A new absorbable collagen membrane to reduce adhesions in
Transcript of A new absorbable collagen membrane to reduce adhesions in
ARTICLE IN PRESS
www.icvts.org
doi:10.1510/icvts.2009.215251
Interactive CardioVascular and Thoracic Surgery 10 (2010) 213–216
� 2010 Published by European Association for Cardio-Thoracic Surgery
New
IdeasInstitutional
ReportW
orkin
ProgressReport
ESCVSArticle
NegativeResults
State-of-the-artBest
EvidenceTopic
BriefCom
munication
CaseReport
Follow-up
PaperEditorial
ProtocolProposalfor
Bail-out
ProcedureN
omenclature
HistoricalPages
Institutional report - Experimental
A new absorbable collagen membrane to reduce adhesionsin cardiac surgery�
Alain Bel *, Levon Kachatryan , Patrick Bruneval , Severine Peyrard , Christian Gagnieu ,a, a b c d
Jean-Noel Fabiani , Philippe Menaschee f
Assistance Publique-Hopitaux de Paris, Hopital Europeen Georges Pompidou, Department of Cardiovascular Surgery, Ecole de Chirurgie, Paris, Francea
Assistance Publique-Hopitaux de Paris, Hopital Europeen Georges Pompidou, Department of Pathology, Universite Paris Descartes,b
INSERM U 970 Paris, FranceAssistance Publique-Hopitaux de Paris, Hopital Europeen Georges Pompidou, Epidemiology and Clinical Research, Paris, Francec
Laboratoire des Biomateriaux, UPSP 2007.03.135 RTI2B «Reparation Tissulaire, Interactions Biologiques et Biomateriaux»,d
Institut des Sciences Pharmaceutiques et Biologiques (ISPB), Universite Claude Bernard Lyon I, Universite de Lyon, Lyon, FranceAssistance Publique-Hopitaux de Paris, Hopital Europeen Georges Pompidou, Department of Cardiovascular Surgery, Universite Paris Descartes, Paris, Francee
Assistance Publique-Hopitaux de Paris, Hopital Europeen Georges Pompidou, Department of Cardiovascular Surgery, Universite Paris Descartes,f
INSERM U 633, Laboratory of Biosurgical Research, Paris, France
Received 24 June 2009; received in revised form 5 October 2009; accepted 6 October 2009
Abstract
Reduction of sternal adhesions is still an issue in cardiac surgery. To evaluate a new fibrillar porcine collagen absorbable membrane(Cova� CARD), 16 sheep underwent a sternotomy followed by scratching of surface of the heart. They were then divided into three groups:pericardium left opened (ns4), placement of Seprafilm , the reference absorbable substitute (hyaluronic acid and carboxymethylcellulose,�
ns6) or of Cova� CARD membrane (ns6). Four months thereafter, the animals underwent repeat sternotomy and were macroscopicallyassessed for the degree of resorption of the material and the intensity of adhesions. Explanted hearts were blindly evaluated for themagnitude of the inflammatory response and fibrosis. The Cova� CARD membrane was almost totally absorbed by four months and replacedby a loosely adherent tissue. There was no inflammatory reaction and both the extent and density of fibrosis were minimal. The compositescore (median wmin;maxx) integrating tightness of adhesions and histological findings of inflammation and fibrosis was two-fold lower inthe Cova� CARD than in the Seprafilm group (2.0 w0;3.5x vs. 5.5 w3;7x, Ps0.01 by Wilcoxon test). The Cova� CARD membrane might�
represent an attractive pericardial substitute for preventing postoperative adhesions in cardiac surgery.� 2010 Published by European Association for Cardio-Thoracic Surgery. All rights reserved.
Keywords: Biocompatible materials; Reoperation; Surgical adhesions; Collagen membrane
1. Introduction
Despite continuous improvements in preoperative imagingmodalities and surgical techniques, reoperations in cardiacsurgery remain challenging because injury to the heart,great vessels or bypass conduits can be life-threatening.Over the past decades, several pericardial substitutes havebeen developed that broadly fall into two categories: non-absorbable, exemplified by the e-polytetrafluoroethylene(ePTFE) membrane and absorbable. The latter are expect-ed to provide superior healing by guiding tissue regenera-tion as shown in visceral and periodontal surgeries w1x.However, they also raise technical challenges as they haveto combine mechanical strength, suturability and resorptiontime matching the kinetics of the natural healing process.The present study was designed to test a new collagen-
� This study was partially funded by Biom’up� (Lyon, France).*Corresponding author. Department of Cardiovascular Surgery, Hopital Euro-
peen Georges Pompidou, 20, rue Leblanc, 75908 Paris Cedex 15, France.Tel.: q33 1 56 09 36 22; fax: q33 1 56 09 32 61.
E-mail address: [email protected] (A. Bel).
based pericardial substitute (Cova� CARD, Biom’Up, Lyon,France).
2. Materials and methods
Sixteen pre-Alpes sheep, weighing ;60 kg, were used inthis study which was approved by our Institutional ReviewBoard and conducted in compliance with the EuropeanConvention on Animal Care.
2.1. Preparation of pericardial membranes
Cova� CARD is a CE marked patented membrane made ofpurified porcine type I collagen. Briefly, porcine tendonsare washed and incubated in an acid solution. Then, theswollen tendons are grounded and mechanically treated forthe collagen extraction. Purification of the collagen isperformed according to the classical steps of solubilisationand precipitation in acidic conditions with sodium chloride.A viral inactivation step, shown to inactivate viruses andbacteria is performed at the end of the purification processw2x. The collagen obtained is processed to yield an elastic,
Dow
nloaded from https://academ
ic.oup.com/icvts/article/10/2/213/644802 by guest on 24 D
ecember 2021
ARTICLE IN PRESS
214 A. Bel et al. / Interactive CardioVascular and Thoracic Surgery 10 (2010) 213–216
resorbable and suturable membrane and cross-linked withan oxidised polysaccharide. This cross-linking agent pro-vides reproducible and biocompatible medical devices witha controlled resorption time w3x without cellular toxicity.Under dry shape, the membrane has a thickness of approx-imately 100 mm.
2.2. Surgical protocol
After isoflurane-based anaesthesia and endotracheal intu-bation, a median sternotomy was performed, the pericar-dium longitudinally opened and a 4-cm wide, 20 cm longstrip of pericardium removed. The epicardium was smoothlyscratched with a gauze to create local inflammation andthe sheep were then randomly allocated to one of thefollowing three groups. In four animals, the pericardialedges were not reapproximated, thus, leaving a centraldefect similar to what commonly occurs after cardiacoperations (Controls). In six sheep, the defect was closedby the epicardial application of a Seprafilm membrane�
(Genzyme, Cambridge, MA, USA) which currently repre-sents the most commonly used pericardial substitute. In sixother animals, the defect was closed with the Cova� CARDmembrane which was anchored to the pericardial edges bya few 4y0 polypropylene sutures. The chest was then closedconventionally with steel wires.
Four months later, the animals underwent a repeat ster-notomy under a similar anaesthesia protocol. The surgeon,blinded to the treatment group, graded adhesion formationaccording to the score defined by Heydorn et al. w4x: grade0: no adhesions; grade 1: light adhesions easily lysed bydigital dissection; grade 2: stronger adhesions; and grade3: dense adhesions requiring sharp dissection. One scorewas established for each animal. The sheep were theneuthanized with an overdose of IV Dolethal. An in-blockfragment was obtained of the anterior surface of the heartand formed, from the inside to the outside, by the rightventricular wall, the adhesion tissue and sometimes bonefragments. Specimens were fixed in 10% formaldehyde,embedded in paraffin and sectioned into 5 mm slices whichwere stained with hematoxylin-eosin (H&E) and Masson’strichrome to assess the inflammatory reaction and checkfor remnants of the pericardial substitute in the twotreated groups.
2.3. Light microscopic examination
Sections were examined using a 5= magnification objec-tive lens by a pathologist blinded to the treatment group.The severity of the inflammatory reaction was based onthe quantification of inflammatory cells (i.e. neutrophils,plasma cells, lymphocytes) and inflammatory foci and clas-sified from 0 to 3, using an inflammatory reaction scorederived from the one described by Lu et al. w5x: grade0sno cell infiltration; 1ssparse inflammatory cell infiltra-tion; 2sfocal inflammatory cell infiltration; 3sdiffuseinflammatory cell infiltration. Fibrosis was assessed withregard to its extent (0slimited; 1sgreat), density(0sloose; 1sdense) and thickness (0sthin; 1sthick). Acomposite end-point was then created for each heart bysumming the gross adhesion score (from 0 to 3) and the
histological indices (inflammatory reaction score: from 0to 3, and fibrosis score: from 0 to 3).
2.4. Statistical analysis
Percentages were compared by the Fisher’s exact testand a Wilcoxon test was used for comparing scores. Statis-tical significance was set at the 0.05 level without adjust-ment for P-values.
3. Results
3.1. Macroscopic findings
At four months, the Cova� CARD sheets were almostcompletely absorbed and replaced by a loose regeneratedtissue allowing the surgeon to find a smooth cleavage plane.In most cases, adhesions were split by blunt dissection. Thesurface of the heart was smooth and the coronary vesselswere clearly identifiable. At the opposite, the Seprafilm�
membrane was consistently absorbed and associated withtight adherences to the sternum and the rest of thepericardium requiring sharp dissection. The control groupanimals split between no or moderate adhesions.
3.2. Pathology findings
The Cova� CARD group sheep never demonstrated aninflammatory reaction, in contrast to one sham-operatedsheep and two sheep of the Seprafilm group.�
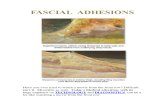
In keeping with these data, the extent and density offibrosis were minimal in the Cova� CARD group, and itsthickness was moderate. The Seprafilm group had the�
worst results for these three criteria, with a wide andharsh fibrosis of moderate thickness (Fig. 1). There werealso some foci of neovascularization and of calcifications.In the two control sheep that experienced adhesions, thefibrosis was of limited extent, density and thickness.
Adhesion and histological scores are summarized in theTable 1.
4. Discussion
Complete closure of the pericardium after cardiac surgery,although theoretically ideal, is not always possible orrecommended because of the risk of compression of bypassconduits or enlarged cardiac cavities. Furthermore, it doesnot prevent from tight pericardial adhesions. Local deliveryof drugs or biologics have been proposed to prevent adhe-sions w6–8x. The keratinocyte growth factor topicallyapplied experimentally w8x presumed to act through aresumption of the pericardial fibrinolytic function by mes-othelial cells. In a clinical setting, however, this approachwould probably not be so effective because the pericardiumhas to be left open most of the time at the end of theprocedure and drained. Indeed, most studies have ratherfocused on biologic or synthetic sheets designed as pericar-dial substitutes w9–13x, among which the ePTFE patch isthe most widely used. Unfortunately, it has a number ofsignificant disadvantages as it remains in situ as a perma-nent foreign body: it may form a fibrous capsule that maynegatively interfere with visualization of the cardiac archi-
Dow
nloaded from https://academ
ic.oup.com/icvts/article/10/2/213/644802 by guest on 24 D
ecember 2021
ARTICLE IN PRESS
215A. Bel et al. / Interactive CardioVascular and Thoracic Surgery 10 (2010) 213–216
New
IdeasInstitutional
ReportW
orkin
ProgressReport
ESCVSArticle
NegativeResults
State-of-the-artBest
EvidenceTopic
BriefCom
munication
CaseReport
Follow-up
PaperEditorial
ProtocolProposalfor
Bail-out
ProcedureN
omenclature
HistoricalPages
Fig. 1. (a) Histological section of the heart covered by a Cova� CARDmembrane sheet. On the left side the myocardium is normal. The epicardiumis mostly normal without any thickening or dense fibrosis. Note: light fibrosis(arrow). H&E stain, original =5. (b) Histological section of the heart coveredby a Seprafilm membrane sheet. On the left side the myocardium is normal.�
The epicardium is thickened by a dense and extensive fibrosis. H&E stain,original =5.
Table 1Comparison of macroscopic and histological data across groups
Controls Seprafilm� Cova� CARD Statisticsns4 ns6 ns6 P-valuesa
Macroscopic findingsComplete resorption, n (%) – 6y6 (100%) 3y6 (50%) –y–y0.18Adhesions, median wmin;maxx 0.75 w0;3x 3 w3;3x 1 w0;2x 0.03y0.91y0.01
Histological findingsInflammatory reaction, n (%) 1y4 (25%) 2y6 (33%) 0y6 (0%) 1.00y0.40y0.46Extent of fibrosis, n (%) 2y4 (50%) 5y6 (83%) 0y6 (0%) 0.50y0.13y0.02Density of fibrosis, n (%) 2y4 (50%) 4y6 (67%) 2y6 (33%) 1.00y1.00y0.57Thickness of fibrosis, n (%) 1y4 (25%) 3y6 (50%) 3y6 (50%) 0.57y0.57y1.00
Composite score, median wmin;maxxb 2.25 w0;6x 5.5 w3;7x 2 w0;3.5x 0.15y0.78y0.01
Seprafilm vs. ControlsyCova� CARD vs. ControlsySeprafilm vs. Cova� CARD.� �a
Composite scoreswadhesion score (from 0, absence to 3, tight)xqwinflammatory reaction score: from 0, absence to 3, diffusexqwfibrosis score: for eachb
component (extension, density and thickness) 1 if present, 0 if absentx.
tecture at the time of the reoperation w14x; it may causean inflammatory reaction w11x. Sakuma et al. w11x havereported that a bioabsorbable gelatin pericardial substitutegenerated less adhesions and inflammation compared with
an ePTFE sheet and was ultimately replaced with regener-ated tissue. However, a gelatin sheet has two substantialdisadvantages. First, due to the absence of structure ofthe gelatin, the sheet swells once wet, which leads to avery malleable, hard to handle material. Second for thesame reason, its tensile strength is not high enough tosteadily hold sutures to the native pericardium, hence, theproposal to lattice the sheet with polyglycolic acid toimprove its mechanical properties w13x.
In human cardiac surgery, two resorbable membranes arecurrently available: the Repel CV membrane (SyntheMed,�
Iselin, NJ, USA) made out of polylactic acid and Sepra-film , composed of carboxymethyl cellulose and hyal-�
uronic acid. The two main disadvantages of thesemembranes are their composition and lack of mechanicalresistance. In a 142-patient study, Repel CV has been�
shown effective in the prevention of pericardial adhesionsw10x but inflammatory reactions have been reported withpolylactic acid w15x. Seprafilm has been widely used in�
abdominal surgery and was more recently introduced forcardiac operations with encouraging results based onreduced tightness and extent of adhesions seen in reoper-ated patients compared with their untreated counterpartsw9x. Technically speaking, Seprafilm becomes a gel which�
sticks to organs preventing from repositioning or suturing.Furthermore, although carboxymethylcellulose and hyal-uronic acid are biocompatible, they do not have specificeffects on cell adhesion, wound healing and tissue remod-elling. Finally, resorption of carboxymethylcellulose doesnot involve naturally present endogenous enzymes (likecollagenases) but occurs by hydrolysis, which causes therelease of non-metabolized fragments.
To try overcoming these hurdles, the Cova� CARDmembrane, made out of purified porcine type I collagen,was tested in the present study. Collagen has an extensivesafety record in cardiovascular applications where it hasbeen mainly used as a topical adjunct to hemostasis or asa coating of vascular prostheses to make them blood-proof.A major advantage of collagen, particularly of porcineorigin, is that its resorption is a naturally occurring eventmediated by macrophage-released collagenases. Cleavageof the triple-helix structure leads to the liberation ofbiocompatible fragments which after denaturation and pro-teolysis are eliminated through kidney clearance without
Dow
nloaded from https://academ
ic.oup.com/icvts/article/10/2/213/644802 by guest on 24 D
ecember 2021
ARTICLE IN PRESS
216 A. Bel et al. / Interactive CardioVascular and Thoracic Surgery 10 (2010) 213–216
the induction of a pathological inflammatory reaction.In the particular setting of adhesion prevention, collagenhas the additional advantage of providing a substrate forcell adhesion and growth, thereby promoting wound heal-ing. Finally, shaping of the collagen is relatively easy andfilms, gel, foam or membranes can be produced to accom-modate the final indication.
The present results document the superiority of the Cova�CARD membrane under our experimental conditions. Duringimplantation, this membrane could be easily manipulated,repositioned if necessary and sutured. The dissection atreoperation was then the easiest in this group, with veryloose adhesions easily cleavable, except for one case.Expectedly, these macroscopic observations translated his-tologically into a loose and limited fibrosis and the lack ofinflammatory cell invasion, neovascularization and calcifi-cations, and the membrane could no longer (or hardly) beidentified. They sharply contrasted with the findings madein the Seprafilm group which featured a dense tissue,�
some foci of inflammatory cells around neovessels, or fociof calcifications. The thickness of the fibrosis was notedsimilar in the two treated groups, probably because of thepreset thickness of the Cova� CARD membrane (150 mmwhen wet). From a surgical point of view, the thickness ofthe healing tissue is not an issue, in contrast to the densityof fibrosis which may increase the difficulties and risks ofdissection.
4.1. Study limitations
We did not include a Repel CV treated group because of�
the limited clinical use of this product or a ePTFEmembrane-treated group as the study focused on absorb-able membranes expected to provide superior healing pat-terns through enhanced tissue regeneration and reducedinflammatory responses as well as avoidance of the risk ofinfection inherent in the introduction of durable foreignmaterials. A sheep model was used (sheep experiencingpostoperative adhesions as in humans) to eliminate thepossible biases associated with scale discrepancies inherentin rodent studies. Reoperation entailed a new sternotomy,which is more accurate than a lateral thoracotomy toinduce tight adhesions between the heart and the sternumbut we acknowledge that the tested material is designedto make dissection of adhesions easier and not to constitutea safety barrier for avoiding cardiac injury at the time ofre-entry into the chest cavity. A 4-month reoperation delaywas chosen to assess outcomes at the expected time ofmaximal inflammatory reactions and check for the biologi-cal membrane resorption. The characteristics of themembrane (thickness and reticulation) were chosen toachieve a full resorption by six months, although, in a ratmodel, the subcutaneously implanted Cova� CARD mem-
brane had completely disappeared by 13 weeks (unpub-lished observations). The absence of cardiopulmonarybypass may have minimized the extent of the whole-bodyinflammatory reaction and consequently reduced the mag-nitude of postoperative adhesions but this limitation appliesequally to all groups.
In conclusion, the present data support the effectivenessof the collagen-based Cova� CARD membrane in reducingpostoperative adhesions following sternotomy and maywarrant its clinical evaluation.
References
w1x Schwartzmann M. Use of collagen membranes for guided bone regen-eration: a review. Implant Dent 2000;9:63–66.
w2x Forest P, Morfin F, Bergeron E, Dore J, Bensa S, Wittmann C, Picot S,Renaud FN, Freney J, Gagnieu C. Validation of a viral and bacterialinactivation step during the extraction and purification process ofporcine collagen. Biomed Mater Eng 2007;17:199–208.
w3x Gagnieu CH, Forest PO. In vivo biodegradability and biocompatibility ofporcine type I atelocollagen newly crosslinked by oxidized glycogen.Biomed Mater Eng 2007;17:9–18.
w4x Heydorn WH, Daniel JS, Wade CE. A new look at pericardial substitutes.J Thorac Cardiovasc Surg 1987;94:291–296.
w5x Lu JH, Chang Y, Sung HW, Chiu YT, Yang PC, Hwang B. Heparinizationon pericardial substitutes can reduce adhesion and epicardial inflam-mation in the dog. J Thorac Cardiovasc Surg 1998;115:1111–1120.
w6x Zhou J, Liwski RS, Elson C, Lee TDG. Reduction in postsurgical adhesionformation after cardiac surgery in a rabbit model using N,O-carboxy-methyl chitosan to block cell adherence. J Thorac Cardiovasc Surg2008;135:777–783.
w7x Wiseman DM, Kamp L, Linsky CB, Jochen RF, Pang RH, Scholz PM.Fibrinolytic drugs prevent pericardial adhesions in the rabbit. J SurgRes 1992;53:362–368.
w8x Lopes JB, Dallan LA, Campana-Filho SP, Lisboa LA, Gutierrez PS, MoreiraLF, Oliveira SA, Stolf NA. Keratinocyte growth factor: a new mesothelialtargeted therapy to reduce postoperative pericardial adhesions. Eur JCardiothorac Surg 2009;35:313–318.
w9x Walther T, Rastan A, Dahmert I, Falk V, Jacobs S, Mohr FW, Kostelka M.A novel adhesion barrier facilitates reoperations in complex congenitalcardiac surgery. J Thorac Cardiovasc Surg 2005;129:359–363.
w10x Lodge AJ, Wells WJ, Backer CL, O’Brien JE Jr, Austin EH, Bacha EA, YehT Jr, DeCampli WM, Lavin PT, Weinstein S. A novel bioresorbable filmreduces postoperative adhesions after infant cardiac surgery. AnnThorac Surg 2008;86:614–621.
w11x Sakuma K, Iguchi A, Ikada Y, Tabayashi K. Closure of the pericardiumusing synthetic bioabsorbable polymers. Ann Thorac Surg 2005;80:1835–1840.
w12x Tsukihara H, Takamoto S, Kitahori K, Matsuda K, Murakami A, NovickRJ, Suematsu Y. Prevention of postoperative pericardial adhesions witha novel regenerative collagen sheet. Ann Thorac Surg 2006;81:650–657.
w13x Yoshioka I, Saiki Y, Sakuma K, Iguchi A, Moriya T, Ikada Y, Tabayashi K.Bioabsorbable gelatin sheets latticed with polyglycolic acid can elimi-nate pericardial adhesion. Ann Thorac Surg 2007;84:864–870.
w14x Ozeren M, Han U, Mavioglu I, Simsek E, Soyal MF, Guler G, Yucel E.Consequences of PTFE membrane used for prevention of re-entryinjuries in rheumatic valve disease. Cardiovasc Surg 2002;10:489–493.
w15x Dawes E, Rushton N. Response of macrophages to poly(L-lactide)particulates which have undergone various degrees of artificial degra-dation. Biomaterials 1997;18:1615–1623.
Dow
nloaded from https://academ
ic.oup.com/icvts/article/10/2/213/644802 by guest on 24 D
ecember 2021