Acne Vulgaris: A Patient and Physician’s Experience › content › pdf › 10.1007... · lege...
Transcript of Acne Vulgaris: A Patient and Physician’s Experience › content › pdf › 10.1007... · lege...

COMMENTARY
Acne Vulgaris: A Patient and Physician’s Experience
Nicola I. Espinosa . Philip R. Cohen
Received: September 3, 2019 / Published online: November 7, 2019� The Author(s) 2019
ABSTRACT
In this article, the first coauthor, a youngwoman with acne vulgaris, shares her experi-ence with the condition; she not only describesthe clinical presentation and the eventual suc-cessful treatment of her acne, but also theemotional consequences that this skin disordercaused. The second coauthor, the patient’sdermatologist, reviews some of the features ofacne vulgaris: morphologic manifestations,pathogenesis, and treatment options. He alsosummarizes the patient’s response to iso-tretinoin therapy. In addition, he reveals hissubsequent enlightenment regarding the acne-
related non-dermatologic effects that thepatient experienced and the significantimprovement of her self-image that occurredfollowing the successful treatment of her acne.
Keywords: Acid; Acutane; Acne vulgaris; 13-cis-retinoic; Isotretinoin; Experience; Patient;Physician; Trans-retinoic; Treatment
Key Summary Points
Acne vulgaris, usually referred to as acne,is an inflammatory condition of the skinthat affects the pilosebaceous follicle.
The pathogenesis of acne is multifactorial:bacterial colonization (byPropionibacterium acnes), follicularhyperkeratinization, inflammation, andsebum production.
The development of acne is influenced bydiet; it is associated with the consumptionof saturated fats, dairy products and foodswith a high glycemic index.
Topical therapies, systemic antibiotics,hormonal agents, isotretinoin andmiscellaneous therapies may beincorporated in the management of acne.
Isotretinoin may be used as the first-linetreatment for severe nodulocystic acne.
The article is part of the Topical Collection on Patientand Physician Perspectives.
Enhanced Digital Features To view enhanced digitalfeatures for this article go to https://doi.org/10.6084/m9.figshare.9959003.
N. I. EspinosaCollege of Sciences, San Diego State University, SanDiego, CA, USA
P. R. Cohen (&)San Diego Family Dermatology, National City, CA,USAe-mail: [email protected]
P. R. CohenDepartment of Dermatology, Touro UniversityCalifornia College of Osteopathic Medicine, Vallejo,CA, USA
Dermatol Ther (Heidelb) (2020) 10:1–14
https://doi.org/10.1007/s13555-019-00335-0

PATIENT’S EXPERIENCE
Cystic acne is a debilitating condition that hada significant impact on my life. So, when myfamily doctor finally referred me to a derma-tologist to see whether I could be treated withisotretinoin (also referred to as 13-cis-retinoicacid), I was absolutely ready.
As superficial as it sounds, the issues I hadwith my outward appearance ran deep. It wasn’t‘‘just acne’’; it was everything to me for 6 years.And as silly as it sounds, I think I identified withthe problems I had with my acne. It was all Icould see when I looked in the mirror and itreflected in my low self-esteem, manifested inthe opportunities I was too afraid or ashamed totake, in how I neglected or avoided others, andthe unnecessary anxiety and disappointmentwith myself.
I had acne when my family and I still lived inHawaii where I was raised and attended tradi-tional public schools, when we moved to Idahowhere I attended an online school for a yearbefore returning to traditional schooling, andwhen we made our last move to California.Throughout these moves and my teen years, Ihad been seen by family doctors in my localtown, and city-based dermatologists in thenearby cities; however, nothing they gave meever worked. After arriving in California, at16 years of age, my acne became even worse.
Since I was 14 years old, I had tested so manytreatments. I had tried topical medications[such as adapalene, benzoyl peroxide, clin-damycin, a combination of adapalene andbenzoyl peroxide, a combination of clin-damycin and benzoyl peroxide, erythromycinand tretinoin (also known as trans-retinoicacid)], oral medications [such as antibiotics(doxycycline and minocycline) and a combi-nation oral contraceptive pill containing ethi-nyl estradiol and norgestimate] and anassortment of facial cleansers, moisturizers,creams, and serums from various companies:Mary Kay, A.C. Care Bee’s, Lancome, Clean &Clear, Cetaphil, Aveeno, Neutrogena, EltaMD,and Shiseido. I had tried it all — as gels, creams,lotions, and ointments at different percentagesand dosages, with different combinations, with
different regimens, and at different times of mylife.
Like many teenagers, I was already very self-conscious and cared about how I looked. How-ever, I observed no improvement in my skinregardless of what I did, or how much money Ispent, or even where I was, or how much timehad passed. This led to both physical and psy-chosocial effects on me.
I was so exhausted. I felt hopeless and,truthfully, ugly. I didn’t want anyone to look atme, so I did everything I could to hide anddirect any attention away from me; however, Istill felt that people were only focusing on myacne when they interacted with me. I also feltlike I was incompetent at everything.
Growing up, as a teenager, was difficult;however, it became even more challenging withmy skin. I usually chose to work alone. I quietlyembraced my self-pity, all under the guise of‘‘independence.’’
In addition, I had spent a lot of time stayingaway from most people and trying to avoid newactivities. In all the schools I went to, I neverjoined a club or openly participated in class oreven talked to anyone (not even during onlineschool!). Assemblies, group projects, presenta-tions, and hands-on work (such as laboratorysessions) were the hardest activities for me todeal with.
In my first year and a half of communitycollege, starting in August 2017, I noticed myacne less often but cared about it much more.Whenever I did have the time to notice whatwas on my face, I immediately felt this urge togo home. Some early mornings I would wake upwith dots of dried blood on my face from pim-ples that popped the night before; it was sophysically and emotionally painful. I dreadedwaking up to this face.
During the drive to school, when I waslooking in the mirror, the sunlight wouldhighlight the horrendous red bumps scatteredall throughout my face — a big one on my nose,tiny ones behind my nose, many spread out onmy cheeks and dotting my forehead and chin,even some on my temples and a couple withinmy eyebrow hairs. If one disappeared, anotherone would show up. It looked as if the pimples
2 Dermatol Ther (Heidelb) (2020) 10:1–14

were running out of room on my face butalways managed to find a spot (Figs. 1 and 2).
Then, early in December 2018, I saw myfamily doctor. He works at a clinic near myhome; he has seen me multiple times since Ihad moved to California, primarily for acnecheckups and prescription refills. At this visit,he finally said, ‘‘I think it’s time for you to go onisotretinoin, but I cannot prescribe it to you. Iam going to refer you to a dermatologist.’’
I had heard so much about this (in)famousmedicine by reading online and watching peo-ple talk about it on YouTube. I knew it was usedas a last resort and that it had a long list ofserious side effects. Some of the side effects mayhave been exaggerated or rare, but the anec-dotes about them were convincing and scary.However, I didn’t care how isotretinoin wouldaffect me if it worked to treat my acne. I knew itwas extremely effective in not only helpingwith acne, but also for clearing it; that was all Ineeded to know.
By mid-January 2019, I had my first derma-tology appointment about Accutane and metDr. Cohen, one of the dermatologists at SanDiego Family Dermatology. My mom was withme since she was hesitant about me taking iso-tretinoin. Dr. Cohen explained the whole
process to me: monthly blood pregnancy tests(the first test at my initial appointment when Iregistered in iPLEDGE and the second testwithin the first 5 days of my menstrual periodand at least 30 days after registering, and sub-sequent tests 3 to 4 days before my appoint-ment at a clinical laboratory), other monthlylaboratory studies, a urine pregnancy test dur-ing my monthly dermatologist appointments,registering in the iPLEDGE Program andmonthly completion of the comprehensionquestions on the iPLEDGE Program website,keeping up with the dosing schedule every day,and monthly trips to the pharmacy to get thenext month’s prescription of the medicine. Dr.Cohen also explained the many risks and rulesthat came with isotretinoin. It was a lot ofinformation and responsibility, but I was ready.
My isotretinoin acne treatment lasted about5 months, from February 16th to July 10th. Onemonth after starting isotretinoin, my facedeveloped much larger and redder pimples;also, there were more lesions on my cheeks. Iwas not worried because I believed the medicinewould eventually work by the end of the treat-ment. Besides, I was already used to prior acnetreatments and being told that the worst comesfirst before getting better.
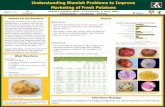
Fig. 1 A 19-year-old woman with severe and recalcitrantacne. Prior to treatment with isotretinoin, right side (a),frontal (b) and left side (c) views of her face show
inflammatory papules and nodules, pustules, comedonesand scarring on both cheeks
Dermatol Ther (Heidelb) (2020) 10:1–14 3

I kept an album on my phone for selfies Itook every other day while on isotretinoin so Icould see my progress over time. This is why Iwas surprised to see how bad my skin was whenI first started the medicine. However, I eventu-ally noticed that my forehead and chin werebeginning to clear up.
By April 2019, the number of pimples on mycheeks was decreasing as well. Although mycheeks were still as red, they were actuallyclearing up. This was wonderful and theimprovement seemed to be happening quickly.Previously, my cheeks were occupied by redpimples; now the acne lesions were fewer andscattered.
By May 2019, my skin was the clearest I hadseen it in such a long time; this is what I hadexpected from the information I had seenonline. However, there were the occasional oneor two pimples that popped up — especially if Ifelt too stressed with school. Also, I still had thescars from past pimples; however, they were alltiny in comparison to the miraculous changethat had occurred on my face.
I graduated community college on May 24th,and I felt invincible. I was proud of myaccomplishments at school and completing asemester where I had tried new things. How-ever, I felt even better knowing my skin looked
great. I felt confident. My clearer skin reinforcedthe positivity and pride I felt from getting mydegree and being accepted to continue my col-lege studies at San Diego State University.
By June 2019, I only had one blemish on myskin. By July 2019, I had none. Dr. Cohen toldme I would have to do one more serum preg-nancy test and an additional appointment toevaluate my skin after being off isotretinoin forat least 4 weeks.
I returned for my August 2019 appointment.My skin had remained almost completely clear(Figs. 3 and 4). However, I noticed that smallpimples only appeared if I was stressed or wasjust not taking care of myself. I realized,throughout this entire process, that I could notjust rely on the medicine. I felt that I also had toconsciously do my part and that I needed todeliberately contribute to my treatment.
To do this, I decided to drink about 65–85 ozof water every day. I was assisted in this taskwith the help of an app called Plant Nanny.Every time I drank water, I had to not only logthe amount of water, but also water a virtualplant. This would keep the plant and the rest ofmy virtual garden alive. I think that maintain-ing my hydration helped me to combat theisotretinoin-related dryness.
Fig. 2 Closer views of the right (a) and left (b) cheeks prior to isotretinoin therapy. In addition to erythematous atrophicscars on her bilateral malar cheeks, there are pustules and inflammatory papules and nodules
4 Dermatol Ther (Heidelb) (2020) 10:1–14

I also forced myself to sleep better. Thisdidn’t always mean going to sleep earlier. Itmeant that I would go to sleep without takingthe stress of school and day-to-day occurrencesto bed with me.
When I woke up each morning, I remindedmyself that I could handle the daily stress of myclasses, projects, presentations and exams. Also,I looked forward to being present in class and Ifelt more comfortable talking to my classmatesand professors. Before, I was anxious all of the
Fig. 3 Resolution of acne after 5 months of isotretinointherapy. The right side (a), frontal (b) and left side(c) views of the woman’s face shows essentially complete
clearing of her acne lesions. There is a single papule on herforehead. The scars on her cheeks are less prominent
Fig. 4 Closer views of the right (a) and left (b) cheeksafter treatment with isotretinoin for 5 months. Shereceived 40 mg daily of isotretinoin the first month and60 mg daily of tretinoin for the second thru fifth months
of treatment. The scars on her bilateral cheeks are lesserythematous. Inflammatory and comedonal acne lesionsare absent
Dermatol Ther (Heidelb) (2020) 10:1–14 5

time; now I was confident that I would notdisappoint myself or others.
I realize that correlation doesn’t equal cau-sation. However, my treatment with iso-tretinoin was definitely the principal factor thatenabled me to physically and psychosociallybecome better; I am so very thankful! Indeed, Ieven got my first job while I was being treatedwith isotretinoin; I will be tutoring college stu-dents in psychology and writing. Although Ibelieve this medicine would not have worked aswell for me if I had not put in the effort tochange my lifestyle, I am convinced that thistherapy did so much for me on its own— just asI had hoped it would.
Since I had so much faith in this medicinefrom the start, my self-esteem continued toimprove as long as I was still taking the pillsevery day. Even in February, when the worst ofmy skin came out and the medicine did notappear to be working, I suppose a placebo effecttook place and I felt like it was working.
My self-esteem was no longer as low as itused to be. I no longer neglected or avoided newclasses, people or activities. Indeed, I was takingnew classes, meeting new classmates and pro-fessors, and finally going to new events.
I was showing my face more often, and I didnot feel afraid or ashamed. I felt happier andmore confident, especially while taking thekickboxing classes twice a week and yoga classonce a week; I had never previously been ath-letic in my life. Similarly, I was participating inclass discussions; I had rarely voluntarily donethat before. This was a huge turnaround for me.
I was very fortunate to have had a relativelysmooth journey with isotretinoin. For the mostpart, the drug-associated side effects that Iexperienced were not like those I had readabout and watched online. The main and onlyside effect that I experienced from isotretinoinwas dryness.
At the beginning, my nose dried up enoughto get occasional nosebleeds, but that stoppedearly on. In contrast, my lips were so drythroughout the entire treatment process that Iwas applying petrolatum to them almost everyhour, every day. After a few months of treat-ment my eyes also became so dry that I had to
completely stop wearing contacts and only wearglasses.
Although these side effects were all nui-sances, they were minor. I felt I was lucky toonly be experiencing these problems from themedicine. I had read and heard about otherpeople suffering from far worse isotretinoin-re-lated side effects: nausea and vomiting, boneand joint pain, decreased night vision, itchyscalp, hair loss or thinning, and depressive orsuicidal thoughts.
I would like to think my skin finally becametired of fighting me and just responded to thetreatment with isotretinoin. I appreciate Dr.Cohen and San Diego Family Dermatology; mydermatologist and the office staff were all veryhelpful and supportive to me. I am so glad thatDr. Cohen started me on this medication andmade sure I was doing okay every month.
I had acne for so many years. In order toensure that isotretinoin worked its best on me, Imade several changes in myself and my life. Inow drink lots of water, keep my lips moistur-ized, stay more physically fit (than I used to be),and allow myself to try new things. This monthI will begin not only my first job as a tutor, butalso my first day at San Diego State University. Iwill be starting with the clearest skin I have everhad in my life, and the most confidence I haveever felt.
PHYSICIAN’S PERSPECTIVE
Acne vulgaris, usually referred to as acne, is avery common skin condition [1]. However, theclinical presentation of acne can vary and thereare several potential treatment modalitiesavailable for patients. This article does notcontain any new studies with human or animalsubjects performed by any of the authors.
Acne lesions include comedones (opencomedones are referred to as black heads andclosed comedones are referred to as whiteheads), papules and pustules, and nodules andcysts. Scarring (which can be atrophic orhypertrophic) may appear at prior lesion sites.Lesions typically appear on the face; however,the chest, back and proximal arms are alsocommon sites [2–4].
6 Dermatol Ther (Heidelb) (2020) 10:1–14

A standardized classification or grading sys-tem for acne does not exist. The AmericanAcademy of Dermatology classified acne intomild, moderate and severe [1]. The UnitedStates Food and Drug Administration (FDA)recommended an Investigator Global Assess-ment scale with grades from 0 (clear skin) to 4(severe); intermediate grades include 1 (almostclear), 2 (mild severity) and 3 (moderate sever-ity) [4].
Acne is an inflammatory condition of theskin that affects the pilosebaceous follicle. Itspathogenesis is multifactorial. The key compo-nents include follicular hyperkeratinization,inflammation, Propionibacterium acnes (morerecently also referred to as Cutibacterium acnes)bacteria colonization, and sebum production[2, 3, 5, 6].
Diet has also been shown to influence thedevelopment of acne. In addition to consump-tion of saturated fats, diets consisting of dairyproducts (including milk) and foods with a highglycemic index (such as baked potatoes, candy,couscous, French fries, high sugar beverages,low-fiber cereals that are high in added sugar,sweetened fruit juices, white pasta, and whiterice) have been associated with acne [7–12].Acne development has also been observed inindividuals attempting to build muscle and/orgain weight by ingesting whey protein supple-ments [13, 14].
The management of acne is guided by theseverity and extent of the lesions. The potentialrisk for acne scarring can be minimized by earlyand effective treatment. The approach to treat-ment may include topical therapies, systemicantibiotics, hormonal agents, isotretinoin andmiscellaneous therapies. Monotherapy or treat-ment regimens that include a combination ofthese modalities may be utilized [1, 2].
Topical therapies include azelaic acid,antimicrobials (such as benzoyl peroxide, clin-damycin, dapsone and erythromycin), retinoids(such as tretinoin which is also referred to astrans-retinoic acid, adapalene and tazarotene)and salicylic acid. Several vehicles can be uti-lized to deliver the agent: bar, cream, foam, gel,lotion, pad, pledget, solution and wash. Con-current topical treatment with benzoyl peroxideand a retinoid should be considered as first-line
therapy for most individuals with comedonalacne and/or inflammatory acne; in addition,topical therapy with a retinoid — with orwithout benzoyl peroxide — should be used formaintenance therapy for most patients withacne [1–4, 12].
The development of antibiotic resistancemay occur when topical antibiotics are used asmonotherapy. However, combinations of ben-zoyl peroxide with either an antibiotic (clin-damycin or erythromycin) or a retinoid(adapalene) are available for treating acne.However, some of the topical therapies shouldnot be used at the same time. For examplebenzoyl peroxide can result in oxidation anddegradation of the isotretinoin molecule. Also,temporary orange discoloration of the skin andhair can occur if benzoyl peroxide and dapsoneare used at the same time [1, 3, 4, 15].
Systemic antibiotics are used in the man-agement of not only moderate to severe acnebut also inflammatory acne that is resistant totopical therapies; they are usually prescribed incombination with benzoyl peroxide and/or atopical retinoid. Tetracyclines (such as doxycy-cline, minocycline and tetracycline) and mac-rolides (such as erythromycin and, lessfrequently, azithromycin) are the mainstayagents used to treat acne. However, otherantibiotics such as trimethoprim (with orwithout sulfamethoxazole), penicillins (such asamoxicillin) and cephalosporins (such ascephalexin) have also been used to treatpatients with acne [1, 3, 4, 12].
Adverse events may occur in individualsreceiving systemic antibiotics. Photosensitivityis a common side effect of tetracyclines; inaddition, these antibiotics should not be used inwomen who are pregnant and children lessthan 9 years of age. Also, the development ofbacterial resistance is a concern when systemicantibiotics are prescribed; therefore, it would beoptimal to limit their use to the shortest possi-ble duration (such as 3 to 4 months) necessaryto successfully treat the patient’s acne[1, 3, 4, 12].
Hormonal agents for acne include combinedoral contraceptive pills (which contain both anestrogen and a progestin component) andspironolactone. The FDA has approved the
Dermatol Ther (Heidelb) (2020) 10:1–14 7

following oral contraceptive pills as second-linetherapy in adolescent or adult women: ethinylestradiol-norgestimate, ethinyl estradiol-norethindrone acetate and ethinyl estradiol-drospirenone. Similar to combined oral contra-ceptive pills, the birth control patch (ethinylestradiol plus norelgestromin) can also beeffective for women with acne; however, higherrates of unintended pregnancies have beenobserved in heavier women (weighing morethan 198 lb or 90 kg) using the patch for con-traception [1, 2, 4, 16].
Certain medications used to treat bacterial orfungal infection can reduce the effectiveness ofcombined oral contraceptives when taken con-comitantly — the antibiotic rifampin and theantifungal griseofulvin. Combined oral contra-ceptives can also be associated with drug-relatedadverse effects such as androgenic effects (hir-sutism and worsening of acne depending on theprogestin component), bloating, decreasedlibido, nausea, and vomiting. In addition, sys-temic adverse events that have been linked tocombined oral contraceptives include cancer(such as a higher incidence of breast and cervi-cal carcinoma), cardiovascular problems (suchas myocardial infarction), stroke and throm-boembolism (deep venous and pulmonary)[1, 2, 4].
Spironolactone is effective in treating hor-monally mediated acne in women. However, itis an aldosterone receptor antagonist and cancause hyperkalemia; indeed, a recent study hasshown that hyperkalemia after initiatingspironolactone was more common in womenbetween 46 and 65 years of age compared tothose in the 18- to 45-year age group [17].Therefore, routine monitoring of serum potas-sium may not be necessary in healthy womenage 45 years or less who do not have renal dis-ease and who are not taking potassium-sparingdiuretic agents [2, 17, 18].
Spironolactone adverse events may includebreast tenderness and menstrual irregularities.In addition, it is contraindicated during preg-nancy since feminization of a male fetus mayoccur. A third-generation or fourth-generationcombined oral contraceptive is often prescribedto women being treated with spironolactone to
ameliorate drug-induced side effects and toprevent pregnancy [19–21].
In addition to conventional treatments ofacne, there are several alternative therapies thatcan be used for the adjuvant management ofthis condition. Some of these therapies includeherbal agents and spices, intralesional corticos-teroids, chemical peels, light devices and lasers.Topical or systemic curcumin (or turmeric) hasbeen used to treat acne [1, 12, 22–24].
An individual inflammatory papule, noduleor cyst, may be clinically treated by injecting alow concentration — such as 3 mg/ml — oftriamcinolone acetonide either into and/oradjacent and beneath the lesion; flatteningoccurs in 2 to 3 days. Chemical peels (usingeither glycolic acid or salicylic acid) may beuseful for treating comedonal acne. However,chemical peels should not be performed inpatients with active infection or open woundsor who have received isotretinoin therapywithin the prior 6 months [1, 12, 25–28].
Photodynamic therapy (utilizing topical5-aminolevulinic acid and intense pulsed blueor red light) may be effective in moderate tosevere acne. Phototherapy using a combinedblue-red light-emitting diode can be performedat home; it safely and effectively treats mild tomoderate acne by attenuating inflammatorycell infiltration, decreasing sebaceous gland sizeand reducing sebum production. Several lasershave also been demonstrated to be beneficial inthe treatment of acne: carbon dioxide, erbium-glass, infrared, potassium titanyl phosphate,and pulsed dye lasers [1, 12, 29–33].
Isotretinoin is an oral systemic retinoid thathas resulted in a significant therapeuticadvancement for the treatment of acne. It canbe used as first-line therapy in the managementof severe nodulocystic acne. In addition, it isindicated for the treatment of recalcitrant acnethat has failed oral antibiotics in combinationwith topical benzoyl peroxide and retinoids.Many of the acne patients who are potentialcandidates for isotretinoin also have severescarring as a consequence of their acne lesions[1, 4, 12, 34, 35].
Isotretinoin effectively targets all aspects ofacne pathogenesis; it decreases not only ker-atinocyte proliferation and thereby reduces
8 Dermatol Ther (Heidelb) (2020) 10:1–14

follicular hyperkeratinization, but also inflam-mation, the growth and colonization of Propi-onibacterium acnes, and sebum production bythe sebaceous glands. An 80% to 90% reductionin inflammatory lesions occurs after a completecourse of isotretinoin. However, 20% to 30% ofisotretinoin-treated patients may developrecurrence of their acne that is severe enough torequire additional therapy, including anothercourse of isotretinoin [1, 2, 12, 34].
Acne patients in whom treatment with iso-tretinoin is being considered should be screenedfor depression and inflammatory bowel disease.Although the evidence regarding an associationbetween isotretinoin and depression is contra-dictory, worsening depression and suicidalideation have been described in some patientson isotretinoin; therefore, counseling andmonitoring patients taking isotretinoin fordepression at each visit may be prudent. Simi-larly, the causal association between iso-tretinoin and inflammatory bowel disease(including ulcerative colitis and Crohn’s dis-ease) is unclear; indeed, some investigators haveobserved an increased risk of developing ulcer-ative colitis in patients being treated with iso-tretinoin [1, 2, 12, 34, 35].
Isotretinoin is a potent teratogen. Sponta-neous abortion is estimated to occur in 50% ofisotretinoin-exposed pregnancies and cardio-vascular and/or skeletal defects are estimated tooccur in 25% of pregnant women who havebeen exposed to isotretinoin. Currently in theUnited States of America, iPLEDGE is the FDA-mandated risk-management program for preg-nancy prevention (http://www.ipledgeprogram.com). Isotretinoin can only be prescribed byclinicians who are registered in iPLEDGE andwritten informed consent must be obtained byall patients who are going to be treated withisotretinoin [1, 2, 12, 34].
The patient taking isotretinoin is alsorequired to register in iPLEDGE. Patients ofchildbearing potential must specify and use twoforms of contraception; in addition, pregnancytests (on the initial office visit or registrationvisit, again within the first 5 days of theirmenstrual period — and at least 30 days afterregistration — before starting the drug, eachmonth during drug treatment and 1 month
after stopping the drug) are required. In addi-tion, both the clinician and patient mustupdate the iPLEDGE site each month confirm-ing the two forms of contraception and that thepatient will neither share the medication nordonate blood during treatment or for 1 monthafter therapy has stopped [1, 2, 12, 34].
In addition to pregnancy testing for patientsof child bearing potential, laboratory monitor-ing for patients being treated with isotretinointraditionally included baseline and monthlyevaluation of complete blood cell countsincluding platelets, serum chemistries [particu-larly liver function tests — aspartate amino-transferase (AST, also referred to as serumglutamic-oxaloacetic transaminase, SGOT) andalanine aminotransferase (ALT, also referred toas serum glutamic-pyruvic transaminase, SGPT)— and less commonly kidney function tests[blood urea nitrogen (BUN) and creatinine], andlipid profile [including cholesterol — total, highdensity lipoprotein (HDL) and low densitylipoprotein (LDL) — and triglycerides] [1].Recent studies have recommended less frequentfollow-up laboratory studies and possibly add-ing gamma-glutamyl transferase (GGT) tomonitor liver function and creatine kinase (CK)to monitor muscle damage [36–38]. In addition,an investigation has shown significantlyincreased plasma homocysteine levels and sig-nificantly decreased folic acid levels in patientsafter isotretinoin therapy; the relevance of theformer and whether supplementation should beinitiated for the latter remain to be determined[39].
The goal cumulative dose of isotretinoin isbased on the patient’s weight; current guideli-nes suggest a cumulative dose between 120 to150 mg/kg. Often, only half or two-thirds of thedaily dosage is given for the initial and possiblysecond month of treatment before increasing tothe standard daily dosage of 1 mg/kg; therefore,approximately 5 months is necessary to reachthe calculated cumulative dose. The dailydosage of isotretinoin is usually divided into amorning and evening dose; since the medica-tion readily dissolves into fat, it is best absorbedwhen taken with food [1, 12].
The most common mucocutaneous sideeffects to isotretinoin include dryness of the
Dermatol Ther (Heidelb) (2020) 10:1–14 9

skin and mucosa of the lips, nose, and eyes.Topical agents should be initiated for xerosis(using moisturizing lotion or cream), cheilitis(applying over-the-counter lip balms), rhinitissicca and nose bleeds (using over-the-countersaline nasal spray) and keratoconjunctivitissicca (using over-the-counter artificial teardrops). Patients may not be able to wear con-tacts on their eyes during isotretinoin treatment[1].
Earlier experiences with isotretinoin raisedconcerns regarding wound healing and thedevelopment of keloids in individuals who hadprocedures while on isotretinoin or after dis-continuation of the drug [40]. However, morerecent reviews suggest that — with the excep-tion of ablative laser resurfacing and der-mabrasion — cosmetic procedures or skinsurgery or wisdom teeth extraction do not needto be avoided during or immediately aftertreatment with isotretinoin [41–44]. Yet, delayof these elective procedures for 6–12 monthsafter completion of isotretinoin therapy — ifpossible — should be considered [1].
Laser in situ keratomileusis (LASIK) andphotorefractive keratectomy (PRK) are not rec-ommended to be performed during isotretinointherapy or within 6 months after completion oftreatment [45, 46]. Also, isotretinoin should notbe prescribed until 6 months following LASIKsurgery [47]. However, recent studies are ques-tioning these current guidelines [45, 48].
MY PATIENT
Nicola was a 19-year-old Filipino woman when Imet her in January 2019. She was in her secondyear of community college and was majoring inpsychology. Her mother had accompanied herto the appointment.
Nicola had a history of recalcitrant acne. Heracne was predominantly inflammatory withintermittent episodes of nodules and cysts. Shehad prominent scarring on her cheeks from herprevious acne lesions.
Topical interventions to treat her acne hadnot been successful. Similarly, she had notimproved with oral antibiotics or a combination
oral contraceptive pill containing ethinylestradiol and norgestimate.
We briefly talked about treatment options.Nicola had no history of either depression orinflammatory bowel disease. Her family doctorhad suggested the possibility of isotretinoin.Therefore, when I suggested isotretinoin for thetreatment of her acne she enthusiasticallyagreed.
I discussed potential adverse events that sheshould expect including dryness of the lips,nasal mucosa and possibly eyes. Other possibleside effects such as muscle and joint pain, moodchange and hair loss were also mentioned. Inaddition, I explained that she could not shareany of the medication and could not donateblood while taking the medication (and for amonth after her last dosage). Finally, I alsostressed that isotretinoin was a teratogen, andshe would need to use a second form of con-traception (besides the birth control pill she wasalready taking) during treatment and for amonth after completion of therapy if she choseto engage in sexual activity.
Nicola understood all of her responsibilitiesincluding checking in with the iPLEDGE website each month. She signed the iPLEDGEagreement. A urine pregnancy test, performedin the office, was negative. Baseline laboratorystudies (complete blood cell counts, serumchemistries including liver function tests, lipidtests including cholesterol and trigylceride, anda serum pregnancy test) to be performed at least30 days later (and within the first 5 days of hermenstrual period) were ordered.
Nicola began isotretinoin after the Februaryoffice visit. Her total dosage was based on herweight: 120 mg per kg. She took 40 mg daily forthe first month and then 60 mg daily thereafter.
Each month Nicola had her laboratorystudies performed a few days before her officevisit; the urine pregnancy test was repeated inthe office. Each month I would monitor herprogress and discuss any symptoms from theisotretinoin. I would also reinforce that sheneither share the medication nor give bloodwhile taking the drug or for 1 month aftertherapy had ended. In addition, after reviewingthe two forms of contraception she was using,
10 Dermatol Ther (Heidelb) (2020) 10:1–14

both of us contacted the iPLEDGE web site andconfirmed this information.
Nicola tolerated the isotretinoin well. Duringthe first month taking the medication, she hadnose bleeds; subsequently, these occurred lessfrequently. Her lips were very dry and she fre-quently applied Vaseline to them. She was notable to tolerate her contact lenses and had towear glasses.
Nicola completed treatment with iso-tretinoin in July 2019. She returned to the office1 month later; her laboratory studies were stillsatisfactory, and the serum pregnancy test wasnegative. Clinical photographs had been takenprior to starting isotretinoin; they were takenagain 1 month after completing therapy (Fig. 5).There had been a significant improvement ofher acne; her face was clear of acne lesions,except for a small papule on her forehead. Theerythematous acne scarring on her cheeks wasstill present, but not as red as before she hadstarted the drug.
Indeed, Nicola’s efficacious clinical resultssecondary to isotretinoin therapy were dra-matic. However, it was not until after reading
Nicola’s ‘experience’ that she shared in thispaper that I became aware of the extent of thepositive impact that this treatment had for her.I had no idea how devastating acne was to her— not only physically but also emotionally. Ialso did not realize the degree to which acnehad altered the perception she had of herselfand the manner in which she conducted herlife. I am truly pleased that I was able to notonly resolve Nicola’s acne but also significantlyimprove her self-esteem and outlook towardlife.
ACKNOWLEDGEMENTS
We thank the participant of the study.
Funding:. The authors are fully responsiblefor all content and editorial decisions andreceived no financial support or other form ofcompensation related to the development ofthis manuscript. No funding was received forpublication of this article.
Fig. 5 Comparison of frontal views of the face prior to(a) and following (b) treatment with isotretinoin for5 months. There has been significant improvement of her
acne with resolution of nearly all inflammatory andcomedonal lesions. Her malar scars are less erythematousand less prominent
Dermatol Ther (Heidelb) (2020) 10:1–14 11

Authorship. All named authors meet theInternational Committee of Medical JournalEditors (ICMJE) criteria for authorship of thismanuscript, take responsibility for the integrityof the work as a whole, and have given finalapproval for the version to be published. Theopinions expressed in the manuscript are thoseof the authors.
Disclosures. Nicola I. Espinosa has nothingto disclose. Philip R. Cohen is a member of thejournal’s Editorial Board.
Compliance with Ethics Guidelines. In-formed consent for publication of the imageswithin the article was obtained from thepatient.
Peer Review. Please note, contrary to thejournal’s standard single-blind peer review pro-cess, as a commentary this article underwentreview by a member of the journal’s EditorialBoard.
Data Availability. Data sharing is notapplicable to this article as no data sets weregenerated or analyzed during the current study.
Open Access. This article is distributedunder the terms of the Creative CommonsAttribution-NonCommercial 4.0 InternationalLicense (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommer-cial use, distribution, and reproduction in anymedium, provided you give appropriate creditto the original author(s) and the source, providea link to the Creative Commons license, andindicate if changes were made.
REFERENCES
1. Zaenglein AI, Pathy AI, Schlosser BJ, Alikhan A,Baldwin HE, Berson DS, Bowe WP, Graber EM,Harper JC, Kang S, Keri JE, Leyden JJ, Reynolds RV,Silverberg NB, Gold LFS, Tollefson MM, Weiss JS,Dolan NC, Sagan AA, Stern M, Boyer KM, BhushanR. Guidelines of care for the management of acnevulgaris. J Am Acad Dermatol. 2016;74(6):945–73.
2. Zaenglein AL. Acne vulgaris. N Engl J Med.2018;379(14):1343–52.
3. Mwanthi M, Zaenglein AL. Update in the manage-ment of acne in adolescence. Curr Opin Pediatr.2018;30(4):492–8.
4. Thiboutot DM, Dreno B, Abanmi A, Alexis AF,Araviiskaia E, Cabal MIB, Bettoli V, Casintahan F,Chow S, da Costa A, Ouazzani TE, Goh C-L, GollnickHPM, Gomez M, Hayashi N, Herane MI, HoneymanJ, Kang S, Kemeny L, Kubba R, Lambert J, Layton AM,Leyden JJ, Lopez-Estebaranz JL, Noppakun N, Och-sendorf F, Oprica C, Orozco B, Perez M, Piquero-Martin J, See J-A, Auh DH, Tan J, Lozada VT, TroielliP, Xiang LF. Practical management of acne for clini-cians: an international consensus from the globalalliance to improve outcomes in acne. J Am AcadDermatol. 2018;78(2 Suppl):S1–23.
5. Kircik LH. Advances in the understanding of thepathogenesis of inflammatory acne. J Drugs Der-matol. 2016;15(1 Suppl 1):s7–10.
6. Zeichner JA. Inflammatory acne treatment: reviewof current and new topical therapeutic options.J Drugs Dermatol. 2016;15(1 Suppl 1):s11–6.
7. Cordain L, Lindeberg S, HurtadoM, Hill K, Eaton SB,Brand-Miller J. Acne vulgaris: a disease of Westerncivilization. Arch Dermatol. 2002;138(12):1584–90.
8. Adebamowo CA, Spiegelman D, Berkey CS, DanbyFW, Rockett HH, Colditz GA, Willett WC, HolmesMD. Milk consumption and acne in teenage boys.J Am Acad Dermatol. 2008;58(5):787–93.
9. Melnik BC. Linking diet to acne metabolomics,inflammation, and comedogenesis: an update. ClinCosmet Investig Dermatol. 2015;8:371–88.
10. LaRosa CL, Quach KA, Koons K, Kunselman AR,Zhu J, Thiboutot DM, Zaenglein AL. Consumptionof dairy in teenagers with and without acne. J AmAcad Dermatol. 2016;75(2):318–22.
11. Burris J, Rietkerk W, Shikany JM, Woolf K. Differ-ences in dietary glycemic load and hormones inNew York City adults with no and moderate/severeacne. J Acad Nutr Diet. 2017;117(9):1375–83.
12. Oon HH, Wong S-N, Wee DC, Cheong WK, GohCL, Tan HH. Acne management guidelines by thedermatological society of Singapore. J Clin AesthetDermatol. 2019;12(7):34–50.
13. Silverberg NB. Whey protein precipitates moderateto severe acne flares in 5 teenaged athletes. Cutis.2012;90(2):70–2.
14. Cengiz FP, Cevirgen Cemil B, Emiroglu N, GulselBahali A, Onsun N. Acne located on the trunk,whey protein supplementation: is there any asso-ciation? Health Promot Perspect. 2017;7(2):106–8.
12 Dermatol Ther (Heidelb) (2020) 10:1–14

15. Del Rosso JQ, Pillai R, Moore R. Absence of degra-dation of tretinoin when benzoyl peroxide is com-bined with an optimized formulation of tretinoingel (0.05%). J Clin Aesthet Dermatol.2010;3(10):26–8.
16. Rice C, Thompson J. Selecting and monitoringhormonal contraceptives: an overview of availableproducts. US Pharm. 2006;6:62–70.
17. Thiede RM, Rastogi S, Nardone B, Sadowsky LM,Rangel SM, West DP, Schlosser BJ. Hyperkalemia inwomen with acne exposed to oral spironolactone: aretrospective study from the RADAR (Research onAdverse Drug events And Reports) program. Int JWoman’s Dermatol. 2019;5(3):155–7.
18. Plovanich M, Weng QY, Mostaghimi A. Low use-fulness of potassium monitoring among healthyyoung women taking spironolactone for acne.JAMA Dermatol. 2015;151(9):941–4.
19. Isvy-Joubert A, Nguyen JM, Gaultier A, Saint-JeanM, Le Moigne M, Boisrobert E, Khammari A, DrenoB. Adult female acne treated with spironolactone: aretrospective data review of 70 cases. Eur J Derma-tol. 2017;27(4):393–8.
20. Charny JW, Choi JK, James WD. Spironolactone forthe treatment of acne in women, a retrospectivestudy of 110 patients. Int J Womens Dermatol.2017;3(2):111–5.
21. Grandhi R, Alikhan A. Spironolactone for treatmentof acne: a 4-year retrospective study. Dermatology.2017;233(2–3):141–4.
22. Vaughn AR, Branum A, Sivamani RK. Effects ofturmeric (Curcuma longa) on skin health: a system-atic review of the clinical evidence. Phytother Res.2016;30(8):1243–64.
23. Panahi Y, Fazlolahzadeh O, Atkin SL, Majeed M,Butler AE, Johnston TP, Sahebkar A. Evidence ofcurcumin and curcumin analogue effects in skindiseases: a narrative review. J Cell Physiol.2019;234(2):1165–78.
24. Yang MY, Chang KC, Chen LY, Hu A. Low-doseblue light irradiation enhances the antimicrobialactivities of curcumin against Propionibacteriumacnes. J Photochem Photobiol B. 2018;189:21–8.
25. Handog EB, Datuin MS, Singzon IA. Chemical peelsfor acne and acne scars in Asians: evidence basedreview. J Cutan Aesthet Surg. 2012;5(4):239–46.
26. Kaminaka C, Uede M, Matsunaka H, Furukawa F,Yamomoto Y. Clinical evaluation of glycolic acidchemical peeling in patients with acne vulgaris: arandomized, double-blind, placebo-controlled,
split-face comparative study. Dermatol Surg.2014;40(3):314–22.
27. Atorzi L, Brundu MA, Orru A, Biggio P. Glycolic acidpeeling in the treatment of acne. J Eur Acad Der-matol Venereol. 1999;12(2):119–22.
28. Levesque A, Hamzavi I, Seite S, Rougier A, Bisson-nette R. Randomized trial comparing a chemicalpeel containing a lipophilic hydroxy acid derivativeof salicylic acid with a salicylic acid peel in subjectswith comedonal acne. J Cosmet Dermatol.2011;10(3):174–8.
29. Mei X, Shi W, Piao Y. Effectiveness of photody-namic therapy with topical 5-aminolevulinic acidand intense pulsed light in Chinese acne vulgarispatients. Photodermatol Photoimmunol Pho-tomed. 2013;29(2):90–6.
30. Kwon HH, Lee JB, Yoon JY, Park SY, Ryu HH, ParkBM, Kim YJ, Suh DH. The clinical and histologicaleffect of home-use, combination blue-red LEDphototherapy for mild-to-moderate acne vulgaris inKorean patients: a double-blind, randomized con-trolled trial. Br J Dermatol. 2013;168(5):1088–94.
31. Alexiades M. Laser and light-based treatments ofacne and acne scarring. Clin Dermatol.2017;35(2):183–9.
32. Wiznia LE, Stevenson ML, Nagler AR. Laser treat-ments of active acne. Lasers Med Sci.2017;32(7):1647–58.
33. Rai R, Natarajan K. Laser and light based treatmentsof acne. Indian J Dermatol Venereol Leprol.2013;79(3):300–9.
34. Bauer LB, Ornelas JN, Elston DM, Alikhan A. Iso-tretinoin: controversies, facts, and recommenda-tions. Expert Rev Clin Pharmacol.2016;9(11):1435–42.
35. Vallerand IA, Lewinson RT, Farris MS, Sibley CD,Ramien ML, Bulloch AGM, Patten SB. Efficacy andadverse events of oral isotretinoin for acne: a sys-tematic review. Br J Dermatol. 2018;178(1):76–85.
36. Lee YH, Scharnitz TP, Muscat J, Chen A, Gupta-Elera G, Kirby JS. Laboratory monitoring duringisotretinoin therapy for acne: a systematic reviewand meta-analysis. JAMA Dermatol.2016;152(1):35–44.
37. Hansen TJ, Lucking S, Miller JJ, Kirby JS, ThiboutotDM, Zaenglein AL. Standardized laboratory moni-toring with use of isotretinoin in acne. J Am AcadDermatol. 2016;75(2):323–8.
38. Webster GF, Webster TG, Grimes LR. Laboratorytests in patients treated with isotretinoin:
Dermatol Ther (Heidelb) (2020) 10:1–14 13

occurrence of liver and muscle abnormalities andfailures of AST and ALT to predict liver abnormality.Dermatol Online J. 2017;23(5):1–3.
39. Kim HJ, Lee SM, Lee JS, Lee SY, Chung EH, Cho MK,Lee SH, Kim JE. Homocysteine, folic acid, andvitamin B12 levels in patients on isotretinointherapy for acne vulgaris: a meta-analysis. J CosmetDermatol. 2019. https://doi.org/10.1111/jocd.13059.
40. Zachariae H. Delayed wound healing and keloidformation following argon laser treatment or der-mabrasion during isotretinoin treatment. Br J Der-matol. 1988;118(5):703–6.
41. Guadanhim LR, Goncalves RG, Bagatin E. Obser-vational retrospective study evaluating the effectsof oral isotretinoin in keloids and hypertrophicscars. Int J Dermatol. 2016;55(11):1255–8.
42. Sharma J, Thiboutot DM, Zaenglein AL. The effectsof isotretinoin on wisdom tooth extraction. J AmAcad Dermatol. 2012;67(4):794–5.
43. Spring LK, Krakowski AC, Alam M, Bhatia A, BrauerJ, Cohen J, Del Rosso JQ, Diaz L, Dover J, Eichen-field LF, Gurtner GC, Hanke CW, Jahnke MN, KellyKM, Khetarpal S, Kinney MA, Levy ML, Leyden J,Longaker MT, Munavalli GS, Ozog DM, Prather H,Shumaker PR, Tanzi E, Torres A, Velez MW, Wald-man AB, Yan AC, Zaenglein AL. Isotretinoin andtiming of procedural interventions: a systematicreview with consensus recommendations. JAMADermatol. 2017;153(8):802–9.
44. Waldman A, Bolotin D, Arndt KA, Dover JS,Geronemus RG, Chapas A, Iyengar S, Kilmer SL,Krakowski AC, Lawrence N, Prather HB, Rohrer TE,Schlosser BJ, Kim JYS, Shumajker PR, Spring LK,Alam M. ASDS guidelines task force consensus rec-ommendations regarding the safety of lasers, der-mabrasion, chemical peels, energy devices, and skinsurgery during and after isotretinoin use. DermatolSurg. 2017;43(10):1249–62.
45. Mahadevappa OH, Mysore V, Viswanath V, Thu-rakkal S, Majid I, Talwar S, Aurgangabadkar SJ,Chatterjee M, Bhat MR, Barua S, Ganjoo A. Surgicaloutcomes in patients taking concomitant or recentintake of oral isotretinoin: a multicentric study-ISO-AIMS study. J Cutan Aesthet Surg.2016;9(2):106–14.
46. Bower KS, Woreta F. Update on contraindicationsfor laser-assisted in situ keratomileusis and pho-torefractive keratectomy. Curr Opin Ophthalmol.2014;25(4):251–7.
47. Miles S, McGlathery W, Abernathie B. The impor-tance of screening for laser-assisted in situ ker-atomileusis operation (LASIK) before prescribingisotretinoin. J Am Acad Dermatol.2006;54(1):180–1.
48. Ortega-Usobiaga J, Llovet-Osuna F, Djodeyre MR,Bilbao-Calabuig R, Gonzalez-Lopez F, Llovet-RausellA, Druchkiv V. Outcomes of laser in situ ker-atomileusis and photorefractive keratectomy inpatients taking isotretinoin. Am J Ophthalmol.2018;192:98–103.
14 Dermatol Ther (Heidelb) (2020) 10:1–14