Anatomy of the Testis
-
Upload
john-rey-abad -
Category
Documents
-
view
223 -
download
0
Transcript of Anatomy of the Testis

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 1/7
Anatomy of the Testis
The testicles are oval shaped, homogeneous low level echogenic structures and measure
approximately 4 x 3 x 2 cm in size. The pediatric testicle measures approximately 1 cubic
centimeter and increases steadily in size from approximately 8 years until puberty when it
reaches mature size. The echo texture of both testicles should be equal and homogeneous (Fig
1a, 1c). The epididymis runs along the posterior aspect of the testicle in a craniocaudal fashion as
it finally reaches the lower pole where it abruptly turns cephalad becoming the ductus deferens.
The epididymal head, or globus major, projects at the cranial end of the testicle and has a slightly
higher echogenicity than the normal testis. It usually measures approximately 10 mm in size and
is best visualized when a small hydrocele is present.
Fig 1 – a. Sagittal view normal with and without Doppler

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 2/7
Fig 1 – b. Mediastinum normal, c. Transverse view normal.
The testicle is enveloped by many layers but is adherent to tunica albuginea (Fig 2a, 2b). The
mediastinum testis is an infolding this tunica albuginea and is the site of entry of vessels and
ducts into the testicle. The mediastinum testis can be visualized as an echogenic linear structure
coursing through the center of the testicle (Fig 1b). The tunica vaginalis is a dual lining structure
containing a visceral and a parietal layer (Fig 2c) and is the site where a hydrocele accumulates.
The scrotal wall is of higher echogenicity than the testicle and should not measure more than 2
mm in size.

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 3/7
Fig 2 – a. Outer layers,
Fig 2 – b. Inner layers,

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 4/7
Physiology
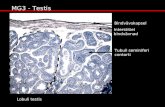
The testes are composed of 90% seminiferous tubules (Sertoli and germ cells) and 10%
interstitial (Leydig Cells, connective tissue, blood supply)
2 major functions of the testes:
I. Spermatogenesis occurs in the Seminiferous Tubules, takes approximately 70 days to
complete, occurs continuously and is regulated by FSH, LH.
Seminiferous tubules
Rete testis
Epididymis – storage and maturation of sperm
Vas/ductus deferens
3 major phases
Mitosis Spermatogonia (germ cells) _ Spermatocytes
Meiosis Spermatocytes (2n) _ Spermatids (1n) haploid like mature sperm
Spermiogenesis spermatids _ mature sperm (sheds cytoplasm, acrosome forms, etc)
Sertoli Cells have supportive function in providing nutrients to developing sperm cells, tight
junctions to provide blood-testis barrier and secrete aqueous secretion into the lumen to aid
sperm transport
II. Biosynthesis of Testosterone (T) – Leydig Cells

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 5/7
Testosterone is synthesized from Cholesterol
Clinical Significance
Ultrasound is the imaging modality of choice for most scrotal and testicular pathology because of
its general availability, low cost, high accuracy, and utilization of nonionizing radiation. The
main indications include acute testicular pain, a palpable mass or scrotal swelling. It is
imperative for the radiology practitioner and residents in training to have broad knowledge of
testicular anatomy, expected normal findings, scanning techniques, pathologic states and disease
processes that affect the testicles, since prompt diagnosis and treatment is vital for outcome.
Hydrocele repair - series
Indications
When the processus vaginalis does not close, or closes after fluid from the abdomen has become
trapped in the scrotal cavity, it is called a hydrocele. The canal (inguinal canal) between the
abdominal cavity (peritoneum) and the scrotum remains open. Fluid from the peritoneum enters
the canal and the scrotum, and causes swelling of the scrotum. In some cases, bowel can also
pass through the processus vaginalis into the scrotum. This is called an inguinal hernia. If a
hydrocele persists past the first six to 12 months of life, it should be surgically repaired. Inguinal

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 6/7
hernia in infants is usually repaired within the first three months of life. It is sometimes difficult
to distinguish a hydrocele from an inguinal hernia on exam.
Normal Anatomy
During development, the scrotal cavity in boys is connected to the abdominal cavity via a
structure called the processus vaginalis. The processus vaginalis usually closes at birth, or soon
after.
Definition
A hydrocele is an accumulation of fluid in any sac-like cavity or duct - specifically in the tunica
vaginalis testis or along the spermatic cord. The condition is caused by inflammation of the
epididymis or testis or by lymphatic or venous obstruction of the cord.
The term hydrocele literally means a sac of water.
Description
Scrotal malignancies are rare and of unknown etiology. There are, however, a number of benign
scrotal conditions that may present as a scrotal mass and must be differentiated from a malignant
process.
A hydrocele is a collection of serous fluid between the two layers of the tunica vaginalis which
normally surrounds the testis. This is the most common benign cause of scrotal swelling and has
been estimated to occur in as many as 1 percent of the adult male population.
Causes
In the pediatric age group, it is usually due to a patent processus vaginalis.
In older men, any process that acts to stimulate increased production of serous fluid (e.g., tumor,
inflammation, trauma) by the tunica or decreases the resorption of this fluid (e.g., inguinal
surgery) by the scrotal lymphatics or venous system will result in the formation of a hydrocele.
Symptoms
Men who appear at a physician's office for the evaluation of a scrotal mass are frequently
asymptomatic. It is not unusual to elicit an incidental history of scrotal or perineal trauma, which
has prompted self-examination and discovery of the mass. The history of frequency, urgency,
and dysuria associated with bacteriuria and of painful scrotal swelling suggests an inflammatory
cause. There may also be pain in the groin or testicle.

8/13/2019 Anatomy of the Testis
http://slidepdf.com/reader/full/anatomy-of-the-testis 7/7
An accurate diagnosis can usually be made solely on the basis of physical findings. A complete
examination of the scrotum - consisting of inspection, palpation, and transillumination - is made
in every case.
The presence of erythema and edema with loss of the normal scrotal rugae is suggestive of an
inflammatory lesion (i.e., epididymitis or epididymo-orchitis.) In the presence of
acuteepididymitis, the epididymis is exquisitely tender to palpation and, in the absence of
orchitis, easily separated from the normal testicle. Pain is aggravated by standing and should be
relieved when the testicle is elevated (Prehn's sign).
A smooth, cystic feeling mass completely surrounding the testicle and not involving the
spermatic cord is characteristic of a hydrocele. A cystic, non-tender mass arising from the head
of the epididymis and distinct from the testicle is characteristic of a spermatocele.
Treatment
When they are small and asymptomatic, hydroceles, spermatoceles, and varicoceles require no
therapy other than reassurance. Indications for intervention include scrotal discomfort or
disfigurement due to the sheer size of the mass. Treatment options include needle aspiration,
aspiration with injection of a sclerosing agent, and surgical excision.
Simple needle aspiration is seldom therapeutic because the cause of the problem is not addressed
and the fluid typically reaccumulates.
Excellent results are possible with either surgical excision or needle aspiration combined with
injection of a sclerosing agent. Success rates ranging from 33 to 100 percent have been reported.
When intervention is indicated, surgical excision is perhaps the most effective form of treatment.
In surgery, the bulk of the hydrocele sac is cut away, and what remains is turned inside out. As a
result, the fluid-secreting surface is now in contact with the inner skin of the scrotum rather than
that of the testicle with which it made previous contact. The scrotal tissue blots up any fluid that
is secreted, unlike the testicular tissue that cannot absorb fluid.












![Malignant mesothelioma of the tunica vaginalis testis: a ...testis. Mesothelioma of the tunica vaginalis testis repre-sent only 0.3–5% of all mesothelial neoplasms [7]. Ac-cording](https://static.fdocuments.in/doc/165x107/60ab9ecd88f9ad6c0664e638/malignant-mesothelioma-of-the-tunica-vaginalis-testis-a-testis-mesothelioma.jpg)





