Acute Vision Loss No laughing matter… Dr Aaron J Wong MH Intern 26 April 2012.
-
Upload
sherman-watkins -
Category
Documents
-
view
216 -
download
1
Transcript of Acute Vision Loss No laughing matter… Dr Aaron J Wong MH Intern 26 April 2012.
Ms Smith
• 70F with no previous ophthalmic history• Sudden loss of vision in R eye• No improvement over 6hr• What do you do?
Outline
• Ophthalmic emergencies - Acute visual loss• Anatomical sieve to the eye• Causes - immediate, emergent, urgent• History & Exam• Cases• Questions
Ophthalmic emergencies
Most sight-threatening conditions present as:• trauma, including chemical burns • acute loss of vision• +/- painful red eye(s)
reduced vision + red eye = emergency
Vision Loss• Rapidity is the most important factor• Acute = minutes to hours; Subacute = days• Chronic = weeks to months• Chronic >>> acute, but ACUTE = EMERGENCY
• Acute persistent visual loss (PVL) = a sudden deficit in visual function in one or both eyes lasting more than 24 hours
• Acute transient visual loss aka. amaurosis fugax
• Ddx for amaurosis fugax are few (temporary vascular occlusion/carotid artery disease, or temporary neuronal depression related to seizure or migraine, ?temporal arteritis)
• Ddx of PVL is large.
Approach to Acute Visual Loss
• Sudden loss or blurring of vision is an emergency > characterize properly
• Always exclude temporal arteritis because of immediate risk to other eye
• Refer, refer, refer! Stratify by – Immediate– Emergent (same day)– Urgent (24-48hr)
Ddx
• ABCDEFG – ED/Trauma
• Probability – Very common, common, uncommon, rare
• VITAMIN CD• Masquerades
• Anatomical
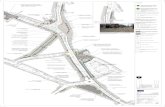
Anatomical Sieve
Taken from: http://www.garetina.com/about-the-eye
Ocular Extraocular
Media Retinal Neural visual pathway
Anatomical SieveOcular
ExtraocularMedia Retinal Neural visual pathway
Keratitis +/- !endophthalmitis
Corneal edemaTrauma!AACG
Hyphema
Lens changes
Uveitis
!Retinal artery occlusion
Retinal vein occlusion
Retinal detachment +/- Vitreous hemorrhage
Acute maculopathy
Optic nerve disease
!Arteritic – GCANon-arteritic
Optic neuritis
ChiasmalPituitary
apoplexy
!RetrochiasmalStroke/TIA
Tumor+haemorrhage
Other – Drugs/Neoplasia
Effects of TraumaOcular
ExtraocularMedia Retinal Neural visual pathway
Keratitis +/- !endophthalmitis
Corneal edemaTrauma!AACG
Hyphema
Lens changes
Uveitis
!Retinal artery occlusion
Retinal vein occlusion
Retinal detachment +/- Vitreous hemorrhage
Acute maculopathy
Optic nerve disease
!Arteritic – GCANon-arteritic
Optic neuritis
ChiasmalPituitary
apoplexy
!RetrochiasmalStroke/TIA
Tumor+haemorrhage
Other – Drugs/Neoplasia
History (HOPC)• Timing —sudden onset of visual loss vs. sudden discovery of preexisting
visual loss• Laterality
– Monocular > anterochiasmal/ocular;– Bilateral > retrochiasmal/extraocular/systemic
• Quality – Diffuse/localized– Across midline– Severity
• Onset– Acute (minutes to hours)– Subacute (days)– Chronic (weeks to years)
• Progression & Duration
History (Assoc Sx)• Trauma• Flashes +/- floaters > retinal detachment/haemorrhage +/- PVD• Diplopia• Pain - presence / absence not as useful; unless pain is severe!
– Anterior segment• Keratitis > sharp superficial pain• AACG > deep brow ache with N&V• Endophthalmitis > deep boring pain
– Optic neuritis > pain worse with eye movement• Redness — Anterior segment disease + uveitis• Other neurological sx- weakness, numbness/tingling, slurred speech,
vertigo/ataxia• Headache - rarely due to a refractive cause• Systemic features - scalp tenderness, jaw claudication, proximal weakness,
fever, night sweats, weight loss
History (Relevant PMHx)• Ophthalmic history
– Past episodes - amaurosis fugax– Recent cataract surgery > retinal detachment, endopthalmitis– Myopia > retinal detachment; Hypermetropia > AACG– Contact lens use - Corneal ulceration in contact lens wearers– Chronic conditions ie. AMD, Glaucoma > acute on chronic presentation– Family hx - Glaucoma
• Systemic diseases/risk factors – Diabetes - RVO, neovascularization +/- vitreous haemorrhage, iris
neovasculization > glaucoma, optic neuropathy, myopic lens shifts, cataracts, corneal abnormalities
– Hypertension > ocular vascular diseases– Coronoary artery disease, PVD, hyperviscosity states
History (Medications)
• Eye drops vs systemic• Anticholinergics: loss of accommodation, angle closure
glaucoma• Topiramate: angle closure glaucoma.• Sildenafil: blue vision, ischemic optic neuropathy• Digoxin: yellow vision• Amiodarone - progressive vision loss• Bisphosphonates: uveitis• Rifabutin: uveitis• Sulfonamides: myopia• Toxins - methanol consumption
Exam
• ABCDEFG – General Inspection of head and neck for trauma
• Visual acuity –one eye at the time, best corrected +/- 1mm pinhole; distance & near
• Confrontation visual fields - red object• Evaluation of EOM• Pupils - symmetry, reactivity to light, pupillary reflex, RAPD!!!
• Fundoscopy +/- slit lamp• +/- Fluorescein application• +/- Intraocular pressure testing (by tonometry or palpation)
Mx (Stratification)• Immediate referral
– Acute central retinal artery occlusion – 8hr window– ?GCA – save the remaining eye– IOP > 40 mm Hg + eye pain ie. AACG– intracranial pathology (stroke, tumor, bleed, or elevated ICP) r/f to
neurological/neurosurgical.• Emergent referral (same day)
– Retinal detachment– Infectious keratitis +/- Endophthalmitis– Hyphema
• Urgent referral (24 – 48hr)– Central retinal vein occlusion.– Acute maculopathy.– Vitreous hemorrhage.– Optic neuritis– Non-infectious uveitis
Case 1 – Ms Smith
• 70F with no previous ophthalmic hx• Hx– Sudden loss of vision in R eye <6hr ago– Painless, no redness– Transient blurring of vision 2wk ago but recovered– PMHx – IHD, diabetes (on meds)
• O/E– VA (R eye) <6/60 – VA (L eye) 6/9– RAPD
Case 1 – CRAO
• Hx– Rapid onset, painless
• O/E– Pale retina– Arterial narowing– Cherry red macula (>4hr)– Embolus may be seen– Optic disc not pale or swollen
Case 1 – CRAO
• Mx– Exclude GCA – Hx & urgent CRP/ESR– Immediate referral to ophthal; <8hr window– Lower IOP - azetazolamide 500mg stat– Ocular massage
• Use index fingers of each hand • [5s pressure, 5s release] x20
– Start aspirin– Investigate for TIA
• Cardiac exam• Carotid US• Echocardiogram• Lipids, fasting BSL (CV RF)
Case 2 – Ms Lee• 70F with no previous ophthalmic hx• Hx
– Ongoing diplopia & blurred vision– Sudden loss of vision in R eye– Painless, no redness– Temporal headache, scalp tenderness– Jaw claudication, myalgia, fatigue– Fever/night sweats, anorexia, weight loss– PMHx – polymyalgia rheumatica
• O/E– VA (R eye) hand movements– VA (L eye) 6/6– RAPD
Case 2 – GCA
• Mx: – Immediate referral– Corticosteroids
• Methylprednisolone 1 g IV, daily for 3 days• Prednis(ol)one 40 to 60 mg orally, daily in the morning for 2 to 4
weeks. • at weekly intervals reduce the daily dose by a maximum of 10%—
provided the ESR and CRP levels remain normal– Aspirin 100 mg orally, daily– Ix
• Urgent ESR, CRP• Temporal artery biopsy (3-5cm)
Case 3 – Mr Yao• 70M basketball player from China• Hx
– Reduced vision in R eye– SEVERELY painful – deep brow ache/headache, red eye– Haloes around lights, photophobia– Abdo pain, N&V– Ophthal hx – hypermetropia, +3.0 D
• O/E– Diffusely red eye– VA (R eye) 6/24– VA (L eye) 6/6– Mid-dilated, oval pupil– Dulled & irregular light reflex– Cloudy cornea– IOP 40mmHg, firm globe
Case 3 – AACG
• Mx– Immediate referral– Lower IOP– Medical• Pilocarpine 4% eye drops, 1 drop q5min for 1st hr• Acetazolamide 500mg po/IV, then 250mg po q6hr• Other eye drops ie. timolol, brimonidine, latanoprost
– Laser perpiheral iridotomy to relieve pupil block; – May require trabeculectomy
Case 4 – Mr Wong• 40M amateur boxer, received blow to head• Hx
– Sudden, marked visual loss in R eye– Rapidly progressive– Preceding flashes and floaters– No redness– Ophthal hx – myopic, uses contacts; -8.0 D
• O/E– Bruise to head– VA (R eye) 6/60– VA (L eye) 6/6– VF (R eye) abnormal inferior hemisphere– Dulled red reflex– ?RAPD
Case 4 – Retinal detachment
• Mx– Urgent ophthal referral– Check the other eye! BL in 10%– Rhegmatogenous (primary) vs.
tractional vs. exudative vs. haemorrhagic– Pre-detachment – Cryopexy or laser retinopexy– Scleral buckling + cryopexy/laser– Vitrectomy + cryopexy/laser– Pneumatic retinopexy
Case 5 – Mr Schmoe
• 60M, recent cataract surgery• Hx– Reduced vision over 2 days in R eye– Painful, red– Eyelid edema, congested eye
• O/E– Diffusely red eye– Sediment in anterior chamber– VA (R eye) 6/24– VA (L eye) 6/6
Case 5 – Endopthalmitis
• Mx– Urgent ophthal referral– Ideally, Gram stain from hypopyon at surgery
directs Abx regimen– If significant delay, give empirical Abx• Ciprofloxacin 750mg po stat• Vancomycin up to 1.5g IV stat• DO NOT USE TOPICAL ANTIBIOTICS, AS PRESERVATIVES
ARE TOXIC TO INTRAOCULAR CONTENTS
Sources
• BMJ Best Practice – Vision Loss• UpToDate - Approach to the adult with acute
persistent visual loss• Therapeutic guidelines - Ophthalmic
emergencies, acute vision loss• RVEEH - Golden eye rules• Dr. Mark Daniel - Sudden Visual Loss• Dr Shueh Wen Lim – Acute Vision Loss