A clinical comparative study of GP and TP 1st-line chemotherapies for advanced non-small cell lung...
Transcript of A clinical comparative study of GP and TP 1st-line chemotherapies for advanced non-small cell lung...
Chinese-German Journal of Clinical Oncology November 2010, Vol. 9, No. 11, P621–P624DOI 10.1007/s10330-010-0690-6
Since the 90s of last century, the 3rd generation che-motherapy pharmaceutics such as gemcitabine (GEM) and paclitaxel (PTX) so on, had been used widely and played a vital role in clinical treatment of non-small cell lung cancer (NSCLC). However, comparison studies of gemcitabine and paclitaxel used for lung cancer cure, domestically and abroad, produced inconsistent results [1–5]. To find a more reliable treatment regimen, we com-pared the efficacies and side effects of gemcitabine plus cisplatin (GP) and paclitaxel plus cisplatin (TP) used in NSCLC cases.
Materials and methods
General dataThere were 81 pathologically or cytologically diag-
nosed IIIb–IV NSCLC (non-pleural effusion IIIb) cases re-ceiving initial treatments. Average Karnofsky scale was ≥ 70, and estimated survival time was more than 3 months. There was no other serious illness requiring medical at-tention. Before chemotherapy, WBC ≥ 4.0 × 109 /L, PLT ≥ 100 × 109 /L, and HGB ≥ 100 g/L; liver function, kid-ney function and electrocardiogram were normal; chest CT should be carried out. Except for pregnant/lactating women and patients refusing signing informed consent, previous chemotherapy recipients and patients with su-perior vena cava syndrome, there were 47 cases of mid-grade IIIb and 34 cases of IV; 50 cases of males, and 31 cases of females. The age range was between 32 and 70, with median age of 61 years. There were 39 cases of squa-mous cell carcinoma, 35 cases of adenocarcinoma, 5 cases of adenosquamous carcinoma and 2 cases of large cell car-cinoma. Clinical data involved clinical stage, KPS score and so on, had no differences between two groups.
A clinical comparative study of GP and TP 1st-line chemotherapies for advanced non-small cell lung cancer*Kun Chen, Qiang Lin, Chunlin Chang, Yannan Zhao, Yue'e Liu, Na Wang, Huiling Su, Yuehua Huang
Department of Oncology, The Affiliated North China Petroleum Bureau General Hospital, Hebei Medical University, Renqiu 062552, China
Received: 27 August 2010 / Revised: 20 September 2010 / Accepted: 15 October 2010© Huazhong University of Science and Technology and Springer-Verlag Berlin Heidelberg 2010
Abstract Objective: The aim of the study was to evaluate the efficacies of initial gemcitabine plus cisplatin (GP) and paclitaxel plus cisplatin (TP) 1st-line chemotherapies for advanced non-small cell lung cancer (NSCLC) and observe their side effects. Methods: Eighty-one cases were randomly divided into two groups: GP group and TP group. In GP group, adminis-tered gemcitabine (GEM) 1000 mg/m2 on days 1 and 8; i.v. cisplatin (DDP) 30 mg/m2 from days 2 to 4 on a 28-day cycle. In TP group, administered paclitaxel (PTX) 175 mg/m2 on day 1, i.v. DDP 30 mg/m2 from days 2 to 4 on a 28-day cycle. Results: GP group had an overall response rate (ORR; CR+PR) of 45.0% (18/40). TP had an overall response rate of 43.2% (16/37). Short-term ORR had no significant difference between two groups (χ2 = 0.527, P = 0.957). GP had median survival time of 11 months and 37.7% of one-year survival rate, while TP showed 11 months of median survival time and 31.7% of one-year survival rate. Survival had no significant difference between two groups (χ2 = 0.140, P = 0.708). However, main side effects varied. Thrombocytopenia of GP group was significantly more than that of TP group, while peripheral neuritis, nausea/vomit-ing and myalgia of TP group were significantly more than those of GP group. Conclusion: Both GP and TP regimens had no significant difference in short-term treatment effect and survival rate for initial treatment of advanced NSCLC. However, side effects related to GP regimen treatment were slighter. Therefore, it was considered as the preferred initial first-line treatment for NSCLC.
Key words non-small cell lung cancer (NSCLC); gemcitabine (GEM); paclitaxel (PTX); cisplatin (DDP); chemotherapy
Correspondence to: Qiang Lin. Email: [email protected]* Supported by a grant of Science and Technology Department of Hebei Province (No. 072761711).
622 www. springerlink. com/content/1613-9089
TreatmentsAccording to random number table, patients were ran-
domly divided into two groups: 40 cases in gemcitabine plus cisplatin (GP) group and 41 cases in paclitaxel plus cisplatin (TP) group. Both groups had the same cisplatin (DDP) dose: i.v. with 30 mg/m2 on days 2 to 4, 1000 mg/m2 of gemcitabine (GEM) on days 1 and 8; 175 mg/m2 of paclitaxel (PTX) on day 1 for 3 hours. Both groups had an average 28-day cycle. Before chemotherapy, TP received routine prophylactic anti-allergy treatment. Both groups were given proper antiemetic, hydration and diuretic treatments (1500–2000 mL hydration). Blood RT, liver and kidney functions and ECG were rechecked pre-che-motherapy in each cycle. Blood RT was done at least once a week posterior chemotherapy.
Evaluation criteria of short term treatment efficacy and toxicity
The evaluation at two-week after chemotherapy used WHO criteria [6]. Complete response (CR) is the disap-pearance over 4 weeks of all clinical evidence of active tumor. Partial response (PR) is a 50% or greater decrease in the size of the primary lesion. Stable disease (SD) is a less than 50% decrease to a 25% increase in tumor mass, with no new lesions. Progressive disease (PD) is a more than 25% increase in tumor mass or an appearance of new lesions.
CR + PR was defined as response, while SD + PD was defined non-response. Overall response rate was defined as (CR + PR) / all cases.
Chemotherapy toxicity criteria was estimated by NCI
Common Toxicity Criteria-CTC 2.0 [7].
Subsequent treatmentDocetaxel 2nd-line chemotherapy treatment was given
to the cases with progressive illnesses underlying overall physical conditions.
Statistical analysis SPSS 13.0 biometrics was used for χ2 test or Fisher’s
Exact Test. Kaplan-Meier (KMSA) method was adopted to calculate the survival rate; Log-rank test was used for finding significant difference. P ≤ 0.05 showed that it had statistical significance.
Results
Treatment completion statusForty cases in GP had completed at least two or more
cycles of chemo-treatment, with an average of 4.4 cycles of chemo-treatment. In TP group, only 37 cases com-pleted two or more cycles of chemotherapy with an aver-age of 4.3 cycles. There was no statistical difference (P > 0.05) between completed chemotherapy cycles of the two groups. The reasons why four cases didn’t complete 2 cycles of chemotherapy lay in that two had allergic re-actions, 1 suffered peripheral neurotoxicity, and 1 suf-fered myalgia and joint pain. Toxicity was evaluated for all cases.
Short term response rateResponse rate evaluation was conducted for 77 cases
of patients who had completed chemotherapy for over two cycles. Overall response rates (ORR; CR + PR) of GP group and TP group were 45.0% (18/40) and 43.2% (16/37), respectively. Short-term response rate of GP group was slightly higher than that of TP, but it had no significance (χ2 = 0.527, P = 0.957; Table 1).
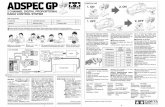
Survival timeGP group had median survival time of 11 months and
37.7% of one-year survival rate, and TP group had medi-an survival time of 11 months and 31.7% of one-year sur-vival rate. Survival had no significant difference between two groups (χ2 = 0.140, P = 0.708), as shown in Fig. 1.
Hematological toxicityThe incidence of hematological toxicity of the two
Table 1 Comparison of response rate in two groupsGroup Response rate (%) CR (%) PR (%) SD (%) PD (%) χ2 P
GP 45.0 2.5 42.5 25.0 30.0 0.527* 0.957TP 43.2 2.7 40.5 29.7 27.0*: Fisher’s exact test
Fig. 1 Comparison of survival in two groups
623Chinese-German J Clin Oncol, November 2010, Vol. 9, No. 11
groups was higher, but it wasn’t associated with fatality. Only severe thrombocytopenia (III/IV grade) had statisti-cal significance (Table 2).
Non-hematologic toxicityNausea and vomiting were most common reactions in
both treatments. Peripheral neuritis, nausea/vomiting, myalgia and hair follicles of TP group were significantly more serious than those of GP group, but all stayed at moderate I/II grade (Table 3).
Discussion
Gemcitabine (2-fluorinated cytidine, gemcitabine, GEM) was a new kind of cytosine nucleoside derivative, categorized as a cyclic antineoplastic pyrimidine antago-nistic agent. Once inside the human body, it would be ac-tivated by the deoxycytidine kinase to form gemcitabine phosphate, gemcitabine diphosphate and gemcitabine tri-phosphate. The latter two were active substances, partici-pating incorporating DNA synthesis and acting on G1/S phase to suppress the DNA synthesis processes. Also, it could inhibit the development of the ribonucleotide re-ductase to reduce intracellular metabolites. At the same time, it had self-synergy effect, and thus led to apoptosis of cancer cells [8]. As its unique anti-tumor mechanism, gemcitabine played an important role in treating pancre-atic cancer, lung cancer, breast cancer and ovarian can-cer. Applications of gemcitabine treatment for advanced non-small cell lung cancer had demonstrated good results [9, 10].
As a type of plant anti-cancer drugs, paclitaxel could make microtubules polymerize to form stable and inac-tive microtubule polymer, which influenced cell mitosis and resulted in apoptosis of cancer cells. As one of the third generation anti-cancer pharmaceutics, it was also very effective in treating some lung cancers. But it had strong side effects like allergic reaction, alopecie, nausea/
vomiting, etc. It had been a concerned topic in clinical tumor therapy field whether gemcitabine plus cisplatin or paclitaxel plus cisplatin was better for clinical tumor therapy.
In 2002, Schiller et al [1] published study results of ECOG1594. The study randomly divided NSCLC pa-tients into four groups which respectively received che-motherapies of paclitaxel plus cisplatin, paclitaxel and carboplatin, docetaxel plus cisplatin and gemcitabine plus cisplatin. The results showed that all four regimens dem-onstrated similar good treatment effects. Zhang et al [11]
reported that major toxicity of NP, DP and GP treating non-small cell lung cancer was myelosuppression and they achieved similar efficacies. Some studies suggested that short-term treatment effect of TP was better than that of GP, and its hematological toxicity was slighter. So TP could be favored as treatment for advanced NSCLC [5]. Whereas, others reported that GP had similar short-term effect as TP, but in TP group, the incidence of leukope-nia and gastrointestinal tract and peripheral neuritis was significantly higher than that of GP. Therefore, clinical application of GP would be safer [3].
We used domestically-produced gemcitabine plus cisplatin regimen for advanced NSCLC treatments and found that although GP introduced higher thrombocyto-penia than TP but without overt hemorrhage. After apply-ing interleukin-11 or similar supplementary medical at-tention, all cases safely overcame myelosuppression stage with no severe posterior consequences. GP also showed fewer incidences of peripheral neuritis, nausea/vomiting and myalgia than TP. It was significantly different from ECOG1594, which might be relative with various treat-ment regimens. In ECOG1594, gemcitabine dosage was administrated with 1000 mg/m2 on days 1, 8 and 15, 3 times in total; cisplatin dose was administrated in one in-fusion with 100 mg/m2 on day 1, which generated more serious side effects. The incidences of III/IV grade granu-locytopenia, thrombocytopenia, anemia, nausea/vomiting were 63%, 50%, 28% and 37% respectively. They were more than that our results. In our study, gemcitabine was reduced to two doses, administrated only on days 1 and 8 and cisplatin was separated into three dosages, which greatly decreased the hematological and gastrointestinal toxicities. Moreover, less hydration liquid dose was re-quired and there was less risk to the patient’s heart and kidney. Short-term treat efficacy reached 45%, median survival time was 11 months and one-year survival rate was 37.3%, which all were equal to that of ECOG1594. Therefore, this treat regimen was more suitable for Chi-nese patients with NSCLC.
To sum up, domestically-produced gemcitabine plus cisplatin (GP) provided better short-term medical effica-cy and survival time, and induced fewer side effects, and the GP regimen also had less impact on quality of life of
Table 2 Comparison of hematological toxicities in two groupsCase (%) χ2 PGP TP
Platelet 11 (27.5) 3 (7.3) 5.769 0.016Neutrophil 15 (37.5) 20 (48.8) 1.050 0.306Hemoglobin 3 (7.5) 3 (7.3) 0.001 0.975
Table 3 Comparison of non-hematological toxicities in two groupsCase (%) χ2 PGP TP
Nausea and vomitting (III/IV) 7 (17.5) 16 (39.0) 4.614 0.032Peripheral neuritis (I/II) 3 (7.5) 13 (31.7) 7.485 0.006Myosalgia (I/II) 4 (10.0) 24 (58.5) 9.350 0.002Alopecia (I/II) 10 (25.0) 22 (53.7) 7.500 0.006
624 www. springerlink. com/content/1613-9089
patients. It could be considered as the preferred choice of first line treatment for initial advanced NSCLC.
References
Schiller JH, Harrington D, Belani CP, et al. Comparison of four che-motherapy regimens for advanced non-small cell lung cancer. N Engl J Med, 2002, 346: 92–98.Scagliotti GV, De Marinis F, Rinaldi M, et al. Phase III randomized trial comparing three platinum-based doublets in advanced non-small-cell lung cancer. J Clin Oncol, 2002, 20: 4285–4291.Jiang T, Xiong HQ, Tang XK, et al. A clinical study on efficacy of gem-citabine and carboplatin versus paclitaxel and carboplatin in the treat-ment of advanced non-small cell lung cancer. Chin J Lung Cancer (Chinese), 2003, 6: 89–91.Zheng J, Bai H, Ye JZ, et al. The clinical observation of gemcitabine or paclitaxel combined with cisplatin in the treatment of advanced patients with non-small cell lung cancer. Chin Clin Oncol (Chinese), 2003, 8: 263–265.Zhou H, Tang M, Shi L. Comparison of paclitaxel plus cisplatin vs
1.
2.
3.
4.
5.
gemcitabine and cisplatin treatments for advanced non-small cell lung cancer. Guangdong Med J (Chinese), 2006, 27: 1389–1391.Sun Y, Zhou JC. Medical oncology. 4th edition. Beijing: Beijing Peo-ple’s Medical Publishing House, 2004. 106–107.Trotti A, Byhardt R, Stetz J, et al. Common toxicity criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys, 2000, 47: 13–47.Sun Y. Anticancer drugs. 1st edition. Beijing: Peking University Medial Press, 2006. 135–138.Cheng XM, Wang HM, Yu Y, et al. Combination of gemcitabine and carboplatin in the treatment of patients with non-small cell lung can-cer. Cancer Res Prev Treat (Chinese), 2006, 33: 442–443.Su W, Cao H, Wang Y. Gemcitabine plus cisplatin combination in treatment of elderly patients with advanced cancer. Cancer Res Prev Treat (Chinese), 2008, 35: 355–357.Zhang AQ, Guo GF. Advanced non-small cell lung cancer treatment with vinorelbine, docetaxel, gemcitabine combined with cisplatin, respectively: a report of 95 patients. Tumor (Chinese), 2002, 22: 152–153.
6.
7.
8.
9.
10.
11.