Abstract Book - MedEspera · 2018. 7. 12. · Abstract Book MedEspera 2018 The 7th International...
Transcript of Abstract Book - MedEspera · 2018. 7. 12. · Abstract Book MedEspera 2018 The 7th International...
-
MINISTRY OF HEALTH, LABOUR AND SOCIAL
PROTECTION OF THE REPUBLIC OF MOLDOVA
Nicolae Testemitanu State University of Medicine
and Pharmacy of the Republic of Moldova
Association of Medical Students and Residents
Abstract Book
MedEspera 2018
The 7th International Medical Congress
for Students and Young Doctors
May 3-5, 2018
Chisinau
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
2
MedEspera 2018: 7th Intern. Medical Congress for Students and Young Doctors,
May 3-5, 2018, Chisinau, Republic of Moldova
Chairman of Editorial Board: Gheorghe Rojnoveanu
Organizing committee: Valeria Turcan
Descrierea CIP a Camerei Naționale a Cărții
"Medespera 2018", International Medical Congress (7 ; 2018 ; Chisinau). MedEspera 2018:
7th International Medical Congr. for Students and Young Doctors, May 3-5, 2018, Chișinău:
Abstract Book / chairman of the ed. board.: Gheorghe Rojnoveanu ; org. com.: Valeria Turcan.
Chișinău: S. n., 2018 (Tipografia Editurii “Universul”. — 327 p.
Antetit.: Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of
Moldova, Assoc. of Med. Students and Residents — 550 ex.
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
3
CONTENTS
MESSAGE OF THE RECTOR ……………………………………………………………………….
WELCOME MESSAGE OF THE ORGANIZING COMMITTEE …………………………………..
ABSTRACTS ………………………………………………………………………………………….
CLINICAL CASES ……………………………………………………………………………………
ORAL PRESENTATIONS ………………………………………………………………………….
POSTERS …………………………………………………………………………………………….
INTERNAL MEDICINE I …………………………………………………………………………….
ORAL PRESENTATIONS …………………………………………………………………………
POSTERS ……………………………………………………………………………………………
INTERNAL MEDICINE II …………………………………………………………………………….
ORAL PRESENTATIONS ………………………………………………………………………….
POSTERS ……………………………………………………………………………………………
SURGERY SECTION I …………………………………………………………………………………
ORAL PRESENTATIONS …………………………………………………………………………..
POSTERS …………………………………………………………………………………………….
SURGERY SECTION II …………………………………………………………………………………
ORAL PRESENTATIONS ………………………………………………………………………….
POSTERS …………………………………………………………………………………………….
PUBLIC HEALTH ………………………………………………………………………………………
ORAL PRESENTATIONS …………………………………………………………………………..
POSTERS …………………………………………………………………………………………….
FUNDAMENTAL SCIENCES ………………………………………………………………………….
ORAL PRESENTATIONS …………………………………………………………………………...
POSTERS ……………………………………………………………………………………………..
DENTAL MEDICINE SECTION ………………………………………………………………………..
ORAL PRESENTATION …………………………………………………………………………….
POSTERS ……………………………………………………………………………………………...
PHARMACY SECTION …………………………………………………………………………………
ORAL PRESENTATIONS …………………………………………………………………………...
ETHICS SECTION ……………………………………………………………………………………….
INDEX …………………………………………………………………………………………………….
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
4
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
5
MESSAGE OF THE RECTOR
At Nicolae Testemitanu State University of Medicine and Pharmacy of the
Republic of Moldova we always encourage youth in their initiatives. It is our
responsibility to inspire them to create, to develop
and surpass their own limits. MedEspera
International Congress for Students and Young
Doctors serves as proof of our commitment in this
regard. The Association of Students and Residents
in Medicine organizes it bi-annually. We
appreciate them for their inexhaustible force and
idealistic desire to execute at this level.
This year, Nicolae Testemitanu SUMPh will
host the 7th edition of the Congress. We hope this
will be a great opportunity for students and young
doctors to exchange ideas and research experience.
The number of foreign MedEspera participants
highlights the fact that medicine has no boundaries.
We hope this year won’t be an exception and our foreign colleagues will attend
this event and will be fully satisfied with the obtained results and experience.
We wish you all good luck! Don’t forget to follow your dreams and work hard
to achieve your goals. Take full advantage of this event and feel free to share your
experience and learn something new from your colleagues.
I wholeheartedly hope your impressions of Moldova and Nicolae Testemitanu
SUMPh will be unforgettable!
Rector Ion Ababii
MD, PhD, Professor
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
6
WELCOME MESSAGE
OF THE ORGANIZING COMMITTEE
Dear colleagues and friends,
We have the honor and pleasure to welcome you to MedEspera International
Congress for Students and Young Doctors. Welcome to Nicolae Testemitanu State
University of Medicine and Pharmacy of the Republic of Moldova! Beside the new
experience, this 7th edition of MedEspera will bring you the most recent
achievements in the fields of medicine, dentistry, pharmacy and public health. We
hope you will enjoy the program we’ve prepared, which includes conferences,
workshops, discussions as well as a social program to familiarize you with the
hospitality of our country and the beauty of our traditions.
The idea of organizing this Congress sparked among a group of our senior
colleagues several years ago. Since the very 1st edition, MedEspera became
popular among medical students and young doctors from the Republic of Moldova
and abroad.
It is our duty to uphold the reputation, popularity and quality of this event. We
are fully committed to make everything in our power to continuously increase the
quality of this event, and we sincerely wish for you to make the best of it!
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
7
President of Honour
Ion ABABII, Rector of Nicolae Testemitanu State University of Medicine and
Pharmacy of the Republic of Moldova, MD, PhD, Professor, Academician of
Academy of Science of Moldova
Members of Honour
Christoph LANGE, MD, PhD, FISA, FERS, Head of Clinical Infectious
Diseases Research Center in Borstel, Professor at International Health/Infectious
Diseases department, University of Lübeck, Germany
Martin COATH, BS, MS, PhD in Neuroscience, Associate lecturer at the
University of Plymouth, Research Fellow at the University of Lapland, United
Kingdom
Benjamin R. THOMAS, DDS, MPH, Periodontist at Sierra Dental Partnership,
Alberta, Canada
Stephen B. MACKLER, DDS, MS, Adjunct Faculty Dept of Periodontics,
UNC School of Dentistry, Chapel Hill, NC, USA
Lenuta PROFIRE, PharmD, PhD, Professor, Head of the Pharmaceutical
Chemistry Department at Grigore T. Popa University of Medicine and
Pharmacy, Iasi, Romania
Viorica CHELBAN, MD, MSc, MRCP, Research Fellow at the University
College London Institute of Neurology, United Kingdom
Organizing Committee
Head of Organizing Committee:
Valeria TURCAN
President of Association of Medical Students and Residents:
Gheorghe BURUIANA
Executive Secretary:
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
8
Olga CLIPII
Staff:
Gheorghe Buruiana, Valeria Turcan, Olga Clipii, Ana-Maria Buliga, Olga
Blobstein, Mihaela Turcanu, Galina Dobrostomat, Elena Ciumac, Dumitrita
Nichiforeac, Camelia Calistru, Sergiu Gavriliuc, Mihaela Taraburca, Alexandrina
Cenusa, Cristina Ermurachi, Nicoleta Florea, Galina Panus, Nicoleta Damian,
Marina Cisa, Laura Tarlapan, Corina Darii, Ana Tabarcea, Vlad Filimon, Nicu
Ribac, Rodion Cujba, Varvara Naghita, Eugenia Dumbravanu, Diana Tambala,
Pavel Chior, Valentin Butnari, Ana Picalau, Radu Cazacu, Igor Gusev, Emanuel
Haig Dikran, Irina Sirbu, Marin Foteniuc, Ion Ernu, Lina-Andreea Robu, Petru
Dodita, Nicoleta Pricop, Sergiu Calancea, Iurie Noroc, Constantin Tataru, Victoria
Taralunga, Anastasia Melnic, Olga Rosu, Alexandrina Buruiana, Mariana Brunchi,
Dumitru Cartaleanu, Alexei Antoci, Mihail Balan, Tudor Gulica, Tudor
Ostapovici, Sorina-Mihaela Rojnita, Corneliu Ursu, Victor Schiopu, Corina
Condur-Scerbatiuc.
Chairman of the Editorial Board
Gheorghe ROJNOVEANU
Vice-Rector for Scientific Activity, Nicolae Testemitanu State University of
Medicine and Pharmacy of the Republic of Moldova
MD, PhD, Professor
Members:
Olga Cernetchi, MD, PhD, Professor
Mihail Gavriliuc, MD, PhD,
Professor
Evghenii Gutu, MD, PhD, Professor
Emil Ceban, MD, PhD, Professor
Marcel Abras, MD, PhD, Associate
Professor
Victoria Cravet
Didina Nistreanu, PhD, Associate
Professor
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
9
Silvia Stratulat, MD, PhD, Associate
Professor
Gheorghe Placinta, MD, PhD,
Associate Professor
Mircea Betiu, MD, PhD, Associate
Professor
Sergiu Ciobanu, MD, PhD, Associate
Professor
Nicolae Ciobanu, MD, PhD,
Associate Professor
Serghei Suman, MD, PhD, Associate
Professor
Ludmila Bologa, MD, PhD,
Associate Professor
Ina Pogonea, MD, PhD, Associate
Professor
Angela Cazacu-Stratu, MD, PhD,
Associate Professor
Igor Cemortan, MD, PhD, Associate
Professor
Stela Cojocaru, MD, PhD, Associate
Professor
Stepco Elena, MD, PhD, Associate
Professor
Livia Uncu, MD, PhD, Associate
Professor
Dumitru Harea, MD, PhD,
University Assistant
Angela Babuci, MD, University
Assistant
Andrei Mostovei, MD, PhD
Adrian Hotineanu, MD, PhD,
Professor
Boris Topor, MD, PhD, Professor
Eugen Bendelic, MD, PhD, Professor
Evghenii Gutu, MD, PhD, Professor
Gheorghe Ciobanu, MD, PhD,
Professor
Igor Misin, MD, PhD, Professor,
Researcher
Ilia Cateriniuc, MD, PhD, Professor
Jana Bernic, MD, PhD, Professor
Larisa Spinei, MD, PhD, Professor
Liliana Groppa, MD, PhD, Professor
Minodora Mazur, MD, PhD,
Professor
Ninel Revenco, MD, PhD, Professor
Oleg Lozan, MD, PhD, Professor
Valeriu Revenco, MD, PhD,
Professor
Victor Ghicavii, MD, PhD, Professor
Victor Vovc, MD, PhD, Professor
Vitalie Lisnic, MD, PhD, Professor
Vladimir Valica, MD, PhD, Professor
Adela Turcan, MD, PhD, Associate
Professor
Adriana Paladi, PhD, Associate
Professor
Ala Paduca, MD, PhD, Associate
Professor
Ala Pascari-Negrescu, MD, PhD,
Associate Professor
Alexandra Grejdieru, MD, PhD,
Associate Professor
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
10
Alexandru Betisor, MD, PhD,
Associate Professor
Alexandru Corlateanu, MD, PhD,
Associate Professor
Alexandru Jalba, MD, PhD,
Associate Professor
Andrei Oprea, MD, PhD, Associate
Professor
Andrei Padure, MD, PhD, Associate
Professor
Andrian Cotelea, MD, PhD,
Associate Professor
Angela Corduneanu, MD, PhD,
Associate Professor
Angela Paraschiv, MD, PhD,
Associate Professor
Angela Peltec, MD, PhD, Associate
Professor
Artiom Jucov, MD,PhD, Associate
Professor
Aureliu Bodiu, MD, PhD, Associate
Professor
Boris Sasu, MD, PhD, Associate
Professor
Corina Cardaniuc, MD, PhD,
Associate Professor
Corina Scutari, MD, PhD, Associate
Professor
Cornelia Talmaci, MD, PhD,
Associate Professor
Diana Manea, MD, PhD, Associate
Professor
Diana Uncuta, MD, PhD, Associate
Professor
Dumitru Casian, MD, PhD,
Associate Professor
Dumitru Sirbu, MD, PhD, Associate
Professor
Elena Bodrug, MD, PhD, Associate
Professor
Elena Deseatnicova, MD, PhD,
Associate Professor
Elena Manole, MD, PhD, Associate
Professor
Eugen Gorgos, MD, University
Assistant
Eugen Melnic, MD, PhD, Associate
Professor
Galina Obreja, MD, PhD, Associate
Professor
Georgeta Mihalache, MD, PhD,
Associate Professor
Ghenadie Curocichin, MD, PhD,
Associate Professor
Grigore Verega, MD, PhD, Associate
Professor
Ianos Coretchi, MD, PhD, Associate
Professor
Ilie Suharschi, MD, PhD, Associate
Professor
Ion Codreanu, MD, PhD, Associate
Professor
Jana Chihai, MD, PhD, Associate
Professor
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
11
Larisa Rotaru, MD, PhD, Associate
Professor
Lilian Saptefrati, MD, PhD,
Associate Professor
Livi Grib, MD, PhD, Associate
Professor
Lorina Vudu, MD, PhD, Associate
Professor
Lucia Turcan, MD, PhD, Associate
Professor
Lucian Danilov, MD, PhD, Associate
Professor
Luminita Gutu, MD, PhD, Associate
Professor
Marina Sangheli, MD, PhD,
Associate Professor
Marin Vozian, MD, PhD, Associate
Professor
Oleg Arnaut, MD, PhD, Associate
Professor
Oleg Solomon, MD, PhD, Associate
Professor
Oleg Zanoaga, MD, PhD, Associate
Professor
Olga Cirstea, MD, PhD, Associate
Professor
Olga Tagadiuc, MD, PhD, Associate
Professor
Oxana Maliga, MD, PhD, Associate
Professor
Oxana Munteanu, MD, PhD,
Associate Professor
Pavel Banov, MD, PhD, Associate
Professor
Polina Ababii, MD, PhD, Associate
Professor
Rodica Catrinici, MD, PhD,
Associate Professor
Rodica Comendant, MD, PhD,
Associate Professor
Ruslan Baltaga, MD, PhD, Associate
Professor
Sergiu Berliba, MD, PhD, Associate
Professor
Stela Adauji, MD, PhD, Associate
Professor
Svetlana Agachi, MD, PhD,
Associate Professor
Svetlana Diacova, MD, PhD,
Associate Professor
Svetlana Lozovanu, MD, PhD,
Associate Professor
Tamara Tudose, MD, PhD, Associate
Professor
Tatiana Calalb, MD, PhD, Associate
Professor
Tatiana Chiru, MD, PhD, Associate
Professor
Tatiana Tazlavan, MD, PhD,
Associate Professor
Toader Timis, MD, PhD, Associate
Professor
Valentina Vorojbit, MD, PhD,
Associate Professor
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
12
Valentin Bendelic, MD, PhD, Associate Professor
Valeriu Cobet, MD, PhD, Associate
Professor
Vasile Culiuc, MD, PhD, Associate
Professor
Viorel Nacu, MD, PhD, Associate
Professor
Viorica Ochisor, MD, PhD, Associate
Professor
Vitalie Chirila, MD, PhD, Associate
Professor
Vitalie Ojovan, PhD, Associate
Professor
Uliana Tabuica, MD, PhD, Associate
Professor
Svetlana Turcan, MD, PhD, Senior
Scientific Researcher
Andrei Romancenco, MD, Director
of University Center for Simulation in
Medical Training
Corina Iliadi-Tulbure, MD, PhD,
University Assistant
Cristina Scerbatiuc, MD, PhD,
University Assistant
Diana Boleac, MD, PhD, University
Assistant
Diana Calaras, MD, PhD, University
Assistant
Irina Sagaidac, MD, PhD,
University Assistant
Svetlana Plamadeala, MD, PhD,
University Assistant
Zinaida Alexa, MD, PhD,
University Assistant
Alexandru Garbuz, MD,
University Assistant
Andrei Bradu, MD, University
Assistant
Constantin Ceclu, MD, University
Assistant
Cristina Ciobanu, MD, University
Assistant
Cristina Postaru, MD, University
Assistant
Daniela Cepoi-Bulgac, MD,
University Assistant
Daniela Rusnac, MD, University
Assistant
Ecaterina Carpenco, MD,
University Assistant
Elena Chitan, MD, University
Assistant
Egor Porosencov, MD, University
Assistant
Iulia Emet, MD, University
Assistant
Lilia Tacu, MD, University
Assistant
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
13
Natalia Bivol, MD, University
Assistant
Natalia Scurtov, MD, University
Assistant
Olga Cheptanaru, MD, University
Assistant
Radu Rusu, MD, University
Assistant
Rodica Stratu, MD, University
Assistant
Sergiu Ursul, MD, University
Assistant
Valentina Vilc, MD, University
Assistant
Victor Cazac, MD, University
Assistant
Victoria Simon, MD, University
Assistant
Vitalii Pintea, MD, University
Assistant
Vladislav Badan, MD, University
Assistant
Ion Banari, PhD, University
Assistant
Ludmila Rubanovici, PhD,
Lecturer
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
14
ABSTRACTS
CLINICAL CASES
DEPARTMENT OF SURGERY AND SEMIOLOGY no.3
1. PRIMARY HYDATID CYST OF SKELETAL MUSCLE: A CASE REPORT
Authors: Gutu Serghei, Predenciuc Alexandru
Scientific adviser: Popa Gheorghe, Associate professor, Department of General Surgery and
Semiology no.3
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Hydatid cyst, also called hydatidosis, is caused by Echinococcus granulosus. It is
still a major health problem in many parts of the world with 2-3 million cases confirmed each
year. Most of these cases involve liver (50-70%) and lungs (20-30%), but some of them have
rare locations, such as skeletal muscles (0.7-5%). The absence of specific clinical signs and
symptoms makes it difficult to establish a diagnosis, while first signs may appear as
neurovascular lesions due to compression. The most useful method of diagnosis is ultrasound
with high sensitivity (93-98%), followed by CT and MRI. There are two types of treatment: open
surgery and percutaneous drainage, both associated with Albendazole and Mebendazole or
Albendazole and Praziquantel administration.
Case report. A 33-year-old patient was admitted to Department of general surgery with a lump
on the inner proximal part of the right thigh that patient discovered six month ago, which
interfered with the patients daily activities. The patient underwent ultrasound exam of the lump
and internal abdominal organs, plain chest X-ray, lump puncture for bacteriological test and
general blood and urine analysis. All results came normal and with no imagistic findings, except
a multicystic lesion separated by septae that can be attributed to Gharbi type III hydatid cyst. The
patient underwent surgical treatment with no early postoperative complications and received
chemotherapy with Albendazole and Mebendazol.
Conclusions. Hydatid cyst should be included in the differential diagnosis of a patient with slow
growing subcutaneous masses. Imaging data are required when cystic mass are suspected.
Surgical treatment associated with chemotherapy must always be a fist priority for better results
with minimal recurrence.
Key words: hydatid cyst, ultrasound, differential diagnosis.
DEPARTMENT OF INTERNAL MEDICINE, CARDIOLOGY
2. LEFT ATRIAL MASS IN A PATIENT WITH MITRAL STENOSIS AND ATRIAL FIBRILLATION-THROMBUS OR MYXOMA?
Author: Timbur Natalia
Scientific advisers: Tasnic Mihail, Batrinac Aureliu, MD, PhD, Associate professor
Medpark International Hospital, Cardiology and Interventional Cardiology Department, Cardiac
Surgery Department of the Republic of Moldova
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. The discovery of a large left atrial mass through echocardiography obliges the
clinician to perform a differential diagnosis to distinguish tumor from thrombus. In fact,
magnetic resonance imagery could be useful to identify the mass but it could not distinguish
tumor from organized thrombus. Certainly, surgery is the best solution for a successful diagnosis.
http://cardiologie.usmf.md/en/
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
15
Case report. The 67-year-old woman was admitted to cardiology department with dyspnea,
orthopnea, palpitations, and fatigue. Anamnesis: 10 years of atrial fibrillation and type 2 diabetes
and 15 years with arterial hypertension. By the time of addressing, the patient has been
administering anticoagulants for several months with warfarin while maintaining INR-2.
Physical examination revealed an irregular pulse, at a rate of 110 beats/min. The
electrocardiogram revealed an atrial fibrillation with rate 150-100 b/min. The chest X-ray -
pulmonary congestion. TTE - revealed a severe mitral stenosis (GPmax – 33 mm/hg, area - 0,6
cm2) with third degree mitral regurgitation and left atrial mass (50*36 mm), third-degree
tricuspid regurgitation. Left atrium was enlarged (67*84 mm), severe pulmonary arterial
hypertension. These findings were confirmed by TEE. The preoperative coronarography showed
neovascularization among the mass and huge fistula from the circumflex artery in the tumour
mass and left atrium. We strongly suspected a vascular tumor, especially myxoma. Preoperative
decision was made to perform cardiac MRI - “hook”- shaped mass formation, fixed to the upper
rear wall of the LA, 7 cm long, massive thrombus. Cardio-surgical intervention was performed:
MV prosthesis MDT “Hancock-II ultra” N29, complex plastic repair of TrV, removing the
massive thrombus from the LA. After surgery, the patient had uncomplicated recovery.
Conclusions. Atrial mass management will be based on clinical history (mitral stenosis,
permanent atrial fibrillation) and echocardiographic data. If atrial mass persists during treatment
with anticoagulants, cardiac MRI and coronarography are useful for diagnosis. However, the
final diagnosis is established during cardiac surgery.
Key words: atrial fibrillation, atrial mass, MRI, coronarography, surgery
3. SITUS INVERSUS WITH DEXTROCARDIA AND AORTIC VALVE REGURGITATION: A CASE REPORT
Authors: Victoria Vatamanu-Paiu, Darciuc Radu
Scientific adviser: Batrinac Aureliu, MD, PhD, Associate professor
Medpark International Hospital, Cardiology and Interventional Cardiology Department, Cardiac
Surgery Department of the Republic of Moldova
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Dextrocardia with situs inversus is a rare congenital condition with less than 1
person in 10 000, in wich the internal organs are mirrored inside the human body. The majority
of the patients with dextrocardia and situs inversus are phenotypically normal and have a normal
life without any complications related to their congenital condition. About 5-10% of the these
patients develop another congenital defects. There are only few published cases of the patients
with situs inversus with dextrocardia associated with aortic valve regurgitation.
Case report. The 33 years old male with dextrocardia and situs inversus diagnosed in the
childhood was consulted during routine medical examination. Chest radiography showed
dextrocardia and situs inversus. The electrocardiogram showed sinus rhythm with right axis
deviation and reverse R-wave progression in the precordial leads. He was examined by
transthoracic echocardiography and third degree aortic regurgitation was found, moderate
dilatation of the sinus of Valsalva – 43 mm, and no dilatation of the ascending aorta – 35 mm.
There were no data for aortic dissection. The ejection fraction of the left ventricle was 55%.
Computer tomography (CT) showed reversed positioning of mediastinal and abdominal organs –
complete situs inversus and dextrocardia. On CT there were no signs of stenosis or dissections of
the thoracic and abdominal aorta. The patient was referred to cardiac surgery for correction of
valvular pathology. A complex aortic valve repair was performed. Postoperative period was
without complications. On control echocardiography after one month there was no important
aortic regurgitation.
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
16
Conclusions. Dextrocardia with situs inversus and aortic valve regurgitation is a very rare
cardiac pathology. If cardiac surgery is necessary it can be challenging but feasible with good
results.
Key words: dextrocardia, situs inversus, aortic regurgitation, CT, cardiac surgery
4. CEREBRAL COMPLICATIONS OF ATRIAL FIBRILLATION
Author: Victoria Panfili
Scientific adviser: Angela Tcaciuc, MD, PhD, Associate professor, Department of Cardiology
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Atrial fibrillation is one of the great problems that cardiologists around the world
are trying to solve, according to the World Heart Federation (WHF) between 1990 and 2013. The
total number of diagnosed AF cases has increased globally from less than 7 million to over 11
million, and this number continues to grow. The prevalence of AF varies between 0.5% and 1%
in the general population and increases in relation to age, exceeding 6% among subjects over 80
years old. The incidence of AF is between 0.21 and 0.41 per 1 000 persons/year. It is estimated
that by 2030, 14 - 17 million patients in the European Union will suffer from AF, plus 120 000 -
215 000 newly diagnosed patients per year. Taking into account th upper mentioned data, we
decided to examine atrial fibrillation complications, evaluate anticoagulant treatment and
maintenance of therapeutic INR importance in patients with AF, as well as the value of
kinetotherapy in patients with stroke.
Case report. We will present a clinical case, about a 65 years old female, who has been
suffering from AF for 5 years and who maintained INR (between 2 – 3) within the normal limits.
She had interrupted the administration of the anticoagulant treatment, prior to a mini-invasive
intervention, and as a result, the value of the INR has decreased < 1.1 in 4 days. The patient
underwent a cardioembolic stroke. We examined this patient, clinically and paraclinically. She
was examined before and after stroke, the following instrumental examinations being performed:
electrocardiogram, echocardiography, doppler of carotid arteries, and cerebral Computed
Tomography before and post fibrinolysis. We used CHA2DS2-VASc scores for AF stroke risk
(that was at that moment 4 points from 9), HAS-BLED scores for bleeding risk assessment (that
was at that moment 4 points from 9), and MMSE (Mini-Mental state Examination), for mental
status examination, that at the moment of stroke was 5 out of 30 points. Now the patient's
MMSE scores is 27 points because at the moment of the stroke the correct and fast measures
were taken the right pharmaceutical and kinetotherapeutical treatment were administered.
Conclusions. The risk of cardioembolic stroke to the patient with AF is very high and depends
on age and the presence of other comorbidities. Anticoagulant treatment in AF patients is
paramount, cessation of anticoagulant treatment leads to serious complications such as stroke.
Fibrinolytic therapy in stroke patients that is included in the therapeutic window significantly
reduces post-thromboembolic sequelae. Kinetotherapy has to be performed and individualized as
early as possible, which will allow the patient to recover spectacularly.
Key words: atrial fibrillation, stroke, anticoagulant treatment
5. TREATMENT FOR VENTRICULAR TACHYCARDIA IN THE ABSENCE OF STRUCTURAL HEART DISEASE.
Authors: Radu Darciuc1, Daniela Ivanov1, Eraslan Hakan2, Diker Erdem2 1Medpark International Hospital, Cardiology and Interventional Cardiology Department,
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova 2TOBB University of Economics and Technology Hospital, Cardiology Department, Ankara,
Turkey
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
17
Background. According to the recent data in up to 10% of the patients with ventricular
tachycardia (VT) there is an absence of structural heart disease. Several types of VT could be
present in such patients: right ventricular outflow tract (RVO T) VT, caticholaminergic
polymorphic VT, idiopathic left VT, Brugada syndrome, long QT syndrome. According to the
VT type the management can be pharmacological therapy, radio-frequency ablation,
implantation of cardioverter defibrillator or a combination of them. The decision about the
management is based on the type of VT, data obtained from echocardiography, magnetic
resonance imaging (MRI) and electrophysiological study (EPS).
Case report. We present a case of a 48 years old female who had frequent attacks of palpitations
with presyncopes. On Holter ECG monitoring there were 32066 premature ventricular
complexes (PVCs) and 493 non-sustaned episodes of VT during 24 hours with left bundle
branch block morphology, inferior axis and transition zone in V4. The patient could not receive
amiodarone because of an allergic reaction. Treatment with beta-blockers, verapamil and
propafenone was tried but with no sufficient improvement. On echocardiography and MRI she
had no structural heart disease. We suspected RVOT VT and evaluated the patient during EPS,
where RVOT VT was induced. The earliest activation point was find to be in postero-septal
RVOT area and several applications of radio-frequency energy were performed. Immediately
after ablation there were no more PVCs, with solitary PVCs in next days. She continued the
medical treatment with bisoprolol 5mg/day and propafenone 300 mg/day. We evaluated the
patient after one month on Holter ECG. There was a decrease of PVCs number to 4123, but were
137 non-sustained paroxysms of VT during 24 hours. We decided to repeat the ablation. On
basal ECG during second EPS there were no PVCs, but they appeared after dobutamine infusion.
Radio-frequency energy was applied in postero-septal RVOT area with disappearance of PVCs.
The patient continued the treatment with metoprolol 100mg/day. On Holter ECG monitoring
after one month there were 5195 PVCs during 48 hours and no more paroxysms of VT. We
recommended to continue the treatment with metoprolol 100md/day only.
Conclusions. Electrophysiological study is an important tool in evaluating ventricular
tachycardia and radio-frequency ablation is a therapy of choice is selected patients.
Key words: ventricular tachycardia, structural disease.
6. A CASE OF CHAGAS CARDIOMYOPATHY IN REPUBLIC OF MOLDOVA
Authors. Mihail Tasnic, Eraslan Hakan
Medpark International Hospital, Cardiology and Interventional Cardiology Department, Cardiac
Surgery Department of the Republic of Moldova
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Chagas disease (CD) (American trypanosomiasis) is generated by the protozoan
parasite Trypanosoma cruzi (T.cruzi) and transmitted by the reduviid bug in Latin America.
Approximately 8-12 million people are infected with T.cruzi in Central and South America.
Estimates of the number of annual deaths are around 50,000, 60% being related to sudden
cardiac death. Overall, 4.2% of Latin American individuals living in European countries are
chronically infected with T.cruzi.
Case report. We present the case of a young man of 29 years old, professional football player
originating from Brazil. The patient was admitted for establishing the cause of the patient
syncope developed during physical activity. The past medical history was without particularities.
We evaluated the patient by basic ECG, echocardiography, and effort test – all without
abnormalities. Holter ECG monitoring revealed multiple episodes of unstained ventricular
tachycardia and several episodes of complete atrioventricular block – maximal pause 3.5 sec. We
have also found frequent polymorphic ventricular extrasystole, disappearing during physical
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
18
effort. Biochemical panel was without abnormalities. Heart MRI showed multiple regions of
myocardial infiltration, and cardiosclerosis. The heart MRI image was typical for Chagas
cardiomyopathy, considering the patient origin. Because of the absence of experience with CD in
Republic of Moldova, we have sent the patient for serological evaluation in European cardiac
centers. Given the concomitant episodes of complete atrioventricular block, we couldn’t
prescribe any antiarrhythmic drug for the ventricular tachycardia. The patient was recommended
to avoid any physical activity. For arrhythmia control we indicated implantation of device with
pacemaker and ICD functions. Serological diagnosis of CD was thereafter confirmed. Patient got
recommendation to return in Brazil to the national center for Chagas disease, because of their
huge experience. In Brazil, during physical effort – playing football, patient suffered syncope
and died, probably because of malignant ventricular arrhythmia.
Conclusions. Heart diseases caused by different germs, atypical for Republic of Moldova or this
part of the Europe, should be taken in consideration in all causes of unexplained heart functional
or morphological abnormalities, especially in patients who are coming from other geographical
regions or travelling abroad.
Key words: Chagas disease, cardiomyopathy
7. PARTICULARITIES OF ACUTE MYOCARDIAL INFARCTION APPROACH IN A PATIENT WITH CORONARY ARTERIES ANOMALY
Authors. Constantin Cozma, Hakan Eraslan, Mihail Tasnic
Medpark International Hospital, Cardiology and Interventional Cardiology Department, Cardiac
Surgery Department
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Acute myocardial infarction among the young population is rare and presents
diagnostic and approach difficulties that lead to treatment delay in emergency cases and worse
outcome for patients. This case focuses on a young man who developed an inferior myocardial
infarction as a result of embolization of the left coronary artery system associated with the right
coronary anomaly.
Case report. A 25 year old man presented in the emergency room with a 4 hours history of
severe retrosternal crushing pain, radiating down his left arm and associated with sweating,
nausea, and breathlessness. He had never previously experienced chest pain at rest or on
exertion. He was a smoker. The last 2 weeks have been really stressful so the patient smoked
more than usual. He didn’t have a family history of ischaemic heart disease or sudden cardiac
death. At first examination he was pale and sweaty with a tachycardia of 110 beats/min. His
blood pressure was 140/100 mm Hg. Transthoracic echocardiography revealed hypokinesia of
the inferior wall. A coronary angiogram showed the absence of right coronary ostium (ostial
trombosis?) and filling of the right coronary artery through collateral vessels from the left
coronary system; LAD and OM I distal thrombosis. No right coronary ostium was observed in
the aortogram. None of the coronary arteries showed any sign of atherosclerosis. We performed
thrombolysis (Actilyse) with clinical and ECG improvement. After 72 hours angiography - LAD
and OM I successful total trombolysis, couldn't find RCA origin - suspicion of anomalous origin
of the right coronary artery. The patient was discharged on the 5th day of hospitalization in good
condition. Recommended: hereditary screening thrombophilia panel and Coronary CT
Angiography (CTA). CTA showed - Anomalous Right Coronary Artery From the Left Coronary
Sinus With an Interarterial Course, as well as right coronary artery ostial and proximal
hypoplasia, and a fistule LAD pulmonary artery RCA.
Conclusions.
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
19
1. Congenital ostial coronary artery atresia/hypoplasia should be a part of the differential
diagnosis particularly in young patients presenting with a totally occluded coronary artery and no
cardiovascular risk factors.
2. Thrombolysis can be a good choice for treatment of STEMI if primary PCI has failed.
3. Patients with suspicion of anomalous coronary arteries should perform CT angiography (CTA)
to confirm originated sites, anatomic route and whether complicated with other congenital
malformation.
Key words: myocardial infarction, coronary anomaly
8. SWITCHING THE LITTLE KIDS LIVES ON
Authors. Gratiana-Andreea Lates, Roberta Angheleanu, Anamaria-Romina Jugariu, Tímea
Katona, Razvan-Gabriel Budeanu
Scientific advisers: Valentin-Ionut Stroe, MD, PhD; Horatiu Suciu, MD, PhD, Professor
University of Medicine and Pharmacy of Targu Mures
Background. Cormatrix is an innovation in bioengineering, introduced in the medical world in
2013. The material is based on the extracellular matrix derived from the porcine intestine
submucosa, allowing for tissue restructure and growth in the "site" where it is used. The
composition consists of collagen, glycosaminoglycans, glycoproteins, proteoglycans and growth
factors VEGF, FGF. The superior characteristics are given by acellularity, resistance to infection,
anti-inflammatory effect and immunomodulator, the most important element being the reactivity
depending on the impulse from the tissue where it is involved.
Case report. At the Institute of Cardiovascular and Transplant Diseases in Targu Mures,
Cormatrix has been in used since 2013 and has been useful as a biocompatible tissue in arterial
switch procedures of transposition of great vessels. A 12 days old patient diagnosed with
transposition of great vessels was received by Institute of Cardiovasculare and Transplant
Diseases from Targu Mures for a arterial switch surgery. The surgery implies total
cardiopulmonary by-pass and at 26 Celsius degrees in the operating theater the great vessels are
cut from their emerging. The coronary arteries are excised from the future pulmonary artery and
reimplanted in neo-aortic wall; the resulting parietal defect after the coronary arteries excision is
repaired with a Cormatrix patch plasty. Literature showed that in 30% of cases where pericardial
patch was used it led to a pulmonary supravalvular stenosis. The post-surgery echographics at 3
months, 6 months and 1 years where Cormatrix was used showed no change in circulatory flow
in the pulmonary cormatrix patch segment.
Conclusions. In conclusion Cormatrix patch seems to have better results in reconstruction of the
pulmonary artery wall defects in transposition of great vessels surgery because it has a high level
of biocompatibility and a better reintegration in the vessel tissues .
Key words: cormatrix, bioengineering
9. SLEEP APNEA SYNDROME AS A CAUSE OF SEVERE PULMONARY HYPERTENSION
Author: Vlad Filimon
Scientific advisers: Filimon Silvia, David A., Sircu V., Institute of Cardiology, Institute of
Phtisiopneumology Chiril Draganiuc
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Sleep apnea is a disorder characterized by pauses in breathing or periods of
shallow breathing during sleep. There are three forms of sleep apnea: obstructive (OSA), central
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
20
(CSA), and a combination of the two called mixed. OSA affects 1 to 6% of adults and 2% of
children, but CSA affects less than 1% of people.
Case report. Patient X, 58 years old, of female, was admitted at the Institute of Cardiology with
mixed (inspiratory and expiratory) dyspnea at minimal effort, ankle swelling, general weakness,
dizziness. The patient suffers from arterial hypertension during 14-year with maximum levels
180/90 mmHg, working blood pressure being - 130/80 mmHg. At home regular treatment with
tab. Bisoprolol 2.5 mg in the morning, tab. Aspirin 75 mg/day, tab. Losartan 50 mg in the
evening, tab. Torasemidi 10 mg in the morning, over a day. The general condition worsened the
last month when signs of congestive heart failure progressed. The echocardiographical
examination revealed severe cardiomegaly (LA - 50 mm, LV - 60 mm, RA - 51 mm, RV - 40
mm), preserved left ventricular function (EF - 58%), reduced right ventricular function (TAPSE -
16 mm), severe pulmonary hypertension (PASP - 140 mmHg). To determine the cause of the
pulmonary hypertension, a number of investigations were performed. Pulmonary artery
angiography by computed tomography revealed pulmonary artery enlargement (40 mm) and
dilated intrapulmonary arteries, but no data on thrombosis. Spirography has revealed severe
changes in the function of external respiratory organs, being restrictive. Laboratory analyzes
excluded the systemic sclerodermia (ANA-negative, Anti Scl-70 antibodies – 1.5 U/ml, Anti
Centromer B antibodies – 0.3 U/ml) and normal values of D-dimers (0.24 ng/ml) excluded the
presence of venous thrombosis. To exclude the presence of Sleep Apnea Syndrome, cardio-
respiratory polygraphy was performed. A severe form of Sleep Apnea-Hypopnea Syndrome was
recorded, with the Apnea-Hypopnea Index (AHI) – 84.3/hour, with severe intermittent and
continue nocturnal hypoxemia in close correlation with respiratory events, having a Desaturation
Index (DI) – 82 6/hour. Average SaO2 – 69.6%, SaO2 minimum – 42%, SaO2
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
21
sphincterotomy was performed. Percutaneous transhepatic cholangiography and cannulation
guide wire technique was used, with a modified Burhenne technique. Stones were pushed into
the duodenum with Fogarty Balloon, stent inserted. Post interventional radiology revealed that
CBD was cleared. Patient made good recovery.
Conclusions. Elective methods in the diagnosis of choledocholithiasis are MRCP in
colangiographic regime, ERSP and percutaneous transhepatic cholangiography. Modified
Burhenne technique can be used in treating choledocholithiasis.
Key words: choledocolithiasis, biliary lithiasis, surgery
11. TRAUMATIC RECTAL WOUND AND CONSEQUENCES OF DIAGNOSTIC AND MANAGEMENT ERRORS
Author: Varvara Naghita
Scientific adviser: Rojnoveanu Gheorghe, MD, PhD, Professor, Department of Surgery no.1
Nicolae Anestiadi
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. “Hopkins Medicine” medical journal reports medical error as the third cause of
patients’ death. Meanwhile, WHO determined that 23% of European citizens state that they have
suffered from a medical error, while 18% say that they still have complications from them. Also,
WHO established that one of 20 patients got a nosocomial infection during their hospital
admission. Several studies highlighted a rate of 15% to 30% of rectal postoperative infection,
retrospectively linked to delayed diagnosis, fecaloid infection, inefficient primary treatment and
inadequate drainage. This affects the wound’s regeneration rate and leads to complications such
as perirectal abscesses and fistulas, suture inconsistency, sepsis etc., which can result in
prolonged hospital stay, hospital readmission, home nursing wound care needs, and the
expenditure of significant medical costs.
Case report. Patient R, age 52 years, is hospitalized with a perianal wound following a 1m fall
on a metal nail. Clinical and instrumental examinations showed stable hemodynamics, painless
palpation of the abdomen, no pneumoperitoneum. Status localis: perianal, on the right a wound 4
cm x 8 cm depth was detected. Primary surgical wound debridement was performed under
general anesthesia, and no lesions of the pelvic organs were discovered. Laparoscopy revealed a
retroperitoneal hematoma, which was drained, and no penetration into the abdomen cavity was
seen. The patient’s condition worsened on the second day and an exploratory laparotomy was
performed, where a second retroperitoneal hematoma and color changed blood in recto-sigma
was detected. A terminal sigmostoma was applied for the exclusion of the extraperitoneal lesion
of the rectum without succeeding in suturing the rectum wound. Subsequently, the evolution of
the patient was negative and a retroperitoneal phlegmon developed. A second laparotomy
followed with the suture of rectal wound and debridement of putrid retroperitoneal phlegmon.
The postoperative period evolves severely but favorably with the formation of the pararectal
fistula, which imposes multiple cares and readmissions over a period of 2 years with the intent of
closing the fistula (rectum stenting, reconstructive surgeries for rectum extirpation and the
transanal colon dissension, protection ileostoma) and, finally, a permanent terminal colostoma
was applied.
Conclusions. In the presented case, the severity of rectum wound, the delayed and wrong
diagnosis as well as the errors in patient approach had increased the severity of the disease, with
multiple postoperative complications, high medical costs and had led to disability.
Key words: traumatic rectum wound, diagnostic and tactical errors, complications, treatment.
12. A COMPLEX CASE OF PANCREATIC CANCER COMPLICATED WITH GASTRIC VARICES AND DEEP VEIN THROMBOSIS
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
22
Authors: Elena-Lavinia Pastramoiu, Viorel Moise
Scientific adviser: Motoc Radu
University of Medicine and Pharmacy of Targu Mures
Background. Pancreatic cancer is a highly lethal malignancy with few effective therapies.
Pancreatic cancer is often associated with thromboembolic disease, as the malignant condition
induces a prothrombotic and a hypercoagulable state.
Case report. This is a case of a 63 years old patient, diagnosed with pancreatic cancer with
hepatic and splenic metastasis detected on CT, with a level of Carbohydrate antigen (CA) 19-9
of 2556 UI/ml and several associated comorbidities: a moderate form of iron deficiency anemia (
Hb -7.4 g/dL, Ht - 25.2%, serum iron - 3.28 µmol/L), large gastric varices at the level of the
fornix secondary to segmental portal hypertension, but with no signs of bleeding, incomplete
intestinal metaplasia and Helicobacter Pylori infection at the level of the antrum and type 2
diabetes insulin dependent. The patient presented in our Medical Clinic complaining pain and
functional impotence of the right inferior limb. We performed a Doppler ultrasound that revealed
femoral-popliteal-tibial thrombosis of the right inferior limb and thrombosis of the internal
saphenous vein. Due to the association of the thrombotic disease with the gastric varices, the
initiation of antithrombotic therapy was questioned because of the high risk of variceal rupture
and massive bleeding. The patient was recommended endoscopic injection sclerotherapy, but the
procedure could not be performed due to the lack of compliance. A treatment the with low
molecular weight heparin (Fragmin 2500 IU) and Vessel Due F was initiated. The patient
condition was ameliorated during the admission and she was discharged with oncological and
gastroenterological follow-up.
Conclusions. The peculiarity of this case consists in the association of the thrombotic condition
with the gastric varices, both as complications of pancreatic cancer. The treatment in this case
has to be carefully chosen, as the patient is at high risk of developing both gastric bleeding and
thrombotic embolism.
Key words: pancreatic cancer, thromboembolism, gastric varices
DEPARTMENT OF PEDIATRICS
13. HIGH SERUM UNCONJUGATED BILIRUBIN LEVELS IN A PATIENT WITH MUTATIONS IN THE UGT1A1 GENE – CLINICAL CASE PRESENTATION
Author: Elena Ciumac
Scientific adviser: Donos Ala, MD, PhD, Professor, Department of Pediatrics
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. The UGT1A1 gene plays a significant role in the glucuronidation of bilirubin, and
the mutations of this gene lead to limitations in the synthesis of the glucuronyltransferase
enzyme, which contributes to the increase in free serum bilirubin. This clinical condition is
called Gilbert's syndrome. The patient with Gilbert syndrome has no clinical manifestations until
the second decade of life. Scientific studies demonstrate that free serum bilirubin in patients with
Gilbert syndrome is almost entirely unconjugated. We present the case study of a 17-year-old
patient with Gilbert's syndrome, confirmed by molecular genetics tests.
Case report. Patient was born from the first pregnancy with satisfactory evolution. Weight at
birth was 3500g, height 52 cm, Apgar score 8/8. She was breastfed until the age of 1.5 years.
Growth and development was within normal values, but after 4-5 years of age, she began to
manifest periodically poor appetite, vomiting, abdominal pain, constipation. The dynamical
assessment of clinical and paraclinical examinations revealed reactive pancreatitis episodes, “S”-
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
23
type gall bladder deformity, biliary stasis, hepatosplenomegaly (on ultrasonography non-
homogeneous aspect of parenchyma with mild to moderate increased echogenicity). At the age
of 10, she was diagnosed with left nephroptosis, secondary chronic pyelonephritis and chronic
cystitis. She was diagnosed with adenoiditis and chronic sinusitis, episodes of otitis. On July 20,
2015, patient presented with jaundice. The hemoleucogram revealed mild anemia (hemoglobin
was 112 g/l, erythrocyte 3.8 mln/mcl). The biochemical examination revealed increased bilirubin
levels, mainly on the basis of free bilirubin: total bilirubin was 36.0 mmol/l, conjugated bilirubin
was 9.0 mmol/l, free bilirubin 27.0 mmol/l. Serum glucose was at normal level (4.9 mmol/l),
thymol test - 1.0 (normal value). The transaminase levels were normal (ALT 13.6 IU, AST 20.1
IU). From the history, serum bilirubin levels were normal until adolescence. At the age of 17, the
level of bilirubin increased considerably, leading to suspected viral hepatitis, which could be
present considering that hepatitis was present in the family. For differential diagnosis purpose,
markers of viral hepatitis were tested: anti-HBs antibodies
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
24
which were successfully treated. On the 25th day of life, the newborn was transferred to the
neurosurgical unit for reservoir implant, cerebrospinal fluid (CSF) drainage and further
treatment. Due to the favorable evolution, after 20 days he was transferred back to the premature
care unit.
Conclusions. Recognition of early signs of intraventricular hemorrhage with catastrophic or
saltatory pattern, proper prenatal and neonatal care is essential in order to reduce mortality
among preterm newborns.
Key words: intraventricular Hemorrhage, ventriculomegaly, preterm infants
15. CLINICAL MANAGEMENT IN PREGNANCY COMPLICATED WITH HELLP SYNDROME. CLINICAL CASE PRESENTATION
Author: Valentina Gurau
Scientific adviser: Corina Iliadi-Tulbure, MD, PhD, Associate professor; Victor Petrov, MD,
PhD, Associate professor; Zinaida Sarbu, MD, PhD, Associate professor; Department of
Obstetrics and Gynecology no.2
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Preeclampsia complicates 2-3% of all pregnancies (5-7% in nulliparous women)
and remains a leading cause of maternal and perinatal mortality and morbidity. HELLP
syndrome is a rare manifestation of hypertensive diseases of pregnancy and represents the most
severe end of the pre-eclampsia spectrum. It occurs in 0.5 to 1% of all pregnancies and in 10-
20% of cases with severe preeclampsia. Although variable, the onset of the HELLP syndrome is
usually rapid.
Case report. Patient X, 31y.o, primigesta, 39 w.g. was admitted to the maternity unit
complaining of amniotic fluid leakage. She was not in labor on admission and her vital signs
were normal: blood pressure (BP) was 130/80 mm Hg, pulse - 76/min. Her antenatal history was
uneventful before this admission. Physical examination revealed peripheral edema, pathological
weight add + 17 kg. Vaginal delivery according to the protocol was established. Over one hour,
suddenly, the patient accused pronounced epigastric pain, occipital headache associated with
high BP 180/110 mm Hg. Laboratory investigations included: thrombocytopenia - 120×109 g/l,
leukocytosis - 12.4×109g/l. Liver function tests included increased concentrations of alkaline
phosphatase - 126 u/l, LDH - 4886 u/l, ALAT - 317 u/1, ASAT - 500 u/1. Urinalysis for protein -
4.32 g/l. On the background of hypotensive therapy, the 150/100 mm Hg BP and symptoms of
organ damage persisted. At this stage a diagnosis of HELLP syndrome was considered. In view
of the rapid progression of the disease and the gestational age, it was decided to proceed to
urgent delivery by caesarean section. One infant was delivered, with intrauterine growth
restriction (weight - 2390g). In dynamics, hemolysis syndrome is also associated (haemoglobin -
90 g/l, erythrocytes - 2.9×1012g/l, haematocrit - 0.27%). Postoperative period was complicated
by CID syndrome and acute renal failure. Clinical management was performed according to the
protocols and patient was discharged in satisfactory condition at 11th postpartum day.
Conclusions. HELLP syndrome is a severe complication of pregnancy, fulminant evolution
being frequently evaluated in primiparous without pre-existing medical conditions. Due to
maternal and fetal impact, HELLP syndrome needs an urgent delivery by caesarian section,
which is the essential method indicated in the severe form.
Key words: HELLP syndrome, pregnancy.
16. MANAGEMENT OF GIANT OVARIAN CYST IN PREGNANCY. CLINICAL CASE REPORT
Authors: Cristina Mursiev, Munteanu Igor
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
25
Scientific adviser: Iliadi-Tulbure Corina, MD, PhD, Associate professor; Sarbu Zinaida, MD,
PhD, Associate professor, Departement of Obstetrics and Gynecology no.2
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Ovarian cysts are met in women of various ages, most commonly occurring during
a woman's childbearing years, pregnant women not being an exception. Moreover, studies
conclude that ovarian cancer is among top five types of cancers detected during pregnancy. The
latest data show that the incidence of ovarian cysts in pregnancy varies from 0.15 to 5.7%
malignancies ranging from 0.8 to 13%. Their evolution is frequently hard to predict, some cysts
stop growing or disappear, while other may rupture, torsion or cause the obstruction of the
delivery pathways. Only ovarian cysts at risk of complication are to be considered. These are
mainly ovarian cysts, which, whatever their echogenic features, have a size ≥5 cm. Their
prevalence is estimated between 0.5 and 2 per thousand of pregnancies.
Case report. Patient X, 21 y.o., primigesta, pregnant 36-37 w. a., underwent a routine
gynecological and ultrasonographic examination, during which she was firstly diagnosed with a
giant 195x115 mm cyst in the projection of the right adnexa, supposedly originating from the
ovary. Considering the gestational term and the lack of data for cyst complications, an
expectative management was chosen and a re-evaluation was scheduled in two weeks.
Consequently, the woman was admitted to the IMSP IM and C 3rd level hospital for further
monitoring, investigations and establishing the optimal birth management. The next performed
USG showed that the dimensions of the cyst have grown to 223x123 mm, it was mainly situated
in the subhepatic space, it’s precise origin was hard to determine. It was decided to finish the
pregnancy via caesarean section and invite a general surgeon to the intervention, in case other
surgical manipulations would be needed. The tumoral markers were determined, with no
deviations found: CA125 – 13,5 (N≤ 35); HE4 – 35 (N≤70); ROMA index – 3,4 (N 0 – 11,4%).
At the term of 38-39 w.a. an elective caesarean section was performed. It was established that the
cyst had an ovarian origin and was fully extracted. The abdominal cavity was drained. Total
haemorage-800 ml. The woman and the newborn were discharged home on the 4th postoperatory
day. The histological exam revealed an ovarian dymorphus sero-mucinous cystadenome, with a
2+ to 3+ mucin reaction, follicular cysts and lonely, distrofic primordial follicles.
Conclusions. Though ovarian cysts are seldom met in pregnancy, their presence may have
serious repercussions on the evolution of the pregnancy and on the fetus. This is why, even in the
absence of symptoms, an USG supervision combined with other methods for diagnostic is
necessary. The decision upon the optimal birth way should be taken individually in each case,
the histological exam being crucial for establishing the final diagnosis.
Key words: ovarian cyst, pregnancy
DEPARTMENT OF INFECTIOUS DISEASES
17. DENGUE INFECTION: A CASE PRESENTATION
Author: Corina Pocnea
Scientific adviser: Gheorghe Placintă, MD, PhD, Associate professor, Department of Infectious
diseases
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Dengue disease is an acute viral illness with the common symptoms, such as: high
fever, muscle and joint pain, myalgia, cutaneous rash, hemorrhagic episodes. According to the
WHO, the number of cases increased to 390 million per year in more than 100 countries,
especially in the tropical and subtropical regions.
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
26
Case report. A 35-year-old woman from Chisinau, Republic of Moldova presented to the
Hospital of Infectious Diseases “T. Ciorba” with weakness, rash, fever 39C and pronounced
sweating. The first symptoms appeared on 21.01.2016 including strong headache and fever
38.4C. Then scarlatiform maculopapular rashes occurred on the upper chest, on the sternum, and
on shoulders. The eruption was red, confluent and without hemorrhagic component. On the fifth
day appeared myalgia in the thoracic region and in the iliac region. On the sixth day of illness,
the scarlatiform maculopapular rashes spread throughout the body. Bleeding signs were not
detected. On 26th January the patient addressed at Medpark hospital, where she had her blood
tests taken and was directed to the Hospital of Infection Diseases “T. Ciorba”. Epidemiological
anamnesis: on the 18th January 2016 the patient returned from Bali, Indonesia, where she spent
12 days with her girlfriend and girlfriend’s husband, who are from Moscow. She reported that
they were bitten by mosquitoes. Exactly the same day as the patient got sick, her girlfriend
started having fever and skin rash. On 27th January she addressed to the Infectious Disease
Hospital in Moscow, where the diagnosis of Dengue Fever was established to her. Laboratory
investigations: General blood analysis-erythrocytopenia (2.9*1012/L),
leucocytopenia(2.3*109/L) and lymphocytosis (51.7%). The biochemical analysis of the blood
didn’t show any pathological changes, as well as didn’t the general urinalysis.
Conclusions. Dengue Virus belongs to the same family of Flaviviridae as Zika Virus, also both
of them are tropical infections, spreaded in the same areas and transmitted by the same
mosquitoes. The vaccine was developed, but it’s not available in our country so for this patient
it’s important to avoid reinfection with other serotypes of the virus, which can therefore lead to
the development of Dengue shock syndrome. Early diagnosis of travel-imported cases is
important to reduce the risk of localized outbreaks of tropical arboviruses such as Dengue Virus
and the risk of local transmission from body fluids or vertical transmission.
Key words: dengue Virus, case report, infection.
DEPARTMENT OF NEUROSURGERY
18. ISOLATED POST STROKE EPILEPTIC SEIZURES IN WOMEN
Author: Victoria Duca
Scientific adviser: Mihail Gavriliuc, MD, PhD, Professor, Department of Neurology and
Neurosurgery.
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Introduction. Seizures are a known complication of stroke. They may increase the cerebral
lesions and induce epileptic status or encephalopathy. The correlation between brain structural
damage, epileptic foci, antiepileptic drugs and clinical outcome is unknown. Late-onset seizures
are thought to be caused by gliosis and the development of a meningocerebral cicatrix. Changes
in membrane properties, deafferentation, selective neuronal loss, and collateral sprouting may
result in hyperexcitability and neuronal synchrony strong enough to cause seizures. Can we
consider as Epilepsy one grand-mal seizure after a massive ischemic stroke?
Case report. A 41 year – old woman with a history of thrombosis of the right coronary artery,
myocardial infarction at the age of 35, was confirmed with primary antiphospholipid syndrome.
After two years, she developed cerebral infarction in MCA territory, and with mild left
hemiparesis she was hospitalized at the Neurological Institute. The 3T cerebral MRT was
performed on Siemens Magnetom Skyra 3T, and confirmed a large cerebral infarction in the right
hemisphere with a density of 12 UH, dimensions 9.0 x 5.0 x 6.0 cm without mass effect. She
continued anticoagulation therapy – warfarin – under the INR (2.0 - 2.5) control. At the age of 39
the patient developed a single generalized tonic - clonic epileptic seizure. Routine EEG,
prolonged EEG (2 hours) at the Nicolet EEG Wireless Amplifier System were performed. EEG
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
27
data showed focalized slow spike – wave: theta waves right F – C – T and T posterior spike.
Hyperventilation has induced F bilateral extension, without secondary generalization. Photic
stimulation test maintains focalized epileptic activity. Lamotrigine was initiated in increasing
doses reaching the therapeutic dose – 200 mg/24 hours. Epileptic seizures have not recurred.
Free period of seizures - 3 years with antiepileptic treatment. EEG and cerebral MRI monitoring
were performed regularly, once a year over the last 3 years. Cerebral MRI did not reveal adjacent
lesions. EEG showed the disappearance of sharp waves and the persistence of slow F – C right
waves.
Conclusions. According to the literature data, the seizures could repeat at any time, i.e. over 5
years or 10 after the stroke. In the 3-year period without seizures probably there was no
transformation of a structurally damaged brain into an epileptic one. The last definition of
epilepsy by R. Fisher confirmed that one epileptic seizure cannot be epilepsy. The severity and
location of the infarction advocates a vascular epilepsy, not epileptogenic foci.
Key words: stroke, seizures, antiepileptic drugs
19. TREATMENT OF CHRONIC LYMPHOCYTIC LEUKEMIA – A DIFFICULT CHOICE FOR SEVERE COMPLICATIONS: A CASE REPORT
Authors: Razvan-Gabriel Budeanu, Anamaria-Romina Jugariu, Timea Katona, Alexandru-
Emil Baetu, Gratiana-Andreea Lates
Scientific adviser: Ioan Macarie, MD, PhD, Associate professor
University of Medicine and Pharmacy of Targu Mures
Background. Chronic lymphocytic leukemia (CLL) is the most common form of adult leukemia
in the western European countries and is characterized by the relentless accumulation of
monoclonal B cells with the appearance of small mature lymphocytes and with a characteristic
immunophenotype. Even with the right treatment, this disease is known to have a variable
course: some patients die within one year after diagnosis while others live for longer than ten
years.
Case report. A 59-year-old female with a past medical history of ischemic cardiopathy and
hypothyroidism was admitted to the Haematology Unit of Mures County Emergency Hospital
with severe anemia, chronic fatigue and leukocytosis. After the anemia was corrected, the
diagnosis of chronic lymphocytic leukemia was confirmed by complete blood count and
immunophenotyping for which the patients was only observed for 2 years. Due to the secondary
severe anemia the treatment with Fludarabine is started as monochemotherapy first line
treatment. After one month the patient is hospitalized with severe anemia with Coombs’ test
positive for which methylprednisolone is administered for one week and COP chemotherapy is
induced. Because of the gastrointestinal side effects, the COP chemotherapy is ceased and
Fludarabine treatment is reintroduced. The treatment is continued for one year but the multiple
side effects (hemolytic anemia, herpes zoster, Listeria meningitis) determined cessation of
Fludarabine and Chlorambucil treatment was introduced. The treatment with Chlorambucil was
continued for 3 years. Even though the patient supported well the treatment, the splenomegaly
has progressively increased (from 3 cm to 8 cm) and the infectious diseases appeared
(Acinetobacter pneumonia and pharyngeal candidiasis).
Conclusions. Even though the treatment is accordingly to the actual international guides, the
individual responsibility to the drugs and the unpredictable evolution of this disease may be a
challenge in treating chronic lymphocytic leukemia.
Key words: chronic lymphocytic leukemia, treatment, drug selection, side effects
20. FORENSIC ASPECTS OF NON-TRAUMATIC INTRACEREBRAL HEMORRHAGE: A CASE REPORT
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
28
Authors: Tabian Daniel1, Diac Madalina1, Damian Simona Irina1,2, Riscanu Laura
Adriana1,2, Knieling A.1,2, Enea M.2 Scientific adviser: Bulgaru Iliescu Diana, MD, PhD, Associate professor 1Iasi Forensic Institute, Romania 2Grigore T. Popa University of Medicine and Pharmacy, Iasi, Romania
Background. Cases when unexpected death occurs, when the patient is in apparent health or the
event comes during presumably normal activity, especially when it is unwitnessed or when the
victim is found without apparent signs of foul play, may pose a significant challenge to the
coroner in reaching a proper determination of the cause and the manner of death. Spontaneous
intracerebral hemorrhage (ICH) is a bleeding into the parenchyma of the brain and accounts for
approximately 10 % to 20 % of all strokes. ICH is a multi-factorial disease caused by several
interacting and overlapping risk factors and etiologies. When massive ICH, not connected with
head trauma, has occurred, and it is multifocal or not located in one of the typical sites for
hypertensive hemorrhage, one of a multitude of other causes must be suspected. High alcohol
intake increases the risk of all stroke subtypes and of the development of liver diseases and may
induce hypertension, by affecting brain function and producing a series of alcohol-related or
alcohol caused diseases and is associated with changes in the coagulation system. Liver cirrhosis
is a well-known risk factor for ICH, due to impaired coagulation, despite the relatively rare
occurrence of ICH in cirrhotic patients.
Case report. The authors report a case of a 48 years old man, who was admitted in the
Neurosurgery Department, being found in the street, with a present state of consciousness,
presenting aphasia, right hemiplegia. The first computer tomography revealed left side temporal-
parietal-occipital intracerebral hematoma of 52/20/45 mm, postcentral intergyral subarachnoid
hemorrhage, and cerebral atrophy. On the second computer tomography, the lesions underwent
moderate resorption, and a conservative treatment for ICH was chosen. After 28 days from the
admission in the hospital, the patient died, due to a cardio-respiratory arrest. The release
diagnosis was: Left Side parietal-occipital itracerebral haematoma. Right hemiparesis. Hepatic
encephalopaty. Mixed decompensated alcoholic liver cirrhosis. Scleral and tegumentary
jaundice. Ascites. Hypersplenism. Severe thrombocytopenia. Hypoalbuminemia.
Bronchopneumonia. Schizophrenia. The body was brought for autopsy at the Iasi Forensic
Institute. The necropsic examinatiation revealed: right side occipital epicranial hemorrhagic
infiltration, a left side parietal-occipital lobe blood collection, cerebral oedema, pachypleuritis,
bronchopneumonia, ascites (5 liters), cirrhosis, and splenomegaly.
Conclusions. Proper documentation of injuries, along with history of the case, has a huge
importance in reaching a conclusion on both the cause and the manner of death. In this case, the
absence of external head injuries, the absence of underlying brain lesions that would be
suggestive for a head trauma, the presence of risk factors for primary non-traumatic ICH, make a
context in which the case may be properly interpreted.
Key words: Head injuries, intracerebral hemorrhage, case report.
21. FOSTER KENNEDY SYNDROME AS AN INITIAL PRESENTATION OF NEUROFIBROMATOSIS TYPE 2: A CASE REPORT
Authors: Alexandru Sumleanschi, Serghei Borodin
Scientific adviser: Aureliu Bodiu, MD, PhD, Professor, Department of Neurosurgery, Republican
Clinical Hospital
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
29
Background. Foster Kennedy syndrome (FKS) is described as ipsilateral optic atrophy and
contralateral papilledema from an intracranial mass. FKS is uncommon manifestation of
Neurofibromatosis type 2 (NF2), which is generally presented with hearing loss and tinnitus.
Case report. In this report we present a 26-year-old female with the atypical presentation of
NF2. First symptoms were progressive vision loss and cognitive dysfunction. Ophthalmological
examination revealed right-sided papilledema and left-sided optic atrophy. Magnetic resonance
imaging (MRI) of the brain revealed bilateral vestibulocochlear schwannoma and three
intracranial meningiomas, involving the parafalcine region and the olfactory groove. Whole
spine MRI showed one intramedullary tumor at C1-C2 level, multiple spinal canal nodules in
cervico-dorsal regions and one Th12-L2 extramedullary tumor. Based on clinical and imaging
findings the diagnosis of neurofibromatosis type 2 was established. The patient underwent
surgical resection of giant parasagittal meningioma, subtotal resection of the olfactory groove
meningioma and total resection of Th12-L2 meningioma. Six months after brain surgery, she
underwent Gamma knife radiosurgery for remnant frontobasal meningioma and for both
vestibulocochlear schwannomas. Despite the combined treatment of intracranial lesions, only an
insignificant vision improvement was achieved.
Conclusions. FKS can be the presenting symptom of NF2. Early detection and treatment of
ophthalmologic manifestations of NF2 may prevent amblyopia development.
Key words: Foster Kennedy syndrome, neurofibromatosis type 2, intracranial meningioma,
intramedullary tumor, extramedullary tumor
DEPARTMENT OF NEUROLOGY no.1
22. INTRACEREBRAL HEMORRHAGE IN A PATIENT WITH MOYAMOYA SYNDROME: CASE REPORT
Authors: Pavel Gavriliuc1, 2, Elena Costru-Tașnic1, Tatiana Pleșcan1, Dacin Ianuș2
Scientific adviser: Gavriliuc Mihail1, MD, PhD, Professor, Department of Neurology and
Neurosurgery 1Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova 2Institute of Neurology and Neurosurgery of the Republic of Moldova
Background. Moyamoya disease is a cerebrovascular disease that is characterized by bilateral
chronic and progressive stenosis or occlusion of the arteries around the circle of Willis with
development of collateral circulation, of unknown etiology. It has a high incidence in Japan and
Asian population, with fewer cases described in Europe. Similar angiographic findings can be
seen in patients with other medical conditions that are described as Moyamoya syndrome. Main
clinical features include transient ischemic attacks, ischemic strokes, and hemorrhagic strokes.
Case report. We describe a 38-year-old female patient that presented with an intracerebral
hemorrhage with a typical location for hypertensive bleeds. She had no vascular risk factors, but
a high normal blood pressure (140/90 mmHg), and elevated ESR. A magnetic resonance
angiography showed occlusion of internal carotid artery with development of collateral cerebral
circulation on the side of the bleeding. Unilateral affection and elevated ESR were more
characteristic for a moyamoya syndrome within a systemic disease.
Conclusions. Despite a typical hypertensive location of the bleeding, vascular imaging is
warranted in all patients with intracerebral bleedings to evaluate for atypical etiologies. Our case
represents a patient that might benefit from revascularization surgery in the context of
multifactorial risk factor control.
Key words: Moyamoya syndrome, stroke, hemorrhage, intracerebral, collateral flow.
23. POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME MIMICKING
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
30
STROKE IN A YOUNG WOMAN
Authors: Elena Costru-Tasnic1, Pavel Gavriliuc1,2, Tatiana Plescan2, Olesea Odainic2
Scientific adviser: Mihail Gavriliuc1, MD, PhD, Professor, Department of Neurology and
Neurosurgery 1Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova 2Institute of Neurology and Neurosurgery of the Republic of Moldova
Background. Stroke in young patients (
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
31
min and 5 minutes respectively. The patient developed respiratory distress syndrome in the first
few hours. He had inter- and subcostal retractions, grunting, tachypnea (80 breaths per minute),
nasal flaring and the pulse was 127 beats per minute with a SpO2 under 90% in room air and
higher than 95% with oxygen supplementation. The treatment with Dexamethasone showed no
improvement and an urgent Chest X ray was ordered which revealed a left pneumothorax with
mediastinal shift to the opposite site. ABG revealed severe acidosis. (pH – 7.13, PCO2 – 70, PO2
– 46 mmHg). In view of impending respiratory failure and shock baby was intubated, the
pneumothorax was drained. Hemoculture was positive with GBS. The antibiotic therapy
(Ampicillin/Sulbactam and Amikacin) was started and the patient was carefully monitored.
Conclusions. In conclusion, although respiratory distress syndrome is rare in near term or term
newborn, is usually secondary to a parenchimal pathology, being a common case of spontaneous
pneumothorax in these infants. Early recognition and treatment is life saving. Usual
manifestation is progressive respiratory difficulty starting soon after birth.
Key words: GBS infection, respiratory distress, near term infant, spontaneous pneumothorax
DEPARTMENT OF MOLECULAR BIOLOGY AND HUMAN GENETICS
25. DUCHENNE MUSCULAR DYSTROPHY AND LIMB-GIRDLE MUSCULAR DYSTROPHY: CLINICAL CASES
Author: Nadejda Bejan
Scientific adviser: Sprincean Mariana, MD, PhD, Associate professor, Department of Molecular
Biology and Human Genetics
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background : Muscular dystrophies (MD) represent a large group of genetic disorders that are
manifested by progressive increase of muscle weakness. Duchenne muscular dystrophy (DMD)
is an X-linked disorder and limb-girdle muscular dystrophies (LGMDs) include over thirty
subtypes, that are classified in autosomal dominant (1A-1H) and recessive (2A-2W). Our aims
was to highlight the clinical and genetic aspects in MD by reporting two clinical cases with the
aim of improving the early diagnosis.
Case report. The study was performed on the basis of the literature review and presentation of
two clinical cases: a 6-year-old boy with DMD and another 17 years old boy with LGMD.
Patient G.V. was diagnosed with DMD at the age of 3 years. Electroneuromyography (ENMG)
and genetic test (deletion of exons 45-52 in the dystrophin gene) confirmed the diagnosis. He has
the following clinical signs: calf pseudohypertrophy, waddling gait, lordosis, elevated serum
creatine kinase (CK) - 14 740 U/l, MB fraction – 833 U/l, lactate dehydrogenase (LDH) – 1934
U/l. Patient M.A. was diagnosed with LGMD at the age of 7 years through ENMG. He presents
severe motor deficit, waddling gait, hypoplasia of the thigh muscles, permanent asthenia, total
CK - 486 U/l, MB fraction - 36 U/l, LDH - 358 U/l. He has first-degree disability and
cardiomyopathy.
Conclusions. The first signs of MD (DMD and LGMD) occur at early stages, but often are not
recognized. Genetic counseling and prenatal diagnosis will significantly reduce morbidity and
mortality, will contribute to the improving of the quality of life.
Key words: Muscular dystrophies (MD), Duchenne muscular dystrophy (DMD), limb-girdle
muscular dystrophies (LGMDs).
26. THE CLINICAL-GENETIC PARTICULARITIES IN APERT SYNDROME
Authors: Olga Nadjmacova, Tatiana Țurcanu
-
The 7th International Medical Congress for Students and Young Doctors ____________________________________________________________________________________
32
Scientific adviser: Sprincean Mariana, MD, PhD, associate professor, Department of Molecular
Biology and Human Genetics
Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova
Background. Apert syndrome (AS) is a dominant autosomal genetic disorder caused by
heterogeneous mutation in FGFR2 genes on chromosome 10q26 and belongs to a group of
disorders known as craniofacial congenital malformations. AS can promote the premature fusion
of bones in the skull, hands, and feet. The incidence of infants born with Apert syndrome is
approximately 1 in 50000 to 80000. In this study is emphasized the importance of clinical and
genetic approaches in the research on the specific diagnosis in patients with Apert syndrome.
Case report. The clinical particularities of Apert syndrome are determined by craniosynostosis
result from the premature fusion of the skull bones. The child present following clinical features:
short anterioposterior diameter with high forehead and flat occiput, flat facies, shallow orbits,
proptosis, hypertelorism, small nose, maxillary hypoplasia, a cleft palate, low set ears, and
cutaneous syndactyly of the fingers and toes. The neuroimaging of the head revealed
craniosynostosis of the skull bones. The diagnosis of Apert syndrome was confirmed by clinical
manifestations and paraclinical investigations. The treatment of Apert syndrome is directed
toward the specific symptoms that are apparent in each individual.
C








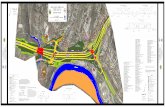







![[XLS]engineeringstudentsdata.comengineeringstudentsdata.com/downloads/2018/2018 AP... · Web view2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018 2018](https://static.fdocuments.in/doc/165x107/5ad1e56f7f8b9a482c8bcbab/xlseng-apweb-view2018-2018-2018-2018-2018-2018-2018-2018-2018-2018-2018-2018.jpg)


