Acute Coronary Syndrome (ACS) - Mandeville Fire … 1 inch NTG paste TD Unstable Angina NTG 0.4 mg²...
Transcript of Acute Coronary Syndrome (ACS) - Mandeville Fire … 1 inch NTG paste TD Unstable Angina NTG 0.4 mg²...
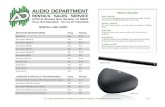
Routine Medical Care
12-lead EKG (ASAP)
Aspirin 160 - 325mg¹ PO (chewed)
Notifying the receiving ED as early as possible should take high priority when infarct is suspected. Transport to a hospital with cardiac catheterization capabilities.
Acute Coronary Syndromes include unstable angina and ST elevated myocardial infarction (STEMI)
Stable Angina
NTG 0.4 mg² SL repeat q 3 min PRN
X 3 doses with SBP >100 and/or Apply 1 inch NTG paste TD
AMI (STEMI)
NTG 0.4 mg² SL repeat q 3 min PRN
X 3 doses with SBP >100 and/or Apply 1 inch NTG paste TD
Unstable Angina
NTG 0.4 mg² SL repeat q 3 min PRN
X 3 doses with SBP >100 and/or Apply 1 inch NTG paste TD
Morphine Sulfate 2-4mg IV / IO q 2min. PRN to MAX of 10mg
OR Fentanyl 25-50mcg IV/IN/IM q 2min. PRN to MAX of 200mcg
¹ Aspirin (ASA) is contraindicated in pts with current or recent GI bleeding & known ASA allergic reactions . ASA is relatively contraindicated in patients with history of asthma and Medical Control is to be contacted prior to administration.
² Nitroglycerin (NTG) is contraindicated in patients who have taken Viagra or Levitra within the past 24 hours (Cialis in the past 48 hours). NTG SL tablets and NTG SL spray may be used interchangeably.
•Age and cardiac risk factors (defined in the Protocol Preambles) are a key evaluation tool in this protocol. Major riskfactors should be documented on the EMS Run Report.
•If the administration of one NTG results in a substantial decrease in blood pressure, discontinue further NTG use; thisresponse may be indicative of an MI involving the right ventricle. This hypotension usually responds well to a fluid bolus (NS). A common finding associated with a right sided inferior MI is ST elevation in V4R with bradycardia.
•Treat life-threatening arrhythmias per the appropriate protocol before initiating this ACS protocol.
• Consider a right sided 12-lead EKG (V4R) for suspected Inferior STEMI (leads II, III, AvF).
•Ventricular ectopy typically does not require treatment unless the ectopic beats are greater than the number of regular(non ectopic) beats and / or a patient is hemodynamically unstable.
•Paramedics treating patients within this protocol should minimize on scene time to 15 minutes for STEMI.
Stable Angina • can be controlled by NTG & lifestylemodification • pain at rest is unusual• precipitating factors are usually known andpredictable • relieved by rest or NTG
Unstable Angina (considered an ACS) • pain at rest• pain does not follow a pattern or the usualpain pattern worsens • usually not relieved by rest or medication• highly suggestive of impairment tovasculature and/or myocardium
Acute Coronary Syndrome (ACS)
Chest Pain not relieved & SBP ≥ 100mm/Hg
Chest Pain not relieved & SBP ≥ 100mm/Hg
Revised July, 2015
Morphine Sulfate 2-4mg IV / IO q 2min. PRN to MAX of 10mg
OR Fentanyl 25-50mcg IV/IN/IM q 2min. PRN to MAX of 200mcg
Consider Zofran 4mg IV PRN for nausea/vomiting with active chest pain
1
ASYSTOLE / PEA
ASYSTOLE / PEA
AHA ACLS 2015 updates places special attention on the value of chest compressions & minimizing interruptions to < 5 seconds. Manual chest compression rate = 100-120/minutes pausing only to verify
cardiac rhythm & check pulses every 2 minutes. Mechanical chest compressions are per manufacturer’s recommendations. Ventilations are withheld during the first 8 minutes unless otherwise indicated.
Confirm absence of pulse, apnea & no signs of life. Immediately begin effective chest compressions
Attach Monitor without interrupting Chest Compressions; confirm Asystole / PEA
Consider Carotid or Femoral Doppler to confirm absence of pulse
· Establish IV/IO access ASAP without interrupting chestcompressions
· Epinephrine 1mg IV/IO ASAP repeat q 3 - 5min
Search & treat for possible contributing factors3
Hs & Ts
< 5 sec pause q 2 min for rhythm / pulse check
Only if acidosis is suspected (i.e. prolonged down time)Sodium Bicarbonate 1mEq/kg*
3Contributing Factors:· Hypoglycemia – treat with Dextrose 50%· Hyperkalemia – Calcium Chloride 8mg/kg for known hyperkalemia· OD - of tricyclic antidepressants Sodium Bicarb and/or Narcan 2mg IV for narcotic OD· Tension pneumothorax - Needle Decompression or Heimlich Valve Kit· Hypothermia – avoid rigorous movement of patient; especially if patient regains pulse. Excessive movement could cause V-Fib or
V-Tach. This is rare but when it occurs the VF/VT is almost always refractory.· Hypovolemia – Fluid bolus* With proper and effective CPR, acidosis, in the absence of prolonged down time, usually does not occur and therefore, SodiumBicarbonate should not be needed.
· Effective chest compressions &Early defibrillation takes priorityover ANY OTHER TREATMENT.
· Withhold ventilations during the first 4cycles of chest compressionsUNLESS indicated by nature of arrest(choking, peds, lung disease, etc)
· IV / IO access & First line medications(Early Epinephrine administration haspriority over any advanced airway.
· ET without ventilations is a means ofsecuring the airway if resources allow
· Pause for ≈ 5 sec q 2 min to verifyEKG & pulse check
After 4 cycles of chest compressions, begin ventilations (unless indicated earlier) at 1 per 6 – 8 sec / 8 -10 min
Revised 6/2016
2
Bradycardia (Symptomatic)
Atropine 0.5mg IV/IO may repeatq 3 - 5 min to a max of 3 mg. If pt is, or becomes unstable do not delay T.C.P.
Obtain 12-lead EKG
Supportive care; monitor for s/s of symptomatic bradycardia.
Contact Med-Control IF needed
TCP, set rate b/t 70-80 bpmStart at 50 milliamperes (mA), increase output until
capture is achieved¹ then add 2 mA for safety margin.
Dopamine 2 to 10mcg/kg/minEpi 2 – 10 mcg/min
Pre-medicate with Versed 2.5 - 5 mg IV/IO if possible
¹ Widening of QRS and a broad T wave after each spike.
•Symptomatic bradycardia is defined as pulse < 60 beats per minute (bpm) with a SBP <100mm/Hg, SOB, altered mentalstatus, and/or other signs of hypoperfusion. (Well conditioned athletes could have HR < 60 & SBP < 100 normally)
•Patients presenting with possible cardiac related chest pain and/or STEMI should NOT receive atropine, unlesshemodynamically unstable, prior to consulting with Medical Control.
•Transplanted hearts will not respond to Atropine; TCP is the treatment of choice
• TCP is the treatment of choice for 2nd degree type II and 3rd degree AV heart blocks with serious S/S. Contact MedicalControl if no serious S/S exist. Atropine is NOT indicated for AV blocks at this level.
AV Block AV Block -- 22°° IIII or 3or 3°° NonNon--SymptomaticSymptomatic
If symptomatic prepare for TCP
Each patient will obviously present differently therefore, it is unrealistic to indicate when TCP is or is not needed. Paramedics should use their clinical judgment to make that decision; if in doubt call Medical Control.
Routine Medical CareAtropine is NOT indicated
for 22°° II or 3II or 3°° AV blocks
SymptomaticSymptomatic((Non 2Non 2°° II or 3 II or 3 °°))
Transcutaneous Pacingas needed
At ANY TIME the above rhythms are present Transcutaneous Pacing (TCP) Pads MUST be
applied (asymptomatic or symptomatic).
Revised 6/2016 3
CARDIAC ARREST
· HISTORY:· Estimated down time; Events leading to arrest, DNR / Living Will, Underlying Causes, SAMPLE History, Crime Scene
SIGNS AND SYMTOMS:Unresponsive, No Signs of Life,
Apneic, Pulseless
Rhythm Shockable?
TEAM APPROACHTeam Leader Designates Assignments and Actions
Defibrillate at Maximum Energy Level3 &
Immediately Resume Effective Chest Compressions x 2 Minutes
Pause q 2 min for < 5 sec to determine pulse & rhythm
IV / IO Access Without Interrupting Chest Compressions ASAP
Epi 1:10.000 q 3 – 5 minutes ASAP during the beginning of chest
compressions cycles for optimum effectiveness
Pearls:·
1 Respiratory / Ventilatory management becomes a higher priority if indicated as cause for arrest (Choking, Pediatrics, COPD, etc.) otherwise an Oral Pharyngeal Airway with a NRB @ 15 LPM is appropriate. Also, endotracheal intubation connected to BVM & 100% O2 without ventilation is appropriate to secure an airway without compromising chest compressions
· 3 Regardless of defibrillator model, initial and subsequent joule settings will be at maximum energy
· High quality chest compressions with minimal interruptions have a greater impact on patient outcome than anyintervention.
· Ventilations (when indicated) should be no more than 8 – 10 per minute. Avoid hyperventilation.
V-Fib / Pulseless V-Tach??
Immediate Manual Chest Compressions at 120/Min x 2 Minutes Without Ventilations unless indicated1
Mechanical Chest Compressions per Manufacturer’s Recommendation
Connect Patient to Defibrillator / AED While Continuing Chest Compressions
Asystole / PEA
CARDIAC ARREST
Effective Chest Compressions, Early administration of
Epinephrine 1:10,000 IV / IO, andFocus on Treatment for
Underlying Causes (Hs & Ts)
Anti-Arrhythmics should be attempted after the 2nd or 3rd
Defibrillation (See V-Fib / Pulseless V-Tach Protocol)
Pause q 2 min for < 5 sec to determine pulse & rhythm
Refer to Asystole / PEA ProtocolAfter 4 Cycles of 2 minutes Chest
Compressions, an Advanced Airway should be completed and the
Appropriate Protocol continued
Secure an Airway without Ventilating (unless indicated) OPA, NRB & Provide
High-Flow O2
NOYES
Early administration of Epinephrine 1:10,000 IV / IO
Revised 6/2016
4
CHF / Pulmonary Edema
Routine Medical Care (including temperature)
Recognition is Key
Medical History Indications
• Hx of CHF, MI, A-fib, renalfailure
• Orthopnea (# of pillows underhead to facilitate breathing)
• Paroxysmal Nocturnal Dyspnea
• Prior intubation
• Recent or increasing dyspneaupon exertion (DOE)
• Takes diuretic
Physical Exam Indications
• Dyspnea
• Hepatojugular Reflux¹
• HTN
• JVD at 30° elevation
• Pitting edema
• Rales / Rhonchi (gurgles)
• TachycardiaBlood Pressure
& Early 12 lead EKG
to assess for STEMI
• Nitroglycerine (NTG) 0.4mg SL, & may repeat q 5min as long as SBP >100mmHg,
ALSO • NTG paste 1in. TD may be used to supplement NTG
SL per SBP >90mmHg
Dopamine Infusion 5 – 20 mcg/kg/min or
Norepinephrine 1 – 10 mcg/min
BVM’s are NOT only for apneic
patients! Positive Pressure
Ventilation (PPV).
¹ Hepatojugular reflux indicates right sided heart failure. With the patient sitting at a 30° angle, palpate the abdomen over the liver lightly, if the jugular veins rise ≈ 4 cm = positive reflux.
• Consider myocardial infarction as a cause of pulmonary edema—transport to facility with cardiac catheterization lab.
• In the elderly and recently institutionalized patients consider pneumonia.
• Avoid NTG in patients that have taken Viagra or Levitra in the past 24 hours, or Cialis in the past 48 hours
• Consider the use of quantitative ETCO2 as a diagnostic tool.
Contact Medical Control immediately after the starting the infusion. Because
CPAP has the potential to further decrease blood pressure, contact
Medical Control for the use of CPAP.
Systolic BP > 100mm/Hg with pulmonary edema and/or R.R. ≥ 30
Systolic BP < 90 – 100mm/Hg
Revised July, 2013
Early CPAP 5-10cm H2O for severe dyspnea related to acute pulmonary edema
5
Resuscitation should not be attempted in the following situations prior to contacting Medical Control:
Lividity Rigor mortisBody decomposition, decapitation, hemi-corpectomy or incineration Any reason to believe CPR is not indicated or desired, especially with known terminal
illness.Presence of legal documents (“Advance Directives,” “Living Wills,” POLST
(Physicians Orders for Life Sustaining Treatments) or “DNR”) stating resuscitative efforts be withheld.
CRIME SCENE PRESERVATION
EKG electrodes may be placed posteriorly or on limbs whenever necessary.
Every effort possible should be made to preserve a crime scene
DOCUMENTATION
Asystole EKG strip in at least two leads should be included in the EMS Run Report along with proper documentation.
Document the scene findings including: medications, medical history, last time pt was spoken to, position found, skin temp, pupils, any trauma or deformity etc…
Contact Medical Control for DNAR & time of death
If EMS arrives to find CPR in progress on a patient who is clearly deceased or a patient who meets the criteria listed above in the blue box, CPR can be stopped with orders from Medical Control.For traumatic DNAR, see the Adult Traumatic Prehospital Termination of Resuscitation Protocol.
ATTEMPT TDO RESUSCITATE (DNAR)
DO NOT ATTEMPT TO RESUSCITATE (DNAR)
DO NOT ATTEMPT TO RESUSCITATE (DNAR)
Revised 6/2016
6
Repeat Primary Assessment
Post Resuscitation
Management protocol Monitor EtCO2 (ideal >20 mm/Hg)
Resp rate < 12 (do not hyperventilate)Maintain SpO2 ≥ 94%
If post VT / VF arrest, contact Med Control for anti-arrythmic therapy
Hypotension Significant Ectopy Bradycardia
For refractory shock:
Consider 1000ml NS bolus
and/or
Dopamine 5-20 mcg/kg/min
or
Norepinephrine 1-10 mcg/min
Treat per appropriateCardiac protocol
Treat per Bradycardia protocol
If arrest reoccurs, immediately treat according to appropriate protocol and/or initial successful treatment
Contact Medical Control if further consultation or orders are needed
• If upon successful electrical conversion of VF / VT prior to having administered an anti-arrhythmic, contactMedical Control before administering 150mg Amiodarone over 10 minutes.
• Titrate Dopamine 5-20mcg/kg/min or Norepinephrine 1-10mcg/min to MAP > 80 / SBP > 90 mm/Hg
• The condition of the post-resuscitation patients fluctuates rapidly, they require close monitoring and post ROSCcare may be planned with online Medical Control
• Hyperventilation is a significant cause of hypotension by decreasing venous return to the heart in post-arrestpatients; this must be avoided at all costs.
Remain on scene to stabilize ▪ Confirm airway/monitor EtCO2▪ Obtain vital signs▪ Obtain12-lead EKG
Revised 6/2016
Post Resuscitation
7
TACHYCARDIA (STABLE NARROW COMPLEX)
TACHYCARDIA (STABLE NARROW COMPLEX)
Stable Narrow Complex >150 bpm
Routine Medical Care with 12-lead EKG
Valsalva Maneuver
Regular Rhythm Irregular Rhythm
Adenosine 6mg IV/IO rapid pushNOTE: Distal IV administration can be
ineffective
If no rhythm ∆ Adenosine 12mg IV/IO rapid push
If no rhythm ∆, Diltiazem 10 mg slow IV/IO over 2 min.Watch for hypotension reaction to medication!!
If no ∆, Repeat Diltiazem 10 mg slow IV/IO over 2 min.
Symptomatic A-Fib or A-Flutter with rapid ventricular response confirmed by
12-lead EKG?
Prior to administration of Adenosine / Diltiazem begin
printing EKG
Despite 12-lead analysis, if still unable to determine whether the rhythm is regular or irregular and the QRS is ≤ .12 sec, give Adenosine 6mg IV as a diagnostic tool to slow the rate.
Identify & Treat Underlying CauseDetermine if Tachycardia is Primary cause of s/s or secondary to underlying condition
Persistent Tachycardia causing: Hypotension?, Acutely Altered Mental Status?, Signs of Hypoperfusion?, Heartfailure?
IF YES: Go to “UNSTABLE (NARROW COMPLEX) TACHYCARDIA"
If no rhythm ∆, Diltiazem 10 mg slow IV/IO over 2 min.Watch for hypotension reaction to medication!!
If no ∆, Repeat Diltiazem 10 mg slow IV/IO over 2 min.
8
TACHYCARDIA (UNSTABLE NARROW COMPLEX)
TACHYCARDIA (UNSTABLE NARROW COMPLEX)
IDENTIFY & TREAT UNDERLYING CAUSEDetermine if Tachycardia is Primary cause of s/s or secondary to underlying condition
Routine Medical Care with 12-lead EKG
IF Patient Condition Permits, Premedicate with Versed 2.5 – 5 mg IV A brief trial of Adenosine 6mg IV for regular narrow complex may be attempted
Synchronized cardioversion:
Initial electrical therapy can begin at 100 joules
Cardioversion Successful?
Upon conversion provide supportive care as clinically indicated
If no conversion contact Medical Control for further orders
Persistent Tachycardia Causing: Hypotension or Acutely Altered Mental Status or Signs of Hypoperfusion orIschemic Chest Discomfort or Acute Heart Failure
See: Stable (Narrow Complex) Tachycardia
NO
YES
Synchronized cardioversion: Double initial energy dose in a “stepwise fashion” (AHA 2015)
YES
NO
Revised 6/2016
9
TACHYCARDIA (STABLE WIDE COMPLEX)
TACHYCARDIA (STABLE WIDE COMPLEX)
Stable Wide Complex (QRS > 0.12) Typically >150 bpm Routine Medical Care
12Lead EKG
Consider expert consultation
YES
Amiodarone 150mg over 10 minutes
Provide supportive care and treat any other complaints per the appropriate protocol.
With polymorphic (irregular) VT, defibrillate at a high energy (150 – 200 joules) setting will most likely be the most effective treatment. The pt is not likely to be stable but stable pts should receive
Magnesium Sulfate 1-2grams IV, Torsades de pointes.
If V-Tach exists after Amiodarone bolus contact Medical Control for further orders
Persistent Tachycardia Causing:
Hypotension or Acutely Altered Mental Status or
Ischemic Chest Pain or Acute Heart Failure
See Unstable Wide Complex Tachycardia
YES
NO
12 Lead Confirms V-Tach? Consider Adenosine ONLY if regular & monomorphic rhythm
NO
CAUTION !!!
Revised 6/2016
10
TACHYCARDIA - UNSTABLE (WIDE COMPLEX)
TACHYCARDIA - UNSTABLE (WIDE COMPLEX)
Unstable Wide Complex > 150 bpm
Contact Medical Control for further orders
Persistent Tachycardia Causing:Hypotension or
Acutely Altered Mental Status orSigns of Hypoperfusion or
Ischemic Chest Discomfort orAcute Heart Failure
See Tachycardia – Stable (Wide Complex)
NO
YES
If patient condition permitsConsider Premedication with Versed 2.5 – 5 mg IV
Synchronized cardioversion:Wide Regular Complex 100 joules
Wide Irregular (Polymorphic) Complexes – Unsynchronized Defibrillation 120 – 200 joules Successful Conversion?
Repeat Electrical Therapy by doubling initial joule levelSuccessful Conversion?
NO
NO
Amiodarone: Loading Dose 150mg over 10 min
YES
YES
CAUTION: Watchout for Hypotension, Pulseless Dysrhytmias, Recurrence of conditions producing hypoperfusion
11
Ventricular Fibrillation / Pulseless V-Tach
Ventricular Fibrillation / Pulseless V-Tach
American Heart Association’s Advanced Cardiopulmonary Life Support (ACLS) 2015 updates places special attention on the value of chest compressions. New guidelines denote specific times when pausing chest compressions is permissible. Refer to the “Pulseless Rhythm Preamble” for more information
Pt apneic and pulseless Begin Manual Continuous Chest
Compressions (CCC) @ 120/min for 2 minutes.
Attach defib pads without interrupting compression / confirm V-Fib /V-Tach
Resume CPR/CCR while chargingDefibrillate @ Maximum energy levels
& immediately resume CPR/CCR for 2 min
After 2 min CPR/CCR Check rhythm, Shockable?
♦ IF Pulses are present, begin PostResuscitation care.
♦ IF NO Pulses are present, go toAsystole / PEA protocol
Establish IV/IO access ASAPEpi 1:10,000 1mg IV/IO q 3-5 min
* First line medications should be given prior to placement of any advanced airway. When CPR is being performed & Once the an advanced airway is confirmed, no longer deliver “cycles” of CPR. Give continuous chest compressions without stopping for ventilations. Pause for <10 sec q 2 min to verify ECG & Pulses. Ventilate q 6-8 seconds ≈ 8 - 10 times / min. CPR guidelines are listed in the Preambles.
Cardiac arrests must be worked on scene for no less than 30 minutes.
f acidosis is suspected (prolonged down time or possible tricyclic OD) Sodium Bicarbonate 1mEq/kg IV/IO
Amiodarone is the antiarrhythmic of choice.
All Medications should be given as soon as possible after defib to allow for maximum circulation prior to pulse & rhythm checks Amiodarone 300mg IV/IO; after 10min second dose is 150mg Magnesium sulfate 1 -2 gm; only for torsades de pointes
Effective CPR performed PTA?
AED used PTA?EMS witnessed arrest?
Determine need of CCR vs CPR?
Priorities are:1. Effective Chest Compressions2. Early Defibrillation3. Early Epi Administration
1st SHOCK
No
No
DOUBLE SEQUENTIAL DEFIBRILLATION MAY BE ATTEMPTED FOR SEVERE REFRACTORY V-FIB (AFTER 5TH SHOCK) WITH SIMILAR MONITORS (i.e. 2
Physio monitors or 2 Zoll monitors, etc.)
Refer to the Cardiac Arrest Protocol
Yes
Resume CPR/CCR while chargingDefibrillate @ Maximum energy levels
& immediately resume CPR/CCR for 2 min2nd SHOCK
After 2 min CPR/CCR Check rhythm, Shockable?
Mechanical Chest Compression Devices should be used according to manufacturer's reccomendations Coronay-Cerebral Resuscitations (CCR) is recomended vs CPR UNLESS underlying causes of cardiac arrest indicate otherwise As Resources allow, an advanced airway should be utilized to secure the airway
Resume CPR/CCR while charging Defibrillate @ Maximum energy levels
& immediately resume CPR/CCR for 2 min3rd SHOCK
Revised 6/201612
All of the following MUST be met to consider “ ”
Pulseless and apneic prior to EMS arrival18 years of age or older> 30 min resuscitation (by EMS) following appropriate pulseless protocol> 30 min of chest compressions with interruptions only for rhythm checks ETT or supraglottic airway with proper documentation of quantitative¹ capnographyPatent IV / IO lineWhen system configuration allows, it is preferable to have two on-duty paramedics, one of which is at a supervisory level and/or an on-line medical director, on scene verifying proper basic and advanced treatments.Patient could not have been in a prolonged perfusing rhythm at anytime (V-Fib is not a perfusing rhythm)
Patient’s immediate family members must have been fully informed of situation, if on scene A safe environment for EMS / first responders
TERMINATION GRANTED ?
Post Termination Procedures:
This patient/body becomes property of the Coroner’s office once pronounced.
ETT / Supraglottic Airways must remain in place. IV / IO’s cannot be taken out.ECG electrodes & Defib pads remain. Do not remove decompression needles (if applicable).
Continue resuscitative efforts.Package patient and transport to the receiving facility.Advise medical direction of any additional changes in the patient’s condition.
¹ Quantitative capnography is defined in the Protocol Preambles.
² Deterioration of a safe scene in which the EMT’s are in danger takes priority over scene time on cardiac arrests. If the scene has become too
dangerous to provide patient care, law enforcement must be dispatched with documentation reflecting such on the run report.
Termination of Resuscitation does not apply in public venues (areas that cannot be readily secured by law enforcement or the coroner) or at any time the medics feel their safety is compromised.
YES NO
If all the above are met, contact Medical Control with your patient report; The Medical Control Physician will determine whether to continue resuscitative efforts beyond this point.
IF NOT, PACKAGE THE PATIENT FOR TRANSPORT TO THE NEAREST MOST APPROPRIATE EMERGENCY DEPARTMENT
TERMINATION OF RESUSCITATION (NON-TRAUMATIC)
TERMINATION OF RESUSCITATION (NON-TRAUMATIC)
Revised 6/2016 13