Cultivate Health Rod Carter, Pharm.D. Leticia Shea, Pharm.D.
ACLS Pharmacotherapy Update Jessica Schwenk, Pharm.D. September 14, 2013.
-
Upload
dangelo-dimmer -
Category
Documents
-
view
217 -
download
0
Transcript of ACLS Pharmacotherapy Update Jessica Schwenk, Pharm.D. September 14, 2013.

ACLS Pharmacotherapy Update
Jessica Schwenk, Pharm.D.September 14, 2013

Introduction
ObjectivesACLS Guideline Overview
Access for Medications in ACLS

Objectives
• Identify and describe medications used in Advanced Cardiovascular Life Support (ACLS)
• Understand indications, mechanism of action, dose, administration, and precautions for ACLS medications
• Recognize place in therapy for medications in updated ACLS algorithms

ACLS Guidelines
• Developed by American Heart Association– Released every 5 years– Published in Circulation
• Most Recent– 2010 Guidelines for advanced cardiac life support
• Used comprehensive review of resuscitation literature performed by the International Liaison Committee on Resuscitation (ILCOR)


ACLS Guidelines
• First priority– High quality CPR– Early defibrillation
• Second priority– Medication administration– Advanced airway
• For drug administration or ventilation

Access for Medications in ACLS
• Intravenous (IV) Route– Preferred route
• Central line not required; can interrupt CPR
– Medications take 1-2 minutes to reach central circulation
• Give medications as IV bolus, flush with 20 mL fluid

Access for Medications in ACLS
• Intraosseous (IO) Route– Secondary method– Safe and effective for administering medications,
fluids, and blood as well as drawing blood– ALL medications that can be given IV can be given
IO• Administer medications and flush with at least 20 mL
fluid (as with IV administration)

Access for Medications in ACLS
• Endotracheal (ET) Route– Not preferred; last resort– Medication doses are 2-2.5 times IV/IO doses
• Optimal dosing not known
– Medications that can be given ET: epinephrine, vasopressin, lidocaine (atropine, naloxone)
• Dilute with 5-10 mL SW/NS, administer into ET tube, follow with several positive pressure breaths

ACLS Medications
Adult cardiac arrest algorithm





Adult cardiac arrest algorithm
• Medications:– Ventricular fibrillation or ventricular tachycardia
(VF/VT)• Vasopressors: epinephrine, vasopressin• Antiarrhythmics: amiodarone
– Not on algorithm: lidocaine, magnesium
– Asystole/Pulseless electrical activity (PEA)• Vasopressors: epinephrine, vasopressin

Adult cardiac arrest algorithm
• Vasopressor medications– Include: epinephrine, norepinephrine, vasopressin– Goal: increase coronary and cerebral perfusion– Effects:
• Increase systemic arteriolar vasoconstriction• Maintain vascular tone• Shunt blood to heart and brain
– ONLY medications shown to improve ROSC and short term survival

Adult cardiac arrest algorithm
• Epinephrine (Adrenaline)– MOA: ɑ- and β-receptor agonist
• ɑ-receptor stimulation restores circulation• β-receptor stimulation
– May lower defibrillation threshold– Increases myocardial oxygen demand

Adult cardiac arrest algorithm
• Epinephrine – Dose and Administration– VF, PVT, asystole, PEA
• IV/IO: 1 mg every 3-5 minutes– Concentration 0.1mg/ml (1:10,000 or 1 mg/10ml)– Flush with 20 ml NS (central line preferred)
• ET: 2-2.5 mg every 3-5 minutes– Dilute in 5-10 ml SW or NS (use epi 1 mg/ml or 1:1,000)

Vasopressors
• Vasopressin (antidiuretic hormone)– MOA: acts on V1 receptor (among others) to
cause vasoconstriction• Increases blood pressure and systemic vascular
resistance
– Benefits over epinephrine• Not inhibited by metabolic acidosis• No β-receptor activity
– Vasopressin vs. epinephrine for cardiac arrest?• No significant difference in ROSC when given 2 doses

Vasopressors
• Vasopressin– Dose and Administration– VF, PVT, asystole, PEA
• IV/IO: 40 units one time (to replace 1st or 2nd dose of epinephrine every 3-5 minutes)
– 40 Units/2 ml (2 vials of 20 units/ml)– Flush with 20 ml NS
• ET: 80-100 units one time (to replace 1st or 2nd dose of epinephrine every 3-5 minutes)
– Dilute in 5-10 ml SW or NS

Adult cardiac arrest algorithm
• Antiarrhythmic medications for cardiac arrest (pulseless VF/VT) include:– Amiodarone
• Not on algorithm: lidocaine, magnesium
– Goal: increase the fibrillation threshold• Prevent development or recurrence of VF and PVT

Adult cardiac arrest algorithm
• Amiodarone (Cordarone, Pacerone)– MOA: Class III antiarrhythmic (potassium channel
blocker)• Acutely: inhibits α- and β-adrenergic stimulation, blocks
calcium channels
– Side effects (acute):• Hypotension, fever, elevated LFTs, confusion, nausea,
thrombocytopenia

Adult cardiac arrest algorithm
• Amiodarone– Dose and administration– Pulseless VF/VT
• 300 mg bolus IV/IO, follow with 150 mg in 3-5 minutes• Give IV/IO push. If possible dilute in 20-30 ml D5W
– Amiodarone vial concentration is 50 mg/ml– Flush with 20 ml
• Central line preferred• Incompatible with sodium bicarbonate

Other antiarrhythmics
• Lidocaine (NOT on algorithm for VF/PVT)– MOA: Class Ib antiarrhythmic, sodium channel
blocker– 2010 Guidelines: “There is inadequate evidence to
support or refute the use of lidocaine…” in refractory VF/VT
• Amiodarone beneficial over lidocaine for survival-to-admission
• May be considered if amiodarone is not available

Other Antiarrhythmics
• Lidocaine (NOT on algorithm for VF/PVT)– Dose and Administration
• IV/IO: 1-1.5 mg/kg, then 0.5-0.75 mg/kg every 5 to 10 minutes
– Lidocaine 100 mg/5 ml syringe (20 mg/ml)
• ET: 2-3 mg/kg in 10 ml NS
– Dose and Administration• Monitoring: discontinue if signs of toxicity
– Sedations, seizures, confusion

Other Antiarrhythmics
• Magnesium (NOT on algorithm for VF/PVT)– Use: suspected hypomagnesemia, Torsades de
Pointes– Dose and Administration (cardiac arrest)
• Magnesium 1-2 g IV/IO – Magnesium sulfate 50% vials (1 g/2 mL or 0.5 g/ml)
• Dilute to 10 ml (NS)• Administer over 5-20 minutes
– Monitor: • Hypotension, respiratory and CNS depression

ACLS Medications
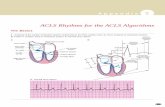
Adult bradycardia algorithm (with pulse)


Adult bradycardia algorithm (with pulse)

Adult bradycardia algorithm (with pulse)

Adult bradycardia algorithm (with pulse)
• Medications– Atropine– Dopamine– Epinephrine

Adult bradycardia algorithm (with pulse)
• Atropine– MOA: anticholinergic agent, blocks acetylcholine
at M2-receptors of heart – Dose and administration
• 0.5 mg IV/IO bolus, repeat every 3-5 minutes• Max 3 mg total dose• Atropine syringe 1 mg/10 ml (0.1 mg/ml)
– Contraindications/Precautions• Evidence of a high degree (second degree [Mobitz] type
II or third degree) atrioventricular (AV) block • May be harmful in cardiac ischemia

Adult bradycardia algorithm (with pulse)
• Dopamine– MOA: adrenergic and dopaminergic receptor
agonist, stimulation of β1-recptors increases HR– Dose and Administration
• 2-10 mcg/kg/min IV/IO infusion (up to 20 mcg/kg/min)• Titrate to response, increase by 5 mcg/kg/min every
10-30 minutes as needed• Premade bags are 200 mg/250 ml D5W (800 mcg/ml)• Central line preferred• Incompatible with sodium bicarbonate

Adult bradycardia algorithm (with pulse)
• Epinephrine– MOA: adrenergic agonist, stimulation of β1-
recptors increases HR– Dose and Administration
• 2-10 mcg/min IV/IO infusion• Titrate to response• Standard drip 4 mg/250 ml NS or D5W (16 mcg/ml)• Central line preferred• Incompatible with sodium bicarbonate

ACLS Medications
Adult tachycardia algorithm (with pulse)



Adult tachycardia algorithm (with pulse)
• Medications– Regular narrow complex
• Adenosine• Calcium channel blockers or beta blocker
– Irregular narrow complex• Calcium channel blocker or beta blocker• Amiodarone

Adult tachycardia algorithm (with pulse)
• Medications– Regular wide complex
• Adenosine• Calcium channel blockers or beta blocker• Antiarrhythmics: procainamide, amiodarone, sotolol
– Irregular wide complex• Antiarrhythmics: procainamide, amiodarone, sotolol• Polymorphic VT, Torsades de Pointes: magnesium

Adult tachycardia algorithm (with pulse)
• Adenosine– Dose and Administration
• 6-12 mg IV into large proximal vein—fast• Flush with 20 mL immediately, elevate limb
– Extremely short half life
• May repeat 2nd and 3rd dose of 12 mg• Larger doses (18 mg IV)
– Theophylline or theobromine, caffeine;
• Smaller doses (3mg IV) – Dipyridamole or carbamazepine, transplanted hearts, or into a
central vein.

Adult tachycardia algorithm (with pulse)
• Adenosine– Side effects
• Chest discomfort, dyspnea, and flushing• Warn patient!
– Monitoring• Continuous ECG recording during administration• If adenosine fails to convert SVT, watch for atrial flutter
or a non-reentrant SVT

Adult tachycardia algorithm (with pulse)
• Diltiazem– First choice for acute a-fib with RVR– Dose and administration
• Bolus 15-20 mg IV push over 2 minutes (0.25 mg/kg)• Repeat with 20-25 mg IV push over 2 minutes after 15
minutes (0.35 mg/kg)– Diltiazem vials 5 mg/ml
• IV infusion 5-10 mg/hour, titrate up by 5 mg/hour as needed
– Diltiazem infusion 1 mg/ml
– Monitor: ECG, blood pressure

Adult tachycardia algorithm (with pulse)
• Verapamil– Dose and administration
• 2.5-5 mg IV push over 2 minutes• Repeat with 5-10 mg over 2 minutes after 15-30
minutes– Maximum total dose 20 mg
– Monitor: ECG, blood pressure

Adult tachycardia algorithm (with pulse)
• Metoprolol– Dose and administration
• 5 mg IV push over 1 minute for 3 doses every 2-5 minutes
– Monitor: ECG, blood pressure

Adult tachycardia algorithm (with pulse)
• Atenolol– Dose and administration
• 5 mg slow IV push over 5 minutes• Repeat in 10 minutes
– Monitor: ECG, blood pressure

Adult tachycardia algorithm (with pulse)
• Esmolol– Dose and administration
• 500 mcg/kg IV push over 1 minute (may repeat)– 10 mg/ml
• IV infusion 50 mcg/kg/minute for 4 minutes• Titrate by 50 mcg/kg/minute at least every 4 minutes
– Max 200 mcg/kg/min
• Repeat in 10 minutes
– Monitor: ECG, blood pressure

Adult tachycardia algorithm (with pulse)
• Procainamide– Class 1a antiarrhythmic (sodium channel blocker)– Dose and administration
• IV infusion 20 mg/min (20 mg/ml in D5W)– Alternate dosing: 100 mg IV push over 2 min every 5 min
• Continue until the arrhythmia is suppressed, or:– Hypotension– QRS widens 50% beyond baseline– Max dose of 17 mg/kg
• Maintenance infusion 1-3 mg/min (2 mg/ml in D5W)
– Monitor: ECG, QT interval, pulse, blood pressure• ADR: dysrhythmia, systemic lupus erythematosus (up to
30%), hematologic effects, hepatotoxicity

Adult tachycardia algorithm (with pulse)
• Amiodarone– Dose and administration
• 150 mg IV over 10 min, repeat for recurrence– Mix in 100 ml D5W (1.5 mg/ml)
• Follow IV infusion 1 mg/min for 6 hours, then 0.5 mg/min 0.5 mg/min IV for 18 hours
– Infusion 1.5 mg/ml
• Max 2.2 g/24 hr• Central line preferred• Use in-line filter• Incompatible with sodium bicarbonate
– Monitor: ECG, pulse, blood pressure• ADR: hyper/hypthyroidism, lupus, vision impairment,
renal/liver impairment, pulmonary fibrosis

Adult tachycardia algorithm (with pulse)
• Magnesium– Torsades de Pointes– Dose and Administration
• Magnesium 1-2 g IV– Magnesium sulfate 50% vials (1 g/2 mL or 0.5 g/ml)
• Dilute to 10 ml (NS)• Administer over 5-20 minutes• Maintenance infusion 0.5-1 g/hour
– To correct deficiency
– Monitor: • hypotension, respiratory and CNS depression

Extravasation
• Hyaluronidase (150 units/ml)– Inject 0.2 ml subq around the area of the
extravasation (5 injections)• Amiodarone (hot compress)• Calcium (cold compress)
• Phentolamine (5 mg with 9 ml NS)– Inject small amount into blanched area, additional
as needed• Epineprine (norepinephrine, phenylephrine)• Dopamine• Vasopressin

What else is in the crash cart?

References• ACLS Provider Manual Supplementary Material (2012). American Heart Association
Web site. Available at: http://www.hearttraining.com/media/documents/ACLS. Accessed August 13, 2013.
• Barletta, JF. Cardiopulmonary resuscitation. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, editors. Pharmacotherapy. A Pathophysiologic Approach. 6th ed. New York (NY): McGraw Hill;2005:171-184.
• Bauman JL, Schoen MD. Arrhythmias. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, editors. Pharmacotherapy. A Pathophysiologic Approach. 6th ed. New York (NY): McGraw Hill;2005:321-356.
• DRUGDEX® System [Internet database]. Greenwood Village, Colo: Thomson Healthcare. Updated periodically.
• Hazinski MF, Nolan JP, Billi JE, et al. 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122:e1-330.
• Lacy CF, Armstrong LL, Goldman MP, Lance LL. Lexi-Comp’s Drug Information Handbook. 17th ed. Hudson (OH): Lexi-Comp;2008.
• Ponzer CN, Advanced cardiac life support (ACLS) in adults. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2013.