. Results: There were 102 cases of CIRE during the study period. The only covariate independently associated with CIRE in all multivariate analyses was the cumulative number of prior antibiotic exposures. Compared with CSE controls, the odds ratios (95% confidence interval) were 1.43 (1.19–1.72), 2.05 (1.70–2.47) and 2.93 (2.43–3.53) for 1, 2 and ≥3 antibiotic exposures, respectively. The strength of this association was comparable for the hospitalized control group and analyses stratified by organism and presence of the blaKPC gene.
Predictive Models for Identification of Hospitalized Patients Harboring KPC-Producing K. pneumoniae. Tumbarello M at al Antimicrob Ag chemother 2014, april 14
To identify factors that could predict isolation of KPC-Kp in clinical samples from hospitalized patients, a retrospective, matched (1:2) case-control studies in five large Italian hospitals (Rome, Bolonia, Turin, Genoa, Udine) was conducted. For each case enrolled, we randomly selected two matched controls with no KPC-Kp-positive cultures of any type during their hospitalization. Matching involved hospital, ward, and month/year of admission, as well as time at risk for KPC-Kp isolation. A subgroup analysis was also carried out to identify risk factors specifically associated with true KPC Kp infection . During the study period, 668 patients in participating hospitals had at least one clinical culture positive for KPC Kp. Eleven cases were excluded because of missing data. Four hundred twenty-six (64.8%) of the remaining 657 cases were classified as true infections.
Predictive Models for Identification of Hospitalized Patients Harboring KPC-Producing K. pneumoniae. Tumbarello M at al Antimicrob Ag chemother 2014, april 14
Logistic regression analysis of risk factors for KPC Kp strain isolation or infection
Antimicrobial Stewardship: DEFINITIONS
An activity that optimizes antimicrobial management and includes selection, dosing, route and duration of antimicrobial therapy.
A marriage of infection control (Epidemiologist), and antimicrobial management (Infectious Diseases specialist) finalized to share the principles of the optimized treatment between the bench to bed side point of view and the hospital-wide vision
Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Dellit TH, et al. Clin Infect Dis 2007; 44:159–177
How to lay out a stewardship program ?
-Hospital wide
-Drug directed
-Setting directed
-Disease directed
-the consumptions of antimicrobials
-the consumptions & the appropriateness of selected drugs
-the main management principles of antimicrobial treatments
-the management principles of selected diseases
THE HISTORICAL PERIODS of ANTIMICROBIAL STEWARDSHIP
The MIDDLE AGE
COMPULSORY PROGRAMS
The REINASSANCE
SEMI-COMPULSORY PROGRAMS (post prescription reviews)
The NEXT FUTURE
SHARED NEW PARADIGMS for MANAGEMENT
PROBLEM-DRIVEN PROTOCOLS and PROGRAMS
6.
There are 2 core strategies, both proactive, that provide the foundation for an
antimicrobial stewardship program. These strategies are not mutually exclusive.
A. Prospective audit with intervention and feedback. Prospective audit of antimicrobial use with direct interaction and feedback to the prescriber, performed by either an infectious diseases physician or a clinical pharmacist with infectious diseases training, can result in reduced inappropriate use of antimicrobials (A-I).
B. Formulary restriction and preauthorization. Formulary restriction and preauthorization requirements can lead to immediate and significant reductions in antimicrobial use and cost (A-II) and may be beneficial as part of a multifaceted response to a nosocomial outbreak of infection (B-II). The use of preauthorization requirements as a means of controlling antimicrobial resistance is less clear, because a long-term beneficial impact on resistance has not been established, and in some circumstances, use may simply shift to an alternative agent with resulting increased resistance (B-II).
Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Dellit TH, et al. Clin Infect Dis 2007; 44:159–177
THE GOAL IS THE APPROPRIATENESS of the prescriptions not only the costs saving
A marriage of infection control (Epidemiologist) and antimicrobial management (Infectious Diseases specialist) finalized to share the principles of the optimized treatment between the bench to bed side point of view and the hospital-wide vision
Checking the quality instead of the quantity
The MULTIFACETED concept of APPROPRIATENESS
- RIGHT INDICATION (epidemiologically, microbiologically and PK/PD driven)
- RIGHT DAILY DOSE
- RIGHT MODALITY OF ADMINISTRATION
- RIGHT PRESCRIBER
- SHARED CRITERIA FOR DE-ESCALATION / INTERRUPTION
- IMPROVEMENT OF MICROBIOLOGICAL WORK UP
Transforming the hospital formulary in a true clinical instrument ! From the formulary to a shared management guidelines
Antimicrobial stewardship programs: the devil is in the details Cunha CB et al, Virulence 2013; 4: 147–149
Antimicrobial stewardship is a developing field, and every program must
be tailored to its respective institution / unit and each article has a
distinctive focus and perspective.
S. Orsola-Malpighi Teaching Hospital – A PRESENT TOWARDS THE FUTURE
- SESPIS TEAM - PNEUMONIA TASK FORCE - BUNDLE FOR THE MANAGEMENT OF CANDIDEMIA - BD GLUCAN DRIVEN DE-ESCALATION OF EMPIRICAL ANTIFUNGAL TX - AMBIHOW PROTOCOL - SCORE /CTPA DRIVEN ANTIMOLDS Tx FOR POSSIBLE INFECTIONS - CORRECT PCT USE
NEW PARADIGMS OF MANAGEMENT FOR SPECIFIC PROBLEMS
ongoing the interventional phase ongoing observational phase ongoing under submission to Ethical Committee ongoing multidisciplinary discussion ongoing ongoing (40% reduction of requests)
Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department Gaieski DF et al, Crit Care Med 2010; 38:1045–1053
The epidemiology of adults with severe sepsis and septic shock in Scottish emergency departments. Gray A et al, Emerg Med J 2012 Jun 29
The epidemiology of adults with severe sepsis and septic shock in Scottish emergency departments. Gray A et al, Emerg Med J 2012 Jun 29
Sepsis resuscitation bundle compliance
55
29
66
48
%
LACTATE MEASUREMENT
BLOOD CULTURE TAKEN
ATB WITHIN 3 H
FLUID RESUSCITATION WHEN SBP < 90 mmHg
MORTALITY 28.3%
SEPSIS TEAM for patients admitted to ED with a diagnosis > severe sepsis
a quasi-experimental study
ED EVALUATION
Severe sepsis/septic shock diagnosis
RESUSCITATORY BUNDLE
+
ID EVALUATION (within 20’)
DIAGNOSTIC and
THERAPEUTIC MANAGEMENT
ED EVALUATION
Severe sepsis/septic shock diagnosis
RESUSCITATORY BUNDLE
+
DIAGNOSTIC and
THERAPEUTIC MANAGEMENT
STUDY ARM
S. Orsola H
CONTROL ARM
Maggiore H
SEPSIS TEAM for patients admitted to ED with a diagnosis > severe sepsis
obsevational phase: The first 200 cases
Sepsis resuscitation bundle compliance
55
29
66
48
%
LACTATE MEASUREMENT
BLOOD CULTURE TAKEN
ATB WITHIN 3 H
FLUID RESUSCITATION WHEN SBP < 90 mmHg
MORTALITY 28.3%
MORTALITY 31.3%
PROCALCITONIN – three working fields - Diagnostic marker
- Prognostic marker
- Stewardship instrument
Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Schueltz P et al Clin Infect Dis 2012; 55:651–662
Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Schuetz P, et al Cochrane Database Syst Rev 2012; 9:CD007498.
Outcomes associated with PCT monitoring in ICU studies
Procalcitonin for reduced antibiotic exposure in the critical care setting: A systematic review and an economic evaluation Heyland DK et al, Crit Care Med 2011; 39
Effect of procalcitonin-guided therapy on duration of antibiotic utilization
Procalcitonin for reduced antibiotic exposure in the critical care setting: A systematic review and an economic evaluation Heyland DK et al, Crit Care Med 2011; 39
Effect of procalcitonin-guided therapy on hospital mortality
Procalcitonin for reduced antibiotic exposure in the critical care setting: A systematic review and an economic evaluation Heyland DK et al, Crit Care Med 2011; 39
Base case cost-minimization analyses
Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial Jensen JU et al Crit Care Med 2011; 39:
Design: Randomized controlled open-label trial.
Setting: Nine multidisciplinary intensive care units across Denmark.
Patients: A total of 1200 critically ill patients were included and randomized either to
the “standard- of-care-only arm,” receiving treatment according to the current
international guidelines and blinded to procalcitonin levels, or to the “procalcitonin
arm,” in which current guidelines were supplemented with a drug-escalation algorithm
and intensified diagnostics based on daily procalcitonin measurements.
Primary End Point: to determine whether the prompt availability of procalcitonin levels
and a corresponding, obligatory guideline for antimicrobial interventions would result
ininitiation of appropriate antimicrobial therapy earlier in infected critically ill patients
and thus improve 28-day survival compared with standard clinical judgment unenhanced
by available procalcitonin levels
Secondary End Points: whether the procalcitonin guided strategy would lead to a
shorter duration of organ failure or a shorter stay in the intensive care unit
Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial Jensen JU et al Crit Care Med 2011; 39:
Methods :In the procalcitonin group, the use of antimicrobial interventions was guided by the same clinical guidelines as in the standard-of-care-only group and additionally by daily procalcitonin measurements classified as “alert procalcitonin” or “nonalert procalcitonin” with a corresponding obligatory intervention algorithm. “Alert procalcitonin” was defined as a procalcitonin 1.0 ng/mL that was not decreasing at least 10% from the previous day. At baseline, a single procalcitonin measurement of 1.0 ng/mL was considered to be “alert procalcitonin.” Whenever an “alert procalcitonin” occurred, the intervention principles were 1) to substantially increase the antimicrobial spectrum covered and 2) to intensify the diagnostic effort to find uncontrolled sources of infection. The new concept was represted by the indication to start or escalate antimcrobial therapy in situations in which, according to the hypothesis, uncontrolled infection was developing in a clinical picture not clearly indicating therapy shift.
“Alert procalcitonin” at baseline was an independent predictor of 28- day all-cause mortality (OR 1.4; 95% CI 1.1– 1.9) In a logistic regression model, the risk of having severe sepsis or septic shock on day 5 increased with the number of “alert PCT” within the first 5 days (OR no “alert PCT,” 1.0 [reference]; one “alert PCT,” 2.2; 95% CI, 1.2– 4.1; two or more “alert PCT,” 3.0; 95% CI, 1.9–4.8).
Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial Jensen JU et al Crit Care Med 2011; 39:
Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial Jensen JU et al Crit Care Med 2011; 39:
SOC PCT driven p
number (%) intensive care unit days spent with at least three antimicrobials
2721 (57.7%) 3570 (65.5%) .002
mean time to appropriate antimicrobials
(overall) 0.4 days 0.2 days NS
mean time to appropriate antimicrobials (BSI) 0.8 days 0.1 days .02
Culture performed 6641 7874 NS
days spent on mechanical ventilation, 2,861 3,569 .001
median ICU admission length 5 6 .005
Secondary Outcomes
Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial Jensen JU et al Crit Care Med 2011; 39:
Primary outcome Kaplan-Meier estimates of 28-day survival
A strategy with escalation of broad spectrum antimicrobials in the
intensive care unit guided by daily procalcitonin measurements as used
in this trial did not improve survival and did lead to an increased use
of broad-spectrum antimicrobials.
Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial Jensen JU et al Crit Care Med 2011; 39:
Early assessment of pancreatic infections and overall prognosis in severe acute pancreatitis by procalcitonin (PCT): a prospective international multicenter study Rau BM et al, Ann Surg. 2007;245:745-54
A total of 104 patients with predicted severe AP were enrolled in five European academic surgical centers within 96 hours of symptom onset. PCT and CRP were measured over a maximum of 21 consecutive days and in weekly intervals thereafter
A PCT value of > 3.5 ng/mL on 2 consecutive days was superior to CRP > 430 mg/L for the assessment of infected necrosis with MODS or nonsurvival as determined by ROC analysis with a sensitivity and specificity of 93% and 88% for PCT and 40% and 100% for CRP, respectively (P < 0.01). The single or combined prediction of the two major complications was already possible on the third and fourth day after onset of symptoms with a sensitivity and specificity of 79% and 93% for PCT > 3.8 ng/mL compared with 36% and 97% for CRP > 430 mg/L, respectively (P = 0.002).
PCT CRP
Early assessment of pancreatic infections and overall prognosis in severe acute pancreatitis by procalcitonin (PCT): a prospective international multicenter study Rau BM et al, Ann Surg. 2007;245:745-54
Impact of Rapid Organism Identification via Matrix-Assisted Laser Desorption / Ionization Time-of-Flight Combined With Antimicrobial Stewardship Team Intervention in Adult Patients With Bacteremia and Candidemia. Huang AM et al Clin Infect Dis 2013; 57: 1237-45
A pre–post quasi-experimental study was conducted to analyze the impact of MALDI-TOF with AST intervention in patients with bloodstream infections. The AST provided evidence based antibiotic recommendations after receiving real-time notification following blood culture Gram stain, organism identification, and antimicrobial susceptibilities. Outcomes were compared to a historic control group. A total of 501 patients with bacteremia or candidemia were included in the final analysis: 245 patients in the intervention group and 256 patients in the pre-intervention group
Impact of Rapid Organism Identification via Matrix-Assisted Laser Desorption / Ionization Time-of-Flight Combined With Antimicrobial Stewardship Team Intervention in Adult Patients With Bacteremia and Candidemia. Huang AM et al Clin Infect Dis 2013; 57: 1237-45
Outcomes
The 2005 ATS/IDSA guidelines for nosocomial pneumonia defined healthcare-
associated pneumonia (HCAP) as including patients who had recent contact with
healthcare environments through nursing homes, hemodialysis centers, or recent
hospitalization, distinguished from CAP because of higher prevalence of drug
resistant pathogens, recommending that all patients with HCAP be treated
empirically with multiple antibiotics, directed against multidrug resistant
microorganisms.
NHAP
Dialysis
Previous hospitalization
Antibiotics
Infusions
Immunosuppression
MDR
HCAP: what you get is what you put in
HCAP = HAP Aggressive broad spectrum therapy LINEZOLID + CARBAPENEM
HCAP = hospitalized CAP?
Standard CAP therapy
AMPICILLIN-SBC + MACROLIDE
Risk Factors for Drug-Resistant Pathogens in CAP and HCAP Shindo Y et al, Am J Respir Crit Care Med 2013; 188:985–995
A prospective observational study conducted in hospitalized patients with pneumonia at ten institutions in Japan. Pathogens identified as not susceptible to ceftriaxone, ampicillin-sulbactam,macrolides,and respiratory fluoroquinolones were defined as drug resistant pathogens (DRP). In total, 1,413 patients (887 CAP and 526 HCAP) were analyzed.
Identified pathogens (770/1413) according to type of pneumonia: THE TOP THREE
%
Risk Factors for Drug-Resistant Pathogens in CAP and HCAP Shindo Y et al, Am J Respir Crit Care Med 2013; 188:985–995
Variable OR 95% CI
prior hospitalization 2.06 1.23–3.43
immunosuppression 2.31 1.05–5.11
previous antibiotic use 2.45 1.51–3.98
use of gastric acid suppressive agents 2.22 1.39–3.57
tube feeding 2.43 1.18–5.00
non-ambulatory status 2.45 1.40–4.30
DRPs were more frequently found in patients with HCAP (26.6%) than in patients with CAP (8.6%)
Independent risk factors for DRP
Risk Factors for Drug-Resistant Pathogens in CAP and HCAP Shindo Y et al, Am J Respir Crit Care Med 2013; 188:985–995
Number of risk factors for CAP drug resistance
35.9%
Risk Factors for Drug-Resistant Pathogens in CAP and HCAP Shindo Y et al, Am J Respir Crit Care Med 2013; 188:985–995
Outcomes according to type of pneumonia
HCAP CAP P % %
drug-resistant pathogens 8.6 26.6 <.001
Inappropriate initial antibiotic treatment 15.6 32.5 <.001
Mechanical ventilation 9.8 8.4 .366
30-d mortality 20.3 7.0 <.001
In-hospital mortality 24.9 10.0 .030
Building a prediction rule based on well defined Risk Factors and not on a simple disease definition, is possible
A New Strategy for Healthcare-Associated Pneumonia: A 2-Year Prospective Multicenter- Cohort Study Using Risk Factors for MDR Pathogens To Select Initial Empiric Therapy. Maruyama T et al, Clin Infect Dis 2013; 57:1373-83
multicenter cohort study of 445 pneumonia patients, including both CAP (n=124) and HCAP (n=321).
A New Strategy for Healthcare-Associated Pneumonia: A 2-Year Prospective Multicenter- Cohort Study Using Risk Factors for MDR Pathogens To Select Initial Empiric Therapy. Maruyama T et al, Clin Infect Dis 2013; 57:1373-83
microorganism
HCAP with 0-1 RF (n=151)
HCAP with >2 RF (n=170)
P % %
S. pneumoniae 39.1 27.6 .03
S. aureus 4.6 17.6 <.001
MRSA 0 12.9 .366
Enterobacteriaceae 2.6 12.4 .001
P. aeruginosa 2.0 11.2 .001
MDR gram negatives 2.0 27.1 <.001
CAUSATIVE MICROORGANISMS
In total, 93.1% of HCAP patients were treated according to the therapy algorithm, with only 53% receiving broad spectrum empiric therapy.
A New Strategy for Healthcare-Associated Pneumonia: A 2-Year Prospective Multicenter- Cohort Study Using Risk Factors for MDR Pathogens To Select Initial Empiric Therapy. Maruyama T et al, Clin Infect Dis 2013; 57:1373-83
30-DAY MORTALITY
In the subgroup with less than 2 RF the incidence of difficult to treat pathogens is low, justifying a conservative therapeutic approach