A Review- Pharmaceutical and Pharmacokinetic Aspect of Nanocrystalline Suspensions
-
Upload
dhaval-shah -
Category
Documents
-
view
198 -
download
5
Transcript of A Review- Pharmaceutical and Pharmacokinetic Aspect of Nanocrystalline Suspensions

REVIEW
A Review: Pharmaceutical and Pharmacokinetic Aspectof Nanocrystalline Suspensions
DHAVAL A. SHAH,1 SHARAD B. MURDANDE,2 RUTESH H. DAVE1
1Arnold & Marie Schwartz College of Pharmacy and Health Sciences, Long Island University, Brooklyn, New York 112012Drug Product Design, Pfizer Worldwide R&D, Groton, Connecticut 06340
Received 7 August 2015; revised 23 September 2015; accepted 25 September 2015
Published online in Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/jps.24694
ABSTRACT: Nanocrystals have emerged as a potential formulation strategy to eliminate the bioavailability-related problems by enhancingthe initial dissolution rate and moderately super-saturating the thermodynamic solubility. This review contains an in-depth knowledge of,the processing method for formulation, an accurate quantitative assessment of the solubility and dissolution rates and their correlation toobserve pharmacokinetic data. Poor aqueous solubility is considered the major hurdle in the development of pharmaceutical compounds.Because of a lack of understanding with regard to the change in the thermodynamic and kinetic properties (i.e., solubility and dissolutionrate) upon nanosizing, we critically reviewed the literatures for solubility determination to understand the significance and accuracy of theimplemented analytical method. In the latter part, we reviewed reports that have quantitatively studied the effect of the particle size andthe surface area change on the initial dissolution rate enhancement using alternative approaches besides the sink condition dissolution.The lack of an apparent relationship between the dissolution rate enhancement and the observed bioavailability are discussed by reviewingthe reported in vivo data on animal models along with the particle size and food effect. The review will provide comprehensive informationto the pharmaceutical scientist in the area of nanoparticulate drug delivery. C© 2015 Wiley Periodicals, Inc. and the American PharmacistsAssociation J Pharm SciKeywords: nanocrystals; nanosuspensions; nanoparticles; solubility; dissolution; pharmacokinetics; food interactions; bioavailability;particle size reduction
INTRODUCTION
Recent advances in synthetic, analytical, and purificationchemistry, along with the development of specialized toolssuch as high-throughput screening, combinatorial chemistry,and proteomics, have led to a sharp influx of discovery com-pounds entering into development. Many of these compoundsare highly lipophilic, as the in vitro screening techniques placeconsiderable emphasis on the interaction of compounds with de-fined molecular targets. In recent years, it has been estimatedthat up to 70% of the new drugs discovered by the pharmaceu-tical industry are poorly soluble or lipophilic compounds. Pooraqueous solubility is one of the major hurdles in the develop-ment of new compounds into oral dosage forms, as absorptionis limited by dissolution for these compounds.1
The well-known Biopharmaceutics Classification System(BCS) is frequently used to categorize pharmaceutical com-pounds. According to the BCS system, poorly soluble com-pounds belong to Class II (low solubility, high permeability)or Class IV (low solubility, low permeability). In another words,we can also say that Class II and IV compounds provide moreopportunities for the development of newer technologies toovercome the solubility- or dissolution-related issues based onchemical and physical properties of the compounds. This per-ception is widely used and well established within the pharma-ceutical industry. However, using the BCS system for guidancein formulation selection may sometimes oversimplify the com-
Correspondence to: Rutesh H. Dave (Telephone: +718-488-1660; Fax: +718-780-4586; E-mail: [email protected])
Journal of Pharmaceutical SciencesC© 2015 Wiley Periodicals, Inc. and the American Pharmacists Association
plex nature of drug dissolution, solubility, and permeability.Poorly water-soluble compounds can possess such a low aque-ous solubility that the dissolution rate, even from micronizedparticle, is very slow. In this case, it is not possible to reach suf-ficiently high drug concentrations in the gastrointestinal tractfor an effective flux across the epithelial membrane. Other fac-tors, such as efflux transport or pre-systemic metabolism, canalso negatively influence oral bioavailability.
Therefore, it is recommended to classify compounds intoslightly different categories, as they can show dissolutionrate-limited, solubility-limited, or permeability-limited oralbioavailability. Butler and Dressman2 designed the “Developa-bility Classification System (DCS),” as another way to catego-rize compounds in a more bio-relevant manner. This system dis-tinguishes between dissolution rate-limited compounds (DCSClass IIa) and solubility-limited compounds (DCS Class IIb).
In order to select the right formulation approach and to ad-dress the compound-specific issues with a suitable formulationtype, it is imperative to first understand the bioavailability lim-iting factors. Selection of the right formulation approach is oneof the key activities for formulators in the pharmaceutical in-dustry. Key factors include the physicochemical properties ofactive pharmaceutical ingredient (API), such as aqueous solu-bility, the melting point temperature, and chemical stability. Inaddition, the formulator needs information about the potencyof the compound and the desired route of administration to de-termine the type of final dosage form as well as the requireddrug load. All these factors can be considered in decision trees,which are often used in the industry to guide the formulator.
However, there are some biopharmaceutical-relevant as-pects that need more attention in order to avoid false nega-tive results. In addition, it is also important to note that there
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES 1

2 REVIEW
is no uniform approach that solves all the formulation-relatedproblems. Each technology has its own advantages and disad-vantages. Depending on the formulator’s understanding of theinterplay between the physicochemical properties of the drug,the special aspects of the various formulation options and therequired in vivo performance, the higher the chance that the op-timal formulation approach will be chosen. This minimizes therisk of late failures in the human clinical trials, for example, dueto insufficient or highly variable drug exposures. Compoundsshowing dissolution rate limited bioavailability may be referredto as DCS Class IIa compounds, but they represent only onepart of the BCS Class II compounds. The extent of the oralbioavailability of such compounds directly correlates with theirdissolution rate in vitro. The fraction of the dose that dissolvesin the lumen is readily absorbed through the intestinal mem-brane. Consequently, the bioavailability of such compounds canbe improved by any technique that increases the primarily thedissolution rate. Various formulation approaches are known tolead to increased dissolution rate and bioavailability, includ-ing salt formation, the use of cocrystals, particle size reduction,complexing with cyclodextrins,3 microemulsions,4 and solid dis-persion technologies.5,6 The formulator has to select the optimalformulation approach based on the properties of a specific drugmolecule. However, all these technologies have certain limita-tions and cannot be used as universal formulation techniquesfor all the poorly soluble compounds, especially those whichare insoluble in both aqueous as well as non-aqueous solvents.7
To prevent the removal of poorly soluble compounds from thepharmaceutical pipeline, a broad-based technology is requiredfor drug molecules that are insoluble or poorly soluble in bothaqueous and non-aqueous solvents. This will have the tremen-dous impact in discovery sciences and will improve the perfor-mance of existing molecules suffering from formulation-relatedissues.8
In the last two decades, after the introduction of Nanocrystal R© technology, particle-size reduction approaches havegrown to a commercial level. Several formulation ap-proaches have been reported to formulate the nanoparticles,such as nanocrystalline suspensions, Poly Lactic-co-Glycolicacid(PLGA)based nanoparticles, nanosphears, and solid-lipidnanoparticles. By the virtue of their large surface area (SA)
dcdt = AD(Cs−C)
hln SS0
= 2MYDrRT hH = k
(√L/
√V
)
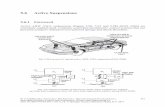
Noyes–Whitney Equation Ostwald–Freundlich Prandtl Equation
dc/dt = Dissolution velocity S = Solubility at Temp T hH = Hydrodynamic boundary layer thicknessA = Surface area S0 = Solubility of infinite big particle k = ConstantD = Diffusion coefficient M = Molecular weight L = length of surface in flow directionCs = Saturation solubility D = Density V = relative velocity of flowing liquidC = Drug concentration in U = Interfacial tensionSolution at time t R = Gas constanth = Thickness of diffusion layer r = Radius
T = Temperature
to volume ratio, nanocrystals provide an alternative methodto formulate poorly soluble compounds. Nanosizing refers tothe reduction of the APIs’ particle size down to the sub-micronrange. Nanosuspensions are sub-micron colloidal dispersions ofdiscrete particles that have been stabilized using a surfactantand a polymer or a mixture of both.9 Stabilized sub-micron
particles in nanosuspensions can be further processed intostandard dosage forms, such as tablets or capsules, which arebest suited for oral administration.
It has been studied and observed that the reduction in par-ticle size in the micron or nano range have a positive impact onthe in vitro dissolution rate, which can be used to predict in vivoenhancement in bioavailability for poorly soluble compounds.10
Compound-specific properties, such as high melting point, highlog P value and poor aqueous solubility, are required to considerbefore the selection of this approach. Therefore, BCS Class IIand IV compounds would theoretically be good candidates forthe nanosizing approach, along with some exceptions, such asfenofibrate (FBT) (low melting point).11 Drug nanocrystals ex-hibit many advantages, including high efficiency of drug load-ing, easy scale-up for manufacture, relatively low cost for prepa-ration, and applicability to various administration routes, suchas oral, parenteral, ocular, and pulmonary delivery (Table 1).All these advantages have led to successful promotion of drugnanocrystals from experimental research to patients’ usage.The availability of several products on the market shows thetherapeutic and commercial effectiveness of the approach.12
The pioneering work of many academics and industrial re-searchers has laid the foundation for broad utilization and ac-ceptance of this approach within the field of pharmaceuticalsciences.
By definition, nanosizing is particle-size reduction to 1 and1000 nm. Because of their small size, these particles can varydistinctly in their properties from micronized drug particles.Similarly to other colloidal systems, drug nanocrystals tend toreduce their energy state by forming larger agglomerates orcrystal growth, which is why they are often stabilized with sur-factants, stabilizers, or with a mixture of both. Reduction of theparticle size to the nanometer range results in a substantialincrease in SA (A), thus, this factor alone will result in a fasterdissolution rate as described by Noyes–Whitney.13 In addition,the Prandtl equation shows that the drug nanocrystals showeddecreased diffusional distance “h”. This further enhances thedissolution rate. Finally, the concentration gradient (Cs − Cx) isalso of high importance. There are reports that drug nanocrys-tals have shown increased saturation/thermodynamic solubil-ity (Cs). This can be explained by the Ostwald–Freundlichequation14 and by the Kelvin equation.15
It is still not clear to what extend the saturation solubilitycan be increased solely as a function of particle size. Most prob-ably the increased solubility of drug nanocrystals is a combinedeffect of nanosized drug particles and solid-state effects causedby the particle fractionation during the process. A number ofauthors have reported improvement from a 10% increase in
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 3
Table 1. Advantages of Nanocrystals in Different Route ofAdministration
Route Advantages
Oral � Increase bioavailability� Decrease in fed/fast variations� Increase rate of absorption; decrease in Tmax
and increase in Cmax� Quick and easy to formulate
Parenteral � About 100% bioavailability can be achieved ifgiven as an IV formulation
� Targeting drug delivery� Avoidance of organic solvent, surfactants, pH
extremes
Pulmonary � Used in nebulizer as a liquid solution or drypowder
� A single drop can contain many nanoparticles� Increase the concentration and or loading of
nanocrystalline dispersion
saturation solubility to several folds using differentapproaches.16–20 Below are the established equations to de-scribe nanocrystals and their physicochemical properties.
Advantages of nanocrystals over conventional and specialdrug delivery systems:
1. Because of high surface enlargement factor in nanocrys-tals, there is an increase in the dissolution rate as wellas a modest increase in saturation solubility as comparedwith micronized particles.
2. With a size range in nanometers, it can be injected as aIV to get 100% bioavailability.
3. Dose reduction and patient compliance.4. Lessen or eliminate the food effect on bioavailability.5. Targeted drug delivery either by transcellular or intra-
cellular uptake.6. Molecule can be delivered via a required route with ease
in scale up.
This review focuses on the various established approachesfor the formulation of nanocrystals, the different published an-alytical methods applied for thermodynamic solubility deter-mination, assessment of dissolution properties and dissolutionrate enhancement upon nanosizing, the effect on pharmacoki-netic (PK) properties such as bioavailability, the area undercurve (AUC), and the half-life due to size reduction as well asfuture research opportunities.
FORMULATION APPROACHES FOR NANOCRYSTALS
Before the first top-down processes were developed (i.e., tech-niques reducing the size of larger crystals by means of attritionforces), nanosized drug particles were produced using a sim-ple precipitation approach known as solvent–anti-solvent ad-dition technique. It is also referred as one of the “bottom-up”approaches. However, it is often difficult to control the particlegrowth/crystal growth using this technique as well as to scaleup by maintaining all the parameters constant. Therefore, itwas suggested to perform the precipitation step in conjunctionwith immediate lyophilization, or spray-drying, in order to re-duce the risk of crystal growth.
Top-Down Approach
There are two basic approaches which are well established forthe formulation of nanocrystals:
1. Top down: Involves the mechanical reduction of the par-ticle size by wet media milling or high-pressure homoge-nization (HPH).
2. Bottom up: Involves the generation of nanosized particlesfrom dissolved molecules by means of precipitation.9
Top-down methods can be further divided in to twoapproaches—homogenization and attrition wet media milling.
Attrition Wet Media Milling
This technology was developed at the Pharmaceutical ResearchDivision of Eastman Kodak (Sterling Winthrop, Inc.), whichwas set-up as NanoSystems LLC and later acquired by Elan.An active drug substance is dispersed with an aqueous solutionin which the stabilizers were pre-dissolved. As the surface ofnanocrystals is highly cohesive and has high surface energy,it should be stabilized by a single or mixture of stabilizers.Stabilizers can be ionic or stearic and can be used as a singleand/or in a combination of polymeric as well as surfactant sta-bilizers. This solution is poured in the grinding chamber alongwith spherical beads/balls while the beads are rotated at veryhigh speed. It is believed that because of the attrition betweenmolecules’ surface and surface of the beads, particle size reduc-tion occurs; the beads/balls serving as a milling media. Beadsare available in various sizes and are of different materials,but generally are made of glass, zirconium oxide, or polymericmaterial. The type of material the beads are made of is a crit-ical factor as they can interact with the active drug substance.There is a fair chance that an impurity related to the materialof beads may contaminate the final product. Yttrium-stabilizedzirconium oxide is the most widely used type of bead by ma-jor pharmaceutical companies because in most cases, it doesnot interact with active drug substances. Although expensive,these beads are the best alternative to avoiding impurities inthe final formulation.21
The size of the beads has a direct relationship with the de-sired particle size range in the formulation of nanocrystals.22
The usual duration for conventional milling using overheadstirring is somewhere between 3 and 12 h. Certainly, these pa-rameters can change from molecule to molecule. Milling shouldbe stopped once the desired particle size range is achieved. Therotational speed of the milling media is also a critical parame-ter. With the too slow speed, the beads cannot rotate efficientlyand milling cannot be performed accurately, and with the toofast speed, the evenly rotating balls may remain at the uppersurface of the media and milling does not take place. With asystematic study by trial and error the formulator selects thestabilizers, as well as other milling parameters and optimizesthem in order to achieve the desired particle size range andstability. The final product characteristics can vary, depend-ing on the amount of beads, the ratio of active drug substanceto the amount of beads, the ratio of concentrations of activesubstance to the stabilizer, milling time, milling temperatureas well as milling duration.23 This method is simple, inexpen-sive, and easily scalable. The only drawback associated withthis technology is the contamination related to the beading
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

4 REVIEW
material. That aside, several products have successfullyreached the commercial level using this technology.
High-Pressure Homogenization
There are several established methods for the formulation ofnanocrystals using the homogenization approach. The microflu-idization technology (Insoluble Drug Delivery-Particles IDD-PTM Technology), Dissocubes R© technology, and Nanopure R©
technology are examples of the methods that fall under thiscategory. Microfluidizers are known as high shear fluid pro-cessors that are unique in their ability to achieve monomodalparticle size reduction. It reduces particle size by a frontal colli-sion of fluid streams under pressure of up to 1700 bar.24 At veryhigh pressure, collision and cavitation occur. The major draw-back associated with this method is that it requires at least50–75 cycles to achieve the desired nanometer size range. Thismakes the method more tedious and relatively more time con-suming as compared to milling. Dissocubes R© technology workswith piston gap homogenizer, which was developed by Mullerand his colleagues. In this method, a crude aqueous suspensionof active drug substance and stabilizer is forced through a tinyhole, which can reach a pressure of up to 4000 bar. The widthof the homogenization gap is adjustable, which is typically inthe micrometer range.
Compared with wet media ball milling, there are fewerchances to generate impurities with HPH. The negative aspectsof using this method are cavitation, which causes mechanicalwear, as well as noise, although fragmentation is a beneficialeffect associated with cavitation. The main source of impuritycomes from the wearing out of equipment parts. Almost all ma-chine parts are made of stainless steel, which leads to a very lowimpurity level when the nanosuspension is prepared using theHPH. Krause and Muller25 carried out a comparative study andobserved a negligible amount of iron impurities in the nanosus-pension formulated with 20 cycles at 1500 bar. Wear and tearoccurs only when very hard material is processed through thepiston gap. Using stainless steel material can also lead to wearand tear as the new type of homogenization valves used todayare made of ceramic tips which are able to withstand the harshprocessing conditions.26 Homogenizers vary in size from a smallscale to large scale production.27 Many research studies havereported minimal growth of microorganisms as a result of theHPH process.28 These improve the shelf life of the nanosuspen-sion and avoid the need for further studies that are requiredif it is administered orally. However, it is not a rule of thumb,the HPH is generally used for relatively soft material and beadmedia mill is used for relatively harder or harsh material.
Combinative Approach
In order to proceed with both the top down technology (wet me-dia milling, HPH) micronized powder is required as the startingmaterial, which leads to a long process time. In order to over-come this drawback, a combinative formulation approach wasdeveloped. The combinative approach was first developed andintroduced by Baxter Inc. as NanoedgeTM technology. Today fivecombinative methods have been successfully developed.
1. NanoedgeTM—microprecipitation + HPH2. H69—microprecipitation immediately followed by HPH
(minimization of time between two steps in order to pro-duce even smaller crystals)
3. H42—drug pre-treatment by means of spray-drying fol-lowed by standard HPH
4. H96—Freeze drying combination with HPH5. CT—Media milling followed by HPH
In the microprecipitation stage, the drug is usually dissolvedin a suitable organic solvent that is miscible with water. Thedrug solution is then added to an aqueous solution in whichstabilizers have been pre-dissolved. The drug solution is addedin a controlled manner to prevent inadequate crystal growth.After the microprecipitation step, precipitates are convertedinto more stable crystals in the nanometer size range with thehelp of top down technologies (i.e., HPH, media milling, andsonication). The amount of residual content in the final prod-uct is the major concern while using a combinational approachduring scale up. The presence of organic solvent can alter thephysicochemical properties of the active drug substance.29 Itmay also be responsible for the Ostwald’s ripening. To preventthis from happening, an alternative method was developed bySalazar et al.21 known as H 42 and H 96 technology. H42 usesthe spray drying of the microprecipitated solution that was de-veloped with the bottom-up approach, and then followed byHPH. In the case of H96, it employs the freeze drying of the mi-croprecipitated solution, followed by a top-down approach. In-deed, on the one hand, this method has more advantages thanany single step conventional method, but on the other hand,any additional steps in the procedure require more careful andmore extensive research, and control of additional parameters,which will increase the cost of the end product development. Todate, no product has been developed and marketed using thistechnology, but research papers have been published for theformulation or production of nanocrystals using the combina-tive approach. Among these, the top-down approaches are moreconvenient because of the ease of being able to govern the parti-cle size range as well as the ease of scaling up. Because of thesebenefits, several products have been successfully launched tothe commercial level.
Bottom-Up Approach
This method is also known as the precipitation approach.Hydrosols30 and Nanomorph31 techniques are examples of thebottom-up approach. The particles generated by Nanomorphtechnology are amorphous in nature, which give an advantageof both a higher supersaturation and a higher dissolution rate.It is well known that amorphous systems are high energy sys-tems; therefore, because of their high rate of crystallization, un-controllable crystal growth occurs, which leads to a reduction insolubility and eventually, reduction in bioavailability. Althoughboth technologies are scalable, they require the control of dif-ferent parameters, such as temperature and the stoichiometryof the solute, solvent, and the stabilizer.
UNDERSTANDING SOLUBILITY BEHAVIOR ANDMETHODS OF DETERMINATION
Several research papers have discussed the impact of solubilityand particle size on the PK performance of nanocrystals. Someof the literature has reported that the generation of surface cur-vature and crystal defects on the particle surface have an enor-mous impact on its solubility behavior. Another possible causemight be the development of high energy surfaces through
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 5
attrition during particle size reduction. According to the litera-ture, solubility may range from one-fold to several fold, based onparticle size.17–19 Bioavailability enhancement associated withnanocrystalline API is attributed to an increase in the dissolu-tion rate because of the enlargement of SA and some increasein solubility based on particle size. This solubility enhance-ment should be in fair agreement with what would be expectedbased on the Ostwald–Freundlich equation. A change in solu-bility is more significant when particle size is reduced to below100 nm, which can also be described by the Ostwald–Freundlichequation. Rapid dissolution associated with a nanoparticulatesystem is clear evidence of a generation of transient super sat-uration of a solution compared with the bulk solubility of astable crystal form. In the case of crystalline nanoparticles, thedegree of supersaturation is low compared with high energyamorphous solids, as particle size has limited impact on satu-ration solubility.
Determining accurate solubility is vital to characterize theeffectiveness of the formulation. There are several challengesassociated with the accurate determination of solubility of anyformulation, as it varies case by case. Accurate measurementis significantly more complicated in the case of nanoparticulatesystems, as they have the tendency to remain in suspendedform in the solution after using conventional approaches. It isalmost impossible to visualize the presence of nanoparticles inthe filtrate with the naked eye. The intrinsic solubility of poorlysoluble compounds is extremely low in number; therefore, thepresence of a couple of undissolved particles can lead to a signif-icant error in measurement. While reviewing the literature fordetermining solubility by a separation-based method, we havefound the absence of a validated universal method for accuratesolubility determination. This makes it even more challengingwhen dealing with particle size in the nanometer range, as com-pared with the micronized or bulk particles. The following arethe general challenges associated with solubility determinationof the nanoparticulate system.
1. No standard method is available in the literature for sol-ubility determination,
2. Difficulty in separation of the dissolved and undissolvednanocrystals/particles because of smaller size.
3. Confirmation that equilibrium is attained or not.4. Reproducibility of results.5. Validation of method for accuracy.
In addition to the above challenges, one also has to considerother process parameters which vary with the physicochemicalproperties of the active drug substance for solubility determina-tion. For instance, if the API is weakly acidic or basic, then thepH of the solution plays an important role. It is difficult to deter-mine whether or not equilibrium is attained in this particularcase. Several researches have published different approachesfor the solubility determination of nanocrystals. Although nu-merous methods for the separation of dissolved and undissolvednanoparticles have been reported in the literature, these are themost common approaches used described in Figure 1. An aque-ous solubility determination by separation-based approach iswidely accepted, has been used in industry and academia formany decades, and is the most convenient way to determinesolubility. Typically, it is a two-step process: initially, an excessamount of drug is dispersed in an aqueous or buffer solution.
The equilibrium is established by shaking or stirring the solu-tion at a specific rpm for a specific time and temperature, atwhich we want to determine the solubility. Usually the sam-ples are withdrawn after 24 and 48 h. Samples were either cen-trifuged or filtered from syringe filters. A sample analysis wasperformed using the HPLC and UV. In the case of crystallinenanoparticles, the research articles listed in the Table 2 havereported the solubility determination data for nanosuspensionsand nanocrystals by utilizing a separation-based approach astheir primary method for solubility determination. The mostcommonly reported approaches for solubility determination ofnanoparticles are by shake-flask method at a specific temper-ature. Most of them have overestimated the thermodynamicsolubility associated with nanocrystals, which is why it is im-portant to consider some additional factors during solubilitydetermination when particle size is reduced to nano from mi-cron range. The selection of appropriate pore size filters withrespect to the particle size of crystals, and the selection of anappropriate spectroscopic analytical method, is the key factorthat needs to be taken in to consideration for accurate solubilitydetermination of crystalline nanoparticles.
Bernard Van Eerdenbrugh reported that the UV spectra is areliable tool to determine the concentration of micronized par-ticles, however, it is not a reliable tool for the determinationof the concentration of nanosuspensions, as it is overestimat-ing the actual solubility data. With particles in the nanome-ter range, they itself absorbs the UV light. Therefore, the ab-sorbance data are the mixture of the dissolved and undissolvednanosized particles.32 Today, the measurement of the dissolveddrug concentration using an in situ UV probe is the preferrednoninvasive method because of its sophistication in terms ofcontingency and its ability to record data from the start of dis-solution. However, absorption of light from particles is size de-pendent and it is having a great influence on smaller particles.With felodipine as a model drug, an observation has been madethat both nanoparticulates of felodipine and free felodipine inthe solution absorb light in a similar way, which results in anoverestimation of dissolved concentration than what was actu-ally dissolved.33 The results were also dramatic, even for thesecond derivative of UV spectra. Moreover, the generation ofnanoparticles occurs when working with nanosuspensions orsupersaturated systems, so caution should be taken.
The solubility associated with crystalline nanoparticles ismoderately higher (10%–15%)16 compared with what is re-ported in Table 2.34–44 In the case of indomethacin, the reportedsolubility enhancement was nearly twofold higher. The same istrue in the case of oridonin,36 reccardin D,38 and simvastatin39
where reported solubility was substantially higher as comparedwith bulk crystal solubility. One possible reason behind thismisleading data may be the use of an inappropriate separatingmethod and/or analytical method. Nanoparticles with an aver-age size of 200–400 nm can easily pass through 0.22 or 0.45 :mpore sized filters. Determining the concentration of such a fil-tered solution using UV leads to a further over-estimation ofactual data because of the mixture of absorbance of both theundissolved and dissolved particles. Moreover, centrifugationat moderate speed of about 10,000–30,000 rpm is not suffi-cient to suspend particles in the nanometer range, therefore,the resultant supernatant contains a mixture of dissolved andundissolved particles. It is noticeable that care should be takenin choosing syringe filters for appropriate pore size. Juene-mann et al.45 were able to show in their study a differentiation
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

6 REVIEW
Tab
le2.
Exp
erim
enta
lSol
ubi
lity
Det
erm
inat
ion
wit
hS
epar
atio
n-B
ased
App
roac
h
Dru
gM
eth
odF
iltr
atio
nP
arti
cle
Siz
ean
dA
nal
ytic
alIn
stru
men
tR
epor
ted
Sol
ubi
lity
Ref
eren
ce
Indo
met
hac
in(I
ND
)S
hak
e-fl
ask
at25°C
0.2:
mU
VN
Sa:5
.86
±1.
2m
g/10
0m
L34
Ph
ysic
alm
ix:2
.30
±0.
51m
g/10
0m
LP
oly
1:0.
91±
0.26
mg/
100
mL
Pol
y2:
1.44
±0.
34m
g/10
0m
L
Indo
met
hac
in(I
ND
)S
hak
e-fl
ask
for
12h
inac
etat
ebu
ffer
pH5
NM
bU
VIN
D–p
hys
ical
mix
:4.8
9±
0.18
:g/
mL
35P.
size
:80:
mN
ano-
IND
/F68
:6.4
3±
0.06
:g/
mL
580
±30
nm
Nan
o-I
ND
/F12
7:4.
80±
0.0:
g/m
L58
0±
20n
mN
ano-
IND
/pol
ysor
bate
:80:
10.9
±1.
54:
g/m
LN
otde
term
ined
Ori
don
in(O
RI)
Con
stan
t-te
mpe
ratu
resh
aker
at37°C
and
100
rpm
inph
osph
ate
buff
erso
luti
on(p
H7.
4)
0.22
:m
mic
ropo
refi
lmU
VO
RI(
com
mer
cial
):99
±2:
g/m
L36
P.si
ze:2
00–4
00n
mO
RI
nan
ocry
stal
:170
±10
:g/
mL
How
ever
,au
thor
repo
rted
slow
decr
ease
inso
lubi
lity
afte
rac
hie
vin
gsu
per
satu
rati
onfo
rN
C.c
Can
desa
rtan
cile
xeti
l24
hst
irri
ng,
foll
owed
byce
ntr
ifu
gati
onat
25,0
00rp
min
phos
phat
ebu
ffer
con
tain
ing
0.7%
Tw
een
20(p
H6.
5)
0.2:
mU
VP.
size
:223
.5±
5.4
Bu
lk:1
25±
6.9:
g/m
LN
C:2
805
±29
.5:
g/m
L22
.44-
fold
impr
ovem
ent
37
Ric
card
inD
Sti
rrin
gin
PB
S(p
H7.
4)bu
ffer
at25°C
and
100
rpm
0.22
:m
mic
ropo
rou
sm
embr
ane
filt
er
HP
LC
P.si
ze:1
84.1
±3.
15n
mP.
size
:815
.37
±9.
65n
m
Bu
lk:0
.619
2±
0.02
45:
g/m
L38
NS
(eva
pora
tive
prec
ipit
atio
nin
toaq
ueo
us
solu
tion
):24
2.1
±12
.1:
g/m
LN
S(m
icro
flu
idiz
atio
n):
31.5
±1.
9:
g/m
L
Sim
vast
atin
Pow
der
form
:sh
ake-
flas
km
eth
odat
37°C
,0.
22:
mW
hat
man
filt
erS
upe
rnat
ant
UV
P.si
ze:3
00.3
nm
Sol
ubi
lity
enh
ance
men
t:36
.14-
fold
39
NS
:cen
trif
uga
tion
at10
,000
rpm
Fen
ofibr
ate
Sh
ake
flas
km
eth
od,s
usp
ensi
oneq
uil
ibra
ted
at37°C
for
72h
0.22
:m
mem
bran
efi
lter
HP
LC
Sol
ubi
lity
40N
S:P
.siz
e:60
6n
mC
onc.
SD
S%
(W/V
)B
ulk
-sol
ubi
lity
(:g/
mL
)0.
00.
34±
0.03
0.1
1.42
±0.
100.
1511
.95
±0.
160.
226
.38
±0.
390.
376
.11
±0.
380.
413
1.95
±1.
680.
518
3.09
±2.
170.
729
0.43
±5.
70
Con
tin
ued
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 7
Tab
le2.
Con
tin
ued
Dru
gM
eth
odF
iltr
atio
nP
arti
cle
Siz
ean
dA
nal
ytic
alIn
stru
men
tR
epor
ted
Sol
ubi
lity
Ref
eren
ce
Ato
rvas
tati
nca
lciu
mS
hak
efl
ask
met
hod
,for
24h
and
37°C
inD
Iw
ater
0.1:
mm
embr
ane
filt
erU
V41
P.si
ze:c
omm
erci
al:3
8.3
±0.
6:
m14
2.2
±0.
5:
g/m
L
Tu
rrax
R©=
21.5
±0.
03:
m18
5.1
±1.
2:
g/m
LH
PH
d:3
.12
±0.
05:
m29
9.8
±0.
6:
g/m
LH
PH
(20
cycl
es@
1500
bar:
=0.4
46±
0.02
:m
386.
5±
0.7:
g/m
L
Mel
oxic
amS
hak
efl
ask
met
hod
,for
24h
and
37°C
inD
Iw
ater
,sti
rred
sam
ple
wer
efu
rth
erce
ntr
ifu
ged
at10
,000
rpm
for
15m
in
0.22
:m
nyl
on-
mem
bran
efi
lter
UV
42
P.si
ze:
Raw
:4.4
±0.
50:
g/m
LR
aw:4
6.39
±7.
37:
mP
hys
ical
mix
ture
:5.8
3±
0.62
:g/
mL
Son
icat
ed:0
.259
±0.
03:
mS
pray
-dri
edN
C:2
1.84
±0.
78:
g/m
L
Son
icat
ed+H
PH
:0.2
12±
0.04
:m
Spr
ay-d
ried
:0.1
78±
0.02
:g/
mL
Lu
tein
Sam
ples
wer
eke
pton
shak
er10
0rp
man
d25°C
dist
ille
dw
ater
(pH
=5.
5)an
ddi
stil
led
wat
erco
nta
inin
gsu
rfac
tan
tso
luti
on(0
.05%
,w/w
Pla
nta
care
R©20
00,p
H=
10.5
).S
ampl
esw
ere
cen
trif
uge
dat
23,8
00g
for
2h
0.2:
mfi
lter
UV
DIw
ater
:<0.
054:
g/m
LD
Iwat
er+
surf
acta
nt:
0.54
:g/
mL
nan
ocry
stal
:up
to14
.3(>
264-
fold
than
wat
eran
d>
26.3
-fol
dw
ater
wit
hsu
rfac
tan
t)
43
P.si
ze:4
29n
m
Qu
erce
tin
Sam
ples
wer
eke
pton
ash
ake
at37°C
and
100
rpm
.Sam
ple
wer
ew
ith
draw
nan
dtr
ansf
erto
ult
rafr
eetu
bew
ith
cuto
ffof
10kD
aan
dce
ntr
ifu
ged
at20
,000
gfo
r30
min
at4°
C
NM
HP
LC
Bu
lk:1
0.28
g/m
L44
P.si
ze:
PM
:16.
42g/
mL
Dri
ed-E
PA
S:2
82.6
±50
.3n
mE
PA
S(e
vapo
rati
vepr
ecip
itat
ion
into
aqu
eou
sso
luti
on):
422.
4g/
mL
HP
H:2
13.6
±29
.3n
mH
PH
:278
.6g/
mL
aN
S,n
anos
usp
ensi
ons.
bN
M,n
otm
enti
oned
.c N
C,n
anoc
ryst
aldH
PH
,hig
h-p
ress
ure
hom
ogen
izat
ion
.
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

8 REVIEW
Figure 1. Reported approaches for the solubility determination.
between suspended submicron colloidal particles and molecu-larly dissolved particles. It has been reported that the resultsof solubility and dissolution of nanocrystals are comparablewith each other if the analysis is performed with filters havingpore size � 0.1 :m. Using larger 0.2 and 0.45 :m filters, thenanocrystalline system shows apparent supersaturated behav-ior because of the combinatory effect of dissolved and undis-solved nanocrystalline particles. In other words, it has beendemonstrated that filters with a bigger pore size may not besufficient enough to hold back the colloidal particles. An ex-cellent demonstration has been reported by carrying out thestudy of a selection of appropriate filters and their impact onobserved in vitro results. It was also compared with an in silicomodel for more precise justification of the experimental data.Overall, the conclusion and recommendation has been madefor using filters with smaller pore sizes (i.e., 0.1 and 0.02 :m)when dealing with nanoparticles.
Kinetic solubility determination by nephelometric or turbidi-metric methods during early screening of the drug molecule wasintroduced earlier by Bevan and Lloyd.46 Bernard Van Eerden-brugh critically evaluated different methods for the solubilitydetermination of nanocrystals using four model compounds:itraconazole, loviride, phenytoin, and naproxen. The data ob-tained show that separation-based methodologies were not suf-ficient to determine solubility, as the data were not in fair agree-ment with the Ostwald–Freundlich equation. Noninvasiveanalytical techniques, such as light scattering and turbidime-try, were found to be more reliable for appropriate understand-ing of the solubility behavior of crystalline nanoparticles. Inthe case of amorphous nanosuspensions, Lindfors et al.33 havedetermined the solubility by plotting scattering intensity withthe drug concentrations. Presence of excessive stabilizers innanosystems also tends to generate the scattering of intensity.Hence, the method that Lindfors demonstrated is not accurateenough because of the summation of scattering intensities thatare generated by dissolved nanoparticles and micelles. In or-der to eliminate this, Van Eerdenbrugh et al.16 have chosenthe point of intersection at which scattering is exclusively dueto the dissolved drug concentration and determine the solu-bility. Measures solubility data by scattering, for loviride wascomparable to bulk solubility data. It was not feasible to
determine solubility for itraconazole from the turbidimetrymethod, as the method cannot be distinguished because of verylow solubility. Solubility determination for phenytoin can bedetermined precisely with both light scattering and turbidime-try. In the case of naproxen, determined solubility values wereslightly less than the unmilled compound but the results werewithin the standard margin of error. Hence, this shows thatboth turbidimetry and light scattering methods can be appliedto obtain more realistic solubility data for crystalline nanopar-ticles. Scattering can be used more precisely for compoundsthat have low scattering intensities and turbidimetry can beapplied on compounds having higher scattering intensities.Moreover, the solubility enhancement was in fair agreementwith the theoretical prediction from the Ostwald–Freundlichequation. For the theoretical calculation, the interfacial ten-sion was estimated (interfacial tension of typical pharmaceu-tical API ranges between 5 and 50 mN/m) as described in thereference literature.47 Experimental data and theoretical pre-dictions were also in agreement with the Ostwald–Freundlichequation, suggesting that solubility enhancement should bemarginal in the case of crystalline nanoparticles and both thelight scattering and turbidimetry are good noninvasive meth-ods for the solubility determination of nanocrystals. However,there are certain assumptions and limitations associated withthese analytical methods. In most cases, the dynamic light scat-tering is used to measure the light scattering intensity. Theinstrument assumes each particle as a sphere and carries outthe determination. When the particles are not spherical ini-tially or if the particles tend to change shape during disso-lution or solubilization, they may have different results thanthose measured by the instrument. Therefore, the impact ofparticle shape is a factor that also needs to be considered, as itplays major role during dissolution and solubilization. Anhaltet al.48 has reported a method for the solubility determinationby real time measuring the light scattering. The main focus wasto determine the equilibrium solubility and dissolution rate ofa crystalline nanosuspension with different particle size usingFBT as a model compound. The solubility results of the lightscattering method were fair enough to justify it as a reliableanalytical tool for the solubility measurement. Reported sol-ubility enhancement for nanocrystals was around 10%–15%,
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 9
Table 3. Alternative Approaches for Accurate Solubility Determination
Analytical Method, Compound and Particle Size Solubility Determination Solubility Enhancement Ratio Reference
Light scattering 48
Fenofibrate 8.69 ± 0.78 :g/ml140 nm 10.38 ± 0.01 :g/ml 1.19270 nm 8.70 ± 0.24 :g/ml 1.001070 nm 9.62 ± 0.50 :g/ml 1.11
Light scattering and turbidimetry 16
Loviride (162 nm) 0.0108 mg/mL 1.10Scattering – 0.0119 mg/mL
Itraconazole (220 nm) 0.0047 mg/mL 1.15Scattering – 0.0054 mg/mL
Phenytoin (406 nm) 0.0667 mg/mL 1.07Scattering – 0.0711 ± 0.007 mg/mLTurbidity – 0.07 ± 0.0034 mg/mL 1.05
Naproxen (288 nm) 0.2116 mg/mL 0.97Scattering – 0.2053 ± 0.003 mg/mLTurbidity – 0.2083 ± 0.0024 mg/mL 0.97
Separation-based methodology (ultracentrifugation, filtration—0.1 :m, 0.02 :m, and dissolution) 51
Griseofulvin-micro 7.63 ± 0.89 :g/mL 1.10362 nm 8.40 ± 0.25 :g/mL122 nm 9.99 ± 0.15 :g/mL 1.30Compound X-micro 65.17 ± 1.58 :g/mL 0.97238 nm 63.41 ± 1.26 :g/mL93 nm 89.06 ± 6.36 :g/mL 1.36Fenofibrate-micro 0.74 ± 0.27 :g/mL 1.11290 nm 0.82 ± 0.26 :g/mLCelecoxib-micro 1.00 ± 0.03 :g/mL 1.11341 nm 1.11 ± 0.03 :g/mL
which justifies the previously reported solubility data by VanEerdenbrugh.16 However, one should consider certain limita-tions before utilizing this light scattering method. Most impor-tantly, the sample has to be ultra clean; the presence of any dustand debris may lead to the generation of scattering intensitythat affects to the observed data. The use of a plastic cuvette isalso a potential source of error. Moreover, as light scattering isless sensitive to small particles, the results are slanted towardsthe larger sized particles as they have a tendency to generatemore scattering of light. Besides these methods, other analyti-cal techniques like potentiometry and pulse polarography havealso been reported for real time solubility measurement.49,50
However, these methods are not universal and can be used fora fewer number APIs with certain properties (i.e., electroac-tive). In the case of potentiometric measurement, each time aspecific electrode has to use for the specific API.
In general, separation-based methods are universally ac-cepted as they do not require a high level of experimental skill.Murdande et al.51 has reported three different approaches (ul-tracentrifugation, ultracentrifugation with filter, dissolution) todetermine the accurate solubility. Ultracentrifugation was usedafter optimizing different parameters such as speed, time, andtemperature for the satisfactory separation of dissolved andundissolved nanocrystals. Syringe filters were also used (i.e.,0.1 and 0.02 :m) based on the particle size to determine sol-ubility from the supernatant of the ultra-centrifuged sample.In addition, dissolution data at the end of the experiment wasalso evaluated for the total dissolved concentration based on the
theoretical knowledge that nanocrystals should reach the satu-ration level at equilibrium. Results from all three methods weresimilar and in fair agreement with the Ostwald–Freundlichequation. The results from the solubility determination usingthe separation-based approach described above are in Table 3.Interfacial solubility (the concentration in a boundary layer of aspherical particle) plays an important role. As the particle sizedecreases, the SA increases proportionally, along with the in-terfacial tension. Sun et al.52 have determined the equilibriumsolubility of coenzyme Q10 nanocrystals and bulk drug in threedifferent dissolution media, which were mixtures of differentconcentrations of tween 20 and isopropanol. Solubility usuallyleads via diffusion and the driving force would be the differencebetween the solubility at the boundary layer and the bulk drugconcentration. Based on observations, they had also proposeda solubility model for nanocrystals and bulk drugs.52
Another separation-based approach is the determination ofsolubility and/or drug release with the application of equi-librium dialysis. The published research has applied thisconcept, mainly for the nanoparticle-based formulation oflarge molecules and a few for small molecules, and de-termined the equilibrium solubility and drug release fromnanoparticulate formulation. The most common approaches in-clude: sac dialysis,53,54 side by side dialysis,55–57 and reversedialysis.58,59 In dialysis, separation is achieved by means ofa semi-permeable membrane using molecular weight cut-offmembrane. Assuming that the dialysis membrane is perme-able to free API only, Frank et al.60 reported the quantification
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

10 REVIEW
of molecularly dissolved, poorly soluble drug by using the equi-librium dialysis method and determined the apparent solubility(molecularly dissolved API + miscellany solubilized drug). Thesolubility of the drug in both the Hanks Balance salt solutionsand the supplementary salts (HBSS++) and fasted-state sim-ulated intestinal fluid (FaSSIF) buffer were nearly the samewithin the margin of error.60 It is well known that nanoparti-cles have a rapid release dissolution kinetics. Efforts have beenmade to determine the interplay of the diffusion rate, size ofthe molecular weight cutoff (MWCO) membrane, and concen-tration difference of the donor and receiver compartment byMoreno-Bautista and Tam.61 Decreasing the dialysis cassettesto smaller MWCO showed a reduction in the diffusion rate. Thecompounds having a molecular weight of around 200–400 Dashowed a diffusion rate profile several times higher with 10 kDamembrane compared to 2 kDa membrane MWCO. The cassetteshaving a pore size smaller than the drug molecule should besuitable for the evaluation of the dissolution rate of nanopar-ticles. Furthermore, the release profile from the dialysis cas-settes failed to catch some necessary events, such as the bursteffect and lag time, which leads to a question the suitability ofthe method for true discrimination of the rapid release kineticsof submicron size colloidal particles. This situation promptedZambito et al.62 to ask question whether the dialysis is a re-liable method for studying drug release from nanoparticulatesystems. Their study concluded that for nanoparticles, the dial-ysis method was insufficient in expressing the discriminationand founded results were deceptive. Because of a reversible in-teraction between the drug and dispersed nanoparticles, therate of permeation through the dialysis membrane was neg-ligible as compared with the plain drug solution. Hence, thekinetic release was found to be far less and unrealistic. Withsuch a study, the release kinetic is governed by the dialysismembrane (not dependent on the drug release from colloidalparticles), which makes it unreliable for the in vitro predictionsand means the data may not be very discriminative.
DISSOLUTION
Dissolution is known as a significant tool for the analysis ofpharmaceutical formulations. Indeed, it has somewhat poten-tial to predict the in vivo performance. Prediction of the extentof absorption can be made from the rate of drug release in thegastrointestinal tract.63 A drug candidate has to pass throughsome pre-requisites steps before being absorbed into the sys-temic circulation. Dissolution is one of the essential steps foreffective absorption of a drug candidate and is a key parame-ter for assessing the onset of action of an oral dosage form. Asper the well-known BCS, classification compounds belonging toClass II and IV are poorly soluble in nature, especially onesbelonging to Class II, which have a dissolution rate of limitedabsorption because of their low aqueous solubility.64 In anotherwords, the rate of absorption is proportional to the rate of disso-lution in the gastrointestinal tract. For a given drug moiety thatdissolves in the gastrointestinal tract, its dissolution can be tai-lored by either generating amorphous systems or reducing theparticle size to the micron or submicron level (i.e., nanometer).The motivation for the development of nanosystems has beengenerated from the increased number of new chemical entitieswith poor aqueous solubility. For such low aqueous-soluble com-pounds, even micronization is not sufficient enough to eliminate
the problem. The reduction of particle size leads to an increasein the SA of the drug particle. The SA enhancement factor frommicron to nanoparticle is about 10-fold. Thus, significant en-hancement in SA has a positive impact on the dissolution rateof a drug particle. This positive effect on the dissolution ratecan create a higher concentration difference between the gut lu-men and the blood, which increases the absorption via passivediffusion and leads to an improved therapeutic response. Directproportionality of the rate of dissolution with respect to specificSA has been well documented by the Noyes–Whitney equation.As a follow up to this, Nernst–Brunner and Danckwerts alsoproposed modified equations to describe the dissolution behav-ior a solid powder.
Noyes − Whitney Equation :dMdt
= k(Cs − C) (1)
Nernst − Brunner Equation :dMdt
= SDh
(Cs − C) (2)
Danckwerts′ surface − renewal model :dMdt
= S√
DP (Cs − C)
(3)
This section will provide an overview of the different estab-lished methods to assess the dissolution for nanocrystals. Asof now, it is well understood that particle size is inversely pro-portional to SA and the dissolution rate has a direct relation-ship with the change in SA. The major challenge is to developa discriminative dissolution method for poorly water-solubledrugs. Earlier reports have indicated that there is an alterationof wetting behavior with particle size reduction. In the caseof nanoparticles, the wetting phenomenon is more prominent,which leads the dissolution rate to increase more quickly. More-over, the reduction in the diffusional distance upon size reduc-tion generates a moderate spring effect that quickly achievessupersaturation level with respect to particle size during dis-solution (Fig. 2). Therefore, the traditional methods are inad-equate to determine the actual dissolution rate enhancementfor nanoparticles which intensify the need for an appropriatemethod to perform the dissolution study of nanoparticles.
Sink Condition (Conventional) Dissolution
Sink condition dissolution condition is defined as the volumeof the dissolution medium which can dissolve more than threetimes the amount of the dose used in the dissolution study.65
In most cases, the dissolution study is performed using a USPtype – I or II apparatus. Usually for a study of a drug releaseprofile, the dissolution is carried out in 900 mL of dissolutionmedia (i.e., in a different pH or in deionized water) at 37 ± 0.5°Ctemperature and by rotating at a specific rpm (i.e., 100 rpm).Samples are withdrawn at specific time intervals throughoutthe dissolution study. After each sample withdrawal, the sameamount of the fresh dissolution media, which is equilibrated atthe same temperature, is introduced to maintain perfect sinkcondition. In most cases, samples will be filtered prior to anal-ysis. However, for the nanoparticles, sink condition dissolutionwill provide good qualitative and less quantitative informationregarding the dissolution behavior of the formulation. So, thecomparison of dissolution profiles between nanosuspension andmicrosuspension will show the impact of particle size on disso-lution velocity. The literature has reported a higher dissolution
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 11
Figure 2. In vitro surface dissolution, (A) surface image dissolution in correspondence with diffusional layer thickness (h), and (B) intrinsicdissolution profile in correspondence with the surface image dissolution.
rate for the nanosuspensions,66,67 which dissolve instanta-neously as compared with micronized suspension. Hence, sinkcondition dissolution is an appropriate tool for QC analysis.However, because of the instantaneous dissolution behavior ofnanocrystals during sink condition, it is challenging to quan-titatively discriminate dissolution rate enhancement with re-spect to particle size. In addition, the long sampling intervalduring conventional dissolution also adds to the difficulty. Inresponse to these problems, few scientists have tried alterna-tive approaches.
Flow-Through Cell
The flow-through cell dissolution apparatus demonstrated thecapability of studying the dissolution of all kinds of formula-tions, such as tablets, capsules, and powders.68,69 Heng et al.70
have carried out dissolution studies and compared the dissolu-tion rate by asking the question, “What is the suitable disso-lution method for drug nanoparticles?” Initial dissolution rateswere determined for the paddle, basket, and flow-through ap-paratus. The initial dissolution rate was calculated from thefollowing equation:
( dMdt
)Nanoparticles( dM
dt
)Unprocessed
=[slope
( %dissolvedtime
)]nanoparticles[
slope( %dissolved
Time
)]unprocessed
The paddle and basket dissolution apparatus were describedas inappropriate for nanoparticles because of their tendency toform aggregates. The ratios obtained for the initial dissolutionrate enhancement in both cases did not agree with the modelpredicted values. Dissolution studies via the dialysis process(membrane with MWCO 12–14 kDa) were found to be very slowand having a limited ability for size discrimination. As a result,there was no significant difference noted in the dissolution pro-files between nanoparticles and the unprocessed powder. Basedon the analysis, the flow-through cell set-up was described asappropriate for dissolution of nanoparticulate powder by mini-mizing the wetting problems.71 The experimental data for thedissolution profiles were able to discriminate well with the un-processed powder. The initial reported dissolution rate ratiowas the average number of the triplicate study and was inagreement (6.95 vs. 7.97) with model predicted value. The au-thors concluded it as the most suitable analytical process forthe dissolution of nanoparticulate powders. However, selection
of an appropriate flow rate is required for proper discriminationbecause a change in the flow rate can generate change in therelease behavior. Note that the presence of air can also affectthe flow rate during the study, which may alter the dissolu-tion behavior. Therefore, the study should be carried out withcaution.
Alternative Approaches
Nanosuspensions/nanocrystals exhibit instantaneous dissolu-tion behavior, making it difficult to monitor them with conven-tional methods, which requires sample withdrawals, as well asdilution and filtration steps before quantitative analysis. In situfiber optic probes are not able to provide an accurate quantita-tive determination because of the generation of absorbance byboth the dissolved and undissolved nanocrystalline particles.32
Recently, Kayaert et al.72 reported an alternative approach bystudying the dissolution behavior of nanosuspensions using asolution calorimeter. The use of a solution calorimeter for dis-solution study has been previously reported for polymer andpolymeric blends.73 This dissolution study was examined basedon appraising the change in the heat throughout the process. Inother words, heat required for the dissolution process is mea-sured. The methodology consists of sealing the breakable glassampoule along with nanosuspension using bees wax. The glassvial should be kept in the sample cell, surrounded by the me-dia in which the dissolution study is intended to perform. Afterreaching the required temperature, the glass vial should bebroken, and the dissolution process is started. The rate of dis-solution can be then assessed by converting the raw data (i.e.,temperature vs. time and cumulative heat vs. time) to percent-age dissolved versus time. The dissolution process for nanosus-pensions was observed to be extremely fast. It takes just 20 s tocomplete the dissolution process for nanosuspension, whereasin the case of crude suspension, it was found to be between8 and 15 min For the traditional dissolution apparatus (i.e.,basket and paddle), the earliest sample one can withdraw isat 2 min. Hence, the solution calorimeter unquestionably pro-vides the advantage of real time measurement compared withtraditional methods. Consumption and/or production of heatcan be monitored from the beginning of the dissolution processwithout disturbing (i.e., sample withdrawal) the system. Thereare drawbacks with this method, which need to be consideredfor an accurate evaluation of the data generated. The method
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

12 REVIEW
measures the summation of the total heat change, which in-cludes contributions from the breakage of the glass ampoule,heat change from other excipients in the formulations, and heatchange due to the dissolution process. Therefore, a careful eval-uation of the data is warranted by considering all these con-tributing factors. In addition, the reported dissolution time isfar shorter (i.e., 20 s to 15 min) using this method, but a singleexperiment requires additional time for the equilibration beforethe test and also requires post-test time after the dissolution,making it more time consuming than the conventional dissolu-tion methods. Furthermore, the instrument is very subtle andrequires a skilled operator. Recently, another separation-basedapproach was reported by Shah et al.74 using a modified dial-ysis method known as pulsatile microdialysis (PMD)75 for thecharacterization of supersaturation and precipitation behaviorof poorly soluble drugs. Here, the pore size for the dialysis probewas approximately 18 kDA (�2 nm). Hence, the final sampleshould contain only the dissolved drug. This analytical methodcan be useful for characterization of high energy solid forms(amorphous) or nanoamorphous33 forms because of the advan-tage of quick sampling (i.e., 10 s). As a more convenient directsampling method, PMD may not be much useful for the study ofnanocrystals with the size range of 150–400 nm because of theavailability of the syringe filters with pore size 0.1 :m. The useof 0.02 :m (�20 nm) anotop syringe filters for the dissolutionstudy has also been reported in the literature.45 As a result, itmay be of great interest if the comparison of the sample anal-ysis from PMD and the sample analysis from 0.02 :m syringefilters has been carried out to describe the usefulness of themethod more precisely.
Another separation-based approach has been reported byMurdande et al.51 by modifying the traditional sink dissolu-tion to various non-sink conditions. Non-sink conditions canbe generated by pre-dissolving API in the dissolution me-dia prior to perform the dissolution experiment. Recently, an-other literature has also reported the dissolution of nanocrys-talline suspension for poorly soluble molecules using non-sinkconditions.76 Because of the lack of discrimination during theinitial phase of dissolution by sink dissolution, the goal wasto slow down the dissolution velocity of nanocrystals and mi-cronized crystals in such way that the initial dissolution phasebecomes more discriminative. Here, the samples were filteredwith both 0.02 :m (for nano) and 0.1 :m (for micro) after es-tablishing the filter binding capacity of the each model com-pounds. As the saturation level increases, the rate of disso-lution decreases, creating a more discriminating portrayal ofthe initial dissolution rate enhancement (i.e., at 75% satura-tion level the initial rate of dissolution, 10 :m:362 nm:122 nmwere 1.0:1.8:3.6). The observed data look more promising com-pared with the data obtained under sink conditions. However,filtration from 20 nm pore size of filters should be performedcarefully because of the chance of blockage or clogging of thepores by larger size particles. From our knowledge, all theseapproaches are reported specifically for nanocrystals. One canselect any analytical method listed above based on their re-quirements and the availability of resources.
PK BEHAVIOR OF CRYSTALLINE NANOPARTICLES
Different formulations have different effects on the PK profileof the same drug. Besides chemical properties, a change in the
physical property (i.e., particle size reduction) may also have aconsiderable impact on altering the PK behavior of a molecule.The reduction of the particle size increases the dissolution ve-locity and may have some effect on in vitro solubility. Similarbehavior was observed in the case of in vivo parameters, suchas AUC (+ve), Cmax (+ve), Tmax (−ve), and fed/fast variability(−ve). A reduction of particle size improves the dissolution rate,which increases the absorption of the drug in the body, and itleads to an increase in PK performance. Compounds belong-ing to the BCS Class II have issues related to poor solubility,dissolution-rate-limited absorption, and bioavailability. Parti-cle size reduction can improve the bioavailability of such com-pounds by improving the dissolution rate. For the nanocrystals,an increase in the oral bioavailability of the compounds can beattributed to an increase in the SA.77
Improvement in Oral Bioavailability
An improvement in the dissolution rate and adhesion to thegut wall can be considered the main contributing factors forenhancing bioavailability and overall PK performance. Afteroral administration, the formulation disintegrates and beginsthe dissolution process. The dissolution rate resembles theconcentration gradient in the physiological environment. Asa result, an improvement in the dissolution rate leads to anenhancement in the absorption, and finally, in the bioavail-ability of the compound. Because of the smaller size of thenanoparticles, they tend to adhere to the gut wall.78 Bioavail-ability enhancement can be achieved both actively and pas-sively. The classic example for bioavailability enhancement hasbeen represented in the case of danazol, which is poorly sol-uble (<1 :g/mL) and one of the most challenging compoundto work within the pharmaceutical industry.79 In vivo studiesof nanosuspensions of danazol (169 nm) in beagle dogs haveshown enormous enhancement in Cmax and a 16-fold enhance-ment in relative bioavailability, compared with the micronizedsuspension.12 Therefore, it is understood that by reducing theparticle size, the solubility issue associated with danazol canbe solved. Moreover, it can also be delivered at a lower dose byenhancing the therapeutic outcome of the compound. FBT isanother classic example of a poorly soluble drug with a high logP (i.e., 5.3) value. FBT is used in hypercholesterolemia and hasa solubility and dissolution-rate-limited absorption property.Bioavailability of FBT is attributed to the dissolution behaviorof particles in the gastric environment. A comparison of the PKprofile of nanocrystals and coarse powder demonstrated signif-icant enhancement in the rate of absorption after oral adminis-tration. The Cmax of nanocrystals was observed to be five timeshigher than that of the coarse powder, along with a higher AUCand Tmax.80 Zuo et al.40 made an effort to compare formulatednanocrystalline particles with the commercial nanocrystallineformulation LipidilTM-ez with respect to in vitro and in vivobehavior. No significant difference was observed between thetwo nanocrystalline formulations, suggesting that variabilitywill be less when particle size is reduced to nanometer range.Certainly, the re-dispersion behavior of dried nanocrystals alsoplays a contributing role by demonstrating reversible or irre-versible aggregation behavior. Bioavailability can be altered byseveral factors in the gastric environment, such as pH change,food effect, the presence of salts, and so on. In all the reportedcases reported in the Table 4,12,40,80–88 a significant enhance-ment in dissolution rate was observed for the nanocrystals,
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 13
Table 4. Effect on In Vivo Parameters
Compound Animal Model PK Parameters Comment Reference
Aripiprazole Beagle dogs NSa (350 nm) Coarse suspension 71% enhancement inrelative bioavailability
81Tmax (h) 1.04 ± 0.24 3.33 ± 1.50
Cmax (ng/mL) 137.37 ± 17.38 43.10 ± 11.68AUC (ng h/mL) 618.15 ± 81.28 386.06 ± 78.54
Nitrendipine Rat NS (209 nm) Tablet Fivefold enhancement inrelative bioavailability
82Tmax (h) 1 ± 0 2.2 ± 1.17
Cmax (:g/mL) 3.65 ± 0.43 0.60 ± 0.11AUC (:g h/mL) 17.12 ± 2.59 3.44 ± 0.47
Danazol Beagle dogs NS (169 nm) Coarse suspension 16-fold enhancement inrelative bioavailability
12Tmax (h) 1.5 ± 0.3 1.7 ± 0.4
Cmax (:g/mL) 3.01 ± 0.80 0.20 ± 0.06AUC (:g h/mL) 16.5 ± 3.2 1.0 ± 0.4
Naproxen Rat NS (270 nm) Unmilled suspension �1.25-fold enhancement inrelative bioavailability
83Tmax (min) 23.7 ± 5.1 33.5 ± 2.9
Cmax (:g/mL) 187 ± 18 126 ± 4AUC (:g min/mL) 19,062 ± 573 15228 ± 994
Apigenin Rat NCb (400—800 nm) Coarse powder �3.5-fold enhancement inrelative bioavailability
84Tmax (min) 90 ± 14 120 ± 16
Cmax (:g/mL) 5.4 ± 0.6 1.5 ± 0.2AUC (:g min/mL) 1509 ± 196 445 ± 45
Cefpodoxime proxetil Rabbit SDNSc (<300 nm) Microsuspension �1.6-fold enhancement inrelative bioavailability
85Tmax (h) 0.75 ± 0.11 1.75 ± 0.68
Cmax (:g/mL) 18.36 ± 2.03 10.88 ± 1.01AUC (mg h/mL) 47.55 ± 4.33 29.78 ± 3.47
Baicalein Rat Baicalin NC (335 nm) Coarse powder �1.6-fold enhancement inrelative bioavailability
86Tmax (h) 0.92 ± 0.38 1.67 ± 0.29
Cmax (:g/mL) 11.12 ± 1.25 7.18 ± 1.25AUC (:g h/mL) 119.25 ± 20.26 71.41 ± 4.38
Simvastatin Rat NC (387 nm) Coarse powder �1.5-fold enhancement inrelative bioavailability
87Tmax (h) 1.99 ± 0.05 2.88 ± 0.08
Cmax (ng/mL) 450.3 ± 140.5 300.2 ± 67.01AUC (ng h/mL) 1110.3 ± 280.62 770.9 ± 110.3
Fenofibrate Rabbit NC (460 nm) Coarse powder �4.7-fold enhancement inrelative bioavailability
80Tmax (h) �0.4 �1
Cmax (:g/mL) 536.66 ± 35.09 113.46 ± 29.05AUC (:g h/mL) 134.38 ± 6.47 28.41 ± 5.52
BMS-347070 Beagle dog NC Micronized �2.7-fold enhancement inrelative bioavailability
88Tmax (h) 2 3
Cmax (ng/mL) 1475 ± 375 483 ± 79AUC (ng h/mL) 28,613 ± 3850 10,870 ± 1651
Fenofibrate Beagle dog SDNCd LipidilTM-ez No significant difference inrelative bioavailability
40Tmax (h) 2.8 ± 1.8 5.2 ± 9.2
Cmax (ng/mL) 2075.2 ± 1101.1 2349.5 ± 1050.5AUC (ng h/mL) 30,496 ± 6541 34,035.9 ± 19,286.4
aNS, nanosuspension.bNC, nanocrystal.cSDNS, spray-dried nanosuspension.dSDNC, spray-dried nanocrystals.
which caused a significant reduction in the time to reach max-imum concentration, an improvement in the rate of absorp-tion, peak plasma concentration, and enhancement in relativebioavailability.
Food Effect
In most cases, food increases the bioavailability of the drug byincreasing bile secretion and increasing the duration of gas-tric emptying time. For a drug molecule’s clinical efficacy and
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

14 REVIEW
Table 5. Food Effect
PK Parameter
Fed Fast
Compound NSa Refb NS Ref Reference
ELND-006 Tmax (h) 1.4 3 1.4 1.8 90Cmax (ng/mL) 365 159 294 49.4
AUC (ng h/mL) 3063 1767 2430 315Fc 110 63.4 87.2 11.3
Fed Fast
NCd Jetmilled NC Jetmilled
Cilostazole Tmax (h) 1 1 1.3 ± 0.5 1 91Cmax (ng/mL) 4872 ± 112 2901 ± 314 5371 ± 1173 1029 ± 218
AUC (ng h/mL) 13,589 ± 3895 10,669 ± 3417 17,832 ± 4994 2875 ± 587F 0.67 ± 0.22 0.53 ± 0.21 0.86 ± 0.29 0.15 ± 0.04
Fed Fast
SNCDe SDDf SNCD SDD
Ziprasidone Cmax (ng/mL) 260 285 416 140 92AUC (ng h/mL) 1911 1949 2044 879
aNS, nanosuspensions.bRef, reference sample.cRelative bioavailability.dNC, nanocrystal.eSNCD, solid nanocrystalline dispersion.fSDD, solid amorphous spray-dried dispersion.
future success, persistence in oral bioavailability can only beachieved by eliminating the food effect.89 The presence of bilesalts in the gastric environment also has an impact on the dis-solution behavior of the molecule. It has been reported that thepresence of food reduces the dissolution behavior of micronizedparticles in certain cases as reported in Table 5.90–92 The ratioof bioavailability of the fed to fast state was observed to be closeto 1 in the case of nanocrystals, while micronized formulationof the same drug showed a significantly higher ratio (approx.sixfold) of the fed to fast state by demonstrating the poten-tial food effect after oral administration to an animal modelwith the same dosing. Bile salt secretion usually increasesin the fed state.93 A change in concentration of the bile saltin the stomach leads to a change in dissolution behavior andslows down or enhances absorption of the drug as depicted inFigure 3. This phenomenon causes a large variability from pa-tient to patient and also from fed state to fast state. Micronizedor larger particles that have shown improved absorption in thefed state might be because of the micelle formation. For thenanocrystals though, they are not helping in improving the in-trinsic solubility, but they provide an advantage by enhancingthe initial dissolution rate because of the larger SA. The higherrate of dissolution leads to an increased rate of absorption, andeventually, enhancement in the overall bioavailability, irrespec-tive of the fed or fast state. Hence, it can be stated that the bilesalts concentrations have significantly less effect on the absorp-tion behavior of nanoparticles. The same observation has beenreported for cilostazole91 [fed/fast ratio—0.78 (nano vs. 3.53jet-milled)]. Thombre et al.92 have reported the PK behavior ofan anti-psychotic drug ziprasidone in beagle dogs by conduct-ing the fed- and fasted-state bioavailability experiment for the
both solid nanocrystalline dispersion and the commercial blend(amorphous spray dried dispersion). The commercial blend hasshown a twofold improvement in bioavailability in the fed stateas compared with the fasted state, indicating the failure of thecommercial blend to prevent variability in absorption behaviorirrespective of the food state. A similar food effect was observedwith human data. On the other hand, nanocrystals have provento be efficient enough to prevent the variability from fed to faststate by generating a similar bioavailability profile in beagledogs. From the reported literature, it can be concluded that vul-nerability in the variation of oral bioavailability for potentialdrugs can be avoided with reduction in particle size to nanome-ter scale.
Particle Size Effect: Micro Versus Nano
The effect of particle size on in vitro and in vivo performance iswell documented elsewhere.91,94–96 Different particle sizes havea different effect on the initial dissolution rate, the rate of ab-sorption, and on oral bioavailability. Moreover, particles withnanometer size range may have the tendency to pass throughboth active and passive diffusion pathway, which increases thechances for sub-micron particles to reach to peak plasma con-centration with a reduction in time compared to macro/largeparticles. Sun et al.97 have shown the effects of particle size,ranging from micron to nanometer size, on Cmax, Tmax, andAUC.98 A large increase in bioavailability was observed for theboth nanoparticles (i.e., 300 and 750 nm) as compared withthe micron size particles and coarse powder, which is reportedin Table 6. The rise in bioavailability can be attributed to in-creased SA and adhesion behavior of nanosized particles. There
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 15
Figure 3. Effect of food on dissolution of nanocrystals and microcrystals.
Table 6. Particle Size Effect: Micro versus Nano
PK Parameter
Compound Size (nm) Tmax (h) Cmax (ng/mL) AUC (:g h/mL) Reference
Itraconazole 300 3 712 ± 121 9967 ± 2527 97750 4 501 ± 73 8649 ± 15805500 3 218 ± 86 1271 ± 398
Powder – 40 ± 9 197 ± 61Nitrendipine 200 1.0 ± 0.0 3.65 ± 0.43 17.12 ± 2.59 98
620 1.0 ± 0.0 2.75 ± 0.50 14.36 ± 2.752700 0.8 ± 0.1 1.74 ± 0.26 8.19 ± 0.854100 0.7 ± 0.1 1.19 ± 0.08 7.41 ± 0.46
20,200 3.4 ± 1.2 1.04 ± 0.21 6.89 ± 1.15Powder 4.1 ± 2.4 0.42 ± 0.08 2.76 ± 0.46
was significant difference observed in the dissolution profilesbetween both of the nanoparticles (i.e., 300 and 750 nm), butno significant difference has been reported in the PK profiles.The same observation was reported by Xia et al.98 by studyingeffect of particle size on the oral bioavailability of nitrendipinein the rat model. The overall bioavailability was reported tobe a ninefold increase compared with the coarse powder and athreefold increase as compared with the micronized particles.Comparing the PK parameters for both nanoparticles (200 vs.620 nm), a slight improvement was noted in Cmax, Tmax, andAUC. Based on the literature data, an interesting area for afurther research is possible, by lowering the particle size downto the 50 nm range with a narrow size distribution and mea-suring the relative bioavailability. This may have more pro-nounced effect on the bioavailability because of the further im-provement in the thermodynamic solubility suggested by theOstwald–Freundlich equation. A comparison of adhesion rates,
along with the various particle size ranges, starting from 50 nmto micron level, will also be an interesting area to explore forfurther understanding the particle size effect on the bioavail-ability.
SUMMARY
Drug nanocrystal formulation is a well-established and suc-cessful approach, and it is described in the initial phase ofthis review article. Nanocrystal formulation approach is morepromising because most of the major pharmaceutical compa-nies have adopted this approach because of its effectiveness andconvenience. During the early phase development and duringformulation development for pre-clinical studies, it is more con-venient to formulate the nanocrystal for the determination ofthe exposure and the PK parameters to confirm the candidacy
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

16 REVIEW
of the drug molecule. It is also important to know the thermody-namic and the kinetic behavior with respect to size reduction.Several approaches have been tried by researchers for the accu-rate determination of thermodynamic solubility (Tables 2 and3). Some have reported suspicious results due to generation ofartifacts by the analytical method for the solubility determi-nation. Despite the shortcomings of some of the conventionalmethods for determining solubility (specifically for nanoparti-cles), others have reported excellent results by adopting newerapproaches for the solubility determination. The boost in ther-modynamic solubility can be observed only when the particlesize is reduced to approximately 50–80 nm, in the remainderof the cases, only kinetic boost (i.e., the dissolution rate) canbe observed without greatly impacting the thermodynamic sol-ubility. As the nanocrystals have a high dissolution velocity,the traditional dissolution method is not suitable to discrimi-nate the quantitative difference in the dissolution behavior forthe nanoparticle. However, there are several alternative ap-proaches that have been described in this review article fordiscriminative analysis of the dissolution rate enhancementupon nanosizing. The initial dissolution rate enhancement as-sociated with particle size is a potential parameter for the esti-mation of bioavailability enhancement. More advanced work iswarranted in this area to understand the behavior of nanocrys-tals and to avoid excessive animal studies. The effect of food isfound to be negligible in the case of nanocrystals as comparedwith microcrystals. The particle size is shown to be a dominantcharacteristic in governing dissolution and bioavailability per-formances. Furthermore, some issues such as rate of adhesionalong with particle size change, and the mechanism of diffusion(i.e., active or passive) across the cell membrane still requireadditional study. The field of nanocrystal is growing rapidlyand is receiving the attention of researchers. In the comingdecade, nano formulations have great potential to go beyondits present level, largely because of having the advantage ofdelivering large and small drug molecules at specific targets.
Conflict of interest: The authors reports no conflict of interest.
REFERENCES
1. Lipinski C. 2002. Poor aqueous solubility—An industry wide problemin drug discovery. Am Pharm Rev 5:82–85.2. Butler JM, Dressman JB. 2010. The developability classification sys-tem: Application of biopharmaceutics concepts to formulation develop-ment. J Pharm Sci 99(12):4940–4954.3. Stella VJ, Rajewski RA. 1997. Cyclodextrins: Their future in drugformulation and delivery. Pharm Res 14(5):556–567.4. Jayne M, Lawrence GDR. 2000. Microemulsion-based media as noveldrug delivery systems. Adv Drug Deliv Rev 45:89–121.5. Serajuddin ATM. 1999. Solid dispersion of poorly water-solubledrugs: Early promises, subsequent problems, and recent break-throughs. J Pharm Sci 88(10):1058–1066.6. Dave RH, Shah DA, Patel PG. 2014. Development and evaluationof high loading oral dissolving film of aspirin and acetaminophen.J Pharm Sci Pharmacol 1(2):11.7. Rabinow BE. 2004. Nanosuspensions in drug delivery. Nat Rev DrugDiscov 3(9):785–796.8. Merisko-Liversidge E, Liversidge GG, Cooper ER. 2003. Nanosiz-ing: A formulation approach for poorly-water-soluble compounds. EurJ Pharm Sci 18(2):113–120.9. Verma S, Gokhale R, Burgess DJ. 2009. A comparative studyof top-down and bottom-up approaches for the preparation of mi-cro/nanosuspensions. Int J Pharm 380(1–2):216–222.
10. Kesisoglou F, Panmai S, Wu Y. 2007. Nanosizing—Oral formulationdevelopment and biopharmaceutical evaluation. Adv Drug Deliv Rev59(7):631–644.11. Amidon GL, Lennernas H, Shah VP, Crison JR. 1995 A theoreticalbasis for a biopharmaceutic drug classification: The correlation of invitro drug product dissolution and in vivo bioavailibilty. Pharm Res12(3):413–420.12. Liversidge GG, Cundy KC. 1995. Particle size reduction for im-provement of oral bioavailability of hydrophobic drugs: I. Absolute oralbioavailability of nanocrystalline danazol in beagle dogs. Int J Pharm125(1):91–97.13. Noyes AA, Whitney WR. 1897. The rate of solution of solid sub-stances in their own solutions. J Am Chem Soc 19(12):930–934.14. Kipp JE. 2004. The role of solid nanoparticle technology in theparenteral delivery of poorly water-soluble drugs. Int J Pharm 284(1–2):109–122.15. Muller RH, Benita S, Bohm B, Eds. 1998. Emulsions and nanosus-pensions for the formulation of poorly soluble drugs. Stuttgart Med-pharm Scientific Publishers, Germany.16. Van Eerdenbrugh B, Vermant J, Martens JA, Froyen L, HumbeeckJV, Van den Mooter G, Augustijns P. 2010. Solubility increases asso-ciated with crystalline drug nanoparticles: Methodologies and signifi-cance. Mol Pharm 7(5):1858–1870.17. Dai WG, Dong LC, Song YQ. 2007. Nanosizing of a drug/carrageenan complex to increase solubility and dissolution rate. IntJ Pharm 342(1–2):201–207.18. Hecq J, Deleers M, Fanara D, Vranckx H, Amighi K. 2005. Prepara-tion and characterization of nanocrystals for solubility and dissolutionrate enhancement of nifedipine. Int J Pharm 299(1–2):167–177.19. Muller RH, Peters K. 1998. Nanosuspensions for the formulation ofpoorly soluble drugs: I. Preparation by a size-reduction technique. IntJ Pharm 160(2):229–237.20. Moschwitzer JP. 2012. Drug nanocrystals in the commercial phar-maceutical development process. Int J Pharm 453(1):142–156.21. Salazar J, Muller RH, Moschwitzer JP. 2014. Combinative particlesize reduction technologies for the production of drug nanocrystals. JPharm 2014:14.22. Weber U. 2010. The effect of grinding media performance on millinga water-based color pigment. Chem Eng Technol 33(9):1456–1463.23. Singh SK, Srinivasan KK, Gowthamarajan K, Singare DS, PrakashD, Gaikwad NB. 2011. Investigation of preparation parameters ofnanosuspension by top-down media milling to improve the dissolutionof poorly water-soluble glyburide. Eur J Pharm Biopharm 78(3):441–446.24. Junghanns JU, Muller RH. 2008. Nanocrystal technology, drug de-livery and clinical applications. Int J Nanomed 3(3):295–309.25. Krause KP, Muller RH. 2001. Production and characterisation ofhighly concentrated nanosuspensions by high pressure homogenisa-tion. Int J Pharm 214(1–2):21–24.26. Innings F, Tragardh C. 2007. Analysis of the flow field in a high-pressure homogenizer. Exp Ther Fluid Sci 32(2):345–354.27. Keck CM, Muller RH. 2006. Drug nanocrystals of poorly solubledrugs produced by high pressure homogenisation. Eur J Pharm Bio-pharm 62(1):3–16.28. Bevilacqua A, Costa C, Corbo MR, Sinigaglia M. 2009. Effects of thehigh pressure of homogenization on some spoiling micro-organisms,representative of fruit juice microflora, inoculated in saline solution.Lett Appl Microbiol 48(2):261–267.29. Moschwitzer J, Muller RH. 2006. New method for the effective pro-duction of ultrafine drug nanocrystals. J Nanosci Nanotechnol 6(9–10):3145–3153.30. Sucker Heinz LM. 1987. Pharmaceutical colloidal hydrosols for in-jection. A61K 09/10 ed., United Kingdom: Sandoz.31. Auweter H, Andre V, Horn D, Luddecke E. 1998. The function ofgelatin in controlled precopitation processes of nanosize particles. JDispersion Sci Technol 19(2–3):163–184.32. Van Eerdenbrugh B, Alonzo DE, Taylor LS. 2011. Influence of parti-cle size on the ultraviolet spectrum of particulate-containing solutions:
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694

REVIEW 17
Implications for in-situ concentration monitoring using UV/Vis fiber-optic probes. Pharm Res 28(7):1643–1652.33. Lindfors L, Forssen S, Skantze P, Skantze U, Zackrisson A, OlssonU. 2006. Amorphous drug nanosuspensions. 2. Experimental determi-nation of bulk monomer concentrations. Langmuir 22(3):911–916.34. Rezaei Mokarram A, Kebriaee Zadeh A, Keshavarz M, Ahmadi A,Mohtat B. 2010. Preparation and in-vitro evaluation of indomethacinnanoparticles. Daru 18(3):185–192.35. Sarnes A, Ostergaard J, Jensen SS, Aaltonen J, Rantanen J, Hir-vonen J, Peltonen L. 2013. Dissolution study of nanocrystal powders ofa poorly soluble drug by UV imaging and channel flow methods. Eur JPharm Sci 50(3–4):511–519.36. Gao L, Zhang D, Chen M, Zheng T, Wang S. 2007. Preparationand characterization of an oridonin nanosuspension for solubility anddissolution velocity enhancement. Drug Dev Ind Pharm 33(12):1332–1339.37. Detroja C, Chavhan S, Sawant K. 2011. Enhanced antihyperten-sive activity of candesartan cilexetil nanosuspension: Formulation,characterization and pharmacodynamic study. Sci Pharm 79(3):635–651.38. Liu G, Zhang D, Jiao Y, Guo H, Zheng D, Jia L, Duan C, Liu Y, TianX, Shen J, Li C, Zhang Q, Lou H. 2013. In vitro and in vivo evaluation ofriccardin D nanosuspensions with different particle size. Colloids SurfsB Biointerfaces 102:620–626.39. Pandya VM, Patel JK, Patel DJ. 2011. Formulation, optimizationand characterization of simvastatin nanosuspension prepared by nano-precipitation technique. Der Pharmacia Lettre 3(2):129–140.40. Zuo B, Sun Y, Li H, Liu X, Zhai Y, Sun J, He Z. 2013. Preparationand in vitro/in vivo evaluation of fenofibrate nanocrystals. Int J Pharm455(1–2):267–275.41. Arunkumar N, Deecaraman M, Rani C, Mohanraj KP, Venkatesku-mar K. 2010. Formulation development and in vitro evaluation ofnanosuspensions loaded with Atorvastatin calcium. Asian J Pharm4(1):28–33.42. Raval AJ, Patel MM. 2011. Preparation and characterizationof nanoparticles for solubility and dissolution rate enhancement ofmeloxicam. Intl Res J Pharm 1(2):42–49.43. Mitri K, Shegokar R, Gohla S, Anselmi C, Muller RH. 2011. Luteinnanocrystals as antioxidant formulation for oral and dermal delivery.Int J Pharm 420(1):141–146.44. Gao L, Liu G, Wang X, Liu F, Xu Y, Ma J. 2011. Preparation ofa chemically stable quercetin formulation using nanosuspension tech-nology. Int J Pharm 404(1–2):231–237.45. Juenemann D, Jantratid E, Wagner C, Reppas C, Vertzoni M, Dress-man JB. 2011. Biorelevant in vitro dissolution testing of products con-taining micronized or nanosized fenofibrate with a view to predictingplasma profiles. Eur J Pharm Biopharm 77(2):257–264.46. Bevan CD, Lloyd RS. 2000. A high-throughput screening method forthe determination of aqueous drug solubility using laser nephelometryin microtiter plates. Anal Chem 72(8):1781–1787.47. Lindfors L, Forssen S, Westergren J, Olsson U. 2008. Nucleationand crystal growth in supersaturated solutions of a model drug. J Col-loid Interface Sci 325(2):404–413.48. Anhalt K, Geissler S, Harms M, Weigandt M, Fricker G. 2012.Development of a new method to assess nanocrystal dissolution basedon light scattering. Pharm Res 29(10):2887–2901.49. Rosenblatt KM, Douroumis D, Bunjes H. 2007. Drug release fromdifferently structured monoolein/poloxamer nanodispersions studiedwith differential pulse polarography and ultrafiltration at low pres-sure. J Pharm Sci 96(6):1564–1575.50. Mora L, Chumbimuni-Torres KY, Clawson C, Hernandez L, ZhangL, Wang J. 2009. Real-time electrochemical monitoring of drug releasefrom therapeutic nanoparticles. J Control Release 140(1):69–73.51. Murdande SB, Shah DA, Dave RH. 2015. Impact of nanosizingon solubility and dissolution rate of poorly soluble pharmaceuticals.J Pharm Sci 104(6):2094–2102.52. Sun J, Wang F, Sui Y, She Z, Zhai W, Wang C, Deng Y. 2012. Effectof particle size on solubility, dissolution rate, and oral bioavailability:
Evaluation using coenzyme Q10 as naked nanocrystals. Int J Nanomed7:5733–5744.53. Avgoustakis K, Beletsi A, Panagi Z, Klepetsanis P, Karydas AG,Ithakissios DS. 2002. PLGA-mPEG nanoparticles of cisplatin: In vitronanoparticle degradation, in vitro drug release and in vivo drug resi-dence in blood properties. J Control Release 79(1–3):123–135.54. Saarinen-Savolainen P, Jarvinen T, Taipale H, Urtti A. 1997.Method for evaluating drug release from liposomes in sink conditions.Int J Pharm 159(1):27–33.55. Johnston MJ, Edwards K, Karlsson G, Cullis PR. 2008. Influenceof drug-to-lipid ratio on drug release properties and liposome integrityin liposomal doxorubicin formulations. J Liposome Res 18(2):145–157.56. Henriksen I, Sande SA, Smistad G, Agren T, Karlsen J. 1995. Invitro evaluation of drug release kinetics from liposomes by fractionaldialysis. Int J Pharm 119(2):231–238.57. Ammoury N, Fessi H, Devissaguet JP, Puisieux F, Benita S. 1990.In vitro release kinetic pattern of indomethacin from Poly(D, L-Lactide)nanocapsules. J Pharm Sci 79(9):763–767.58. Chidambaram N, Burgess DJ. 1999. A novel in vitro release methodfor submicron-sized dispersed systems. AAPS PharmSci 1(3):32–40.59. Muthu MS, Singh S. 2009. Poly (D, L-lactide) nanosuspensions ofrisperidone for parenteral delivery: Formulation and in-vitro evalua-tion. Curr Drug Deliv 6(1):62–68.60. Frank KJ, Westedt U, Rosenblatt KM, Holig P, Rosenberg J,Magerlein M, Brandl M, Fricker G. 2012. Impact of FaSSIF on thesolubility and dissolution-/permeation rate of a poorly water-solublecompound. Eur J Pharm Sci 47(1):16–20.61. Moreno-Bautista G, Tam KC. 2011. Evaluation of dialysis mem-brane process for quantifying the in vitro drug-release from colloidaldrug carriers. Colloids Surf A 389(1–3):299–303.62. Zambito Y, Pedreschi E, Di Colo G. 2012. Is dialysis a reliablemethod for studying drug release from nanoparticulate systems?—Acase study. Int J Pharm 434(1–2):28–34.63. Kataoka M, Itsubata S, Masaoka Y, Sakuma S, Yamashita S. 2011.In vitro dissolution/permeation system to predict the oral absorption ofpoorly water-soluble drugs: Effect of food and dose strength on it. BiolPharm Bull 34(3):401–407.64. Shahbaziniaz M, Foroutan SM, Bolourchian N. 2013. Dissolutionrate enhancement of clarithromycin using ternary ground mixtures:Nanocrystal formation. Iran J Pharm Res 12(4):587–598.65. Brown CK, Friedel HD, Barker AR, Buhse LF, Keitel S, CecilTL, Kraemer J, Morris JM, Reppas C, Stickelmeyer MP, Yomota C,Shah VP. 2011. FIP/AAPS Joint Workshop Report: Dissolution/in vitrorelease testing of novel/special dosage forms. Indian J Pharm Sci73(3):338–353.66. Badawi AA, El-Nabarawi MA, El-Setouhy DA, Alsammit SA. 2011.Formulation and stability testing of itraconazole crystalline nanopar-ticles. AAPS PharmSciTech 12(3):811–820.67. Song J, Wang Y, Song Y, Chan H, Bi C, Yang X, Yan R, ZhengY. 2014. Development and characterisation of ursolic acid nanocrys-tals without stabilizer having improved dissolution rate and in vitroanticancer activity. AAPS PharmSciTech 15(1):11–19.68. Neisingh SE, Sam AP, de Nijs H. 1986. A dissolution method forhard and soft gelatin capsules containing testosterone undecanoate inoleic acid. Drug Dev Ind Pharm 12(5):651–663.69. Nicklasson M, Orbe A, Lindberg J, Borga B, Magnusson AB, NilssonG, Ahlgren R, Jacobsen L. 1991. A collaborative study of the in vitrodissolution of phenacetin crystals comparing the flow through methodwith the USP Paddle method. Int J Pharm 69(3):255–264.70. Heng D, Cutler DJ, Chan HK, Yun J, Raper JA. 2008. What is a suit-able dissolution method for drug nanoparticles? Pharm Res 25(7):1696–1701.71. Langenbucher F, Benz D, Kurth W, Moller H, Otz M. 1989. Stan-dardized flow-cell method as an alternative to existing pharmacopoeialdissolution testing. Pharm Ind 51:1276–1281.72. Kayaert P, Li B, Jimidar I, Rombaut P, Ahssini F, Van den MooterG. 2010. Solution calorimetry as an alternative approach for dissolutiontesting of nanosuspensions. Eur J Pharm Biopharm 76(3):507–513.
DOI 10.1002/jps.24694 Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES

18 REVIEW
73. Conti S, Gaisford S, Buckton G, Conte U. 2006. Solution calorimetryto monitor swelling and dissolution of polymers and polymer blends.Thermochim Acta 450(1–2):56–60.74. Shah KB, Patel PG, Khairuzzaman A, Bellantone RA. 2014. Animproved method for the characterization of supersaturation and pre-cipitation of poorly soluble drugs using pulsatile microdialysis (PMD).Int J Pharm 468(1–2):64–74.75. Bellantone RA. 2012. Method for use of microdialysis. PatentUS8333107. G01N 15/08.76. Liu P, De Wulf O, Laru J, Heikkila T, van Veen B, Kiesvaara J, Hir-vonen J, Peltonen L, Laaksonen T. 2013. Dissolution studies of poorlysoluble drug nanosuspensions in non-sink conditions. AAPS Pharm-SciTech 14(2):748–756.77. Hu J, Johnston KP, Williams RO, 3rd. 2004. Nanoparticle engi-neering processes for enhancing the dissolution rates of poorly watersoluble drugs. Drug Dev Ind Pharm 30(3):233–245.78. Ponchel G, Montisci M-J, Dembri A, Durrer C, Duchene D. 1997.Mucoadhesion of colloidal particulate systems in the gastro-intestinaltract. Eur J Pharm Biopharm 44(1):25–31.79. Pedersen BL, Mullertz A, Brondsted H, Kristensen HG. 2000. Acomparison of the solubility of danazol in human and simulated gas-trointestinal fluids. Pharm Res 17(7):891–894.80. Ige PP, Baria RK, Gattani SG. 2013. Fabrication of fenofibratenanocrystals by probe sonication method for enhancement of dissolu-tion rate and oral bioavailability. Colloids Surf B Biointerfaces 108:366–373.81. Xu Y, Liu X, Lian R, Zheng S, Yin Z, Lu Y, Wu W. 2012. Enhanceddissolution and oral bioavailability of aripiprazole nanosuspensionsprepared by nanoprecipitation/homogenization based on acid-base neu-tralization. Int J Pharm 438(1–2):287–295.82. Xia D, Quan P, Piao H, Sun S, Yin Y, Cui F. 2010. Prepara-tion of stable nitrendipine nanosuspensions using the precipitation-ultrasonication method for enhancement of dissolution and oralbioavailability. Eur J Pharm Sci 40(4):325–334.83. Liversidge GG, Conzentino P. 1995. Drug particle size reduction fordecreasing gastric irritancy and enhancing absorption of naproxen inrats. Int J Pharm 125(2):309–313.84. Zhang J, Huang Y, Liu D, Gao Y, Qian S. 2013. Preparation ofapigenin nanocrystals using supercritical antisolvent process for disso-lution and bioavailability enhancement. Eur J Pharm Sci 48(4–5):740–747.85. Gao Y, Qian S, Zhang J. 2010. Physicochemical and pharmacoki-netic characterization of a spray-dried cefpodoxime proxetil nanosus-pension. Chem Pharm Bull 58(7):912–917.86. Zhang J, Lv H, Jiang K, Gao Y. 2011. Enhanced bioavailabilityafter oral and pulmonary administration of baicalein nanocrystal. IntJ Pharm 420(1):180–188.
87. Jiang T, Han N, Zhao B, Xie Y, Wang S. 2012. Enhanced disso-lution rate and oral bioavailability of simvastatin nanocrystal pre-pared by sonoprecipitation. Drug Dev Ind Pharmacy 38(10):1230–1239.88. Yin SX, Franchini M, Chen J, Hsieh A, Jen S, Lee T, Hussain M,Smith R. 2005. Bioavailability enhancement of a COX-2 inhibitor, BMS-347070, from a nanocrystalline dispersion prepared by spray-drying. JPharm Sci 94(7):1598–1607.89. Prajapati HN, Dalrymple DM, Serajuddin AT. 2012. A comparativeevaluation of mono-, di- and triglyceride of medium chain fatty acidsby lipid/surfactant/water phase diagram, solubility determination anddispersion testing for application in pharmaceutical dosage form devel-opment. Pharm Res 29(1):285–305.90. Quinn K, Gullapalli RP, Merisko-Liversidge E, Goldbach E, WongA, Liversidge GG, Hoffman W, Sauer JM, Bullock J, Tonn G. 2012. Aformulation strategy for gamma secretase inhibitor ELND006, a BCSclass II compound: Development of a nanosuspension formulation withimproved oral bioavailability and reduced food effects in dogs. J PharmSci 101(4):1462–1474.91. Jinno J, Kamada N, Miyake M, Yamada K, Mukai T, Odomi M,Toguchi H, Liversidge GG, Higaki K, Kimura T. 2006. Effect of particlesize reduction on dissolution and oral absorption of a poorly water-soluble drug, cilostazol, in beagle dogs. J Control Release 111(1–2):56–64.92. Thombre AG, Caldwell WB, Friesen DT, McCray SB, SuttonSC. 2012. Solid nanocrystalline dispersions of ziprasidone with en-hanced bioavailability in the fasted state. Mol Pharm 9(12):3526–3534.93. Lentz KA. 2008. Current methods for predicting human food effect.AAPS journal 10(2):282–288.94. Rao GC, Kumar MS, Mathivanan N, Rao ME. 2004. Nanosuspen-sions as the most promising approach in nanoparticulate drug deliverysystems. Pharmazie 59(1):5–9.95. Ghosh I, Bose S, Vippagunta R, Harmon F. 2011. Nanosuspensionfor improving the bioavailability of a poorly soluble drug and screeningof stabilizing agents to inhibit crystal growth. Int J Pharm 409(1–2):260–268.96. Dong Y, Ng WK, Shen S, Kim S, Tan RB. 2009. Preparation andcharacterization of spironolactone nanoparticles by antisolvent precip-itation. Int J Pharm 375(1–2):84–88.97. Sun W, Mao S, Shi Y, Li LC, Fang L. 2011. Nanonization of itra-conazole by high pressure homogenization: Stabilizer optimization andeffect of particle size on oral absorption. J Pharm Sci 100(8):3365–3373.98. Xia D, Cui F, Piao H, Cun D, Jiang Y, Ouyang M, Quan P. 2010.Effect of crystal size on the in vitro dissolution and oral absorption ofnitrendipine in rats. Pharm Res 27(9):1965–1976.
Shah, Murdande, and Dave, JOURNAL OF PHARMACEUTICAL SCIENCES DOI 10.1002/jps.24694