ACLS 2005 Update
-
Upload
snakeeyes-nongan -
Category
Documents
-
view
36 -
download
0
description
Transcript of ACLS 2005 Update
Overview
• Goal = review major changes to CPR, ALS, electrical therapies, cardiac arrest, arrythmia algorithms, post – resusc care
• Briefly review some Landmark papers.• AEDs, ACS, CVA, toxicology and other special
resusc situations not included
ACLS 2005 Guidelines
VISIT www.circulationha.org
Circulation 2005. Dec 13: 112(24): p3667-3813 and Supp 11: p 1-211.
Global Comments
• BACK TO THE BASICS– Increased emphasis on CPR– Decreased emphasis on drugs
• SIMPLER– Consistent ratios for CPR– Less algorithms (PEA/Asystole out)– Tachycardia much simpler
• EVIDENCE “BASED”– Nice to see Landmark papers incorporated.– Recognition of importance of survival to discharge vs
survival to admission
Part 3/4: CPR/Adult BLS
• Lay Rescuers– Lay rescuers not taught artificial respirations or pulse
checks– Lay rescuers taught to look for “normal” breathing– Lay rescuers not taught the jaw thrust
• Age definitions– Neonatal age applies to baby deliver up until they leave
hospital– Different age cut offs for Lay rescuers
• <1year, 1-8 year, >8 year (Lay rescuer)• <1year, 1-adolescent, >adolescent to adult (HCP)
Part 3/4: CPR/Adult BLS
• Ventilations– Less important than compressions (EARLY)
– Ventilate enough to make chest rise
– Rate about 10 per minute after advanced airway
– AVOID over - ventilation (decreased venous return, decreased cardiac output)
– AVOID rapid/forceful breaths
– AVOID interruption of compressions after advanced airway placed
“LOW AND SLOW” ventilations
Part 3/4: CPR/Adult BLS • Compressions
– More important than ventilation – Rate about 100 compressions per minute– Push hard enough to compress the chest– Allow full recoil of chest– Allow equal time for compression and recoil– MINIMIZE interruptions in compressions
• Synchronicity– Unsynchronized ventilation/compression after
advanced airway placed
“HARD AND FAST” compressions
ED Interruptions in Compressions• Transfer to ED bed• Pulse checks• Placing patient on the monitor
and defibrillator• Rhythm checks• Vascular access• Airway management• Defibrillation• Drug delivery• Bedside ultrasound• ABG draw• Physical examination• Changeover of compressor
• We should minimize CPR interruptions
ACLS 2005Compress/
Ventilation ratio
Adult/
Adolescent
Child Infant
Single
Layperson
30:2 30:2 30:2
Double
Layperson
30:2 30:2 30:2
Single HCP 30:2 30:2 30:2
Double HCP 30:2 15:2 15:2
After Advanced Airway Device Placed: 100 compression/min10 breaths per minute (unsynchronized)
ACLS 2005Compress/
Ventilation ratio
Adult/
Adolescent
Child Infant
Single
Layperson
30:2 30:2 30:2
Double
Layperson
30:2 30:2 30:2
Single HCP 30:2 30:2 30:2
Double HCP 30:2 15:2 15:2
After Advanced Airway Device Placed: 100 compression/min10 breaths per minute (unsynchronized)
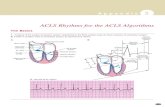
Part 5: Electrical Therapy
M o n op h a s ic
R e c tilin e ar T ru nca te d E xp on en tia l
B ip h a s ic
D e fib rilla to rs
Part 5: Electrical TherapyTruncatedExponential Rectilinear
Biphasic = increased ROSC, no increase Survival to hospital discharge
Recommended Energy for Defibrillation
Energy Monophasic Biphasic
Rectilinear
Biphasic
Truncated Exponential
Biphasic
Unknown
1st shock 360J 120J 150J 200J
Subsequent
shocks360J = or >
120J
= or >
150J
= or >
200J
Lifepak 12 and 20Peds: 2 J/kg then 4 J/kg
Evidence for CPR before defibrillation
• Cobb JAMA 1999– Prospective observational trial, N=1117
– Pre-intervention = defibrillate ASAP
– Post-intervention = 90 sec CPR before defib
– Survival to d/c Defib First CPR First PNNT
• Overall 24% 30% .04 16
• Response < 4min 31% 32% .87
• Response > 4min 17% 27% .007 10
Evidence for CPR before defibrillation
• Wik JAMA 2003– Randomized clinical trial, N=200
– Defibrillate ASAP vs CPR X 3 min before defibrillation
– Survival to d/c Defib First CPR First PNNT
• Overall 15% 22% .17
• Response < 5min 29% 23% .61
• Response > 5min 4% 22% .006 5.5
A priori subgroup analysis
Evidence for CPR before defibrillation
• Jacobs. Emerg Med Australasia. Feb 2005.– Randomized clinical trial, N=256
– Defibrillate ASAP vs CPR X 90 sec before defibrillation
– Survival to d/c Defib First CPR First OR 95%CI
• Overall 5.1% 4.2% .81 (.3-2.6)
– Survival to d/c Defib First CPR First P• Response < 5min 0% 12% .25
• Response > 5min 4.9% 3.5% .74
Post hoc subgroup analysis
Timing of Defibrillation
• ACLS 2005 Recommendation– CPR X 5 cycles of 30:2 (about 2 min)
recommended for out-of-hospital VF arrest• Response time > 4-5 minutes
• Unwitnessed
Part 7.2: Management of Cardiac Arrest
• ACLS Pulseless Algorithm 2005– Vfib Algorithm– PEA Algorithm– Asystole Algorithm
Circulation 2005;112:IV-58-66IV-
Notes on VF and pulseless VT
• CPR 30:2 until defibrillator ready• One shock, not three• 150J (not 360J) – Lifepak 12/20• CPR X 2min right after shock (no
rhythm check)• Timing of intubation not specified• Timing of vasopressor not specified• Epinephrine 1mg or vasopressin 40IU• Timing of antiarrythmic not specified• Amiodarone 300mg or Lidocaine 1.5
mg/kg
Amiodarone for Vfib/pulseless VT
• ARREST TRIAL • DBRCT, N=504• Amio vs Placebo
• Survival PL Amio P– Admission 34% 44% .03
– Discharge 13.4% 13.2% NS
• ALIVE TRIAL• DBRCT, N = 347• Amio vs Lidocaine
• Survival Lido Amio P– Admission 12% 23% .009
– Discharge 3.8% 6.8% NS
Kudenchuk et. al. NEJM 1999. 341(12): p.871. Dorian et. al. NEJM 2002. 346(12): p.884.
Circulation 2005;112:IV-58-66IV-
Notes on pulseless PEA/asystole
• Focus is on quality CPR and look for and treat reversible causes
• Atropine• Epinephrine or Vasopressin• PACING is OUT!
– Three RCTS of prehospital transcutaneous pacing showed no benefit
Why Vasopressin? Or why not……
• Linder. Lancet 1997.– N=40, out of hospital Vfib, vasopressin vs epi– Increased survival to admission not discharge
• Stiell. Lancet 2001.– N=200, in-hospital Vfib/PEA/asystole– Vasopressin vs epi– No difference in survival to discharge (power
0.8)
Vasopressin• Wenzel. NEJM 2004. 350(2). P 105-113.
– DBRCT, N= 1186– Out-of-hospital vfib/PEA/asystole– Vasopressin 40IU vs Epinephrine 1mg– Survival all patients AVP EPI P
• Admission 36% 31% .06• Discharge 10% 10% .99
– Survival Asystole AVP EPI P NNT• Admission 29% 20% .02• Discharge 4.7% 1.5% .04 31
Problem = multiple subgroup analysis (29); suspected type I (alpha) error
Bradycardia Notes
• No major changes• Increased emphasis on early pacing for
unstable patients• Atropine unlikely to work with infranodal
blocks/escape rhythms– 2nd degree type II AVB– 3rd degree AVB– Wide QRS escape rhythm
Tachycardia Algorithm
• General Comments– Much simpler– Cardiac function/Ejection Fraction decision
branches removed– Less drugs listed at each box– Less emphasis on trying to distinguish Vtach vs
SVT + aberrancy– Nice approach …………..
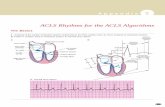
A C LS 20 05 A pp roa ch
R e g u la r Irre g u la r
N a rro w
R e g u la r Irre g u la r
W ide
S T A B LE U N S T A B LEC a rd io ve rt
T a ch yca rd ia
Wide QRS Tachycardia
A d e no s in e fo r S V T +aP ro ca in e a 1s t line op tion
L id o ca in e N O T 1s t lineS o ta lo l N O T 1 s t line
A m io d aro neC a rd iove rs ion
V ta chR e g u la r S V T + a b erra n cy
R e g u la r
P ro lon g e d Q T c:P a c in g , iso p ro te ren o l,
L id oca ine
N o rm a l b a se line Q T c:A m io o r L id oca ine
D e fib rilla teM a g ne s ium
S to p R x , co rre c t lyte s,tre a t is che m ia
T o rsa d es
T re a t a s p er A fib
A F IB + B B B
A V O ID A V N b lo cke rsA m ida ro ne
A F IB + W P W
T o rsa d esIrre g u la r S V T + a b be ra n cy
Irre g u la r
S tab leW id e Q R S
AFIB + WPW
• Tijunelis. CJEM 2005. Vol7(4)p. 262-5.– Literature review of Afib + WPW treated with amiodarone– No controlled studies– 10 case reports– 7/10 developed Vfib or unstable VT
• AMIODARONE NOT SAFE for AFIB +WPW • CARDIOVERSION is the treatment of choice
Induced Hypothermia:NEJM Feb 2002 --what is the evidence?
• Austrian Study – RCT, N=136
– Witnessed VF/pulseless VT
– Excluded: Sats < 85%, hypotension > 30 min, coagulopathy, etc
– 32-34 degrees X 24hrs
– Result cool warm NNT
• Neurofn 6mo 55% 39% 6
• Mortality 6mo 41% 55% 7
• Australian Study – RCT, N=77– Initial VF rhythm then comatose– Excluded: SBP<90 despite epi,
non-primary-cardiac etiologies– 33 degrees X 18hrs– Result cool warm NNT
• Survival 49% 26% 4
– Outcome = survival to discharge home or neurorehab unit
Part 7.5: Postresuscitation
• ACLS 2005 Guideline for Induced Hypothermia– Recommended for post Vfib arrest with ROSC
but remains comatose– “Consider” for non-VF arrest
Why the emphasis on CPR and defibrillation?
• OPALS study– Stiell. NEJM 2004. 351(7). P 647-656.
BLS + Rapid Defibrillation
N = 139112 months
ALS care (ETT,iv,drugs)
N = 424736 months
Why the emphasis on CPR and defibrillation?
• OPALS study– Stiell. NEJM 2004. 351(7). P 647-656.
BLS + Rapid Defibrillation
Survival to 11% 15% p.001Admission
Survival to 5.0% 5.1% p.83 Discharge
ALS care (ETT,iv,drugs)
Why the emphasis on CPR and defibrillation?
• OPALS study– Stiell. NEJM 2004. 351(7). P 647-656.– Logistic Regression OR for survival
• Witnessed arrest 4.4• Bystander CPR 3.7• AED < 8min 3.4
Take home points
• One shock (not three) for VF• Lower energy with biphasic defibrillators• Less emphasis on drugs• More emphasis on CPR
– CPR 30:2 ratio– CPR before defibrillation for response times > 4
minutes– Quality CPR with minimal interruptions– Should we call ourselves CPR-coaches?– Why isn’t CPR taught in high-school?