Abdominal Aortic Aneurysm - Wikipedia, The Free Encyclopedia
Abdominal Aortic Aneurysm
-
Upload
alebelucci69 -
Category
Documents
-
view
20 -
download
0
Transcript of Abdominal Aortic Aneurysm
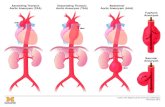
Types of Aneurysms True vs. False (pseudoaneurysm)
True: involves all 3 layers of the arterial wall
False: presence of blood flow outside of normal layers of arterial wall. Wall of false aneurysm is compose of the compressed, surrounding tissues.
Types of Aneurysms Etiology
Degenerative- complex process that involves some degree of calcification, atherosclerotic pathology as well as degeneration by MMPs.
Inflammatory- thick inflammatory wall with fibrotic process in retroperitoneum that can encase aorta as well as surrounding structures. Associated with other inflammatory conditions : Takayasu’s, Giant cell arteritis, Polyarteritis nodosa, Behcet’s, Cogans’.
Post-dissection- up to 20% of aneurysms are related to previous dissection. Overtime, develops into true aneurysm
Traumatic- false aneurysms Developmental Anomalies- persistent sciatic arteries, aberrant right
subclavian artery. Infectious- Can be primary or secondary infections. Congenital- Tuberous sclerosis, aortic coarctation, Marfan’s.
Assessing the AAA patient Normal - aorta 1-2.4cm & iliac 0.6-1.2cm Aneurysm - Aorta >3cm & iliac > 2cm RF for aneurysm
Older age, male gender, white race, positive family history, smoking, HTN, hypercholesterolemia, PVD, CAD.
Ultrasound used to diagnose and monitor AAA until aneurysm
approaches size at which repair considered. Computed Tomography
used in preop assessment of AAA.
Ruptured AAA No significant overall change in mortality with
open repair from 1991-2006 Overall mortality for ruptured AAA = 90%
Mortality rate for patients who arrive at hosptial alive = 40-70%
High postop mortality rate due to MI, renal failure, and multi-organ failure Ischemia-reperfusion injury, hemorrhagic shock, lower
torso ischemia rEVAR significantly reduces mortality of ruptured
AAA patients (31 vs 50%)
Screening for AAA US Preventive Services Task Force
Men 65-75 yo who have ever smoked No for or against men 65-75yo who have never smoked Does not recommend screening for women
Society of Vascular Surgery, Medicare Screening Men who have smoked at least 100 cigarettes during
their life men and women with a family history of AAA
Only screen patients who are candidates for repair.
Choosing between Surgery & Observation
1. Risk for AAA rupture without surgery
2. Operative risk of repair
3. Patient’s life expectancy
4. Personal preferance of patient
1. Risk of Rupture Size matters:
Aneurysm > 5cm 6-16% and > 7cm 33% annual rupture rate
Wall stress analysis Saccular aneurysm have higher rate of rupture HTN, COPD, active smoking are independent
predictors of rupture (+) family hx tend to rupture Expansion rate
2. Operative Risk of Repair Mortality after:
elective open AAA ~ 5% EVAR 1%
6 independent RF’s for mortality Open repair Creatinine > 1.8, CHF, EKG detected ischemia,
Pulmonary dysfunction, older age, female gender. Cardiac, pulmonary, renal, and GI risks with
each proceudre.
3. Patient’s Life Expectancy Very difficult to assess due to patient’s
co-morbidities Typical 60yo surviving AAA repair has
13year life-expectacy, 70yo has 10year life-expectancy, and 80 yo has 6 year life-expectancy.
4. Personal Preference of Patient Fear of AAA vs. Fear of surgery Anecdotal experiences of friends and
family Procedures provided in community by
interventional specialists and surgeons.
Medical Management of AAA Smoking Cessation- Single most important modifiable risk factor Exercise Therapy- Evidence suggests may benefit small
aneurysms Beta Blockers- May decrease the rate of expansion? Important
cardiovascular effects thus use advocated. ACE inhibitors- Evidence is mixed, however, implicated in less
aneurysm rupture. Doxycycline
Antibiotic activiety against chlamydia species Suppresses expression of MMP
Statins - associated with reduced aneurysm expansion rates. Decreases MMP-9 in aneurysm wall.
EVAR vs. OPEN EVAR-1 and DREAM Trials
Randomized AAA > 5.5 cm to EVAR vs. open repair Lower 30-day mortality for EVAR (1.6% EVAR vs.
4.6% open) Peripop mortality and severe complications 4.7%
EVAR & 9.8% open repair (DREAM) Similar all-cause mortality at 2 years Higher rate of secondary interventions in EVAR
group Total cost of Tx & 4 years of f/u is significantly
increased for EVAR.
Open Repair Transabdominal Approach
Previous retroperitoneal surgery
Ruptured AAA Exposure of mid/distal
portions of visceral vessels or R renal artery
R internal or external iliac artery
Co-existant abdominal pathology
Left-sided vena cava
Retroperitoneal Approach
Mult. Previous intraperitoneal procedures
Abd wall stoma, ectopic/ anomaly of kidney
Inflammatory aneurysm Proximal aortic access,
endarterectomy of viceral/renal arteries needed
Obese patients Fewer GI complications
Open Repair-Complications Cardiac Pulmonary Renal Lower Extremity Ischemia Spinal Cord Ischemia Incisional Hernia
14.2% ventral hernia, 9.7% SBO Graft Infection
Open Repair Complications:Colon Ischemia
Collaterals from SMA, IMA, internal iliac artery, and profunda femoris supply sigmoid colon
Mortality 40-65%, full-thickness necrosis 80-100% Occurs in 0.6-3% of elective and 7-27% of ruptured
AAA (much more common endoscopically than clinically)
Si/Sx: persistent acidosis & shock, increased WBCs and lactate levels, fluid sequestration, bloody bowel movements.
TX: Ischemia limited to mucosa/submucosa- npo, IVF, IV abx Transmural ischemia- bowel resection, fecal diversion, creation
of ostomy, washout of abdomen, IV abx.
Open Repair- Concomitant Pathology Treat the most life-threatening process first Avoid simultaneous operations that increase the risk
for prosthetic graft infection If secondary procedure can be staged without
increased risk - do aneurysm repair first Clean procedures (ie:nephrectomy, oophrectomy) can
be performed simultaneously with open AAA repair GI procedures should not occur at same time as open
repair Abort surgery if metastatic disease or abscesses which
increase risk for graft infection discovered.
Inflammatory AAA Perianeurysmal fibrosis & inflammation 5% of AAA Treatment of AAA resolves the periaortic
inflammation in 53% (open & EVAR) Duodenum, left renal vein, and ureters often
involved in inflammation. PreOp ureteral stent placement
recommended.
Infected AAA 0.65% of AAA Can be primary or secondary infection Potential causes of infection:
Continguous spread of local infxn, septic embolization from distal site, bacteremia.
In the past syphilis and steptococcal species was common: Now: staph and salmonella.
With HIV and wide-spread abx use- can be caused by any bacterial or fungal infection
Dx: fever, abdominal/back pain, high ESR, bacteremia.
Types of Endoleak Type I
Usually identified and treated @ time of stent graft implantation Must be treated if found on post-op imaging Associated with high likelihood of AAA rupture Bridge with short aortic cuff, Palmaz stent
Type II 10-20% of post-op CT scan show Type II leak 80% resolve spontaneously at 6 months Indication to treat: persistent leak, aneurysm growth Transcatheter tx (coil embolization)
Type III 0-1.5% incidence Strong predictor of rupture Tx: re-establish continuity by additional component to bridge gap or cover
hole. Type IV
Majority resolve within one month of stent graft implantation
EVAR Complications:EuroSTAR Registry
Annual Incidence of Complication (per 1,000 patients)
From Van Marrewijk CJ, Leurs LJ, Valabhaneni SR, et al. Risk-adjusted outcome analysis of endovascular abdominal aortic aneurysm repair. J Endovasc Ther. 2005; 12; 417-429
AneuRx Ancure Excluder Talent Zenith
Type I & II endoleak
52 86 50 66 41
Migration 43 5 11 24 7
Graft Occlusion
19 33 11 23 35
Rupture 4 0 1 5 2
EVAR complications Stent-graft infection
Net infection rate of 0.43% Pelvic ischemia
Internal iliac occlusion during EVAR Si/sx: buttock claudication (most common
16-50%), buttock necrosis, colon necrosis, spinal ischemia, lumbosacral plexus ischemia, ED (15-17%).
Ischemic colitis < 2%
Long-Term Outcome of Open or Endovascular Repair of Abdominal Aortic Aneurysm
De Bruin et al.
DREAM study groupThe New England Journal of Medicine
May 2010
Introduction Previous studies have shown initial survival benefit in
patients undergoing EVAR vs. Open repair of AAA
Concern that EVAR is not as durable as AAA and is associated with greater risk of rupture and secondary interventions.
Goal: Analyze results of Dutch Randomized Endovascular Aneurysm Repair (DREAM) study to provide long-term data comparing open repair vs. EVAR
Methods Multicenter, randomized, controlled trial comparing open
repair vs. EVAR in 351 patients AAA > 5cm Patients had to be candidates for both techniques of
repair Exclusion Criteria:
Ruptured or inflammatory aneurysms, anatomical variations, connective-tissue diseases, hx of organ transplant or life-expectancy < 2 years.
F/U visits at 30 days, 6/12/18/24months after procedure After first 2 years, pts received questionnaires every 6
months.
Methods EVAR patient received CT scan annually All patients were called at 5 years and invited
for f/u CT scan. Data acquisition stopped Feb 2009 Primary outcome was rate of death from any
cause & reintervention Survival calculated on intention-to-treat basis.
Results November 2000-December 2003 178 patients Open repair vs. 173 EVAR Mean age 7yo, 91% male, 43.9% concomittant
cardiac disease. 6 pts did not undergo aneurysm repair
4 declined tx, 1 died from rupture, 1 died from PNA.
8 in hosptial deaths open vs. 2 EVAR Mean f/u 6.4 years 25% of open patient underwent CT scan at 5
years, 100% of EVAR
Results @ 6 years post-op:
Survival rate: 69.9% open, 68.9% EVAR Freedom from reintervention: 81.9% open vs.
70.4% EVAR Analysis of causes of death
EVAR- mostly miscellaneous rather than CV Reintervention
Open repair- majority done for hernia repair EVAR- endoleak, endograft migration
Discussion “No significant difference between
endovascular repair and open repair in rate of overall survival at a median of 6.4 years.”
Previously DREAM and EVAR-1 trials demonstrated early (2years) survival advantage for EVAR group.
Significantly higher rate of reinterventions in EVAR group than open group
Study limited by difference in f/u between the open and endovascular group.
Conclusion At 6 years, Open repair and EVAR have
similar rates of suvival EVAR has a greater rate of
reintervention
Total Percutaneous Access for Endovascular Aortic Aneurysm Repair (“Preclose” technique)
Lee WA, Brown MP, Nelson PR, Huber TS.
Journal of Vascular Surgery 2007 June; 45(6):1095-101
University of Florida, Gainesville
large single institutional experience with the method and outcomes of a variation of the Preclose technique using the 6F Perclose Proglide (Abbott Vascular) device during endovascular aortic repairs.
Retrospective review of patient who underwent EVAR/TEVAR from Oct 03-Aug06
183 perc femoral access with 12-24F Perclose technique with Proglide device compared to 154 patients with open surgical exposure of femoral arteries
Anesthia used for Preclose vs. open: general, 49% vs 55%; regional, 45% vs 44%; and local, 5% vs 1% (P = .10).
Percutaneous group broken down into group of smaller 12-16F and group of larger 18-24F sheaths.
Data points: perioperative outcomes, procedure times, operating room usage costs, and technical success (in-hospital or 30-day).
F/U: CT scan at 1 month post-op The list price for each Perclose Proglide device is (US) $295.
Dilator set $170.44 cost of the operating room is (US) $3935 for the first 60 minutes
(not prorated for shorter periods) and then $50/min thereafter.
Results 137 EVAR, 118 TEVAR, 7 iliac repairs performed 381 femoral arteries accessed with 12-24F sheaths
279 were with 559 Proglide devices using Preclose technique in 183 patients
4 femoral artereries required 1 device (1.4%) -all 12F sheaths
270 arteries (96.8%) required 2 devices 5 arteries (1.8%) required 3 devices 63% of sheaths were > 18F
Overall technical success of Preclose technique was 94.3%
99% for smaller sheaths and 91% for larger sheaths.
Results 16 complications
13 open repairs of femoral arteries 2 emergent placement of covered stent for severe
retroperitoneal hemorrhage. 1 necrotizing arteritis with mycotic
pseudoaneurysm requiring replacement of femoral artery with autogenous femoral vein.
All cause mortality 2.2% Access mortality 0%
Results Surgical Group- 154 endovascular repairs
108 EVAR and 46 TEVAR 258 femoral exposures
Technical success rate 93.8% 16 complications
10 endarterectomies with patch angioplasty 3 wound infections 2 infected seromas requiring I&D 1 severe arteritis requiring debridement and replacement
of CFA with autogenous femoral vein. All cause mortality 1.3% 0% access-related mortality
Results Significantly lower OR time for Preclose
group: EVAR: 115 vs 128 min TEVAR: 80 vs 112 min
Cost: OR + Proglide vs. OR+ Surgery EVAR: $7881 vs $7351 TEVAR: $5679 vs $6556
Discussion Percutaneous Access
Shorter procedure time Fewer wound complications Increased patient comfort Limited by size of delivery system.
In this study: Smaller sheaths had higher technical success All complications occurred intra-op No access-related mortality Accessing anterior aspect of mid-common femoral artery is
crucial in preventing hemorrhagic complications.
Discussion Contraindications to Preclose:
Coagulopathy is contra-indication to use of this device due to inability to control “needle-hole bleeding”
Severe calcifications Groin scarring Obesity Previous use of percutaneous closure devices. High (suprainguinal ligament) femoral bifurcation Need for frequent introducer sheath removals and insertions Proximal iliac occlusive disease Small iliofemoral arteries relative to profile of device being
used
Conclusion Prospective, randomized study is
needed to truly validate this technique Percutaneous EVAR is safe and
effective Long-term data is needed to evaluate
effect on femoral artery.