An optimized buffer system for NMR-based urinary … · 2017. 4. 5. · An optimized buffer system...
Transcript of An optimized buffer system for NMR-based urinary … · 2017. 4. 5. · An optimized buffer system...

PAPER www.rsc.org/analyst | Analyst
An optimized buffer system for NMR-based urinary metabonomics witheffective pH control, chemical shift consistency and dilution minimization†
Chaoni Xiao,ab Fuhua Hao,a Xiaorong Qin,c Yulan Wang*a and Huiru Tang*a
Received 23rd October 2008, Accepted 26th January 2009
First published as an Advance Article on the web 23rd February 2009
DOI: 10.1039/b818802e
NMR-based metabonomics has been widely employed to understand the stressor-induced
perturbations to mammalian metabolism. However, inter-sample chemical shift variations for
metabolites remain an outstanding problem for effective data mining. In this work, we systematically
investigated the effects of pH and ionic strength on the chemical shifts for a mixture of 9 urinary
metabolites. We found that the chemical shifts were decreased with the rise of pH but increased with the
increase of ionic strength, which probably resulted from the pH- and ionic strength-induced alteration
to the ionization equilibrium for the function groups. We also found that the chemical shift variations
for most metabolites were reduced to less than 0.004 ppm when the pH was 7.1–7.7 and the salt
concentration was less than 0.15 M. Based on subsequent optimization to minimize chemical shift
variation, sample dilution and maximize the signal-to-noise ratio, we proposed a new buffer system
consisting of K2HPO4 and NaH2PO4 (pH 7.4, 1.5 M) with buffer–urine volume ratio of 1 : 10 for
human urinary metabonomic studies; we suggest that the chemical shifts for the proton signals of
citrate and aromatic signals of histidine be corrected prior to multivariate data analysis especially when
high resolution data were employed. Based on these, an optimized sample preparation method has been
developed for NMR-based urinary metabonomic studies.
Introduction
NMR-based metabonomics has been widely employed as
a powerful tool to probe the systemic metabolic responses to
perturbations resulting from chemical toxicity,1–4 diseases,5–7
stresses,8 aging9 and nutritional interventions.10–13 However,
inter-sample chemical shift variations can lead to spurious clus-
tering and false interpretation for multivariate data analysis
especially in the cases of urinalysis. Traditionally, the 1H NMR
spectra were bucketed into bins with 0.04 ppm to increase
tolerance for chemical shift variation14–16 and reduce the
computation load. But such large buckets will inevitably
combine the different metabolite signals with the opposite
changes in the same bin, which may obscure the metabolic
changes and overshadow the contributions of low-concentration
metabolites. When smaller buckets17–19 (e.g. 0.004 ppm) or full
resolution NMR data20–22 were employed to maximize informa-
tion output, even small chemical shift variations may cause
noticeable problems in data analysis. Although some post-
acquisition data processing methods for peak alignments23–25
have been proposed during recent years which can reduce
aState Key Laboratory of Magnetic Resonance and Atomic and MolecularPhysics, Wuhan Centre for Magnetic Resonance, Wuhan Institute ofPhysics and Mathematics, The Chinese Academy of Sciences, Wuhan430071, P. R. China. E-mail: [email protected]; [email protected]; Fax: +86-(0)27-87199291; Tel: +86(0)27-87198430bGraduate School of the Chinese Academy of Sciences, Beijing 100049,P.R. ChinacCollege of Chemical Engineering and Technology, Wuhan University ofScience and Technology, Wuhan 430081, P.R. China
† Electronic supplementary information (ESI) available: some 1H NMRspectra for metabolites. See DOI: 10.1039/b818802e
916 | Analyst, 2009, 134, 916–925
chemical shift inconsistency to some extent, these methods are
not effective for the severely overlapped signals and unknown
peaks in 1H NMR spectra. The best strategy is to eliminate such
inconsistency from the sources (e.g. during sample preparation
and data acquisition). Therefore, it is essential to understand
how the factors such as pH and salt concentration affect the
chemical shifts so as to minimize the induced chemical shift
inconsistency.
The pH has a strong impact on the chemical shifts of urinary
metabolites with ionizable groups. Normally, the pH values for
human urine samples26,27 vary from 5.5 to 6.5 and may extend to
4.6–8.0 depending on dietary intakes, xenobiotic treatments and
health status. Urine samples are often composed of carboxylic
acids such as citrate and hippurate, organic amines such as
dimethylamine (DMA) and trimethylamine (TMA), and amino
acids such as glycine, taurine and histidine.28,29 The chemical
shifts of these metabolites are dependent on the sample pH due to
ionization of carboxyl or amino groups, and such dependence
was described previously by the Henderson–Hasselbalch equa-
tion.30 Although the proton chemical shift variation has already
been investigated in previous studies for some urine metabo-
lites29,31,32 including citrate, hippurate, creatinine and glycine, the
studied pH range was limited and organic bases such as DMA
and TMA were not considered.
In addition, urine contains a variable amount of ionic
species27,33 such as Na+ (90–240 mmol/L), K+ (34–68 mmol/L),
Ca2+ and Mg2+ (1–10 mmol/L), which may also affect the
metabolite chemical shifts due to both ionic strength and bind-
ings. For example, the inter-sample chemical shift variation
for citrate may result from the difference of the divalent
cation concentrations34 apart from pH variation. A recent study
This journal is ª The Royal Society of Chemistry 2009

showed35 that the addition of about 4.2 mM EDTA to urine
reduced chemical shift changes for some metabolites such as
citrate and alanine, resulting from the stronger bindings of
EDTA with Ca2+ and Mg2+. However, signals of EDTA and its
complexes with Ca2+ and Mg2+ (about 6 peaks) will be intro-
duced, which may overlap with other metabolite signals in NMR
spectra; EDTA will not easily remove the chemical shift changes
induced by other ions such as Na+ and K+ (i.e. ionic strength).
Therefore, some systematic investigations remain to be per-
formed to understand the effects of ionic strength on urinary
signal variability.
In order to reduce the chemical shift variation for the
metabonomics studies, the pH consistency was controlled by
adjusting the sample pH to a fixed value or using buffer. For
example, hydrochloric acid was used to adjust the urine pH to
about 2.5 in some studies of inborn error of metabolism.36,37
Although this method was effective to reduce the inter-sample
pH variation, it was labor-intensive and not suited for high
throughput studies especially when hundreds of samples were
involved. In addition, such pH is close to the pKa values of most
amino acids (e.g. pKa z 1.5–2.6) and their proton chemical shifts
will be sensitive to any minor pH changes; such strong acidity can
also cause the degradation of some metabolites (e.g. hydrolysis).
In the other method, NaH2PO4/Na2HPO4 buffer38,39 was
employed to stabilize the urine pH to about 7.4 though a few
studies40–42 were carried out at pH 5.0, 7.1 and 7.3. However, high
concentration buffer cannot be employed, due to low water
solubility of Na2HPO4$12H2O, limiting the buffer capacity. In
addition, Na2HPO4$12H2O often precipitates even at moderate
buffer concentration (e.g. 0.2 M) during low temperature
storage, causing the changes of buffer composition and capacity.
Recently, attempts have been made to optimize buffer systems
for metabonomic urinalysis: a final buffer concentration of 0.3 M
was recommended for normal human urine and 1 M for
concentrated samples.26 Although this method will undoubtedly
bring the sample pH to a constant, such a high salt concentration
may conceivably cause potential difficulties for tuning and
matching of the probe circuits and adverse effects on the signal-
to-noise ratio (SNR). Sample dilution will further reduce the
SNR with the recommended buffer–urine volume ratio of 1 : 2.
Therefore, buffer optimization is still required to comprehen-
sively consider the pH control, dilution minimization and SNR.
In this work, we systematically investigated the effects of pH
and ionic strength on 1H NMR chemical shifts using a mixture
solution of 9 typical urinary metabolites including acetate, hip-
purate, citrate, DMA, TMA, creatinine, glycine, histidine and
urea. The dependence of chemical shifts on pH and ionic strength
was discussed and the optimal pH and ionic strength were
determined. Based on verification with 10 human urine samples,
we proposed a K2HPO4/NaH2PO4 buffer system and recom-
mended a new urine preparation method for the NMR-based
metabonomic studies.
Experimental
Chemicals
Acetate, hippurate, citrate, dimethylamine (DMA), trimethyl-
amine (TMA), creatinine, glycine, histidine, urea, NaCl, NaOH,
This journal is ª The Royal Society of Chemistry 2009
HCl, K2HPO4, Na2HPO4$12H2O and NaH2PO4$2H2O were all
purchased as analytical grade from Guoyao Chemical Co. Ltd.
(Shanghai, China) and used without further treatments. Deute-
rium oxide (D2O, 99.9% D) and sodium 3-trimethly-
silyl[2,2,3,3-2H4] propionate (TSP) were purchased from
Cambridge Isotope Laboratories, Inc. (MA, USA). Double
distilled water purified on a Millipore system was used for
preparing all the solutions.
Urine sample collection
Spot urine samples were collected from 5 male and 5 female
healthy volunteers aged between 28 and 63 years old, without
diet restriction, and were used immediately after collection.
pH measurements
The pH values were measured using a Mettler Toledo pH meter
(Delta 320) equipped with a Mettler Toledo combination glass
electrode at room temperature (25–26 �C). The pH meter was
calibrated using commercially available two-point standard
buffers (pH 4.01 and 7.00) before measurements. All the pH
measurements were performed three times to ensure accuracy
before NMR experiments.
Sample preparation for NMR measurements
A series of solutions containing various NaCl concentrations
were prepared with a mixture of 9 typical urinary metabolites
including acetate, hippurate, citrate, creatinine, DMA, TMA,
glycine, histidine (about 1.0 mM each) and urea (30 mM). Each
of the solutions (pH, �6.0) was then divided into 22 aliquots, the
aliquot (0.55 mL) was added by 0.05 mL D2O containing TSP
(0.1%, m/v), where D2O was used as a field lock and TSP as an
internal chemical shift reference. The aliquots were titrated with
either 0.2 M HCl or 0.2 M NaOH solution to obtain the pH
range from 1.5 to 12.7 with about 0.5 unit intervals. The NaCl
concentrations in the titrated solutions were 0, 0.1, 0.2, 0.5 and
1.0 M, respectively. A total of 110 solutions so prepared were
subjected to 1H NMR analysis to obtain chemical shifts of those
metabolites at different pH values and ionic strengths.
Two buffer systems were prepared in D2O containing TSP
(0.05%, m/v) for pH control of the human urine samples, namely,
sodium phosphate buffer solution (0.2 M, pH 7.4) consisting of
Na2HPO4$12H2O and NaH2PO4$2H2O (molar ratio of 4 : 1),
and potassium sodium buffer solutions (0.2, 0.5, 1.0, 1.5 and
2.0 M, pH 7.4) with K2HPO4 and NaH2PO4$2H2O (molar ratio
of 4 : 1).
Two human urine samples, A (pH 5.8) and B (pH 6.3), were
employed to optimize buffer concentration and the buffer-to-
urine volume ratio (VBuffer/VUrine). The aliquot urines (4 mL)
were added with the variable amount of K2HPO4/NaH2PO4
buffer (0.2, 0.5, 1.0, 1.5 and 2.0 M, pH 7.4), from 0.0 to 2.0 mL
with 0.2 or 0.4 mL intervals, respectively. For the validation
of the optimized buffer system, 10 human urine samples (pH,
5.8–8.0) were mixed with K2HPO4/NaH2PO4 buffer (0, 0.5, 1.5
and 2.0 M) at VBuffer/VUrine (1 : 10) corresponding to the final
buffer concentrations (CFB) of 0, 0.045, 0.136 and 0.181M,
respectively. For the purpose of comparison, the same 10 urine
samples were prepared with Na2HPO4/NaH2PO4 buffer in the
Analyst, 2009, 134, 916–925 | 917

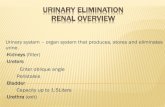
Fig. 1 The structures of some urinary metabolites.
traditional way (0.2 M; pH 7.4; VBuffer/VUrine 1 : 2) giving a CFB
of 0.067 M. The buffered urine samples (0.6 mL) were then
transferred into 5 mm diameter NMR tubes, respectively,
following agitation and centrifugation (10 000 rpm, 10 min), for
NMR analysis.
NMR measurements
The 1H NMR spectra were acquired at 298 K on a Bruker AVII
500 MHz spectrometer operating at 500.13 MHz equipped with
an inverse triple resonance probe (TXI) with a shielded Z-
gradient. The standard one-dimensional pulse sequence (RD–
90�–t1–90�–tm–90�–acquisition) was employed with a weak
continuous wave irradiation equivalent to 50 Hz during the
recycle delay (RD, 2 s) and mixing time (tm, 0.1 s) to suppress
water signal. t1 was set to 4 ms and the 90� pulse length was
adjusted to about 10 ms for each sample individually. For all the
spectra, 32 transients were accumulated with 32k data points and
a spectral width of 20 ppm. An exponential line-broadening
factor of 1 Hz was applied to all free induction decays and zero-
filled to 64k prior to Fourier transformation. Chemical shifts of
the proton resonances were recorded relative to an internal
reference (TSP, 0.0 ppm).
Titration data analysis
The pH dependence of 1H NMR chemical shifts of the tested
metabolites in the mixture was fitted into the modified Hender-
son–Hasselbalch equation30 (eqn (1)),
dobs ¼ dmin þXi¼1; n
�Di =
1þ 10ðpH�pKaiÞ
�(1)
where dobs is the observed chemical shift at a given pH, dmin is
chemical shift of a metabolite in the fully ionized form; pKai and
Di denote the apparent ionization constant and the chemical shift
difference between fully ionized and unionized forms for the ith
equilibrium process, respectively; n is the number of ionization
processes in a molecule. The ionization constant has a relation-
ship with ionic strength (I) as described by the following equa-
tion43 (eqn (2)),
pKa � pKa0 ¼ xI1/2 � jI (2)
where pKa and pKa0 are ionization constants with a given ionic
strength and no salts, respectively; x and j are two constants
associated with ion interactions in the system studied.
Results and discussion
The effects of pH and ionic strength on 1H chemical shifts of
urinary metabolites
A mixed solution of acetate, hippurate, citrate, DMA, TMA,
creatinine, glycine, histidine and urea (the structures of them
were shown in Fig. 1) was employed to consider the most
abundant urinary metabolites representing carboxylic acids
(acetate, hippurate and citrate), amines (DMA and TMA), and
amino acids (glycine and histidine); the majority of these
metabolites exhibit high sensitivity to chemical shifts against pH
variations due to their ionizable groups. Fig. 2 shows the
918 | Analyst, 2009, 134, 916–925
dependence of 1H NMR chemical shifts on pH (1.5–12.7) of the
solutions containing different NaCl concentrations (0, 0.1, 0.2,
0.5 and 1.0 M). The open symbols were the measured data points
and solid lines represented the theoretically calculated data from
the Henderson–Hasselbalch equation (eqn (1))30 at a given NaCl
concentration. The pKa and D values were obtained by fitting the
dependence of chemical shifts on pH at 5 salt concentrations and
are tabulated in Table 1; the reported errors in these values were
standard errors generated from the fitting processes. To the best
of our knowledge, this is the first time that the impacts of pH and
ionic strength on the chemical shifts of all these 9 urinary
metabolites are investigated systematically in such broad ranges
of pH and salt concentration (ionic strength).
The titration profiles for all the tested metabolites (Fig. 2)
clearly showed dependence of the chemical shifts on the sample
pH and salt concentration. Visual inspection noticed that the
chemical shifts of citrate, creatinine, DMA and TMA had a high
sensitivity on ionic strengths whereas those of other metabolites
such as glycine and histidine only exhibited a mild salt sensi-
tivity. At a given salt concentration, 1H chemical shifts for the
metabolites decreased with the increase of pH (as also shown in
Fig. S-1 in the ESI†). Similar results were also observed for
citrate, creatinine, hippurate and glycine in a previous study31
though in a much narrower pH range (3.8–7.9). Such chemical
shift changes were originated from the pH-induced alteration in
ionization process of the functional groups and thus the electron
density around the nuclei concerned. For carboxyl and amino
groups, the increase of pH leads to the increase of RCOO� or
the decrease of RNH3+ concentration which enhances field-
shielding effects on the protons in the molecules, and thus
moving the proton peaks to upper field (or smaller chemical
shift values).
In addition, the pH titration curves for all metabolite chemical
shifts went through some transitions associated with the
This journal is ª The Royal Society of Chemistry 2009

Fig. 2 The pH dependence of the 1H NMR chemical shifts for some urinary metabolites in the model solutions containing NaCl of 0 M (,), 0.1 M (B),
0.2 M (O), 0.5 M (P) and 1.0 M (>); salt concentration increased from blue to red lines; the inserts showed regional expansions; open symbols were the
measured data points and the solid curves were calculated data from eqn (1).
ionization processes of relevant functional groups (Fig. 2). For
example, only one transition was observed for acetate, hippurate,
DMA and TMA at pH 4.76, 3.62, 11.38 and 10.15, respectively,
which coincided with pKa values of their only functional groups;
a single transition at pH 4.89 for creatinine is also in reasonable
agreement with the ionization of the –CONH group (reported
pKa z 4.8);44 for glycine, two transitions at pH 2.33 and 10.01
coincided with the pKa values of its carboxyl and amino groups.
In theory, citrate ought to have three transitions owing to its
three carboxyl groups (pKa, 3.13, 4.7 and 6.4).44 Our experi-
mental data, however, only showed one broad transition at pH
3–6 which was probably because the ionization constants for
three carboxyl groups were too close to each other. For histidine,
apart from two transitions at pH ca. 1.50 and 9.48 associated
with the carboxyl and amino groups, another transition was
clearly observable at pH z 6.1 from 2-CH, 5-CH and b-CH2
which resulted from the ionization of the NH group in the
imidazole ring (reported pKa 6.04).44
This journal is ª The Royal Society of Chemistry 2009
Furthermore, the maximum chemical shift changes resulting
from the pH-induced transitions differed markedly for different
metabolites as indicated by the D values in Table 1. In general,
ionization of a carboxyl group led to the D values of 0.16–0.36
ppm (e.g. CH3 of acetate, CH2 of hippurate and a-CH2 of
glycine), whereas ionization of an amino group showed the D
values of 0.37–0.69 ppm (a-CH2 of glycine, CH3 of DMA and
TMA). This is probably related to the difference of ionizable
groups (–COOH, –NH2 and N–H) or charge distributions.
Moreover, different proton resonances of the same metabolite
also showed the different D values. For example, the ionization
of the carboxyl group in hippurate resulted in much greater
chemical shift changes for CH2 (0.22 ppm) than for aromatic
protons (�0.01 ppm); the ionization of –CONH in creatinine led
to larger chemical shift changes for CH2 (0.23 ppm) than for CH3
(0.08 ppm). This is not surprising and can be explained by
proximity effects of the ionizable groups on the observed
protons, which is in reasonable agreement with previous findings
Analyst, 2009, 134, 916–925 | 919

Table 1 The pKa and D values of the metabolites in the mixture with different NaCl concentrations
Compound NaCl (M) pKa1a Db pKa2 D pKa3 D
d1H(pH z 7.4)
Acetate (CH3) (pKa 4.76)c 0 4.76 � 0.00 0.16 � 0.01 1.9220.1 4.62 � 0.00 0.16 � 0.010.2 4.58 � 0.00 0.16 � 0.010.5 4.53 � 0.00 0.16 � 0.011.0 4.47 � 0.00 0.16 � 0.01
Hippurate (CH2) (pKa 3.62) 0 3.62 � 0.01 0.22 � 0.00 3.9740.1 3.45 � 0.01 0.22 � 0.000.2 3.41 � 0.02 0.23 � 0.000.5 3.37 � 0.01 0.23 � 0.001.0 3.28 � 0.02 0.23 � 0.00
Hippurate (o-ArH) 0 5.00 � 0.01 0.01 � 0.00 7.8460.1 4.84 � 0.01 0.01 � 0.000.2 4.79 � 0.01 0.01 � 0.000.5 4.73 � 0.01 0.01 � 0.001.0 4.85 � 0.05 0.01 � 0.00
Hippurate (p-ArH) 0 2.43 � 0.97 0.009 � 0.007 7.6400.1 2.08 � 1.47 0.009 � 0.010.2 1.90 � 2.25 0.009 � 0.0270.5 — —1.0 — —
Citrate (CH) pKa
(3.13,4.7,6.4)0 3.15 � 0.18 0.13 � 0.01 4.73 � 0.25 0.09 � 0.01 6.30 � 0.08 0.09 � 0.01 2.6430.1 2.91 � 0.12 0.14 � 0.01 4.32 � 0.14 0.08 � 0.01 5.74 � 0.04 0.09 � 0.010.2 2.95 � 0.09 0.15 � 0.01 4.25 � 0.15 0.09 � 0.01 5.49 � 0.03 0.09 � 0.010.5 2.94 � 0.04 0.12 � 0.01 4.41 � 0.07 0.10 � 0.01 5.45 � 0.04 0.12 � 0.011.0 2.48 � 0.13 0.17 � 0.01 3.83 � 0.15 0.09 � 0.01 5.01 � 0.04 0.10 � 0.01
Citrate (CH0) 0 3.13 � 0.05 0.10 � 0.01 4.63 � 0.08 0.12 � 0.01 6.17 � 0.05 0.16 � 0.01 2.5520.1 2.92 � 0.02 0.10 � 0.01 4.28 � 0.03 0.13 � 0.01 5.69 � 0.02 0.15 � 0.010.2 2.94 � 0.03 0.09 � 0.01 4.25 � 0.07 0.13 � 0.01 5.49 � 0.04 0.16 � 0.010.5 2.89 � 0.01 0.07 � 0.00 4.26 � 0.02 0.14 � 0.00 5.44 � 0.02 0.17 � 0.001.0 2.62 � 0.04 0.09 � 0.00 3.91 � 0.08 0.15 � 0.01 5.03 � 0.05 0.15 � 0.01
DMA (CH3) (pKa 10.8) 0 11.38 � 0.03 0.45 � 0.01 2.7280.1 11.58 � 0.03 0.47 � 0.010.2 11.59 � 0.04 0.48 � 0.010.5 11.60 � 0.05 0.49 � 0.011.0 11.67 � 0.04 0.50 � 0.01
TMA (CH3) (pKa 9.8) 0 10.15 � 0.02 0.69 � 0.01 2.9000.1 10.41 � 0.03 0.69 � 0.010.2 10.55 � 0.02 0.71 � 0.010.5 10.58 � 0.04 0.71 � 0.011.0 10.78 � 0.02 0.73 � 0.01
Creatinine (CH3)(pKa 4.83, 9.2)
0 4.89 � 0.01 0.08 � 0.01 3.0460.1 4.95 � 0.01 0.08 � 0.010.2 5.01 � 0.01 0.08 � 0.010.5 5.04 � 0.01 0.08 � 0.011.0 5.06 � 0.01 0.08 � 0.01
Creatinine (CH2) 0 4.92 � 0.01 0.23 � 0.01 4.0600.1 4.96 � 0.01 0.23 � 0.010.2 5.00 � 0.01 0.23 � 0.010.5 5.02 � 0.01 0.24 � 0.011.0 5.03 � 0.01 0.24 � 0.01
Glycine (CH2)(pKa 2.34, 9.6)
0 2.33 � 0.05 0.36 � 0.02 10.01 � 0.02 0.37 � 0.00 3.5640.1 2.30 � 0.08 0.36 � 0.03 10.06 � 0.03 0.37 � 0.000.2 2.38 � 0.07 0.35 � 0.02 10.10 � 0.03 0.37 � 0.000.5 2.36 � 0.08 0.35 � 0.02 10.14 � 0.04 0.37 � 0.011.0 2.30 � 0.06 0.36 � 0.02 10.16 � 0.03 0.38 � 0.01
Histidine (a-CH)(pKa 1.82, 6.04, 9.33)
0 0.88 � 0.63 1.88 � 2.49 6.30 � 0.20 0.03 � 0.00 9.48 � 0.01 0.48 � 0.00 3.9850.1 1.41 � 0.32 0.74 � 0.41 6.28 � 0.32 0.04 � 0.00 9.45 � 0.02 0.47 � 0.010.2 1.72 � 0.17 0.49 � 0.11 6.46 � 0.27 0.05 � 0.00 9.49 � 0.03 0.47 � 0.010.5 1.75 � 0.15 0.48 � 0.09 6.54 � 0.29 0.05 � 0.00 9.49 � 0.03 0.48 � 0.011.0 1.74 � 0.13 0.48 � 0.07 6.93 � 0.25 0.07 � 0.00 9.55 � 0.04 0.46 � 0.01
Histidine (b-CH2) 0 1.22 � 0.45 0.28 � 0.24 6.09 � 0.02 0.13 � 0.00 9.48 � 0.01 0.27 � 0.00 3.2110.1 1.23 � 1.06 0.30 � 0.59 6.12 � 0.06 0.13 � 0.00 9.43 � 0.03 0.27 � 0.000.2 1.44 � 0.82 0.24 � 0.34 6.17 � 0.07 0.13 � 0.00 9.45 � 0.03 0.27 � 0.000.5 1.53 � 0.41 0.20 � 0.13 6.32 � 0.06 0.14 � 0.00 9.47 � 0.03 0.27 � 0.001.0 1.72 � 0.36 0.13 � 0.05 6.40 � 0.08 0.15 � 0.00 9.52 � 0.04 0.27 � 0.00
Histidine (2-CH) 0 6.11 � 0.01 0.91 � 0.00 7.7900.1 6.12 � 0.01 0.89 � 0.000.2 6.14 � 0.03 0.92 � 0.000.5 6.23 � 0.01 0.90 � 0.001.0 6.23 � 0.02 0.91 � 0.01
920 | Analyst, 2009, 134, 916–925 This journal is ª The Royal Society of Chemistry 2009

Table 1 (Contd. )
Compound NaCl (M) pKa1a Db pKa2 D pKa3 D
d1H(pH z 7.4)
Histidine (5-CH) 0 6.14 � 0.01 0.13 � 0.00 9.49 � 0.02 0.33 � 0.00 7.0640.1 6.17 � 0.01 0.13 � 0.00 9.43 � 0.04 0.33 � 0.000.2 6.17 � 0.04 0.13 � 0.01 9.50 � 0.11 0.34 � 0.000.5 6.27 � 0.02 0.14 � 0.00 9.43 � 0.04 0.34 � 0.001.0 6.29 � 0.03 0.13 � 0.00 9.51 � 0.07 0.34 � 0.00
a The fitted data of pKa. b The chemical shift difference between the ionized and unionized forms. c The pKa values in ref. 44; —: pKa was not obtainedfrom the fitted process.
Fig. 3 The effects of pH on the 1H NMR data for some urinary
metabolites without added salt (the solid lines were for visual guidance
only): (A) the chemical shift changes relative to that at pH 7.4 (Dd ¼ dpH
� d7.4, dpH and d7.4 were chemical shifts at a given pH and at pH 7.4,
respectively); the insert showed the regional expansion for pH 6.7–7.8; the
keys for symbols: histidine 5-CH (C) and 2-CH (B), citrate CH (,) and
CH0 (-), glycine (�), TMA (O), DMA (:), acetate ( ), creatinine (P)
and hippurate (*); (B) the intensity of urea signal relative to TSP as
a function of pH.
from the pH effects on 13C chemical shifts for short chain fatty
acids.45,46 It is interesting to note that ionization of a functional
group will induce small changes to the chemical shift of a given
proton when it is positioned six bonds away from the group. For
instance, 2-CH of histidine is more than six bonds away from the
amino and carboxyl groups and shows no chemical shift transi-
tions from the ionization of these two groups. Similarly, the
ionization of the carboxyl group induced small chemical shift
changes (D < 0.01 ppm) for aromatic protons of hippurate which
are located at more than seven bonds from the group.
The above discussion indicated that maximum chemical shift
changes occurred when pH was close to pKa. However, when the
pH was more than two units away from the pKa value (i.e. pH <
pKa � 2, pH > pKa + 2) of a given ionizable group, the proton
chemical shifts will no longer be sensitive to the ionization of the
group, which is clearly illustrated by the data of acetate (Fig. 2).
For all tested metabolites, their chemical shifts showed less pH
dependence at the extreme pH (i.e. pH < 1.5 and pH > 12) and
perhaps at neutral pH as well. The extreme acidic and basic
conditions are not suitable for urinary metabonomics studies
because such harsh conditions may lead to chemical degradation
such as hydrolysis and be drastically different from the normal
physiological conditions (urine pH z 4.8–8.0). Therefore, only
the neutral pH range seems to be the best choice and deserves
more detailed analysis.
Fig. 3A displayed the changes of chemical shifts relative to that
at pH 7.4 with no added salt. Within the pH range of 7.1–7.7 (as
shown in the inserted expansion), most metabolite resonances
had a chemical shift variation of 0.002 ppm or less with the
exception noted only for the proton resonances of citrate (<0.008
ppm) and histidine (<0.02 ppm). At such a pH region, it is also
beneficial to extract information about exchangeable protons.
This was clearly illustrated in Fig. 3B, where the urea signal
intensity relative to TSP (d 0.0) showed little changes in the pH
range of 7.1–7.7, but significantly diminished in the mild acid (pH
< 5) and base (pH > 9) probably due to the enhanced exchange
rate of exchangeable protons (–NH2).
To understand how ionic strength affects the chemical shifts at
the optimized pH region (7.1–7.7), the 1H chemical shift varia-
tions of the metabolite mixture were plotted as a function of the
added NaCl concentrations at a fixed pH (7.40 � 0.05) (the 1H
NMR spectra were also shown in Fig. S-2 of the ESI†). Fig. 4A
showed that an increase of NaCl resulted in a clear increase of
chemical shifts except for one signal of citrate. When the salt
concentration was lower than 0.15 M, the proton chemical shift
variations was less than 0.004 ppm for most metabolites.
This journal is ª The Royal Society of Chemistry 2009
The exception was clearly observable for the high field doublet of
citrate (about 0.005 ppm) and two imidazole protons (about
0.008 ppm) in histidine. It was noted that two protons of citrate
behaved differently, the exact reason for such a difference
remains unknown even though it may be related to their spatial
Analyst, 2009, 134, 916–925 | 921

Fig. 4 The effects of ionic strength on the NMR and pKa data for some
urinary metabolites at pH z 7.4: (A) the chemical shift changes as
a function of NaCl (Dd ¼ dI � d0, where dI and d0 represented chemical
shifts at a given salt concentration and at no added salt, respectively); the
solid lines were for visual guidance only; (B) the pKa changes as a func-
tion of NaCl (pKa and pKa0 were the calculated ionization
constants based on eqn (2) at the given salt concentration and at no added
salt, respectively); (C) the signal-to-noise ratio of the NMR signals
normalized against that for salt-free solution as a function of NaCl
concentration; the solid lines were for visual guidance only; the keys for
symbols: histidine 5-CH (C) and 2-CH (B), citrate CH (,) and CH0
(-), glycine (�), TMA (O), DMA(:), acetate ( ), creatinine (P) and
hippurate (*).
positioning. The effects of ionic strength on chemical shifts were
observed for amino acid residues of some proteins and explained
as the electrostatic effects47 or pKa dependence of salts.48 For all
metabolites studied here, the salt-induced pKa changes were
922 | Analyst, 2009, 134, 916–925
fitted to the empirical relationship described in eqn (2) (Fig. 4B).
Over the salt concentration of 0–1.0 M, the pKa values of the
carboxyl groups in acetate, citrate and hippurate decreased with
the increase of ionic strength whereas those of amino groups in
DMA, TMA and creatinine showed opposite trends. However,
glycine and histidine showed broad increases of pKa for both
amino and carboxyl groups, which were also observed in the
potentiometric titration studies of some other amino acids
reported previously.43 Therefore, our results indicated that the
salt dependence of chemical shifts was probably due to alteration
of ionization constants. Furthermore, the signal-to-noise ratio
(SNR) for the same signals at different salt concentrations was
calculated against the area of the same baseline region (�2 to �5
ppm). Fig. 4C clearly showed that the normalized SNR for each
metabolite decreased with the rise of salt concentration, and the
SNR reduction was less than 15% when the salt concentration
was below 0.15 M compared with the salt-free solution.
All these observations from the metabolite mixture suggested
that, when the small buckets (e.g. 0.004 ppm) were employed in
multivariate data analysis for NMR-based urinary metabonomic
studies, the pH range of 7.1–7.7 and the added salt concentration
of 0.15 M should be targeted to minimize the chemical shift
variation. However, it is still necessary to optimize the buffer
conditions for real urine samples.
Optimizing urine sample preparation
Phosphate salt (H2PO4�/HPO4
2�) has a pKa value49 of 6.8 and
thus good buffer capacity in the pH range of 5.8–7.8, which is
well suited for the targeted urine pH control (7.1–7.7). In tradi-
tional metabonomics studies, NaH2PO4/Na2HPO4 buffer was
often used to control the pH of urine samples. However, high
concentration buffer cannot be allowed due to the low solubility
of Na2HPO4$12H2O (4.2 g/100g water, 20 �C), and thus a large
amount of buffer has to be added to urine, which will inevitably
cause sample dilution. Furthermore, Na2HPO4$12H2O often
precipitates even with moderate buffer concentration (e.g. 0.2 M)
during low temperature storage, resulting in changes of buffer
composition. It is therefore desirable to seek alternative buffer
systems with high buffer capacity to overcome the above short-
comings.
We chose K2HPO4 and NaH2PO4 salts as the buffer pair
because both of them have high solubility (K2HPO4, 167g/100g
water; NaH2PO4$2H2O, 15.6g/100g water; 20 �C). Two of 10
human urine samples, designated A (4 mL, pH 5.8) and B (4 mL,
pH 6.3), were titrated with K2HPO4/NaH2PO4 buffer (pH 7.4) at
5 different concentrations (0.2, 0.5, 1.0, 1.5 and 2.0 M). The
results (Fig. 5A and 5B) showed that, for both urine samples,
their pH values were responsive to the volume and concentration
of buffer added. To reach the optimal pH range (7.1–7.7) dis-
cussed in the earlier section, sample A required the buffer–urine
ratios (VBuffer : VUrine) to be greater than 1 : 2 for 0.2 M buffer
and about 1 : 10, 1 : 20 for 1.5 and 2.0 M buffers, respectively. As
for sample B with a higher initial pH, the ratios were merely 1 : 2,
1 : 20, less than 1 : 20 for 0.2, 1.5 and 2.0 M buffers, respectively.
It is clear that the urine pH was only determined by the final
buffer concentration CFB (Fig. 5C). For the traditional urine
preparation method (0.2 M buffer, pH¼ 7.4, VBuffer : VUrine¼ 1 :
2, CFB ¼ 0.067 M), samples A and B had about 30% dilution and
This journal is ª The Royal Society of Chemistry 2009

Fig. 5 Optimization of the buffer system (the solid lines were for visual guidance only): (A) the pH values of human urine sample A (4 mL, pH 5.8) as
titrated with buffer concentration of 0.2 M (B), 0.5 M (P), 1.0 M (O), 1.5 M (,), 2.0 M ( ); (B) the pH values of human urine sample B (4 mL, pH 6.3)
as titrated with buffer concentration of 0.2 M (C), 0.5 M (;), 1.0 M (:), 1.5 M (-) and 2.0 M (�); (C) the urine pH values as a function of the
final buffer concentration (CFB) for sample A (lower curve) and B (upper curve); (D) the signal-to-noise ratio (SNR) as a function of CFB for sample B
NMR spectra (relative to that without buffer); the keys for symbols: histidine 5-CH (C), citrate CH (,), glycine (�), DMA (:), creatinine (P) and
hippurate (*).
their pH values can only be adjusted to 7.00 and 7.20. In contrast,
when 1.5 M buffer (pH ¼ 7.4, VBuffer : VUrine ¼ 1 : 10, CFB ¼0.136 M) was used, both urine samples had only less than 10%
dilution and their pH values reached to 7.20 and 7.35, respec-
tively. Similarly, the use of 2.0 M buffer (pH ¼ 7.4, VBuffer :
VUrine¼ 1 : 10, CFB¼ 0.181 M) can make both samples reach pH
7.23 and 7.40, respectively. Therefore, the higher concentration
buffer is beneficial to control the sample pH to the optimal level
with much less sample dilution.
However, a high salt concentration has some adverse effects
on the signal-to-noise ratio (SNR). Fig. 5D showed that the
SNR for some metabolites decreased with the increase of final
buffer concentrations. For example, with CFB values of 0.136
and 0.181 M, the SNR of creatinine was reduced for about 15%
and 20% respectively and such a reduction was about 5% (CFB,
0.136 M) and 13% (CFB, 0.181 M) for glycine and DMA. More
seriously, when a CFB of 0.181 M was employed, obvious
difficulties were experienced in tuning and matching of probe
circuits. It is worth noting that urine samples normally contain
more than 0.1 M salts already and the amount of salt added
ought to be minimized. In contrast, when traditional sample
preparation was employed (CFB, 0.067 M), the SNR had more
than 30% reduction for all metabolites tested, probably due to
salt effects and sample dilution. Based on the above discussion,
we concluded that the 1.5 M K2HPO4/NaH2PO4 buffer (pH
7.4) with the buffer–urine ratio of 1 : 10 (CFB, 0.136 M) should
be employed for human urine preparation in metabonomics
studies.
This journal is ª The Royal Society of Chemistry 2009
Verification of the optimized urine preparation method
To verify the robustness of the above preparation method for
a larger set of samples, 10 human urine samples (pH, 5.8–8.0)
were prepared with K2HPO4/NaH2PO4 buffer having different
concentrations at VBuffer : VUrine (1 : 10), respectively. For the
purpose of comparison, these samples were also prepared in the
traditional way (0.2 M Na2HPO4/NaH2PO4 buffer, VBuffer :
VUrine ¼ 1 : 2). Fig. 6A showed that the pH ranges were signifi-
cantly narrowed with the increase of CFB. For example, when
CFB was 0.067 M, the pH values of the tested urine samples
ranged between 7.0 and 7.7 which was close but failed to achieve
optimal pH target (7.1–7.7). In contrast, when CFB was 0.136 M
or higher, the pH range was narrowed to 7.1–7.5 and met the
demand of targeted pH.
With a CFB of 0.136 M or higher, the chemical shift ranges for
most metabolites were also narrowed considerably (as shown
Fig. S-3 for the citrate and DMA signals in the ESI†). Such
effects were more clearly indicated in Fig. 6B by the standard
deviation (SD) of the chemical shifts as a function of CFB. It was
obvious that the SD for some urine metabolites had a marked
decrease with the increase of CFB from 0 to 0.067 M due to
the minimization of pH variations (from 2.14 to 0.64). When
CFB was greater than 0.067 M, such SDs reached a plateau
(the expanded region in Fig. 6B). For example, when CFB was
0.136 M, the SD was reduced to less than 0.002 ppm for the
signals of acetate, glycine, DMA, TMA and hippurate. The
exception is again observed for the two protons of citrate (SD,
Analyst, 2009, 134, 916–925 | 923

Fig. 6 Verification of the optimized buffer system: (A) the pH distri-
bution for 10 human urine samples as a function of the final buffer
concentration (CFB); (B) standard deviation of the metabolite chemical
shifts for 10 human urine samples as a function of the final buffer
concentration (CFB); the solid lines were for visual guidance only; the
keys for symbols: histidine 5-CH (C) and 2-CH (B), citrate CH (,) and
CH0 (-), glycine (�), TMA (O), DMA (:), acetate ( ), creatinine (P)
and hippurate (*).
0.004 ppm) and the imidazole protons of histidine (SD, 0.009
ppm for 5-CH and 0.025 ppm for 2-CH). It is thus suggested that
the chemical shifts for the two metabolites (a total of four signals)
should be corrected before multivariate data analysis, especially
when high resolution spectral data were employed. Based on
these, we recommend that a CFB of 0.136 M is used in routine
work since such a buffer will give some safety margin in terms of
pH control and chemical shift consistency with respect to the
0.067 M buffer.
Conclusions
Chemical shift variations of urinary metabolite signals clearly
resulted from the alteration of ionization equilibrium induced by
pH and ionic strength. The effects of ionic strength on chemical
shifts can be explained by salt-induced ionization constant
changes for the ionizable groups. By taking chemical shift
consistency, the signal-to-noise ratio, sample dilution effects and
low temperature buffer storage into consideration, we found that
K2HPO4/NaH2PO4 buffer (pH 7.4, 1.5 M) with the buffer–urine
volume ratio of 1 : 10 was optimal for the NMR-based urinary
924 | Analyst, 2009, 134, 916–925
metabonomic studies. With such preparation, the sample pH
values were adequately controlled to pH 7.1–7.7 for normal
human urine, and chemical shifts of most metabolites with
ionizable groups were controlled within 0.002 ppm (1.2 Hz on
600 MHz data) the only exception of that for citrate and histi-
dine. High resolution bucketing and full resolution data analysis
can be carried out with some corrections for the chemical shifts
of citrate resonances and two singlets of histidine in the aromatic
region using already reported peak alignment methods.23–25
Acknowledgements
We thank Mr Xianwang Jiang of Wuhan Institute of Physics and
Mathematics for assistance in data fitting. We acknowledge the
financial supports from the National Basic Research Program of
China (2007CB914701, 2006CB503909 for H. T. and
2009CB118804 for Y. W.), National Natural Science Foundation
of China (20575074, 20825520 for H. T. and 20775087 for Y. W.)
and the Knowledge Innovation Program of the Chinese
Academy of Sciences (KJCX2-YW-W11 for Y. W., KSCX1-
YW-02 for H. T.).
References
1 J. K. Nicholson, J. Connelly, J. C. Lindon and E. Holmes, Nat. Rev.Drug. Discov., 2002, 1, 153–161.
2 J. G. Bundy, E. M. Lenz, N. J. Bailey, C. L. Gavaghan, C. Svendsen,D. Spurgeon, P. K. Hankard, D. Osborn, J. M. Weeks, S. A. Trauger,P. Speir, I. Sanders, J. C. Lindon, J. K. Nicholson and H. R. Tang,Environ. Toxicol. Chem., 2002, 21, 1966–1972.
3 Y. L. Wang, M. E. Bollard, J. K. Nicholson and E. Holmes, J. Pharm.Biomed. Anal., 2006, 40, 375–381.
4 I. K. Yap, T. A. Clayton, H. R. Tang, J. R. Everett, G. Hanton,J. P. Provost, J. L. Le Net, C. Charuel, J. C. Lindon andJ. K. Nicholson, J. Proteome Res., 2006, 5, 2675–2684.
5 J. T. Brindle, H. Antti, E. Holmes, G. Tranter, J. K. Nicholson,H. W. Bethell, S. Clarke, P. M. Schofield, E. McKilligin,D. E. Mosedale and D. J. Grainger, Nat. Med., 2002, 8, 1439–1444.
6 Y. L. Wang, E. Holmes, J. K. Nicholson, O. Cloarec, J. Chollet,M. Tanner, B. H. Singer and J. Utzinger, Proc. Natl. Acad. Sci.USA, 2004, 101, 12676–12681.
7 Y. L. Wang, J. Utzinger, S. H. Xiao, J. Xue, J. K. Nicholson,M. Tanner, B. H. Singer and E. Holmes, Mol. Biochem. Parasitol.,2006, 146, 1–9.
8 Y. L. Wang, E. Holmes, H. R. Tang, J. C. Lindon, N. Sprenger,M. E. Turini, G. Bergonzelli, L. B. Fay, S. Kochhar andJ. K. Nicholson, J. Proteome Res., 2006, 5, 1535–1542.
9 Y. L. Wang, D. Lawler, B. Larson, Z. Ramadan, S. Kochhar,E. Holmes and J. K. Nicholson, J. Proteome Res., 2007, 6, 1846–1854.
10 K. S. Solanky, N. J. Bailey, B. M. Beckwith-Hall, A. Davis,S. Bingham, E. Holmes, J. K. Nicholson and A. Cassidy, Anal.Biochem., 2003, 323, 197–204.
11 K. S. Solanky, N. J. Bailey, B. M. Beckwith-Hall, S. Bingham,A. Davis, E. Holmes, J. K. Nicholson and A. Cassidy, J. Nutr.Biochem., 2005, 16, 236–244.
12 F. P. Martin, E. F. Verdu, Y. L. Wang, M. E. Dumas, I. K. Yap,O. Cloarec, G. E. Bergonzelli, I. Corthesy-Theulaz, S. Kochhar,E. Holmes, J. C. Lindon, S. M. Collins and J. K. Nicholson,J. Proteome Res., 2006, 5, 2185–2193.
13 A. Fardet, C. Canlet, G. Gottardi, B. Lyan, R. Llorach, C. Remesy,A. Mazur, A. Paris and A. Scalbert, J. Nutr., 2007, 137, 923–929.
14 J. C. Lindon, E. Holmes and J. K. Nicholson, Prog. Nucl. Magn.Reson. Spectrosc., 2001, 39, 1–40.
15 Y. L. Wang, H. R. Tang, J. K. Nicholson, P. J. Hylands, J. Sampsonand E. Holmes, J. Agric. Food Chem., 2005, 53, 191–196.
16 M. E. Bollard, H. C. Keun, O. Beckonert, T. M. Ebbels, H. Antti,A. W. Nicholls, J. P. Shockcor, G. H. Cantor, G. Stevens,J. C. Lindon, E. Holmes and J. K. Nicholson, Toxicol. Appl.Pharmacol., 2005, 204, 135–151.
This journal is ª The Royal Society of Chemistry 2009

17 C. N. Xiao, H. Dai, H. B. Liu, Y. L. Wang and H. R. Tang, J. Agric.Food Chem., 2008, 56, 10142–10153.
18 Y. X. Yang, C. L. Li, X. Nie, X. S. Feng, W. X. Chen, Y. Yue,H. R. Tang and F. Deng, J. Proteome Res., 2007, 6, 2605–2614.
19 W. X. Chen, H. Y. Lou, H. P. Zhang, X. Nie, Y. Xiang, Y. X. Yang,G. Y. Wu, J. P. Qi, Y. Yue, H. Lei, H. R. Tang and F. Deng, Prog.Biochem. Biophys., 2008, 35, 1142–1153.
20 O. Cloarec, M. E. Dumas, J. Trygg, A. Craig, R. H. Barton,J. C. Lindon, J. K. Nicholson and E. Holmes, Anal. Chem., 2005,77, 517–526.
21 B. Rasmussen, O. Cloarec, H. R. Tang, D. Staerk andJ. W. Jaroszewski, Planta Med., 2006, 72, 556–563.
22 M. Li, B. H. Wang, M. H. Zhang, M. Rantalainen, S. Y. Wang,H. K. Zhou, Y. Zhang, J. Shen, X. Y. Pang, M. L. Zhang, H. Wei,Y. Chen, H. F. Lu, J. Zuo, M. M. Su, Y. P. Qiu, W. Jia,C. N. Xiao, L. M. Smith, S. L. Yang, E. Holmes, H. R. Tang,G. P. Zhao, J. K. Nicholson, L. J. Li and L. P. Zhao, Proc. Natl.Acad. Sci. USA, 2008, 105, 2117–2122.
23 J. Forshed, I. S. Koistinen and S. P. Jacobsson, Anal. Chim. Acta,2003, 487, 189–199.
24 G. C. Lee and D. L. Woodruff, Anal. Chim. Acta, 2004, 513, 413–416.
25 R. Stoyanova, A. W. Nicholls, J. K. Nicholson, J. C. Lindon andT. R. Brown, J. Magn. Reson., 2004, 170, 329–335.
26 M. Lauridsen, S. H. Hansen, J. W. Jaroszewski and C. Cornett, Anal.Chem., 2007, 79, 1181–1186.
27 Y. C. Wang, in Diagnostics, ed. W. B. Chen, People’s MedicalPublishing House, Beijing, 5th edn, 2001, ch. 3, pp. 344–347.
28 M. E. Bollard, E. G. Stanley, J. C. Lindon, J. K. Nicholson andE. Holmes, NMR Biomed., 2005, 18, 143–162.
29 W. J. Yang, Y. W. Wang, Q. F. Zhou and H. R. Tang, Sci. China Ser.B-Chem., 2008, 51, 218–225.
30 A. R. Quirt, J. R. Lyerla Jr., I. R. Peat, J. S. Cohen, W. F. Reynoldsand M. H. Freedman, J. Am. Chem. Soc., 1974, 96, 570–574.
31 J. R. Bales, D. P. Higham, I. Howe, J. K. Nicholson and P. J. Sadler,Clin. Chem., 1984, 30, 426–432.
32 H. Miyataka, T. Ozaki and S. Himeno, Biol. Pharm. Bull., 2007, 30,667–670.
33 J. C. Lindon, J. K. Nicholson and J. R. Everett, Annu. Rep. NMRSpectrosc., 1999, 38, 1–88.
This journal is ª The Royal Society of Chemistry 2009
34 B. C. Potts, A. J. Deese, G. J. Stevens, M. D. Reily, D. G. Robertsonand J. Theiss, J. Pharm. Biomed. Anal., 2001, 26, 463–476.
35 V. M. Asiago, G. A. N. Gowda, S. Zhang, N. Shanaiah, J. Clark andD. Raftery, Metabolomics, 2008, 4, 328–336.
36 R. A. Wevers, U. Engelke, J. J. Rotteveel, A. Heerschap, J. G. DeJong, N. G. Abeling, A. H. van Gennip and R. A. De Abreu,J. Inherit. Metab. Dis., 1997, 20, 345–350.
37 S. H. Moolenaar, J. Poggi-Bach, U. F. Engelke, J. M. Corstiaensen,A. Heerschap, J. G. de Jong, B. A. Binzak, J. Vockley andR. A. Wevers, Clin. Chem., 1999, 45, 459–464.
38 E. Holmes, A. W. Nicholls, J. C. Lindon, S. C. Connor, J. C. Connelly,J. N. Haselden, S. J. Damment, M. Spraul, P. Neidig andJ. K. Nicholson, Chem. Res. Toxicol., 2000, 13, 471–478.
39 A. W. Nicholls, E. Holmes, J. C. Lindon, J. P. Shockcor,R. D. Farrant, J. N. Haselden, S. J. Damment, C. J. Waterfield andJ. K. Nicholson, Chem. Res. Toxicol., 2001, 14, 975–987.
40 M. A. Constantinou, E. Papakonstantinou, M. Spraul,S. Sevastiadou, C. Costalos, M. A. Koupparis, S. Kleopatra,A. Tsantili-Kakoulidou and E. Mikros, Anal. Chim. Acta, 2005,542, 169–177.
41 J. L. Griffin, L. A. Walker, R. F. Shore and J. K. Nicholson, Chem.Res. Toxicol., 2001, 14, 1428–1434.
42 K. S. Solanky, N. J. C. Bailey, E. Holmes, J. C. Lindon, A. L. Davis,T. P. J. Mulder, J. P. M. Van Duynhoven and J. K. Nicholson,J. Agric. Food Chem., 2003, 51, 4139–4145.
43 F. Rey, A. Varela, J. M. Antelo and F. Arce, J. Chem. Eng. Data,1989, 34, 35–37.
44 R. M. C. Dawson, D. C. Elliott, W. H. Elliott and K. M. Jones, inData for biochemical research, Oxford University Press, Oxford, 3rdedn, 1986, pp. 103–115.
45 D. P. Cistola, D. M. Small and J. A. Hamilton, J. Lipid Res., 1982, 23,795–799.
46 B. Henry, P. Tekely and J. J. Delpuech, J. Am. Chem. Soc., 2002, 124,2025–2034.
47 K. K. Lee, C. A. Fitch, J. T. J. Lecomte and B. Garcia-Moreno,Biochemistry, 2002, 41, 5656–5667.
48 Y. H. Kao, C. A. Fitch, S. Bhattacharya, C. J. Sarkisian, J. T. J. Lecomteand B. Garcia-Moreno, Biophys. J., 2000, 79, 1637–1654.
49 W. D. Kumler and J. J. Eiler, J. Am. Chem. Soc., 1943, 65, 2355–2361.
Analyst, 2009, 134, 916–925 | 925