Anemia
description
Transcript of Anemia
-
AnemiaRobb Friedman, MDModified by Sean Hesselbacher, MD, Eyal Oren, MD, David Antonetti, MD and Cathy Okuliar, MD
-
What is Anemia?ANEMIA IS NEVER NORMALReduction below normal in the mass of red blood cells in the circulationHemoglobin concentration, hematocrit, RBC countMen: HGB < 14 or HCT < 41%Women: HGB < 12.0 or HCT < 36%
-
Anemia and Volume StatusHGB and HCT are CONCENTRATIONSTherefore dependent upon plasma volumeAcute bleeds not reflected for 24-36 hrsDue to volume deficit being slowly repaired via movement of fluid from extravascular space to intravascularAnemic patients who are dehydrated will not appear anemicPregnant women expand RBCs 25% but plasma volume increases 50%, producing physiologic anemia
-
Anemia: Special CasesErythrocytosisPeople who live at high altitude have greater RBC volumeSmokers have increased HCT impairs the ability of the RBCs to deliver O2African-American HGBs are 0.5 to 1.0g/dL lower than CaucasiansAthletes (increased plasma volume, Fe deficiency, hemolysis, polycythemia, use of performance enhancing agents)
-
Anemia and the ElderlyMultiple studies show that the elderly do not have a lower normal rangeAnemia, while common in the elderly, is still abnormalHGB < 13 in males and < 12 in females associated with an increased relative risk of mortality (1.6 and 2.3 respectively)
-
Anemia: HistoryIs the patient bleeding?NSAIDs, ASAMenstrual history, if applicable (include older women)Prior intestinal surgery?Hx of hemorrhoids, hematochezia, or melena?Past medical history of anemia? Family history?Alcohol, nutritional questionsLiver, renal diseasesEthnicityEnvironmental/work toxins (ie lead)
-
Symptoms of AnemiaDecreased O2 deliveryHypovolemia if acute lossExertional dyspnea, fatigue, palpitations, lightheadednessSevere: heart failure, anginaPica craving for clay or paper productsPagophagia craving for ice
-
Signs of AnemiaTachycardia, tachypnea, orthostasisPallorJaundiceMurmurKoilonychia or Spoon nailsSplenomegaly, lymphadenopathyPetechiae, ecchymosesAtrophy of tongue papillaeHeme + stool
-
The Four Causes of AnemiaDecreased red blood cell productionIncreased red blood cell destructionRed blood cell lossRed blood cell sequestration* Underlying disorder is abnormal production vs. premature loss
-
Decreased RBC productionDeficiency of iron, B12, folateMarrow is dysfunctional from myelodysplasia, tumor infiltration, aplastic anemia, etc.Bone marrow is suppressed by chemotherapy or radiationLow levels of erythropoeitin, thyroid hormone, or androgens
-
Increased RBC destructionRBCs live about 100 daysAcquired: autoimmune hemolytic anemia, TTP-HUS, DIC, malariaInherited: spherocytosis, sickle cell, thalassemia
-
RBC LossBleeding!Obvious vs occultIatrogenic: venesection e.g. daily CBC, surgical, hemodialysisRetroperitoneal
-
Approach to Anemia
-
Approach to AnemiaLOOK AT THE SMEAR!!!!Convenient to separate into three classes based on the size of the RBCMCV and RDWMicrocytosis: < 80 fLNormocytosis: 80-100 fLMacrocytosis: >100 fLCBC, reticulocyte count, Fe, Ferritin, TIBC, folate, B12, LDH, CMP, ESR
-
ReticulocytesNucleated RBCs form in marrow where they mature for 3 days and then spend 1 day in circulation (before maturing to RBC)Given avg life span of RBC of 100 days, 1% of RBCs are destroyed each dayRetics form 1% of circulating RBCs qdNl RBC count is 5 million/uL so marrow makes 50,000 reticulocytes/uL blood qdWith epo, can increase to 250,000 retics/uL blood qd (given nl marrow and replete iron, folate, b12)
-
Reticulocyte CountAssess adequacy of bone marrow response to anemiaMust adjust for the degree of anemia, use Reticulocyte Production IndexRI = (measured retic) x (Hct/45) / (Correction Factor)CF: Hct 41-50 (1); 30-40 (1.5); 20-29 (2); 10-19 (2.5) Reflects increased circulating time for retics as Epo pushes them out of the marrow earlierRI < 1.0 is abnormally low and indicates inadequate marrow response
-
Microcytic AnemiaIron Deficiency AnemiaThallasemia Anemia of chronic diseaseSideroblastic anemia
- Iron Deficiency AnemiaThe definitive test is serum ferritinLow serum ferritin (
-
Iron deficiency
-
ThalassemiaDecreased production of either -globin or -globin chainsAbnormal hemoglobin electrophoresisPolychromasia (dark staining retics), target cells, basophilic stipplingNormal/increased RBC massMentzer index: MCV/RBC ct < 13
-
Alpha-ThalassemiaAlpha-Thalassemia: 4 genes1/4: silent carrier2/4: Alpha-Thalassemia trait, microcytosis and mild anemia3/4: excess Beta-chains form tetramers, results in severe anemia and microcytosis4/4: hydrops fetalisMost common in SE Asian populations
-
Basophilic stippling
-
Beta-Thalassemia2 genes1/2 mutation: Beta-Thal trait, increased Hgb A2, rarely anemic, mild microcytosis2/2 mutation: Beta-Thalassemia disease, Hgb F, microcytosis, anemiaUsually found in people of African or Mediterranean descent but has world-wide distribution
-
Beta - Thalassemia
-
Sideroblastic Anemia
Failure of synthesis of porphyrin ringHereditary Acquired (INH, EtOH, B6 deficiency, Lead) Smear: sideroblasts and basophilic stippling
-
Macrocytic Anemia (MCV>100)Drug Induced (hydroxyurea, AZT, MTX, chemotherapy, anticonvulsants)B12 / folate deficiencyMyelodysplastic syndromeLiver diseaseAlcohol abuseReticulocytes Hypothyroidism
-
Folate and B12Serum folate usually sufficient, but if folate level is normal but folate deficiency is suspected, check serum homocysteine (elevated because of impaired folate dependent conversion of homocysteine to methionine) or RBC-folate.B12 can be spuriously low a more sensitive and specific test is serum methylmalonic acid level, will be increased if B12 is low.Classically check Schilling Test for B12 deficiency (parietal cell antibody or Intrinsic Factor antibody)
-
B12 and Folate Deficiency
-
Myelodysplastic SyndromePrimary bone marrow disorder, often found in elderlyMacrocytosis, anemiaPseudo-Pelger-Huet abnormality the bilobed nucleus
-
Normocytic AnemiaLarge and complicated group of disorders!Hemolytic anemiasAnemia of chronic diseaseBone marrow disorderNutritional (early Fe, B12, folate deficiency)Renal insufficiency
-
Nutritional AnemiasIron deficiency and B12/folate deficiency can present with normocytic anemia esp. if both deficiencies are concurrent.Check iron studies and B12, folate levels.
-
Anemia of Renal InsufficiencyUnremarkable peripheral blood smearInappropriately normal erythropoietin levelAnemia usually severe and symptomatic when Cr > 3.0Mild to moderate anemia found in Cr 1.5-3.0Tx: Epogen or similar, Fe (oral, IV) if iron stores are found to be low
-
Hemolytic Anemias
-
Evaluation of HemolysisLDH: increasesIndirect bilirubin increases (increased Hgb catabolism)Haptoglobin decreasesReticulocyte count increasesUrine hemosiderin test = present in intravascular, absent in extravascular hemolysis!Coombs test: (+) = autoimmune hemolytic anemia(-) consider PNH (abnormal GPI protein, send flow for CD55 and CD59)
-
Hemolytic Anemia: Intrinsic causesSpherocytosis, Sickle Cell
-
More hemolytic anemias
-
Anemia of Chronic DiseaseThought to be a cytokine mediated process which inhibits red blood cell production or interferes with action of erythropoietinTherefore, the disease needs to be inflammatoryDecreased iron utilization/mobilizationSeen with rheumatologic diseases, chronic infections, malignancyIndices: Low Fe, Low TIBC, Nl/increased FerritinMay be seen in conjunction with Fe-deficiency
-
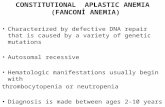
Anemia due to Primary Bone Marrow DisorderMyelodysplastic syndromeBone marrow infiltration: nucleated red blood cells found in circulationMight see rouleaux formation in multiple myelomaWBC, plts often abnormalBone marrow biopsy
-
Anemia: TreatmentsTransfusion triggersCAD: Hgb > 10All pts: Hgb > 7.0Iron supplementationErythropoietin analogsB12, folate
-
What in the world is a Howell-Jolly Body?
-
Acanthocytes vs EchinocytesAcanthocytes: spur cells found in liver diseaseEchinocytes: burr cells found in renal disease
-
Helmet vs. Teardrop Cells
-
Anemia: SummaryANEMIA IS NEVER NORMALDetermine if ACUTE or CHRONICCONSIDER THE FOUR CAUSESCALCULATE the RETIC INDEXLOOK AT THE SMEARCONSIDER THE ETIOLOGY BASED ON RBC MORPHOLOGY AND LABORATORY STUDIESTREAT APPROPRIATELY
-
MKSAP Questions
-
An 80-year-old man who had a hemicolectomy for colon cancer is evaluated because of a 4-month history of diarrhea, anorexia, and fatigue. He had a remote history of alcoholism. On physical examination, he is cachectic and mildly confused. His pulse rate is 70/min, and blood pressure is 140/85 mm Hg. His tongue is smooth. The abdomen is soft; there are no palpable masses or hepatosplenomegaly. A stool specimen is negative for occult blood. Neurologic examination shows loss of position sense in the feet. He has a wide-based gait. The Romberg test is positive. His hemoglobin is 9.4 g/dL, reticulocyte count is 2.5%, mean corpuscular volume is 125 fL, and serum lactate dehydrogenase is 400 U/L. Which of the following is the most likely cause for his symptoms?( A ) Alcoholic cerebellar degeneration ( B ) Vitamin B12 deficiency ( C ) Brain metastases ( D ) Folate deficiency ( E ) Liver metastases
-
Critique (Correct Answer = B) The patient most likely has vitamin B12 deficiency, based on the degree of macrocytosis and neurologic findings. An elevated serum lactate dehydrogenase level, due to intramarrow cell death from ineffective erythropoiesis, is consistent with this diagnosis. Severe macrocytosis (mean corpuscular volume > 120 fL) is often associated with vitamin B12 deficiency or folate deficiency (megaloblastic anemia), usually seen in conjunction with oval macrocytes. The presence of frequent hypersegmented neutrophils (> 5 segments) is strongly suggestive of vitamin B12 or folate deficiency. Bone marrow morphology in patients with vitamin B12 or folate deficiency is referred to as megaloblastic and is characterized by the presence of large cells with immature nuclear chromatin but maturing erythrocyte cytoplasm (nuclear-cytoplasmic dissociation). Anemia accompanies this process; hence the term ineffective erythropoiesis. The intramarrow death of megaloblastic cells causes the serum lactate dehydrogenase level to rise. If a patient has a low serum vitamin B12 or folate level, a bone marrow examination is probably unnecessary. However, the physician should determine the cause of the deficiency. If a patient has a normal serum vitamin B12 or folate level, a bone marrow examination is frequently helpful to exclude myelodysplastic syndromes or other infiltrative marrow disorders. Folate deficiency can induce megaloblastosis within weeks to months, whereas vitamin B12 deficiency requires years to cause megaloblastosis since stores of vitamin B12 persist for years in the liver and other tissues. In patients with vitamin B12 or folate deficiency, parenteral or oral repletion of vitamin B12 or folate reverses some morphologic abnormalities within hours. Serum folate levels fluctuate quickly with changes in dietary consumption. Low erythrocyte folate levels often reflect prior nutritional depletion. In patients who are hospitalized and are begun on regular diets, the erythrocyte folate test may provide a better assessment of tissue folate levels than determination of the serum folate level. The erythrocyte folate test often requires a special laboratory, and results often are not quickly available. In patients with megaloblastic anemias, erythrocyte production is diminished and a corrected reticulocyte count is inappropriately low for the degree of anemia. This patient had a corrected reticulocyte count of 1% (inappropriately low for a hemoglobin level of 9.4 g/dL). In addition to changes in the blood, the epithelial cells in patients with megaloblastic anemias may become atrophic and cause a smooth tongue and cheilosis. Posterior column dysfunction, particularly in patients with vitamin B12 deficiency, may lead to changes in vibratory or position sense, causing ataxia. Signs of dementia may appear. However, neurologic dysfunction is very uncommon in adults with folate deficiency. Alcoholic cerebellar degeneration results in ataxia but not position loss. Although liver metastases are possible in a patient with a history of colon cancer, their presence would not account for the neurological findings in this patient. Brain metastases would most likely produce focal neurological findings and also would not account for the blood findings.
-
A 26-year-old man is evaluated because of progressive fatigue, dyspnea on exertion, and orthostatic dizziness for the past 2 to 3 weeks. He takes no medications. Physical examination is normal except for pallor. Laboratory Studies: Hematocrit 13%Leukocyte count 8300/L; normal differential. Reticulocyte count: 0, Platelet count 320,000/L. A routine biochemical profile, including liver function tests, is normal. A chest radiograph shows normal lung fields and a widened mediastinum, suggestive of an anterior mediastinal mass. Bone marrow biopsy shows absent erythrocyte precursors, normal megakaryocytes, and normal leukocyte numbers and maturation. Which of the following is the most likely cause of the mediastinal mass and anemia?( A ) Hodgkins disease ( B ) Non-Hodgkins lymphoma ( C ) Thyroid carcinoma ( D ) Thymoma ( E ) Germ cell carcinoma
-
Critique (Correct Answer = D) Each of the listed neoplasms may present as an anterior mediastinal mass and may be associated with anemia of chronic disease. However, pure red cell aplasia (which this patient has) is often associated with a benign or invasive thymoma. Approximately 5% to 15% of thymomas occur in patients with pure red cell aplasia. Other thymoma-associated autoimmune disorders include myasthenia gravis, systemic lupus erythematosus, thrombocytopenia, and, rarely, malabsorption states. A careful search by CT or MRI is always warranted in patients with newly diagnosed or relapsing red cell aplasia or myasthenia. The other listed entities are also included in the differential diagnosis for an anterior mediastinal mass. Germ cell tumors have not been associated with pure red cell aplasia, and Hodgkins disease, non-Hodgkins lymphoma, and thyroid carcinoma are rarely associated with this disorder. Chronic lymphocytic leukemia is also commonly associated with red cell aplasia and may present with variable degrees of lymphadenopathy but not with an isolated anterior mediastinal mass, as in the patient discussed here.
-
A 36-year-old black man with known sickle cell anemia is evaluated because of a 2-week history of fever, a macular rash on his trunk, and arthralgias. Subsequently, he developed weakness and dyspnea on exertion. Several of his children had febrile illnesses with associated rashes and fatigue over the past month. These illnesses resolved spontaneously without sequelae. On physical examination, his temperature is 38.8 C (101.8 F), pulse rate is 100/min, and blood pressure is 160/70 mm Hg. A maculopapular, truncal rash is noted. There is conjunctival pallor. The remainder of his examination is unremarkable. Laboratory StudiesHemoglobin 5.2 g/dLLeukocyte count 5000/LReticulocyte count 0%Platelet count 130,000/LSerum lactate dehydrogenase 622 U/LWhich of the following is the most likely diagnosis?( A ) Paroxysmal nocturnal hemoglobinuria ( B ) Parvovirus infection ( C ) Glucose-6-phosphate dehydrogenase deficiency ( D ) Aplastic anemia
-
Critique (Correct Answer = B) Patients with hemolytic disorders may occasionally present with reticulocytopenia and an aplastic crisis. This patient has sickle cell anemia with parvovirus infection, which is causing an aplastic crisis. Parvovirus may infect patients with hemolytic anemias (for example, patients with hereditary spherocytosis, sickle cell disease, or thalassemia). In children with sickle cell anemia, over 80% of aplastic crises may be attributed to parvovirus infections. In adults, the usual presenting features are rash, arthritis, and anemia. The slapped cheek syndrome is rarely a presenting feature. There is usually a complete suppression of erythropoiesis to a reticulocyte level of 0%. The bone marrow shows giant dysplastic (megaloblastoid) erythroblasts, occasionally with viral inclusions. The diagnosis is usually made by demonstrating IgM antibodies to the virus. IgG antibodies appear later during the course of the infection and persist. Parvovirus in the blood may be detected by the polymerase chain reaction, which is the definitive diagnostic method. Occasionally, other blood components such as leukocytes and platelets are affected and result in mild to moderate pancytopenia. The diagnosis of paroxysmal nocturnal hemoglobinuria (PNH) should be considered in patients with bone marrow failure or aplasia, unusual location of thromboses, and unexplained hemolysis. The anemia may be severe, and patients with PNH typically have reticulocytopenia. There is no characteristic finding on bone marrow examination, although the bone marrow of patients with PNH may demonstrate myelodysplastic changes. The diagnosis is based on demonstration of exquisite sensitivity to complement-mediated lysis by the sucrose lysis test or the acidified serum lysis test (Hams test). Glucose-6-phosphate dehydrogenase (G6PD) deficiency is another cause of hemolysis that occasionally is associated with reticulocytopenia. In patients with G6PD deficiency, erythrocytes are subject to oxidative stresses. Hemoglobin becomes oxidized and precipitates within the erythrocytes, which then undergo destruction by the reticuloendothelial system. G6PD deficiency is an autosomal recessive disorder that predominantly affects males. After a hemolytic episode, qualitative assays may be normal because only erythrocytes that are resistant to G6PD remain. The African variant of G6PD is associated with a mild form of hemolysis, whereas the Mediterranean variant is usually severe. Causes include infectious stresses, drugs such as quinidine and sulfonamides, or, in the Mediterranean variant, favism (consumption of fava beans). Therapy requires avoiding certain medications and supportive care in crisis situations. In contrast to this patients presentation, patients with aplastic anemia have pancytopenia with severe anemia, reticulocytopenia, thrombocytopenia, and granulocytopenia. In patients with severe aplastic anemia, the bone marrow examination shows less than 5% cellularity with only residual lymphocytes and plasma cells. The abnormal cells described above that are attributable to parvovirus infection are not seen.
-
A 36-year-old man is evaluated because of fatigue. He has had two episodes of acute gouty arthritis over the past 6 months. He has a 10-year history of significant alcohol use, but he quit drinking 4 months ago. He works in a factory making battery products. A complete blood count obtained prior to elective hernia repair surgery 4 years ago was normal. He takes no medications. On physical examination, his temperature is 37.3 C (99.1 F), pulse is 60/min, and blood pressure is 135/70 mm Hg. His skin is normal. There is slight scleral icterus. There is a blue line at the edge of his gums. The remainder of the examination is normal. Stool specimens are negative for blood on three occasions. Laboratory StudiesHemoglobin 7.5 g/dLMean corpuscular volume 71 flLeukocyte count 9400/LReticulocyte count 5.3%Platelet count 435,000/LSerum lactate dehydrogenase 553 U/LSerum uric acid 11 mg/dLA peripheral blood smear is shown. Which of the following diagnostic studies is most useful for determining the cause of this patients anemia?( A ) Serum iron, total iron-binding capacity, and ferritin levels ( B ) Serum lead levels ( C ) Direct and indirect antiglobulin tests ( D ) Hemoglobin A2 quantitation ( E ) Serum ethanol and folic acid levels
-
Critique (Correct Answer = B) The patient has chronic lead intoxication that can be confirmed by measuring serum lead levels. He has a hypochromic, microcytic anemia with coarse basophilic stippling and reticulocytosis. He also has evidence of hemolytic anemia with increased serum lactate dehydrogenase and indirect bilirubin levels. His physical examination is remarkable for gingival lead lines. Bone marrow examination shows erythroid hyperplasia and ringed sideroblasts. The anemia of lead poisoning fits this description. Sideroblastic anemia with hypochromic indices is typical. Hemolysis is common, and basophilic stippling, blue staining polyribosomal aggregates with mitochondrial fragments in the erythrocytes, is frequently seen. Lead inhibits pyrimidine 5-nucleotidase which normally clears ribosomal fragments. Occupational exposures to lead are relatively uncommon today. However, workers who produce batteries or are exposed to paint, particularly those who remove leaded paint from old buildings, are at greatest risk if they are not protected from inhalation of paint particles during the sanding process. Other manifestations of lead toxicity in adults include peripheral neuropathy, abdominal colic, and saturnine gout (effects of lead on renal tubules that prevent the excretion of uric acid). Chelation therapy is indicated for patients with serum lead levels exceeding 70 g/dL and should be continued until lead levels fall below 40 g/dL. Agents such as EDTA or dimercaprol may also be effective. This patient is unlikely to have iron deficiency since his reticulocytes are increased. In addition, basophilic stippling usually is not seen in patients with iron deficiency. Thalassemia is associated with a microcytic anemia, reticulocytosis, and basophilic stippling. However, a normal complete blood count 4 years ago rules out this possibility. Therefore, quantitative studies to measure hemoglobin A2 are not necessary. Autoimmune hemolytic anemia should be excluded by performing a direct antiglobulin test in any patient who has evidence of hemolysis on a peripheral blood smear. However, the lead lines on this patients gingivae are classic for lead poisoning, and autoimmune hemolytic anemia therefore is less likely. Alcoholism may cause a transient sideroblastic anemia, which resolves with cessation of alcohol intake. Folic acid deficiency may complicate alcoholism but usually presents with macrocytosis.
-
A 22-year-old man is evaluated in the intensive care unit because of bleeding immediately after scoliosis surgery. During surgery, 12 units of packed red blood cells and 12 units of fresh frozen plasma were transfused. There is no history of a bleeding disorder or of drug administration that could affect platelet function. On physical examination, the patient is afebrile. His pulse rate is 100/min, and blood pressure is 110/72 mm Hg. Petechiae are present on his arms, and blood is oozing from the drains. Laboratory StudiesHemoglobin 9.0 g/dLPlatelet count 43,000/LProthrombin time 12 sActivated partial thromboplastin time 32 sPlasma fibrinogen 400 g/dLd-Dimers NegativeWhich of the following is the most likely cause of the thrombocytopenia and bleeding?( A ) Dilutional thrombocytopenia ( B ) Incompatible blood transfusion ( C ) Posttransfusion purpura ( D ) Septic transfusion reaction
-
Critique (Correct Answer = A) Approximately a 50% reduction in the platelet count occurs when transfusions of 1.5 to 2 times the blood volume are given over 4 to 8 hours. Blood stored for more that 2 to 3 days has essentially no platelets, which explains the thrombocytopenia. Fresh frozen plasma contains all of the clotting proteins in normal concentrations. This patient received one unit of fresh frozen plasma for each unit of transfused red blood cells, which resulted in no measurable alteration in the prothrombin time or activated partial thromboplastin time. Incompatible red blood cell transfusions can lead to the development of disseminated intravascular coagulation, which is characterized by thrombocytopenia. The other hallmarks of disseminated intravascular coagulation are absent in this patient, namely, he has a normal fibrinogen, prothrombin time, activated partial thromboplastin time, and negative d-dimers. Posttransfusion purpura is characterized by profound thrombocytopenia that develops 5 to 7 days after a transfusion. It occurs in patients who are negative for the PLA-1 human platelet antigen and have been transfused or pregnant in the past. Posttransfusion purpura almost always occurs in women. Septic transfusion reactions can be associated with thrombocytopenia when either bacteremia or endotoxemia causes disseminated intravascular coagulation. This patient has no indication of either sepsis or disseminated intravascular coagulation.