A case profile of sle
-
Upload
mohammed-sadiq-azam -
Category
Health & Medicine
-
view
669 -
download
2
Transcript of A case profile of sle

In the Name of God, Most Gracious, Most Merciful

- Dr. Mohammed Sadiq Azam
- Dr. N.SamathaPostgraduates M-I, Prof. Md. Siraj’s Unit
Department of Internal Medicine
Deccan College of Medical Sciences
A CASE PROFILE OF SLE

November 2006
CASE 1

HISTORY – CHIEF COMPLAINTS
• Mrs. A, 32/F, presented on 14/08/2006 with c/o:
• FEVER – 15 days (on/off since 6 months)
• Oral Ulcers – 15 days
• Loose stools – 15 days
• Generalized body pains – 15 days
• Generalised weakness – 15 days
• Generalised swelling – 15 days

HISTORY OF PRESENTING ILLNESS
• Asymptomatic 6 months ago, when she developed fever with chills and rigors for which she took symptomatic treatment – low grade fever +/- ever since.
• 1 month ago, she developed moderate to high grade fever with chills and rigor with generalized body pains involving all joints (non migratory, not flitting/fleeting, relieved by analgesics).
• Got admitted at a private nursing home on 4/5/2006 and has been treated for typhoid fever for one week with Inj. Cefotaxime 1g iv BD.
• No relief in symptoms even with therapy, hence got discharged and went home.
• One week later she developed swelling all over the body with oral ulcers and persistent low grade temperature with random spikes.

PAST HISTORY
• No past H/O exposure to an adult case of TB, no past documented H/s/o of typhoid, malaria, dengue, chickungunya, exanthematous fevers in past/childhood, no rheumatic history.
• No h/o rash anywhere on face or body, no h/o photosensitivity.
• No h/s/o high risk behaviour.
• No h/o exposure to heavy metals.

PERSONAL / FAMILY HISTORY
• Mixed diet, sleep decreased, loss of weight / loss of appetite +
• Bladder and bowel movementts – normal.
• Recently married (<1yr), no issues, no abortions.
• Menstrual history: Menarche: 14 yrs, cycles 5/28, regular, normal flow, no pain, no clots.
• Teacher by occupation at a private school. Illness has affected her school performance (increased sick absenteeism)
• ALLERGIC to Penicillin.
• Family History: No similar complaints in family.

ON EXAMINATION:
• Moderately built lady, sitting on the bed, is conscious, cooperative, coherent, oriented to time, place and person.
• Dyspnoeic, Tachypnoeic, Anaemic ++, BPPE ++, Facial puffiness +, Abdomen distended, no generalised LA, I -, Cy -, Cl -.
• Oral ulcers +, buccal mucosa 2 ulcers on each side, approx 1x2cm size, floor granular, egde sloping, no slough, sub mandibular tender LA +
• VITALS: BP-100/70mmHg, PR-95bpm, reg, normal vol & character,
Temp: 100 F, JVP: raised (8mm)
• CVS: S1, S2 +, no murmurs/added sounds
• RS: BAE+, NVBS, B/L basal creps + occasionally
• P/A: Abd distended, FF + (SD+, FT -), no palpable organomegaly.
• CNS: NFND, PERRLA+, B/L plantars flexor.

PROVISIONAL DIAGNOSIS
Pyrexia for evaluation:
• ? Koch’s
• ? Connective Tissue Disorder
• ? Malignancy

INVESTIGATIONS:
• CBP:
• Hb: 8.5g% , TC- 2,300 cells/cu.mm, DC – N79, L16, M3, E2, Platelet count- 1.09 lakh.
• Reticulocyte count: 2.5%, ESR- 35/40mm
• LFT – ALP, AST/ALT – Normal
• BU/SC – Normal (42/0.9)
• S.Albumin – 5g% 3.4g% (over 15 days)
• P/S: Pancytopaenia, BM aspiration: Hypercellular marrow, no abnormal/ immature cells in either.
• CxR PA: WNL, Mantoux: Negative
• S.Electrolytes: Na: 110, K: 3.9, Cl: 90, Urine Na:79 meq/l (20-80)

INVESTIGATIONS:
• CUE:
• Alb + 3 + (over 15 days)
• RBCs: NIL 5-6 (over 15 days)
• Pus cells 3-4 plenty (over 15 days)
• 24h urine protein: 1200mg/24 hrs
• Urine C/S : Sterile
• Blood for CRP: Positive
• Blood for RA Factor: Negative
• S.Uric acid: 4.5

INVESTIGATIONS:
• USG abdomen: Moderate ascites +, no organomegaly, no lymphadenopathy. Apparent mild thickening of rectal walls, bilateral mild pleural effusion.
• Ascitic fluid analysis:
• GM Stain: No organisms seen, AFB: Negative
• Protein: 1.7 mg/dl, Alb: 0.21mg/dl, Glucose: 91mg/dl
• ADA: 02 U/L, LDH: Normal
• Ascitic fluid cytology: only 2 cells – lymphocytes.
• HbsAg: Negative, HIV: Non Reactive

GOING BACK…
PROVISIONAL DIAGNOSIS
• Pyrexia for evaluation:
• ? Koch’s
• ? Connective Tissue Disease
• ? Malignancy

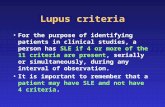
CRITERIA FOR SLE:
1. Malar Rash
2. Discoid Rash
3. Photosensitivity
4. Oral Ulcers
5. Arthritis
6. Serositis (Effusions/Ascites)
7. Renal disorder (Proteinuria >0.5g/d or >/= 3+ or cellular casts)
8. Neurologic disorder (Seizures, Psychosis with no other cause)
9. Haematologic disorder (Haemolytic anaemia or leucopaenia
(<4000/uL) or lymphopaenia or thrombocytopaenia (<100000/uL) in the absence of offending drugs)
10. Immunologic disorder (Anti dsDNA, anti-Sm, and/or anti-phospholipid Ab)
11. Antinuclear antibodies (ANA) positive

INVESTIGATIONS:
• ANA: POSITIVE
• Anti dsDNA: POSITIVE

FINAL DIAGNOSIS
Connective Tissue Disorder:
• Systemic Lupus Erythmatosus

TREATMENT:
• Started on Steroids, Oral Prednisolone 1mg/kg/day
• Supportive therapy

FOLLOW UP:
• Patient developed GTCS involving Right UL/LL 3 days after initiating therapy.
• CT Brain (Plain):
• Focal hypodensity in Rt. High parietal lobe posteriorly (?infarct). Suggested review with contrast after 1 week
• Review scan: Hypodensities in bilateral parieto-occipital regions s/o infarct.
• Wedge shaped hypodense areas of alterations valus (16-24 Hz) noted in posterior parietal regions bilaterally. s/o Infarct, ? White matter oedema.

FOLLOW UP:
• MRI Brain with MR Venogram:
• Bilateral cortical and subcortical T2 hyperintensity in parieto-occipital and frontal lodes which may represent mutiple infarcts (? secondary to vasculitis).

FOLLOW UP:
• Uptitrated the steroid
• Added LMWX, Sodium Valproate 300mg BD with Folic acid 1g OD
• Supportive therapy.
• Patient is on regular follow up.
• Conceived 6 months later, had a FTND, baby healthy, resumed job, has a healthy good QOL now.

August 2002
CASE 2

CASE SNIPPET
• Mrs. R, 48/F, presented in August 2002 with c/o fever on/off since
4 months, low grade, no chills/rigors. Since 2 weeks she had an
associated generalized swelling all over the body and joint pains
involving all the joints, no stiffness/no obvious deformity. On
admission and evaluation she was found to have pancytopaenia,
serositis and albuminuria. Workup revealed a positive ANA and
dsDNA. She was advised a renal biopsy but she refused.
• In view of clinical features and lab investigations she was
diagnosed as a case of connective tissue disease – SLE and
started on methylprednisolone 1mg/kg/day, supportive therapy
and discharged after stabilisation. She was advised regular
follow-up.

CASE SNIPPET
• 5 months later (January 2003), she presented with puffiness
of the face and decreased urine output. RFT revealed
oliguria (300ml/24h) with nephrotic range proteinuria
(4000mg/d) and elevated BU/SC (157/3.5mg/dl).
• Renal biopsy was done after obtaining an informed consent
of the patient and it was consistent with WHO Stage 4
Lupus Nephritis.
• She was started on pulse therapy with Cyclophosphamide,
uptitrated on methylprednisolone and managed with
supportive care.

CASE SNIPPET
• She started showing signs of clinical remission within one
week. (Urine output improved to 1060ml/d, 24h urine
protein – 200mg/d, BU/SC – 55/1.5mg/dl)
• 2 weeks after starting therapy, her RFTs stabilised to normal
range and she was discharged. Her pulse therapy was
continued and cyclophosphamide was gradually tapered off.
Steroid was tapered to minimum effective dose.
• She is currently on Tab.Methylprednisolone 5mg/day.
• 10 years since initial diagnosis, she is asymptomatic, CBP
and RFTs are stable and she has a healthy QOL.

December 2011
CASE 3

CASE SNIPPET
• Mrs. D, 25/F, was brought to the ER with c/o weakness of all four
limbs since 10 days. She had recently been diagnosed with SLE
at an outside centre. On admission, her power was 0/5 in both LL
and 2/5 in both UL with a sensory level at C5 spinal level. Her
Serum potassium was 1.6meq/l. She was tachypnoeic/ dyspnoeic
and showed signs of respiratory muscle weakness.
• A provisional diagnosis of SLE associated Transverse myelitis
(AIDP) vs. Hypokalemic paralysis was made.
• She was started on Injectable high dose steroid for the AIDP and
Inj. Potassium chloride 60meq/500ml NS to correct the potassium
deficit.

CASE SNIPPET
• 2 days after initiating therapy, her symptoms improved. Power in
UL was 4+/5 and in LL was 4/5. Her sensory deficit disappeared.
• MRI spine was done which was normal.
• Patient made a complete recovery and was discharged after 1
week.
• She is currently on follow up for identifying the cause of
hypokalemia and evaluating the D/D of AIDP sec to SLE vasculitis
vs. Hypokalemic periodic paralysis.

January 2012
CASE 4

Chief complaints
• Mrs Vijaya, 31 yrs female, a House wife,
Presented on 12/12/2011 with C/O
Fever : 2 months
Malar rash : 45 days
Headache : 45 days

History of present illness
Patient was apparently asymptomatic 2 months back when she
developed fever associated with generalised body pains, rash on
palms,back and arms, joint pains, anorexia, sleeplessness and
headache.
• Patient presented to a local hospital, treated symptomatically,
fever was relieved on medication and was discharged.
• 10-15 days later she developed malar rash,and persistent fever.
• Then, she presented to Esra hospital with fever and malar rash.

History of present illness
• Fever was intermittent, low grade, on and off, no chills/rigors,
associated joint pains mostly involving large joints[non migratory
and non fleeting]
• From day1 of fever, she developed macular erythema on palms,
upperback and extensor aspect of arms and 10-15 days later she
developed malar rash,which is slightly raised erythematous rash
on cheek and nose, precipitated by sun exposure and non
pruritic.
• No history S/O purpura, no orogenital eruptions or scaly lesions
on anyother part of the body.

History of present illness
• No past H/O exposure to C/O TB,mite bite,tick bite,or
exposure to rats or cats
• No history S/O malaria,chikungunya,dengue,typhoid
• No history of visual disturbances,altered sensorium & no
complaints S/O motor or sensory impairment
• No H/O cough or dyspnoea
• No history of drug allergy
• No H/O similar complaints in the past

Personal/family history
• Mixed diet,decreased appetite,decreased sleep
• Bowel and bladder habits regular
• Menstrual history-menarche at 13,cycles regular,4/30,no
dysmenorrhea,no clots
• No similar complaints in the family

General examination
• Patient is conscious, coherent, cooperative, comfortably sitting on bed,
well oriented to time, place & person
• Weight - 56kgs, Height - 158 cms
• Pallor +,no icterus no cyanosis,no clubbing,no lymphadenopathy,no pedal
edema
• Normal hair
• Malar rash on face ,macular erythema on palms and back,non-discoid,non
blanchable
• No orogenital ulcers
• EYES appear normal O/E
• URT normal,no congestion or secretions noted


Physical examination
• Vitals ,BP 110/80, PR 80b/m, regular, normal volume,character,
all peripheral pulses felt. Temp 100F , RR 16/min
• RS-BAE+,NVBS,no ADV sounds
• CVS-S1,S2 heard, no murmurs
• P/A-soft ,no tenderness,no organomegaly,BS+
• CNS-NFND,Plantars-flexor
• Muskuloskeletal system examination-no swelling or redness or
tenderness over large or small joints,no limitation of
movements at joints,no pain,no stiffness

Provisional diagnosis
Pyrexia for evaluation
? Connective tissue disorder
? Granulomatous disease
? Enteric fever
? Malignancy

Investigations
CBP - HGB:10.7gm%,WBC-1,700/cu.mm, plt-
89,000,N69,M5,L10,E2
PS - Normocytic normochromic,leucopenia,lymphopenia
CUE - Pus cells-0-1,no rbc,no cystals,no casts
LFT - Sr bilirubin-1.08,SGOT-134U/L,Sr albumin- 4.3gm/dl, ALP-WNL
RFT -NORMAL
Sr electrolytes - Sr Na-146/k-3.9/Cl-100
Chest xray - Normal
ESR -26/55mm

Investigations
VDRL- NR
Widal test- Negative
Dengue NS1 Ag &IgM, IgG -Negative
HBs Ag/Anti HAV/Anti HCV /Anti HEV- Negative
HIV - NR
USG ABD/Pelvis - Normal
ANA - POSITIVE(2.975)
Anti ds DNA Antibodies-positive(233IU/ml)

CRITERIA FOR SLE
1. MALAR RASH
2. Discoid Rash
3. PHOTOSENSITIVITY
4. Oral ulcers
5. Arthritis
6. Renal disorder
7. HEMATOLOGICAL DISORDER
8. Serositis
9. Neurological disorder
10. IMMUNOLOGICAL (Anti-Sm, and/or anti-phospholipid, Anti dsDNA)
11. ANTINUCLEAR ANTIBODIES-ANA POSITIVE

Diagnosis
SYSTEMIC LUPUS ERYTHEMATOSIS

Management Supportive therapy
Inj.Solumedrol 1g iv OD
At discharge, Tab.Azathioprine, added at 2mg/kg/day,
along with oral prednisolone, 40mg bid
At follow up, patient cell counts improved, rash faded
comparatively, but complained of alopecia,GI symptoms

Thank You