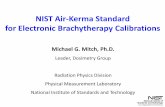
A Robust Quality Assurance Program for Determination of the Air Kerma Strength and Source...
Transcript of A Robust Quality Assurance Program for Determination of the Air Kerma Strength and Source...
S100 Abstracts / Brachytherapy 13 (2014) S15eS126
a single dwell position. Four different shield thicknesses (0, 3, 6, and 10mm) and three different source depths (0, 5, and 10 mm) in water wereconsidered, with the lead shield placed at the phantom surface.Backscatter dose enhancement and transmission data were obtained as thedose ratio with and without the shield, in the phantom and in the airvolume, respectively. Results were corrected to account for a realisticclinical case with multiple dwell positions.Results: Maximal backscatter dose enhancement in water was 3.5, 1.0, and0.8 mm for 60Co, 192Ir, and 169Yb, respectively. Similar results wereobtained in skin and polyethylene. The magnitude of the doseenhancement at the water phantom surface depended on the source depth(see figure 1), but was not sensitive to lead thickness in the consideredgeometries. Transmission data for 60Co and 192Ir were smaller than thosereported by Papagiannis et al. [Med Phys 35, 4898-4906 (2008)] forbrachytherapy facility shielding; differences increased as the emittedphoton energy increased. For 169Yb, the difference was negligible.
Figure 1. Shielded to unshielded absorbed dose ratio in the z-axis (axis
orthogonal to the phantom surface) for all three sources (60Co, 192Ir, and169Yb) and for the three different geometrical configurations used accord-
ing to source location: surface brachytherapy, and interstitial brachyther-
apy with source depth ds 5 5 mm and 10 mm. Results correspond to
those of a lead thickness tPb 5 6 mm.
Conclusions: The backscatter dose produced by the lead shield forbrachytherapy can be minimized using a few-millimeter thick bolus.Transmission data obtained in this work as a function of lead thicknessmay be used to estimate the influence on healthy organ equivalent dosefor a real treatment with HDR surface or interstitial brachytherapy withlead shields. The use of the lead shield is justified.
PO31
A Robust Quality Assurance Program for Determination of the Air
Kerma Strength and Source Characteristics of the Xoft Axxent
Electronic Brachytherapy Source
Sujatha Pai, MS, DABMP1, Dharani Rajendran, MS1, Rakesh R. Patel,
MD2. 1Good Samaritan Hospital, Radion Global, Inc, Cupertino, CA;2Targeted Radiation Institute, Pleasanton, CA.
Purpose: A robust quality assurance protocol is developed after analyzingthe source output variations and reliability of the Xoft Axxent electronicbrachytherapy source for surface application.Materials and Methods: The nominal dose rate at the skin surface wasobtained using the TG-61 in-air method for four applicators with the endcap attached. In addition, daily Air Kerma measurements (AKS) wereperformed using an ADCL calibrated well chamber-electrometer systembefore each treatment. A total of 30 consecutive sources were calibrated
and evaluated for source strength reproducibility and reliability. Theparameters measured are as follows:
1. The air kerma strength (AKS) for all the sources was comparedwith respect to each other and to the manufacturer calibration.
2. The dose rate parameters were measured in accordance with theAAPM TG 61 calibration protocol for different surface applicators(diameter 10, 20, 35, 50mm) were compared for 30 differentsources.
3. AKS reproducibility and life expectancy is evaluated for all thesources.
Results: For the 30 sources evaluated, the maximum variance in AKS was13%. The variation in the dose rates were measured for 10, 20, 35 and 50mm cone sizes with 30 consecutive sources were 23%, 16% 11%, and10% respectively.The individual source AKS measured using the ADCL calibrated wellchamber & electrometer system fluctuated by an average of 3% (S.D. �2%) with respect to the manufacturer calibration value. On the subsequenttreatment days the AKS measurement showed a variance of 1.2% (S.D.�1.2%). The source life expectancy was 500 min (S.D �200 min).Source failure was defined as either a complete source failure, or an AKSfluctuation of greater than 10% compared to the previous treatment day.Conclusions: The daily fluctuation of AKS was within 3% and was withinacceptable range. The AKS and the dose rate variability between differentsources were significant warranting separate in-air dose ratemeasurements for each source independently. A robust quality assuranceprogram for electronic brachytherapy is designed at our institution toinclude a TG61 in air dose rate measurement for each surface applicatorbefore it is used for patient treatments. Upon a source failure, thetreatment times for all the patients are updated to reflect the new sourceparameters. Since the life expectancy of the source is unpredictable, werecommend calibrating multiple back-up sources.
PO32
HDR GYN: Tandem and Ring Planning Procedure for Special Cases
Ileana Iftimia, PhD, Per Halvorsen, MS, Eileen Cirino, MS, Janna Finn,
CMD, Andrea McKee, MD. Radiation Oncology, Lahey Clinic, Burlington,
MA.
Purpose: To develop a planning methodology for special cases such ascombinations of EBRT with/without an SBRT boost and HDRbrachytherapy.Materials and Methods: Currently for HDR Tandem and Ring (T&R)treatments we prescribe 25 Gy over 5 insertions to point ‘‘A’’ following a45 to 54 Gy EBRT treatment. Plans are done for each implant. If thetumor is visible on MR images, the standard pear shaped isodosedistribution is adjusted to cover the tumor with the prescribed dose. Wecontour bladder/rectum/sigmoid to establish the HDR D2cc tolerances forthese critical structures taking into account the EBRT dose for each case.We report D0.1cc, D1cc, and D2cc for the critical structures and D90,D100, V100, V150, and V200 for the tumor volume. We record thecumulative EBRT - HDR BED/EQD2 (D2cc) for bladder, rectum, andsigmoid, and compare with ABS tolerances (D2cc BED tolerance 150,125, 125 for bladder, rectum, and sigmoid, respectively). When the EBRTplan is AP-PA or 4 fields, the BED-EQD2 calculations to establish theD2cc tolerances for the HDR critical structures have limited accuracy,since the hotspots for the EBRT and HDR plans may not be in the samelocations. Using the standard formulas and the EBRT doses for thatpatient, a table is created to estimate the D2cc dose tolerance and a T&Rplan is generated. Since these calculations consider the worst casescenario, (i.e., the hotspots for the EBRT and HDR are in the samelocations), they could be too restrictive for the HDR T&R plan. This mayresult in an unwarranted target under-dose. For those cases we developeda procedure using the MIM software. We export to MIM the EBRTplan(s) and the first HDR T&R plan and a BED composite plan isobtained. A DVH analysis is performed to estimate the cumulative D2ccfor the critical structures. The remaining dose up to the tolerance leveldivided by the number of untreated HDR fractions is used as a maximumallowable dose for the remaining T&R plans. Using these MIM results