ab
-
Upload
heather-ryan -
Category
Documents
-
view
218 -
download
1
Transcript of ab

Clinical Paper
TMJ Disorders/Facial Pain
Int. J. Oral Maxillofac. Surg. 2010; 39: 767–773doi:10.1016/j.ijom.2010.03.025, available online at http://www.sciencedirect.com
Effects of myogenous facialpain on muscle activity of headand neck
A. Monaco, A. Spadaro, R. Cattaneo, M. Giannoni: Effects of myogenous facial painon muscle activity of head and neck. Int. J. Oral Maxillofac. Surg. 2010; 39: 767–773.# 2010 International Association of Oral and Maxillofacial Surgeons. Published byElsevier Ltd. All rights reserved.0901-5027/080767 + 07 $36.00/0 # 2010 Inte
rnational Association of Oral and Maxillofacial SurgeA. Monaco1,a, A. Spadaro1,a,R. Cattaneo1,a, M. Giannoni2,3,a
1Department of Gnatology and ProstethicDentistry, School of Dentistry, University ofL’Aquila, Italy; 2Department ofOdontostomatological Clinic, School ofDentistry, University of L’Aquila, Italy;3Department of Surgical Science, School ofDentistry, University of L’Aquila, Italy
Abstract. This study evaluated the effects of visual input on surfaceelectromyography (sEMG) of some stomathognatic and neck muscles (anteriortemporalis, masseter, anterior digastric and sternocleidomastoid muscles) inpatients experiencing myogenous facial pain compared with healthy volunteers. Allsubjects kept the mandible at rest with teeth apart and underwent a 15-s sEMGrecording of anterior temporalis, masseter, digastric and sternocleidomastoidmuscles. Each recording was carried out with closed and then open eyes. The sEMGactivity of each muscle was compared between the two groups. In the study group,anterior temporalis, masseter and sternocleidomastoid sEMG with closed eyesshowed higher values compared with controls (p < 0.05). In the study group, leftand right anterior temporalis (p < 0.003) and right digastric (p < 0.03) sEMG withopen eyes showed higher values than sEMG with closed eyes. In the control groupno significant differences were observed between closed and open eyes. In patientswith myogenous facial pain, visual input appears to be associated with a significantincrease in the sEMG activity of some head and neck muscles.
Key words: myogenous facial pain; muscleactivity; head; neck; facial pain.
Accepted for publication 19 March 2010Available online 2 May 2010
a These authors contributed equally to thiswork.
Myogenous facial pain is defined as facialpain that originates from the musculoske-letal structures of the masticatory system.The pain is usually exacerbated by chew-ing or other jaw functions and is oftenaccompanied, singularly or in combina-tion, by limitation of jaw movement, mus-cular and fascial tenderness or jointsoreness20. It appears to be multifactorial,potentially involving a complex interplayof anatomic structures, biomechanicalfunction, environmental demands and psy-chosocial responses, each capable of con-tributing to clinical manifestations andsymptoms14.
Myogenous facial pain is a commonsymptom of temporomandibular disorders(TMD). Myogenous facial pain affectsseveral muscle parameters leading toreduction in maximal voluntary bite force,endurance time and extended recoverytime7.
The aetiology and pathophysiology ofmyogenous facial pain are not fully under-stood. Treatment modalities are non-spe-cific and do not directly target thecausative factors. Surface electromyogra-phy (sEMG) has been used to evaluate themuscle activity of patients suffering frommyogenous facial pain. It has been sug-
gested that the mandible elevator musclesof individuals with dental Class I pain(Angle’s classification) without myogen-ous facial pain signs or symptoms3 withthe mandible at rest and in the absence ofexteroceptive stimuli, showed constantsEMG values ranging from 1.4 to2.2 mV6,25.
It is debatable whether patients suffer-ing from myogenous facial pain showhigher rest sEMG values of the anteriortemporalis, masseter, sternomastoid and
ons. Published by Elsevier Ltd. All rights reserved.

768 Monaco et al.
digastric muscles compared with healthypeople. A source of uncertainty could bethat previous studies did not make clearwhether individuals were recorded withtheir eyes open or closed; because visionplays an important role in the multisensoryprocess of postural stabilisation.
Visual input can be used by oculomotormuscular systems and neck/trunk musclesto follow a moving object32. Ocular nucleicontrol the eye position in the orbit; theysend fibres to the nuclei that control neckand head movements and receive afferentinput from vestibular nuclei. It has beenobserved that a modification of ocularproprioception modifies head and bodyposture1,3,27. The role of trigeminal affer-ences on tonic-postural regulation hasbeen recorded17.
In this complex system, adaptive mod-ifications can be induced by sensorialdysfunction and stimulations derivingfrom a discrepancy of information in con-tiguous systems24. Information comingfrom well-integrated peripheral receptorsmay not require adaptive modifications ofthe system. sEMG activity could showsuch adaptation. With the eyes open, asignificant increase in rest sEMG activitywas observed in the temporal anteriorismuscles11,19,28. The visual input effect onthe sEMG activity of the sternocleidomas-toid and masseter muscles at rest has alsobeen proved29.
MONACO et al.21 found that in childrenpresenting with myopic defects, the sEMGof the anterior temporalis muscle at restincreases when the eyes are open. Anotherstudy found positive correlations betweenthe amount of mandibular laterodeviation,
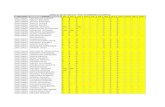
Table 1. Age and sex of study and control grou
Study group
Patients Sex Age
1 Male 272 Male 463 Female 184 Male 305 Male 376 Male 387 Female 218 Female 229 Female 27
10 Male 2011 Female 2712 Female 2413 Female 1914 Female 2415 Female 2116 Male 2617 Male 4118 Female 1919 Female 2420 Female 22
diottric defects, sEMG asymmetry andincreased sEMG values of the anteriortemporalis in the mandibular rest positionwith the eyes open22.
It is possible that people suffering frommuscular pain show less muscle toleranceand are more sensitive than normalhealthy volunteers to variation of sEMGrecording when visual input requires adap-tive behaviour.
The purpose of this study was to deter-mine the effects of myogenous facial painon the sEMG activity of the head andmasticatory muscles at rest and the effectof visual input on the sEMG activity ofpatients with myogenous facial pain atrest. This information could be of greatinterest to researchers because it couldhelp to clarify the physiological behaviourof a dysfunctional stomatognathic systemcompared with a healthy one.
Material and methods
The study included 40 individuals dividedinto a study and a control group. The studygroup included 20 patients with myogeniccraniomandibular dysfunction; 12 womenand 8 men, ranging in age from 19 to 41years (mean 30.6, SD 8.2 years; Table 1).The study subjects were selected frompatients with myogenous facial pain fromthe TMD centre at the authors’ institution,who fulfilled they following inclusion cri-teria: absence of visual defects; naturaldentition and bilateral molar support;absence of any previous orthodontic orgnathologic treatment; recent history ofpain in or around the temporomandibularjoint (TMJ) (preauricolar area, cheek area,
p.
Control group
Patients Sex Age
1 Male 232 Female 213 Female 234 Female 265 Male 286 Female 377 Female 278 Female 239 Male 20
10 Male 2111 Female 1812 Female 1913 Male 2414 Female 1915 Male 1816 Male 2317 Male 2318 Female 2319 Male 3020 Male 27
parietal area, temporal area, periorbitalarea) according to a research diagnosticcriteria (RDC) questionnaire4; presence ofspontaneous muscle pain (exacerbated bymeteorological changes, certain weatherconditions or palpation in the cervical andmasticatory muscles); self-reported teethclenching during the day; and if difficul-ties were experienced when performingfunctional jaw movements. Patients withsymptoms caused by trauma or surgerywere not included.
The control group included 20 healthyvolunteers; 10 female and 10 male, ran-ging in age from 18 to 37 years (mean27.8, SD 9.1 years). They were volunteersselected from medical and dentalstudents and people referred to the dentaldepartment for conservative or hygienetreatment according to the followinginclusion criteria: absence of visualdefects; natural dentition and bilateralmolar support; absence of any previousorthodontic or gnathologic treatment; nohistory of pain in or around the TMJ(according to RDC questionnaire4);absence of facial pain or other chronicpain condition (symptom free); and med-ication free.
The study was approved by the EthicsCommittee of the University of L’Aquilaand signed informed consent was obtainedfrom all subjects.
At the first visit, a trained dentist clini-cally evaluated all subjects to confirm thatthey complied with the inclusion criteria.For the study subjects these were: naturaldentition and bilateral molar support;absence of any previous orthodontic orgnathologic treatment; recent history ofpain in or around TMJ; and presence ofspontaneous muscle pain. For the controlgroup they were: natural dentition andbilateral molar support; absence of anyprevious orthodontic or gnathologic treat-ment; no history of pain in or around theTMJ. At the second visit, a trainedophthalmologist gave each participant acomplete ophthalmological and orthopticevaluation to confirm the absence of visualdefects. At the third visit, all subjects wereinvestigated by sEMG.
Each individual was submitted to twosEMG recordings in the mandibular restposition (lips in normal soft contact, noocclusal contact), one with closed and onewith open eyes. During the first recordingthe subjects were asked to keep their eyesclosed for 5 min in a dark room to avoidvisual information. 15 s of sEMG wererecorded for each trial. During the secondrecording the subjects were asked to keeptheir eyes open while looking straightahead. 15 s of sEMG were recorded for

Effects of myogenous facial pain on muscle activity of head and neck 769
Fig. 1. Closed and open eyes sEMG for a TMD patient in the study group. Note the ‘tonic’ change of anterior temporalis muscles. See text forabbreviations. The numbers on the right of the tracks represent the RMS in microvolts for each muscle.
each trial. The mean of three consecutiverecording epochs without movement arte-facts was chosen for statistical analysis.The sEMG values were processed inamplitude domain using the root meansquare (RMS) measured in microvolts.
sEMG measurement
The subjects were seated upright on acomfortable wooden chair. The headwas positioned with the Frankfort planparallel to the floor. During the firstrecording the room was silent and notilluminated; during the second recordingthe room was silent and softly illuminated.
sEMG activity was recorded (K7-Myo-tronics-Noromed, Inc., Kent, WA, USA)using bipolar surface electrodes at singledifferential with an inter-electrode dis-tance of 2.1 cm. The surface electrodeswere affixed with adhesive tape to the
Fig. 2. Closed and open eyes sEMG for a healthyanterior temporalis muscles values (LTA, left antnumbers on the right of the tracks represent the RMthe reader is referred to the web version of the a
alcohol-treated skin, to reduce skin impe-dance, over the superficial areas of theright masseter (RMM), left masseter(LMM), right anterior temporalis (RTA),left anterior temporalis (LTA), right digas-tric (RDA) left digastric (LDA), rightsternocleidomastoid (RSC) and left ster-nocleidomastoid (LSC) muscles. The elec-trodes were placed parallel to the musclefibres of left and right homologous mus-cles. Eight channel surface electromyo-graphy equipment was used(Myotronics-Noromed). The signalsobtained were amplified, recorded andcomputed using software for the clinicalenvironment (K7-Myotronics-Noromed);RMS, expressed in microvolts, was usedas amplitude indicator of the signal. Three15 s epochs were recorded for each per-formance.
To avoid movement artefacts or spon-taneous activity (swallowing or blinking)
subject in the control group. Note the unchanged ‘terior temporalis, black; RTA, right anterior tempoS in microvolts for each muscle. (For interpretation
rticle.)
the sEMG epochs were evaluated on-lineand recorded only if they were artefactfree. The sEMG pattern of swallowing issimple to detect3; sEMG epochs present-ing swallowing were detected and deletedon-line. Blinking did not affect sEMGvalues because the sEMG signal waspass-band (20–400 Hz) filtered. Blinkingis characterized by a frequency lower than20 Hz.
Figures 1 and 2 show the sEMG withclosed (on the left) and open (on the right)eyes in one case of significant change ofsEMG (Fig. 1) and in one case of unchan-ging sEMG (Fig. 2). In Fig. 2 two episodesof blinking can be discerned. Electrodeposition, equipment, head position andsubject were not changed during the test,so the results are probably due to visualinput. Figure 3 shows an episode of dryspontaneous saliva swallowing. The eventis simple to detect and the operator deleted
onic’ EMG and that blinking does not affect theralis, red). See text for other abbreviations. The
of the references to colour in this figure legend,

770 Monaco et al.
Fig. 3. Spontaneous dry swallowing for the TMD patient shown in Fig. 1. See text forabbreviations. The numbers on the right of the tracks represent the RMS in microvolts foreach muscle.
the epoch on-line2. The sEMG values wereexamined by the same operator with noknowledge of the purpose of the record-ing.
Table 3. sEMG mean values and standard deviation for study and control group in open eyescondition. Values are represented in microvolts. See text for abbreviations.
Control group Study group p
LTA 1.85(1.59) 3.65(1.86) 0.002**
RTA 1.75(2.01) 3.81(1.57) 0.007**
LMM 1.06(0.50) 1.65(1.10) 0.01*
RMM 1.03(0.45) 1.58(1.28) 0.03*
LSM 1.50(0.77) 2.71(2.68) 0.02*
RSM 1.55(0.47) 1.81(1.33) nsLDA 1.83(0.74) 1.96(1.02) nsRDA 1.72(0.76) 2.17(1.23) ns
ns: non-significant.* Significant difference.** Highly significant difference.
Table 2. sEMG mean values and standard deviation for study and control group in closed eyescondition. Values are represented in microvolts. See text for abbreviations.
Control group Study group p
LTA 1.43(0.83) 2.39(1.64) 0.01*
RTA 1.25(0.63) 2.24(1.32) 0.0003**
LMM 1.04(0.46) 1.52(0.95) 0.01*
RMM 1.06(0.45) 1.69(1.54) 0.03*
LSM 1.50(0.56) 2.34(1.93) 0.01*
RSM 1.57(0.54) 1.63(1.28) nsLDA 1.85(0.82) 2.00(1.17) nsRDA 1.69(0.80) 1.96(1.25) ns
ns: non-significant.* Significant difference.** Highly significant difference.
Statistical analysis
A paired t-test was performed using Statastatistics package to obtain a comparisonbetween mean and variance values ofelectromyography data between depen-dent or independent groups. Differenceswith a value of p < 0.05 and p < 0.005were regarded as significant and highlysignificant, respectively.
The first step was to make a paired t-testfor independent samples to compare theclosed eyes condition between study andcontrol group. The null hypothesis impliesthat for closed eyes, the study and controlgroup show no significant difference. Inthis case, the closed eyes sEMGs for thecontrol and study groups behave in a homo-geneous way. The alternative hypothesisimplies that closed eyes sEMGs for thestudy and control groups show significantdifference. In this case, the two groups aredifferent in the rest closed eyes sEMGs.
The second step was to perform a pairedt-test for dependent samples to comparesEMG data, in closed and open eyes, instudy and control groups separately. Thenull hypothesis suggests that the open eyescondition does not change the sEMG pat-tern of the closed eyes condition. Thealternative hypothesis suggests that theopen eyes condition changes the sEMGpattern compared with the closed eyescondition, implying a significant effectof visual input on sEMG data.
Results
Table 1 shows the age and sex of allparticipants. Comparison according tothe age of the individual showed no sig-nificant differences between the groups.Table 2 gives the EMG mean values andstandard deviation (in parenthesis) for thestudy and control groups in the closed eyescondition. The study group showed a sta-
tistically significant increase in left(p < 0.01) and right masseter (p < 0.03),in left (p < 0.01) and right (p < 0.0003)anterior temporalis and in left sternoclei-domastoid (p < 0.01) sEMG activity com-pared with control group. Table 3 gives theEMG results for the open eyes condition.The study group showed a statisticallysignificant increase in left (p < 0.01)and right (p < 0.03) masseter, in left(p < 0.002) and right (p < 0.007) anteriortemporalis and in left sternocleidomastoid(p < 0.02) sEMG activity compared withthe control group.
Table 4 gives the EMG values for thestudy group in the closed and open eyeconditions. A highly significant increasefor sEMG activity in the open eye condi-tion was observed in left and right anteriortemporalis (p < 0.003) and right digastric(p < 0.03). Table 5 gives the value for thecontrol group in the closed and open eyeconditions. No significant differenceswere observed in the sEMG values.
Discussion
The purpose of this study was to determinethe effects of myogenous facial pain onrest sEMG activity of head and mastica-tory muscles and the effect of visual inputon rest sEMG activity in patients withmyogenous facial pain.

Effects of myogenous facial pain on muscle activity of head and neck 771
Table 4. sEMG mean values and standard deviation for study group in closed and open eyesconditions. Values are represented in microvolts. See text for abbreviations.
Closed eyes Open eyes p
LTA 2.39(1.64) 3.65(1.86) 0.003**
RTA 2.24(1.32) 3.81(1.57) 0.003**
LMM 1.52(0.95) 1.65(1.10) nsRMM 1.69(1.54) 1.58(1.28) nsLSM 2.34(1.93) 2.71(2.68) nsRSM 1.63(1.28) 1.81(1.33) nsLDA 2.00(1.17) 1.96(1.02) nsRDA 1.96(1.25) 2.17(1.23) 0.03*
ns: non-significant.* Significant difference.** Highly significant difference.
Table 5. sEMG mean values and standard deviation for control group in closed and open eyesconditions. Values are represented in microvolts. See text for abbreviations.
Closed eyes Open eyes p
LTA 1.43(0.83) 1.85(1.59) nsRTA 1.25(0.63) 1.75(2.01) nsLMM 1.40(0.46) 1.06(0.50) nsRMM 1.06(0.45) 1.03(0.45) nsLSM 1.50(0.56) 1.50(0.77) nsRSM 1.57(0.54) 1.55(0.47) nsLDA 1.85(0.82) 1.83(0.74) nsRDA 1.69(0.80) 1.72(0.76) ns
ns: non-significant.*Significant difference.**Highly significant difference.
Masticatory muscle activity, controlledby the trigeminal nerve, is regulated byseveral inputs coming from the proprio-ception of neuromuscular spindles. Theseinputs have an important role in mainte-nance and in modification of muscularbase tone: a non-physiologic trigeminalproprioception can induce an altered mas-ticatory muscle efferent activity. There is aconvergence of nociceptive and proprio-ceptive afferences in the sensorial nucleiof the trigeminal nerve12, including neckand C1–C3 proprioception. It is possiblethat nociceptive stimuli, such as myogen-ous facial pain, can induce an alteration ofmasticatory muscle resting tone. The sig-nificant difference of LTA, RTA, LMM,RMM, LSM sEMG activity between studyand control groups with eyes closed seemsto confirm this hypothesis.
Proprioception messages from the neckmuscles are integrated in the central ner-vous system and contribute to controlbalance and body orientation10. Centripe-tal impulses from neck proprioceptorscooperate with the labyrinth impulses topromote oculomotor muscular activitythrough the cervical–vestibular–ocularreflex9.
Some important encephalic nuclei (tri-geminal nuclei, oculomotor nuclei, vestib-ular nuclei, accessorial nerve nuclei) are
integrated in the medial longitudinal fas-ciculus. Ocular proprioceptive receptorssend afferent signals to trigeminal andcuneate nuclei. The anatomic and physio-logic links of these anatomical structuresimply a co-ordinated integration of pro-prioceptive ocular and stomatognathicafferences.
Some studies suggest that mandibleelevator muscles of individuals with classI pain (according with Angle’s classifica-tion) without TMD signs or symptomshave constant sEMG values in the man-dibular rest position and in the absence ofexteroceptive stimuli6,25.
There is heated discussion about theusefulness of sEMG in the diagnosis andstudy of TMD but most reviews suggestsome cautions. It is generally thought thatthe physiological variables that have to betaken into account are age, sex, skeletalmorphology and psychological factors.The authors agree with this, so to improvetheir data they screened the study andcontrol group for the criteria given inthe Materials and Methods section. Theythink that doing this could overcome theproblem.
There is no agreement on the actualeffect of morphology on the anterior tem-poralis muscle. Some authors (speciallyduring the 1980s) suggested some kind of
relation15,33, but others (in the late 1990sand more recently) propose that there is nocorrelation5,23,30,31.
The same argument could be made forpsychological factors. There is some evi-dence about the incidence of depressionand anxiety, especially cognitive symp-toms, in myogenous facial pain, but thereis no clear evidence in the literature thatthese factors could influence the sEMGvalues of stomatognathic muscles. Forexample, RISSEN et al.26 showed no sig-nificant correlation between the psycho-physiological stress reaction and sEMG,and no association was found betweensEMG activity and pain, and betweennegative stress rating and pain. Othershave reported that patients with pain hadhigher anxiety, especially cognitive symp-toms, and feelings of muscle tension thandid controls. These authors stated thatEMG activity in the masseter regionswas not significantly different betweenthe pain and control groups16,18.
Many sEMG studies are concerned withfunctional activity, such as clenching, andfew of them have studied the rest position.None of them used the present strict inclu-sive criteria, and none studied the differ-ence between the anterior temporalissEMG in open and closed eye conditions.The present work is not concerned withthe rest activity of one muscle, isometricactivity during clenching or other func-tional and specific activities of the stoma-tognathic system. It tries to show throughsEMG activity that changing the physio-logical status (open versus closed eyes), insome way, could be considered a non-specific stimulus requiring orientationactivity.
The results of sEMG activity at restobserved in the healthy group, comparingclosed and open eye conditions, agree withthose of HOLMGREN et al.8 who did not findany significant change in resting masseteractivity when visual input was varied, anddisagree with the studies of MIRALLES thatfound a significant decrease in sEMGvalues of the above mentioned musclesin the closed eye condition19. Differentmethods could explain the discrepancybetween the present results and those ofMIRALLES.
The selection criteria in the HOLMGREN
and MIRALLES studies differ from the pre-sent ones. The authors’ strict inclusioncriteria for the control group included,among the others, a complete ophthalmol-ogist and orthoptist evaluation to confirmabsence of visual defects. MIRALLES’ workfocused on EMG activity of the sterno-cleidomastoid and masseter muscles in thesupine and lateral decubitus positions. The

772 Monaco et al.
present results concern the anterior tem-poralis muscle, in the upright seated posi-tion, with the head in a neutral position.One result quoted by the authors was thatafter 5 min in lateral decubitus in a darkroom and in the rest position, the sEMG ofthe sternomastoid and masseter wasreduced in both groups: 22 patients withmyogenic cranio-cervical-mandibulardysfunction and 18 healthy subjects.
MIRALLES’ rest position is difficult toconsider as a reference point. The authorconcluded by saying that ‘the significantchange in EMG activity, mainly observedat rest, suggests that the visual input effectis weak’. But it is possible that after 5 minin decubitus, in a dark room, people, ifthey are ‘healthy’, fall asleep, resulting inthis change in sEMG activity. Moreover,the change between waking and the firstsleep stage (sleep onset latency), detect-able only with a polysomnograph record,range from 3 to 15 min in the healthy.
HOLMGREN’s work did not comparepatients with healthy controls, did not takeinto account visual defects, data were notconsistent regarding open or closed eyesand concentrated attention on the sEMG(anterior temporalis and masseter mus-cles) effects of splint therapy. The presentdata, in part, confirm those of HOLMGREN,but extend the observation because whatthe authors have seen seems to be an effectdue to myogenous facial pain and does notseem related simply to opening the eyes.
MIRALLES considered open eyes thereference condition and closed eyes thetest condition. On the contrary, accordingto WIDMALM et al.34, in order to avoid orsignificantly reduce artefacts on the scalpmuscles, the present study consideredclosed eyes the reference condition andopen eyes the test condition.
The present study showed a significantinfluence of visual input on LTA, RTAand LDA sEMG activity in the studygroup subjects, as previously con-firmed21,22. This suggests that ocular pro-prioceptive stimuli, in patients withmyogenous facial pain, are an importantinput that could lead to tonic muscularadjustments of mandibular posture.Patients with myogenous facial pain, oncetheir physiological adaptation mechan-isms have been overridden, represent analarmed postural system that suffers thechanges of environmental demands.
The present findings indicate that inpatients with myogenous facial pain, theopen eyes condition, compared with theclosed eyes one, is associated with achange in the head and neck sEMG activ-ity in the mandibular rest position. Thisbehaviour is not present in the healthy
control subjects, suggesting that indivi-duals with class I without myogenousfacial pain signs or symptoms and withclinically verified correct vision accept theexteroceptive visual input without anadaptive mechanism on the sEMG patternof the stomatognathic system.
These observations suggest that thevisual input effect could be a good pro-vocation test for assessing a neuromuscu-lar reply that will be more significant inneurogenic facilitation areas13.
Future investigation will be aimed atevaluating these variables in a longitudinalmodel and evaluating them before and afterthe resolution of myogenous facial pain inorder to clarify the mechanism at work.
Competing interests
None declared.
Funding
None.
Ethical approval
Not required.
References
1. Buisseret-Delmas C, Epelbaum M,Buisseret P. The vestibular nuclei ofthe cat receive a primary afferent projec-tion from receptors in extraocular mus-cles. Exp Brain Res 1990: 81: 654–658.
2. Crary MA, Carnaby Mann GD, Gro-
her ME. Identification of swallowingevents from sEMG signals obtained fromhealthy adults. Dysphagia 2007: 22: 94–99.
3. Donaldson IM, Knoxx PC. Afferentsignals from pigeon extraocular musclesmodify the vestibular responses of unitsin the abducens nucleus. Proc R Soc LondB Biol Sci 1991: 244: 233–239.
4. Dworkin SF, LeResche L. Researchdiagnostic criteria for temporomandibu-lar disorders: review, criteria, examina-tions and specifications, critique. JCraniomand Disord Facial Oral Pain1992: 6: 301–355.
5. Farella M, Michelotti A, Carbone G,Gallo LM, Palla S, Martina R. Habi-tual daily masseter activity of subjects withdifferent vertical craniofacial morphology.Eur J Oral Sci 2005: 113: 380–385.
6. Ferrario VF, Sforza c. Miani JR,D’Addona. Barbini E. Electromyo-graphic activity of human masticatorymuscles in normal Young people. Statis-tical evaluation of reference values forclinical applications. J Oral Rehabil 1993:20: 271–280.
7. Gavish A, Winocur E, Astandzedov-
Nachmias T, Gavit E. Effect of con-
trolled masticatory exercise on pain andmuscle performance in myofascial painpatients: a pilot study. J CraniomandPract 2006: 24: 184–190.
8. Holmgren K, Sheikholeslam A, Riise
C. An electromyographic study of theimmediate effect of an occlusal split onthe postural activity on the anterior tem-poral and masseter muscles in differentbody positions with and without visualinput. J Oral Rehabil 1985: 12: 483–490.
9. Ito S, Taketomi M, Hirano M. Effectson tonic neck reflex on optokinetic nys-tagmus in rabbits. Acta Otolaryngol(Stockh) 1995: 115: 134–136.
10. Kavounoudias A, Gilhodes JC, Roll
R, Roll JP. From balance regulation tobody orientation. Two goals for muscleproprioceptive information processing?Exp Brain Res 1999: 1124: 80–88.
11. Kawamura Y. Neurophysiologic back-ground of occlusion. Periodontics 1967:5: 175–183.
12. Kerr FWL. Structural relation of thetrigeminal spinal tract to upper cervicalroots and the solitary nucleus in the cat.Exp Neurol 1961: 4: 134–148.
13. Korr IM. The collected papers of I.M.Korr. Indianapolis: American Academyof Osteopathy 1995: p. 119–228.
14. Liebenson CS. Pathogenesis of chronicback pain. J Manipulative Physiol Ther1992: 15: 299–308.
15. Lowe AA, Takada K. Associationsbetween anterior temporal, masseter,and orbicularis oris muscle activity andcraniofacial morphology in children. AmJ Orthod 1984: 86: 319–330.
16. Marbach JJ, Lund P. Depression, anhe-donia and anxiety in temporomandibularjoint and other facial pain syndromes.Pain 1981: 11: 73–84.
17. Meyer. Baron JB. Variation of ortho-static postural tonic activity during regio-nal anesthesia of the trigeminal nerve.Aggressiologie 1973: 14: 37–43.
18. Michelotti A, Martina R, Russo M,Romeo R. Personality characteristics oftemporomandibular disorder patientsusing MMPI. Cranio 1998: 16: 119–125.
19. Miralles R, Gutierrez C, Zucchino
G, Cavada G, Carvajal R, Valen-
zuela S, Palazzi C. Visual input effecton EMG activity of sternocleidomastoidand masseter muscles in healthy subjectsand in patients with myogenic cranio-cervical-mandibular dysfunction. J Cra-niomand Pract 1998: 16: 168–184.
20. Mohl ND, McCall WD, Lund JP,Plesh O. Devices for the diagnosis andtreatment of temporomandibular disor-ders. Part I: introduction, scientific evi-dence, and jaw tracking. J Prosthet Dent1990: 63: 198–201.
21. Monaco A, Cattaneo R, Spadaro A,Giannoni M, Di Martino S, Gatto R.Visual input effect on EMG activity ofmasticatory and postural muscles inhealthy and myopic children. Eur J Pae-diatr Dent 2006: 7: 18–22.

Effects of myogenous facial pain on muscle activity of head and neck 773
22. Monaco A, Cattaneo R, Spadaro A,Marzo G, Gatto R. Ocular correctioneffects on EMG activity of stomatognathicmuscles in children with functional man-dibular lateral-deviation: a case controlstudy. Eur J Paediatr Dent 2006: 7: 81–88.
23. Morales PG, Buschang PH, Throck-
morton GS, English JD. Maximum biteforce, muscle efficiency and mechanicaladvantage in children with vertical growthpatterns. Eur J Orthod 2003: 25: 265–272.
24. Oddson LIE. Control of voluntary trunkmovements in man. Acta Otolaryngol(Suppl. 574)1990 p. 1–90.13.
25. Rilo B, Santana U, Mora MJ,Cadarso CM. Myoelectrical activity ofclinical rest position and jaw muscleactivity in young adults. J Oral Rehabil1997: 24: 735–740.
26. Rissen D, Melin B, Sandsjo L, Dohns
I, Lundberg U. Surface EMG and psy-cholophysiological stress reactions inwoman during repetitive work. Eur JAppl Physiol 2000: 83: 215–222.
27. Schmid W, Mongini F, Felisio A. Acomputer-based assessment of structuraland displacement asymmetries of themandible. Am J Orthod 1991: 100: 19–34.
28. Shahani M. Influence of visual input onmonosynaptic reflex. Electromyogr ClinNeurophysiol 1977: 17: 3–11.
29. Sharifi Milani R, Deville de Periere
D, Micallef JP. Relationship betweendental occlusion and visual focusing. JCraniomand Pract 1998: 16: 109–118.
30. Tuxena A, Bakkea M, Pinholt EM.Comparative data from young men andwomen on masseter muscle fibres, func-tion and facial morphology. Arch OralBiol 1999: 44: 509–518.
31. Ueda HM, Miyamoto K, Saifuddin MD,IshizukaY DDS, Tanne K. Masticatorymuscle activity in children and adults withdifferent facial types. Am J Orthod Den-tofacial Orthop 2000: 118: 63–68.
32. Valentino B, Fabozzo A. Interactionbetween the muscles of the neck and theextraocular muscles of the myopic eye.
An electromyographic study. Surg RadiolAnat 1993: 15: 321–323.
33. Van Sickels JE, Rugh JD, Chu GW,Lemke RR. Electromyographic relaxedmandibular position in long-faced sub-jects. J Prosthet Dent 1985: 54: 578–581.
34. Widmalm SE, Lee YS, McKay DC.Clinical use of qualitative electromyogra-phy in the evaluation of jaw muscle func-tion: a practitioner’s guide. Cranio 2007:25: 63–73.
Address:Annalisa MonacoGnatology Clinic and
Prosthetic DepartmentUniversity of L’AquilaVia Vetoio Delta 6 CAP 67100 L’AquilaItalyTel: +39 0862 433837Fax: +39 0862 433826E-mail: [email protected]