A Rising Generation - Mayo Clinic School of Continuous ... - Cystic Fibrosis.pdf©2015 MFMER |...
Transcript of A Rising Generation - Mayo Clinic School of Continuous ... - Cystic Fibrosis.pdf©2015 MFMER |...
©2015 MFMER | slide-1
A Rising GenerationExploring the Pharmacotherapy Advancements for Cystic Fibrosis
P. Zach White, PharmDPGY1 Pediatric Pharmacy ResidentPharmacy Grand Rounds March 1, 2016
©2015 MFMER | slide-2
Pre-Assessment QuestionWhat is the newest FDA-approved treatment category for cystic fibrosis? A) Mucolytics B) Cystic fibrosis transmembrane conductance
regulator protein (CFTR) modulators C) Pancreatic enzyme replacementD) Inhaled antibiotics
©2015 MFMER | slide-3
Objectives• Discuss the pathophysiology of cystic fibrosis
(CF)• Review current pharmacotherapy treatments for
CF• Explore the literature assessing the efficacy of
newer pharmacotherapy agents for CF
©2015 MFMER | slide-4
Cystic Fibrosis• Autosomal recessive disease causing a mutation
of the CFTR gene located on chromosome 7• Affecting the lungs, pancreas, intestines, sweat
glands, and vas deferens• 70,000 people have CF worldwide
- 40% in the United States
• 1,000 new cases diagnosed annually
Cystic Fibrosis FoundationEur Respir J. 2015 Jul;46(1):133-41
CFTR: cystic fibrosis transmembrane conductance regulator protein
©2015 MFMER | slide-5
Early Detection
• 75% of patients are diagnosed by 2 years of age- All 50 states implement newborn screening
- Elevated immunoreactive trypsinogen
• 50% of CF population is now > 18 years of age- 75% of the CF population will be > 18 years old by 2025
US Pharm. 2015;40(7): 45-49
©2015 MFMER | slide-6
Life Expectancy
European Lung White BookEur Respir J. 2015 Jul;46(1):133-41
Pancreatic Enzymes
Airway Clearance
Antistaphylococcal Antibiotics
Antipsuedomonal Antibiotics
Lung Transplant
Inhaled Tobramycin
Age
(Yea
rs)
05
101520253035404550
1930 1940 1950 1960 1970 1980 1990 2000 2010 2015
CFTR Modulators
CFTR: cystic fibrosis transmembrane conductance regulator protein
©2015 MFMER | slide-7
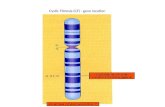
Normal CFTR Function
Na+ Na+Cl- Cl-
CFTR Na+ Channel
Pancreas
Lungs
H2OH2O
Na+
CFTR: cystic fibrosis transmembrane conductance regulator protein
Cl-
©2015 MFMER | slide-8
CF Pathophysiology
CFTR gene defect
Defective ion transport
Airway surface liquid depletion
Defective mucociliary clearance
Mucus obstruction
Infection Inflammation
Respir Care 2009; 54(5);595-602
©2015 MFMER | slide-9
Genetic Variants in CF• Over 1800 CFTR genetic mutations identified
Most Common CFTR MutationsPhe508del (formerly ∆F508) 394delTTG551D 3905insTG542X Q359K/T360N1303K 621+1G->TW1282 R117HR553X R1162X
Cystic Fibrosis Foundation
©2015 MFMER | slide-10
CF Mutation Classes
Class Description Mutation ExampleI No CFTR synthesis G542XII CFTR incorrectly processed and does not
reach cell membrane Phe508del
III CFTR reaches cell membrane but there is abnormal channel regulation G551D
IV CFTR reaches cell membrane but openchannel time is reduced R334W
V Reduced CFTR synthesis R117HVI CFTR reaches cell membrane but rapid
protein turnover leads to shortened t½ 1811+1.6kbA>G
t½: half-life European Lung White Book
©2015 MFMER | slide-11
CFTR in Cystic Fibrosis
Cl- Cl- Cl-
H2O H2O
Na+Na+
Na+
Group II Mutation“Correctors”
mRNA
Group III Mutation“Potentiators”
©2015 MFMER | slide-12
Assessment Question #1
Which of the following about CF is false?
A) Phe508del is the most common genetic mutation B) CFTR mutations affect Cl-, Na+, and H2OC) Average life expectancy is now over 40 years of ageD) CFTR is a Na+ channelE) All the above are true
©2015 MFMER | slide-13
Current Pharmacotherapy Pulmonary Management Nutrition Support
Airway clearance- Hypertonic saline- Dornase alpha- Acetylcysteine
Pancreatic Enzymes- Acid blockers
Bronchodilators Nutritional Support- High caloric diet- Appetite stimulants
Antibiotics Fat-soluble vitamin supplementationAnti-inflammatory medicationsCFTR modulators
US Pharm. 2015;40(7): 45-49
©2015 MFMER | slide-14
MucolyticsDrug Route Indication Comment
Sodium Chloride7% Inhaled Mucolysis and sputum
induction
• >6 years old• Used chronically• Administer after a
bronchodilator
Dornase alfa Inhaled Mucolysis
• Cleaves extracellular DNA
• > 3 months of age• Used chronically
Acetylcysteine Inhaled
Adjunctive treatment of bronchopulmonary disorders caused by mucous obstruction
• Not for chronic use• Administer after
bronchodilator
US Pharm. 2015;40(7): 45-49
©2015 MFMER | slide-15
Antibiotics • Pseudomonas aeruginosa
Drug Route Comment
Tobramycin Inhaled/IV
• BID for 28 days, alternating 28-day periods
• Home inhaler• IV: once daily dosing
Aztreonam Inhaled/IV • Inhaled for >7 years oldCefepime
Ceftazidime IV • Higher doses in pediatrics with resistant pseudomonas
Azithromycin Oral • 3 days weekly
US Pharm. 2015;40(7): 45-49AM J Respir Crit Care Med Vol 180. pp 802-808, 2009
©2015 MFMER | slide-16
Anti-inflammatory Agents• Routine use of oral or inhaled corticosteroids is
not recommended• Short courses of systemic corticosteroids may
offer benefit without long-term adverse effects• CF Foundation concludes there is not sufficient
evidence to recommend the routine use in the setting of an acute exacerbation
AM J Respir Crit Care Med Vol 180. pp 802-808, 2009
©2015 MFMER | slide-17
Enzyme Replacement• Obstructed pancreatic and biliary ducts
- Decreased absorption of fat, protein, and fat-soluble vitamins
• Pancrelipase- Titrated to effect (i.e. steatorrhea)
- Not to exceed 2,500 lipase U/kg/meal
- Best absorbed by increasing pH of gastric acid
- Do not crush/chew - can sprinkle on applesauce
US Pharm. 2015;40(7): 45-49
©2015 MFMER | slide-18
‘Tune-Up’• 14 day hospitalization course
- scheduled or unscheduled
• Goal: Improve respiratory function and prevent rehospitalization due to pulmonary exacerbations or pneumonia
• IV antibiotics, vest therapy, chest x-rays, hearing tests, pulmonary function tests, nutrition optimization
AM J Respir Crit Care Med Vol 180. pp 802-808, 2009
©2015 MFMER | slide-19
Assessment Question #2Which of the following is true regarding current pharmacotherapy treatment of CF?A) Absorption of fat-soluble vitamins is not of concern in patients with CFB) Dornase alpha works by osmotically drawing water into the thickened mucus layer C) Pancreatic enzymes should not be taken with regards to meals or snacks D) Routine use of systemic corticosteroids are not recommended in patients with CF
©2015 MFMER | slide-20
A CFTR Potentiator in Patients with Cystic Fibrosis and the G511D Mutation
Ramsey et. alN Engl J Med 2011;365:1663-72
©2015 MFMER | slide-21
A CFTR Potentiator in Patients with Cystic Fibrosis and the G511D Mutation
Patient Number N = 161
Study Design Randomized, double-blind, placebo-controlled, international trial
Interventions Ivacaftor 150 mg every 12 hours vs. placebo
Duration 24 weeks, with treatment effect assessed through week 48
Inclusion• At least one G551D CFTR mutation• >12 years of age• FEV1 40% to 90% of predicted normal value
Primary Outcome Absolute change from baseline in the % of FEV1 at 24 weeks
Secondary Outcomes• Absolute change in weight gain through week 48• CFQ-R scores assessing quality of life through week 48• # pulmonary exacerbations through week 48
N Engl J Med 2011;365:1663-72.FEV1: forced expiratory volume in 1 secondCFQ-R: Cystic Fibrosis Questionnaire-Revised
©2015 MFMER | slide-22
Results
Result Ivacaftor P value
Primary OutcomeAbsolute change from baseline in the % of FEV1
10.6 < 0.001
Secondary OutcomesAbsolute change in weight (kg) 2.7 < 0.001Absolute change in CFQ-R from baseline 8.6 < 0.001Pulmonary exacerbation risk reduction 55% 0.001
FEV1: forced expiratory volume in 1 secondCFQ-R: Cystic Fibrosis Questionnaire-Revised
©2015 MFMER | slide-23
IvacaftorKalydeco®
FDA Approval January 2012
IndicationTreatment of CF in patients > 2 years old that have one of the following mutations: G551D, G1244E, G1249D, G1278R, G551S, S125IN, S1225P, S549N or S549R
Contraindications None
Limitations Not effective in patients homozygous for F508del CFTR mutation
Supplied 150 mg tablets50 mg or 75 mg unit-dosed oral granule packets
Metabolism CYP3A
Dosing• Patients > 6 years of age: 150 mg q12h • Patients 2-6 years of age and > 14 kg: 75 mg q12h• Patients 2-6 years of age and < 14kg: 50 mg q12h
Pearls Take with fat-containing meal
Cost $300,000 annually
Kalydeco (ivacaftor) package insert; Vertex Pharmaceuticals Inc; Feb 2016
CYP: cytochrome P450
©2015 MFMER | slide-24
Lumacaftor-Ivacaftor in Patients with Cystic Fibrosis Homozygous for
Phe508del CFTRWainwright et. al
N Engl J Med 2015;373:220-31
©2015 MFMER | slide-25
TRAFFIC and TRANSPORT trialsPatient Number N = 1108
Study Design Phase III, multinational, randomized, double-blind, placebo-controlled, parallel-group
Interventions LUM-IVA 600-125 mg once daily vs. LUM-IVA 400-125 mg twice daily vs. placebo
Duration 24 weeks
Inclusion• Homozygous for Phe508del CFTR mutation• >12 years of age• FEV1 40% to 90% of predicted normal value
Primary Outcome Absolute change from baseline in the % of FEV1 at 24 weeks
Secondary Outcomes• Absolute change in BMI through week 24• CFQ-R scores assessing quality of life• # pulmonary exacerbations through week 24
N Engl J Med 2015;373:220-31.LUM-IVA: lumacaftor/ivacaftorFEV1: forced expiratory volume in 1 secondBMI: body-mass index CFQ-R: Cystic Fibrosis Questionnaire-Revised
©2015 MFMER | slide-26
Baseline Demographics
Characteristic Placebo N = 371
LUM–IVA600 mg daily
N = 368
LUM-IVA 400 mg q12h
N = 369Female sex (%) 48.8 49.5 49.3
Mean age (years) 25.4 24.5 25.3
Baseline FEV1 (%) 60.4 60.8 60.5
Mean BMI 21.0 21.0 21.5
% use of maintenance medicationsBronchodilatorsDornase alphaInhaled antibioticsAzithromycinInhaled hypertonic salineInhaled glucocorticoids
92.275.769.562.859.359.3
92.978.563.063.353.557.9
93.274.061.058.361.557.5
N Engl J Med 2015;373:220-31.LUM-IVA: lumacaftor/ivacaftorFEV1: forced expiratory volume in 1 secondBMI: body mass index
©2015 MFMER | slide-27
Results
ResultLUM–IVA600 mg
dailyP value
LUM-IVA 400 mg q12h
P value
Primary Outcome% FEV1 absolute change from baseline
3.3 < 0.001 2.8 < 0.001
Secondary OutcomesAbsolute BMI change from baseline
0.28 <0.001 0.24 < 0.001
Absolute change in CFQ-R from baseline
3.1 0.007 2.2 0.05
FEV1: forced expiratory volume in 1 secondBMI: body-mass index CFQ-R: Cystic Fibrosis Quiestionaire-Revised
©2015 MFMER | slide-28
Pulmonary Exacerbations
0
50
100
150
200
250
300
Pulmonary Exacerbations
PlaceboLUM-IVA 600-125 mgLUM-IVA 400-125 q12h
P < 0.001
P < 0.001
Num
ber o
f Eve
nts
©2015 MFMER | slide-29
Events Leading to Hospitalization
0
5
10
15
20
25
30
35
40
45
50
Events Leading to Hospitalization
PlaceboLUM-IVA 600-125 mgLUM-IVA 400-125 q12h
39%P = 0.003
61%P < 0.001
Eve
nt R
ate/
48
wee
ks
©2015 MFMER | slide-30
Events Leading to IV Antibiotic Treatment
0
10
20
30
40
50
60
70
Events Leading to IV Antibiotic Treatment
PlaceboLUM-IVA 600-125 mgLUM-IVA 400-125 q12h
45%P < 0.001
56%P < 0.001
Eve
nt R
ate/
48
wee
ks
©2015 MFMER | slide-31
Safety
Placebo LUM–IVA600 mg daily
LUM-IVA 400 mg q12h
Serious AE 28.6% 22.8% 17.3%
Discontinuation due to AE 1.6% 3.8% 4.6%
Most common adverse eventsInfective pulmonary exacerbationCoughIncrease in sputum production
49.9%40%
18.9%
39.3%32.8%14.9%
35.8%28.2%14.6%
AE: adverse event
©2015 MFMER | slide-32
Subgroup Analysis
• FEV1 > 70% not statistically significant in 1 of 2 studies for the LUM-IVA 400-125 mg q12h group
• Otherwise, subgroup analysis showed no other differences in FEV1 outcomes
SubgroupsPatients < 18 years of age or > 18 years of age
GenderFEV1 <70% or >70%
Pseudomonas aeruginosa positive/negative
©2015 MFMER | slide-33
Lumacaftor-IvacaftorOrkambi®
FDA Approval July 2015
Indication Treatment of CF in patients > 12 years old that are homozygous for the F508del mutation in the CFTR gene
Contraindications None
Supplied LUM-IVA 200 mg-125 mg tablets
Metabolism LUM excreted unchanged in the fecesIVA metabolized by CYP3A
Dosing
• No dose adjustments needed for mild hepatic impairment• Mild adjustments needed for moderate hepatic impairment• If patient is taking strong CYP3A inhibitors, initiate LUM-IVA at
half of the dose for first 7 days of treatment
Pearls Take with fat-containing meals
Cost $259,000 annually
LUM-IVA: lumacaftor/ivacaftor Orkambi (lumacaftor/ivacaftor) package insertVertex Pharmacetuicals, Inc; Feb 2016
©2015 MFMER | slide-34
Assessment Question #3Which of the following is true about the results of lumacaftor-ivacaftor when compared to placebo? A) LUM-IVA reduced the rate of pulmonary exacerbations, improved
FEV1, and had significantly more serious adverse events
B) LUM-IVA reduced the rate of pulmonary exacerbations, did not show FEV1 improvement, and did not have more serious adverse events
C) LUM-IVA reduced the rate of pulmonary exacerbations, improved FEV1, and did not have more serious adverse events
D) None of the above
LUM-IVA: lumacaftor-ivacaftorFEV1: forced expiratory volume in 1 second
©2015 MFMER | slide-35
Assessment
Strengths LimitationsWide range of FEV1 included Did not include patients < 12 yearsApplicable to a significant percentage of CF patients
Difficult to extrapolate to patients heterozygous for F508del
Patients randomized appropriately Didn’t assess potential benefit to patients with G511D mutation
Appropriate subgroup analysis
FEV1: forced expiratory volume in 1 second
©2015 MFMER | slide-36
Conclusions
Authors’ Conclusions• LUM-IVA is a milestone treatment for 45% of CF patients homozygous
for Phe508del• LUM-IVA has an acceptable side-effect profile
Seminarian’s Conclusions • LUM-IVA provides moderate FEV1 benefit and significant benefit in
preventing pulmonary exacerbations to patients with the most common type of CFTR mutation
• The side effect profile makes it an attractive pharmacotherapy adjunct • Cost can be a deal-breaker for many patients• Studies need to be conducted to determine effectiveness for patients
heterozygous for Phe508del
©2015 MFMER | slide-37
New Treatment Ideas in the Pipeline• Inhaled drug to repair CFTR-encoded mRNA in
hetero- or homozygous Phe508del• Combination corrector and anti-inflammatory• Drugs that prolong effects of hypertonic saline• Anti-infective agent nearly identical to iron
shown to kill resistant pseudomonas• Different formulations of pancreatic enzyme
replacement
Cystic Fibrosis Foundation
©2015 MFMER | slide-38
Treatment Agents Closest to ApprovalCFTR Modulation• Ataluren (Phase 3)
• VX-661 + ivacaftor (Phase 3)
Restore Airway Surface Liquid• Inhaled Mannitol (Phase 3)
Anti-Infective• Inhaled Levofloxacin (Phase 3)
• Inhaled Liposomal Amikacin (Phase 3)
• Vancomycin Inhalation Powder (Phase 2)Cystic Fibrosis Foundation
©2015 MFMER | slide-39
Overall Conclusions • The life expectancy for the CF patient is rising
- 75% of CF patients > 18 years of age by 2025
• Pharmacotherapy focusing on CFTR modulation• LUM-IVA showed improvement in exacerbation
prevention for patients with the most common CFTR mutation
• New agents continue to improve the quality of life for CF patients
©2015 MFMER | slide-40
P. Zach White, PharmDPGY1 Pediatric Pharmacy [email protected]
A Rising GenerationExploring the Pharmacotherapy Advancements for Cystic Fibrosis