Alterations in Acute and Late Cytokine Expression Correlate with Radiation-induced Fibrosis
Transcript of Alterations in Acute and Late Cytokine Expression Correlate with Radiation-induced Fibrosis

Proceedings of the 51st Annual ASTRO Meeting S541
Conclusions: Mesenchymal stem cells are surprisingly resistant to direct ionizing radiation for certain functional endpoints, inparticular for apoptosis. Nevertheless gene expression data suggest important radiation effects on cell differentiation/development.By contrast, MSC are highly sensitive to inhibitors of c-kit/PDGF and VEGFR2/PDGF signaling. These findings may contribute tothe understanding and optimization of tumor radiotherapy and radiation side effect analysis.
Author Disclosure: E. Sommer, None; U. Wirkner, None; R. Saffrich, None; P.E. Huber, None.
2800 Radiation-induced Alpha5 Beta1 Integrin Upregulation on the Surfaces of Pancreatic Cancer Cells
Involves Increased Trafficking in Early and/or Late EndosomesD. L. Livant1, H. Yao1, Z. Zeng1, E. Staszewski1, A. Spalding2
1University of Michigan, Ann Arbor, MI, 2Norton Healthcare, Louisville, KY
Purpose/Objective(s): Ionizing radiation rapidly induces Panc-1, MiaPaCa, and BxPC-3 human pancreatic cancer cell invasion,which is mediated by the alpha5 beta1 integrin fibronectin receptor (FnR). Here, we report the effects of radiation on the levels andlocalization of alpha5 beta1 integrin, and on early and late endosomes.
Materials/Methods: Adherent Panc1, MiaPaCa, and BxPC-3 cells were irradiated once with 2 Gy (Panc1) or 3 Gy (MiaPaCa andBxPC-3). One hour later, fluorescent immunostaining was performed with anti alpha 5 antiserum (Ab), P1D6 anti alpha 5 beta 1 mono-clonal antibody (MAb), anti EEA-1 MAb, or anti LAMP-1 Ab. Panc1 and BxPC-3 tumors in nude mice received 2 Gy on each of 5 daysbefore excision. Frozen sections were bound to fluorescent anti alpha 5 Ab, P1D6 anti alpha5 beta1 MAb, anti EEA-1 MAb, or antiLAMP-1 Ab. Immunofluorescence quantitation of adherent cells and sectioned tumors was performed by confocal microscopy.
Results: Radiation caused a rapid upregulation of surface alpha5 beta1 integrin FnR in Panc-1, MiaPaCa, and BxPC-3 cells. The sub-cellular localization of alpha5 beta1 also changed significantly: a rapid transition from low cytoplasmic perinuclear levels in unirradiatedBxPC-3, MiaPaCa, and Panc-1 cells to high membrane levels shortly after radiation. Consistent results were obtained in nude mice bear-ing BxPC-3 and Panc1 tumors. Frozen sections of unirradiated tumors, immunostained with fluorescent anti alpha5 beta1 and anti MMP1 Abs, showed only low levels of perinuclear alpha 5 beta 1 and MMP 1; while cells of irradiated tumors had high membrane levels ofboth proteins. Radiation-induced alpha5 beta1 upregulation may occur via recycling through early endosomes, a direct, short receptorrecycling pathway. Alternatively, radiation-induced alpha5 beta1 upregulation may involve recycling through late endosomes, an in-direct, longer receptor recycling pathway involving association with the trans-Golgi network. Our results suggest that radiation-inducedalpha5 integrin upregulation in Panc1 cells occurs exclusively through increased rates of receptor recycling through early endosomes,without increased alpha5 gene transcription. Our results also show that alpha5 beta1 upregulation in MiaPaCa and BxPC-3 cells is due toincreased trafficking through late endosomes, as well as increased alpha5 transcription, since RT-PCR analysis of irradiated MiaPaCaand BxPC-3 cells showed a 3- to 5-fold induction of alpha 5 mRNA. In MiaPaCa cells, radiation-induced alpha5 beta1 upregulationappears to involve increases in both early and late endosomal trafficking; while in BxPC-3 cells, radiation-induced alpha5 beta1 upre-gulation appears to involve late endosomal trafficking almost exclusively.
Author Disclosure: D.L. Livant, None; H. Yao, None; Z. Zeng, None; E. Staszewski, None; A. Spalding, None.
2801 Hypoxia Manipulation in Solid Tumors has the Potential to Influence Lung Metastases In Vivo
S. Masunaga1, Y. Matumoto2, R. Hirayama2, G. Kashino1, M. Suzuki1, Y. Kinashi1, Y. Liu1, K. Ando2, K. Ono1
1Particle Radiat. Oncol. Res. Center, Res. Reactor Inst., Kyoto Univ., Osaka, Japan, 2Heavy-Ion Radiobiology Res. Group,National Institute of Radiological Sciences, Chiba, Japan
Purpose/Objective(s): To evaluate the effect of manipulating intratumor hypoxia during radiotherapy on lung metastasis, includ-ing its effect on the sensitivity of quiescent tumor cells.
Materials/Methods: B16-BL6 melanoma tumor-bearing C57BL/6 mice were continuously given 5-bromo-2’-deoxyuridine(BrdU) to label all proliferating (P) cells. They received g-ray irradiation following loading with the acute hypoxia-releasing agentnicotinamide or local hyperthermia at mild temperatures (MTH). Immediately after the irradiation, cells from some tumors wereisolated and incubated with a cytokinesis blocker. The sensitivity of quiescent (Q) cells was assessed in terms of the micronucleusfrequency using immunofluorescence staining for BrdU. That of the total (= P + Q) tumor cell population was determined fromBrdU non-treated tumors. In other tumor-bearing mice, 17 days after irradiation, macroscopic lung metastases were enumerated.
Results: In the total cells, a more marked enhancement in sensitivity was observed with nicotinamide than MTH. In Q cells, MTHcombination induced a more marked enhancement than nicotinamide. Both nicotinamide and MTH reduced the size of the hypoxicfraction in the two cell populations, especially nicotinamide in the total cells and MTH in Q cells. Without g-ray irradiation, nic-otinamide loading tended to decrease the number of lung metastases. With g-ray irradiation, nicotinamide loading and MTH, es-pecially the former, reduced the number of metastases more than g-ray irradiation only.
Conclusions: Hypoxia manipulation in solid tumors has the potential to influence lung metastases. Notably, acute hypoxia-releas-ing nicotinamide may be promising for reducing the number of lung metastases.
Author Disclosure: S. Masunaga, None; Y. Matumoto, None; R. Hirayama, None; G. Kashino, None; M. Suzuki, None; Y. Kin-ashi, None; Y. Liu, None; K. Ando, None; K. Ono, None.
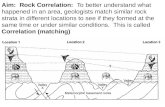
2802 Alterations in Acute and Late Cytokine Expression Correlate with Radiation-induced Fibrosis
C. B. Simone, D. Ly, B. P. Soule, J. E. Savage, J. B. Mitchell, N. L. Simone
National Cancer Institute, Bethesda, MD
Purpose/Objective(s): Radiation therapy induces fibrotic changes in normal tissue. TGF-b and IL-13 have been implicated in in-dependent pathways that lead to fibrosis. Little is known, however, regarding the role of other cytokines in fibrogenesis or their

S542 I. J. Radiation Oncology d Biology d Physics Volume 75, Number 3, Supplement, 2009
response to radiation. This in vivo study examines the acute and late effects of radiation on cytokines previously reported to havea qualitative association with fibrogenesis.
Materials/Methods: The right hind legs of nine-week old CH3 mice were irradiated in a single 35 Gy fraction. Mice were sac-rificed at 1hr, 7 days, 14 days, 30 days, 90 days, or 120 days post-irradiation. Left hind legs served as controls. Protein lysates fromhind leg skeletal tissue were evaluated for expression of IL-1a, IL-1ß, IL-2, IL-4, IL-5, IL-6, IL-10, IL-17, MCP-1a, IFN-g, MIP-1a, TNF-a, Eotaxin, GM-CSF, and CXCL-1 using a multiplexed ELISA. IL-13 and TGF-ß were evaluated by single analyteELISA. Expression of each cytokine was compared to controls for each time point.
Results: Expression of all analyzed cytokines increased 1hr after radiation. Cytokine expression was decreased 7, 14, and 30 daysafter radiation, except for TGF-ß (239.8% increase at day 14, 169.2% at day 30), IL-13 (162.5% increase at day 7, 30.7% at day 30),and Eotaxin (76.5% increase at day 30). At day 90, there was moderate increase in IL-1ß, IL-4, and IL-10 (11.0%-23.6%) andconsiderable increase in IL-5, IL-6, MIP-1a, Eotaxin, and CXCL-1 (44.7%-123.3%). IL-1b, IL-5, and IL-6 remained elevatedat day 120 (19.0-106.0%). IL-1a (55.0%), IL-13 (165.1%), and TGF-ß (140.0%) were also significantly elevated at day 120.
Conclusions: Radiation induced an acute cytokine response reflected in a global increase in cytokine expression 1hr post-irradi-ation most evident for IL-13 (894.4%) and IL-6 (412.6%). Subacutely (days 7, 14, 30), cytokine expression was generally de-creased below baseline levels. This may represent the suppressive effect of anti-inflammatory regulatory mechanisms. In thelate setting (days 90, 120), increased expression of pro-inflammatory cytokines (IL-1a, IL-1ß, IL-6) and TH2-associated pro-fi-brotic cytokines (IL-4, IL-5, IL-13, Eotaxin) was observed. This coincided with a decrease in anti-inflammatory IL-10. Radiationappears to induce dysregulated cytokine production. Altered expression of both TH2/eosinophil-associated cytokines (IL-4, IL-5,IL-13, Eotaxin) and cytokines that influence TH17-mediated and other inflammation (TGF-ß, IL-6) was observed. While eachpathway has been implicated in fibrogenesis independently, these data suggest that both may mediate radiation-induced fibrosis.As such, therapies that modulate cytokine expression, such as targeted immunomodulators, may alter the development or progres-sion of radiation-induced fibrosis.
Author Disclosure: C.B. Simone, None; D. Ly, Research year sponsored by the National Institutes of Health (NIH) Clinical Re-search Training Program, a partnership by the NIH and Pfizer Inc. (via a grant to the Foundation for NIH from Pfizer Inc.), C. OtherResearch Support; B.P. Soule, None; J.E. Savage, None; J.B. Mitchell, None; N.L. Simone, None.
2803 Disruption of GBM - Endothelial Cell Interactions Through Antagonism of CXCR4 Signaling Inhibits
Tumor Cell GrowthS. R. Rao, M. Woerner, A. Choe, D. Piwnica-Worms, J. Leonard, J. R. Simpson, J. B. Rubin
Washington University School of Medicine, St. Louis, MO
Purpose/Objective(s): Despite significant research and multi-modal therapy, GBM (Glioblastoma) remains a disease with poorprognosis. Emerging research now suggests that endothelial cells (EC) form a microenvironmental niche critical to GBM prolif-eration and protection. Recent work in hematological malignancies reveals that the CXCL12/CXCR4 pathway facilitates locali-zation of tumor cells to a protective microenvironmental niche. As GBM cells express the CXCR4 receptor and brain ECsproduce high levels of the ligand CXCL12, we sought to examine if similar mechanisms might contribute to GBM growth.
Materials/Methods: We developed a unique co-culture model using extracellular matrix, primary human brain ECs and GBMcells to provide an improved in-vitro model for GBM incorporating the microenvironment. Both primary, collected from patients,and cultured GBM cells, U87MG, were used. The CXCR4 pathway antagonist, AMD3100, and the VEGF pathway inhibitor, bev-acizumab, were evaluated for their effects on cell interactions and growth. GBM cell growth was measured by either biolumines-cent imaging of firefly luciferase expressed in U87MG cells or by GFAP immunolabeling for primary GBM specimens. For cell co-localization studies we utilized mCherry expressed in EC and either GFP in U87MG or GFAP immunolabeling in primary GBMsamples for cell identification. TUNEL and BrDU labeling were employed to assess cell death and proliferation.
Results: In this model, EC adopt a cellular phenotype similar to that seen in-vivo and form a tubule-like network. We show that ECprovide trophic support for GBM cells in both U87MG, as well as primary GBM specimens. Furthermore, GBM cells migrate to-ward EC, demonstrating a strong co-localization. Inhibition of this co-localization by the CXCR4 receptor antagonist, AMD3100,indicates that the chemo-attraction is mediated by the CXCR4-CXCL12 chemokine pathway. Furthermore, disruption of this in-teraction attenuates the trophic effects of EC on GBM cells.
Conclusions: These findings lend further support to manipulation of the tumor microenvironment as a promising approach to blocktumor growth. More specifically, they suggest that disruption of the interaction between GBM cells and EC by inhibition ofCXCR4-CXCL12 signaling may serve as an entirely novel mechanism to block GBM growth. Future studies aim to examinewhether exploitation of this mechanism may improve the efficacy of chemotherapy and radiation in treating GBM.
Author Disclosure: S.R. Rao, None; M. Woerner, None; A. Choe, None; D. Piwnica-Worms, None; J. Leonard, None; J.R. Simp-son, None; J.B. Rubin, None.
2804 Radioresistance of Non-small Cell Lung Cancer Stem Cells
S. D. Parikh1, V. Levina2, T. Wang2, M. K. Gibson2, A. E. Lokshin2
1University of Pittsburgh Medical Center, Pittsburgh, PA, 2University of Pittsburgh Cancer Institute, Pittsburgh, PA
Purpose/Objective(s): Cancer stem cells (CSCs) are thought to be responsible for tumor regeneration after treatment. It has beenshown that lung CSCs are chemoresistant. These cells have been found to be highly tumorogenic and have high metastatic poten-tial. They also express specific markers specific to CSCs. We investigated whether NSCLC CSCs are radioresistant and whetherthey share a similar marker profile.
Materials/Methods: NSCLC cell lines H460 and A549 were used in these experiments. Cells were irradiated (100,000 cells/1 mLof media) to doses of 0 Gy-10 Gy using a Cs137 gamma irradiator. Following radiation, cells were plated into 6-well plates andgrown in media supplemented with 10% FBS, under adherent conditions, for a duration of 7-10 days. The appearance of colonies