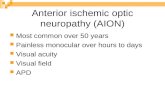
Anterior Ischemic Optic Neuropathy
-
Upload
sohan-singh -
Category
Documents
-
view
212 -
download
0
Transcript of Anterior Ischemic Optic Neuropathy

Anterior Ischemic Optic Neuropathy
VIII. Clinical Features and Pathogenesis of Post-hemorrhagic Amaurosis
SO HAN SINGH HAYREH, MD, PhD, DSc, FRCS
In memory of Paul Henkind, whose friendship I enjoyed and cherished
for a quarter of a century.
Abstract: Visual disturbance after marked andjor recurrent blood loss has been known for at least 25 centuries, since Hippocrates; however, so far its clinical features have been controversial and its pathogenesis enigmatic. The author studied seven patients, four of whom were seen soon after the visual loss and followed prospectively. A detailed review of the extensive literature and analysis of the cases provide relevant information on the subject. The blood loss is usually from the gastrointestinal (GI) tract, less often from other sites. There is typically a time lag between the bleeding and the onset of visual loss-usually up to 1 0 days, less often even 2 to 3 weeks. The ocular findings are typically those of anterior ischemic optic neuropathy (AION) and are usually bilateral. Considerable evidence has accumulated that blood loss, with or without arterial hypotension, causes increase in release of renin and endogenous vasoconstrictor agents (e.g., angiotensin , epinephrine, and vasopressin) because of activation of the sympathoadrenergic system and vasomotor center. Our experimental studies on renovascular malignant hypertension indicate that endogenous vasoconstrictor agents produce choroidal ischemia and AION. In view of all the evidence, it is postulated that in the production of AION after blood loss, release of endogenous vasoconstrictor agents is probably a very important factor, with arterial hypotension an additional factor; increased platelet aggregation may also play a role. [Key words: angiotensin, anterior ischemic optic neuropathy, blood loss, hemorrhage, ischemia, optic neNe, renin .] Ophthalmology 94:1488-1502, 1987
From the Department of Ophthalmology, University of Iowa, Iowa.
Presented in part at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Sarasota, May 8, 1987.
Supported by grant EY-1151 from the National Institutes of Health, and in part by an unrestricted grant from Research to Prevent Blindness, Inc.
Reprint requests to Sohan Singh Hayreh, MD, PhD, DSc, FRCS, Department of Ophthalmology, University of Iowa Hospitals and Clinics, Iowa City, lA 52242.
Almost 25 centuries ago, in a description ofthe "black disease," Hippocrates1 wrote ". . . the patient vomits black, bloody material . . . and he has pain in his head and does not see with his eyes. . . . " I have been able to trace about 600 cases of this condition (usually called posthemorrhagic amaurosis) recorded in the literature in hundreds of publications. It seems that the first definite case of this disease was reported by Nicholas Fon
1488

HAYREH • OPTIC NEUROPATHY
tanus2 in 1641 in his Collection ofRare Observations, describing the visual loss developed after therapeutic venesection. In 1781 , Truka de Krzowitz3 reviewed from the literature a large number of cases of visual loss after bleeding from different causes. Since then there have been many serial reviews. For example, in 1876 Fries4 reviewed 106 cases (reported during the previous 235 years); in 1904 Singer,5 198 cases (including those of Fries4); in 1912 Zentmayer,6 24 cases; in 1924 Harbridge,7 240 cases; in 1949 Locket,8 47 cases (reported from 1924 to 1947); and in 1955 Unger,9 286 cases (reported between 1941 and 1953). Since then, there have been many more case reports. Although hundreds of cases have been reported in hundreds of publications over the past 31h centuries, with few exceptions they are essentially anecdotal, retrospective case reviews, frequently with inadequate information on the various parameters required to understand the pathogenesis of the condition. It is no wonder that the mechanism of visual loss after distant systemic hemorrhage still remains an enigma, as do some other features of the disease. The case reports pose other problems in addition to their anecdotal and retrospective nature. For example, because the patients were severely ill with systemic disease and massive blood loss, and the visual loss was a secondary consideration (or even not appreciated by the patient during the acute illness), most ofthem were seen by ophthalmologists months or years after the visual loss. There was little or no information about the systemic condition (e.g., blood pressure [BP] and hematologic status) at the time of visual loss, nor about the ocular lesions during the acute phase of the disease and their evolution. When the patients were seen during the acute phase, the ophthalmoscopic findings were distorted by the preconceived notion that blood loss and retinal ischemia were the essential causes of this entity; or sometimes the findings were totally misinterpreted. The other important cause of confusion has been the constant mixing of at least two types of visual loss produced by massive systemic bleeding, i.e., one developing during the syncopal phase (accompanying or immediately after the hemorrhage, usually lasting for a few minutes and rarely longer), and the other, which usually occurs after an interval of several days or even weeks and rarely simultaneously. The former is transient and recovers without any treatment, whereas the latter type is almost always permanent with poor prognosis for recovery. In some of the cases, visual loss was wrongly attributed to blood loss; for example, in a young man with multiple sclerosis, visual loss 2 weeks after blood donation was attributed to blood loss10 whet} it may well have been due to retrobulbar neuritis; in another patiept with active giant-cell arteritis, bilateral optic nerve infarction was wrongly attributed to bleeding. II In still another example, blindness in one eye was attributed to blood loss after traumatic wounds, when in fact compression of the eyeball during surgery produced central retinal artery occlusion. 12 There are many other instances in which central retinal artery occlusion has been wrongly
attributed to massive bleeding. These are just three of many examples of mistaken diagnosis included in this group. Hence our difficulty in understanding the nature of this disease.
A wide variety of mechanisms has been postulated to explain visual loss after distant systemic hemorrhages. The primary site of the lesion, in the earlier literature, was thought to be the retina; however, it has been considered more recently to be the anterior part of the optic nerve, although a few authors postulated the involvement of higher visual pathways. It has been described as resulting from primary ischemia of the retina, 13- 22 focal anoxia of the retina,23 thrombotic foci causing degeneration and diffuse retinal edema,24 embolism or thrombosis of the central retinal artery,25·26 vasospasm or constriction of the retinal arteries, 19·20·27 central retinal vein thrombosis,28 optic atrophy owing to the combined effect of hemorrhage and toxemia, 15 edema and multiple hemorrhages in the optic nerve,29 retrobulbar optic neuritis,26·30 a lesion in the optic nerve just behind the lamina cribrosa, 14
31 ·23·24 ischemic fatty degeneration of the
optic nerve, hemorrhage into the optic nerve sheath,29·32 exudation into the sheath of the optic nerve with associated cerebral edema sufficient to produce compression of the vascular supply of the optic nerve and retina,33 hemodilution and hypoproteinemia leading to edema of the optic nerve and vascular compression,8 ischemia of the anterior part of the optic nerve secondary to extreme hypotension or to stenosis or embolism of the optic nerve branches from the ophthalmic artery,34 and thrombotic or embolic occlusion of vessels in the visual cortex or optic radiation. 35·36 The vascular changes and ischemia have been attributed by a majority of authors to anemia and/or arterial hypotension after hemorrhage, but others have postulated a variety of other causes, including endothelial damage owing to blood loss and thrombosis on damaged endothelium,37
changed consistency of the blood, 38 and endarteritis fibrosa.39 Its prevalence after repeated hemorrhages and the lapse of time between the hemorrhage and the visual loss was thought to suggest a possible role of some hemoclastic shock, anaphylactic crisis, toxemia owing to pro
15 27 35 40 5found hemolysis, or other unknown causes, · · · -4or autointoxication added to ischemia.46 There has also been speculation that visual loss is due to lack ofoxygen, similar to quinine amblyopia.20·47 Roe47 thought it was due to a combination of ischemia, acidosis, and the injudicious exposure of eyes to light. This extremely brief overview of the theories on pathogenesis of the visual loss after distant systemic hemorrhage reflects the extent of our ignorance on the subject.
During the past 8 years, at least seven patients, with visual loss after massive systemic hemorrhages, were referred to my Ocular Vascular Clinic at Iowa City. Four of them were referred during the acute phase, soon after the visual loss, and I was able to follow them in detail, prospectively, to gain a comprehensive understanding of the nature of the visual loss and its pathogenesis. The following are brief summaries of the four cases.
1489

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
CASE REPORTS
Case 1. A 61-year-old white man was fust seen in our clinic on March 20, 1981. Around March 7, 1981 he had vomited about I liter of blood-stained material and passed grossly bloody stool, and later he had melena. He was admitted to a local hospital in the forenoon ofMarch 12, 1981. At admission his BP was 104/52 mmHg, pulse was 82/minute, and hemoglobin level was 6 gfdl. He had a blood transfusion (4 U of packed cells) that day and that raised his hemoglobin to 10 g/dl. He had a normal chemical profile, prothrombin, and partial thromboplastin time. A few hours after the transfusion, a "film" developed suddenly over his right eye, which slowly progressed that day, at first involving the upper field but a few hours later the entire field of vision. When he went to sleep that day, he could still see something but by next morning the right eye was completely blind. The vision did not change after that. He denied having any other ocular or systemic symptoms at the time of onset of the visual Joss. He gave a history of gastric bleeding in October 1973 and at that time his BP was 120/60 mmHg, pulse rate was 76/minute, and hemoglobin level was 6.1 g/dl; he received 4 U ofwhole blood, which raised his hemoglobin level to 10.8 g/dl. His normal BP, recorded by his local physician, was 110/60 mmHg in January 1971 and 110/75 mmHg in January 1987, with a pulse rate of 70 to 72/minute on both occasions.
On examination in our clinic on March 20, 1981, his visual acuity was no light perception in the right eye and 6/6 in the left eye. On plotting the visual fields with a Goldmann perimeter, the left eye showed an inferior temporal paracentral visual field defect with I-2e isopter and inferior notching with I-4e and V -4e isopters. He identified 10/14 AO plates with his left eye. The anterior segment of the eye was normal except for more than a 4.2 log units relative afferent pupillary defect on the right side. The lens and vitreous were clear in both eyes. The intraocular pressure was 12 mmHg in both eyes. Right fundus showed moderate optic disc swelling with mild pallor and fine hemorrhages superotemporal to the disc margin (Fig lA). The left fundus showed no apparent abnormality except for mild pallor of the superior two thirds of the optic disc (Fig IB). Fluorescein fundus angiography of the right eye showed a marked choroidal filling defect, especially in the peripapillary choroid (Fig IC), normal retinal circulation, and late staining of the optic disc (Fig I D). Visual-evoked response showed a normal response on the left side, but was nonrecordable on the right. Results of radiologic examination of the skull showed no abnormality. We thought that in the left eye he had most probably had a mild episode of asymptomatic anterior ischemic optic neuropathy after his previous episode of gastric bleeding in 1973, because it showed pallor of the disc and visual field defects at the initial visit, with no evidence of fresh anterior ischemic optic neuropathy. The patient was seen on three follow-up visits during the next year. On May 12, 1981, marked atrophy had developed in the right optic disc (Fig IE), with no light perception; it did not change on further followup. The left eye remained stable.
Case 2. Perforation of a peptic ulcer developed in a 56-yearold white man on May 14, 1985. He was admitted to the hospital, and his BP was 90/60 mmHg and his hemoglobin level was 6.4 g/dl. He required 15 U of blood transfusion preoperatively; after that, his BP was 130/70 mmHg and hemoglobin was 16.3 g/dl. He had a partial gastrectomy performed on May 15, 1985. On May 20, 1985, his hemoglobin
level was 12.9 g/dl and he was maintaining a BP of 110 to 130 mmHg systolic and 70 to 80 mmHg diastolic. His 4:00 AM BP every day was lowest, about 110/65 mmHg. On May 24, 1985, he woke up with a shadow in the lower half of the visual field of the left eye. At 4:00 and 8:00 that morning, his BP was 110 to 120/60 to 70 mmHg. The visual defect remained the same till May 26, 1985, when he woke up with a marked loss of vision. At 4:00 that morning, his BP was 100/60 mmHg. He had no other ocular or systemic symptoms. He was discharged from the hospital that day.
On examination in our clinic on May 26, 1985, the visual acuity was bare light perception without projection in the left eye and 6/6 in the right eye. On plotting the visual fields with a Goldmann perimeter, in the left eye a small island of field was seen in the inferior temporal peripheral region with V-4e isopter only, and the visual field in the left eye was perfectly normal. The anterior segment was normal except for the presence of2.8log units relative afferent pupillary defect in the left eye. The lens and vitreous were clear in both eyes. The intraocular pressure was 15 and 10 mmHg in the right and left eyes, respectively. The right fundus was normal except for a small cotton-wool spot about 1 disc diameter (DD) superotemporal to the disc (Fig 2A). The left fundus showed the optic disc markedly swollen and hyperemic, with no other abnormality (Fig 2B). Results of fluorescein fundus angiography showed optic disc staining on the left side, with no apparent abnormality in the right eye during the late phase. Results of ultrasound examination of the optic nerves showed no abnormality. Neurologic evaluation results disclosed no abnormality. Hematologic examination results on May 26, 1985, showed the following values: hemoglobin, 12.6 g/d1; hematocrit, 38%; and platelets, 444,000/cm, with no other abnormality.
The patient was followed periodically as an outpatient. On June 28, 1985, the left disc became atrophic. When last seen on April6, 1987, the right eye was normal and the left eye had bare light perception with optic atrophy (Figs 2C, D).
Case 3. A 59-year-old white man, with a history of recurrent bleeding peptic ulcer since 1951, had black stools during the night and woke up on September 29, 1986, with blurred vision in the superior nasal quadrant of the left eye. His BP that day was 128/82 mmHg. The next day, he noticed further worsening of the visual field defect in the left eye. He was admitted to his local hospital on September 30, 1986, for management of recently developed black stools, blood Joss, and anemia. His BP was 128/78 mmHg at the time of admission. He had a hemoglobin level of 7.7 g/dl, which within a few hours dropped to 6.6 g/dl. He was transfused 4 U of packed erythrocytes, which brought his hemoglobin level to 11.0 g/dl soon after that and 13.2 g/dl 2 days later. Frequent monitoring of his BP showed that although during the day it was about 130/70 mmHg, during the night it dropped to a fairly low level, being 94/60 mmHg at 3 to 4 AM. He had been discovered to be diabetic about 6 months earlier, and was well controlled with oral antidiabetic therapy.
He was seen by his local ophthalmologist on September 30, 1986, when the visual acuity was 6/9 in the left eye with optic disc edema, and the right eye showed no abnormality. He was seen in our clinic on October 3, 1986. At that time, the visual acuity was 6/6 in both eyes. On plotting the visual fields with a Goldmann perimeter, the right eye showed no visual field defect but the left eye showed a markedly constricted field with loss of nasal half of the field with all the isopters. Anterior segment was normal except for the presence of a 1.5 log units relative afferent pupillary defect in the left eye. The lens and vitreous were clear. The right fundus showed moderate optic
1490

HAYREH • OPTIC NEUROPATHY
A-C D,E
Fig I. Case I. A and 8, fundus photographs of right and left eyes, respectively. C and D, fluorescein fundus angiograms of right eye during retinal arteriovenous and late phases, respectively, on March 20, 1981. Notice patchy choroidal filling with a prominent temporal peripapillary choroidal filling defect in angiogram (C) and late staining of the disc (D). E, fundus photograph of right eye on May 12, 1981 .
1491

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
A,B C,D
Fig 2. Case 2. Fundus photographs of the right (A) and left (B) eyes on May 28, 1985, and of the right (C) and left (D) eyes on October 21, 1985. Notice the presence of a cotton-wool spot (arrow) in (A).
disc edema, involving the two thirds of the disc in the superior nasal area, with no other abnormality (Fig 3A). The left fundus showed marked pale optic disc edema, with a cotton-wool spot about 0.5 DO inferotemporal to the optic disc (Fig 3B). Results of fluorescein fundus angiography of the left eye showed delayed and patchy choroidal and optic disc filling (Fig 3C), with late staining of both optic discs-involving the entire disc in the left eye (Fig 30) and mostly three quarters of the right disc in the superonasal region (Fig 3E).
The patient continued to have progressive deterioration of vision and visual fields in both eyes. The left eye, 2 weeks after the initial visit, showed markedly constricted visual fields so that with I-2e only a paracentral 6° field was present and with V-4e only a 25° field was present, with a visual acuity of6/18. In another week, it deteriorated to 6/60, and only a 10° field temporal to fixation was recorded with V -4e only. One month later, the visual acuity in the left eye was 6/90 and a 5° temporal island field with V-4e only. A temporal defect with I-2e and l-4e developed in the right eye 1 week after the initial visit to our clinic, although the visual acuity had remained 6/6 centrally. Two weeks later although the right disc looked almost normal, the left disc showed generalized marked pallor
with no edema (Fig 3F). On December 19, 1986, the visual acuity was 6/6 in the right eye and 6/120 in the left, with only a tiny island of visual field in the inferior temporal region of the left eye and stable visual field in the right eye. Results of fundus examination showed optic atrophy in the left eye and normal-looking disc in the right. Results of detailed neurologic, systemic, and cardiovascular evaluation showed no other abnormality.
At last examination on March 13, 1987, the visual acuity in the left eye had deteriorated to hand motions only, and no visual field could be plotted. The patient was still having recurrent gastrointestinal (GI) bleeding; the last episode had occurred 1 month before. The right eye showed no change.
Case 4. A 57-year-old white man, on November 28, 1986, at 3 AM started to have black stools. He was admitted to the hospital at ll AM on November 29. At the time of admission, his BP was 124/64 mmHg and his hemoglobin level was 8 gjdl. He had 700 ml of blood transfusion, which raised the hemoglobin level that day to 11.1 g/dl, hematocrit level to 33%, and platelet count to 323,000/mm3• He was found to have multiple duodenal ulcers. He was discharged from the hospital on December 3, 1986. When he awoke on the morning of December
1492

HAYREH • OPTIC NEUROPATHY
A-C 0-F
Fig 3. Case 3. A and 8, fundus photographs of right and left eyes, respectively. C-E, fluorescein fundus angiograms of left eye (C and D) during retinal arterial and late phases respectively, and ofright eye (E) during the late phase, on October 3, 1986. Notice the presence ofa cotton-wool spot (arrow) (B), non filling ofthe disc in superior three quarters ofdisc with patch choroidal filling (C), and late staining ofthe discs (D and E). F, fundus photograph of left eye on October 24, 1986.
1493

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
A,B C,D
Fig 4. Case 4. Fundus photograph (A) and fluorescein fundus angiograms (Band C) during the retinal arteriovenous and late phase, respectively, of the left eye on December 15, 1986. Notice patchy choroidal filling (B) and optic disc staining (C). D, fundus photograph ofleft eye on January 19, 1987.
5, 1986, he noticed blurred vision in the inferior part of the visual field of the left eye. It gradually progressed during the following days to involve the superior field, so that by December 9, 1986, the vision was blurred all over the left eye. He saw his local ophthalmologist that day who found his visual acuity in the left eye to be only counting fingers, marked relative afferent pupillary defect, a temporal island of visual field, and marked optic disc edema in that eye; he gave a retrobulbar injection of depot corticosteroids but that did not improve the vision.
He was referred to our clinic on December 15, 1986. At that time his visual acuity was counting fingers at about 6 feet eccentrically in a temporal island. Visual field plotting with a Goldmann perimeter showed the loss of central and entire nasal half field of vision; the patient could see I-4e in the temporal field, from the blind spot temporally in the left eye, and normal fields in the right eye. There was a 2.7 log units relative afferent pupillary defect in the left eye. The anterior segment was normal in both eyes, with the intraocular pressure of 20 and 19 mmHg in the right and left eye, respectively. The lens was clear in both eyes. The left fundus showed optic disc edema (Fig 4A), and the right fundus showed three drusen-like
white spots in the macular region, with no other abnormality in either eye. Fluorescein fundus angiography results disclosed sluggish choroidal circulation (Fig 4B) and late disc staining (Fig 4C). His hemoglobin level was 13.0 gjdl, hematocrit level was 39%, and platelet count was 429,000/mm3• He was found to have no other hematologic or cardiovascular abnormality. He was seen again on January 19, 1987, when there was no change in his visual status. Generalized pallor with no edema had developed in the left optic disc (Fig 4D). When last seen on April 7, 1987, the left eye showed no further change and the right eye was normal.
DISCUSSION
This article has two principal objectives: ( 1) to give a comprehensive clinical picture of this disease, based on an exhaustive review of the literature and my own experience; and (2) to discuss its pathogenesis, in the light of current knowledge.
1494

HAYREH • OPTIC NEUROPATHY
CLINICAL FEATURES Site and type of bleeding. The most common source
of bleeding in these cases is from the GI tract; the next most common is the uterus (reports of such cases are innumerable in the literature), but it can be from other sites, including nose, lungs, repeated therapeutic bloodletting by venesection, and wounds. In 1876 Fries4 found bleeding from the GI tract in 35.5% of cases studied, the uterus in 25.0%, bloodletting in 25.0%, epistaxis in 7.3%, wound bleeding in 7.3%, hemoptysis in 1.0%, and urethral bleeding in 1%. In 1904 Singer5 found bleeding from the GI tract in 40.2% of cases studied, the uterus in 32.8%, bloodletting in 14.3%, epistaxis in 7.4%, wounds in 3.2%, hemoptysis in 1.0%, and urethral bleeding in 1.0%. In 1949 Lockets found bleeding from GI tract in 47.0% of cases studied, the uterus in 32.5%, epistaxis in 9.0%, and from miscellaneous sources in 11.5%. Of my seven cases, recurrent GI bleeding occurred in six and recurrent uterine bleeding in one. There are some rare types reported in the literature. Visual loss developed in a hemophiliac after tooth extraction.4s Visual loss after bleeding is extremely uncommon in healthy persons with no evidence of previous recurrent bleeding; however, there are rare case
42 49 50reports of visual loss after traumatic wounds. 15· · ·During recent years, there have been anecdotal case reports after various surgical procedures associated with massive blood loss (e.g., gastrectomy, thyroidectomy, pulmonary resection, cardiopulmonary bypass, and other types of heart surgery, cholecystectomy, and so on). 51-55 There is one case report of blindness after cutting the radial artery. 56 The bleeding is usually massive and recurrent, but the condition can, very rarely, occur after a single hemorrhage.
Age and sex distribution. Patients of all ages and both sexes have been reported. The youngest reported case is a 2-year-old child with hydrocephalus, in whom the visual loss occurred shortly after application of leeches to the forehead 57-it is possible that this may not be a true case of this condition. Carreras Matas5s reported a 4year-old boy with bilateral optic atrophy whose mother suffered from uterine bleeding during pregnancy; the author postulated that the blindness was due to that. Singer5 found 45.4% men and 54.6% women in his series; however, among the 66 patients with GI bleeding and visual loss, 76% were men. Lockets found an overall 50%-male-to-50%-female sex ratio, but visual loss after gastric hemorrhage was more common in men than in women. He also found that 51% of patients were under 40 years of age (1.5 times more women than men), 49% were older than 40 years of age, (2.5 times more men than women), and 31% older than 50 years ofage. Ofmy six cases with GI bleeding, five were men ('Yith gastric bleeding) and one a woman (with bleeding from the colon); the age of the five with gastric bleeding varied between 56 and 64. The one patient with colon bleeding was 83 years of age, and the one with uterine bleeding was 41 years of age.
Time interval between hemorrhage and onset of visual disturbance. When this information is available, typi
cally there is a time lag between the bleeding and the onset ofvisual loss. Singer5in 120 cases, found the onset of visual loss occurring during the bleeding in 8.3%, immediately after that in 11.6%, within the first 12 hours in 14.2%, 12 to 48 hours in 19.2%, 3 to 10 days in 39.2%, 2 weeks in 4.2%, and 18 to 60 days in 3.3%. Locket,s in 4 7 cases, found the time of onset of visual loss after the last hemorrhage to be immediate in 15%, within 1 week in 56%, within two weeks in 18%, within 3 weeks in 7%, and after 3 weeks in 4%. Unfortunately, in these analyses cases of transient visual loss during the syncopal phase have been mixed with cases of the true disease, in which the visual loss is of a permanent nature. In the true posthemorrhagic group, the visual loss rarely can occur during or immediately after the bleeding.5·59·60 In my four cases reported here in detail, the visual loss occurred within a few hours (in two eyes of 2 patients), about 1 week (in two eyes of 2 patients), and 10 to 11 days (in 1 eye) after the bleeding; in one eye, I discovered a visual field defect, of which the patient had not been aware for years because of normal visual acuity. The visual loss developed in these four patients after they had had adequate blood transfusion (after a few hours in one, 7 to 10 days in the remaining threein one of these three patients it developed in one eye before the transfusion and in the second eye about 1 week after the transfusion). In my remaining three cases, no definite history about this was available.
Laterality. The visual disturbance is usually bilateral. Singer5 found a bilateral incidence in 86%-in nine of ten cases when it occurred during hemorrhage, in 13 of 14 when occurring immediately after bleeding, and in 41 of 4 7 when visual loss developed between 3 and 10 days after bleeding. Both eyes may be involved simultaneously or there may be an interval of hours or days between the involvement of the two eyes. Of my seven cases, the visual loss was bilateral in four and both eyes were involved almost simultaneously in two, at a 1-week interval in one and at two separate episodes ofGI bleeding 8 years apart in one.
Visual symptoms. These may vary from blurred vision to complete loss of vision in one or both eyes, or at first in one and later on in the second. The onset of visual loss is usually sudden (visual loss frequently discovered on awakening), but a progressive visual loss during several hours and rarely during several days has been reported. The visual symptoms may vary from hazy vision to central scotoma, altitudinal defect, concentric contraction, or no light perception.
Visual acuity and visual fields. Visual acuity may vary from normal to no light perception. There are optic nerve-related visual field defects. Typically, it is an infe
20 21 34 35 253 61rior altitudinal hemianopic defect, 15· · · · .4 , · ·62 but61 63 64the visual fields may show marked constriction, 34· · ·
superior altitudinal defect,62 nasal hemianopic defect,65 central scotoma,61 or some other type. Grout61 found the inferior altitudinal defect in 23% of cases studied, concentric contraction in 20%, central scotoma in 13%, and homonymous hemianopic defects in 10%. In my seven cases, visual acuity in the involved eye at initial
1495

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
examination was 6/6 (in three eyes oftwo patients), 6/12 to 6/18 (in two eyes of two patients), hand motions (in both eyes of 1 patient), light perception in a temporal island (in one eye), and no light perception (in one eye). Where visual fields could be plotted with a Goldmann perimeter, the preserved visual function was usually in the temporal part with constriction of the fields, with one patient having central scotoma in both eyes initially. In the right eye of case 3, at initial examination, 5 days after the bleeding (despite optic disc edema) no subjective or objective visual loss was detected, but 1 week later a visual field defect with 6/6 visual acuity developed.
Ocular lesions. The anterior segment of the eye shows no abnormality other than pupillary abnormalities secondary to the visual loss. The primary ocular lesions are in the fundus.
FUNDUS LESIONS
The basic changes in the fundus are those related to the optic disc, with a rare lesion in the retina. In the old literature, it was stated frequently that the optic disc and rest of the fundus were pale, and the pallor was erroneously thought to be primarily due to anemia and loss of blood-similar to the pale skin seen in such patients. Because the color of the background of the fundus depends on the color ofthe retinal pigment epithelium and not on the amount of hemoglobin or blood there, anemic patients cannot have pale fundi. The pale optic disc in these cases is due to optic atrophy and not due to anemia.
Optic disc changes. The essential initial lesion in the fundus in this condition is the presence of optic disc edema, involving the entire or a part of the disc, with or without a few splinter hemorrhages at or near the disc margin. The pattern and evolution of optic disc changes seen in the disease is typically that seen in AION, i.e., edema during the initial stages (Figs lA, 2B, 3A, 3B, 4A), and gradual development of atrophic changes with time, so that in about 2 months the edema is resolved and the disc is pale (Figs lB, IE, 2D, 3E, 4D). In the literature, pallor of the disc is overstressed in this condition, and this erroneous impression may be partly due to the fact that many of these cases are not seen during the early stages but only when the atrophic phase has set in, and the disc has resolving edema with pallor or even optic atrophy. Our detailed prospective studies in about 600 cases with AION resulting from various causes has demonstrated clearly that the "pale optic disc edema" described as a characteristic feature ofAION is simply a persistent myth; these eyes during the initial stages usually do not have pale optic disc edema, except in eyes where AION is due to complete occlusion of the feeding posterior ciliary arteries (e.g., in giant-cell arteritis or other types of vasculitides or embolic occlusion).66-69 Very rarely, the fundus has been reported as normal in these eyes at the time of onset ofvisualloss,23•70 whereas in a few cases the presence ofoptic disc edema at the first examination soon after the visual loss has been re
ported.53 Pears and Pickering23 reported a case in which on the day of onset of blindness the fundus was normal, but 5 days later the disc was edematous and 5 weeks later it was atrophic. Optic atrophy is the almost universally reported late lesion in these eyes, ever since von Graefe32 in 1860. All seven of my cases presented with optic disc changes typical of AION. One eye had optic disc edema 5 days after the GI bleeding (right eye ofcase 3, Fig 3A) with no subjective or objective visual loss (similar to that reported by me previously71 ), and visual field defect developed in this eye 1 week later.
Other fundus lesions. Usually there is no other abnormality in the fundus. The presence ofa rare cotton-wool spot and/or retinal hemorrhage has been reported. I saw an isolated cotton-wool spot in two eyes among my cases (Figs 2A, 3B). In the old literature, pallor of the fundus and narrowing of the retinal arteries were mentioned very frequently; these subjective findings were based on an assumption that blood loss and associated anemia must produce them. Some old reports even mentioned the presence of retinal edema posteriorlyprobably the peripapillary extension ofoptic disc edema was interpreted erroneously as retinal edema.
Fluorescein fundus angiographic findings. In the eyes with visual loss in my patients, angiography results showed normal retinal circulation but delayed choroidal filling, particularly in the peripapillary region (Figs 1 C, 3C, 4B) and poor perfusion of the optic disc, and optic disc staining (Figs lC,D; 3C,E; 4B,C). Poor perfusion of the optic disc and its staining has also been reported by
72other authors.63·Visual recovery. It is generally agreed that the visual
loss is usually permanent and there is seldom any appreciable visual recovery. The data on this aspect of the subject, reported in the literature, are of a very poor quality, because of multiple problems with the available case reports; there is mixing of the transient syncopal type of visual loss (with good prospect for visual recovery) and the genuine posthemorrhagic visual loss (usually with poor prognosis). Also, in a seriously sick patient, the initial poor visual acuity recording may be misleading. The following information, based on a review of the reported cases, must be interpreted in the light of these and other serious limitations. In 1896 Pergens73 found complete blindness in both eyes in 36% of cases studied and in one eye in 18%, marked reduction of vision in 18%, and complete recovery in 8%. In 1904 Singer5 found no improvement in 45.9% of cases, variable improvement in 39.1 %, complete recovery in 13.5%, recovery with subsequent failure in 1.5%. Singer5 further correlated visual recovery with the lapse of time between the bleeding and the onset of blindness in 113 cases, and found that 22% showed a variable amount of recovery if the visual loss developed during the bleeding (9 cases), in 71% ifwithin 12 hours(31 cases), in41.5% if within 12 hours to 10 days (65 cases), and in 50% if longer than 10 days (8 cases), and in the rest there was either no recovery or it got worse. Terson43 found permanent blindness in 50%. Tidy74 found complete blindness in 33% of cases, no improvement in 50%, good to
1496

HAYREH • OPTIC NEUROPATHY
complete recovery in I0%, and variable improvement in 7%. Lockets found complete recovery in 14% of cases, some recovery in 50%, and none in 36%. Unger9 (on a review of 286 cases reported between 1941 and 1953) found permanent visual loss in 55%, some visual improvement in 34% and recovery to normal in II%. Thus, in these series, about 10% of the cases showed complete recovery of vision while about one half to three quarters showed no improvement. In my seven cases, none showed any visual recovery. In six eyes, the visual loss was progressive initially (initial visual loss and further deterioration usually noticed on awakening in the morning): over the first few days (within 1 week) in five eyes, and during several weeks in one eye. Rarely recurrence of bleeding may cause further deterioration of vision.7·s This was seen in three of my cases-cases 1 and 3, and in another woman with repeated uterine bleeding (due to extensive endometriosis) who had multiple bilateral recurrences of visual loss over the 4-year period I followed her. Visual recovery after blood trans
21 75 ·76fusion has been claimed by some authors,s. 1s· ·whereas a number of patients lost vision after they had
63blood transfusion, 1s· ·77 as occurred in some ofmy cases also.
PATHOGENESIS
The various theories put forward in the literature to explain the visual loss after distant systemic bleeding were reviewed very briefly in beginning of this article. During recent years, a consensus has emerged that it is due to ischemia of the anterior part of the optic nerve; that is, it represents AION. It is well established that the earliest fundus change after visual loss is almost invariably optic disc edema, which in about 2 months evolves into optic atrophy-very typical findings and course for AION. Histopathologic findings in three cases14·24·7s (22 days, 11 days, and 3 112 years, respectively, after onset of blindness) also confirmed the presence of AION. However, the pathogenesis ofAION in this condition is still a highly controversial subject and the exact mechanism remains an enigma. In the literature, the most prevalent view is that anemia and/or arterial hypotension, after massive blood loss, are the primary factors responsible for the development of visual loss in these patients. The following is a brief summary of the views expressed,
Anemia. This has been blamed as an important cause of the visual loss in these patients by many authors.s,1s·23·35·41·5s·60·74·79-s2 Some ofthe authors in the last century and around the turn of the century thought that the ocular changes were akin to those seen in chlorosis (i.e., iron deficiency anemia), which was prevalent then. It was believed that after hemorrhages the v6lume of blood is rapidly made up, but it takes a long time for the hemoglobin level to recover. Fall in the hemoglobin level produces a lack ofoxygen that is responsible for the hypoxia or ischemia. Lockets thought that hemodilution of blood, with fall in the hemoglobin level and plasma proteins, is important, because the visual symptoms typically occur hours or days after the bleeding, when the
volume of the blood has returned to normal. He postulated that low plasma proteins cause optic nerve edema, which in turn causes ischemia, and ischemia causes damage to capillary and vessel walls, acidosis, capillary vasodilatation, arteriolar constriction, and compression of venules, so that a vicious circle is set up.
Arterial hypotension. This also has been thought to be very important, if not the only factor responsible for visual loss. The visual loss has been considered similar to the visual loss after postural hypotension. It has been postulated that capillaries suffer anoxic damage when the blood pressure in them is insufficient to maintain adequate circulation.53 In patients with malignant arterial hypertension, if the BP is lowered precipitously, loss of vision resulting from development of AION has been well documented.s3-s7 In these patients with malignant arterial hypertension, it has been postulated that a sudden fall of systemic blood pressure causes failure of the autoregulatory mechanism of circulation in the optic nerve headss; however, this may not apply to patients after hemorrhages because they do not have the predisposing factor of malignant arterial hypertension. Development of AION in patients who suffer marked arterial hypotension during shock or surgical procedure has been reported.55·s9-91
Combined effect of anemia and arterial hypotension. This has been the favorite view in the literature. W olff20 postulated that inferior altitudinal hemianopia seen in these patients was due to the effect of gravity, which normally plays no part in the distribution ofblood in the retina. However, according to him, in severe bleeding, in which the blood flow is very much slowed, gravity determines that lower part of the retina would receive more blood than the upper, just sufficient to ward off spasm of the retinal arteries owing to ischemia. Hartmann and Perfonry19 and Hollenhorst and Wagener 21 put forward similar speculations. Unfortunately, all these authors erroneously thought that inferior altitudinal visual field defect, seen in these patients, was secondary to ischemia of the upper half of the retina and not to optic nerve involvement; we know now that that is incorrect. Watkins et al92 postulated that optic disc edema in these cases was due to anoxia of optic nerve, resulting from loss of blood. Presencia et als 1speculated that the combined effect of anemia and arterial hypotension was responsible, interfering with the autoregulatory mechanisms ofthe optic nerve head. Restoration or improvement in the vision after blood transfusion in
21 ·53·76these cases has been reported,s,ts, ·93 and it has been thought to be due to correction of anemia and/or hypotension. However, loss of vision after adequate blood transfusion was seen in almost all my cases and has also been reported in the literature,1s·21·63·77 and there are also case reports in which patients after systemic hemorrhages associated with marked arterial hypotension and
2379 94 97low hemoglobin never developed AION, 13• · · thereby suggesting that there must be other factors responsible for development of AION.
In my cases, the BPs and hemoglobin levels at the time of onset of visual loss were within normal limits,
1497

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
except in one case in which we have no definite data at the time of visual loss in the first eye, but we know that they were normal when visual loss developed in the second eye. Before blood transfusion in these patients, however, there was a markedly low level of hemoglobin in all, and marked arterial hypotension in two.
From a review of the literature and from the information provided by my cases, it can be concluded that for an understanding of pathogenesis, one has to consider a number of factors in these cases, including the following. (I) The visual loss usually develops hours, days, or even weeks after systemic bleeding (80-85%5•8), and is uncommon during or immediately after bleeding (15-20%5•8). Unfortunately, the syncopal type of transient visual loss has been mixed with the true posthemorrhagic visual loss in the data available in the literature. (2) The visual loss is usually seen after recurrent hemorrhages, and is very uncommon after a single hemorrhage in a perfectly healthy person. (3) In almost all my cases
21 63and others, 18• • •77 visual loss was noted after adequate blood transfusion (hence, hemoglobin level within normal limits). (4) Visual loss occurred in many cases in the literature and in almost all my cases, when the BP recorded during the day was within normal limits. (5) Visual loss frequently develops or progresses during sleep.
These factors strongly suggest that in most cases neither arterial hypotension alone nor low hemoglobin level can explain the sudden development of visual loss resulting from AION. One has to look elsewhere for an answer. Available evidence indicates that the following two factors most probably play crucial roles.
Release of endogenous vasoconstrictor agents after recurrent hemorrhages. Hodge et al98 found that in dogs hemorrhage causes an increase in the concentration of circulating angiotensin, even when there is no fall of arterial mean or pulse pressure. Similarly, Bunag et al99
showed that in dogs bleeding caused renal release of renin whether or not there was measurable change in either arterial pressure or total renal blood flow, and they also found that hemorrhage-induced release of renin occurred more consistently in dogs fed a low-sodium diet than in those fed a standard diet. These findings contradicted the usual view that release of renin during hemorrhage is entirely dependent on the associated arterial hypotension. 100 According to Bunage et al,99 increased vasomotor discharge induced by bleeding causes renal release of renin, and they concluded that neural stimuli are capable of causing release of renin in the absence of gross change in renal perfusion pressure of flow. A considerable body of evidence has accumulated showing that the sympathoadrenergic system can influence renin release, and the subject has been sum
102 Inmarized recently by Zanchetti and co-workers. 101 •
brief, most of the experiments have shown an increase in peripheral renin or in renin release after intravenous or intra-arterial infusion of catecholamines and during electrical stimulation of renal nerves and of vasomotor centers in the brainstem. There is suggestion that the sympathetic control of renin is centrally organized be~
cause brainstem stimulation influences renin release. Sympathetic discharge provoked by carotid occlusion also causes release of renin. Hodge et al 103 found that hemorrhage caused a greater rise of angiotensin concentration (without any gross change in BP in the carotid sinus) than did carotid occlusion, and they concluded that concentration ofangiotensin in the blood is affected by cardiovascular reflexes. More recent evidence104•105
has provided the mechanism by which nonhypotensive hemorrhage may evoke the release of renin and other vasoconstrictors. As described earlier, both neural and humoral adrenergic stimuli working directly on the release mechanism in the renal juxtaglomerular apparatus can increase renal secretion of renin when arterial pressure is normal or even elevated. Thus, the renal baroreceptor mechanism, which provides for elaboration of renin in the face of a fall in renal perfusion pressure, can be compensated for by neural or humoral activation of adrenergic renin release mechanisms. A number of interventions are capable of increasing the secretion of renin in the absence of a fall in arterial or intrarenal pressure. It is beyond the scope of this article to discuss even summarily the complicated subject of regulation and release of renin, angiotensin, and other endogenous vasoconstrictor agents. In conclusion, all the available evidence indicates that activation of the sympathetic nervous system and increased circulating levels of three humoral agents, angiotensin, epinephrine, and vasopressin, all lead to vasoconstriction in a circumstance such as nonhypotensive hemorrhage, and at least one of the humoral factors (epinephrine) is also known to increase renin secretion by the kidney. 104•105
In our experimental studies on renovascular malignant arterial hypertension in rhesus monkeys, we pointed out that the available evidence strongly indicates that the renin-angiotensin-aldosterone system plays an important role in not only the development and maintenance of hypertension 106 but also in the production of hypertensive optic neuropathy and other fundus lesions.88•107•108 Based on that experience, I think that in the development of AION after distant hemorrhage, increase in levels of angiotensin II and other vasoconstrictor agents in the blood most probably plays an important role. Angiotensin II is the most powerful vasoconstrictor substance known and it also potentiates the vasoconstrictor activity of norepinephrine; the latter is released in excessive amounts due to angiotensin stimulating the sympathetic nervous system. We discussed at length the important role played by angiotensin in the pathogenesis of hypertensive optic neuropathy88 and hypertensive choroidopathy. 108 Briefly, because choriocapillaris are very leaky, the plasma (along with angiotensin and other vasoconstrictor agents in it) leaks freely into the choroidal interstitial fluid. A rise in the level of these agents in the choroidal interstitial fluid would produce ischemia of the anterior part of the optic nerve by the following two mechanisms.
Vasoconstriction ofthe peripapillary choroidal vessels. The primary source of blood supply to the optic nerve head and retrolaminar region of the optic nerve is the
1498

HAYREH • OPTIC NEUROPATHY
peripapillary choroid. 109 A high level of endogenous vasoconstrictor agents (such as angiotensin, epinephrine, and vasopressin) in the peripapillary region, by their direct action on the peripapillary choroidal blood vessels, and also perhaps in response to activation of their sympathetic innervation, would cause peripapillary choroidal vasoconstriction. Aim and Bill110 showed that sympathetic stimulation causes a marked vasoconstriction in the choroid. Fluorescein fundus angiographic findings in experimental malignant arterial hypertension88·108 and in the current cases (Figs lC, 3C, 4B) also showed that. Therefore, peripapillary choroidal vasoconstriction causes secondary ischemia of the anterior part of the optic nerve.
Absence ofblood-optic nerve head barrier. The Border Tissue of Elschnig, separating the prelaminar region of the optic nerve head and the peripapillary choroid, is freely permeable, allowing a considerable amount of fluid to flow from the peripapillary choroid into the anterior part of the optic nerve (see Hayreh 111 for a detailed review). The vasoconstrictor agents from the peripapillary choroidal interstitial fluid would diffuse into the optic nerve head through the Border Tissue of Elschnig. In the tissues of the optic nerve head, they would produce vasoconstriction and occlusion by direct action on the capillaries and other vessels there; this was also suggested by the experimental studies of Sassi and Anderson. 112
The two mechanisms must interfere jointly with the blood supply of the anterior part of the optic nerve and cause variable degrees ofischemia in different eyes, even including AION. It could be asked, in these cases of AION after massive bleeding, why are there no other fundus lesions of malignant arterial hypertension or lesions resulting from vasoconstrictor agents? In this connection, the detailed studies ofPears and Pickering23 are most relevant. In their eight cases of massive systemic hemorrhage, AION developed in one, whereas the remaining seven showed the presence of an occasional cotton-wool spot and a rare retinal hemorrhage without any visual symptoms or visual loss. They concluded that "The close similarity between the retinal lesions seen in the malignant phase of hypertension and those which occur after gastrointestinal haemorrhage suggests that they may have a common pathogenesis.'m Among my cases, two eyes (Figs 2A, 3B) showed the presence of an isolated cotton-wool spot in the retina-AION or visual loss never developed in one of those eyes. These retinal lesions almost never produce visual symptoms, so that patients with these retinal lesions, after recurrent systemic hemorrhages, may never be seen by ophthalmologists. These may occur far more frequently than so far realized, as indicated by the studies ofPearsand Pickering.23 Also, the difference in responses of' retinal and optic nerve head blood vessels may be due to the fact that retinal vascular bed has a good blood-retinal barrier, but in the optic nerve, head there is no blood-optic nerve barrier (because. of leaky Border Tissue of Elschnig). The other factor that could logically determine the extent of the fundus lesions is the concentration of cir
culating angiotensin and other vasoconstrictor agents, and the length of time they remain elevated. In malignant arterial hypertension, much higher levels of angiotensin II and vasopressor agents may be maintained for a much longer duration than in a transient phenomenon such as a massive systemic bleeding. To develop hypertensive retinopathy and hypertensive choroidopathy, we may require much higher concentration, maintained for a much longer time, than for the production of AION. Evidently, this conclusion is speculative because we have no firm evidence for it so far.
Arterial hypotension. This may also play an important additional role in the production of AION in a proportion of these cases, by the following mechanism. Blood flow in the anterior part of the optic nerve depends on at least four parameters: ( 1) mean blood pressure (i.e., diastolic BP + 1/3 of the difference between the systolic and diastolic BP) in the capillaries of the optic nerve head and peripapillary choroidal arteries; (2) intraocular pressure; (3) peripheral vascular resistance; and (4) presence or absence of blood flow autoregulation. The blood flow in the anterior part of the optic nerve can be calculated by the following formula:
_ perfusion pressure Blood flow - . h I I . penp era vascu ar resistance
(perfusion pressure = mean arterial blood pressure minus intraocular pressure). It is well known that during sleep the systemic arterial blood pressure falls appreciably in susceptible persons; this was recorded in some of my patients, in whom BP was monitored frequently around the clock. Arterial hypotension thus reduces the blood flow in the optic nerve head, if the autoregulation decompensates (because of perfusion pressure falling below the critical level).
Pathogenesis. Based on these observations, one can postulate that the following combination would compromise the blood flow in the optic nerve head.
(1) Increase in peripheral vascular resistance. The absence of blood-optic nerve head barrier allows the endogenous vasoconstrictor agents, such as angiotensin, epinephrine, and vasopressin (liberated in response to recurrent hemorrhages), to leak into the optic nerve head tissues, producing vasoconstriction. This may also be produced by vasoconstriction of the peripapillary choroidal arteries (as discussed above). The vasoconstriction by itself may cause AION.
(2) Fall of systemic blood pressure. This occurs immediately after the bleeding owing to hypovolemia or during sleep (although the BP during waking hours may be within normal limits in the latter). The fact that, in many of my patients, the initial visual loss or further deterioration was noticed on waking up in the morning strongly suggests the role of hypotension during sleep in the development of AION. The same applies to a vast majority of the nonarteritic AION cases.
(3) Failure of autoregulation of the blood flow. This happens if the perfusion pressure falls below the critical Ievel113 because of one or both factors mentioned previously.
1499

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
Thus, a fall of perfusion pressure to a very low level, vasoconstriction of vessels in the optic nerve head, accompanied by increase in peripheral vascular resistance, and failure of autoregulation, would compromise the blood flow in the anterior part of the optic nerve and result in the development of AION. If the optic nerve head ischemia is subclinical, symptomless optic disc edema may develop in the eye, as was seen in the right eye of case 3 at the initial visit. I have seen more than two dozen eyes with symptomless optic disc edema as initial signs of nonarteritic AION, in our prospective studies on AION; its pathogenesis is discussed elsewhere.71
Interindividual variation in development of AION after massive systemic hemorrhage could be due to differences in individual responses and susceptibility. That is, in certain individuals much more angiotensin and other endogenous vasoconstrictor agents may be liberated after an equal amount of hemorrhage than in others, because of interindividual differences in liberation of catecholamines and other sympathoadrenergic and vasomotor neural responses. It is possible that in the pathogenesis of idiopathic nonarteritic AION similar release ofendogenous vasoconstrictor agents in response to sympathetic neural stimuli may play an important role.
It is possible that recurrent hemorrhages may also produce increased platelet aggregation, and that, in turn, may produce microembolism and play some role in the production of AION. In my cases, there was an increase in platelet counts soon after the hemorrhage.
This hypothesis thus helps to explain most of the features of the visual loss after distant systemic hemorrhages. There seems little evidence to support the theory that a mere fall in hemoglobin level causes AION. I could not find any evidence in the literature that a fall in hemoglobin level causes release of angiotensin or other vasopressor agents.
Conclusion. From the available evidence in the literature, from my cases, and from our experimental studies on renovascular malignant arterial hypertension, it is postulated that release of angiotensin and other endogenous vasoconstrictor agents (secondary to recurrent massive systemic hemorrhages, with or without arterial hypotension) is most probably a very important factor in the production of AION. Arterial hypotension seems to be an additional important factor. Increased platelet aggregation may also play a role. There is no available evidence to indicate that fall in hemoglobin level is responsible for the development of AION.
MANAGEMENT
It has been claimed in a few cases in the old literature that marked visual recovery occurred after immediate
18 21 76 93and adequate blood transfusion8· · · • ; however, there are many more case reports, including my own, in which the patients in fact lost vision despite immediate and adequate blood transfusion, with hemoglobin levels and BP within normal limits. No doubt prompt and
adequate blood transfusion is indicated if a patient has lost massive amounts of blood, to replace that and to prevent other complications, but it appears to have little effect in the management of visual loss. Locket8 also advised a rich diet, including adequate protein intake, because he thought protein deficiency played an important role in the pathogenesis. Unfortunately, we have no definite treatment yet that has been shown to help these patients. Because the evidence discussed earlier suggests a role of angiotensin and other endogenous vasoconstrictors in the production of AION, use of drugs to prevent their production (e.g., inhibitors ofangiotensinconverting enzyme) or to counteract their actions may have a role to play in its management or even prevention, and the same may apply to idiopathic nonarteritic AION, which is a common visually crippling disorder. These are the future avenues to be explored.
ACKNOWLEDGMENTS
I am grateful to my wife, Shelagh, for her help in the preparation of the manuscript and for translating the relevant original Greek work ofHippocrates and Latin work ofN. Fontanus (1641 ); this is her tribute to Paul Henkind. I am indebted to Dr. Michael J. Brody, Professor of Pharmacology at the University of Iowa, for his expert advice on the complicated topic of renin, angiotensin, and endogenous vasoconstrictor agents. Dr. Brody, who also knew Paul Henkind, has paid his tribute by his contributions to this article.
REFERENCES
1. Hippocrates. Oeuvres Completes d'Hippocrates. Littre E, ed. Amsterdam: Adolf M. Hakkert, 1851; 7:110-13.
2. Fontanus N. Observationum rariorum analecta. Amstelodami: Sumpt. H. Laurentii, 1641.
3. Truka de Krzowitz W. Historia Amauroseos, Omnis Aevi Observata Medica Continens. Vienna 1781.
4. Fries S. Amblyopieen und Amaurosen nach Blutverlust. Klin Monatsbl Augenheilkd 1876; 14(3): 3-73.
5. Singer K. Ueber Sehstorungen nach Blutverlust. Beitr z Augenheilkd 1904; 6(53) 1-30.
6. Zentmayer W. Visual disturbances from distant hemorrhage. JAMA 1912; 59:1050-5.
7. Harbridge DF. Optic atrophy manifested by visual disturbance following distant hemorrhage. Am J Ophthalmol1924; 7:192-6.
8. Locket S. Blindness associated with haemorrhage. Br J Ophthalmol 1949; 33:543-55.
9. Unger L. Uber Sehstorungen nach Blutverlusten. Klin Monatsbl Augenheilkd 1955; 126:41-50.
10. Duggan WF. Use of vasodilators in treatment of retrobulbar neuritis. Arch Ophthalmol1936; 16:380-99.
11. Rootman J, Butler D. lschaemic optic neuropathy-a combined mechanism. Br J Ophthalmol 1980; 64:826-31.
12. Deveckova D, Selecka I. Monolateral amaurosis following loss of blood. Cs Oftal1972; 28:141-4.
13. Ulrich R. Ueber Netzhautblutungen bei Anamie, sowie, uber das Verhalten des intraocularen Drucks bei Blutverlusten, bei Chinin-und Chlorai-Vergiftungen. Graefes Arch Clin Exp Ophthalmol 1887; 33(2): 1-46.
14. Ziegler E. Zur Kenntniss der Entstehung der Amaurose nach Blut
1500

HAYREH • OPTIC NEUROPATHY
verlust. Aus dem pathologischen . Beitr z Path Anal u Physiol; Jena, 1887; 2:57-72.
15. Terrien F. Amaurose post-hemorragique. Arch d'Ophtalmol 1921; 39:263-9.
16. Collins ET. Discussion of paper by Whiting M. Diseases of the optic nerve: I. Optic atrophy following haemorrhage from the alimentary tract. Trans Ophthalmol Soc UK 1929; 49:150.
17. Whiting M. Optic atrophy following haemorrhage from the alimentary tract. Trans Ophthalmol Soc UK 1929; 49:144-54.
18. Langdon HM. Amaurosis after uterine hemorrhage: with restoration of vision following transfusion. Arch Ophthalmol 1933; 10:99-102.
19. Hartmann E, Parfonry J. Cecile par perle de sang amelioree par !'acetylcholine mais conservant un retrecissement binasal du champ visuel. Bull Soc Ophtalmol Fr 1934; 56-61.
20. Wolff E. The causation of amblyopia following gastric and other haemorrhages. Trans Ophthalmol Soc UK 1935; 55:342-9.
21 . Hollenhorst RW, Wagener HP. Loss of vision after distant hemorrhage. Am J Med Sci 1950; 219:209-18.
22. Cordes FC. Retinal ischemia with visual loss. Am J Ophthalmol 1958; 45(4):79-88.
23. Pears MA, Pickering GW. Changes in the fundus oculi after haemorrhage. Q J Med 1960; 29:153-78.
24. Gorlitz M. Histologische untersuchung eines Falles von Erblindung nach schweren Blutverlust. Klin Monatsbl Augenheilkd 1920; 64:763-82.
25. Theobald S. A case of atrophy of the optic nerves following haemorrhage from the stomach, with a consideration of the causes of post-haemorrhagic blindness. Am J Ophthalmol1899; 16:145-52.
26. Scheffler MM. Visual loss following distant hemorrhage. Arch Ophthalmol 1943; 29:449-56.
27 . Duggan WF. Clinical vascular physiology of the eye. Am J Ophthalmol 1943; 26:354-68.
28. Cox RA. Amblyopia resulting from hemorrhage. Arch Ophthalmol 1944; 368-71.
29. Leber T. Graefe-Saemisch-Hess Handbuch der gesamten augenheilkunde, Auft . Bd. 7, T. ii , 1916; 342-7.
30. Hoffman FW. Ein Fall von Amaurose nach Hamatemesis. Klin Monatsbl Augenheilkd 1883; 21 :171-80.
31 . Westhoff, Ziegler. Cited by Theobald.25
32. von Graefe A. Faile von plotzlicher und incurabler Amaurose nach Haematemesis. Graefes Arch Clin Exp Ophthalmol1860; 7(2):14350.
33. Fisher JH. Discussion in paper by Whiting M. Optic atrophy following haemorrhage from the alimentary tract. Trans Ophthalmol Soc UK 1929; 49:151.
34. Harrington DO. The Visual Fields-A Textbook and Atlas of Clinical Perimetry. 2nd ed. StLouis: CV Mosby Co, 1964:186.
35. KOmmell R. Die Sehstorungen nach Blutverlust. In: Schiek F, Bruckner A, eds. Kurzes Handbuch der Ophthalmologie, Berlin: Julius Springer, 1932: 7:62-88.
36. Walsh FB. Clinical Neuro-ophthalmology, Baltimore: Williams & Wilkins, 1947; 1046-8.
37. Uhthoff W. Beitrage zu den Sehstorungen und Augenhintergrundsveranderungen bei Anamie. Ber 0 d Versamme d deutsch ophth Gesellsch, MOnchen 1922; 43:204-12.
38. Wilbrand H, Saenger A. Die plotzlichen, Erblindungen nach Blutverlust. In: Die Neurologie des Auges. 3rd ed. Wiesbaden: JF Bergmann, 1906: part 2, 907-23. '
39. Raehlmann E. Ueber einige Beziehungen der Netzhauteirculation zu allgemeinen Storungen des Blutkreislaufes. Arch f Path Anat, Berlin 1885; 102:221-57.
40. Holden WA. The pathology of the amblyopia following profuse hemorrhage and of that following the ingestion of methyl alcohol, with remarks on the pathogenesis of optic-nerve atrophy in general. Arch Ophthalmol1899; 28:125-34.
41 . Groenouw A. Sehstorungen nach Blutverlusten. In: Graefe-Sae
misch Handbuch Gesamten der Augenheilkunde. Leipzig: Wilhelm Engelmann, 1904; 11(1):304-14.
42. Pincus F. Uber Sehstorungen nach Blutverlust. Graefes Arch Clin Exp Ophthalmol1919; 98:152-70.
43. Terson A. Sur Ia pathogenie et le traitement des troubles visuels apres les pertes de sang. Ann d'Oculistique 1922; 159:23-65.
44. Ronne H. Kurzes Handbuch der Ophthalmologie, Vol 5. Berlin: Julius Springer, 1930; 702-4.
45. Duke-Elder WS. Text-book of Ophthalmology. London: Kimpton, 1941; 3:2556-60.
46. Riser, Felgines, Gayral, Geraud, Ribaut. L'amaurose post-hemorragique. Rev Otoneurolophtalmol1951 ; 23:175-81.
47. Roe 0 . On blindness after loss of blood. Acta Ophthalmol 1942; 20:48-55.
48. Stirling JW. Bilateral amaurosis following severe haemorrhage after extraction of a tooth-partial recovery. Ophthalmic Rev 1904; 23:219-23.
49. Proell. Ueber Sehstorungen nach Blutverlust. Med Klin, Berlin 1908; 444-8.
50. Goulden C. In discussion of paper by Wolff E. The causation of amblyopia following gastric and other haemorrhages. Trans Ophthalmol Soc UK 1935; 55:348.
51 . Reuter J. Sehstorungen nach chirurgischen Eingriffen, hier Erblindung nach magenresektion. Zentralbl Chir 1947; 72:361-3.
52. Grossmann EE, Holm AG. Amblyopia following postthyroidectomy hemorrhage? Relieved with stellate ganglion block and intravenous procaine. Am J Ophthalmol1950; 33:1099-1103.
53. Chisholm lA. Optic neuropathy of recurrent blood loss. Br J Ophthalmol 1969; 53:289-95.
54. Walkup HE, Murphy JD. Retinal ischemia with unilateral blindness -a complication occurring during pulmonary resection in the prone position; report of two cases. J Thorac Cardiovasc Surg 1952; 23:174-5.
55. Sweeney PJ, Breuer AC, Selhorst JB, et al. Ischemic optic neuropathy: a complication of cardiopulmonary bypass surgery. Neurology 1982; 32:560-2.
56. Carlini V. Amaurosi consecutiva ad anemia acuta per emorragia. Clin Ocul, Palermo 1906; 7:2353-68.
57. Gooch. 1830 (cited by Fries4) .
58. Carreras Matas M. Contribuci6n al estudio de Ia atrofia 6ptica en Ia infancia; atrofia 6ptica consecutive a hemorragias de Ia madre, de los ultimos periodos del embarazo. Arch Soc Oftal Hisp-Amer 1954; 14:405-14.
59. Perrin M. Discussion in paper by Terson A. Les troubles visuels apres les pertes de sang. Arch d'Ophtalmol1922; 39:57.
60. Lazaro EJ, Cinotti AA, Eichler PN, Khwaja AA. Amaurosis due to massive gastrointestinal hemorrhages. Am J Gastroenterol 1971 ; 55:50-3.
61 . Grout GH. A case of permanent impairment of vision following gastro-intestinal hemorrhage. Arch Ophthalmol 1914; 43:234-6.
62. Hughes B: Blood supply of the optic nerves and chiasma and its clinical significance. Br J Ophthalmol1958; 42:106-25.
63. Ballen PH, Fox MJ, Weissman GS. Ischemic optic neuropathy secondary to intestinal hemorrhage. Ann Ophthalmol1985; 17:486-8.
64. Calhoun FP. The report of a case of "optic atrophy, caused by uterine hemorrhage." Ophthalmic Record 1913; 22:358-61.
65. de Schweinitz GE. In discussion of paper by Langdon HM. Amaurosis after uterine hemorrhage: With restoration of vision following transfusion. Arch Ophthalmol 1933; 10:101-2.
66. Hayreh SS. Anterior ischaemic optic neuropathy: II. Fundus on ophthalmoscopy and fluorescein angiography. Br J Ophthalmol 1974; 58:964-80.
67. Hayreh SS. Anterior ischemic optic neuropathy. Berlin: SpringerVerlag, 1975; 44.
68. Hayreh SS. Ischemic optic neuropathy. lnt Ophthalmol 1978; 1:9-18.
1501

OPHTHALMOLOGY • NOVEMBER 1987 • VOLUME 94 • NUMBER 11
69. Hayreh SS. Anterior ischemic optic neuropathy. Arch Neural 1981; 38:675-8.
70. Alfano JE, Roper KL. Visual disturbances following acute blood loss. Am J Ophthalmol1954; 38:817-24.
71. Hayreh SS. Anterior ischemic optic neuropathy: V. Optic disc edema an early sign. Arch Ophthalmol 1981; 99:1030-40.
72. Beylot J, Valla! M, Pesme D. N(write optique apres hemorragie digestive. Sem Hop Paris 1976; 52:1921-2.
73. Pergens E. L'amaurose et l'amblyopie apres hematemese. Ann d'Oculistique 1896; 115:5-32.
74. Tidy HL. Loss of vision following haemorrhage. Br Med J 1941; 1:774-6.
75. Barr AS. Amblyopia after hemorrhage. Am J Ophthalmol 1934; 17:396-9.
76. Goldfeder AE, Rapoport KN. Ueber einen durch Bluttransfusion geheilten Fall von scheveren Sehsti:irungen nach Blutverlust. Klin Monatsbl Augenheilkd 1934; 93:666-71.
77. Klewin KM, Appen RE, Kaufman PL. Amaurosis and blood loss. Am J Ophthalmol1978; 86:669-72.
78. Hirschberg J. Amaurose nach Blutverlust. Ber u d Versamml d ophth Gesellsch, Stuttgart 1881; 13:69-72.
79. Pagenstecher A. Ueber Augenhindergrundsveranderungen bei inneren Krankheiten, spec. bei anamischen Zustanden. Arch Augenheilkd, Wiesbaden 1905; 52:237-61.
80. Tassman IS. The Eye Manifestations of Internal Diseases. StLouis: CV Mosby Co, 1942:417-23.
81. Presencia AC, Hernandez AM, Guia ED. Amaurosis following blood loss. Ophthalmologica 1985; 191:119-21.
82. Gowers WR. A Manual and Atlas of Medical Ophthalmoscopy, 4th ed. Philadelphia: Blakiston's Son & Co., 1904:224-230.
83. Cove DH, Seddon M, Fletcher RF, Dukes DC. Blindness after treatment for malignant hypertension. Br Med J 1979; 2:245-6.
84. Hulse JA, Taylor DSI, Dillon MJ. Blindness and paraplegia in severe childhood hypertension. Lancet 1979; 2:553-6.
85. Pryor JS, Davies PO, Hamilton DV. Blindness and malignant hypertension. Lancet 1979; 2:803.
86. Wetherill JH. Blindness after treatment for malignant hypertension. Br Med J 1979; 2:550.
87. Taylor D, Ramsay J, Day S, Dillon M. Infarction of the optic nerve head in children with accelerated hypertension. Br J Ophthalmol 1981; 65:153-60.
88. Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension: V. Hypertensive optic neuropathy. Ophthalmology 1986; 93:74-87.
89. Foulds WS. Visual disturbances in systemic disorders-optic neuropathy and systemic disease. Trans Ophthalmol Soc UK 1969; 89:125-46.
90. Drance SM, Morgan RW, Sweeney VP. Shock-induced optic neuropathy. N Engl J Med 1973; 288:392-5.
91. Jaben SL, Glaser JS, Daily M. Ischemic optic neuropathy following general surgical procedures. J Clin Neuroophthalrnol 1983; 3:23944.
92. Watkins CH, Wagener HP, Brown RW. Cerebral symptoms accompanied by choked optic discs in types of blood dyscrasia. Am J Ophthalmol1941; 24:1374-83.
93. Puppel E. Sehsti:irungen nach Genitalblutungen. Berlin: Monatschr f Geburtsh u Gynaek, 1924; 65:351-8.
94. Ulrich R. Ein neuer ophthalmoskopischer Befund nach Blutverlust. Klin Monatsbl Augenheilkd 1883; 21:183-7.
95. Mackenzie S. Diseases of retina and choroid. I. On anaemia as a cause of retinal haemorrhage. Trans Ophthalmol Soc UK 1884; 4:138-42.
96. Moore RF. Medical Ophthalmology, 2nd ed. London: Churchill 1925; 98-100.
97. Pines N. Retinitis nephritica or albuminurica. Br J Ophthalmol1931; 15:75-101 and 15:129-52.
98. Hodge RL, Lowe RD, Vane JR. The effect of acute increases in blood volume on the concentration of circulating angiotensin in dogs. J Physiol1965; 181 :59P-60P.
99. Bunag RD, Page IH, McCubbin JW. Neural stimulation of release of renin. Circ Res 1966; 19:851-8.
100. Huidobro F, Braun-Menendez E. Secretion of renin by intact kidney. Am J Physiol1942; 137:47-55.
101. Zanchetti A, Stella A. Neural control of renin release. Clin Sci Mol Med 1975; 48(Suppl)2:215-23.
102. Zanchetti A, Stella A, Leonetti G, Morganti A, Terzoli. Control of renin release: a review of experimental evidence and clinical implications. Am J Cardiol 1976; 37:675-90.
103. Hodge RL, Lowe RD, Vane JR. Increased angiotensin formation in response to carotid occlusion in the dog. Nature 1966; 211 :491-3.
104. Thames MD. Renin release: reflex control and adrenergic mechanisms. J Hypertension 1984; 2(Suppl 1 ):57 -66.
105. Kopp U, DiBona GF. Catecholarnines and neurosympathetic control of renal function. In: Fisher JW, ed. Kidney Hormones. London: Fisher-Duncan Ltd., 1986; 3:621-60.
106. Hayreh SS, Servais GE, Virdi PS, et al. Fundus lesions in malignant hypertension: Ill. Arterial blood pressure, biochemical, and fundus changes. Ophthalmology 1986; 93:45-59.
107. Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension: IV. Focal intraretinal periarteriolar transudates. Ophthalmology 1986; 93:60-73.
108. Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension: VI. Hypertensive choroidopathy. Ophthalmology 1986; 93:1383-400.
109. Hayreh SS. Structure and blood supply of the optic nerve. In: Heilmann K, Richardson KT, eds. Glaucoma: Conceptions of a Disease, Pathogenesis, Diagnosis, Therapy. Stuttgart: Georg Thieme, 1978; 78-96.
110. Aim A, Bill A The effect of stimulation of the cervical sympathetic chain on retinal oxygen tension and on uveal, retinal and cerebral blood flow in cats. Acta Physiol Scand 1973; 88:84-94.
111. Hayreh SS. Fluids in the anterior part of the optic nerve in health and disease. Surv Ophthalmol1978; 1-25.
112. Sassi N, Anderson DR. Blockage of axonal transport in optic nerve induced by elevation of intraocular pressure: effect of arterial hypertension induced by angiotensin I. Arch Ophthalmol 1983; 101:94-7.
113. Strandgaard S. Autoregulation of cerebral circulation, in hypertension. Acta Neural Scand 1978; 57(Suppl66):1-82.
1502