Acta Neurochir 2012_ p1781.pdf
Transcript of Acta Neurochir 2012_ p1781.pdf

CLINICAL ARTICLE
Management of C2 fractures using Iso-C3D guidance: a singleinstitution's experience
Sven R. Kantelhardt & Naureen Keric & Alf Giese
Received: 24 April 2012 /Accepted: 27 June 2012 /Published online: 12 July 2012# Springer-Verlag 2012
AbstractBackground About 20 % of cervical fractures involvethe C2 vertebra. Many surgical techniques have beenproposed according to the type of fracture. However,morbidity and mortality of these procedures is oftenhigh, which can be attributed to the old age and signif-icant co-morbidities of the affected population and thecomplex anatomy of C2. To target the latter, severalauthors have applied iso-C3D guidance for most of thecommon techniques. We here present our experienceusing a fixed protocol and iso-C3D guidance in all casesof traumatic C2 fractures.Methods Sixteen patients were operated upon betweenApril 2011 and April 2012 using Iso-C3D guidance, follow-ing a fixed routine protocol. The screw position was verifiedby CT-scanning. Intraoperative and clinical parameters wereevaluated.Results Six patients received anterior lag-screw fixation ofodontoid fractures. Two underwent isolated posterior lag-screw fixation of hangman’s fracture. C1 and/or C3 lateralmass, and/or C2 isthmic screws were placed in eightpatients. No screw had to be revised, 3 minor breachingsof the cortical bone of <2 mm were observed.The samestandard protocol for draping, registration of the navigationand Iso-C3D guided drilling could be applied for anterior andposterior procedures, leaving only two variables. This led torapid acceptance of the technique among OR-staff and sur-geons, who felt comfortable with iso-C3D guidance afteronly five cases.
Conclusions Iso-C3D guidance is a safe and straightforwardtechnique for anterior and posterior screw placement in theupper cervical spine.
Keywords C2 fractures . Iso-C3D guidance .
Spinal image-guidance . Spinal trauma
Introduction
About 20 % of all severe traumatic injuries of the cervicalspine involve the second vertebrae [4]. The most commontype of fractures of the second cervical vertebra (C2) areodontoid fractures, which alone account for about 5–15 %of cervical fractures and show an increased rate in elderlypatients [3, 6]. No generally accepted guidelines or treat-ment standards exist for these patients [6]. While manysurgical techniques have been developed to re-establishstability, or to minimize or prevent neurological deficits,non-unions and immobilization-related complications [1, 5,8], some authors propose conservative treatment with a rigidcervical collar as a possible alternative, especially in oldermultimorbid patients [7]. The authors of the latter studypoint out that morbidity and mortalitiy rates of surgicalinterventions are still high. Important reasons for this arereduced clinical condition and co-morbidities of the oftenelderly patients, besides the highly variable anatomy of theupper cervical spine and its close relation to surroundingneurovascular structures [13]. While the patient's generalcondition cannot be influenced by the surgeon, the applica-tion of isocentric 3D C-arm fluoroscopy and image-guidance (iso-C3D guidance) might help to reduce surgery-related complications. Several authors applied this tech-nique for distinct indications, such as anterior lag-screwfixation of type II or III odontoid fractures [6, 14], C1 lateralmass and C2 isthmic screw placement in C1/C2 instability
S. R. Kantelhardt (*) :N. Keric :A. GieseDepartment of Neurosurgery, University Medical Center,Johannes-Gutenberg University Mainz,Langenbeckstr. 1,55131 Mainz, Germanye-mail: [email protected]
Acta Neurochir (2012) 154:1781–1787DOI 10.1007/s00701-012-1443-9

[15], transarticular C1/C2 fixation [2], hangman’s-fractureand traumatic spondylolisthesis C2/C3 [8, 13]. All thesedata suggest that iso-C3D guidance is a technique whichcan be applied for all kind of procedures in the uppercervical region.
We therefore developed a routine procedure applying iso-C3D guidance in all cases of upper cervical instability. Thisarticle summarizes our first experiences following this regime.
Patients and methods
All patients who presented between April 2011 and April2012 in the neurosurgical department of the Mainz Univer-sity Hospital with traumatic fractures involving C2 wereincluded in this series. Fractures were diagnosed by CT-scanning, and, if required, CT-angiography (CT-A) andflexion/extension films were obtained. All patients werescheduled for fixation surgery.
The patients are reviewed retrospectively in this series.We recorded type of fracture and surgical intervention,complications related to surgery and other complications,time in OR and time for surgery, time in Mayfield clamp,time of postoperative hospitalization as well as intraopera-tive X-ray time and dose.
Surgical technique
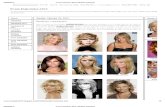
In all cases in which iso-C3D fluoroscopy was applied(Arcardis orbisR, Siemens AG, Erlangen/Germany), the in-strument was connected to an image-guidance system (Koli-briR, Brainlab AG, Feldkirchen/Germany). The surgicalprocedure was chosen according to the type of fracture.Prior to surgery, the patient's head was fixed in a Mayfieldclamp and the patient was positioned in supine or proneposition, according to the selected anterior or posteriorapproach. Lateral flexion/extension tests were performedunder fluoroscopy in the Mayfield clamp and reduction ofdislocated fractures was performed if indicated. Followingthis, the surgical field was disinfected. Surgical drapes wereplaced allowing free rotation of the likewise sterile drapedisocentric C-arm during surgery (Fig. 1). Drill guides wereregistered to the image-guidance device (Fig. 2).
Odontoid fractures of Anderson type II were primarilytreated by image-guided insertion of a K-wire and place-ment of a cannulated anterior lag-screw over this wire(Weber-Schultheiss screw, Synthes, Umkirch/Germany). Ifa posterior approach was selected, 2.9 mm burr holes for theimplantation of lateral mass screws (C1 and/or C3) and/orC2 isthmic screws were placed under image-guidance. Thiswas followed by a second iso-C3D fluoroscopy, confirmingthe burr hole position. Only then were screws (Vertex,
Medtronic, Tolochenanz/Switzerland) implanted, followedby another 3D scan. In two cases posterior lag-screw(Kleinfragment Titan, spongiosa lag-screw, Synthes,Umkirch/Germany) fixation was applied without fusion toadjacent segments. These screws were implanted using thesame technique as for C2 isthmic screws with polyaxialheads. All operations were performed by two surgeonswho previously had been using the same surgical techniqueswithout image-guidance.
Results
Between April 2011 and April 2012, 16 patients (9 female, 7males; mean age 65y; range, 9 to 89) with traumatic C2fractures were surgically treated in our department. Twopatients had motor vehicle accidents and 14 presented afterground level falls. In 14 cases the patients were admitted tothe hospital directly after trauma, while one patient pre-sented four weeks later with nuchal pain. CT imagingrevealed an odontoid II fracture with signs of non-unionformation. One other patient presented with a mobile non-union odontoid type II fracture after a traumatic neck injury40 years previously.
On admission none of the patients showed neurologicaldeficits, all complained about nuchal pain and rigidity andeach acute trauma case was placed in a rigid cervical collar.All fractures were diagnosed by CT imaging. In the caseswith delayed presentation, lateral flexion/extension filmswere additionally acquired to confirm or rule out mobilenon-union. All patients underwent postoperative CT scan-ning to confirm correct implant positions. The mean lengthof clinical follow-up was 5.9 months (range 2 to 10 months).
Type of fracture
One patient presented with a multi fragment odontoid frac-ture of type I+II (6 %), nine patients had type II odontoidfractures (56 %). In one of these patients the type II fracturewas combined with a fractured C1 arch and in one othercase an odontoid type II fracture was combined with afractured C2 arch. One further patient presented with a highodontoid type III fracture (6 %). Two patients presented withisolated hangman’s fractures (13 %), while three showedhangman’s fractures with notable C2/3 instability on lateralflexion/extension fluoroscopy (traumatic spondylolisthesisC2/C3, 19 %).
Surgical procedure
All six patients with isolated acute type II or III odontoidfractures were treated with single anterior lag-screw fixation(Fig. 3a).
1782 Acta Neurochir (2012) 154:1781–1787

A combined C1/C2 lesion and a multi-fragment type Iodontoid fracture, as well as two type II odontoid fractureswith delayed presentation and mobile non-union, were trea-ted with C1 lateral mass and C2 isthmic screw placement.Isolated hangman’s fractures without dislocation of C2/3 onCT and lateral flexion/extension fluoroscopy were treated byisolated posterior lag screw fixation (Fig. 3b). Three cases ofC2/3 instability (spondylolisthesis C2/C3) were treated byposterior C2 isthmic screws and C3 lateral mass screws(Fig. 3c). In one case with combined Anderson type IIodontoid fracture and fractured C2 arch, C1 and C3 lateralmass screws were placed, sparing C2 completely, because ofan anatomical variant with a very prominent vertebral artery
and remaining C2 isthmic diameters of <2 mm (Fig. 3d).The application of C1 lateral mass and C2 isthmic screws,rather than C1/2 transarticular screws, allowed standardiza-tion of the posterior approach. In all posterior cases a mid-line incision of about 7 cm exposing the vertebral columnfrom the occiput to C2 or C3 was performed. Pre- andintraoperative procedures (placement of the Mayfield clamp,positioning draping, registration of navigation and image-guided drilling) followed the same routine in all cases. Onlytwo issues were variable: positioning of the patient in proneor supine position and, in posterior cases, the number ofscrews to be placed (C1 and/or C3 lateral mass screws and/or C2 isthmic screws). This standardization of pre- and
A
B
C
Fig. 1 a shows the steriledraping of the patient (detailsshow the operating field and theC-arms display with 3D recon-struction of the patients cervicalspine). The draping allows freerotation of the likewise steriledraped C-arm for intraoperativeiso-C3D scanning (b), red linesindicate the optical axisbetween camera of the Kolibrinavigation device and theiso-C3D-arm. c shows thenavigation device, consisting of3D camera for tracking of theC-arm and instruments, and thenavigation work-station. Theinlayed image shows the screenof the navigation device duringregistration of a drill guide
Acta Neurochir (2012) 154:1781–1787 1783

intraoperative procedures allowed integration of the iso-C3D
guidance as routine procedure and greatly enhancedacceptance of the new technique. OR staff and surgeonsagreed after about five cases that they felt comfortable with
A
B
CFig. 2 Figure 2 shows theiso-C3D guided drilling processin an anterior case. a shows theinsertion of the navigation-tracked drill guide followingby the drilling process (b).Panel c shows the screen of thenavigation workstation withthe planned screw and thetrajectory targeted by thenavigation-tracked drill guide
A
B
C
D
Fig. 3 Figure 3 shows pre- andpostoperative CT-scans of threecases. The first column depictssagittal reconstructions of thepreoperative CT-scan. The fol-lowing columns show sagittaland axial reconstructions of thepostoperative CT-scans. a:Odontoid fracture type II fixedwith a single anterior lag-screw.b: Hangman’s fracture, fixed bylag-screws in the C2 isthmuses,avoiding fixation of the C2/3segment. d: Hangman’s fracturewith notable C2/3 instability onlateral flexion/extension stud-ies. This fracture was fixed bylag-screws in the C2 isthmusesand C3 lateral mass screws. d:Fixation of a combined type IIodontoid fracture and fracturesof the C2 arch by C1 and C3lateral mass screws. C2 isthmicscrews were not placed becausethe patient displayed ananatomic variant with C2isthmuses of <2 mm diameter
1784 Acta Neurochir (2012) 154:1781–1787

the handling of iso-C3D guidance for the fixation of C2fractures.
Accuracy of the image-guided technique
In anterior procedures the reference star of the image-guidance system was fixed to the Mayfield clamp (Fig. 2).In the first three cases where we chose posterior approachesthe reference star was fixed to the C2 spineous process.In later cases, paralleling anterior procedures, the refer-ence star was likewise fixed to the Mayfield clamp,further standardizing anterior and posterior procedures.After fixing of the reference star, a 3D fluoroscopy wasperformed and the data was uploaded to the KolibriR
workstation.Fixation of the reference star to the spineous process of
the (fractured) C2 was subjectively considered rather unsafe,because of the often high mobility of the bone fragments,even though postoperative CT-scanning of the resultingscrew position did not reveal any misplacement. In proce-dures with the reference star fixed to the Mayfieldclamp, intraoperative targeting of landmarks, such asexposed spineous processes, etc. always resulted ingood accuracy.
In none of the 16 cases did screws placed with iso-C3D
guidance have to be revised because of deviations from theplanned trajectory. No screw trajectory violated the C2transversal foramen or nerval structures (no perforationsinto the spinal channel, no perforations of intervertebralforamina). Clinically silent lateral cortical breachingsof <2 mm were observed in 3 cases, all other screwswere correct. All screws were successfully placed inproximal and distal bone fragments of the concernedvertebra.
Intraoperative X-ray
Average intraoperative radiation time was 258 s (X-raytime in anterior cases was 330 s and 216 s in posteriorcases); this included 3D scanning for registration andfinal confirmation of the implant positions at the end ofsurgery. Average radiation dose was 242 cGy/cm2,194 cGy/cm2 in anterior and 266 cGy/cm2 in posterior cases(Table 1)
Time for surgery
Average time in the OR was 221 min, average time in theMayfield clamp was 154 min. In anterior cases average ORtime was 212 min and 108 min in the Mayfield clamp. Forposterior cases average OR time was 225 min and 181 minin the Mayfield clamp (Table 1). The average time for C1lateral mass and C2 isthmic screw placement was 175 min.
Complications
Four surgery related complications (two major, two minor)were observed.
In a 78-year-old female an anterior lag screw was shownin the correct position on day 1 after surgery. However,2 days later she complained of dysphagia. Repeated CTexamination showed screw loosening and dislocation intoprevertebral soft tissue. She was revised on day 4 andunderwent C1 lateral mass and C2 isthmic screw placement.
The second major complication was observed in a 82 yearold female. Fatal ischemic cerebellar and brain-stem infarc-tion occurred 12 h after placement of C1 lateral mass and C2isthmic screws. Unfortunately, no CT-A was performedbefore surgery. Retrospective evaluation of the initial CT-scan and a postoperative CT-A revealed that fragments ofthe fractured C1 arch compromised the elongated vertebralarteries bilaterally in the absence of screw violations of thetraverse foramen. The right sided artery was occluded. Dis-location of bone fragments by pre- or intraoperative manip-ulation or by the C1 lateral mass screw's polyaxial head androd were considered as possible reasons.
The first minor complication occurred in a 63 year oldfemale with traumatic non-union odontoid fracture type II.Postoperatively and at last follow up (5 months after sur-gery) an occipital hypaesthesia corresponding to the left C1dermatoma was noted. A postoperative CT-scan revealed nonerve root compression. An intraoperative lesion of left C1nerve root during preparation of the left C1 lateral mass isthe suspected cause of this neurological deficit. The secondminor complication occurred in a 63 year old male patientwho suffered a motor vehicle accident including a multi-fragment type I odontoid fracture. He underwent C1 lateralmass and C2 isthmic screw placement. The patient could notbe mobilized directly after surgery due to other injuriesincluding several extremity fractures. On day 11 after sur-gery a local wound healing disorder was diagnosed andlocally revised on day 12.
Non-surgical complications included development of achronic subdural hematoma, probably associated to the pri-mary trauma, and one intraoperative non ST-elevation car-diac infarction, which, however, was followed by a fatalmajor infarction 5 days postoperatively.
Postoperative hospitalization
Average postoperative hospitalization was 13 days includ-ing hospitalization for non-surgical complications and treat-ment of other injuries which were acquired together with C2fracture. Following anterior screw fixation, average postop-erative hospitalization was slightly longer than followingposterior procedures (14 days and 12 days respectively,Table 1).
Acta Neurochir (2012) 154:1781–1787 1785

Discussion
All 16 patients presenting with traumatic fractures involvingC2 were stabilized by iso-C3D guided screw placement. Intro-duction of a standard protocol with only two variables sup-ported rapid integration of iso-C3D guidance as routineprocedure. The high acceptance among OR staff and surgeonsalike after only about five cases documented this impressively.
Anterior lag-screw fixation of type II and high type IIIodontoid fractures can be regarded as standard treatment andhas been combined with iso-C3D guidance (Martirosyan et al.,26 patients in the navigated group [6]; Yang et al., 13 patients inthe navigated group [14]). Posterior C1/C2 fixation by C1lateral mass and C2 isthmic screw placement using iso-C3D
guidance was described by Yang et al. (12 patients in thenavigated group [15]) and iso-C3D guided C1/C2 transarticularfixation was described by Börm et al. (14 patients in thenavigated group [2]). In our department, we prefer C1 lateralmass and C2 isthmic screws instead of transarticular C1/C2fixation. Like the groups around Ringel and Tessitore [9, 12],we considered this a safe technique. Besides, the technique caneasily be adapted to the C2/C3 segment or to the placement ofC2 isthmic lag-screws. Thus we could standardize our posteriorapproach for all cases involing C1-C3. Iso-C3D guided isolatedposterior lag-screw fixation of the C2 isthmuses was to ourknowledge described in only two case-reports [8, 10], whileiso-C3D guided placement of C2 isthmic screws in combinationwith lateral mass screws in C3 (andC4) for hangman’s fractureshas been described by Tian et al. in a series of 14 cases [13].
These reports and series show that iso-C3D guidance canin principle be applied in all kind of C2 fractures, thought ithas not yet been integrated in a routine protocol for all uppercervical fractures, nor have the different techniques beenreviewed in a single series.
In our series, accuracy of screw positioning by iso-C3D
guidance was satisfactory in all cases. No screw had to berevised because of misplacement, no screw entirely missed
one of the fragments, and no neurovascular structures werecompressed by the screws' trajectories. This corresponds tothe results cited above [2, 6, 13–15]. Fixation of the refer-ence star to the Mayfield-clamp proved a safe, fast andefficient way to register iso-C3D based image-guidance. Itavoided further crowding of the surgical field by the spine-ous process clamp and star. Furthermore, it allowed foranterior procedures and gave assistance during the surgicalapproach before exposure of a spineous process. It couldtherefore in principle be applied for percutaneous screwplacement as recently performed by Sugimoto et al.(although these authors exposed the C2 spineous processfor fixation of the reference star) [10].
In their studies on anterior odontoid screw fixation, Mar-tirosyan et al. and Yang et al. report operating times of83 min [6] and 91.5 min [14], respectively,while our patientsspent in average 108 min in the Mayfield clamp. Unfortu-nately, we did not record the time from skin incision to skinclosure, which would be about 20 min less and thus corre-spond to the results published by others. Interestingly, Mar-tirosyan reports longer operating times without image-guidance (115 min in average), while Yang et al. report theopposite (81.6 min on average for conventional procedures).
For posterior procedures (C1 lateral mass and C2 isthmicscrews) Yang’s group reported average operating times of130 min with iso-C3D guidance and 145 min for conven-tional operations [15], which roughly correlates to our175 min in the Mayfield clamp. For the other proceduresno operating times are published. In our series, however, ORand Mayfield-clamp times for C1 lateral mass and C2 isth-mic screw placement did not differ largely from C2 isthmicand C3 lateral mass screw placements (181 min in averagefor all posterior procedures), which corresponds well withthe application of a standardized protocol.
Yang et al. report average radiation times of 42.9 s iniso-C3D guided and 68.1 s in conventional cases, respectively[14]. This is much shorter than in our data, however it remains
Table 1 Table 1 summarizessome clinical and technical dataof the patients enrolled in thisseries. Please note that the totalnumber of operations was 17 inonly 16 patients, as one patientunderwent revision surgery
Anterior C2lag-screwfixation(n06)
Posteriorstabilization(C1/2/3)(n011)
C2 lag-screwfixation only(ant + post)(n08)
All operations(n017)
Average age [y] 79 59 80 66
Male/female 2/4 6/6 3/5 7/10
Time in OR [min] 212 225 200 221
Time in Mayfield clamp [min] 108 181 121 154
X-ray time [s] 330 216 270 258
Radiation [cGy/cm2] 194 266 267 242
Surgery related complications % 16 (n01) 27 (n03) 12.5 (n01) 24 (n04)
nonsurgical- complications % 16 (n01) 9 (n01) 12.5 (n01) 6 (n01)
Postoperative hospitalization [d] 14 13 12 13
1786 Acta Neurochir (2012) 154:1781–1787

unclear whether it includes time for iso-C3D scanning as itdoes in our data. For posterior procedures (C1 lateral mass andC2 isthmic screws), Yang et al. report fluoroscopy time of 47 s[15]; again our times are significantly longer but include timefor 3D scanning.
In our series, the rate of surgical complications was higherin posterior (27 %) than anterior procedures (16 %). Onepatient died of cerebellar infarction. CT-A revealed occlusionof the right vertebral arteries at the level of the fractured C1arc. This might be attributed to bony fragments, but the closetime relation to surgery (12 h) suggests a connection either tointra-/perioperative manipulation or possible compression ofthe vertebral artery by the rod and/or polyaxial screw head, asdescribed previously [11]. Preoperative CT-A might havebeen helpful and we now perform it in all cases. Howevernone of the complications in our series was related to, or couldhave been avoided by iso-C3D guidance.
Literature gives heterogeneous data for surgical complica-tions following iso-C3D guided C2 stabilization (8.3–42 % [6,14]). However, generally very few of these complications areof importance in the context of iso-C3D guidance. Tian et al.report of two screws which deviated into C2 traverse foramenin 14 patients. Both narrowed the foraminal diameter less than50 % and were conservatively treated with aspirin for12 months [13]. Börm et al. report of one misplaced trans-articular screw (lateral deviation in C1) which was not revisedand showed good fusion after 12 months [2].
Summarizing our experience, iso-C3D guidance is a feasi-ble and safe technique for screw placement in the uppercervical spine. It can be applied independently of the preferredsurgical techniques (anterior, posterior, Magerl, Harms, etc.).Furthermore, it facilitates individual solutions if, for anatom-ical or other reasons, standard procedures have to be modified.
Conflicts of interest None.
References
1. Böhler J (1982) Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am 64(1):18–27
2. Börm W, König RW, Albrecht A, Richter HP, Kast E (2004)Percutaneous transarticular atlantoaxial screw fixation using acannulated screw system and image guidance. Minim InvasiveNeurosurg 47(2):111–114
3. Denaro V, Papalia R, Di Martino A, Denaro L, Maffulli N(2011) The best surgical treatment for type II fractures of thedens is still controversial. Clin Orthop Relat Res 469(3):742–750
4. Greenberg MS (2006) Handbook of neurosurgery, 6th edn. Thiememedical publishers, New York, p 724
5. Grob D, Magerl F (1987) Operative stabilisierung bei frakturenvon C1 und C2. Orthopäde 16(1):46–54
6. Martirosyan NL, Kalb S, Cavalcanti DD, Lochhead RA, UscholdTD, Loh A, Theodore N (2004) Comparative Analysis of Isocen-tric 3-dimensional C-arm Fluoroscopy and Biplanar Fluoroscopyfor Anterior Screw Fixation in Odontoid Fractures. J Spinal DisordTech. PMID:22158300
7. Molinari RW, Khera OA, Gruhn WL, McAssey RW (2011) Rigidcervical collar treatment for geriatric type II odontoid fractures.Eur Spine J. PMID:22094387
8. Rajasekaran S, Vidyadhara S, Shetty AP (2007) Iso-C3Dfluoroscopy-based navigation in direct pedicle screw fixation ofhangman fracture: a case report. J Spinal Disord Tech 20(8):616–619
9. Ringel F, Reinke A, Stüer C, Meyer B, Stoffel M (2012) PosteriorC1-2 fusion with C1 lateral mass and C2 isthmic screws: accuracyof screw position, alignment and patient outcome. Acta Neurochir(Wien) 154(2):305–312
10. Sugimoto Y, Ito Y, Shimokawa T, Shiozaki Y, Mazaki T (2010)Percutaneous screw fixation for traumatic spondylolisthesis of theaxis using iso-C3D fluoroscopy-assisted navigation (case report).Minim Invasive Neurosurg 53(2):83–85
11. Terterov S, Taghva A, Khalessi AA, Hsieh PC (2011) Symptom-atic vertebral artery compression by the rod of a C1-C2 posteriorfusion construct: case report and review of the literature. Spine 36(10):E678–E681
12. Tessitore E, Bartoli A, Schaller K, Payer M (2011) Accuracy offreehand fluoroscopy-guided placement of C1 lateral mass and C2isthmic screws in atlanto-axial instability. Acta Neurochir (Wien)153(7):1417–1425
13. Tian W, Weng C, Liu B, Li Q, Hu L, Li ZY, Liu YJ, Sun YZ (2011)Posterior fixation and fusion of unstable hangman’s fracture byusing intraoperative three-dimensional fluoroscopy-based naviga-tion. Eur Spine J. PMID:22109567
14. Yang YL, Fu BS, Li RW, Smith PN, Mu WD, Li LX, Zhou DS(2011) Anterior single screw fixation of odontoid fracture withintraoperative Iso-C 3-dimensional imaging. Eur Spine J 20(11):1899–1907
15. Yang YL, Zhou DS, He JL (2011) Comparison of IsocentricC-Arm 3-Dimensional Navigation and Conventional Fluoroscopyfor C1 Lateral Mass and C2 Pedicle Screw Placement for Atlan-toaxial Instability. J Spinal Disord Tech. PMID:22105103
Acta Neurochir (2012) 154:1781–1787 1787

Copyright of Acta Neurochirurgica is the property of Springer Science & Business Media B.V. and its content
may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express
written permission. However, users may print, download, or email articles for individual use.