A postmortem study of focal adenitis in salivary and lacrimal glands
-
Upload
margaretha -
Category
Documents
-
view
213 -
download
1
Transcript of A postmortem study of focal adenitis in salivary and lacrimal glands

Journal of Autoimmunity (1989) 2,553-558
A Postmortem Study of Focal Adenitis in Salivary and Lacrimal Glands
Margaretha Segkrberg-Konttinen
Fourth Department of Medicine, Helsinki University Central Hospital, Helsinki, Finland
Investigations were carried out on 102 consecutive medicolegal post- mortem subjects to identify signs of focal adenltis in labial, submandibu- lar, and lacrimal glands. There were 19 subjects (18.6744) with focus scores exceeding 1 in one or two of the types of glands. Among the 19, five had had a disease which is generally associated with Sjagren’s syndrome or is autoimmune in nature. In another 63 subjects occasional lymphocytic foci were found in one, two, or all three types of gland. Fibrosis, atrophy, and fatty change had occurred most often in the labial sallvary glands in those over 50 years of age with or without high focus scores. Fibrosis, atrophy, and fat infiltration had hardly ever occurred in the lacrimal glands, although this is the type of gland in which high focus scores occur most often. The results suggest that there may be a common autoimmune basis for Sjiigren’s syndrome and other diseases, the mechanisms of which are still incompletely understood. A focus score exceeding 1 may be an lndi- cator of Sjbgren’s syndrome, but the diagnosis should not be established on the biopsy findings alone.
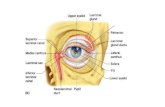
Introduction
The diagnosis of Sjogren’s syndrome (SS) is based on the clinical picture, laboratory findings, and biopsy specimens of the salivary glands. Among the salivary glands, the small labial glands are the first choice, for technical reasons and for the patient’s own comfort, though histologic changes typical for SS have also been noted in the major salivary glands; it has been suggested [l] that the histopathologic findings of the submandibular salivary gland is the most sensitive indicator of SS.
Slight, diffuse mononuclear cell infiltration with occasional lymphocytic foci is common in salivary and lacrimal glands in various disorders. More extensive infil- tration seems to occur above all in patients with SS, and the labial salivary gland
Correspondence to: Margaretha Segerberg-Konttinen, MD, 4th Department of Medicine, Unioninkatu 38,00170 Helsinki, Finland.
553
0896-8411/89/040553+06$03.00/0 0 1989 Academic Press Limited

554 M. Seaerbera-Konttinen
biopsy appears to be a more specific and more sensitive diagnostic test than other procedures, such as sialometry and sialography. In SS the labial salivary gland focus score should be at least 1 [2].
There are few extensive studies of the histology of minor and major salivary and lacrimal glands in patients with SS. There is no report on how often focus scores exceeding 1 occur in salivary and lacrimal glands in conditions other than SS. This question is included in the present study.
Materials and methods
Gross and microscopic examinations were carried out on submandibular, lacrimal, and labial salivary glands from 102 consecutive subjects undergoing medicolegal postmortem examination at the Department of Forensic Medicine of the University of Helsinki. The glands were fixed in 10% formalin, embedded in paraffin wax, sectioned using standard techniques and stained with hematoxylin and eosin.
Glands with pathological changes due to infection or neoplasm were not included. Gland lobules with duct dilatation caused by obstruction and gland tissue with extravascular polymorphonuclear leukocytes were discarded. Subjects with lym- phoma or leukemia, a recent history of immunosuppressive therapy, visible autolytic changes, hematomas or other recent damage to the face or neck were excluded.
Glands were accepted if they contained an adequate amount of representative gland tissue (2 cm’ for submandibular glands, 1 cm2 for lacrimal glands, and 8 mm2 for labial salivary glands corresponding to at least four labial salivary glands).
For every subject, sex, age, number of foci in labial, lacrimal, and submandibular glands, gland tissue damage, gland focus score, diseases and drugs mentioned in the autopsy request or revealed at the autopsy were recorded. Some of the subjects had died of accidents or suicides and showed no signs of disease.
A focus is defined as an aggregate of 50 or more inflammatory mononuclear cells, and the focus score is the number of foci in a 4-mm2 area of gland tissue [3,4].
Results
The subjects consisted of 58 males aged 17 to 92 years, and 44 females aged 20 to 96 years. Twenty of them (11 males aged 32 to 80 years and nine females aged 47 to 9 1 years) had no foci in the labial, lacrimal, or submandibular glands. In none were signs of autoimmune disease noted. In 63 cases slight mononuclear cell infiltrate was noted in one, two, or all three types of glands. One deceased in this group, a 73-year-old woman with focus scores under 1 in all types of gland had had rheumatoid arthritis with very slight articular deformation.
Focus scores exceeding 1 were noted in 19 cases-13 times in lacrimal glands, five in labial glands, and four in submandibular glands (Table 1). Among the 19, three had had insulin-dependent diabetes mellitus, one rheumatoid arthritis, one per- nicious anemia, and one obstruction of the bile ducts-a definite diagnosis of primary biliary cirrhosis could not be established in the latter case. Focus scores exceeding 1 in two types of gland were noted in one case of diabetes, and in the one case each of bile duct obstruction, and rheumatoid arthritis.

Focal adenitis in salivary and lacrimal glands 555
Table 1. Occurrence of focus scores exceeding 1 in various diseases
Focus score of gland
No. Sex Age Labial Lacrimal Submandibular Cause of death
1 2 3 4 5 6 7 8 9
10
11 12 13 14 15 16 17 18
19
F 55 M 50 F 64 F 92 M 58 F 83 F 85 M 17 F 86 M 19
F 81 M 57 M 81 M 92 F 60 F 74 M 34 F 96
M 34
- -
1.80 2.20 - - - -
2.80 -
5.00 -
2.20 -
1.30 2.00 1.40 2.20 -
2.00
- -
2.00 -
5.60
- 1.46 -
- 1.25 -
1.14 -
2.10 1.72 1.66
- 1.00
3.00 12.00
- - -
2.85 - - - - - - -
Cerebellar hemorrhage Epilepsia Diabetes mellitus Obstruction of bile ducts Rheumatoid arthritis Cerebral thrombosis Cardiac disease Addict of organic solvents Bone fracture Suicide. No history or
signs of illness Bone fracture Carotid obstruction Cardiac disease Bone fracture Diabetes mellitus Pernicious anemia Diabetes mellitus Cardiac disorder with
arterial hypertension Traffic accident. No history
or signs of illness
Degenerative changes of the labial salivary glands had occurred in 26 of the 50 cadavers over 50 years of age with focus scores under 1. In the same patient group,
fibrosis, atrophy, or fatty infiltration of the submandibular gland had occurred in nine cases; fatty infiltration in the lacrimal gland had occurred in one case (Table 2).
Among those with focus scores exceeding 1, fibrosis, atrophy, or fatty change had not occurred in the lacrimal glands, although this was the type of gland in which high focus scores were noted most frequently. High focus scores in the labial salivary glands were seen in five of the 14 patients over 50 years of age, and in the same group degenerative changes in the labial glands had occurred in eight cases (Table 3).
Discussion
The labial salivary gland biopsy is regarded as a very useful aid in the diagnosis of the
oral component of SS [2,3,5]. Focal sialadenitis has been regarded as the single most important criterion in the diagnosis of SS. It is included in the modern sets of diagnostic criteria for SS [6-91 and deserves close attention. In this study, as in earlier ones [lO-151, degenerative changes in the glands occurred more frequently with advancing age, but age alone does not explain the inflammatory changes noted in the glands. Ischemia, primary acinar atrophy [ 141 and repeated episodes of subclinical dacryoadenitis [ 161 have been suggested as etiological factors in keratoconjunctivitis

556 M. Segerberg-Konttinen
Table 2. Distribution and number of patients with focus scores under 1 in all glands. The table shows the prevalence of fibrosis, atrophy, and fatty
change in different decades
Fibrosis, atrophy, fat
Age No. Labial Lacrimal Submandibular
-20 21-30 31-40 41-50 51-60 61-70 71-80 81-
1- - - 4- - -
11 2 - 2 17 2 - 1 11 5 - 3 16 8 1 5 15 7 - -
8 6 - 1
Table 3. Distribution and number of patients withfocus scores exceeding 1 in at least one type of gland. The table shows the prevalence of fibrosis, atrophy, and fat, and the
prevalence of focus scores exceeding 1 in d$erent decades
Age
Fibrosis, atrophy, fat Focus scores exceeding 1
No. Labial Lacrimal Submandibular Labial Lacrimal Submandibular
-20 2 - 21-30 0 - 31-40 2 - 41-50 1 - 51-60 4 2 61-70 1 - 71-80 1 1 81- 8 5
- - - 2 - - - - - - - 1 - 2 -
- 1 - - 1 - 1 1 3 1 - - 1 1 - - - - 1 -
- 1 3 4 2
sicca. The present study revealed that the labial salivary glands appear to be more liable than the submandibular and lacrimal glands to fibrotic, atrophic, and fatty
change. In less than half the cases with labial gland changes inflammation of the glandular tissue was observed. This suggests that degenerative changes are not always associated with an inflammatory disorder, but may be a result of a transient inflammation.
In a postmortem study performed by Chisholm et al. [17], slight or moderate lymphocytic infiltration of the submandibular and salivary glands had occurred in persons with no known history of SS. The authors demonstrated a correlation between inflammation in the submandibular and labial salivary glands. Recently, Wise et al. compared parotid and minor salivary gland biopsy specimens from patients with suspected SS. They found that the parotid gland biopsy adds little in

Focal adenitis in salivary and lacrimal glands 557
the diagnosis but may aid in estimating the duration and severity of the disease [ 18). A
drawback with medicolegal postmortem investigations is that a clinical history is not
always available. Thus some of the cases studied may have had an autoimmune disorder with symptoms too slight or diffuse to awaken suspicions of the disease. Another drawback is the cost that would amount for elaborate scanning tests for diseases in cases in which the cause of death is obvious.
Recent studies have shown that SS is obviously associated with more immunologi- cal disorders and diseases than previously has been recognized [ 19,201. Sometimes a
different disease is revealed in a salivary gland biopsy obtained from a patient sus-
pected of having primary SS [21]. Diabetes and focal adenitis have been mentioned by other authors [ 1,121 but to the best of the author’s knowledge, no extensive study has been performed on the subject. It is established that autoimmune mechanisms play a major role in the pathogenesis of insulin-dependent diabetes mellitus, though
the precise origin and nature of these mechanisms are still obscure [22,23]. In the light of the occurrence of focal sialadenitis in diseases other than SS, these
conditions should be carefully excluded when diagnosing SS. This is also one of the
reasons why various diagnostic criteria are not based solely on the histopathologic demonstration of focal sialadenitis.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
References
Waterhouse, J. P. and I. Doniach. 1986. Post-mortem prevalence of focal lymphocytic adenitis of the submandibular salivary gland. 3. Path. Bact. 91: 53-64 Daniels, T. E. 1984. Labial salivary gland biopsy in Sjogren’s syndrome. Arthritis Rheum. 27: 147-156 Greenspan, J. S., T. E. Daniels, N. Talal, and R. A. Sylvester. 1974. The histopathology of Sjogren’s syndrome in labial salivary gland biopsies. Oral Surg. 37: 217-229 Chisholm, D. M. and D. K. Mason. 1968. Labial salivary gland biopsy in Sjogren’s disease. 3. Clin. Pathol. 21: 656-660 Tarpley, T. M. Jr., L. G. Anderson, and C. L. White. 1974. Minor salivary gland involve- ment in Sjogren’s syndrome. Oral Surg. 37: 64-74 Manthorpe, R., P. Oxholm , J. U. Prause, and M. Schiedt. 1986. The Copenhagen criteria for Sjogren’s syndrome. Stand. 3. Rheum. (suppl) 61: 19-2 1 Skopouli, F. N., A. A. Drosos, T. Papaioannou, and H. M. Moutsopoulos. 1986. Preliminary diagnostic criteria for Sjiigren’s syndrome. Stand. 3. Rheum. (suppl) 61: 22-25 Homma, M., T. Tojo, M. Akizuki, and H. Yamagata. 1986. Criteria for Sjogren’s syndrome in Japan. Scand.3. Rheum. (suppl) 61: 26-27 Fox, R. I., C. Robinson, J. Curd, P. Michelson, R. Bone, and F. V. Howell. 1986. First International Symposium on Sjiigren’s syndrome: suggested criteria for classification. Stand. 3. Rheum. (suppl) 61: 28-30 Waterhouse, J. P., D. M. Chisholm, R. B. Winter, R. B. Patel, and R. S. Yale. 1973. Replacement of functional parenchymal cells by fat and connective tissue in human sub- mandibular salivary glands: An age related change.3. Oral Puthol. 2: 16-27 Scott, J. 1977. A morphometric study of age changes in the histology of the ducts of human submandibular salivary glands. Arch. Oral Biol. 22: 243-249 Ettinger, R. L. 1981. Xerostomia-a complication of ageing. Austr’ulz’an Dent. 3. 26: 365-37 1 Syrjlnen, S. 1982. Salivary glands in rheumatoid arthritis. Thesis. Proc. Finn. Dent. Sot. 78 (suppl3): l-77 Murray, S. B., W. R. Lee, and J. Williamson. 1981. Ageing changes in the lacrimal gland: A histological study.3. Clin. Experimental Gerontol. 3: l-27

558 M. Segerberg-Konttinen
15.
16.
17.
18.
19.
20.
21.
22.
23.
Nasu, M., 0. Matsubara, and H. Yamamoto. 1984. Post-mortem prevalence of lympho- cytic infiltration of the lacrymal gland: a comparative study in autoimmune and non- autoimmune diseases. 3. Pathol. 143: 11-15 Damato, B. E., D. Allan, S. B. Murray, and W. R. Lee. 1984. Senile atrophy of the human lacrimal gland: the contribution of chronic inflammatory disease. Brit. 3. Ophthalmol. 68: 674-680 Chisholm D. M., J. P. Waterhouse, and D. K. Mason. 1970. Lymphocytic sialadenitis in the major and minor glands: a correlation in postmortem subjects. 3. Clin. Puthol. 23: 690-694 Wise, C. M., C. A. Agudelo, E. L. Semble, T. E. Stump, and R. D. Woodruff. 1988. Comparison of parotid and minor salivary gland biopsy specimens in the diagnosis of Sjogren’s syndrome. Arthritis Rheum. 31: 662-666 Drosos, A. A., A. P. Andonopoulos, J. S. Costopoulos, E. D. Stavropoulos, C. S. Papadimitriou, and H. M. Moutsopoulos. 1988. Sjogren’s syndrome in progressive systemic sclerosis. 3. Rheumatol. 15: 965-968 Coil, J., A. Rives, M. C. Grino, J. Setoain, J. Vivancos, and A. Balcells. 1987. Prevalence of Sjogren’s syndrome in autoimmune diseases. Ann. Rheum. Dis. 46: 286-289 Melson, R. D., P. M. Speight, J. Ryan, and J. D. Perry. 1988. Sarcoidosis in a patient presenting with clinical and histological features of primary Sjogren’s syndrome. Ann. Rheum. Dis. 47: 166-168 Bottazzo, J. F. 1985. Etiology of diabetes: the role of autoimmune mechanisms. Diabetes Annu. 1: 16-52 Eisenberth, G. S. 1986. Type I diabetes mellitus: a chronic autoimmune disease. N. Erzgl. 3. Med. 314: 1360-1368