ACL - Sport Specific Rehabilitation
description
Transcript of ACL - Sport Specific Rehabilitation

FLEX THERAPISTS CEUs 1422 Monterey Street, Suite C-102
San Luis Obispo, Ca 93401
Ph (805) 543-5100 Fax (805) 543-5106
www.flextherapistceus.com
Return to Sports Guidelines Following ACL Reconstruction
Table of Contents
1. Soccer Pages 304 - 312
2. Alpine Skiing Pages 313 - 325
3. Basketball Pages 326 – 336
4. American Football Pages 337 - 344

304 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
Football (soccer) is the most popular sport worldwide, with an estimated 300 million active players (as documented by the Fédération Internationale de Football Association). Anterior cruciate ligament
(ACL) injury is one of the most serious injuries in soccer and a potentially career-ending one.54 The incidence of ACL injuries in soccer players accounts for thousands of ACL tears per year.1 Despite
the high number of injuries1,3,14 and re-lated literature, there is still no consen-sus on the optimal surgical technique for ACL reconstruction5 and even less agreement on the ideal rehabilitation protocol following surgery.30,51 Recently, van Grinsven et al51 proposed an optimal evidence-based rehabilitation program. Their systematic review indicated that
TT SYNOPSIS: Successful return to play remains a challenge for a soccer player after anterior cruciate ligament reconstruction. In addition to a successful surgical intervention, a soccer-specific functional rehabilitation program is essential to achieve this goal. Soccer-like elements should be incorporated in the early stages of rehabilita-tion to provide neuromuscular training specific to the needs of the player. Gym-based and, later, field-based drills are gradually intensified and pro-gressed until the player demonstrates the ability to return to team practice. In addition to the recovery of basic attributes such as mobility, flexibility, strength, and agility, the surgically repaired knee must also regain soccer-specific neuromuscular control and conditioning for an effective return to
sports. The individual coaching of the player by the sports physiotherapist and compliance with the training program by the player are key factors in the rehabilitation process. To minimize reinjury risk and to maximize the player’s career, concepts of soccer-specific injury prevention programs should be incorporated into the training routine during and after the rehabilitation of players post–ACL reconstruction.
TT LEVEL OF EVIDENCE: Therapy, level 5. J Orthop Sports Phys Ther 2012;42(4):304-312. doi:10.2519/jospt.2012.4005
TT KEY WORDS: ACL, football/soccer, functional training, injury prevention
1Research Associate, FIFA-Medical Assessment and Research Centre (F-MARC), Schulthess Clinic, Zürich, Switzerland. 2Director of Training and Conditioning, New York Knicks (NBA), New York, NY; Physical Therapist of the England National Football Team (UK); Former Head Physical Therapist, Leeds United Football Club and Chelsea Football Club (Premier League, England), UK. 3Scientific Director of CeRiSM, Research Center for Sports, Mountain and Health, University of Verona, Rovereto (TN), Italy. Address correspondence to Dr Mario Bizzini, F-MARC, Schulthess Clinic, Lengghalde 2, 8008 Zürich, Switzerland. E-mail: [email protected]
MARIO BIZZINI, PT, PhD1 • DAVE HANCOCK, MSc, MCSP, BHSc, HPC2 • FRANCO IMPELLIZZERI, PhD3
Suggestions From the Field for Return to Sports Participation Following Anterior Cruciate Ligament Reconstruction: Soccer
interventions for the early rehabilitation phases, which included pain/swelling control, neuromuscular training, and ear-ly weight-bearing, range-of-motion, and strengthening exercises, are supported by evidence. Criteria for return to sports in-clude “hop tests and strength of the ham-strings and quadriceps at least of 85% compared to the contralateral side” and
“when the patient toler-ates sport-specific activi-ties.”51 This description, albeit offering a minimal standard for the knee, is
clearly not detailed enough when dealing with athletes (ie, soccer players) aiming for a return to competitive sports after ACL reconstruction.
Some authors have described guide-lines for return to play after ACL sur-gery10,28,34; however, few publications have specifically discussed the return to competitive soccer.43,44 In a recent review, Kvist28 located 39 articles that presented outcomes after ACL reconstruction and criteria for returning to sports. In most cases, the decision of when to allow the patient/athlete to return to sport was empirical and time based, ranging from 3 to 12 months postsurgery. Functional training and testing have also been ad-vocated, ranging from plyometrics and running programs to isokinetic train-ing/testing and jump/hop training/test-ing.10,20,37 However, descriptions of the late phases of the rehabilitation process often remain generic. Myer et al34 also introduced a detailed criteria-based re-habilitation protocol for the return to sport after ACL reconstruction; however, the “reintegration to interval sport par-ticipation” was not specifically described. Therefore, it is perhaps understandable
SUPPLEMENTAL VIDEO ONLINE
42-04 Bizzini.indd 304 3/21/2012 4:32:29 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 305
that Walden et al53 found a significantly higher risk of new knee injury (either reinjury or contralateral injury) in elite soccer players who had a previous ACL injury/reconstruction.
The major challenge is to integrate sports-specific elements within the re-habilitation and training of the soccer athlete, considering that a soccer player has different neuromuscular and physi-ological demands than an ice hockey
or basketball player.49 One of the key elements to a soccer-specific rehabili-tation program is an understanding of the physical demands of the sport and the level of play to which the player needs to return. Consideration of the frequency and intensity of training ses-sions and games is very important. Soc-cer is a physically demanding sport, with match analysis studies showing that soc-cer players repeatedly produce maximal
or near maximal actions (eg, striding, turning, cutting, sprinting, jumping) of short duration with brief recovery peri-ods.33,48,49 These activities, which require coordination and power, place consid-erable demands on the neuromuscular system. A carefully planned rehabilita-tion program that addresses all aspects of the game is vital to return the player to maximum function, while minimiz-ing risk of reinjury. The following is our
TABLE 1 Phases of Rehabilitation
Abbreviations: ADL, activities of daily living; ROM, range of motion; RSSA, repeated-shuttle-sprint-ability test; Yo-Yo, Yo-Yo intermittent recovery test.*The timing of each phase is dependent on additional surgical procedures and individual progress in rehabilitation/training.†Details provided in the text.
Phase 1 Phase 2 Phase 3Return to Reduced Soccer Practice
Return to Full Soccer Practice
Timing* 4-6 wk 4-6 to 8-12 wk 8-12 to 16-24 wk 16-24 to ? wk
Criteria to enter this
phase
• Minimal pain/swelling
• Near full ROM
• Good patella mobility
• Sufficient quadriceps
control
• Normal gait pattern
• No pain/swelling
• Full ROM
• Good neuromuscular
control at knee, hip, trunk
• Quadriceps and hamstrings
strength >75% of
noninvolved limb
• Good hop/jump and land-
ing techniques
• No pain/swelling
• Symmetrical ROM
• Optimal soccer-specific
neuromuscular control
• Quadriceps and hamstrings
strength >85% of
noninvolved limb
• Hop index >80% of
noninvolved limb
• No pain/swelling
• Symmetrical ROM
• Optimal soccer-specific
neuromuscular control
• Quadriceps and
hamstrings strength >95%
of noninvolved limb
• Hop index >90% of
noninvolved limb
• Satisfactory Yo-Yo and
RSSA test results
Goals of this phase • Control pain/swelling
• Improve ROM
• Quadriceps activation
• ADL activities
• Prepare basic soccer-
specific neuromuscular
control
• Prepare the player for the
more intense phase 3
• Optimize soccer-specific
neuromuscular control
• Prepare the player for
return to team practice
• Bring the player back
to unrestricted team
practice, with full
possession of his soccer
skills and conditioning
• Final preparation of the
player for the needs and
demands of competitive
soccer
Functional training†
Additional training • Strengthen noninvolved
limb
• Trunk and hip basic core
stability exercises
• Cardiovascular (upper-body
ergometer)
• Core stability
• Strengthen involved limb
(open/closed chain)
• Cardiovascular training
(basic, bike)
• Flexibility
• Core stability/strength
• Strength training (body-
machine exercise)
• Cardiovascular soccer-
specific training (interval,
bike)
• Flexibility
• Core stability/strength
• Strength training (body-
machine exercise) focused
on addressing remaining
deficits
• Flexibility
• Continue additional train-
ing, in the form of a soccer-
specific warm-up (11+)
Pool activities • Gait training
• Simple exercises (ROM,
balance)
• Progression toward water
running (wet vest)
• Flexibility/ROM
• Simulated basic soccer
drills (heading the ball)
• Water running: endurance
training
Phase 4
42-04 Bizzini.indd 305 3/21/2012 4:32:30 PM

306 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
perspective on a return-to-play model to prepare soccer players to compete after ACL reconstruction.
PHASES OF THE PROGRAM
A key aspect for successful reha-bilitation of a professional soccer player is a one-to-one (sports phys-
iotherapist-to-athlete) approach. This al-lows daily monitoring of the knee status and progress, and also permits optimal adaptation of the intensity and content of the rehabilitation program. A close cooperation between the athlete, phys-iotherapist, surgeon, athletic trainer, and coach is another key factor.
The rehabilitation may arbitrarily be divided into 4 phases: (1) protection and controlled ambulation, (2) controlled training, (3) intensive training, and (4) return to play.7,8 The time frame for each phase varies depending on the surgical procedure and individual response to treatment. The overall guiding principle is that the program should be soccer spe-
cific, criteria based, and intensive but not aggressive (TABLE 1).7,17,21,43
Myer et al34 presented a criteria-driv-en progression through the return-to-sport phase of rehabilitation following ACL reconstruction. The authors pro-posed objective assessments of strength, stability, balance, limb symmetry, power, agility, technique, and endurance to guide the athlete back to sports. Recently, Impellizzeri and Marcora23 critically dis-cussed the validity of physiological and performance tests in sports. As the focus of this paper is on functional rehabilita-tion, we will not cover the assessments for all phases in detail but, rather, provide updated evidence-based and clinical-expertise guidelines.
Phase 1This phase, focusing on recovery of mo-tion and ambulation and control of swell-ing immediately postsurgery, will not be discussed. The criteria that the patient has to fulfill to enter phase 2 are de-scribed in TABLE 1.
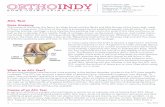
Phase 2This phase includes soccer-specific neu-romuscular training. Initially, the focus is on knee (and lower extremity) stabiliza-tion in weight-bearing positions, starting with static, then dynamic, and eventually reactive exercises.41 Particular attention is given to the varus/valgus and rotational control of the surgically repaired knee and lower extremity, emphasizing prop-er lower extremity alignment (avoiding collapse of the knee medially) and pelvis and trunk stabilization.6,40 Training on unstable surfaces is particularly useful to enhance neuromuscular activation and control (FIGURE 1). Rotational stabiliza-tion can be trained on a simple rotatory unstable surface.7
According to motor-learning prin-ciples (blocked/random practice),46 it is important to exercise in different envi-ronmental conditions (eg, in the gym-nasium, indoor hall, and on the pitch) and with different footwear (eg, with no shoes, athletic shoes, and soccer shoes). The soccer ball should be used, as much as possible, as a tool to enhance reactive stabilization strategies (FIGURE 2). With a field player, the basic passes (feet) are simulated, while basic ball receptions
FIGURE 1. Male professional soccer player on swinging platform (simulation of kicking ball with nonoperated leg).
FIGURE 2. Female amateur soccer player on foam pad (passing back the soccer ball with nonoperated leg).
FIGURE 3. Male professional soccer player sitting on a soccer ball (and juggling another ball).
42-04 Bizzini.indd 306 3/21/2012 4:32:32 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 307
(hands) are used with a goalkeeper. The athlete is allowed to bounce/juggle the ball, and also to execute simple passes (using the internal and external sides of the foot) with the operated leg. Some-times the athlete may combine specific training with less-focused activities (FIGURE 3). Incorporating the soccer ball and soccer-specific equipment (shoes) in phase 2 is not only important to en-hance soccer-specific neuromuscular stabilization strategies but also to pro-mote a positive psychological attitude in rehabilitation.
Later in phase 2, the goal is to con-trol forward, backward, lateral, diagonal, and rotational body displacements, while
focusing on knee stabilization. Working against elastic resistance is considered a powerful tool to train neuromuscular control, as the knee, lower extremity, pel-vis, and upper body need to be controlled based on the direction of the resistance. First, the focus is on proper stabiliza-tion at slower speeds (side to side, with-out jumping), then speeds and dynamic movements are gradually increased. Ba-sic exercises, such as lunges (front, lat-eral, or diagonal), performed with and without trunk rotations, are useful in promoting multiplanar stabilization of the surgically repaired knee.
Some simple forms of quickness drills are also included in this phase. For ex-
ample, the athlete stands still, then, at the start signal, performs soft sprinting over a few meters before stopping and stabiliz-ing on the operated knee, then kicks the ball with the nonoperated leg. This may be performed first in the gym and then on the pitch to best stimulate the motor-learning process.
The basic plyometric techniques (proper landing and stabilization) are progressed from double-leg to single-leg activities (horizontal and vertical jump), emphasizing quality versus quantity of movement. Heading the ball is also prac-ticed, with proper take-off and landing technique(s).
Pool activities are a popular form of
TABLE 2 Progression of Running and Soccer Drills
Part 1 Part 2 Part 3
Level 1 Running: straight line
a. Endurance (time/distance)
b. Player-specific runs, midfield/center forwards distances
c. Shorter distances
d. Gradually increasing speed
e. Forward/backward runs: 1:4 min run-rest ratio building up
to 1:1 min (×4) and 2:1 (×3) to train the anaerobic lactate
threshold. A long recovery time is needed between each set
of exercises (4 min)
Passing
Side footing: start with standing ball and move through the
progressions, then progress to a moving ball both on the floor
and on the volley.
a. Short distances
b. Longer distances
c. Greater velocity on the pass
Dribbling
a. Straight-line ball control
b. Forward/backward turns
c. Instep ball control
d. Outstep ball control
Level 2 Running: figure-of-eight runs
With the same progressions as straight line
Passing: forefoot (on the laces)
a. Short distances
b. Longer distances
c. Greater velocity on the pass: same as with the side-foot
pass once, moved through the progressions, progress to
moving the ball on the floor first to eventually on the volley
a. Volleys side foot/laces/outside of foot
b. Volleys with quick-feet: incorporate quick-feet and volley to
ladders/hurdles/left-right foot on command, quick reaction
volley drills
Lateral dribbling movements
a. Long distances
b. Short distances
c. At speed
d. Side movement with the ball, changing
direction on command, at speed
Level 3 Running: open lateral zigzag runs
a. Endurance base with long turns
b. Gradually reducing distance between cones
c. Increase number of turns and increase speed of turn
Corners
Goal kicks from the hands to on the floor
Follow the above kicking progressions
Level 4 Running: rotations
a. Without the ball
b. With the ball
c. Including pass increase as with the above
Progressions: endurance/distance/repetitions/speed
Free kicks
Follow the above progressions on kicking the ball (distance/
force/speed)
Shooting
As above with regard to progression
Rotation dribbling movements
a. Long rotations with the ball at the feet
b. Short rotations with the ball
c. Quick, sharp turns with the ball to both
left and right sides
d. Sharp turns on receiving a pass or volley
42-04 Bizzini.indd 307 3/21/2012 4:32:33 PM

308 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
additional training for soccer players in this controlled phase.43 Using the prop-erties of water, the athlete may exercise balance and coordination, in addition to performing running exercises (eventually with a wet vest), with minimal loading on the operated knee.
The athlete is ready to move to phase 3 when he/she has reached the criteria described in TABLE 1.
Phase 3More complex and challenging soccer-specific drills characterize phase 3 (TABLE
1).Soccer-Specific Drills TABLE 2 shows an outline of a “classical” progression (3 parts with 4 levels each) for running and soccer drills. Specific parts/levels can be added or removed as the player pro-gresses. There are no set time frames to complete each part at a given level, but performing each point (a, b, c, etc) of the
progression for a level at the same fre-quency for 3 days is recommended before moving to the next level, whether it be distance, time, repetitions, or intensity. This allows for a gradual progression of each part and thus ensures correct func-tion and that no adverse knee reaction is noted before moving on to the next level. Rehabilitation programs have been shown to fail due to a rapid increase in exercise load, whether of speed or dura-tion, or the addition of different exercises that place a higher demand on the knee and graft.34
Star Run Drill This drill can be adapted to running and soccer-specific training. It can incorporate all aspects of soccer, including forward, backward, or multidi-rectional drills, and explosive and reac-tive drills with cutting. The outline of the drill is simple (FIGURE 4). The distances may be increased or decreased, but player position tends to dictate the size of the
square and the intensity with which the player is working. Research from match analyses49 has shown that the sprints are between 10 and 25 m in length and 3 and 5 seconds in duration. The energy systems being used are also an important consideration during these phases of re-habilitation. Soccer players need to train both the anaerobic and aerobic systems, as distances up to 10 km (central defend-ers) or 12 km (midfielders) are covered by top-level professional players in a match.49
Combined Drills Different activities such as quick-feet, short sprints, cutting and accelerating, and body rotations can be trained in a rapid sequence over a pre-defined distance (eg, 20 m). Incorporat-ing various skills into a rapid sequence has proven to be an effective specific quickness and dynamic body control training method for soccer players after knee surgery (ONLINE VIDEO 1).
FIGURE 4. Star run drill. Basic setup and different drills: (A) star run outline, (B) star run with zigzag cutting drill, (C) star run with forward/backward ladder drills, (D) star run with running curves through poles.
42-04 Bizzini.indd 308 3/21/2012 4:32:35 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 309
Contact Situations One aspect of the lat-er sport-specifi c drills is contact, which is a major element of the game of soccer. Al-though ACL ruptures tend to occur more often without contact,42 those occurring from contacts cannot be ignored. Roi et al,44 analyzing data from the Italian Serie A League, determined that ACL contact injuries occurred more frequently during competitive games, while noncontact in-juries occurred more often during train-ing and nono cial games. Mihata et al32
compared a number of di� erent sports (basketball, soccer, and lacrosse) and suggested that the level of allowed con-tact in pivoting sports may be a factor in determining sport-specifi c ACL risk.
Often, the level of contact of the sport is overlooked in the rehabilitation pro-gram and left to players to manage as
they gradually rejoin training. Although there is always risk with contact, we sug-gest that it may be better to include this aspect of the game in a controlled envi-ronment of rehabilitation rather than leave it to the unpredictable environment of a training session. If the player’s knee is able to gradually withstand forces of valgus/varus with and without rotation, they must be able to cope with the grad-ual load/forces of contact. Controlling the decelerating forces from a contact is vital, as it has been shown to reduce the incidence of ACL rupture.9,16 Repetitive training of proper landing techniques has enabled athletes to develop learned responses that may help minimize or pre-vent injury when they are placed in game or practice situations.34,52
Contact can be controlled with block tackles (FIGURE 5) and single-leg kicking of objects that move (FIGURE 6), eventually progressing to actual body load, whether on the ground or in the air (FIGURE 7).Tackle Situations The sliding tackle is another type of contact that must be ad-dressed, as it is an important function of the knee in the defensive side of the game. Graded progressions of landing on the fl oor and kicking a ball away can be included fi rst without another person, and eventually with a therapist asking the
patient to slide in and kick the ball away from the therapist’s feet. Sets and repeti-tions can be added gradually, with speed only being added as the patient is starting to join group training. It is vital, however, that before adding these late-stage drills, all aspects of single-leg hopping and rota-tion training have been completed. The grass surface must also be inspected prior to performing these types of drills, as ex-ternal conditions, such as a slippery wet surface, could place the athlete at great-er risk. The criteria to allow the athlete to progress to phase 4 are described in TABLE 1.
Phase 4, Return to Play: What Does It Mean?Respecting a gradual and progressive re-turn to competitive soccer is crucial for the player following ACL reconstruction. Therefore, it is necessary to di� erentiate between various types of return:• Return to reduced team training prac-
tice (no contact)• Return to full (normal) team training
practice (with contact)• Return to “friendly” games (initially
not over the full duration of a match)• Return to competitive match (initially
not over the full duration of a match)This fi rst return is often the most
crucial. The player must be physically and psychologically ready to shift from individual training, where most situa-tions are intense but controlled, to team training, where the player is also exposed to uncontrolled situations. In this phase, the player also continues to perform specifi c training, focusing on improving identifi ed defi cits (strength, coordina-tion, and endurance) under supervision. Recent research has clearly shown that strength/power and functional defi cits in the involved lower extremity may persist up to 6 or more months after pri-mary ACL reconstruction,20,35,36 and that persistent strength imbalances may be linked with an increased risk of reinjury in soccer.12,29
Thomeé et al50 critically discussed the common muscle strength and hop per-
FIGURE 5. Block tackles at di� erent angles and intensities, on di� erent types of surfaces, from a soft defl ated soccer ball to a harder leather medicine ball.
FIGURE 6. Kicking action into pads while balancing on an unstable surface, incorporating standing balance while making contact. The use of unstable surfaces helps to promote di� erent reactive stabilization strategies.
FIGURE 7. In-air body contact, trying to simulate heading and body contact in the gym environment. Specifi c instructions are given on landing correctly on the forefoot/toes and absorbing the landing forces. Progressions can be added by di� erent directional forces and intensity of body weight contact.
42-04 Bizzini.indd 309 3/21/2012 4:32:36 PM

310 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
REFERENCES
1. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Pre-vention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17:705-729. http://dx.doi.org/10.1007/s00167-009-0813-1
2. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Pre-vention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk fac-tors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17:859-879. http://
formance criteria used prior to return to sport, which may not be demanding and sensitive enough to detect side differenc-es, and proposed new recommendations for muscle function tests in individuals after ACL reconstruction.
Because soccer is a high-intensity intermittent activity, training should include physical exercises aimed to en-hance aerobic fitness, anaerobic power and capacity, repeated sprint ability, and muscle power and strength. Other than coping with the physiological demands of the match, physical training can coun-teract the decline in technical proficien-cy caused by fatigue.26 Several studies have shown different effective training strategies for improving these fitness components.13,15,19,22,24
Functional Tests to Clear Return to Play Myer et al35 recently presented a battery of performance tests (modified NFL Combine testing) to show how unilateral deficits are present and may be hidden in double-leg activities in athletes 1 year after ACL reconstruction. Therefore, the sports physiotherapist needs to regu-larly check single-leg hop tasks of the involved limb, while ensuring that the player continues to demonstrate good overall quality of movement (knee, hip, and trunk).
Unrestricted participation in team practice (without any adverse knee joint reactions) is, of course, an important cri-terion to be able to return to compete in a soccer match. There are no validated sports-specific tests to determine readi-ness to return to full participation in team practice and competitive matches for soccer players after ACL surgery. However, the 2 performance tests con-sidered the best, in terms of validity and reliability in healthy soccer players, are the Yo-Yo intermittent recovery (Yo-Yo) test4 and the repeated shuttle-sprint ability (RSSA) test.25 Data are available for different players’ roles (defender, full-back, midfielder, and forward) that, even if cut-off values do not exist, may help in judging the performance and return-to-play readiness of the player.27 The Yo-
Yo and RSSA tests may also be used to monitor improvement of the athlete over time. Additional specific tests, such as speed dribbling, short-long passing, and shooting, have been proposed in the lit-erature45 but have never been fully scien-tifically validated. These and other skills are practiced daily, and, similar to playing against an opponent, physical and mental preparation must be gradually optimized (TABLE2).
Therefore, to return to full partici-pation after ACL surgery, the soccer player must make a successful progres-sion through the described rehabilitation phases and show satisfactory (as judged by the sports physiotherapist) Yo-Yo and RSSA test results.
PREVENTIONOFREINJURYAFTERACLRECONSTRUCTION
In the last few years, ACL injury prevention programs for female and male soccer players have been devel-
oped and their effectiveness scientifi-cally confirmed.2 A reduction of 30% to 50%, and even higher for females,18 has been shown in the incidence of noncon-tact ACL injuries.47 Programs such as the Perform and Enhance Performance31 and the 11+ (ONLINEVIDEO 2),47 which combine cardiovascular and specific injury pre-vention exercises, should be performed as a warm-up prior to technical and tactical training. Considering the risk of reinjury39,53 and that some aspects of biomechanical and neuromuscular func-tion may be deficient up to several years after the ACL reconstruction,11,34,36 play-ers should ideally continue post–ACL reconstruction neuromuscular training on a regular basis for the remainder of their career.
In this respect, the use of screening tests to identify players at risk for ACL injury may be recommended. The Land-ing Error Scoring System, developed by Padua et al,38 is a valid and reliable clini-cal assessment tool for jump-landing bio-mechanics, and may have the potential to predict ACL injury or reinjury.
SUMMARY
Asoccer player faces many chal-lenges following ACL reconstruc-tion. The player has to deal with the
pressure of his entourage (club, coach, other) and the risk of jeopardizing his career, while pursuing the goal of a suc-cessful return to play. The sports phys-iotherapist plays an important role in monitoring a closely supervised criteria-based program and in guiding the athlete during the rehabilitation and training process. Functional training is a key el-ement in regaining the soccer-specific neuromuscular control necessary to per-form skills ranging from basic to soccer-specific drills. Particular attention should be given to the quality of the movement patterns and stabilization strategies. Re-sidual impairments in strength, power, agility, and sensorimotor capacity should be specifically addressed while the athlete undergoes soccer-specific conditioning and fitness training.
The goal is to reintegrate the player gradually in the game, taking into ac-count his/her individual characteristics. Several evidence-based and empirical cri-teria are needed to plan and monitor the efficient return to competitive soccer. In-jury prevention education should be part of this process to maximize the chance of a durable career. Further research is nec-essary to better understand and assess different aspects of muscle function and motor control after ACL reconstruction in soccer players. t
42-04 Bizzini.indd 310 3/21/2012 4:32:37 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 311
dx.doi.org/10.1007/s00167-009-0823-z 3. Arnason A, Sigurdsson SB, Gudmundsson
A, Holme I, Engebretsen L, Bahr R. Risk fac-tors for injuries in football. Am J Sports Med. 2004;32:5S-16S.
4. Bangsbo J, Iaia FM, Krustrup P. The Yo-Yo inter-mittent recovery test: a useful tool for evaluation of physical performance in intermittent sports. Sports Med. 2008;38:37-51.
5. Beynnon BD, Johnson RJ, Abate JA, Flem-ing BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med. 2005;33:1579-1602. http://dx.doi.org/10.1177/0363546505279913
6. Bizzini M. Sensomotorische Rehabilitation nach Beinverletzungen. Mit Fallbeispielen in allen Hei-lungsstadien. Stuttgart, Germany: Thieme; 2000.
7. Bizzini M, Gorelick M, Drobny T. Lateral meniscus repair in a professional ice hockey goaltender: a case report with a 5-year follow-up. J Orthop Sports Phys Ther. 2006;36:89-100. http://dx.doi.org/10.2519/jospt.2006.2015
8. Bizzini M, Notzli HP, Maffiuletti NA. Femoro-acetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35:1955-1959. http://dx.doi.org/10.1177/0363546507304141
9. Caraffa A, Cerulli G, Projetti M, Aisa G, Rizzo A. Prevention of anterior cruciate ligament injuries in soccer. A prospective controlled study of pro-prioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4:19-21.
10. Cascio BM, Culp L, Cosgarea AJ. Return to play after anterior cruciate ligament reconstruction. Clin Sports Med. 2004;23:395-408. http://dx.doi.org/10.1016/j.csm.2004.03.004
11. Chmielewski TL. Asymmetrical lower extremity loading after ACL reconstruction: more than meets the eye. J Orthop Sports Phys Ther. 2011;41:374-376. http://dx.doi.org/10.2519/jospt.2011.0104
12. Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and preven-tion of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36:1469-1475. http://dx.doi.org/10.1177/0363546508316764
13. Dupont G, Akakpo K, Berthoin S. The ef-fect of in-season, high-intensity interval training in soccer players. J Strength Cond Res. 2004;18:584-589. http://dx.doi.org/10.1519/1533-4287(2004)18<584:TEOIHI>2.0.CO;2
14. Dvorak J, Junge A. Football injuries and physi-cal symptoms. A review of the literature. Am J Sports Med. 2000;28:S3-S9.
15. Ferrari Bravo D, Impellizzeri FM, Rampi-nini E, Castagna C, Bishop D, Wisloff U. Sprint vs. interval training in football. Int J Sports Med. 2008;29:668-674. http://dx.doi.org/10.1055/s-2007-989371
16. Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation pro-
grams for physical active individuals. Phys Ther. 2000;80:128-140.
17. Fuller CW, Walker J. Quantifying the functional rehabilitation of injured football players. Br J Sports Med. 2006;40:151-157. http://dx.doi.org/10.1136/bjsm.2005.021048
18. Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36:1476-1483. http://dx.doi.org/10.1177/0363546508318188
19. Gorostiaga EM, Izquierdo M, Ruesta M, Iribar-ren J, Gonzalez-Badillo JJ, Ibanez J. Strength training effects on physical performance and serum hormones in young soccer players. Eur J Appl Physiol. 2004;91:698-707. http://dx.doi.org/10.1007/s00421-003-1032-y
20. Gustavsson A, Neeter C, Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:778-788. http://dx.doi.org/10.1007/s00167-006-0045-6
21. Hagglund M, Walden M, Ekstrand J. Lower reinjury rate with a coach-controlled reha-bilitation program in amateur male soccer: a randomized controlled trial. Am J Sports Med. 2007;35:1433-1442. http://dx.doi.org/10.1177/0363546507300063
22. Hill-Haas SV, Coutts AJ, Rowsell GJ, Dawson BT. Generic versus small-sided game training in soc-cer. Int J Sports Med. 2009;30:636-642. http://dx.doi.org/10.1055/s-0029-1220730
23. Impellizzeri FM, Marcora SM. Test validation in sport physiology: lessons learned from clinimetrics. Int J Sports Physiol Perform. 2009;4:269-277.
24. Impellizzeri FM, Marcora SM, Castagna C, et al. Physiological and performance effects of generic versus specific aerobic training in soccer play-ers. Int J Sports Med. 2006;27:483-492. http://dx.doi.org/10.1055/s-2005-865839
25. Impellizzeri FM, Rampinini E, Castagna C, et al. Validity of a repeated-sprint test for football. Int J Sports Med. 2008;29:899-905. http://dx.doi.org/10.1055/s-2008-1038491
26. Impellizzeri FM, Rampinini E, Maffiuletti NA, Castagna C, Bizzini M, Wisloff U. Effects of aerobic training on the exercise-induced decline in short-passing ability in junior soccer players. Appl Physiol Nutr Metab. 2008;33:1192-1198. http://dx.doi.org/10.1139/H08-111
27. Krustrup P, Mohr M, Amstrup T, et al. The Yo-Yo intermittent recovery test: physiologi-cal response, reliability, and validity. Med Sci Sports Exerc. 2003;35:697-705. http://dx.doi.org/10.1249/01.MSS.0000058441.94520.32
28. Kvist J. Rehabilitation following anterior cruci-ate ligament injury: current recommenda-tions for sports participation. Sports Med. 2004;34:269-280.
29. Lehance C, Binet J, Bury T, Croisier JL. Muscular strength, functional perfor-mances and injury risk in professional and
junior elite soccer players. Scand J Med Sci Sports. 2009;19:243-251. http://dx.doi.org/10.1111/j.1600-0838.2008.00780.x
30. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40:A1-A37. http://dx.doi.org/10.2519/jospt.2010.0303
31. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in prevent-ing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003-1010. http://dx.doi.org/10.1177/0363546504272261
32. Mihata LC, Beutler AI, Boden BP. Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players: implications for anterior cruciate ligament mechanism and prevention. Am J Sports Med. 2006;34:899-904. http://dx.doi.org/10.1177/0363546505285582
33. Mohr M, Krustrup P, Bangsbo J. Match perfor-mance of high-standard soccer players with special reference to development of fatigue. J Sports Sci. 2003;21:519-528. http://dx.doi.org/10.1080/0264041031000071182
34. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progres-sion through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385-402. http://dx.doi.org/10.2519/jospt.2006.2222
35. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377-387. http://dx.doi.org/10.2519/jospt.2011.3547
36. Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39:127-131. http://dx.doi.org/10.1136/bjsm.2004.010900
37. Neeter C, Gustavsson A, Thomeé P, Augusts-son J, Thomeé R, Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Trauma-tol Arthrosc. 2006;14:571-580. http://dx.doi.org/10.1007/s00167-006-0040-y
38. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Jr., Beutler AI. The Landing Error Scoring System (LESS) is a valid and reli-able clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009;37:1996-2002. http://dx.doi.org/10.1177/0363546509343200
39. Paterno MV, Schmitt LC, Ford KR, et al. Biome-chanical measures during landing and postural stability predict second anterior cruciate liga-ment injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. http://dx.doi.org/10.1177/0363546510376053
40. Powers CM. The influence of abnormal hip
42-04 Bizzini.indd 311 3/21/2012 4:32:38 PM

312 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
@ MORE INFORMATIONWWW.JOSPT.ORG
mechanics on knee injury: a biomechani-cal perspective. J Orthop Sports Phys Ther. 2010;40:42-51. http://dx.doi.org/10.2519/jospt.2010.3337
41. Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength train-ing during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87:737-750. http://dx.doi.org/10.2522/ptj.20060041
42. Rochcongar P, Laboute E, Jan J, Carling C. Rup-tures of the anterior cruciate ligament in soccer. Int J Sports Med. 2009;30:372-378. http://dx.doi.org/10.1055/s-0028-1105947
43. Roi GS, Creta D, Nanni G, Marcacci M, Zaffagnini S, Snyder-Mackler L. Return to official Italian First Division soccer games within 90 days after anterior cruciate ligament reconstruction: a case report. J Orthop Sports Phys Ther. 2005;35:52-61; discussion 61-66. http://dx.doi.org/10.2519/jospt.2005.1583
44. Roi GS, Nanni G, Tencone F. Time to return to professional soccer matches after ACL recon-struction. Sport Sci Health. 2006;1:142-145.
http://dx.doi.org/10.1007/s11332-006-0025-8 45. Rosch D, Hodgson R, Peterson TL, et al. Assess-
ment and evaluation of football performance. Am J Sports Med. 2000;28:S29-S39.
46. Schmidt RA, Lee TD. Motor Control and Learn-ing: A Behavioral Emphasis. 3rd ed. Champaign, IL: Human Kinetics; 1999.
47. Soligard T, Myklebust G, Steffen K, et al. Compre-hensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469.
48. Spencer M, Bishop D, Dawson B, Goodman C. Physiological and metabolic responses of repeated-sprint activities specific to field-based team sports. Sports Med. 2005;35:1025-1044.
49. Stolen T, Chamari K, Castagna C, Wisloff U. Physiology of soccer: an update. Sports Med. 2005;35:501-536.
50. Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1798-1805. http://dx.doi.org/10.1007/s00167-011-1669-8
51. van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation fol-lowing anterior cruciate ligament reconstruc-tion. Knee Surg Sports Traumatol Arthrosc. 2010;18:1128-1144. http://dx.doi.org/10.1007/s00167-009-1027-2
52. Voight M, Cook G. Clinical application of closed kinetic chain exercise. J Sport Rehabil. 1996;5:25-44.
53. Walden M, Hagglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med. 2006;40:158-162. http://dx.doi.org/10.1136/bjsm.2005.021055
54. Walden M, Hagglund M, Magnusson H, Ekstrand J. Anterior cruciate ligament injury in elite foot-ball: a prospective three-cohort study. Knee Surg Sports Traumatol Arthrosc. 2011;19:11-19. http://dx.doi.org/10.1007/s00167-010-1170-9
PUBLISH Your Manuscript in a Journal With International Reach
JOSPT o�ers authors of accepted papers an international audience. The Journal is currently distributed to the members of APTA’s Orthopaedic and Sports Physical Therapy Sections and 22 orthopaedics, manual therapy, and sports groups in 20 countries who provide online access as a member benefit. As a result, the Journal is now distributed monthly to more than 30 000 individuals around the world who specialize in musculoskeletal and sports-related rehabilitation, health, and wellness. In addition, JOSPT reaches students and faculty, physical therapists and physicians at more than 1,400 institutions in 55 countries. Please review our Information for and Instructions to Authors at www.jospt.org and submit your manuscript for peer review at http://mc.manuscriptcentral.com/jospt.
42-04 Bizzini.indd 312 3/21/2012 4:32:39 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 313
[ clinical commentary ]
Although the number of skiing injuries has decreased since the 1970s,10,22,25,33 the incidence of severe ligamentous injuries to the knee, usually involving the anterior cruciate ligament (ACL), has increased.10,22 Deibert et
al10 reported a 280% increase of injuries to the ACL in adults between 1981 and 1994. Florenes et al16 reported as many as 9.8 injuries per 1000 runs in World Cup skiers, 38% of which were to the knee.
Events that were associated with greater speed had higher injury rates. In a study documenting injuries for 25 ski seasons (1980-2005) of the French World Cup team, Pujol et al35 reported 5.7 ACL in-juries per 100 ski seasons. The incidence of reinjury to the same knee was 19%, while the rate of a second injury to either the same or uninjured knee was 39%.35 Overall, injured skiers averaged 2.4 sur-gical procedures. The rate of injury did
TT SYNOPSIS: Alpine skiing is a high-risk sport for injuries to the anterior cruciate ligament (ACL). While descending a hill, a skier must resist large centrifugal forces at a high velocity, while the knees are positioned in postures that place the ACL at risk of injury. Skiers who undergo ACL reconstructive surgery are prone to a high rate of reinjury to the same knee and even ACL injury in the uninjured knee. A rehabilitation program that integrates the best current evidence of ACL reha-bilitation and the science of skiing is essential to a successful return to alpine skiing. Unlike rehabilita-
tion programs developed for court or field athletes, a skiing program must place a large emphasis on slow eccentric-loading and weight-bearing (closed-chain) power and endurance. The purpose of this clinical commentary is to provide the rehabilitation specialist such a program directed toward safely returning the athlete to alpine skiing.
TT LEVEL OF EVIDENCE: Therapy, level 5. J Orthop Sports Phys Ther 2012;42(4):313-325. doi:10.2519/jospt.2012.4024
TT KEY WORDS: ACL, skiing injury, winter sports
1Director and Physical Therapist, Howard Head Sports Medicine, Denver, CO; Doctor of Physical Therapy Student, Rocky Mountain University, Provo, UT. 2Physical Therapist, Howard Head Sports Medicine, Vail, CO. Address correspondence to Dr Dirk Kokmeyer, Howard Head Sports Medicine, 999 18th St, Suite 250, Denver, CO 80202. E-mail: [email protected]
DIRK KOKMEYER, PT, SCS, COMT1 • MICHAEL WAHOFF, PT, SCS, OCS2 • MATT MYMERN, PT, DPT, SCS, CSCS2
Suggestions From the Field for Return-to-Sport Rehabilitation
Following Anterior Cruciate Ligament Reconstruction: Alpine Skiing
not fluctuate during this time.35 High in-jury rates have also been reported in ski patrollers, instructors,44 and recreational skiers.18 Although gender differences have not been demonstrated in professional44 and elite35 skiers, there is evidence that female recreational skiers are more prone to ACL injuries.18
Many factors have been associated with the change in injury rates to the knee.25,33 Ski boots, for example, have be-
come stiffer, with an upper cuff that reaches closer to the knee. Changes in ski design allow for easier turning and better grip on the snow, which enable the trans-
fer of torque through the boot to the knee when a skier is off balance. Additionally, conventional ski bindings may not release when the skier is off balance33,42 and/or proper binding settings may not have been maintained.15 The combination of these elements distributes force and torque from the ski to the knee, which creates an ideal scenario for the knee to be injured.33
MECHANISM OF INJURY
Various mechanisms of ACL injury have been described,14,25,33 including the following. (1) A com-
bined valgus–external rotation mecha-nism of injury occurs during a fall, when the skier’s inside edge engages the snow, while the lower leg externally rotates and abducts as the body of the skier contin-ues forward. (2) A boot-induced anterior drawer mechanism of injury occurs when the skier lands from a jump and the tail of the ski makes contact with the snow, forc-ing the ski boot and lower leg anteriorly. (3) A flexion–internal rotation or phan-tom foot mechanism of injury occurs
SUPPLEMENTAL VIDEO ONLINE
42-04 Kokmeyer.indd 313 3/21/2012 4:33:46 PM

314 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]when the skier is facing downhill, while the body weight is placed on the inside edge of the downhill ski and the uphill ski remains unweighted. As the skier falls backward, the tail of the downhill ski digs into the snow as the ski is forced forward, forcing the leg to internally rotate with a hyperflexed knee. This is believed to be the most common mechanism of injury to the ACL in alpine skiing. (4) A hyper-extension–internal rotation mechanism of injury occurs during a forward fall in combination with hyperextension and in-ternal rotation of the knee.
REHABILITATION
Alpine skiing involves coordi-nated muscle activity to stabilize the trunk and lower extremity
while resisting large centrifugal forces at high velocities.21 The demand for greater muscle activity increases as velocity in-creases, turning radius decreases,2,21 and the grade of the slope increases.9 Slow knee and hip joint angular movements during turns equate to high force pro-duction from the quadriceps and gluteal muscles. Rhythm in movement, balance, and speed are essential to the success of an alpine skier.27
Early Rehabilitation ConsiderationsProtecting healing tissue, increasing joint mobility, and normalizing gait are early rehabilitation goals post–ACL recon-struction. In addition to rehabilitation of the surgical leg, cardiovascular condi-tioning and exercises for the noninjured leg, upper body, and core are recom-mended to prevent deconditioning and provide a sense of well-being.39,40 Em-phasis on strong isometric recruitment of the quadriceps muscles is recommended, because strong isometric activity of the rectus femoris during ski turns26 and of the quadriceps during straight skiing9 has been observed. We advocate the use of either neuromuscular electrical stimula-tion or electromyography-based biofeed-back for quadriceps activation, as both have been shown to be useful in restoring
quadriceps function.12,23,26
We divide our functional rehabili-tation into 3 phases: advanced reha-bilitation, sport-specific training, and return-to-sport training.
Advanced RehabilitationThe advanced-rehabilitation phase may begin between 4 and 6 weeks following surgery, after a set of minimum criteria have been met (TABLE 1).39 These criteria include symmetrical/functional passive and active knee extension, normal gait, minimal joint effusion, no episodes of giving way, and 90% of passive knee flex-ion compared to the contralateral knee.
Therapist discretion is advised when determining whether to advance the athlete. The goals of the advanced reha-bilitation phase are to restore muscular strength, improve cardiovascular endur-ance, and optimize neuromuscular con-trol, balance, and proprioception.39
Restoring muscular strength during this phase is started with closed-kinet-ic-chain (CKC) knee flexion exercises, beginning with bilateral knee flexion in standing (squats) and leg-press exercis-es. Weight shifting from side to side may be incorporated to mimic ski turns and increase CKC tolerance on the involved lower extremity. Restoring strength is
TABLE 1Criteria for Progression and Goals
of Rehabilitation Following Anterior Cruciate Ligament Reconstruction
Minimum Criteria to Progress to Advanced Functional Rehabilitation
1. Minimal joint effusion
2. Normal, symmetrical gait
3. Symmetrical and functional quadriceps recruitment
4. No episodes of giving way or apprehension with closed-kinetic-chain activities or activities of daily living
5. Passive range of motion symmetrical/functional extension, flexion to 90% of contralateral side
Goals of Advanced Phase of Rehabilitation (Weeks 4-6)
1. Restore muscular strength in functional range of motion
2. Optimize neuromuscular control/balance/proprioception
3. Optimize core dynamic stability
4. Improve cardiovascular fitness
Minimum Criteria to Progress to Sport-Specific Training Phase
1. Symmetrical double-limb squat held at 60° for 30 seconds
2. Symmetrical single-limb squat to 30° without varus/valgus compensations
Goals of Sport-Specific Training Phase (Weeks 6-16)
1. Pass functional sports test
2. Strength within 85% or greater of contralateral side
3. Improve cardiovascular fitness
Minimum Criteria to Advance to Return-to-Sport Phase
1. Pass functional sports test
2. Thigh girth within 1 cm of contralateral side, measured at 15 cm above patella
3. Cleared by physician: satisfactory exam
Goals of Return-to-Sport Phase (Weeks 16-24)
1. Achieve maximal neuromuscular control, endurance, strength, power, and balance
2. Safely return athlete to full competitive level while protecting reconstructed anterior cruciate ligament graft
42-04 Kokmeyer.indd 314 3/21/2012 4:33:47 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 315
achieved by utilizing linear periodiza-tion principles. Isometric muscle activa-tion is used during early rehabilitation, as previously described, followed by a progression during the advanced phase from endurance strength to maximum strength to functional strength and pow-er. Therefore, the initial weight (resis-tance) is kept low, and sets are increased in repetition or duration rather than in additional weight. The goal is to utilize proper muscle activation without overly fatiguing the athlete. For example, low resistance on a leg press exercise can be achieved by using 50% of the athlete’s body weight and prescribing an endur-ance set of 15 to 20 repetitions.
Using these principles, the athlete is gradually progressed from shallow knee bending to a skier’s tuck position (FIGURE 1). The knee flexion angle may be increased as the athlete’s endurance and strength increase. However, graft healing time should be balanced with the depth of the skier tuck, because squat positions deeper than 60° can increase anterior tibial translation.13
Berg et al3 measured knee joint angles between 86° and 114° from initiation to completion of a giant slalom turn on the outside leg (FIGURE 2). Although the inside leg achieves greater knee and hip joint angles, the outside leg is the main weight-bearing leg during a turn and demonstrates higher muscular activity, as measured with electromyography.3 Mean hip angles range between 107° and
129° for the outside leg.3 A giant slalom turn has been shown to last nearly twice as long as a parallel turn21 and therefore requires slower angular movement and higher-intensity muscle activity for a lon-ger duration.2 Muscular effort can reach greater than 100% of maximum effort during turns while the knee remains in deep flexion.38 This gives the rationale for maintaining specific joint angles during CKC exercises and training for endurance strength rather than maximum strength.
During the advanced phase, neuro-muscular exercises are progressed from the initial phases of the rehabilitation program. In addition to stabilizing the trunk and lower extremity while resist-ing large centrifugal forces at high ve-locities,21 a skier will often face poor visibility due to weather, rough terrain, and variable snow resistance, requiring optimal balance and coordination. A few examples of applicable exercises, listed in order of difficulty, are standing in a skier tuck position on 2 half foam rollers while weight shifting from side to side to mim-ic ski turns and squatting in a skier tuck position on a BOSU ball (BOSU, Canton, OH) and a fit ball (this exercise may not be appropriate until a later phase, based on the athlete’s ability and therapist’s
judgment). The therapist may add per-turbations to these exercises to increase the level of difficulty for the athlete, who is challenged to maintain a tuck position for maximal tolerable durations (FIGURES
3 through 6).Cardiovascular training is continued
from the previous phase; however, in this phase, treadmill walking with a 7° to 12° incline, elliptical trainer, and rower may be initiated. Resistance on a stationary bike is increased to achieve maximum cardiovascular benefit.
We recommend use of a rehabilitative brace throughout the first phase of reha-bilitation. Patients are advised to use this brace during all daily activities outside the clinic, except while using a continu-ous passive motion device or performing a home exercise routine. An off-the-shelf functional brace is recommended dur-ing the advanced rehabilitation phase and during weight-bearing activities. A custom functional knee brace is fitted after thigh girth has returned and is rec-ommended for the first year of recovery during training and skiing.
The ability of rehabilitative bracing to protect the integrity of the graft and decrease the complication rates of hem-arthrosis and postoperative drainage,
FIGURE 1. Skier tuck position.
FIGURE 2. As a skier negotiates a turn, the outside leg is the main weight-bearing leg. The inside leg accepts less weight but experiences greater joint angles.
42-04 Kokmeyer.indd 315 3/21/2012 4:33:49 PM

316 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
swelling, loss of early extension, and pain has been shown in 3 prospective ran-domized controlled trials.6,19,30 Improved mechanical stability, decreased shear stresses, and protection against injury mechanisms have also been shown.4,8,28 In addition to the protective function a brace can offer, neuromuscular and pro-prioceptive benefits have been observed in cutting activities,6 gait,11 and running.43 Though early bracing has not demon-strated the long-term benefit commonly associated with a successful outcome,8,28 protecting the knee against a catastroph-ic fall is intuitive and the development of position sense and neuromuscular control is a factor that contributes to the overall success of rehabilitation.
Sport-Specific TrainingFollowing successful completion of the advanced phase, the sport-specific train-ing phase begins. This phase may begin between 8 and 10 weeks after surgery. During this phase of rehabilitation, ad-vanced sport-cord and plyometric exer-cises are gradually introduced. Minimum requirements for advancement to this phase are holding a symmetrical bilateral
squat position at 60° of knee flexion for 30 seconds and performing a single-leg squat to 30° of knee flexion while main-taining optimal varus/valgus alignment of the knee within the weight-bearing line of the lower extremity. Meeting these criteria is essential, because this phase of rehabilitation will challenge the athlete to perform specific jump-landing tasks that could place the knee in potentially injurious positions if sufficient stability in a single-leg stance is not present.
Excessive dynamic valgus loading of the knee joint has been shown to lead
to ACL injuries.20 Increased hip adduc-tion and femur internal rotation, and decreased hip extensor, abduction, and ex-ternal rotation strength, are factors shown to increase dynamic valgus.34 A combina-tion of plyometric and neuromuscular stabilization exercises is used to instruct the patient in controlling and reducing valgus kinematics during double- and single-leg drop landing.32 Though alpine skiing lacks the explosiveness of other high-risk sports,2,3 a ski turn can increase valgus torques beyond tissue strength if there is inadequate muscle strength and control to stabilize the joint.36 To simulate the dominance of eccentric activity in ski-ing,2,3,9,21 plyometric exercises are adjusted to emphasize the eccentric phase so that the athlete decelerates and absorbs slow-ly, while the amortization and concentric phases remain unchanged.
FIGURE 3. Skier tuck position on 2 half foam rollers. The athlete maintains a tuck position, while performing slow leans from side to side. Timed sets are performed to improve endurance.
FIGURE 4. Skier tuck position on BOSU. The athlete performs a skier’s tuck on a BOSU. The therapist may add perturbations to challenge the athlete.
FIGURE 5. The athlete performs a skier’s tuck on a BOSU against lateral sport-cord resistance to mimic turns.
FIGURE 6. The athlete is challenged to perform timed tucks, with or without perturbations, on a fit ball. Higher-level neuromuscular performance may be tested while maintaining a skier’s tuck position for maximal tolerable durations.
FIGURE 7. The athlete performs double-limb plyometrics on a Shuttle leg press.
42-04 Kokmeyer.indd 316 3/21/2012 4:33:51 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 317
The goals of the sport-specific training phase are to achieve strength values equal to or greater than 85% of the quadriceps and hamstring muscles of the uninvolved extremity and to successfully complete a functional sports test.39
An excellent means of transitioning an athlete to full weight-bearing CKC plyometric exercises is a Shuttle leg-press device (Shuttle Systems Inc, Glacier, WA) (FIGURE 7). This device allows the athlete to begin jump-landing tasks with mini-mal weight. The athlete is started with double-limb exercises. Once the athlete is able to absorb landing with sufficient knee flexion, he/she may be advanced to single-limb drills. Weight may be in-creased if proper form is maintained.
Once the athlete can tolerate CKC ex-ercises with full weight bearing, endur-ance and strength are challenged with double- and single-limb exercises with and without a sport-cord. When the ath-
lete can demonstrate the ability to per-form landing tasks with a stable knee joint, adequate knee valgus/varus align-ment, and force absorption, the athlete can then be advanced to exercises such as sport-cord forward and backward jog-ging and lateral agility exercises, which require the athlete to perform plyometric movements against sport-cord resistance.
Prior to completion of the sport-spe-cific phase of rehabilitation, the referring surgeon will conduct an examination of the knee. Thigh girth is measured at 15 cm above the patella and evaluated for symmetry. A difference of less than 1 cm in girth is considered satisfactory. The athlete is then taken through the Vail Sport Test.
The Vail Sport Test, originally de-scribed by Hagerman and Atkins,34 is a functional assessment to return to alpine skiing and has been used as a criterion to return to sport, as previously described in the literature.1 Since the inception of this test, it has remained unchanged in design but has undergone scoring changes to increase reliability. A recent study of this test on patients post–ACL reconstruction showed excellent intrarater (ICC range,
0.95-1.0) and interrater reliability (ICC = 0.97; SEM, 1.55). The test is currently be-ing evaluated for construct and criterion validity, with comparisons to the single-leg hop test, Y-balance test, and Marx activity scale.17
The Vail Sport Test involves 4 sport-cord exercises (ONLINE VIDEO). Each exer-cise is judged based on form, time, and pain. Cord tension for lateral jumping ex-cursion and stationary jogging distance is adjusted based on the athlete’s height and weight (APPENDIX). A passing score for this test is 46/54 points. However, from our perspective, a competitive-skiing athlete must pass this test with a perfect score (54/54 points) to advance to the return-to-sport phase of rehabilitation.
The Vail Sport Test begins with a test of CKC endurance and strength. The ath-lete is required to perform single-knee squats for 3 minutes (FIGURE 8). The ten-sion of the sport-cord can be adjusted to the length of the lower extremity. A point is scored for every 30 seconds the athlete completes with proper form. Form scor-ing criteria are carefully graded for lock-ing out (fully extending the knee during the test), dynamic valgus, maintaining an upright position of the trunk, and avoid-ing moving the patella past the vertical line of the great toe on the tested side.
FIGURE 8. Vail Sport Test single-knee bend exercise. The athlete performs a single-knee bend against sport-cord resistance between 30° and 60° of knee flexion.
FIGURE 9. Vail Sport Test lateral agility exercise. The athlete performs a lateral bounding movement against cord resistance, while placing emphasis on knee lower-limb absorption and limiting dynamic valgus.
FIGURE 10. Vail Sport Test forward running exercise. The athlete performs a stationary forward-running movement, while placing emphasis on knee lower-limb absorption and limiting dynamic valgus, against sport-cord resistance.
42-04 Kokmeyer.indd 317 3/21/2012 4:33:53 PM

318 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
The lateral agility test assesses the ability of the athlete to accept load and push off the involved leg in a lateral di-rection against sport-cord resistance (FIGURE 9). The movement is plyometric in nature; however, emphasis is placed on the deceleration and amortization phas-es, where at least 30° of knee flexion must be observed before the concentric phase is initiated. This exercise is tested for 90 seconds. Form criteria similar to those of the single-knee bend are used for this test.
The cord-tension boundary used in the lateral agility test is also used for the forward and backward running tests (FIGURES 10 and 11). During these tests, the athlete is required to perform a sta-tionary running movement. The athlete must bound from one foot to the other during the movement, while absorbing forces using knee flexion to 30°. During the forward running test the athlete faces
away from cord tension and during the backward running test the athlete faces cord tension. The athlete must perform each test for 2 minutes using similar form criteria as for the lateral agility and sin-gle-knee bend tests.
Once the athlete passes the functional sports test with an acceptable score, the rehabilitation team releases the athlete to dry-land training with his/her team. The rehabilitation team coordinates with coaches and trainers to reintroduce more demanding exercises in strength and agility. At the sixth to ninth postoperative month, the athlete may return to alpine skiing, according to an interval program designed to reintegrate skiing while re-fraining from exposing the athlete to competitive-level intensity (TABLES 2 and
3). The athlete is progressed from skiing on groomed terrain at a low intensity, without obstacles, to skiing at increased speed and intensity, with the addition of brushes, gates, moguls, aerials, and park and pipe features, based on the events in which the athlete participates (TABLES 2 and 3). The athlete is not advised to leave the ground during skiing for the first year of rehabilitation. Special case-by-case considerations are made for athletes who are required to jump as a part of their ski event, as in freestyle skiing and other downhill events.
There appears to be overwhelming ev-idence in the current literature that does not support the use of functional knee braces when returning to sport.5,7,19,29,31,37 The current position of the US ski team
TABLE 2 Return-to-Ski Program
Each week, the athlete will perform progression 1 on days 1 and 4. Progression 2 is performed on days 6 and 7.
On days 3 and 4, progressions 1 and 2 are performed. Day 2 and day 5 are off-days.
Progression 1: Directed Free Skiing
1. Free skiing, as outlined by level, focusing on basic athletic stance, balance, joint angles, turn shape
2. Free skiing should begin on groomed, flat to moderate terrain
3. Work to achieve even balance on both legs with trust and confidence on both skis
4. Free ski in sections, working up to longer/full-length runs
5. Nonarcing to arcing turns
Progression 2: Drills (Below Are Examples)
1. Skiing to be performed on groomed, flat to mild terrain
2. Sideslipping into smooth stop on fall line
3. Sideslipping into distinctive stop on fall line
4. Sideslipping diagonally across fall line and switching sides
5. Sideslipping to edge-set and carving across fall line
6. Diagonal skiing, carving
7. Diagonal skiing, carving with flattening of ski
8. Sliding turn in natural-stance position
9. Sliding turn in squat position
10. Sliding turn in squat position with squat pumps
11. Single-leg sliding turns, “heel lift” opposite ski
12. Single-leg sliding turns, “cross-hip” opposite ski
13. Sliding short to medium turns with pole plant
14. Sliding short to medium turns without pole plant
15. Turns with 1 leg lifted
16. Turns with 1000-ft stepping (stepping back and forth throughout the turn)
17. Turns with small hops
FIGURE 11. Vail Sport Test backward running exercise. The athlete performs a stationary backward running movement against sport-cord resistance, while placing emphasis on knee lower-limb absorption and limiting dynamic valgus.
42-04 Kokmeyer.indd 318 3/21/2012 4:33:54 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 319
is that the use of functional knee braces is physician dependent. We recommend using a brace for 1 year, after which the decision to continue bracing during skiing is left to the athlete. Although a systematic review of 12 randomized controlled trials performed in 2007 by Wright and Fetzer45 found no evidence that pain, range of motion, graft stability, and protection from subsequent injuries were affected by the use of braces, we re-fer to 2 specific ski studies for support-ing evidence. Kocher et al24 found that nonbraced skiers were 6.4 times more likely to sustain a knee injury, such as a meniscal tear, chondral injury, or medial collateral ligament tear, than unbraced ACL-deficient knees. Sterett et al41 found
that subsequent injuries on ACL-recon-structed knees in professional skiers were 2.74 times more likely to occur on unbraced knees.
Another prevention strategy that should be incorporated into a skier’s return-to-sport program is injury pre-vention training. The Vermont Safety Research group developed a phased pre-vention program to train skiers to rec-ognize and avoid potentially hazardous maneuvers, as previously described, to prevent injury.14 This program was suc-cessful at reducing injuries to the ACL by 62% in professional skiers.14 Although this has not been tested on elite competi-tive skiers, we believe that every preven-tion strategy should be considered, given
the high reinjury rate in this population.35
As the athlete progresses with ski-ing, exercises for strength, power, agil-ity, and neuromuscular stabilization are recommended. However, intensity and frequency should be adjusted to accom-modate the increased load and activity that the athlete must endure while re-turning to skiing.
CONCLUSION
Alpine skiing is a high-risk sport. Reinjury to the ACL or an injury to the other knee after ACL
surgery is not uncommon in competitive skiers, nor are initial injuries in recre-ational and professional skiers. This can be attributed to several factors, including equipment, positions that place extreme forces and torques on the knee, and an extraordinary demand for neuromus-cular control, endurance, strength, and eccentric control in the lower extremity. These factors create a complex set of re-habilitation challenges for the physical therapist to consider when returning a competitive skier to skiing.
The components of a well-designed re-habilitation program for such an athlete should include the following elements. Each leg should have the neuromuscular control to prevent the knee from posi-tions that place the ACL at risk, such as knee valgus, femur internal rotation, and tibia external rotation. Adequate stability, endurance strength, maximum strength, and power are required to withstand the large centrifugal forces that are placed on the outside leg during ski turns. Empha-sis should be placed on eccentric control during CKC exercises. Educating the ath-lete on strategies to avoid positions that have been shown to be injurious to the ACL may be of benefit. Equipment must be maintained and properly adjusted, considering that the ski-and-boot sys-tem transfers large forces and torques to the knee, especially when bindings do not release. The use of functional bracing in skiing appears to be protective of injuries to the ACL and should be considered. Fi-
TABLE 3 Return-to-Ski Program: Levels 1 to 5
Level 1 (Weeks 0-2)
This phase should be supervised by team medical staff or coach.
Focus: progressions 1 and 2 as outlined in TABLE 2
Intensity: 50% of maximal speed
Duration: progress from 1 to 3 hours
Progress to following phase after 2 weeks in the absence of symptoms
Level 2 (Weeks 2-4)
Focus: progressions 1 and 2 as outlined in TABLE 2
Intensity: 75% of maximal speed
Duration: progress from 2 to 4 hours
Progress to following phase after the fourth week in the absence of symptoms
Level 3 (Weeks 4-6)
Focus: slalom and giant slalom drills using brushes
Intensity: 75% to 90% of maximal levels
Duration: progress from 3 to 5 hours
Progress to following phase after the sixth week in the absence of symptoms
Level 4 (Weeks 6-8)
Focus: skiing all 4 disciplines in all conditions
Intensity: 75% to 100% of maximal levels
Duration: progress from 4 to 6 hours
Increase intensity, duration, and frequency as tolerated
Level 5 (Week 8 and Beyond)
Focus: free ski terrain park and half-pipe
Intensity: 50% to 100% of maximal levels, depending on tricks
Duration: progress from 2 to 4 hours, then progress to full ski session with team/coaches
42-04 Kokmeyer.indd 319 3/21/2012 4:33:55 PM

320 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
REFERENCES
1. Beecher M, Garrison JC, Wyland D. Rehabilita-tion following a minimally invasive procedure for the repair of a combined anterior cruciate and posterior cruciate ligament partial rupture in a 15-year-old athlete. J Orthop Sports Phys Ther. 2010;40:297-309. http://dx.doi.org/10.2519/jospt.2010.3162
2. Berg HE, Eiken O. Muscle control in elite alpine skiing. Med Sci Sports Exerc. 1999;31:1065-1067.
3. Berg HE, Eiken O, Tesch PA. Involvement of ec-centric muscle actions in giant slalom racing. Med Sci Sports Exerc. 1995;27:1666-1670.
4. Beynnon BD, Johnson RJ, Fleming BC, et al. The effect of functional knee bracing on the anterior cruciate ligament in the weightbearing and nonweightbearing knee. Am J Sports Med. 1997;25:353-359.
5. Birmingham TB, Bryant DM, Giffin JR, et al. A randomized controlled trial comparing the effectiveness of functional knee brace and neoprene sleeve use after anterior cruci-ate ligament reconstruction. Am J Sports Med. 2008;36:648-655. http://dx.doi.org/10.1177/0363546507311601
6. Branch TP, Hunter R, Donath M. Dynamic EMG analysis of anterior cruciate deficient legs with and without bracing during cutting. Am J Sports Med. 1989;17:35-41.
7. Brandsson S, Faxen E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? A prospec-tive, randomised study with a two-year follow-up. Scand J Med Sci Sports. 2001;11:110-114.
8. Cawley PW, France EP, Paulos LE. The current state of functional knee bracing research. A review of the literature. Am J Sports Med. 1991;19:226-233.
9. Clarys JP, Alewaeters K, Zinzen E. The influence of geographic variations on the muscular activity in selected sports movements. J Electromyogr Kinesiol. 2001;11:451-457.
10. Deibert MC, Aronsson DD, Johnson RJ, Et-tlinger CF, Shealy JE. Skiing injuries in children, adolescents, and adults. J Bone Joint Surg Am. 1998;80:25-32.
11. DeVita P, Lassiter T, Jr., Hortobagyi T, Torry M. Functional knee brace effects during walking in patients with anterior cruciate ligament recon-struction. Am J Sports Med. 1998;26:778-784.
12. Draper V, Ballard L. Electrical stimulation versus electromyographic biofeedback in the recovery of quadriceps femoris muscle function following anterior cruciate ligament surgery. Phys Ther. 1991;71:455-461; discussion 461-464.
13. Escamilla RF. Knee biomechanics of the dy-namic squat exercise. Med Sci Sports Exerc.
2001;33:127-141.14. Ettlinger CF, Johnson RJ, Shealy JE. A method
to help reduce the risk of serious knee sprains incurred in alpine skiing. Am J Sports Med. 1995;23:531-537.
15. Finch CF, Kelsall HL. The effectiveness of ski bindings and their professional adjustment for preventing alpine skiing injuries. Sports Med. 1998;25:407-416.
16. Florenes TW, Nordsletten L, Heir S, Bahr R. Injuries among World Cup ski and snowboard athletes. Scand J Med Sci Sports. 2012;22:58-66. http://dx.doi.org/10.1111/j.1600-0838.2010.01147.x
17. Garrison CJ, Shanley E, Thigpen C, Geary R, Osler M, DelGiorno J. The reliability of the Vail Sport Test as a measure of physical performance following anterior cruciate ligament reconstruc-tion. Int J Sports Phys Ther. 2012;7:20-30.
18. Greenwald RM, Toelcke T. Gender differences in alpine skiing injuries: a profile of the knee injured skier. In: Johnson RJ, Mote CD, Jr., Eke-land A, eds. Skiing Trauma and Safety: Eleventh Volume. Philadelphia, PA: American Society for Testing and Materials; 1997:111-121.
19. Harilainen A, Sandelin J, Vanhanen I, Kivinen A. Knee brace after bone-tendon-bone anterior cruciate ligament reconstruction. Randomized, prospective study with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1997;5:10-13.
20. Hewett TE, Myer GD, Ford KR, et al. Bio-mechanical measures of neuromuscular control and valgus loading of the knee pre-dict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492-501. http://dx.doi.org/10.1177/0363546504269591
21. Hintermeister RA, O’Connor DD, Lange GW, Dill-man CJ, Steadman JR. Muscle activity in wedge, parallel, and giant slalom skiing. Med Sci Sports Exerc. 1997;29:548-553.
22. Johnson RJ, Ettlinger CF, Shealy JE. Skier injury trends—1972 to 1994. In: Johnson RJ, Mote CD, Jr., Ekeland A, eds. Skiing Trauma and Safety: Eleventh Volume. Philadelphia, PA: American Society for Testing and Materials; 1997:37-48.
23. Kim KM, Croy T, Hertel J, Saliba S. Effects of neuromuscular electrical stimulation after ante-rior cruciate ligament reconstruction on quad-riceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther. 2010;40:383-391. http://dx.doi.org/10.2519/jospt.2010.3184
24. Kocher MS, Sterett WI, Briggs KK, Zurakowski D, Steadman JR. Effect of functional bracing on subsequent knee injury in ACL-deficient profes-sional skiers. J Knee Surg. 2003;16:87-92.
25. Koehle MS, Lloyd-Smith R, Taunton JE. Alpine ski injuries and their prevention. Sports Med. 2002;32:785-793.
26. Kroll J, Wakeling JM, Seifert JG, Muller E. Quadriceps muscle function during recre-ational alpine skiing. Med Sci Sports Exerc. 2010;42:1545-1556. http://dx.doi.org/10.1249/MSS.0b013e3181d299cf
27. Loland S. Alpine skiing technique – practical knowledge and scientific analysis. In: Müller E, Lindinger S, Stöggl T, eds. Science and Ski-ing IV. Maidenhead, UK: Meyer & Meyer Sport; 2009:43-57.
28. Martinek V, Friederich NF. [To brace or not to brace? How effective are knee braces in rehabili-tation?]. Orthopade. 1999;28:565-570.
29. McDevitt ER, Taylor DC, Miller MD, et al. Functional bracing after anterior cruciate liga-ment reconstruction: a prospective, random-ized, multicenter study. Am J Sports Med. 2004;32:1887-1892.
30. Moller E, Forssblad M, Hansson L, Wange P, Weidenhielm L. Bracing versus nonbracing in rehabilitation after anterior cruciate ligament reconstruction: a randomized prospective study with 2-year follow-up. Knee Surg Sports Trauma-tol Arthrosc. 2001;9:102-108.
31. Morrissey MC, Drechsler WI, Morrissey D, Knight PR, Armstrong PW, McAuliffe TB. Effects of distally fixated versus nondistally fixated leg extensor resistance training on knee pain in the early period after anterior cruciate ligament reconstruction. Phys Ther. 2002;82:35-43.
32. Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabiliza-tion and balance training on lower extremity bio-mechanics. Am J Sports Med. 2006;34:445-455. http://dx.doi.org/10.1177/0363546505281241
33. Natri A, Beynnon BD, Ettlinger CF, Johnson RJ, Shealy JE. Alpine ski bindings and injuries. Cur-rent findings. Sports Med. 1999;28:35-48.
34. Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechani-cal perspective. J Orthop Sports Phys Ther. 2010;40:42-51. http://dx.doi.org/10.2519/jospt.2010.3337
35. Pujol N, Blanchi MP, Chambat P. The incidence of anterior cruciate ligament injuries among competitive Alpine skiers: a 25-year investiga-tion. Am J Sports Med. 2007;35:1070-1074. http://dx.doi.org/10.1177/0363546507301083
36. Quinn TP, Mote CD, Jr. Prediction of the loading along the leg during snow skiing. J Biomech. 1992;25:609-625.
37. Risberg MA, Holm I, Steen H, Eriksson J, Ekeland A. The effect of knee bracing after anterior cruciate ligament reconstruction. A prospective, randomized study with two years’ follow-up. Am J Sports Med. 1999;27:76-83.
38. Spitzenpfeil P, Huber A, Waibel K. Mechanical load and muscular expenditure in alpine ski racing and implications for safety and material considerations. In: Müller E, Lindinger S, Stöggl T, eds. Science and Skiing IV. Maidenhead, UK: Meyer & Meyer Sport; 2009:479-486.
39. Stalzer S, Atkins J, Hagerman G. Rehabilita-tion principles. In: Feagin JA, Jr., Steadman JR, eds. The Crucial Principles in Care of the Knee. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:203-219.
40. Steadman JR, Forster RS, Silferskiold JP. Rehabilitation of the knee. Clin Sports Med. 1989;8:605-627.
nally, the physical therapist should incor-porate a well-planned interval program to safely return the skier to skiing. t
42-04 Kokmeyer.indd 320 3/21/2012 4:33:56 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 321
@ MORE INFORMATIONWWW.JOSPT.ORG
41. Sterett WI, Briggs KK, Farley T, Steadman JR. Effect of functional bracing on knee injury in skiers with anterior cruciate ligament recon-struction: a prospective cohort study. Am J Sports Med. 2006;34:1581-1585. http://dx.doi.org/10.1177/0363546506289883
42. St-Onge N, Chevalier Y, Hagemeister N, Van De Putte M, De Guise J. Effect of ski binding param-eters on knee biomechanics: a three-dimension-al computational study. Med Sci Sports Exerc.
2004;36:1218-1225. 43. Theoret D, Lamontagne M. Study on three-
dimensional kinematics and electromyography of ACL deficient knee participants wearing a functional knee brace during running. Knee Surg Sports Traumatol Arthrosc. 2006;14:555-563. http://dx.doi.org/10.1007/s00167-006-0072-3
44. Viola RW, Steadman JR, Mair SD, Briggs KK, Sterett WI. Anterior cruciate ligament injury inci-dence among male and female professional al-
pine skiers. Am J Sports Med. 1999;27:792-795.
45. Wright RW, Fetzer GB. Bracing after ACL re-
construction: a systematic review. Clin Orthop
Relat Res. 2007;455:162-168. http://dx.doi.
org/10.1097/BLO.0b013e31802c9360
SPORT TEST: FUNCTIONAL ASSESSMENT, RETURN TO SPORTName: ___________________ Date: _________
MD: ___________________ DX: ___________ Mo. S/P: ________
Total Points: ___/54 (46/54 = passing score; 54/54 = required passing score for skiing athlete)
Single-Leg Squat (goal: 3 minutes)
1. Knee flexion angle between 30° and 60° Yes (1) ___No (0) ___
2. Athlete performs repetitions without dynamic knee valgus (knee valgus: patella falls medial to the great toe)
Yes (1) ___No (0) ___
3. Athlete avoids locking knee during extension Yes (1) ___No (0) ___
4. Athlete avoids patella extending past the toe during knee flexion Yes (1) ___No (0) ___
5. Athlete maintains upright trunk during knee flexion Yes (1) ___No (0) ___
Minute 1 ___ Minute 2 ___ Minute 3 ___Single-leg squat total points: ___/15If the athlete repeats an error on 3 consecutive repetitions after correction, he/she is not eligible to receive a point for that particular standard (within each 1-minute time frame).
Lateral Agility (goal: 90 seconds)
1. Knee flexion angle is 30° or greater during landing Yes (1) ___No (0) ___
2. Athlete performs repetitions without dynamic knee valgus (knee valgus: patella falls medial to the great toe)
Yes (1) ___No (0) ___
3. Athlete performs repetitions within landing boundaries Yes (1) ___No (0) ___
4. Landing phase does not exceed 1 second in duration Yes (1) ___No (0) ___
5. Athlete maintains upright trunk during knee flexion Yes (1) ___No (0) ___
First 30 seconds ___ Second 30 seconds ___ Third 30 seconds ___Lateral agility total points ___/15If the athlete repeats an error on 3 consecutive repetitions after correction, he/she is not eligible to receive a point for that particular standard (within each 30-second time frame).
Forward Running (goal: 2 minutes)
1. Knee flexion angle between 30° and 60° Yes (1) ___No (0) ___
2. Athlete performs repetitions within landing boundaries Yes (1) ___No (0) ___
APPENDIX
42-04 Kokmeyer.indd 321 3/21/2012 4:33:57 PM

322 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
3. Athlete performs repetitions without dynamic knee valgus (knee valgus: patella falls medial to the great toe)
Yes (1) ___No (0) ___
4. Athlete avoids locking knee during extension Yes (1) ___No (0) ___
5. Landing phase does not exceed 1 second in duration Yes (1) ___No (0) ___
6. Athlete maintains upright trunk during knee flexion Yes (1) ___No (0) ___
Minute 1 ___ Minute 2 ___Forward running total points ___/12If the athlete repeats an error on 3 consecutive repetitions after correction, he/she is not eligible to receive a point for that particular standard (within each 1-minute time frame).
Backward Running (goal: 2 minutes)
1. Knee flexion angle between 30° and 60° Yes (1) ___No (0) ___
2. Athlete performs repetitions within landing boundaries Yes (1) ___No (0) ___
3. Athlete performs repetitions without dynamic knee valgus (knee valgus: patella falls medial to the great toe)
Yes (1) ___No (0) ___
4. Athlete avoids locking knee during extension Yes (1) ___No (0) ___
5. Landing phase does not exceed 1 second in duration Yes (1) ___No (0) ___
6. Athlete maintains upright trunk during knee flexion Yes (1) ___No (0) ___
Minute 1 ___ Minute 2 ___Backward running total points ___/12If the athlete repeats an error on 3 consecutive repetitions after correction, he/she is not eligible to receive a point for that particular standard (within each 1-minute time frame).
Single-Knee BendPurpose:• To test single-leg endurance strength and evaluate patellar trackingSupplies:• SportCord (STI, Baton Rouge, LA; black cord)• Goniometer• StopwatchDescription:• The athlete will perform single-knee bends with cord resistance to 60° at a cadence of 1 second up and 1 second down, for a goal of 3 minutes. The
movement is between 30° and 60° of flexion, with the knee never fully straightening past 30° throughout the 3 minutes. To cue the athlete at a depth of 60°, the buttocks can lightly touch the seat of a chair or object. Two fingers are allowed for balance on a chair back.
Setup:1. With a goniometer, measure a 60° knee bend and place a chair in a position to allow the athlete’s buttocks to lightly touch at that depth.2. The athlete places the heel of the foot on the cord at a position so that the D-ring of the handle is aligned with the knee joint line to remove slack
from the cord.3. Tension is set by pulling the cord handle to the waist line and holding it. Having the athlete hook his/her thumb around the pant line is helpful in
maintaining tension on the cord.4. Two fingers of the opposite hand are allowed to lightly touch another chair back for balance.Technique:• The athlete must perform each repetition of a single-knee bend with the following criteria:
1. Knee flexion angle remains between 30° and 60°.2. Athlete performs repetitions without dynamic knee valgus.3. Athlete avoids locking knee during extension.4. Athlete avoids patella extending past the toe during knee flexion.5. Athlete maintains upright trunk during knee flexion.
APPENDIX
42-04 Kokmeyer.indd 322 3/21/2012 4:33:58 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 323
• Cuing should be provided when 1 of the following compensations is noted. If unable to correct, STOP TEST.Scoring:• The 5 technique criteria are evaluated. The athlete is awarded 1 point per minute for each criterion that is satisfied and may achieve
a maximum of 15 points.• Testing is stopped if and when:
- Form: once the subject is unable to complete single-knee bends without compensation, even with cuing.- Pain: the patient has pain greater than 3/10 OR reproduces his/her pain.- Endurance: the athlete fatigues.
Lateral AgilityPurpose:• To test the ability of the leg to accept load (absorb) and push off in a lateral directionSupplies:• SportCord (STI; black cord)• Stopwatch and tapeDescription:• The athlete will hop laterally with cord resistance from their surgical leg, land momentarily on the nonsurgical leg, only to return onto their surgical
leg with the cord pulling them back to the starting position, for a total test time of 90 seconds. Each repetition of 1 second includes exploding later-ally off the surgical side, landing momentarily on the opposite leg, and then returning to the starting position, with emphasis on absorbing by bend-ing at the hip and knee with 30° of knee excursion. Excursion is defined as the amount of absorption from knee flexion at landing to maximum knee flexion.
Setup:1. Place the belt through the SportCord handles and then attach around the waist.2. Attach the other end of the SportCord to the door jamb or a secure post.3. Stand sideways with the involved leg toward the cord attachment.4. Step away laterally until tension is reached where the athlete slightly compensates with leaning and place a line with tape on the lateral aspect of the
involved foot.5. Measure the distance from the greater trochanter to the floor.6. Use this measured distance to place a second tape line parallel to the first.Technique:• The athlete must perform each lateral hop by landing on or inside the first tape line with the involved foot and on or outside the second tape line
with the uninvolved foot. Only 1 foot should be on the ground at the same time, and the athlete must absorb onto the involved side with the following technique criteria:1. Knee flexion is at 30° or greater during landing.2. Athlete performs repetitions without dynamic knee valgus.3. Athlete performs repetitions within landing boundaries.4. Landing phase does not exceed 1 second in duration.5. Patient maintains upright trunk during knee flexion.
• Cuing should be provided when 1 of the following compensations is noted. If unable to correct, STOP TEST.Scoring:• The 5 technique criteria are evaluated. The athlete is awarded 1 point per 30-second interval for each criterion that is satisfied and may achieve a
maximum of 15 points.• Testing is stopped if and when:
- Form: once the subject is unable to complete single-knee bends without compensation, even with cuing.- Pain: the patient has pain greater than 3/10 OR reproduces his/her pain.- Endurance: the athlete fatigues.
Forward RunningPurpose:• To test the ability of the leg to accept load (absorb) and push off in a forward direction.Supplies:• SportCord (STI; black cord)
APPENDIX
42-04 Kokmeyer.indd 323 3/21/2012 4:33:58 PM

324 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
• Stopwatch and tapeDescription:• The athlete will hop back and forth from the nonsurgical leg onto the surgical leg in a “modified” jogging motion. The cord is attached from behind
the athlete to provide a force pulling backward. There is no significant side-to-side motion, but there is more absorption and up-and-down motion re-quired than there would be if performing only a jogging motion. The goal is 2 minutes total. Emphasis is on absorbing by bending at the hip and knee with 30° of knee excursion. Excursion is defined as the amount of absorption from knee flexion at landing to maximum knee flexion.
Setup:1. Place the belt through the SportCord handles and then attach around the waist.2. Attach the other end of the SportCord to the door jamb or a secure post.3. Stand facing away from the cord attachment so it is pulling backward on the athlete.4. Step forward until tension is reached where the athlete slightly compensates by leaning forward and place a line with tape behind the heels. It should
be the same line as the first line on the lateral agility test.Technique:• The athlete must perform the “modified” (modified because it is more about the absorption than actually jogging) jogging motion while staying in
front of the line. Only 1 foot should be on the ground at the same time, and the athlete must absorb onto the involved leg with the following technique criteria:1. Knee flexion is between 30° and 60° during landing.2. Athlete performs repetitions within landing boundaries.3. Athlete performs repetitions without dynamic knee valgus.4. Athlete avoids locking knee during extension.5. Landing phase does not exceed 1 second in duration.6. Patient maintains upright trunk during knee flexion.
• Cuing should be provided when 1 of the following compensations is noted. If unable to correct, STOP TEST.Scoring:• 1 point is awarded for each technique criterion that is satisfied per minute. A total of 12 points may be awarded for this test.• Testing is stopped if and when:
- Form: once the subject is unable to complete single-knee bends without compensation, even with cuing.- Pain: the patient has pain greater than 3/10 OR reproduces his/her pain.- Endurance: the athlete fatigues.
Backward RunningPurpose:• To test the ability of the leg to accept load (absorb) and push off in a backward direction.Supplies:• SportCord (STI; black cord)• Stopwatch and tapeDescription:• The athlete will hop back and forth from the nonsurgical leg onto the surgical leg in a “modified” jogging motion. The cord is attached in front of the
athlete to provide a force pulling forward. There is no significant side-to-side motion, but there is more absorption and up-and-down motion required than there would be if performing only a jogging motion. The goal is 2 minutes total. Emphasis is on absorbing by bending at the hip and knee with 30° of knee excursion. Excursion is defined as the amount of absorption from knee flexion at landing to maximum knee flexion.
Setup:1. Place the belt through the SportCord handles and then attach around the waist.2. Attach the other end of the SportCord to the door jamb or a secure post.3. Stand facing the cord attachment so it is pulling forward on the athlete.4. Step forward until tension is reached where the athlete slightly compensates by leaning backward and place a line with tape in front of the toes. It
should be the same line as the first line on the lateral agility test.Technique:• The athlete must perform the “modified” (modified because it is more about the absorption than actually jogging) jogging motion while staying in
front of the line. Only 1 foot should be on the ground at the same time, and the athlete must absorb onto the involved leg with the following criteria:1. Knee flexion is between 30° and 60° during landing.2. Athlete performs repetitions within landing boundaries.
APPENDIX
42-04 Kokmeyer.indd 324 3/21/2012 4:33:59 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 325
3. Athlete performs repetitions without dynamic knee valgus.4. Athlete avoids locking knee during extension.5. Landing phase does not exceed 1 second in duration.6. Patient maintains upright trunk during knee flexion.
• Cuing should be provided when 1 of the following compensations is noted. If unable to correct, STOP TEST.Scoring:• 1 point is awarded for each technique criterion that is satisfied per minute. A total of 12 points may be awarded for this test.• Testing is stopped if and when:
- Form: once the subject is unable to complete single-knee bends without compensation, even with cuing.- Pain: the patient has pain greater than 3/10 OR reproduces his/her pain.- Endurance: the athlete fatigues.
Copyright © 2007 Rehabilitation and Performance Center at Vail.
APPENDIX
BROWSE Collections of Articles on JOSPT’s Website
The Journal’s website (www.jospt.org) sorts published articles into more than 50 distinct clinical collections, which can be used as convenient entry points to clinical content by region of the body, sport, and other categories such as di�erential diagnosis and exercise or muscle physiology. In each collection, articles are cited in reverse chronological order, with the most recent first.
In addition, JOSPT o�ers easy online access to special issues and features, including a series on clinical practice guidelines that are linked to the International Classification of Functioning, Disability and Health. Please see “Special Issues & Features” in the right-hand column of the Journal website’s home page.
42-04 Kokmeyer.indd 325 3/21/2012 4:34:00 PM

326 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
Most anterior cruciate ligament (ACL) injuries in basketball are noncontact in nature. The typical mechanisms of ACL tears in basketball include forced excessive valgus stress at the knee, excessive femoral
internal rotation on the tibia, excessive anterior translation of the tibia on the femur, or a combination of the above. As most ACL injuries in basketball occur from a planting, decelerating, pivoting moment
or landing from a vertical leap, the re-habilitation protocol should prepare the player to avoid these risk-associated positions by addressing proper landing mechanics, hip abduction strengthening, cocontraction of the quadriceps and ham-strings for joint stiffness, balance, and proper trunk and knee flexion. Only after
TT SYNOPSIS: The purpose of this paper is to outline the final, functional phases of rehabilitation that address exercises, drills, and return-to-play criteria for the sport of basketball, following ante-rior cruciate ligament (ACL) reconstruction. ACL injuries can be debilitating and affect the quality of life for recreational and elite athletes alike. Tears of the ACL are common in both male and female basketball players, with a higher incidence rate in females. Incidence of a retear to the existing graft or contralateral knee within 5 years of ACL reconstruction with patellar tendon autograft in young (less than 18 to 25 years of age), ac-tive basketball players can be as high as 52%. Reducing the number of ACL injuries or reinjury, of which there are an estimated 80 000 per year
at an associated cost of over a billion dollars, can have significant potential long-term fiscal and health benefits. Following surgical reconstruction of the ACL, implementing a tailored rehabilitation protocol can ensure a successful return to sport. When searching the literature for such protocols, clinicians may struggle to find specific exercises, drills, and return-to-play criteria for particular sports. The intent of this manuscript is to present such a rehabilitation protocol for basketball.
TT LEVEL OF EVIDENCE: Therapy, level 5. J Orthop Sports Phys Ther 2012;42(4):326-336. doi:10.2519/jospt.2012.4030
TT KEY WORDS: ACL, functional rehabilitation, injury, jumping, landing, NBA
1Head Athletic Trainer, Washington Wizards Basketball Club (NBA), Washington, DC. Address correspondence to Mr Eric Waters, Washington Wizards, Sports Medicine, 601 F St NW, Wizards Athletic Training Room, Washington, DC 20004. E-mail: [email protected]
ERIC WATERS, MS, ATC/L, CES, CSCS1
Suggestions From the Field for Return to Sports Participation
Following Anterior Cruciate Ligament Reconstruction: Basketball
these impairments are addressed can the final, functional return phase begin. This final phase of the protocol must seek to challenge the basketball athlete by mim-icking the demands of the sport, which include single-leg jumping, landing, and other deceleration skills executed while dribbling, passing, and rebounding a bas-
ketball or reacting to an offensive player. Once the player satisfies the criteria for each phase and meets the return-to-play crite-ria (APPENDICES A and B), she/he
may begin practice, initially with restric-tions, before returning to play without restriction.
There is scant literature addressing rehabilitation protocols, exercise pro-gressions, and return-to-play criteria specifically for basketball athletes (partic-ularly males) following ACL reconstruc-tion. The goal of this article is to address the current deficiency of the rehabilita-tion literature by providing a framework of functional drills and return-to-play criteria specific to the basketball athlete (high school to elite level) recovering from ACL reconstruction surgery.
FUNCTIONAL REHABILITATION PHASES
Progression criteria and the outline for rehabilitation of the bas-ketball athlete following ACL recon-
struction include 3 phases (APPENDICES
A and B). Phase 1 addresses immediate postsurgical needs, from wound care to the initiation of range of motion (ROM) and general strength acquisition. Phase 2 provides a platform for gaining full ROM
SUPPLEMENTAL VIDEO ONLINE
42-04 Waters.indd 326 3/21/2012 4:35:01 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 327
and strength, while providing a base for neuromuscular coordination and endur-ance exercises. Phase 3 seeks to progress the athlete from the beginning of func-tional work at the end of phase 2 to final return to play through higher-intensity functional rehabilitation.
Phase 1The first phase of most rehabilitation programs following ACL reconstruction focuses on similar goals, without much sport specificity.7,22 These goals focus on ROM and strength gains, return to nor-mal ambulation, performance of trunk/hip strengthening and simple ground-based balance exercises, and cardiovas-cular work. Light sport-specific work may be included during the latter stages of this phase (stationary drills such as sta-tionary ball handling, passing, and free-throw and spot shooting). This article
will concentrate on the functional aspect of rehabilitation found in phases 2 and 3.
Phase 2During phase 2, initiated approximately 10 to 13 weeks postsurgery or when the progression criteria are met (APPENDIX A), the goals of phase 1 are continued, with ROM gains, lower extremity strengthen-ing, and low-intensity agility/neuromus-cular drills as the primary goals.9,20,22,25 Phase 2 functional strengthening and neuromuscular enhancement, in prepa-ration for phase 3 power and basket-ball-specific work, may be completed concurrently. It consists of exercises de-
signed to develop strength through func-tional movements and power and force attenuation skills from low-intensity jumping and landing drills.18
Functional Strength Functional strength enhancement is accomplished with weight-bearing (closed-kinetic-chain) exercises, progressively increasing the amount of weight the athlete can move, while concurrently maintaining proper lower extremity alignment.8 The role of the rehabilitation clinician is to construct exercises that address existing deficits and to provide feedback to the patient that will allow the patient to maintain suitable alignment during the exercis-es.13,26 Following the restoration of base-line bilateral lower extremity strength, as achieved in phase 1 by exercises such as squats (single-leg and double-leg), rota-tional squats (FIGURES 1 and 2), wall slide, leg presses, and hamstring curls, pro-gression to the functional strengthening aspect of ACL rehabilitation can begin.36 The single-leg squat exercise is a basic but vital form of functional strength en-hancement.8,20,26,29 It requires the patient to effectively transmit loads through the lower extremity to the ground, to create the most linear and stable vector move-ment. This is critical for the basketball athlete, particularly during the initiation of a drive to the basket or leaping verti-
FIGURE 1. Rotational squat, starting position.
FIGURE 2. Rotational squat, finishing position.
FIGURE 3. Split squat on foam pad with dribbling.
FIGURE 4. Double-leg tilt board squat with dribble.
FIGURE 5. Double-leg BOSU ball squat with dribble.
42-04 Waters.indd 327 3/21/2012 4:35:03 PM

328 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
cally for a layup. The initial functional strength exercises, such as the single-leg squat, rotational squat (FIGURES 1 and 2), split squat (FIGURE 3), and low-level dou-ble-leg and single-leg hopping and land-ing (FIGURE 11, ONLINE VIDEOS 1 through 4), are designed to effectively integrate all movements while enhancing strength and joint stiffness.Neuromuscular Enhancement Drills In
addition to initial power, strength, and ROM gains, acquisition of balance, kin-esthetic awareness, and neuromuscu-lar coordination is a critical goal of this phase. Balance training on perturbation devices, such as BOSU (BOSU, Canton, OH), tilt board, and foam pads, is intro-duced (FIGURES 3 through 10). In addition, low-intensity jumping and landing drills (both double- and single-leg) (FIGURE 11, ONLINE VIDEOS 1 and 2), cutting drills, and lateral-movement drills while catching, dribbling, and passing a basketball may
be implemented (FIGURES 12 through 14, ONLINE VIDEOS 3 through 5). Elastic resis-tance may be added to challenge bal-ance and increase cocontraction and joint stiffness of the lower extremity. Basketball shooting and passing drills with low-intensity movement may also be introduced at this stage. These exer-cises lead to early-stage re-education of the neuromuscular mechanisms that pro-mote dynamic knee stability.26,31,34 Proper posture upon landing should include pel-vic stability, trunk flexion, and knee flex-
FIGURE 6. Single-leg squat on tilt board with dribble.
FIGURE 7. Double-leg squat on BOSU, with ball catching and passing.
FIGURE 8. Single-leg squat on BOSU, with ball catching and passing.
FIGURE 9. Double-leg ball catches on a tilt board, while clinician provides external perturbations.
FIGURE 10. Single-leg ball catches on a tilt board, while clinician provides external perturbations.
FIGURE 11. Single-leg hop drill with elastic resistance. Player hops in the direction commanded by the clinician, while holding posture and lower-body alignment.
FIGURE 12. Crab dribble drill with elastic resistance. Player slides back and forth between 2 points while dribbling.
FIGURE 13. Defensive slides with elastic resistance. The player executes defensive slides around an arc, while maintaining posture and distance from clinician.
42-04 Waters.indd 328 3/21/2012 4:35:06 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 329
ion without frontal or transverse plane movements at the knee.8,14,23,26 To achieve proper lower extremity alignment dur-ing drills, the clinician may be creative in introducing these types of exercises; however, vigilance must be maintained in providing feedback for the athlete should she/he begin to lose proper pelvic and lower extremity alignment. Use of video (ONLINE VIDEOS 1 and 2) is especially help-ful to provide feedback on all functional exercises being introduced, particularly in landing drills.
The idea of phase 2 as a staging phase
for phase 3 is highlighted by the intro-duction of low-intensity neuromuscu-lar training, movement mechanics, and functional drills that will be carried over to phase 3 at higher intensities. Strength, power and ROM work, cardiovascular training, and core strengthening and sta-bility are also continued in phase 3.
Phase 3This final phase should include a func-tional-rehabilitation progression that ad-dresses the most demanding components of basketball. This phase is divided into 3 elements that should be executed con-currently: continued muscular strength, power, and endurance enhancement; basketball agility drills; and return to basketball play criteria and progression (APPENDIX B).33
Muscular Strength, Power, and Endur-ance Enhancement To enter phase 3, it is imperative that athletes meet the cri-teria that permit them to successfully execute the higher-intensity work. This includes proper gait mechanics,11 ad-equate concentric and eccentric strength
(measured by isokinetic testing),37 power production, cutting and landing skills (single-leg and double-leg), and mus-cular and cardiovascular endurance (APPENDIX B).12,17,33,37 Working on power production has the added benefit of en-hancing both muscular endurance and strength.4,7 Low-impact single-leg and double-leg plyometric exercises, such as lateral hops (with or without resistance) (FIGURE 11), single-leg lateral hops while dribbling or catching (ONLINE VIDEOS 6 and 7), and box jumps, are initiated. Exam-ples of advanced power-based exercises that address muscular strength, power, and endurance include single-leg and double-leg tuck jumps, repeat vertical box jumps (30-cm and 45-cm boxes), split-squat scissor jumps, and single-leg hops with 90°/180° turns while catching and passing a basketball (ONLINE VIDEOS 8 and 9). These exercises address proper creation and dissipation of force and effi-ciency of movement without lateral pelvic excursion or poor lower extremity align-ment. Basketball passes and catches may be added to these exercises to increase
FIGURE 14. Close-out drill. With elastic resistance added to aid in increasing eccentric load, the player accelerates to and decelerates to close out on an offensive player in a controlled manner.
FIGURE 15. Low-post drill. Player with ball attempts to score in the low-post area while being resisted. Player may switch roles to be the resistance provider.
FIGURE 16. Zigzag drill. Sprint into a diagonal cut at 45° around each cone, with or without dribbling a basketball.
42-04 Waters.indd 329 3/21/2012 4:35:08 PM

330 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]difficulty and reflect game situations that require reaction.Basketball-Specific Agility Drills Once the athlete meets the progression crite-ria (APPENDIX B), the athlete may progress to movement in all planes at different speeds, provided there is gradual in-crease in the intensity and difficulty of the movements prior to performing full-speed running, cutting, jumping, and landing. Developing agility requires that the patient relearn intricate footwork and movement patterns that challenge the neuromuscular and proprioceptive systems.2,10 Basketball-specific move-ment drills may be divided into skill drills, reactive drills, contact drills, and a combination of each of these. These ex-ercises must include not only proactive movement patterns and skills, such as initiating a sprint to the basket to score, but also reactive-movement sequences, which include moving laterally while dribbling (FIGURE 12, ONLINE VIDEO 13), de-fending an opposing player (FIGURE 13, ON-
LINE VIDEO 14), or “closing out,” in which a defensive player sprints to an offensive player to defend a shot or drive to the basket (FIGURE 14, ONLINE VIDEO 15). Dif-ferent players (guard, forward, center) require drills specific to their positions. Increasing the area over which the drill is performed, decreasing the rest peri-ods, adding ball handling, passing, and catching, and increasing the speed and intensity of the movements and cuts can increase the difficulty of the task and provide a progression component to this portion of the rehabilitation. Once these skills are relearned and the involved lower extremity is symmetrical in function and alignment to the unin-volved limb at high speed and effort, the athlete can safely begin high-intensity basketball-type activities, such as defen-sive and offensive drills, contact drills, and shooting drills, during practice (FIG-
URE 15). This is followed by return-to-play testing.20,31
The zigzag drill (FIGURE 16, ONLINE VIDEO 16) is designed to address acceleration and deceleration associated with the lat-
Backpedal Sprint
FIGURE 17. Sprint-backpedal drill. Accelerate to the cone, decelerate, backpedal to the baseline, and repeat, with or without dribbling a basketball.
Defensive slide
Defensive slide
Backpedal Sprint
FIGURE 18. Box drill. The patient must continuously move around the basketball lane in the manner shown. The clinician may call for a change in direction (counter versus clockwise) at any time.
42-04 Waters.indd 330 3/21/2012 4:35:09 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 331
eral cuts or V-cuts that are commonly performed by all basketball players. Ac-celerating to a sprint forward, the player reaches a cone and takes a 45°-angle cut, accelerates for a few steps, takes another 45° cut back through the cones, and con-tinues this through several more cones. Adding ball handling to this drill, with right- and left-hand crossover dribbles or catching and throwing passes at the cut points, is effective in adding difficulty.
The sprint-backpedal drill (FIGURE
17, ONLINE VIDEO 17) adds deceleration to a backpedal component. Closing out or accelerating to an opponent and then decelerating as the player reaches the opponent is an important skill to regain. In this drill, the player sprints to a cone at a 30° to 45° angle, stops at the cone, then backpedals at an opposite 30° to 45° angle to the start line, and continues on for as many cones as desired.
The box drill (FIGURE 18) uses the basketball lane area as a template. The player sprints forward along the lane and decelerates at the free-throw line, where a lateral defensive slide begins to the oppo-site side of the lane, before backpedaling to the baseline. This is done repeatedly, with the direction changed on command from the clinician. Forwards and centers may be asked to touch the backboard each time they reach the baseline, and guards and forwards may be asked to pass-catch or dribble through the entirety of the drill.
The star drill (FIGURE 19, ONLINE VIDEO 18) is a reaction drill that focuses on the player’s ability to react to a verbal com-mand to change direction of movement. A series of cones or spots are numbered 1 through 4 (or more). The player is placed in the middle of these cones. Once a num-ber is called out, the player must sprint, with or without dribbling a basketball, to that number, then return to the original position, and the exercise is repeated.
In the ball chase drill (FIGURE 20, ONLINE
VIDEO 19), starting in any spot on the court, the clinician holds 2 basketballs while facing the player. The clinician throws 1 ball anywhere on the court. The player
Start
4
1 2
3
FIGURE 19. Star drill. The clinician calls out a number, the patient must run to that number and back to the starting point, where a new number is called out for the patient to run to. Basketball dribbling may be added for functionality.
Player
Clinician
FIGURE 20. Ball chase drill. The clinician uses 2 balls, tossing one in a random area of the half court. As the player moves as quickly as possible to retrieve the first ball, the clinician tosses the second ball to another random area for the patient to retrieve. This can be done with as many repetitions as desired.
42-04 Waters.indd 331 3/21/2012 4:35:10 PM

332 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]must sprint to the ball and either dribble it to or pass it to the clinician. Just before the clinician receives the ball, the clini-cian throws the other ball to another spot on the floor, challenging the reactivity of the player to visual cues. To increase the difficulty, the player can be asked to drib-ble the ball to a predetermined spot and shoot the ball. As she/he shoots the ball, another ball is thrown somewhere else on the court of play, continuing the drill.
Contact in basketball may also lead to ACL injury.1,3 Therefore, it is crucial, physically as well as mentally, that a con-tact component is added to the program prior to the return to sport. Designed for guards and forwards, the gauntlet drill (FIGURE 21) focuses on the contact a player will make in driving through the lane during play. Several clinicians, coaches, or players line up on each side of the predetermined lane to the basket. Each holds a common handheld basket-ball pad. As the player drives to the bas-ket, clinicians (or assistants) are asked to lightly tap the player with the pad as the player dribbles through the lane. The speed of the player and heaviness of con-tact may increase over time, provided it is done in a controlled manner.
The low-post drill (FIGURE 15, ONLINE
VIDEO 20) utilizes a coach, player, or clini-cian to provide resistance to the back of the low-post player (a forward or center) as the player turns and makes a low-post move. These players often play with their back to the basket and close to the bas-ket, and are often resisted in their efforts to go to the basket. Providing resistance and attempting to push them off balance helps them regain those skills. The player is also asked to play the defensive portion of this drill to react and resist the move-ment of the opposing player. The clinician should look for the player’s willingness to play in a protected position, with knees and trunk flexed while exhibiting pelvic stability.18,23
Landing off balance after being pushed while in the air is a common mechanism of ACL injury in basketball. The leap-contact drill (ONLINE VIDEOS 21
and 22) is intended to re-establish confi-dence in the athlete’s ability to land with proper lower extremity mechanics. The player is asked to jump from the ground or a 30-cm box and, while in the air, is tapped by the clinician to push the player off the line of landing. The player is ex-pected to land in a protected position (knees and trunk flexed with no valgus alignment at the knees) on both feet.26 Progressions include landing on 1 foot and adding jogging prior to the jump.
These contact drills must be done in a controlled manner and only in the fi-nal phases of the ACL rehabilitation pro-gram. This drill should precede return to full-contact practice situations.Return-to-Basketball Criteria and Pro-gression When making the decision to return to basketball-specific sports par-ticipation following ACL reconstruction, very few evidence-based criteria exist.21,32 Typically, once the player is cleared in terms of objective criteria (APPENDICES
A and B), the player is allowed to start practice activities that are noncontact (shell drills, shooting drills, defensive
drills, offensive sets), while the intensity of the activity is gradually elevated. Con-tact drills are allowed when the player is able to go through noncontact drills at full speed, without pain or swelling and with full confidence. It is important to note that gaining the compliance of the coaching staff is helpful in structuring the return to full practice participation. The clinician and basketball player face many challenges in determining the right time to return to play.7 The psychological com-ponent must also be considered,6,35 as the player must feel confident in his/her abil-ity.6 The team personnel (team psycholo-gist, physical therapist, athletic trainer, and coaching staff) may play an impor-tant role in gaining this perspective.
Cardiovascular fitness is an important factor in the return-to-play scenario. Ze-bis et al38 noted that acute fatigue can lead to compromised neuromuscular activity in professional handball players. Cardiovascular fitness testing (of both the aerobic and anaerobic systems) is neces-sary for a safe return to play.33 The final stages of return to play are highlighted by
Player
Clinician
Clinician
Clinician
Clinician
FIGURE 21. Gauntlet drill. As the player dribbles the basketball down the lane, the clinicians gently tap the player with pads to resensitize the player to contact they are accustomed to within the lane.
42-04 Waters.indd 332 3/21/2012 4:35:11 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 333
controlling practice time by monitoring heart rate, recovery, tracking body mass index, and other parameters that are be-yond the scope of this article.12 Once the player, clinician, and coaching staff feel that there has been adequate recovery between bouts of practice (water breaks, free-throws, timeouts) for an entire prac-tice session, it is inferred that the player is capable of returning to full practices without limitations.
Once all criteria are met, the player may return to competitive basketball. At the elite level (professional and colle-giate), monitoring player minutes during competition has been shown to be use-ful in avoiding excessive fatigue. Minute allocations should be decided by con-sensus of the player,19 physician, physi-cal therapist, athletic trainer, and coach. According to the National Basketball As-sociation’s injury surveillance from 1998 to 2011, 74% of all ACL injuries occurred during in-game competition. Because game situations provide the most expo-sure, monitoring player minutes may prevent fatigue38 and allow some control over reinjury.
Gender ConsiderationsIt is reported that female basketball players sustain ACL injuries 3.5 to 9 times more frequently than male play-ers.1,3,5,13,24,30 Despite the great difference in injury rates between these 2 groups, the underlying tenets of sound move-ment mechanics (landing with less ground reaction force; greater flexion angles at the hip, knee, and ankle; and reduced valgus moment at the knee, etc) must be achieved in the rehabilitation protocol.24,27,28 Due to the anatomical, neuromuscular, and strength differences between female and male athletes, time-lines for return to play may be expanded for female athletes.13-16,36 Therefore, when retraining basketball athletes following ACL reconstruction, it is valuable to not only restore preinjury cutting, jump-ing, and landing capabilities but also to enhance them.11,18 This goal can be met equally for both men and women, pro-
vided their existing deficits in neuromus-cular firing patterns, strength, and body position are identified by the clinician and corrected.26,29,31
CONCLUSION
Functional rehabilitation fol-lowing ACL reconstruction sur-gery for a basketball athlete poses
a unique challenge for the athlete and the physical therapist. The amount of high-speed cutting, pivoting, and, most notably, explosive jumping (and landing) from full sprints may place the athlete in compromising positions. Preparing a basketball player for an effective return to play requires that the final and most functional phase of the rehabilitation program encompass a thorough protocol based on exercises that maintain proper lower extremity alignment throughout all the conceivable scenarios of a basketball game. To achieve this goal, a successful rehabilitation program must take into account these unique movements, fitness level, player positions, and even gender.32 It should also contain basketball-related exercises and progressions that spe-cifically address these movements. Ex-amples include drills that challenge the player in different phases of the game of basketball, such as dribbling, passing, and catching a ball while running, cut-ting, and jumping, as well as reacting to ball and player movement. It is the role of the clinician to provide these unique challenges during the functional aspect of the rehabilitation process and to sup-ply feedback to the player to ensure that proper lower-body strength, power, and stability are achieved for a successful re-turn to play. t
REFERENCES
1. Agel J, Arendt EA, Bershadsky B. Anterior cruci-ate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33:524-530. http://dx.doi.org/10.1177/0363546504269937
2. Alentorn-Geli E, Myer GD, Silvers HJ, et al.
Prevention of non-contact anterior cruciate liga-ment injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17:859-879. http://dx.doi.org/10.1007/s00167-009-0823-z
3. Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694-701.
4. Augustsson J, Thomeé R, Karlsson J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruc-tion. Knee Surg Sports Traumatol Arthrosc. 2004;12:350-356. http://dx.doi.org/10.1007/s00167-004-0518-4
5. Barber-Westin SD, Noyes FR, Smith ST, Camp-bell TM. Reducing the risk of noncontact anterior cruciate ligament injuries in the female athlete. Phys Sportsmed. 2009;37:49-61. http://dx.doi.org/10.3810/psm.2009.10.1729
6. Bauman J. Returning to play: the mind does matter. Clin J Sport Med. 2005;15:432-435.
7. Beynnon BD, Uh BS, Johnson RJ, et al. Re-habilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs adminis-tered over 2 different time intervals. Am J Sports Med. 2005;33:347-359.
8. Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18:520-527.
9. Chmielewski TL. Asymmetrical lower extremity loading after ACL reconstruction: more than meets the eye. J Orthop Sports Phys Ther. 2011;41:374-376. http://dx.doi.org/10.2519/jospt.2011.0104
10. Cimino F, Volk BS, Setter D. Anterior cruciate ligament injury: diagnosis, management, and prevention. Am Fam Physician. 2010;82:917-922.
11. DeVita P, Hortobagyi T, Barrier J. Gait bio-mechanics are not normal after anterior cruciate ligament reconstruction and acceler-ated rehabilitation. Med Sci Sports Exerc. 1998;30:1481-1488.
12. Drinkwater EJ, Pyne DB, McKenna MJ. Design and interpretation of anthropometric and fit-ness testing of basketball players. Sports Med. 2008;38:565-578.
13. Dwyer MK, Boudreau SN, Mattacola CG, Uhl TL, Lattermann C. Comparison of lower ex-tremity kinematics and hip muscle activation during rehabilitation tasks between sexes. J Athl Train. 2010;45:181-190. http://dx.doi.org/10.4085/1062-6050-45.2.181
14. Fagenbaum R, Darling WG. Jump landing strate-gies in male and female college athletes and the implications of such strategies for anterior cruciate ligament injury. Am J Sports Med. 2003;31:233-240.
15. Giugliano DN, Solomon JL. ACL tears in fe-male athletes. Phys Med Rehabil Clin N Am. 2007;18:417-438. http://dx.doi.org/10.1016/j.pmr.2007.05.002
42-04 Waters.indd 333 3/21/2012 4:35:12 PM

334 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
@ MORE INFORMATIONWWW.JOSPT.ORG
16. Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and ham-string graft: a prospective clinical investiga-tion. Knee Surg Sports Traumatol Arthrosc. 2006;14:1021-1028. http://dx.doi.org/10.1007/s00167-006-0050-9
17. Gocentas A, Juozulynas A, Obelenis V, Andziulis A, Landor A. Patterns of cardiovascular and ventilatory response to maximal cardiopulmo-nary test in elite basketball players. Medicina (Kaunas). 2005;41:698-704.
18. Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141-150.
19. Manzi V, D’Ottavio S, Impellizzeri FM, Cha-ouachi A, Chamari K, Castagna C. Profile of weekly training load in elite male profes-sional basketball players. J Strength Cond Res. 2010;24:1399-1406. http://dx.doi.org/10.1519/JSC.0b013e3181d7552a
20. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progres-sion through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385-402. http://dx.doi.org/10.2519/jospt.2006.2222
21. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377-387. http://dx.doi.org/10.2519/jospt.2011.3547
22. Neeter C, Gustavsson A, Thomeé P, Augusts-son J, Thomeé R, Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Trauma-tol Arthrosc. 2006;14:571-580. http://dx.doi.org/10.1007/s00167-006-0040-y
23. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Jr., Beutler AI. The Landing Error Scoring System (LESS) is a valid and reli-
able clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009;37:1996-2002. http://dx.doi.org/10.1177/0363546509343200
24. Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Or-thop Sports Phys Ther. 2011;41:553-559. http://dx.doi.org/10.2519/jospt.2011.3591
25. Pezzullo DJ, Fadale P. Current controversies in rehabilitation after anterior cruciate liga-ment reconstruction. Sports Med Arthrosc. 2010;18:43-47. http://dx.doi.org/10.1097/JSA.0b013e3181cdb5d3
26. Podraza JT, White SC. Effect of knee flexion angle on ground reaction forces, knee moments and muscle co-contraction during an impact-like deceleration landing: implications for the non-contact mechanism of ACL injury. Knee. 2010;17:291-295. http://dx.doi.org/10.1016/j.knee.2010.02.013
27. Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechani-cal perspective. J Orthop Sports Phys Ther. 2010;40:42-51. http://dx.doi.org/10.2519/jospt.2010.3337
28. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Ar-throscopy. 2007;23:1320-1325.e6. http://dx.doi.org/10.1016/j.arthro.2007.07.003
29. Quatman CE, Quatman-Yates CC, Hewett TE. A ‘plane’ explanation of anterior cruciate liga-ment injury mechanisms: a systematic review. Sports Med. 2010;40:729-746. http://dx.doi.org/10.2165/11534950-000000000-00000
30. Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an Inter-national Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394-412. http://dx.doi.org/10.1136/bjsm.2008.048934
31. Risberg MA, Mork M, Jenssen HK, Holm I. De-
sign and implementation of a neuromuscular training program following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2001;31:620-631.
32. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruc-tion with patellar tendon autograft. Am J Sports Med. 2009;37:246-251. http://dx.doi.org/10.1177/0363546508325665
33. Thomas AC, McLean SG, Palmieri-Smith RM. Quadriceps and hamstrings fatigue alters hip and knee mechanics. J Appl Biomech. 2010;26:159-170.
34. Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM. Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:2-14. http://dx.doi.org/10.1007/s00167-007-0427-4
35. Weiss MR. Psychological aspects of sport-injury rehabilitation: a developmental perspective. J Athl Train. 2003;38:172-175.
36. Wilk KE, Arrigo C, Andrews JR, Clancy WG. Rehabilitation after anterior cruciate ligament reconstruction in the female athlete. J Athl Train. 1999;34:177-193.
37. Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60-73.
38. Zebis MK, Bencke J, Andersen LL, et al. Acute fatigue impairs neuromuscular activity of anterior cruciate ligament-agonist muscles in female team handball players. Scand J Med Sci Sports. 2010;21:833-840. http://dx.doi.org/10.1111/j.1600-0838.2010.01052.x
Phase 1 (Weeks 0-10 to 0-12, or Progression Criteria Met)Goals• Decrease swelling• Pain management• Restoration of full knee extension and flexion compared bilaterally• Non–weight-bearing strengthening exercises for hip, quadriceps, ham-
strings, lower leg• Introduction of weight-bearing strengthening for ankle, quadriceps, and
gluteals; core strengthening; weight-bearing/balance training• Begin cardiovascular training: stationary bike, elliptical trainer, upper-
body ergometer• Begin stationary ball handling, free-throw shooting, spot-shooting drillsPhase 1 to Phase 2 Progression CriteriaROM criteria:• Near full extension• Flexion of at least 120° (overpressure)
APPENDIX A
REHABILITATION GOALS AND RETURN-TO-PLAY CRITERIA (PHASE 1 TO PHASE 3) FOLLOWING ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION IN A BASKETBALL PLAYER
42-04 Waters.indd 334 3/21/2012 4:35:13 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 335
Strength criteria:• Push strength of at least 50% of uninvolved side on the leg press• Good quadriceps contraction in extension• No extensor lag• Progressively increasing strength in ankle plantar flexion• Single-leg bridging• 4-way hip movements• Internal and external hip rotationGeneral criteria:• Patellar mobility: progressively increasing patellar mobility• Pain: little to no pain during ambulation• Swelling: mild to no swelling following rehabilitation and activities of
daily living• Kinesthetic awareness: increasing ability to balance on involved lower
extremity
Phase 2 (Weeks 13-19, or Progression Criteria Met)Goals• Continuance of phase 1 goals• Regain primary strength of gastrocnemius/soleus, quadriceps/ham-
strings/gluteals, pelvic girdle equal to uninvolved side• Balance and kinesthetic awareness enhancement• Begin low-load jumping and landing skills and testing• Begin straight-ahead running mechanics• Begin low-intensity cutting mechanics, low-intensity acceleration/
deceleration drills• Progress to advanced cardiovascular training: treadmill running, on-
court running, sustained shooting drills• Continue ball-handling/shooting drills, begin moving with ball, dribbling
with the basketball, and low-intensity on-court drillsPhase 2 to Phase 3 Progression CriteriaROM criteria:• Near full extension passively• Flexion of 130° (overpressure)Strength criteria:• Push strength of at least 70% of uninvolved side on the leg press• Isokinetic flexion/extension within 70% of uninvolved side at 60°/s,
180°/s, and 300°/s• Single-leg squat of near equal depth of uninvolved side• Single-leg bridge strength 80% of uninvolved side• Hip internal/external rotators strength 80% of uninvolved side• 4-way hip strength within 80% of uninvolved sideGeneral criteria:• Patellar mobility: near full mobility compared bilaterally• Pain: little or no pain during or after rehabilitation process• Swelling: mild to trace swelling following rehabilitation and activities of
daily living• Power: ability to do vertical 15-cm box jumps, forward, left, and right,
with good control of hip and knee• Kinesthetic awareness: increasing ability to maintain balance dur-
ing perturbation drills, ability to land from 10-cm and 15-cm boxes in forward and right and left landing jumps with proper hip and lower extremity alignment
Basketball-specific criteria:• Ability to maintain lower extremity alignment and balance during de-
fensive slide (FIGURE 13, ONLINE VIDEO 3), crab dribble (FIGURE 12, ONLINE VIDEO 4), crossover step (ONLINE VIDEO 5), lateral hop with dribble (ONLINE VIDEO 6), and lateral hop with catch drills (ONLINE VIDEO 7)
APPENDIX A
Phase 3 (Week 20 to Unrestricted Activity or When Return-to-Play Criteria Are Met)Goals• Continuance of phase 1 and 2 goals• Continue strength, power, agility, basketball skill acquisition• Continue functional strength and power enhancement• Continue eccentric strength and force attenuation enhancement• Progress basketball skill work, agility, and neuromuscular development• Return to full basketball participation: cardiovascular testing, practice
structuring, and game minutes allocationRange of Motion (ROM) Criteria7
• Full knee extension bilaterally16
• 135° of flexion, while progressing to full flexion bilaterally, ideally heel to rear28
Strength Criteria• Knee extension strength (isotonic): 90% of uninvolved side, 3-repeti-
tion maximum19
• Hamstring curl strength (isotonic): 90% of uninvolved side, 3-repetition maximum19
• Leg-press strength (isotonic): 90% of uninvolved side, 3-repetition maximum
• Single-leg squat test: 90% of uninvolved side, 10 repetitions with equal bilateral mechanics of uninvolved side with 18.14-kg weight vest and equal ROM depth of uninvolved side
APPENDIX B
REHABILITATION GOALS AND RETURN-TO-PLAY CRITERIA (PHASE 3 TO UNRESTRICTED ACTIVITY) FOLLOWING ANTERIOR
CRUCIATE LIGAMENT RECONSTRUCTION IN A BASKETBALL PLAYER
42-04 Waters.indd 335 3/21/2012 4:35:14 PM

336 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
Power Criteria• Hamstrings/quadriceps power production (isokinetic): 85% of unin-
volved side at 60°/s, 180°/s, 300°/s• Rotational power squat test: cable resistance (isokinetic readout or
6-repetition maximum; 85% of uninvolved limb) (FIGURES 10 and 11)• Static single-leg vertical jump test: height 85% of uninvolved dominant
limb or 90% of uninvolved nondominant limb (average of 3 trials)• Single-leg broad jump test: single-leg hop for distance 85% to 90% of
uninvolved limb (average of 3 trials)• Single-leg triple jump test: 3 consecutive hops for total distance 85% to
90% of uninvolved limb (average of 3 trials)• Single-leg speed hop test: 10-m single-leg hop for speed, where time to
cover distance is 90% of uninvolved limb (average over 3 trials)• Running single-leg vertical jump test: height of 85% to 90% of unin-
volved dominant limb or 90% to 95% of uninvolved nondominant limb (average of 3 trials)
Neuromuscular/Proprioceptive Awareness Criteria• Landing Error Scoring System18: score of 0 to 2• Single-leg forward hop test: kinematics similar to that of uninvolved
limb (balanced landing; none or minor valgus knee moment; landing foot fixed; attenuation of forces through foot, ankle, knee, hip, and lum-bar spine; proper joint angles at each joint upon landing)
• Single-leg lateral hop test: same criteria as for single-leg forward hop test, following a lateral hop jump and landing (to the same side as the limb used)
• Single-leg fatigued hop test4: single-leg hop test performed following 1
set of knee extension and 1 set of isotonic flexion (50% of 1-repetition maximum of each exercise) exercises to fatigue and a 1-minute rest before beginning test
• Single-leg perturbation test: single-leg minisquat position held for 20 seconds with manual perturbation about the shoulders and hips, main-taining position without contralateral foot touchdown and holding same depth (15°, 30°, 45° knee flexion) throughout the test
Basketball-Specific Criteria• Successful execution of high-intensity basketball-specific drills
in phase 3• Repeat hop drills (hop turns at 90° and 180° with basketball pass and
catch drills) (ONLINE VIDEOS 8 and 9)• Footwork agility drills (stutter step and lateral crossover step ladder
drills) (ONLINE VIDEOS 10 and 11)• Reactive drills (crab dribble, defensive dribble, close-out drills)
(FIGURES 12 through 14, ONLINE VIDEOS 13 through 15)• Basketball agility drills (zigzag, sprint to backpedal, box, star, and ball
chase drills) (FIGURES 16 through 20, ONLINE VIDEOS 16 through 19)• Contact drills (gauntlet drill, low-post drill, leap-contact double-leg,
leap-contact single-leg drills) (FIGURE 21, ONLINE VIDEOS 20 through 22)
Cardiovascular and Psychological Criteria• Cardiovascular capacity test12
• Psychological readiness evaluation (by team psychologist and medical staff)6
APPENDIX B
GO GREEN By Opting Out of the Print Journal
JOSPT subscribers and APTA members of the Orthopaedic and Sports Physical Therapy Sections can help the environment by “opting out” of receiving the Journal in print each month as follows. If you are:
· A JOSPT subscriber: Email your request to [email protected] or call the Journal o�ce toll-free at 1-877-766-3450 and provide your name and subscriber number. · An APTA Orthopaedic or Sports Section member: Go to www.apta.org and update your preferences in the My Profile area of myAPTA. Select “myAPTA” from the horizontal navigation menu (you’ll be asked to login, if you haven’t already done so), then proceed to “My Profile.” Click on the “Email & Publications” tab, choose your “opt out” preferences and save.
Subscribers and members alike will continue to have access to JOSPT online and can retrieve current and archived issues anytime and anywhere you have Internet access.
42-04 Waters.indd 336 3/21/2012 4:35:14 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 337
[ clinical commentary ]
Returning an athlete, specifically an American football player, back to competition after surgery requires a comprehensive approach that, in addition to rehabilitation of the injury, includes nutritional considerations to create
an optimal healing environment for the tissue, cardiovascular fitness considerations based on the needs of the athlete, and an awareness of
the psychosocial factors that are a part of the injury and recovery process. This comprehensive, integrated approach, re-
quiring multidisciplinary input, bridges the gap between rehabilitation and per-formance. There is no one person who
can do everything for the athlete as he progresses from the operat-ing room to return to sport per-formance on the field. There are many healthcare professionals in-
volved in the process, some playing larger roles at certain times than others. In the athlete-centered model, everyone is in-volved in the process, working together to return the athlete to play.
Because the focus of this manuscript is on late-stage functional rehabilitation after anterior cruciate ligament (ACL) reconstruction in an American football player, we will not cover the early stages of rehabilitation. The criteria for entering the functional rehabilitation phase can include but are not limited to the follow-ing: full pain-free knee range of motion, a minimum level of quadriceps strength,12,17 no episodes of giving way and a negative pivot shift test upon examination, no significant increases in edema seen with standard rehabilitation, a minimum knee function questionnaire score,17 and a Functional Movement Screen (FMS) test score of 14 or higher, without asymme-tries or pain. We are strongly in favor of using the FMS to determine an athlete’s readiness to begin the functional stage of
TT SYNOPSIS: Returning an American football player to sport after an anterior cruciate ligament reconstruction is challenging on several fronts. First, there are approximately 15 different positions a football player could play, depending on how specifically you define the positions on the field. Each of these positions has specific demands for optimal size, strength, power, body composi-tion, cardiovascular fitness, and movement. Understanding all of these factors is paramount to returning a football player not only to his sport but also to his specific position. Second, the chaotic, contact-rich nature of the sport requires that heavy demands be placed on the lower extremities to attenuate external contact forces from other players and from ground reaction forces associ-ated with accelerating, decelerating, quick stops and starts, and changing direction. Finally, return to a competitive level of performance is further influenced by playing surface, shoe selection, the
equipment the player wears, and various potential psychosocial factors. It is the responsibility of the clinician to provide a progressive and system-atic rehabilitation program by first introducing preprogrammed movements that, once mastered, are progressed with elements of more reactive and random movement patterns. The precise nature of this systematic progression of advanced rehabilitation is key in developing return-to-play criteria and, ultimately, in readying an American football player for eventual return to sport and a particular position.
TT LEVEL OF EVIDENCE: Therapy, level 5. J Orthop Sports Phys Ther 2012;42(4):337-344. doi:10.2519/jospt.2012.4031
TT KEY WORDS: ACL, criteria, rehabilitation, surgery
1Founder and President, Athletes’ Performance and Core Performance, Phoenix, AZ. 2Vice President, Performance Physical Therapy and Team Sports, Athletes’ Performance and Core Performance, Phoenix, AZ; Head Athletic Trainer/Physical Therapist, Los Angeles Dodgers, Los Angeles, CA. 3Director of Tactical Performance, Athletes’ Performance Florida, The Andrews Institute, Gulf Breeze, FL. 4Rehabilitation Coordinator, Los Angeles Dodgers, Phoenix, AZ; Performance Physical Therapist, Athletes’ Performance, Phoenix, AZ. Athletes’ Performance uses the Functional Movement Screen in its methodology. Dr Smith is also an instructor for Functional Movement Systems. The Functional Movement Screen and the Y-Balance Test are components of the system. Address correspondence to Dr Steve Smith, Rehabilitation Coordinator, Los Angeles Dodgers, Camelback Ranch, Phoenix, AZ 85037. E-mail: [email protected] or [email protected]
MARK VERSTEGEN, MS, CSCS1 • SUSAN FALSONE, PT, MS, SCS, ATC, CSCS, COMT2
RUSSELL ORR, MS, ATC, CSCS3 • STEVE SMITH, PT, DPT, SCS, CSCS4
Suggestions From the Field for Return to Sports Participation
Following Anterior Cruciate Ligament Reconstruction: American Football
SUPPLEMENTAL VIDEO ONLINE
42-04 Verstegen.indd 337 3/21/2012 4:36:06 PM

338 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]rehabilitation, as evidence suggests that it is a useful tool to predict injury risk in multiple populations5,13,29 and it allows one to see if satisfactory results on mea-sures of impairment at a specific joint correlate with multisegmental move-ment competency and adequate motor control before the body is under higher stress in an advanced stage of rehabilita-tion. For similar reasons, a tool like the Y Balance Test could be used to determine if asymmetry exists in the weight-bearing function of the lower extremities.26 The approximate amount of time after an ACL reconstruction that someone would enter into the functional rehabilitation stage varies greatly and is dependent on age of the patient, graft choice, concomi-tant surgical procedures, other coexisting injuries, and preference for use of a crite-ria- or time-based postoperative progres-sion. In general, we feel that this phase should start somewhere around 4 months postsurgery.
SPORT-SPECIFIC REHABILITATION PHASES
There may be several potential phases in a sport-specific functional rehabilitation program that are
neither finite nor definitive. Functional rehabilitation is not a true linear progres-sion, as a rehabilitating player may often work on acquiring several movement competencies and multiple goals at the same time. The functional rehabilitation program emphasizes the achievement of a high level of movement quality with competent skill performance before pro-gressing to the next, more complex phase.
We recommend that phase creation be based on concepts of motor learning, with attention to the necessary move-ment skills needed for the position of the player. Phase progression should move from simple to complex. In each phase, movements and motor qualities that will ultimately be used in competition are the focus. Parameters, instruction, and exer-cise/drill sets are dictated by the athlete’s level of motor learning, movement qual-
ity, proprioceptive capabilities, and tissue tolerance. We have 3 phases for our func-tional rehabilitation program.
Initial Phase: Discrete, Closed Movements in a Blocked-Practice FormatDiscrete movements are defined as move-ments that have a recognizable beginning and end. Closed movements are predict-able (TABLE 1, ONLINE VIDEOS 1 and 2). The athlete has a fixed stimulus or set of in-structions, as directed by the healthcare professional or the athlete’s own pace. Blocked practice, although not proven to improve skill performance or transfer-ence in a game situation, is the perfor-mance of 1 particular skill for a certain
number of repetitions before moving on to the next. The blocked-practice format is an appropriate place to start. Examples of exercises/drills in this phase would be 3 sets of 5 countermovements, single-leg hurdle hops, 30-second linear jogging in-tervals on a treadmill at a specific speed and grade, or 5 repetitions of resisted ac-celeration from a 2-point start.
Intermediate Phase: Combination PhaseIn this phase, combinations of the move-ment and motor-learning components of the initial and final phases of the pro-gram are used (ONLINE VIDEOS 1 and 2). The subphases and drills performed in this phase, like those of the initial and
TABLE 1Initial Phase of Functional Rehabilitation
(online videos 1 and 2)
Movement Term Definition Example
Discrete skill Skill or task organized in a way that the action
is usually brief and has a well-defined
beginning and end
10 yd (10 m) of linear acceleration
Closed skill Skill performed in an environment that is
predictable or stationary and that allows
performers to plan their movements in
advance
Performing 10 yd (10 m) of linear acceleration
with the athlete’s self-determined start or
in response to a predetermined visual or
verbal cue from a coach or rehabilitation
professional
Blocked practice Practice sequence in which individuals
rehearse the same skill repeatedly
Repeating 10 yd (10 m) of linear acceleration
for 10 consecutive repetitions before
moving on to the next drill/skill
TABLE 2 Final Phase of Functional Rehabilitation
Movement Term Definition Example
Serial task Several discrete actions connected together in
sequence, often with the order of the ac-
tions being crucial to performance success
Linking of linear acceleration, linear decelera-
tion, and an outside leg cut to the right
or left
Open skill Skill performed in an environment that is
unpredictable or changing around the
performer and that requires the performer
to adapt their movements in response to
dynamic properties of the environment
Performing/linking several discrete actions in
response to another player’s movements or
in response to a previously undetermined
cue given by a coach or rehabilitation
professional
Random practice Practice sequence in which individuals
perform a number of skills in a (quasi)
random order, thus avoiding or minimizing
consecutive repetitions of any single skill
Randomly changing the other player’s move-
ments or cues given so that the athlete has
to vary their movement response accord-
ingly without repeating the same skill
42-04 Verstegen.indd 338 3/21/2012 4:36:07 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 339
final phases, are at the discretion of the healthcare professional. Examples of exercises/drills in this phase would be a timed T-test, L-drill, 5-10-5/pro agility shuttle, in which several movement skills are linked together but in a predictable order. In these examples, the drill is serial in nature, but the environment is closed and the practice format could be either blocked or random.
Final Phase: Serial, Open Movements in a Random-Practice FormatSerial movements are defined as those that are made up of a series of individu-al movements linked together (TABLE 2). Open movements occur in an environ-ment that is constantly changing and therefore require constant adjustment by the athlete. Random practice is when the athlete practices a number of dif-ferent tasks in no particular order. Ex-amples of exercises/drills in this phase would be when the player, potentially in a position-specific manner, reacts to another player’s movements or the ver-bal and/or visual cues from a coach or rehabilitation professional. The indi-vidual movements are linked together in a changing environment and can be randomly practiced.
Typical and effective rehabilitation fo-cuses on regaining neuromuscular con-trol, reinforcing a movement pattern, and building strength in an atrophied muscle group or limb. It is very typical to see a set/repetition scheme that gener-
ally uses 3 sets of 10 repetitions. The re-habilitation specialist must understand, however, that the athlete does not func-tion in a world of 3 sets of 10. Athletes function in a world of varying intensi-ties, varying speeds, and unpredict-ability. They often must overcome not only the force they generate but also the forces others place on them to the limit of their strength, speed, and range of mo-tion. Movement skills, like rehabilitation phases, must prepare athletes not only to work in their own preplanned motor program but to respond to stimuli that they would not encounter under nor-mal, nonsport playing circumstances. Therefore, sports rehabilitation in this advanced stage must provide varying speeds, intensities, volume, and external forces to prepare the athlete to return to the playing field. A simple force-velocity curve (FIGURE 1) is useful when developing exercises/drills that provide these various stimuli. An understanding of the differ-ent types of strength, the capabilities of the neuromuscular system, and how rel-evant certain types of strength are to a particular position is also essential.27 For example, offensive and defensive linemen may need more exercises/drills that elicit more force production and relatively less velocity of movement, while skill-posi-tion players may need more exercises/drills that elicit more velocity of move-ment and relatively less force production.
Considering the multitude of position-specific movements a football player has to perform, exercise and drill selection, like rehabilitation phases, must progress from simple to complex. Each position-specific movement can be broken down
into its component parts, and the com-ponents can be taught individually be-fore being combined. These complex movements, when broken into their component parts, can be classified into 3 groups of movement possibilities: linear movement, multidirectional movement, and jumping/landing. Once these move-ments are mastered individually, they can be put together to create more complex movement patterns.Linear Movement Linear movement consists of moving in 1 direction (ONLINE
VIDEO 1). An athlete accelerates, runs at top speed, or decelerates. With the ex-ception of track runners and marathon-ers, the majority of athletes do not solely function in a linear movement pattern. Therefore, deceleration is a transitional movement, as the way an athlete deceler-ates will often depend on the next move-ment to be performed. Eccentric strength in both double- and single-leg support is vital when working generally on decel-eration. An athlete must master these movement patterns individually prior to putting them together into more complex movement patterns.Multidirectional Movement Multidirec-tional skills traditionally consist of lat-eral movements, such as shuffle patterns, that combine change of direction through transitional movement skills such as crossover and drop-step techniques. Generally, multidirectional movements are used as transitional movements from one pattern to another and are preceded by plant, cut, pivot, or other rotational movements (ONLINE VIDEO 2). For example, a defensive back covering a wide receiv-er in American football may backpedal
Eccentric strength
Maximal strength
Forc
e
Explosive strength
Assisted movements
Velocity
FIGURE 1. Force-velocity curve (strength types plotted on curve). Adapted from Siff and Verkhoshansky33 and Poliquin and Patterson.27
TABLE 3 Plyometric Session Design
Variable Recommendation
Training frequency/duration of session 2 to 4 times per wk, 10 to 15 min
Movements per session 2 to 3
Sets/repetitions per session 4 to 6 sets, 5 to 8 repetitions
Rest between sets 30 to 90 s
Daily/weekly amount 25 to 50 foot contacts per session, <120 foot contacts per wk
42-04 Verstegen.indd 339 3/21/2012 4:36:08 PM

340 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]and incorporate a pivot into a rotational drop-step technique to transition into a linear-acceleration pattern. The drop-step technique is used as a transitional movement to change from a backward direction to a forward direction. An ath-lete must master many movement pat-terns and transitions individually prior to integrating them into more complex movement patterns.Jumping and Landing An athlete must be able to do both of these movements. The intent of plyometric training is to increase the athlete’s ability to handle rapid-stretch loads within the musculo-tendinous unit during a rapid change of direction, mainly during rotational and deceleratory tasks. Plyometrics are ex-ecuted with double-leg support ( jump), single-leg support (hop), or alternating-leg support (bound). These movements can be done in place or in various vec-tors or planes (linear/sagittal, lateral-medial/frontal, rotational/transverse), with emphasis on vertical or horizontal displacement. Special emphasis is placed on limb alignment and force attenuation during the landing phase. A progressive program is developed by manipulating amplitude, frequency, contact volume, contact linking, and exposure to the stretch-shortening cycle. TABLE 3 shows an example of a plyometric session design.
Specific/Unique Drills in a Given PhaseTABLES 4 and 5 show 2 examples of how an exercise/drill, knowing the terminal skill goal, can be manipulated and progressed through all the phases of the functional rehabilitation program for a lineman and a skill-position player, respectively. Drill selection and progression for each posi-tion are based on all the preceding back-ground information provided.
TABLE 6 shows an example of how dif-ferent types of strength qualities, the force-velocity curve, the movement type, and program phase interact to create the drills that are prescribed to the recover-ing athlete at a specific point in the func-tional rehabilitation process.
TABLE 4Drill Progression Through the Functional Rehabilitation Phases: Offensive Lineman*
Phase Setup and Cues
1. Initial phase (ONLINE VIDEO 1) Perform certain number of repetitions of same skill consecutively
at predetermined distance with a clear beginning and end
Fixed loading style: free, resisted, or assisted
Perform each repetition with player fully rested
Perform individual movement skills in isolation
2. Intermediate phase (ONLINE VIDEO 1) Perform certain number of repetitions of similar movement skills
Create drills linking 2 or more movement skills together
Begin varying environment and/or athlete movement demands (ie, visual,
auditory, reactive, tactile, outcome)
Examples: change/vary distances of individual movement skills, change
work-rest ratios, use a varied loading style with emphasis placed
on resisted loading to increase force production, introduce
preprogrammed contact
3. Final phase Perform terminal movement skill repetitions in a randomized order
Vary environment and/or athlete movement demand (ie, visual, auditory,
reactive, tactile, outcome)
Examples (in addition to those noted above): random contact, reaction
to an offensive player’s movements, with equipment
*Terminal position-specific movement desired: run block, pull right or left. Component movement skills: drop-step, acceleration, outside leg cut, acceleration downfield.
TABLE 5Drill Progression Through the Functional
Rehabilitation Phases: Defensive Back*
*Terminal position-specific movement desired: pass coverage, man to man. Component movement skills: backpedal, 45° drop-step, linear acceleration.
Phase Setup and Cues
1. Initial phase (ONLINE VIDEO 2) Perform certain number of repetitions of same skill consecutively
at predetermined distance with a clear beginning and end
Fixed loading style: free, resisted, or assisted
Perform each repetition with player fully rested
Perform individual movement skills in isolation
2. Intermediate phase (ONLINE VIDEO 2) Perform certain number of repetitions of similar movement skills
Create drills linking 2 or more movement skills together
Begin varying environment and/or athlete movement demands (ie, visual,
auditory, reactive, tactile, outcome)
Examples: change/vary distances of individual movement skills, change
work-rest ratios, use a varied loading style with emphasis placed
on assisted loading to increase velocity of movement, introduce
preprogrammed contact
3. Final phase Perform terminal movement skill repetitions in a randomized order
Vary environment and/or athlete movement demand (ie, visual, auditory,
reactive, tactile, outcome)
Examples (in addition to those noted above): random contact, reaction
to a defensive player’s movements, with equipment, reaction to
a thrown ball
42-04 Verstegen.indd 340 3/21/2012 4:36:09 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 341
RETURN-TO-FOOTBALL CRITERIA
In the current literature, there is a great amount of variability in the cri-teria selected by sports medicine pro-
fessionals to ascertain whether an athlete is ready to return to the team.15 Common criteria include subjective, clinical, and functional components. The absence of pain, the absence of swelling before, dur-ing, and after activity, and self-reports of no episodes of giving way are critical criteria to be met prior to returning to American football. In addition, favor-able scores on self-reported measures of knee function and disability are used.31,37 Likewise, clinical components have in-cluded measures of anterior laxity using arthrometry devices,22,32,35 the absence of a pivot shift upon clinical examination, and a minimum level of proficiency when strength of quadriceps and hamstrings is tested and bilateral comparisons are made.17,37 Various types of functional tests, including hop and agility tests, have also been recommended8,17,18,21,34 as a way to assess dynamic knee stability. There is conflicting evidence on how well subjec-tive or clinical assessment outcomes cor-relate to functional tests.1,16,20,25,30,32,35,37 Consequently, conducting a battery of tests is generally recommended.6,36
The design of any return-to-play test or battery of tests should allow the clini-cian to answer the following question: “Have I minimized all of the potential risk factors for reinjury when my athlete returns to performing his football skill?” It is our responsibility as rehabilitation specialists to identify and minimize all the risk factors that we can and to en-sure adequate tissue tolerance. We must frame the return-to-play question in this context because we are able to affect cer-tain variables that have been shown in the literature to be risk factors for injury. Prospective studies have shown that a history of previous injury continues over-whelmingly to lead all other risk factors for potential future injury.7,23,24 Another risk factor for injury is asymmetry.14,18,19,26
Asymmetries that need to be consid-ered include, among others, mobility, stability, recruitment patterns, strength, and movement patterns. Altered motor control38 and body mass index are also potential risk factors. However, it is our belief that in this population a multisite body composition measurement may be a better marker than body mass index, be-cause the former is an actual site-specific estimate of lean mass and fat mass, while the latter is only a correlation between height and weight.
Outcomes or Functional Tests to Clear Return to PlayA study of elite-level running backs and
wide receivers with ACL reconstruc-tions showed that these athletes gener-ally returned to their first game at 9 to 12 months following surgery.3 For the pur-pose of this paper, “return to football” will be defined as the point at which an ath-lete is ready to return to individual and team practice. Based on clinical experi-ence, we feel that this milestone should be met 1 to 2 months prior to the athlete’s return to a competitive game. This means that our rehabilitation efforts need to fo-cus on returning players to practice and not just up to the point of being able to performance train.
To determine if an athlete is ready to return to any movement-based sport, es-
TABLE 6Example of an Initial-Phase Exercise/Drill Prescription
Strength/Movement GoalLinear Acceleration (ONLINE VIDEO 1)
Multidirectional: Change of Direction (ONLINE VIDEO 2)
Eccentric strength Maximize relative leg strength in
all major muscle groups and
planes of motion eccentrically
for deceleration
Resisted walking lunge Bungee-assisted lateral
cut
Maximum strength Maximize relative leg strength in all
major muscle groups and planes
of motion
Rearfoot-elevated split
squat
Resisted lateral load and
lift wall drill
Starting strength To overcome inertia in a controlled
manner
Box blast: single Crossover with bullet belt
Explosive strength To produce a certain amount of
work in a defined period of time.
To progress, decrease time while
doing same amount of work
Hang clean Drop-step to acceleration
Resisted strength To control body against an outside
force. To be able to stabilize
against a force being applied to
the body or limb
Resisted sled acceleration
runs/starts
Crossover march with sled
resistance
Reactive movements To control body while reacting to
someone else’s movement,
verbal command, or visual
command
Get-up start (verbal) Mirror drill (visual)
Free movements To have the ability to execute a
preprogrammed motor plan
Falling start 6-yd (6-m) hitch right
or left
Assisted movements To control the body movements
while an outside source pushes
the body beyond normal speed
or movement patterns
Bungee assisted (5 yd
[5 m])
Bungee-assisted change
of direction in athletic
base (3 yd [3 m])
42-04 Verstegen.indd 341 3/21/2012 4:36:10 PM

342 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]pecially one that is chaotic and involves violent collisions, the criteria or tests that are used should replicate the condi-tions of the sport and position as closely as possible. The criteria used to assess readiness should include position-spe-cific, random movements that allow for bilateral comparison. Movement-based testing should be done with the athlete in a stressed or fatigued state. Because fa-tigue adversely affects motor control,11 it is important to see these potential prob-lems in a controlled environment before placing the athlete back into such condi-tions under more random circumstances. Giving special consideration to fatigue is supported by the data from Bradley and colleagues,2 who reported that the majority of ACL injuries in the National Football League (NFL) that happened during games occurred later in the game. The work-rest ratios used during testing should also be similar to those occurring during American football. Work done by Iosia and Bishop,10 as well as Hitchcock and colleagues,9 provides insight into the work-rest ratios and exercise intensity that should be used to properly fatigue a football player in a sport-specific manner immediately before testing. Work-rest intervals for the fatigue protocol should be set at approximately 5 to 10 seconds of work to 40 seconds of rest. Also, during the work intervals, the intensity of the activity should be high, due to the fact that football players rely primarily on an anaerobic source of energy for adenos-ine triphosphate (ATP) resynthesis. We recommend that maximum heart rate, recovery heart rate, number of repeti-tions, and wattage (given access to ad-equate equipment) are recorded. Once the athlete is fatigued, a recovery period is given, and then the randomly ordered, position-specific movements are initi-ated. Form breakdown and/or a drop in speed/power are monitored as they were during the fatigue protocol, and recovery time is given as needed. The randomly ordered, position-specific movements are continued until all are completed. An active cool-down period is given fol-
lowing completion. A detailed example of the testing protocol for a wide receiver, including the fatigue protocol, can be found in FIGURE 2.
The position-specific movements are assessed for a comparison of the time it takes to complete the bilateral pattern and a comparison of the control and ease exhibited during transitional move-ments. We want to observe and note any movements that may cause an ACL tear
or that may excessively stress the healing graft. Specifically, we are looking for the absence of excessive sagittal plane shear of the tibiofemoral joint (seen with in-creased tibial angle upon weight accep-tance) and the absence of tibiofemoral rotation stress to the tibiofemoral joint (seen with femoral medial rotation/col-lapse or a pronatory foot collapse with tibial rotation).28 We also recommend a comparison of the first step, stride
50 5
04
040
Fade/Up Post
Corner
OutHook
In
5
9 8
6
7
3
2
01
Slant
HitchQuick Out
WR
6-y hitch, right and left6-y out, right and left3-step slant, right and left10- to 12-y speed out, right and left10- to 14-y hook, right and left18-y comeback, right and left14- to 16-y square in, right and left7-step post-corner, right and left7-step post, right and left20- to 25-y fade, right and left
5-minute dynamic warm-up5- to 10-second high-intensity work intervals with 40-second rest (use a piece of equipment incorporating the entire body), until speed or power drops and/or form breaks downRecovery period where heart rate gets to 65% to 70% of maximum or for 2 to 3 minutesInitiate random, position-specific movements (bilaterally compare each movement in a random order), giving 40-second rest between position-specific patterns, until speed or power drops o� and/or form breaks downRepeat step 3 as neededRepeat step 4 until all patterns are completed5-minute active cool-down
0.1.2.3.4.5.6.7.8.9.
1.2.
3.4.
5.6.7.
Position-Specific Movements: Wide Receiver
Example of a Return-to-Play Testing Protocol: Wide Receiver
4
Comeback
FIGURE 2. Example of a return-to-play testing protocol for a wide receiver. One yd equals 0.91 m. Route distances are not to scale on the figure. Abbreviations: L, left; R, right.
42-04 Verstegen.indd 342 3/21/2012 4:36:11 PM

journal of orthopaedic & sports physical therapy | volume 42 | number 4 | april 2012 | 343
length, and stride frequency bilaterally. Subjective reports of pain or posttest-ing swelling also need to be taken into consideration.
In addition, to more accurately judge the quality of the athlete’s motor control and quantity of the movement skill dis-played for asymmetry, we recommend using some type of system to capture ki-nematic as well as kinetic data.4 If these systems are not available, a skilled eye that has experience observing various movement patterns will suffice. Eventu-ally, having movement-based qualitative standards for performance and skill-level tasks would also be helpful, just as the FMS is currently used to screen and rank dysfunctional and/or painful fun-damental movement. Last, we also see the potential benefit of adding reactions to a thrown football and/or perform-ing the tests in full pads, shells, and/or cleats. These could be used in more advanced testing and could potentially show asymmetries and altered motor control because of the increased difficul-ty and energy costs associated with the additions.
Prevention of Injury After ACL ReconstructionBecause a history of previous injury is the biggest risk factor for future injury, American football players who have un-dergone ACL reconstruction are more likely to be injured in the future. To lessen the risk, a high level of movement com-petency must be maintained through all stages of rehabilitation. Therefore, the athlete must maintain a stable and mo-bile platform from which to move (a high level of “pillar strength”), so that exces-sive external forces inherent to the game do not unexpectedly create macrotrauma or even repetitive chronic microtrauma. One area that can be easily influenced is the athlete’s warm-up for both training and competition. We recommend that the warm-up be dynamic, weight bear-ing, proprioceptively rich, activate key stabilizers, and actively elongate/stretch the myofascial system.
CONCLUSION
The task of returning any ath-lete to sport is both rewarding and challenging, and returning an
American football player to sport is no different. It is best to treat this process as a continuum of care from surgery to re-turn to play. The functional or late-stage portion of the rehabilitation process is not a simple, linear progression but rather a well-thought-out mix of art and science. Any healthcare professional involved in this process should always have a working knowledge of the position-specific move-ment patterns and metabolic characteris-tics of the athlete’s sport. t
REFERENCES
1. Bach BR, Jr., Jones GT, Hager CA, Sweet FA, Luer-gans S. Arthrometric results of arthroscopically assisted anterior cruciate ligament reconstruc-tion using autograft patellar tendon substitution. Am J Sports Med. 1995;23:179-185.
2. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treat-ment trends among team physicians. Arthrosco-py. 2002;18:502-509. http://dx.doi.org/10.1053/jars.2002.30649
3. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receiv-ers in the National Football League. Am J Sports Med. 2006;34:1911-1917. http://dx.doi.org/10.1177/0363546506290186
4. Chmielewski TL. Asymmetrical lower extremity loading after ACL reconstruction: more than meets the eye. J Orthop Sports Phys Ther. 2011;41:374-376. http://dx.doi.org/10.2519/jospt.2011.0104
5. Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5:47-54.
6. Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31:210-215.
7. Faude O, Junge A, Kindermann W, Dvorak J. Risk factors for injuries in elite female soccer players. Br J Sports Med. 2006;40:785-790. http://dx.doi.org/10.1136/bjsm.2006.027540
8. Fitzgerald GK, Lephart SM, Hwang JH, Wain-ner RS. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001;31:588-597.
9. Hitchcock KM, Millard-Stafford ML, Phillips JM, Snow TK. Metabolic and thermoregula-tory responses to a simulated American foot-ball practice in the heat. J Strength Cond Res. 2007;21:710-717. http://dx.doi.org/10.1519/R-20916.1
10. Iosia MF, Bishop PA. Analysis of exercise-to-rest ratios during Division IA televised football competition. J Strength Cond Res. 2008;22:332-340. http://dx.doi.org/10.1519/JSC.0b013e31816607b0
11. Johnston RB, 3rd, Howard ME, Cawley PW, Losse GM. Effect of lower extremity muscular fatigue on motor control performance. Med Sci Sports Exerc. 1998;30:1703-1707.
12. Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231-237. http://dx.doi.org/10.1016/S0736-0266(02)00160-2
13. Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther. 2007;2:147-158.
14. Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76-81.
15. Kvist J. Rehabilitation following anterior cruci-ate ligament injury: current recommenda-tions for sports participation. Sports Med. 2004;34:269-280.
16. Lephart SM, Perrin DH, Fu FH, Gieck JH, McCue FC, Irrgang JJ. Relationship between selected physical characteristics and functional capacity in the anterior cruciate ligament-insufficient ath-lete. J Orthop Sports Phys Ther. 1992;16:174-181.
17. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progres-sion through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385-402. http://dx.doi.org/10.2519/jospt.2006.2222
18. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377-387. http://dx.doi.org/10.2519/jospt.2011.3547
19. Nadler SF, Malanga GA, Feinberg JH, Prybicien M, Stitik TP, DePrince M. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001;80:572-577.
20. Neeb TB, Aufdemkampe G, Wagener JH, Mastenbroek L. Assessing anterior cruciate ligament injuries: the association and differen-tial value of questionnaires, clinical tests, and functional tests. J Orthop Sports Phys Ther. 1997;26:324-331.
21. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am
42-04 Verstegen.indd 343 3/21/2012 4:36:12 PM

344 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy
[ clinical commentary ]
@ MORE INFORMATIONWWW.JOSPT.ORG
J Sports Med. 1991;19:513-518. 22. Noyes FR, Berrios-Torres S, Barber-Westin
SD, Heckmann TP. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associ-ated procedures: a prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc. 2000;8:196-206.
23. Orchard J, Seward H, McGivern J, Hood S. Intrin-sic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196-200.
24. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29:300-303.
25. Petschnig R, Baron R, Albrecht M. The relation-ship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate liga-ment reconstruction. J Orthop Sports Phys Ther. 1998;28:23-31.
26. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911-919. http://dx.doi.org/10.2519/jospt.2006.2244
27. Poliquin C, Patterson P. Classification of strength qualities. Strength Cond J. 1989;11:48-52.
28. Powers CM. The influence of abnormal hip
mechanics on knee injury: a biomechanical per-spective. J Orthop Sports Phys Ther. 2010;40:42-51. http://dx.doi.org/10.2519/jospt.2010.3337
29. Raleigh MF, McFadden DP, Deuster PA, et al. Functional movement screening: a novel tool for injury risk stratification of warfighters. American College of Sports Medicine 57th Annual Meeting, June 2-5, 2010. Baltimore, MD: American College of Sports Medicine; 2010.
30. Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in im-pairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:400-412.
31. Sernert N, Kartus J, Kohler K, et al. Analysis of subjective, objective and functional examination tests after anterior cruciate ligament reconstruc-tion. A follow-up of 527 patients. Knee Surg Sports Traumatol Arthrosc. 1999;7:160-165.
32. Sgaglione NA, Warren RF, Wickiewicz TL, Gold DA, Panariello RA. Primary repair with semiten-dinosus tendon augmentation of acute anterior cruciate ligament injuries. Am J Sports Med. 1990;18:64-73.
33. Siff MC, Verkhoshansky YV. Supertraining: Strength Training for Sporting Excellence. Johan-nesburg, South Africa: University of the Witwa-tersrand; 1998.
34. Tegner Y, Lysholm J, Lysholm M, Gillquist J. A
performance test to monitor rehabilitation and evaluate anterior cruciate ligament injuries. Am J Sports Med. 1986;14:156-159.
35. Tyler TF, McHugh MP, Gleim GW, Nicholas SJ. As-sociation of KT-1000 measurements with clinical tests of knee stability 1 year following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:540-545.
36. Weber MD, Woodall WR. Knee rehabilitation. In: Andrews JR, Harrelson GL, Wilk KE, eds. Physi-cal Rehabilitation of the Injured Athlete. 3rd ed. Philadelphia, PA: Saunders; 2004:377-428.
37. Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60-73.
38. Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospec-tive biomechanical-epidemiologic study. Am J Sports Med. 2007;35:1123-1130. http://dx.doi.org/10.1177/0363546507301585
SEND Letters to the Editor-in-Chief
JOSPT welcomes letters related to professional issues or articles published in the Journal. The Editor-in-Chief reviews and selects letters for publica-tion based on the topic’s relevance, importance, appropriateness, and timeliness. Letters should include a summary statement of any conflict of interest, including financial support related to the issue addressed. In addition, letters are copy edited, and the correspondent is not typically sent a version to approve. Letters to the Editor-in-Chief should be sent electronically to [email protected]. Authors of the relevant manuscript are given the opportunity to respond to the content of the letter.
42-04 Verstegen.indd 344 3/21/2012 4:36:13 PM