AMMONIA METABOLISM IN RENAL FAILURE
-
Upload
peter-richards -
Category
Documents
-
view
220 -
download
2
Transcript of AMMONIA METABOLISM IN RENAL FAILURE

AMMONIA METABOLISM IN RENAL FAILURE
By PETER RICHARDS, Ph.D., M.R.C.P., B. J. HOUGHTON, M.B., M.C.Path. and 0. M. WRONG, D.M., F.R.C.P.
From the Departments of Medicine and Chemical Pathology, St Mary's Hospital Medical School, London, W.2, and from the Department of Medicine, Royal Postgraduate Medical School, London, W. 12
STABLE isotopes such as 15N are rarely used now that radioisotopes and simple, reliable counting equipment are readily available. Sometimes, however, a suitable radioactive isotope does not exist, as in this study, or the radiation hazards involved by its use may be unacceptable. By mass spectrometry the relative proportions of two isotopes of an element which have different atomic weights can be determined (Rittenberg et al., 1939).
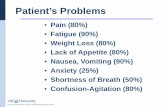
Many of the symptoms of uraemia are caused by the accumulation of products of protein breakdown. Attempts to improve the treatment of chronic renal failure by dietary protein restriction are worth while because the quality of life can be improved, the length of life may be increased, and those patients who are awaiting regular dialysis treatment or a kidney transplant can be kept in good health until the opportunity for further treatment materialises.
Giordano (1963) showed that urremic patients not only stayed in nitrogen balance on a protein intake below the minimum requirement of healthy men, which is about 20 g. per 24 hours, but were actually in positive balance while their blood urea was falling. These observations suggested that the urea nitrogen was used to make body protein.
The re-utilisation of urea nitrogen for protein synthesis is the background to our interest in the metabolism of ammonia in patients with chronic renal failure because it is ammonia nitrogen derived from urea breakdown which is used. First, it will be shown that there was little or no urea in the stools of either normal or uraemic people, except when they took antibiotics. This finding implies that urea is continually being hydrolysed to ammonia by bacterial ureases in the gut. It is then shown by the use of tracer doses of 15N taken as ammonium chloride that ammonia nitrogen absorbed from the gut was incorporated by healthy men into plasma albumin, that protein restriction increased this incorporation, and that incorporation was greatest in uraemic patients who had been protein-restricted for a much longer period.
The concentration of urea and ammonia in the stools of healthy and uraemic people was measured by means of the technique of in vivo dialysis of faeces (Wrong et al., 1965), a technique which yields a fluid which is in diffusion equilibrium with the extracellular fluid of stool. Table I shows that urea was normally absent from the stool until antibiotics were given. Only with an antibiotic mixture containing neomycin, polymyxin, bacitracin and nystatin have we been consistently able to find urea in the stool at near plasma concentration, together with absence of urea splitting organisms on culture. Although the concentration of ammonia fell during treat- ment with antibiotics, a finding which would be anticipated if urea breakdown were reduced, an appreciable concentration remained. This fact indicates that urea metabolism is not the only source of ammonia in the stool. Table I1 shows that even patients whose blood urea exceeded 100 mg./100 ml. (17 mM/1.) had little or no urea in the faeces. In spite of the greatly increased urea-breakdown which this observation implies because the concentration of urea in the fluids entering the alimentary tract corresponds closely to the blood urea, the concentration of ammonia has increased by only 7 mEq/l. This low figure indicates that much of the extra ammonia formed has been reabsorbed, a conclusion which is supported by the observation that the total faecal nitrogen is not significantly increased in ursemia (Stanbury and Lumb, 1962). The concentration of urea in the stool increased to about the level of the blood urea when antibiotics were given and the concentration of ammonia fell simultaneously (Table 111).
103

104 RADIOISOTOPES I N U R O L O G Y A N D R E N A L DISEASE
These observations confirm that ammonia is constantly presented to the liver as a result of urea breakdown in the gut, and that the quantity of ammonia presented is much greater in uremic patients. We therefore gave 15N-labelled ammonium chloride by mouth to trace the fate of ammonia absorbed from the gut. Details of the size and timing of the doses have been published (Richards et al., 1967).
P<
TABLE I
The Effect of Intestinal Antibiotics on the Composition of Fecal Dialysate in Normal Subjects
0.01 0.01
~
Ammonia (m-mole/l.) (m-mole/l.)
Normal
Antibiotics
P<
0
(83)
5.1 0-1 1.6 (49)
0.01
11.2 2.9-44 (83)
7.4 2.8-19.4
(49)
0.01
Combined data from all specimens containing more than 0.5 m-mole/l. of urea. The mean, 95 per cent. range, and the number of observations (in parentheses) are shown for each variable.
TABLE I1
Composition of Fecal Dialysate from Normal and Uremic Subjects
Urea (m-mole/l.)
Normal
I 1 Urremic
I 2.1
0-9'7 (37)
~
Ammonia (m-mole/l.)
11.2 2.9-44 (83)
17.9 4.3-75
(49)
The mean value, the 95 per cent. range, and the number of observations (in parentheses) are shown for each variable.
Some of this ammonia 15N was incorporated into albumin in the liver and appeared in the plasma albumin even when the control subjects took a normal diet (Fig. 1). A much greater l5N
enrichment of plasma albumin was found when the experiment was repeated in two other healthy individuals who had taken a 20-g. protein diet for three weeks (Fig. 2). Essential amino acids were given on the day before and the day of the experiment to ensure that protein synthesis was not impaired because of deficiency of essential amino acids. The greater enrichment of plasma

A M M O N I A M E T A B O L I S M I N R E N A L F A I L U R E 105
albumin after a period of protein restriction was partly a reflection of a greater incorporation of 15N and partly a consequence of the reduced plasma urea concentration, which fell as low as 8 mg./100 ml. Under these circumstances the endogenous ammonia formation from urea break- down was reduced and less ammonia from that source was therefore available to compete with the labelled ammonia nitrogen for incorporation. Increased incorporation of l5N into body protein after protein restriction was confirmed by a fall in the recovery of 15N in urine and fEces from about 70 per cent. of the dose in six days to about half that amount (Figs. 1 and 2). Most of the isotope was recovered in the urine and only a small fraction of the dose appeared in the stool.
TABLE 111
The Effect of Intestinal Antibiotics on Facal Dialysate in Renal Failure
Normal subjects: mean 95 per cent. range
Subject 1: blood urea 160- 185 mg./100 ml. (27-31 m-mole/l.)
Antibiotic mixture days 1-6 inclusive
Day 1 Specimen
3
4
5
6
8
10
Urea (m-mole/l.)
0
0 31.9
29.8 28.1
24.1
7.0
16.3
26.1 14.2
0
Ammonia (m-mole/l.)
11.2 2.9-44
16-4 2.3
2.2 2.5
9.7
35.6
16.6
11.2 12.5
34.0
The enrichment of plasma albumin with 15N was as great in uraemic patients as in protein- restricted healthy people. Utilisation of ammonia nitrogen was therefore markedly increased, for the same plasma albumin enrichment was achieved with an only slightly larger dose of 15N in spite of competition from larger amounts of ammonia derived from intestinal urea breakdown. Figure 3 shows the enrichment of plasma albumin in two patients (E and F), whose plasma urea levels were 120 and 220 mg. per 100 ml. respectively. Patient E had taken a 30-g. protein diet for nine months and F had taken a 20-g. protein diet for longer than one year. The albumin enrichment reached a plateau after mixing was complete, in contrast to normal individuals whose albumin enrichment showed a steady decline. We suspect that the plateau of enrichment in the urmnic patients is a sign of recycling of the isotope.
We previously calculated the total amount of ammonia nitrogen which was incorporated by these patients into plasma albumin in a period of 24 hours (Richards et af., 1967). To do this we made three assumptions:
1. that 15N-labelled ammonia from ammonium chloride was treated by the liver in exactly the same way as 14N ammonia derived from bacterial breakdown of urea in the alimentary tract;
2. that the urea metabolised was mainly broken down to ammonia, and as such was re- absorbed into the portal blood;

106 RADIOISOTOPES I N UROLOGY A N D R E N A L DISEASE
3. that urzmic patients metabolised the same proportion of the body urea pool as the healthy individuals studied by Walser and Bodenlos (1959).
s I Y v)
0.1 tii a= y1 c
15NHk C1 by mouth
-
4 4 4 4 4
s 0.15-
a9 u x aa
la E
0.1 = .n c
c
Cumulative excretion B - - - -5- - - -I,------------- - A I
-100 -
d -0° 's
I W e 'OD- s
- s ---o---- - 6 0 ",
Q---_ 0
3.
I I I
I- .C -
- 4 0 jTj I c -
--;----I----- ----!r--
Cumulative excretion
,-h
.% 0 %
- 2 0 V
Albumin enrichment I - 0 0
*A - - - - _ - - - - - - - - - -4- - - - ~
I5NHL C l by mouth
DAYS FIG. 2
Plasma enrichment and cumulative excretion of 15N by two healthy adults (C and D) after three weeks on a 20-g. protein diet.
The third assumption contained the largest potential error. Three groups of workers have, however, recently shown that urea breakdown increased in proportion to the blood urea and

A M M O N I A M E T A B O L I S M I N R E N A L F A I L U R E 107
therefore in proportion to the body urea pool (Deane et al., 1968; Robson et al., 1968; Scholtz, 1968).
Essential amino acids by mouth 44444 44444 Too
- a -120 1 -Cumulative excretioi --I- - - -1- - - - -
r - -
0 AVS
FIG. 3 Plasma albumin enrichment and cumulative excretion of l5N by two uraemic patients on a
30-g. (E) and 20-g. (F) protein diet.
250 r
1 0 O/O
5 O/Cl
1 .... .... .... .... . . . . .... . . . . .... . . . . .... . . . . .... . . . . .... . . . . .... ..... .... ..... .... ..... .... ..... .... .... .... .... .... .... ....
1000
800
600
400
200
0 PLASMA UREA ''0 OF 15N DOSE AMMONIA NITROGEN mg 1100 ml w a t e r INCORPORATED INTO INCORPORATED INTO
ALBUMIN POOL (66 hrs) ALBUMIN rng in 2 4 h r d 1 - 7 3 m 2
FIG. 4 Comparison of incorporation of ammonia nitrogen into albumin in different individuals: hatched columns-normal individuals on normal diet: stippled columns-normal indi-
viduals on a 20-g. protein diet; solid columns-uraemic patients on a low protein diet.

108 RADIOISOTOPES I N UROLOGY A N D R E N A L DISEASE
Walser (1968) in fact recently concluded that a uraemic patient whose blood urea was over 200 mg./100 ml. and who took a 30-g. protein diet had three times as much ammonia nitrogen available from endogenous urea breakdown as from the protein intake. He calculated that 14 g. of endogenous ammonia nitrogen was available for protein synthesis each day.
The result of our calculation is shown in Figure 4. Between 10 and 15 per cent. of the 15N dose appeared in the albumin of healthy individuals who were studied after a three-week period of protein restriction. We must, however, remember that their blood urea was low, ammonia formation from urea breakdown was therefore reduced, and competition between endogenous ammonia and 15N ammonia was consequently less than normal. Conversely, although only about 7 per cent. of the 15N dose appeared in the albumin of urzmic patients, incorporation took place against competition from very large amounts of ammonia from endogenous urea breakdown. It is no surprise therefore to find that the total incorporation of ammonia nitrogen was far greater in uraemic patients. Their calculated incorporation was 700 and 975 mg. of ammonia nitrogen in 24 hours, an amount equivalent to 5 or 6 g. of protein without making any allowance for incorporation into other body proteins.
We conclude therefore that ammonia nitrogen derived from the continuous breakdown of endogenous urea might be harnessed as a useful source of nitrogen for protein synthesis by urzmic patients, and that they might remain in good health for a long time on a diet which contained considerably less than 20 g. of protein.
The essential nitrogen intake for a urzmic patient may in fact be only the nitrogen oflysine and threonine, provided that men, like mice (Wood and Cooley, 1954), can form the other essential amino acids by transaminating their ketoacid analogues. We can envisage a synthetic diet for uraemic patients which contains only lysine, threonine, the ketoacid analogues of the other essential amino acids, carbohydrate, fat, vitamins and minerals. We are exploring this possibility further.
P. R. was in receipt of a Medical Research Council Clinical Research Fellowship during this work which was also supported by a grant from the Medical Research Council for technical assistance.
REFERENCES
DEANE, N., DESIR, W., and UMEDA, T. (1968). The production and extrarenal metabolism of urea in patients with chronic renal failure treated with diet and dialysis. Proc. Eur. Dial. Transpl. Ass., 4, 245.
GIORDANO, C. (1963). The use of exogenous and endogenous urea for protein synthesis in normal and uraemic subjects. J. Lab. clin. Med., 62, 231.
RICHARDS, P., METCALFE-GIBSON, A., WARD, E. E., WRONG, 0. M., and HOUGHTON, B. J. (1967). Utilisation of ammonia nitrogen for protein synthesis in man and the effect of protein restriction and uraemia. Lancet, 2, 845.
RITTENBERG, D., KESTON, A. S., ROSEBURY, F., and SCHOENHEIMER, R. (1939). The determination of nitrogen isotopes in organic compounds. J. bid. Chem., 127, 291.
ROBSON, A. M., KXRR, D. N. S. , and ASHCROFT, R. (1968). Urea metabolism in chronic urzmia: effect of protein restriction, anabolic steroids and antibiotics. In '' Nutrition in Renal Disease ", ed. Berlyne, G. M., p. 71. Edinburgh: Livingstone.
SCHOLTZ, A. (1968). Investigations on distribution and turnover rate of C14-urea and tritiated water in renal failure. Proc. Eur. Dial. Transpl. Ass., 4, 240.
STANBURY, S. W., and LUMB, G. A. (1962). Metabolic studies of renal osteodystrophy. Medicine, 41, 1.
WALSER, M. (1968). Use of isotopic urea to study the distribution and degradation of urea in man. In " Proceedings of a Conference on Urea Metabolism ". Excerpta med. In press.
WALSER, M., and BODENLOS, L. J. (1959). Urea metabolism in man. J. clin. Invest., 38, 1617. WOOD, J. L., and COOLEY, S. L. (1954). Substitution of a-ketoacids for five amino acids essential
for growth of the rat. Proc. SOC. exp. Biol. Med., 85, 409.
In vivo dialysis of faxes as a method of stool analysis. I. Technique and results in normal subjects. Clin. Sci., 28, 357.
WRONG, 0. M., METCALFE-GIBSON, A., MORRISON, R. B. I., N G , s. T., and HOWARD, A. V. (1965).













![(Pi), [PJ] Pi), - dm5migu4zj3pb.cloudfront.net · 31P-Magnetic ResonanceSpectroscopyAssessmentof Subnormal Oxidative Metabolism in Skeletal Muscleof Renal Failure Patients GeoffreyE.](https://static.fdocuments.in/doc/165x107/5e09012eeed381361417cf43/pi-pj-pi-31p-magnetic-resonancespectroscopyassessmentof-subnormal-oxidative.jpg)



