ACLS Updates 2015 - Your Heartsaudi-heart.com/.../07/ACLS-ACS-Updates-2015-final.pdf · ACLS/ACS...
Transcript of ACLS Updates 2015 - Your Heartsaudi-heart.com/.../07/ACLS-ACS-Updates-2015-final.pdf · ACLS/ACS...

ACLS/ACS Updates 2015 Advanced Cardiovascular Life Support
by:
Fareed Al Nozha, JBIM, ABIM, FKFSH&RC(Cardiology)
Consultant Cardiologist Faculty, National CPR Committee, ACLS Program Head, SHA
Dr Abdulhalim J. kinsara FRCP, FACC, FESC
Ass Professor
Head of Adult cardiology

INTRODUCTION :
(ACLS) guidelines have evolved over the
past several decades based on a combination
of scientific evidence of variable strength
and expert consensus. The (AHA) developed
the most recent ACLS guidelines in 2010
using the comprehensive review of
resuscitation literature performed by the
(ILCOR), and these were updated in 2015
2 2015 Update ACLS/ACS

Emphasis on Chest Compressions
Untrained lay rescuers should provide compression-only
(Hands-Only) CPR, with or without dispatcher guidance,
for adult victims of cardiac arrest. The rescuer should
continue compression-only CPR until the arrival of an
AED or rescuers with additional training. All lay rescuers
should, at a minimum, provide chest compressions for
victims of cardiac arrest. In addition, if the trained lay
rescuer is able to perform rescue breaths, he or she should
add rescue breaths in a ratio of 30 compressions to 2
breaths. The rescuer should continue CPR until an AED
arrives and is ready for use, EMS providers take over care
of the victim, or the victim starts to move.

Chest Compression Rate
In adult victims of cardiac arrest, it is reasonable for
rescuers to perform chest compressions at a rate of 100
to 120/min.

Chest Compression Depth
2015 (New): During manual CPR, rescuers should perform
chest compressions to a depth of at least 2 inches (5 cm.) for
an average adult, while avoiding excessive chest
compressions depths (greater than 2.4 inches [6 cm.])

Use of Social Media to Summon Rescuers
2015 (New): It may be reasonable for communities to
incorporate social media technologies that summon
rescuers who are in close proximity to a victim of
suspected OHCA and are willing and able to perform CPR
Community Lay Rescuer AED Programs
2015 (New): It is recommended that PAD programs for
patients with OHCA be implemented in public locations
where there is a relatively high likelihood of witnessed
cardiac arrest (eg. airports, casinos, sports facilities).

When supplementary oxygen is available, it
may be reasonable to use the maximal
feasible inspired oxygen concentration during
CPR.
Evidence for possible detrimental effects of
hyperoxia in the immediate post-cardiac
arrest period should not be extrapolated to
CPR context

Post-CPR:
When resources are available to titrate FiO2,
it is reasonable to decrease FiO2 when SaO2
is 100% provided the SaO2 is maintained at
94% or greater.

Standard-dose epinephrine (1 mg every 3 to
5 minutes) may be reasonable for patients
in cardiac arrest (Class IIb, LOE B-R).
High-dose epinephrine is not recommended
for routine use in cardiac arrest (Class III:
No Benefit, LOE B-R).

For initial non-shockable rhythm: It may be reasonable
to administer adrenaline as soon as feasible after the
onset of cardiac arrest (Class Iib, LOE C-LD).
For initial shockable rhyhtm: There is insufficient
evidence to make a recommendation as to the optimal
timing of adrenaline, particularly in relation to
defibrillation

Amiodarone may be considered for VF/pVT that is
unresponsive to CPR, defibrillation, and a
vasopressor therapy (Class IIb, LOE B-R).
Lidocaine may be considered as an alternative to
amiodarone for VF/pVT that is unresponsive to
CPR, defibrillation, and vasopressor therapy (Class
IIb, LOE C-LD).

“…none (of the antiarrhythmics) have yet
been proven to increase long term survival or
survival with good neurologic outcome. Thus
establishing vascular access to enable drug
administration should not compromise the
quality of CPR or timely defibrillation, which
are known to improve survival.”

Ultrasound (cardiac or noncardiac)
may be considered during the management of
cardiac arrest, although its usefulness has
not been well established (Class IIb, LOE CEO).
If a qualified sonographer is present and
use of ultrasound does not interfere with the
standard cardiac arrest treatment protocol,
then ultrasound may be considered as an
adjunct to standard patient evaluation (Class
IIb, LOE C-EO).

14

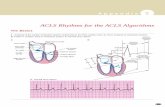
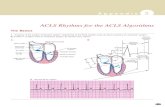
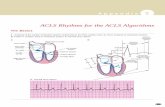
Cardiopulmonary resuscitation (CPR) and
early defibrillation for treatable arrhythmias
remain the cornerstones of basic and
advanced cardiac life support (ACLS).
Excellent chest compressions without
interruption are the key to successful CPR
15 2015 Update ACLS/ACS
ACLS Updates 2015

The performance of teams providing ACLS
improves when there is a single designated
leader who asks for and accepts helpful
suggestions from members of the team, and
when the team practices clear, closed-loop
communication.
16 2015 Update ACLS/ACS
ACLS Updates 2015

17 2015 Update ACLS/ACS

Summary
of Key Issues and Major Changes
The combined use of vasopressin and epinephrine
offers no advantage to using standard-dose
epinephrine in cardiac arrest. Also, vasopressin
does not offer an advantage over the use of
epinephrine alone. Therefore, to simplify the
algorithm, vasopressin has been removed from
the ACLS Algorithm–2015 Update.
18 2015 Update ACLS/ACS

Low ETCO2 in intubated patients after 20 minutes
of CPR is associated with a very low likelihood of
resuscitation. While this parameter should not be
used in isolation for decision making, providers
may consider low ETCO2 after 20 minutes of CPR
in combination with other factors to help determine
when to terminate resuscitation.
Summary
of Key Issues and Major Changes
19 2015 Update ACLS/ACS

Steroids may provide some benefit when bundled
with vasopressin and epinephrine in treating IHCA.
While routine use is not recommended pending
follow-up studies, it would be reasonable for a
provider to administer the bundle for IHCA.
Summary
of Key Issues and Major Changes
20 2015 Update ACLS/ACS

When rapidly implemented, ECPR can prolong
viability, as it may provide time to treat
potentially reversible conditions or arrange for
cardiac transplantation for patients who are not
resuscitated by conventional CPR.
Summary
of Key Issues and Major Changes
21 2015 Update ACLS/ACS

In cardiac arrest patients with nonshockable rhythm
and who are otherwise receiving epinephrine, the
early provision of epinephrine is suggested.
Summary
of Key Issues and Major Changes
22 2015 Update ACLS/ACS

Studies about the use of lidocaine after ROSC are
conflicting, and routine lidocaine use is not
recommended.
However, the initiation or continuation of lidocaine
may be considered immediately after ROSC from
VF/pVT cardiac arrest.
Summary
of Key Issues and Major Changes
23 2015 Update ACLS/ACS

One observational study suggests that ß- blocker
use after cardiac arrest may be associated with
better outcomes than when ß- blockers are not
used.
Although this observational study is not strong
enough evidence to recommend routine use, the
initiation or continuation of an oral or intravenous
(IV) ß-blocker may be considered early after
hospitalization from cardiac arrest due to VF/p VT.
Summary
of Key Issues and Major Changes
24 2015 Update ACLS/ACS

2015 Update ACLS/ACS 25
Targeted temperature management
Upgraded the strength of recommendation to the highest
level for using targeted temperature management in all
comatose patients who achieve ROSC regardless of the
presenting rhythm or whether the arrest occurred in the
out-of-hospital or hospital environment.
The AHA also expanded the targeted temperature range
to 32 C to 36 C.

2015 Update ACLS/ACS 26
Targeted temperature management
New recommendation is for EMS to no longer initiate the
cooling process with chilled saline infusion.
Five randomized controlled trials using chilled IV fluids
following ROSC , one trial using chilled IV fluids during
the resuscitation attempt , and one trial using intra-nasal
cooling could find no survival or neurological recovery
benefits offered by prehospital cooling.
In one of the chilled saline trials, initiating cooling in the
field actually increased the risk of re-arrest and post-
resuscitation pulmonary edema

Acute Coronary Syndromes 2015
Recommendations will be limited to the prehospital
and emergency department phases of care.
In-hospital care is addressed by guidelines for the
management of myocardial infarction published
jointly by the AHA and the American College of
Cardiology Foundation.
27 2015 Update ACLS/ACS

2015 Update ACLS/ACS 28
Prehospital 12-lead ECG should be acquired early for
patients with possible ACS (Class I, LOE B-NR).
Prehospital notification of the receiving hospital (if
fibrinolysis is the likely reperfusion strategy) and/or
prehospital activation of the catheterization laboratory
should occur for all patients with a recognized STEMI
on prehospital ECG (Class I, LOE B-NR).

2015 Update ACLS/ACS 29
Because of high false-negative rates, we recommend
that computer-assisted ECG interpretation not be used
as a sole means to diagnose STEMI (Class III: Harm,
LOE B-NR).
We recommend that computer-assisted ECG
interpretation may be used in conjunction with
physician or trained provider interpretation to
recognize STEMI (Class IIb, LOE C-LD).

2015 Update ACLS/ACS 30
While transmission of the prehospital ECG to the ED
physician may improve positive predictive value (PPV) and
therapeutic decision-making regarding adult patients with
suspected STEMI, if transmission is not performed, it may
be reasonable for trained nonphysician ECG interpretation
to be used as the basis for decision-making, including
activation of the catheterization laboratory, administration
of fibrinolysis, and selection of destination hospital (Class
IIa, LOE B-NR).

2015 Update ACLS/ACS 31
We recommend against using hs-cTnT and cTnI alone
measured at 0 and 2 hours (without performing clinical
risk stratification) to identify patients at low risk for ACS
(Class III: Harm, LOE B-NR).
We recommend that hs-cTnI measurements that are less
than the 99th percentile, measured at 0 and 2 hours, may
be used together with low-risk stratification (TIMI score
of 0 or 1 or low risk per Vancouver rule) to predict a less
than 1% chance of 30-day MACE (Class IIa, LOE B-
NR).

2015 Update ACLS/ACS 32
We recommend that negative cTnI or cTnT
measurements at 0 and between 3 and 6 hours may be
used together with very low-risk stratification (TIMI
score of 0, low-risk score per Vancouver rule, North
American Chest Pain score of 0 and age less than 50
years, or low-risk HEART score) to predict a less than
1% chance of 30-day MACE (Class IIa, LOE B-NR).

Acute Coronary Syndrome-Updated 2015
2015 Update ACLS/ACS 33

2015 Update ACLS/ACS 34
Acute Coronary Syndrome-Updated 2015

Summary of Key Issues and Major Changes
Prehospital ECG acquisition and interpretation
Choosing a reperfusion strategy when prehospital fibrinolysis is available
Choosing a reperfusion strategy at a non–PCI-capable hospital
Troponin to identify patients who can be safely discharged from the emergency department
Interventions that may or may not be of benefit if given before hospital arrival
35 2015 Update ACLS/ACS
Acute Coronary Syndromes 2015