93493980 Degenerative Myopia
-
Upload
ferdinando-baeha -
Category
Documents
-
view
237 -
download
0
Transcript of 93493980 Degenerative Myopia
-
7/24/2019 93493980 Degenerative Myopia
1/49
Degenerative Myopia
Updated November 2007
Overview
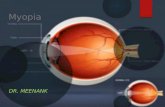
Myopia is a condition whereby images come into focus in front of the eye, resulting in a blurred
image on the retina. The more severe the nearsightedness, the farther the image is from the retina,which results in more blurry vision in the distance.
Myopia causes light rays to focus on the front of the retina. s a result, close ob!ects are seen
clearly, while distant ob!ects appear blurred. Near vision, however, can deteriorate to a level where
reading even close to the face can become difficult.
There are three ways for an eye to become myopic"
The front surface of the eye #the cornea$ is too curved and, therefore, too powerful.
The eyeball itself is too long.
combination of both of the above.
%n many cases, myopia will stabili&e when the growth process has been completed, and glasses canoffer normal vision. 'igher levels of myopia, however, tend to be hereditary, meaning that if there
is a moderately or highly nearsighted parent, the odds are higher for one of the children to be
myopic.
Myopia that develops in childhood is often called !uvenile onset myopia, which almost always
increases in severity with the progression into adulthood.
%n the more severe chronic cases #(degenerative( or (pathological( myopia$, there is the possibility
of sight loss. The deformation of the eye creates stress on the retina, which can become damagedor detached, and this can then provo)e additional changes. This is especially true in degenerative
myopia, which can lead to macula problems #not to be confused with age*related macular
degeneration$.
There are at least four other clinical types of myopia" simple, nocturnal, pseudo, and induced. +orthe purposes of this article, degenerative myopia is described here.
Degenerative Myopia
egenerative myopia is the seventh leading cause of legal blindness, occurring in about 2- of theU.. population. %t is most often seen in people of /hinese, apanese, Middle 1astern and ewish
descent. This condition can start at birth, but most often starts during the pre*teen years. %t is
believed to be hereditary.
egenerative myopia is more severe than other forms of myopia and is associated with retinachanges, potentially causing severe vision loss. %t progresses rapidly, and visual outcome depends
-
7/24/2019 93493980 Degenerative Myopia
2/49
largely on the etent of fundus and lenticular changes. The diagnosis of degenerative myopia is
accompanied by characteristic chorioretinal degenerations. 3athologic myopes, particularly those
with higher refractive errors, are at ris) for retinal detachment and macular changes.
3atients with degenerative myopia typically complain of decreased vision, headaches, and
sensitivity to light. %f retinal degeneration or detachment is present, patients may also report lightflashes and floaters, which are associated with retina changes. Those with degenerative myopia
have an increased incidence of cataract formation #nuclear cataracts are most typical$.
ome of the most typical features of degenerative myopia are"
4itreous li5uefaction and posterior vitreous detachment
3eripapillary atrophy appearing as temporal choroidal or scleral crescents or rings around
the optic disc
6attice degeneration in the peripheral retina
Tilting or malinsertion of the optic disc, usually associated with myopic conus
Thinning of the retinal pigment epithelium with resulting atrophic appearance of the fundus 1ctasia of the sclera posteriorly #posterior staphyloma$
rea)s in ruch8s membrane and choriocapillaris, resulting in lines across the fundus called
(lac5uer crac)s(
+uch8s spot in the macular area.
Myopic degeneration is similar to age*related macular degeneration M$ in that it causes loss of
central vision due to degeneration of the photoreceptor cells. This is caused by separation of the
retina as a result of abnormal elongation of the eyeball. This usually happens because the bac) ofthe eye is larger than normal when the eye is very nearsighted. Mar)ed thinning and stretching may
lead to brea) down of the macula, surrounding retina and it8s underlying tissue. This will cause a
varying amount of blurred vision.
1ven after the eyeball has fully grown #by adulthood$, wea)ness in the sclera #the white outershell$ can lead to development of a posterior staphyloma. This is a distention of the sclera at the
bac) of the globe where the optic disc and macula are located. rea)s in ruch8s membrane and
atrophy of the choroid layer of the retina #where the blood vessels are$ can create lesions )nown as
lac5uer crac)s. lood vessels may protrude through the crac)s and lea) into the subretinal spacebeneath the photoreceptor cells. 9nown as (choroidal neovasculari&ation,( this hemorrhaging can
lead to scarring, retinal separation, and profound sight loss in the central field. %f this occurs,
immediate treatment is needed, which may be in the form ofphotodynamic therapy, antiangiogenicdrug treatmentor both.
Treatment for Prevention of Degenerative Myopia
Two treatments are showing promise. :ne is scleral buc)ling, which can be read about in the
article, (egenerative Myopia" a ;eview of its Nature and its Treatment(,on this site. The other isearly systemic treatment with 7*methylanthine, which has been shown to normali&e the abnormal
growth pattern of myopic eyes in children aged .
http://www.mdsupport.org/library/photther.htmlhttp://www.mdsupport.org/library/anti-angio.htmlhttp://www.mdsupport.org/library/anti-angio.htmlhttp://www.mdsupport.org/library/degenmyopia.htmlhttp://www.mdsupport.org/library/degenmyopia.htmlhttp://www.mdsupport.org/library/anti-angio.htmlhttp://www.mdsupport.org/library/anti-angio.htmlhttp://www.mdsupport.org/library/degenmyopia.htmlhttp://www.mdsupport.org/library/photther.html -
7/24/2019 93493980 Degenerative Myopia
3/49
%n the abstract, (1ffect of 7*methylanthine on eye growth in myopic children( #:phthalmic and
3hysiological :ptics, 4ol. 2?, uppl. =, ugust 200?$, researchers 9laus Trier and oren Mun)
;ibel*Madsen reported that (aial growth in the 7*methylanthine group was reduced by 22- inthe low aial growth stratification layer and by
-
7/24/2019 93493980 Degenerative Myopia
4/49
91C +1TU;1
B 3rogressive global epansion with posterior staphyloma formation and secondary macular
degeneration.
:/%T1 +1TU;1
B 3remature cataract formation.
B 4itreous syneresis, rhegmatogenous retinal detachment, and glaucoma.
%NT;:U/T%:N
Myopia is a common optical aberration. 3hysiological myopia, by far the most prevalent, is lessthan *? in magnitude and is considered a normal biological variation. 1yes that have errors
greater than *? are said to have high myopia. The greater the myopia, the more li)ely are
complications that can threaten vision. subgroup of high myopes have aial lengths that fail tostabili&e during young adulthood. The pathophysiology of this progressive, degenerative form of
myopia is un)nown.
13%1M%:6:DC N 3T':D1N1%
Not all eyes that have myopia greater than *? progressE nor does every eye that has progressivemyopia develop degenerative complications. The worldwide distribution of those who have truly
degenerative myopia is un)nown, but the prevalence of progressive FpathologicalG myopia was
surveyed by +uchsH=I more than J0 years ago. mong =K countries in the study, progressive
myopia was found in 0.>- #1gypt$ to L.?- #pain$ of their populations. sians are )nown to havea high prevalence of myopia. That of progressive myopia in apan was
-
7/24/2019 93493980 Degenerative Myopia
5/49
dominant, but it also can appear sporadically. 3rogressive myopia occurs commonly in association
with
:cular Manifestations of egenerative Myopia
NT:M%/6 MN%+1TT%:N
/orneal astigmatism
eep anterior chamber
ngle iris processes
onular dehiscences
4itreous syneresis
6attice retinal degeneration
cleral epansion and thinning
ecreased ocular rigidity
-
7/24/2019 93493980 Degenerative Myopia
6/49
%ncreased aial length
3osterior staphyloma
Tilted disc
Temporal crescent or halo atrophy
Macular lac5uer crac)s
3igment epithelial thinning
/horoidal attenuation
+UN/T%:N6 MN%+1TT%:N
%mage minification
nisometropic amblyopia
ubnormal visual acuity
4isual field defects
-
7/24/2019 93493980 Degenerative Myopia
7/49
%mpaired dar) adaptation
bnormal color discrimination
uboptimal binocularity
MarfanOs, 1hlersAanlos, and tic)lerOs syndromes, and twin studies confirm its genetic basis.
The most widely accepted environmental influences are ecessive near wor) and increasing formaleducation. ustained accommodation and intraocular pressure #%:3$, both basal and phasic, are
suspected to influence aial elongation in eyes that have decreased scleral resistance,HJI HKI but
recent evidence 5uestions both of these hypotheses. Topical atropine slows the progression ofmyopia in children,H?I but this may be via a mechanism independent of accommodation. +urther, it
appears that at least some degree of active scleral growth and remodeling appears to be involved in
pathological myopia. This may be regulated by various local growth factors, independent of centralnervous system control. 1perimentally, ocular growth can be governed by the application of plus
or minus spectacles,H7I and children who have threshold retinopathy of prematurity develop less
myopia following peripheral retinal ablation.H- of eyes that
had aial lengths less than 2?.KPmm, in ==- that had
-
7/24/2019 93493980 Degenerative Myopia
8/49
L>K
+igure =2?*= 2.K0 right eye. , subretinal hemorrhage is present in the fovea. ,
small wishbone*shaped lac5uer crac) was observed => months later. /, t 27 months from theoriginal bleed, another such crac) was noted along a temporal etension of the growing lac5uer
crac) pattern. This was asymptomatic and the corrected acuity was 20Q?0 #?Q=>.KPmm, and in 2>.KPmm.etermination of glaucomatous changes are especially difficult in highly tilted optic discs, with
posterior staphyloma ad!acent to the myopic disc complicating the evaluation of visual field
defects. lso, pigmentary and normal*tension glaucoma occurs more fre5uently in myopes.
mong the other serious complications of progressive myopia are vitreous syneresis andrhegmatogenous retinal detachment that results from peripheral tears. uch detachments usually
are spontaneous, but they may occur after blunt ocular trauma or subse5uent to cataract surgery,
especially when complicated by capsular rupture and vitreous loss.
The abnormality seen in the myope that !ustifies use of the term degenerative is posteriorstaphyloma #ectasia$, with its devastating secondary effects in the posterior pole. The progressively
myopic eye epands in all its posterior dimensions, and the formation of an e5uatorial staphyloma
with scleral dehiscence is not uncommon, especially in the superotemporal 5uadrant. 4isual loss ismost often due to macular involvement of a posterior pole staphyloma. H==I The deformity occurs
in various locations, described by /urtinH=2I as posterior polar #disc and macula central$, macula
centered with the disc at the margin, peripapillary, inverse #in which the depression etends nasallyfrom the optic nerve head$, and an inferior type that involves the lower portion of the disc and thefundus below it. /omple patterns are termed compound staphylomata. Usually, the edge of the
defect is sharper closer to the disc and more blended away from it. taphylomata that are clear
edged and deep in a young person may occasionally lose some definition as the scleral envelopeenlarges with age.H==I
-
7/24/2019 93493980 Degenerative Myopia
9/49
s the scleral shell epands, the neural retina, pigment epithelium, and choroid stretch and thin to
accommodate the area they cover. Tissue attenuation causes the fundus to have a pale, tessellated
appearance. The pigment epithelial cells are flattened, and a reduction occurs in the thic)ness ofthe choriocapillaris and in the larger vessel layers and pigment of the choroid. This is evident
especially within the staphyloma itself, where the fundus pallor is eaggerated by the increased
visibility of the underlying sclera.
ith time and progression, traction and tension phenomena are observed. The first is a pale,temporal crescent at the disc as the pigment epithelium and choriocapillaris are retracted from the
discOs margin toward the deepest area of the staphyloma. ruchOs membrane is noncellular and
elastic but has a limited capacity to stretch. %f its elastic limit is eceeded, the internal tension isrelieved by formation of microdehiscences called lac5uer crac)s. cute lac5uer crac) formation
near the fovea occasionally is signaled by photopsias and metamorphopsia # +ig. =2?*= $. efects
in the overlying pigment epithelium may appear punctate, but eventually a linear pattern developsthat coincides with the brea)s in ruchOs membrane. /ontinued brea) formation results in a
reticular pattern that usually is most obvious in the deepest recess of the staphyloma and portends a
guarded prognosis for central vision.
The lac5uer crac) defects usually slowly increase in width and grow in number. :ther isolated,round, or irregular pigment epithelial and choriocapillaris defects may develop along the margin or
within the staphyloma. %f a choroidal neovascular membrane invades a crac), an abrupt macular
hemorrhage may be produced. lthough usually self*limited, the hyperpigmented fibrovascularscar that evolves #+RrsterA+uchsO spot$ causes a central or paracentral scotoma. n area of
choroidal and pigment epithelial atrophy develops and surrounds the scar # +ig. =2?*2 $. This
etends and coalesces with areas of atrophy that advance from other lac5uer crac)s, eventually to
produce large geographical areas of destruction in which sclera can be seen through the transparentneural retina. The process is usually bilateral and insidious. s paracentral fiation areas diminish,
even low*vision aids become useless and ambulatory sight is all that remains.
Macular hole formation in etreme myopes may occur, but the eact mechanism is un)nown.hether attenuation of the neural retina and its supportive pigment epithelium and choroid are
responsible is speculative. 4itreous syneresis and posterior vitreous detachment are more common
and occur at an earlier age among high myopes than among othersH=>I E usually they are not
accompanied by vitreomacular traction or an epiretinal membrane and only rarely produce aposterior rhegmatogenous retinal detachment.
%DN:% N N/%66;C T1T%ND
Myopes are recogni&ed easily by their poor distance visual acuity that is improved by negative*
power lenses. egenerative myopia is a diagnosis made when clinical findings and etreme aiallength occur together, as cause and effect.
The need for ancillary diagnostic testing is dictated by the preliminary findings. %f a posterior
staphyloma is detected or 5uestioned, and scan ultrasonography can confirm its presence.
+luorescein angiography and, in some cases, indocyanine green angiography may demonstrate
-
7/24/2019 93493980 Degenerative Myopia
10/49
more etensive lac5uer crac) formation than is detected by ophthalmoscopy and can be used to
rule out choroidal neovasculari&ation.
%++1;1NT%6 %DN:%
The clinician who has ta)en a careful history and performed a meticulous eamination will have nodifficulty in diagnosing
L>?
+igure =2?*2 udden loss of vision. This male /aucasian myope #right eye, *K years of age. , choroidalneovascular membrane invades the fovea. , +luorescein angiography demonstrates the central
membrane that had not been treated. /, The patient underwent a scleral reinforcement procedureon both eyes. +ifteen years later the area of central choriocapillary atrophy has enlarged, but
corrected visual acuity is a surprising 20Q
-
7/24/2019 93493980 Degenerative Myopia
11/49
ome systemic disorders are diagnosed easily, conditions such as albinism and trisomy 2=E others
are more subtle. ecause the cardiovascular complications of MarfanOs syndrome and congenital
rubella and the orthopedic disabilities associated with 1hlersAanlos and tic)lerOs syndromesmay produce morbidity and even mortality, prompt referral to medical and surgical colleagues is
indicated if the patient has not been referred already.
3T':6:DC
Typically, the etremely myopic eye is enlarged in all its posterior dimensions, but particularly inits aial length. nteriorly, the cornea may be slightly thinner and flatter than normal, with a
deeper anterior chamber, and the angle recess shows iris processes attached to the trabeculum. The
lens has a tendency to show early nuclear sclerosis. efects in the &onular membrane are commonand may present a challenge during cataract surgery. The ciliary body may be smaller than normal,
although considerable variability eists.
Denerali&ed scleral thinning is associated with increased scleral elasticity, or decreased ocular
rigidity. 1specially when combined with &onular dehiscence, this results in rapid vitreous fluidegress and global collapse when the eye is opened to atmospheric pressure. udden hypotony can
result in a serous or hemorrhagic choroidal detachment during intraocular surgery. natomically,
the sclera is not only thin but also has an abnormal constitution. The classic electron microscopic
findings of Dar&inoH=?I have been corroborated by others. The collagen fibers are of much smalleraverage diameter than in a normal eye.
ystemic ssociations of egenerative Myopia
lbinism
/ongenital rubella
de 6angeOs syndrome
ownOs syndrome
1hlersAanlos syndrome
-
7/24/2019 93493980 Degenerative Myopia
12/49
+etal alcohol syndrome
Dyrate atrophyShyperornithinemia
6aurenceAMoonAardetAiedl syndrome
MarfanOs syndrome
3ierre ;obinOs syndrome
tic)lerOs syndrome
+urther, the fibrils show greater interfibrillar separation and the normally tightly opposed and
interwoven architecture of the collagen bundlesH=7I gives way to a more uniformly lamellar andeventually amorphous appearance.H=
-
7/24/2019 93493980 Degenerative Myopia
13/49
effectiveness of atropine in eyes genomically destined to become pathologically myopic is
un)nown. :ther approaches presumed to act via modification of accommodation include the use of
bifocals, undercorrection of myopia, and part*time spectacle wear. /linical trials reportcontradictory results,H20I but the regulation of young primate eye growth has proved possible by
using plus and minus lenses to blur the retinal image.H7I
ecause highly myopic eyes have reduced scleral resistance plus a tendency to develop glaucoma,
many investigators have postulated that scleral epansion is caused by raised %:3.HJI3rssinenH2=I found a significant correlation between raised %:3 and myopic progression among
boys, but not among girls, while uinn et al.HKI noted that ocular tension is higher in children who
have myopia than in nonmyopes. /ontrolled trials of %:3 reduction have been reported. H22I H2>IH2JI Timolol maleate was employed,
L>7
all the sub!ects were children, and the focus was not on progressive degenerative myopia.
DoldschmidtOs pilot study of =0 children showed a tendency for the children who had a reductionin %:3 to slow in their progression of myopia,H2>I but ensenOs 2*year study of LJ children did not
prove timolol to be effective. H2JI The possibility remains that optical and pharmacological
methods, alone or in concert, may be devised to retard aial elongation.
%f advancing myopia in children continues beyond pubertal years, follow*up at least yearly isindicated. stereoscopic, indirect ophthalmoscopic, and biomicroscopic search for staphyloma
formation is important and, if suspected, staphyloma formation is investigated further using and
scan ultrasonography. ome of these eyes eventually stabili&e as highly myopic but with no
posterior complications. The ongoing evaluation of any peripheral lattice degeneration lesions thatmay be evident, especially in the event of blunt trauma or an acute posterior vitreous separation, is
critical.
%f staphyloma formation is detected, further caution is warranted. iannual eaminations mayreveal lac5uer crac) development that is not heralded by a photopsia or blurred central vision.
:nce lac5uer crac) formation or areas of choriocapillary and pigment epithelial atrophy are present
in a young adult, it becomes li)ely that the central vision will be threatened in time by advancingatrophy, choroidal neovasculari&ation, or both. The traditional option in the United tates at this
stage has been to continue observation, while ophthalmologists in some eastern 1uropean countries
advocate the use of various tissue etract in!ections, vasodilators, and scleral reinforcement.
lthough the value of reinforcement surgery is unproved,H2KI H2?I it may have application inselected and obviously endangered eyes in which the disease continues to advance.H27I
:ne step short of surgery, or in addition to it, is to lower %:3. No controlled trial has been used to
confirm efficacy or assured safety. Until such information is available, and in the absence of othercontraindications, the use of a tension*reducing agent in FnormalG eyes seems not unreasonable
and has been recommended.H27I ;elative ocular hypotension in eyes prone to develop tears in
ruchOs membrane may help to prolong central vision.
-
7/24/2019 93493980 Degenerative Myopia
14/49
:ther conservative measures include avoidance of eye rubbing, trauma, 4alsalva eertion, and
regular use of anticoagulants such as aspirin #unless re5uired for systemic disease$. ecause topical
corticosteroids fre5uently provo)e a rise in %:3 in the highly myopic eye, these also should beused with caution and with fre5uent tension chec)s.
Myopia*related choroidal neovasculari&ation is a ma!or cause of visual loss, especially whenlocated in a subfoveal location. 3hotodynamic therapy has shown a statistically significant
reduction in visual loss when compared with a placebo group after = year for subfoveal choroidalneovasculari&ation associated with pathological myopia.H2
-
7/24/2019 93493980 Degenerative Myopia
15/49
2. ;oberts , laby . ;efraction status of youths =2A=7 years. 3ub No #';$ 7KA=?>0.
ashington, /" U ept 'ealth, 1ducation and elfareE =L7J.
>. Mutti :, adni) 9, dams . Myopia, the nature versus nurture debate goes on. %nvest
:phthalmol 4is ci. =LL?E>7"LK2A7.
J. 3ruett ;/. 3rogressive myopia and intraocular pressure" what is the lin)ageP cta :phthalmol.
=L
-
7/24/2019 93493980 Degenerative Myopia
16/49
==. teidl M, 3ruett ;/. Macular complications associated with posterior staphyloma. m
:phthalmol. =LL7E=2>"=
-
7/24/2019 93493980 Degenerative Myopia
17/49
20. Doss . 1ffect of spectacle correction on the progression of myopia in children, a literature
review. m :ptom ssoc. =LLJE?K"==7A2. ensen '. Timolol maleate in the control of myopia. cta :phthalmol. =L
-
7/24/2019 93493980 Degenerative Myopia
18/49
by
Brian Ward, Ph.D., M.D.
December 2011
Degenerative myopia deserves our recognition as one of the truly neglected areas ofophthalmology. It is reported to be the seventh ranking cause of legal blindness in the
United Sates of America the fourth ranking cause in Hong Kong and the second in
parts of China and Japan. Degenerative myopia is an important world-health issue
with an unfortunate history of ineffectual treatments that have led most eye specialists
to believe that it is something of a "lost cause." As a result, this condition, which is
responsible for the loss of vision in so many people during the middle years of life
and in old age, seems destined to run its natural course, save for attention to
correction of the refractive error and the treatment of some of its other complications.
To summarize the course of this condition: It presents for the majority of people, as
an inherited genetic condition. This is why the incidence of this condition varies so
much between the various ethnic groups. The genetic defects responsible may be
transmitted between the generations in a variety of ways, and may produce very
different degrees of myopia in different family members.
An affected individual will show accelerated growth of the size of the eye duringthe normal growth-periods of childhood and adolescence, so that, by the late teens, or
the early twenties, the eye is much longer than normal. The eye is said to have high
axial myopia (nearsightedness). Distant objects are focused in front of its retina and
are thus out of focus. If objects are brought close to the eye, a point is reached when
they come into focus. This is known as the far point of the eye. The defocusing of the
retinal image may be corrected by spectacle lenses, contact lenses or by refractive
surgery. In all of these cases, the distant object appears to the eye to be situated at its
far point and is therefore in focus on the retina.
Unfortunately, this form of myopia frequently progresses in adult life, with small
intermittent steps of elongation being observable at any age. The adult progression
appears to be due to the stretching of the walls of the eye. Genetically weak elements
of the scleral wall are prone to thinning and stretching. One of the major forces at
-
7/24/2019 93493980 Degenerative Myopia
19/49
work in this stretching process appears to be the normal intra-ocular pressure.
Much of the sight loss in high axial myopia is thought to be due to the damaging
effects of the stretching and thinning of the inner parts of the eye. The sclera, the
choroid, the retina and the interface between the retina and the vitreous gel are all
affected by deformation. In the central retina, damage to the functioning of the macula
results in fine central-vision loss. This process of macular scarring is termed myopic
macular degeneration. Stresses in the retina and the adjacent parts of the vitreous gel
are also partly responsible for a predisposition to peripheral retinal tears, which may
go on to admit vitreous fluid into the sub-retinal space, producing retinal detachment.
Highly myopic eyes are also liable to loss vision from cataract and glaucoma. They
have an increased vulnerability to the damage effects of eye trauma, which mustinclude the higher incidence of complications in some ophthalmic surgical
procedures. Of all of these sight-threatening complications, myopic macular
degeneration is the most common. It is because of these degenerative complications,
that this disorder is called degenerative myopia
Early attempts to protect the macula from the damaging effects of stretching,
involved surgical procedures to reinforce the thinned weak sclera at the back of the
eye. It had been observed that a bulge (a staphyloma) could often be observed behindthe macula. This very severe localized scleral thinning results in especially severe
stretching of the inner layers in the region of the macula and especially severe damage
to its tissues. Various natural materials had been used for staphyloma support, but it
was donor-sclera that was finally selected for by most surgeons. Today, the results of
these various early operations are difficult to assess, in terms of their safety and their
effectiveness.
In the U.S.A. two prominent groups advocated scleral reinforcement fordegenerative myopia. Dr Brian Curtin lead the effort in New York, while a California-
based group of surgeons used rather different procedures. The "West Coast" approach
evolved from pioneering work by Borley and Snyder at the Stanford medical campus
in San Francisco. Curtin tried different approaches before finally concluding that
these had been ineffective, and noting some significant complications in some of their
-
7/24/2019 93493980 Degenerative Myopia
20/49
cases. Meanwhile, on the West Coast, Snyder, Thompson and Miller continued to
develop their surgical approaches to scleral reinforcement, with no reports of adverse
safety issues. These surgeons had a firm conviction that they were stabilizing axial
myopia progression through their efforts. It is unfortunate that their published reports
are somewhat anecdotal and lack any controlled studies. Perhaps because of the
widespread disappointment with Curtin's conclusions, and the lack of controlled
studies on other techniques, the interest in surgical treatments was largely lost.
In retrospect, these initial attempts at myopia control by scleral grafting are seen to
have been important pioneering innovations, which may have lead to some modest
contributions to saving sight. They were, in retrospect, perhaps providing support
which was rather "too little and too late."
Personal experience with Thompson's technique had showed it to be safe, and a
pilot study indicated an encouraging degree of axial myopia control when compared
to its progression in the unsupported eyes. Thompson's basic approach of "scleral
reinforcement" was found to become more effective when the concept was extended
to one of the buckling of the posterior pole of the eye, by providing a firm structural
connection between the thin weak sclera at the back of the eye and the thicker tissue
at the front of the globe. A gently tensioned sling was positioned over the back of the
eye, under general anesthesia, and its ends were firmly anchored to the thick sclera inthe anterior part of the globe. With this approach, adult eyes showed more stability of
their axial myopia and, unexpectedly, some patients reported small subjective
improvements in their quality of vision. In retrospect, there are some theoretical
reasons why some small vision improvement might have occurred in some patients.
In collaboration with Prof. Elena P. Tarutta, of Moscow, a clinical study was
designed to follow and to evaluate buckled and unbuckled eyes for a period of five
years. Fellow eyes, with similar degrees of high myopia, were designated as thecontrol eyes, and followed according to the same protocol. The majority of the 59
buckled adult eyes showed stabilization of their axial myopia. The five-year follow up
data illustrated this fact and also confirmed that a limited visual acuity improvement
had occurred after buckling in some eyes. The relative stability after surgery meant
that it became appropriate to offer the treatment for the patient's second eye during the
-
7/24/2019 93493980 Degenerative Myopia
21/49
study period; especially where a clear increase in axial length was evident in the
control eye. Parts of this study were presented at the International Myopia Conference
in Singapore in August of 2006. It is the first study to show good safety of a
procedure and a statistically significant efficacy in terms of axial myopia control.
In the study, reported after its conclusion in 2009, it was found that one of the
treated eyes had had a form of myopic macular schisis and local traction detachment.
Post-operatively, this complication was found to have been corrected (incidentally).
The basic buckling surgical procedure has now been modified for the optimal
treatment of this new indication myopic macular schisis. The effectiveness of
buckling for treating existing macular schisis suggests that the buckles being applied
for axial myopia control might well serve to prevent the development of macular
schisis and detachments.
Today the indication for buckling surgery, in cases of Degenerative Myopia, is the
risk of further axial extension in an eye, which is at least 26mm in axial length, at
almost any age. The measurement of 26mm is used, as it is the threshold axial length
for the development of myopic macular degeneration. The refractive error present
may be as little as -6.00 diopters, but it is generally much greater. The risk of Macular
degeneration increased with both the passage of time (i.e. the age of the patient) and
with the magnitude of the axial length of the eye. Buckling adult eyes can stabilizeaxial length and minimize future macular degeneration, but it cannot prevent the
continuation of degenerative processes, which are already at work.
The appropriateness of buckling surgery for high axial myopia should be
considered on a case-by-case basis.
Degenerative myopia may be preventable in the future. Today, however, the usual
treatments are limited to optical correction, intra-ocular pressure control, and attentionto complications that may occur. The use of scleral buckling can prevent axial
extension and minimize the toll of myopic macular degeneration on future visual
function. At-risk eyes deserve careful evaluation and follow-up, with early treatment
where appropriate. New buckling materials are being evaluated for their use in the
more severe cases in all age groups. These are eyes in which greater areas of support
-
7/24/2019 93493980 Degenerative Myopia
22/49
and stronger buckling forces may be helpful. As always, the safety of any treatment
needs to be evaluated in terms of its risk-to-benefit ratio.
It should also be remembered that the prevention of axial myopia increase is also of
value in stabilizing the power of the required corrective lens. This is especially
important where refractive surgical correction is being considered. This benefit of
axial myopia stabilization applies equally to ensuring stability of the effectiveness of
the intraocular lens implant, following cataract surgery.
Brian Ward, Ph.D., M.D.
Retinal Diagnostic Center
3395 S. Bascom Ave, Suite 140
Campbell, California 95008
Journal of Ophthalmology
Volume 2010 (2010), Article ID 1751!, " page#
$oi%10&1155'2010'1751!
a#e eport
*athology of +acular o-eo#chi#i# A##ociate$ .ith Degenerati-e +yopia
Johnny /ang,1,2 +ichael & i-er#,! An$re. A& +o#hfeghi," arry & lynn Jr&," an$
hi3hao han5
1e#earch 4er-ice, oui# 4to6e# le-elan$ VA +e$ical enter, le-elan$, O ""103
50, 84A
2Department of Ophthalmology an$ Vi#ual 4cience#, 8ni-er#ity o#pital# 9ye
In#titute, 8ni-er#ity o#pital# a#e +e$ical enter, a#e e#tern e#er-e 8ni-er#ity,
11100 9ucli$ A-enue, :4D "107, le-elan$, O ""10350, 84A
!/he etina ;roup of a#hington, airfa
-
7/24/2019 93493980 Degenerative Myopia
23/49
54ection of Immunopathology, a=oratory of Immunology, >ational 9ye In#titute,
>ational In#titute# of ealth, ethe#$a, +D 20?23!55, 84A
ecei-e$ 2" +arch 2010@ e-i#e$ ? June 2010@ Accepte$ 1! July 2010
Aca$emic 9$itor% Dariu# +& +o#hfeghi
opyright 2010 Johnny /ang et al& /hi# i# an open acce## article $i#tri=ute$ un$er
the reati-e ommon# Attri=ution icen#e, .hich permit# unre#tricte$ u#e,
$i#tri=ution, an$ repro$uction in any me$ium, pro-i$e$ the original .or6 i# properly
cite$&
A=#tract
/hi# i# a clinicopathological paper on the hi#tologic fin$ing# in myopia3a##ociate$
macular fo-eo#chi#i#& /he fin$ing# on ophthalmic pathological #tu$y of a 7!3year3ol$
.oman .ith high myopia are re-ie.e$& +ultiple retino#chi#i# ca-itie# in-ol-ing =oth
the macula an$ retinal periphery .ere $i#clo#e$& Our paper offer# ti##ue e-i$ence
an$ #upport# recent ocular coherence tomography report# of eye# .ith high myopia
an$ a##ociate$ macular fo-eo#chi#i#&
1& Intro$uction
+yopic fo-eo#chi#i# (+4) in highly myopic eye# i# a more recently recogniBe$ clinical
entity .ho#e clinical $e#cription ha# =een facilitate$ -ia optical coherence
tomography (O/) #tu$ie#& C1, 2& *re-iou#ly, myopic fo-eo#chi#i# ha# =een poorly
characteriBe$ an$ may ha-e =een mi#ta6en for macular hole# or #hallo. retinal
$etachment# C1, !& /he fir#t $e#cription of thi# entity .a# =y *hillip# .ho note$
that localiBe$ po#terior retinal $etachment o-er po#terior #taphyloma can occur e-en
in the a=#ence of a retinal hole C"& +yopic fo-eo#chi#i# affect# ?E to 20E of myopic
eye# .ith #taphyloma# C5, & 8tiliBing O/, it i# no. 6no.n that +4 can lea$ tothe $e-elopment of #u=tle #hallo. retinal $etachment# an$'or macular hole# in
patient# .ith high myopia an$ account for pre-iou#ly un6no.n cau#e# of -i#ion lo##
in the#e patient# C1, 7& /o $ate, pathology of #uch eye# ha# not =een .ell
illu#trate$& erein, .e $e#cri=e a clinicopathologic ca#e of +4 a##ociate$ .ith high
myopia&
2& a#e eport
-
7/24/2019 93493980 Degenerative Myopia
24/49
A 7!3year3ol$ .oman .ith high myopia .a# referre$ .ith complaint# of =ilateral
.or#ening -i#ion& 4he $i$ not report #ymptom# of photop#ia# or #cotoma#& /he =e#t3
correcte$ -i#ual acuity .a# 20'70 OD an$ 20'0 O4 .ith a refraction of
F
1
5
&
5
G
!
&
0
0
H
1
1
!
OD an$
-
7/24/2019 93493980 Degenerative Myopia
25/49
F
1
&
5
G
2
&
2
5
H
7
2
O4& Anterior #egment .a# remar6a=le for only mil$ nuclear #clerotic cataract# O8&
un$u# e
-
7/24/2019 93493980 Degenerative Myopia
26/49
angiogram of the right eye in the early (a) an$ late (=) pha#e# $emon#trating #taining
of the optic ner-e cre#cent# an$ #mall .in$o. $efect# along the macular region&
/.o year# later, #he $ie$ of unrelate$ cau#e# .ithout inter-al ocular e
-
7/24/2019 93493980 Degenerative Myopia
27/49
i#tologically, the right eye $emon#trate$ $egenerati-e retino#chi#i# .ith
inter=ri$ging #tran$# in the outer ple
-
7/24/2019 93493980 Degenerative Myopia
28/49
illu#trate# that retinal #chi#i# ca-itie# can form in -ariou# layer# of the neuro#en#ory
retina in high myope#&
+yopic fo-eo#chi#i# lea$# to $ecrea#e# in -i#ual acuity =ecau#e of $i#ruption of the
neuro#en#ory element# an$ pre$i#po#e# patient# to fo-eal retinal $etachment# C1,
!, 7& John#on re-ie.e$ the interaction# =et.een the -itreou# an$ retina that are
thought to =e cau#e# of the#e -itreoretinal interface a=normalitie# C10& e $i#cu##e#
that +4 i# li6ely cau#e$ =y a relati-e #tiffne## of the inner retina compare$ .ith the
outer retina .ithin the conca-ity of the #taphyloma re#ulting from cortical -itreou#
remnant# after incomplete po#terior -itreou# $etachment (*VD) C10& Al#o, po##i=ly
contri=uting i# a non$i#ten#i=le I+ an$ inner retinal =loo$ -e##el# C10& /he fi=roglial
preretinal mem=rane that .a# a$herent to the I+ in our #pecimen #upport# O/ an$
more recent ultra#tructural #tu$ie# that the preretinal mem=rane# an$ incomplete
*VD in highly myopic patient# contri=ute to +4 formation C, 10, 11& ;aucher et
al& reporte$ the pre#ence of -ertical column3li6e #tructure# #een on O/ .hich arecon#i#tent .ith fin$ing# #een in our #ection# (igure 2($)) C12&
A long3term e-aluation of 2? eye# .ith +4 $emon#trate$ that the natural e-olution
of thi# $i#ea#e i# rather $i-er#e C12& ortunately, patient# may remain #ta=le for
many year# .ithout affecting VA C12& i#6 factor# for .or#ening VA increa#e# .hen
there are a##ociate$ premacular #tructure# #uch a# epiretinal mem=rane# or a
partially $etache$ -itreou# corte< C12& 4e-eral #tu$ie# propo#e that -itrectomy i# a
rea#ona=le con#i$eration in the#e ca#e# C1!1&
inancial Di#clo#ure#
/he author# ha-e no financial intere#t# to $i#clo#e&
Ac6no.le$gment#
/hi# .or6 .a# #upporte$ in part =y the Veteran# Affair# areer De-elopment A.ar$ 2,
Veteran# Affair# oun$ation A.ar$, an$ the >9I Intramural e#earch *rogram&
-
7/24/2019 93493980 Degenerative Myopia
29/49
eference#
1& +& /a6ano an$ 4& :i#hi, Ko-eal retino#chi#i# an$ retinal $etachment in #e-erely
myopic eye# .ith po#terior #taphyloma,L American Journal of Ophthalmology, -ol&
12, no& ", pp& "72"7, 1???& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at
4copu#
2& J& A6i=a, 4& :onno, 9& 4ato, an$ A& No#hi$a, Ketinal $etachment an$ retino#chi#i#
$etecte$ =y optical coherence tomography in myopic eye .ith a macular hole,L
Ophthalmic 4urgery an$ a#er#, -ol& !1, no& !, pp& 2"02"2, 2000& Vie. at 4copu#
!& N& I6uno, & ;omi, an$ N& /ano, K*otent retinal arteriolar traction a# a po##i=le
cau#e of myopic fo-eo#chi#i#,L American Journal of Ophthalmology, -ol& 1!?, no& !,
pp& "2"7, 2005& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at *u=+e$ M
Vie. at 4copu#
"& & I& *hillip#, Ketinal $etachment at the po#terior pole,L riti#h Journal of
Ophthalmology, -ol& "2, no& 12, pp& 7"?75!, 1?5&
5& /& a=a, :& Ohno3+at#ui, an$ :& Ohno3+at#ui, K*re-alence an$ characteri#tic# of
fo-eal retinal $etachment .ithout macular hole in high myopia,L American Journal of
Ophthalmology, -ol& 1!5, no& !, pp& !!!"2, 200!& Vie. at *u=li#her M Vie. at ;oogle
4cholar M Vie. at 4copu#
& ;& *anoBBo an$ A& +ercanti, KOptical coherence tomography fin$ing# in myopic
traction maculopathy,L Archi-e# of Ophthalmology, -ol& 122, no& 10, pp& 1"551"0,
200"& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at *u=+e$ M Vie. at 4copu#
7& >& enhamou, *& +a##in, & aouchine, A& 9rginay, an$ A& ;au$ric, K+acular
retino#chi#i# in highly myopic eye#,L American Journal of Ophthalmology, -ol& 1!!, no&
, pp& 7?"00, 2002& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at 4copu#
& +& Ip, & ;arBa3:arren, J& 4& Du6er, 9& eichel, J& & 4.artB, A& Amiri6ia, an$ & A&
*uliafito, KDifferentiation of $egenerati-e retino#chi#i# from retinal $etachment u#ing
optical coherence tomography,L Ophthalmology, -ol& 10, no& !, pp& 0005, 1???&
Vie. at 4copu#
?& +& & a==, I& ;aroon, an$ & *& aranco, K+yopic macular $egeneration,L
International Ophthalmology linic#, -ol& 21, no& !, pp& 51?, 1?1& Vie. at 4copu#
10& +& & John#on, K*o#terior -itreou# $etachment% e-olution an$ complication# of
it# early #tage#,L American Journal of Ophthalmology, -ol& 1"?, no& !, pp& !71!2,
2010& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at *u=+e$ M Vie. at 4copu#
11& & an$o, N& I6uno, J&34& hoi, N& /ano, I& Namana6a, an$ /& I#hi=a#hi,
K8ltra#tructure of internal limiting mem=rane in myopic fo-eo#chi#i#,L American
-
7/24/2019 93493980 Degenerative Myopia
30/49
Journal of Ophthalmology, -ol& 1!?, no& 1, pp& 1?71??, 2005& Vie. at *u=li#her M Vie.
at ;oogle 4cholar M Vie. at *u=+e$
12& D& ;aucher, & aouchine, & /a$ayoni, *& +a##in, A& 9rginay, >& enhamou, an$
A& ;au$ric, Kong3term follo.3up of high myopic fo-eo#chi#i#% natural cour#e an$
#urgical outcome,L American Journal of Ophthalmology, -ol& 1"!, no& !, pp& "55"2,2007& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at *u=+e$
1!& & :o=aya#hi an$ 4& :i#hi, KVitreou# #urgery for highly myopic eye# .ith fo-eal
$etachment an$ retino#chi#i#,L Ophthalmology, -ol& 110, no& ?, pp& 17021707, 200!&
Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at *u=+e$ M Vie. at 4copu#
1"& 4& :an$a, A& 8emura, N& 4a6amoto, an$ & :ita, KVitrectomy .ith internal limiting
mem=rane peeling for macular retino#chi#i# an$ retinal $etachment .ithout macular
hole in highly myopic eye#,L American Journal of Ophthalmology, -ol& 1!, no& 1, pp&
17710, 200!& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at 4copu#
15& N& I6uno, :& 4ayanagi, an$ :& 4ayanagi, KVitrectomy an$ internal limiting
mem=rane peeling for myopic fo-eo#chi#i#,L American Journal of Ophthalmology, -ol&
1!7, no& ", pp& 71?72", 200"& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at
*u=+e$ M Vie. at 4copu#
1& & & 4pai$e an$ N& i#her, Kemo-al of a$herent cortical -itreou# plaue#
.ithout remo-ing the internal limiting mem=rane in the repair of macular
$etachment# in highly myopic eye#,L etina, -ol& 25, no& !, pp& 2?02?5, 2005& Vie.
at *u=li#her M Vie. at ;oogle 4cholar M Vie. at 4copu#
17& :& otta an$ J& otta, Ketino#chi#i# .ith macular retinal $etachment a##ociate$
.ith -itreomacular traction #yn$rome,L etina, -ol& 2", no& 2, pp& !07!0?, 200"&
Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at 4copu#
1& :& 4ayanagi, N& I6uno, an$ N& /ano, Keoperation for per#i#tent myopic
fo-eo#chi#i# after primary -itrectomy,L American Journal of Ophthalmology, -ol& 1"1,
no& 2, pp& "1""17, 200& Vie. at *u=li#her M Vie. at ;oogle 4cholar M Vie. at *u=+e$
M Vie. at 4copu#
FAQ - Myopia, Degenerative(Powered by Yahoo! Anwer
Doe anyone "now how #ommon the $degenerative myopia$ i%
% am very shortsighted #*L.K$ and !ust heard about (degenerative myopia(. % wonder how many
high degree myopia people will have (degenerative myopia(.**********
http://www.lookfordiagnosis.com/mesh_info.php?term=Myopia%2C+Degenerative&lang=1http://www.lookfordiagnosis.com/mesh_info.php?term=Myopia%2C+Degenerative&lang=1 -
7/24/2019 93493980 Degenerative Myopia
31/49
2- of the population has this. Cou are nearsighted. ny person with a high degree of myopia has a
higher ris) of retinal detachment. %t is not li)ely that you have this but an ophthalmologist #not anoptometrist$ should be consulted if you feel you may have it. #V info$
Do & have degenerative myopia%% have been wearing glasses for myopia since Kth grade, and %8ve had to get new glasses about each
year. % spend a lot of time in front of electronics. % see spots and have a lot of headaches recently. %
want to )now what cures there are and what to do to stop my eyesight from worsening.**********
ee an eye doctor to discuss options. lso chec) out this site"http"QQwww.tlcvision.comQwhy@[email protected] #V info$
Degenerative myopia%
'ow can % tell if % have it or notP %8m => and my vision has been getting worse every year for !ust
about the past 7 years. % believe there was one year when my vision actually got better, but %dunno. 6ast % chec)ed, my vision was *L and *7 in my right and left eye, and % )now it8s gottenworse this year. o % have degenerative myopiaP
orry, % misunderstood. Than)s to everyone who answered. % was under the impression progressive
myopia never gets better, lol. Than)s again. "$**********
hat you are describing is referred to as (progressive( myopia. 3rogressive myopia is agenetically inherited condition. The classical presentation of progressive myopia tends to follow
this time line ** Most first notice a shift into myopia causing a blurring of distance around second
to third grade #7 to < years of age$. The individual then consistantly and continually increases in
nearsightedness until about the age =7 to =L at which time most then become somewhat stable intheir degree of nearsightedness for many years until other vision issues such as cataract may cause
changes. ince % am also a progressive myope, you and % have a common ancestor somewhere. %
received my first set of eyeglasses from my uncle who was an eye doctor. % became stable at age=
-
7/24/2019 93493980 Degenerative Myopia
32/49
nearsighted.
the only way to )now if you have degenerative myopia is to have a dilated eye eamination andhave an eye doctor #optometrist or ophthalmologist$ ma)e that diagnosis for you. your retina either
has a degenerated appearance or it does not. no way to tell by !ust the spectacle ; #whether you
are *L.00 or not$ or whether you are becoming increasingly nearsighted or not #V info$
Degenerative Myopia%%
%8m 2K, and was born with congenital glaucoma and nystagmus so %8ve always worn glasses. bouta year ago my vision changed again from a *> in both eyes to a *K in the left and *J.K0 in the right,
and it seems to be getting worse. %8ve been to 2 :pth. who can find no reason for it, and neither
have made any remar)s about problems with my retina etc. although % do see floaters and such. o% have degenerative myopiaP % mean, normally eyes stabili&e before your 2K rightP Than)s
**********
big change in your need for glasses over a short time period #and at your age$ could have more
to do with your congenital glaucoma. %f it8s been a while since you8re been to the ophthalmologist,you should have your eye pressures chec)ed. hile you8re there you can as) about having your
retina eamined #usually re5uires dilating drops$. %f you don8t feel comfortable with theophthalmologists you8ve seen, maybe you should get another opinion from a different
ophthalmologist.
+loaters are pretty normal, unfortunately. %f your vision is suddenly grey, li)e you8re loo)ing
through a curtain, call your ophthalmologist immediately.
Dood luc) to youZ #V info$
*ow m#h are #o)ored #onta#t for a peron with myopia%% have myopia and % want to get ha&el prescription contacts, does any body have any idea how
much that would costP
'ow much are regular contacts thenP**********
o you wear hard lens, if so they don8t ma)e color contacts. %f you wear soft lens then they areabout >0 dollars a bo. #V info$
& Degenerative Di# Dieae and Di# +pa#e arrowing the ame thing%
The chiropractor told me % had disc space narrowing. %s that the same as degenerative disc diseaseP
%t8s etremely painful and % can8t sit or stand for long periods of time. Than)s for the help.**********
No, they are referring to two different things. is the actual bone of the spine degenerating.
N is the intervertrebral disc, ie the cushion is failing. #V info$
hat i Degenerative +pine and why are there wing invo)ved%
http://answers.yahoo.com/question/?qid=20070618030912AAV0HG2http://answers.yahoo.com/question/?qid=20081029121312AAts62Rhttp://answers.yahoo.com/question/?qid=20090213152331AAVxiNThttp://answers.yahoo.com/question/?qid=20080503195058AAimEt9http://answers.yahoo.com/question/?qid=20070618030912AAV0HG2http://answers.yahoo.com/question/?qid=20081029121312AAts62Rhttp://answers.yahoo.com/question/?qid=20090213152331AAVxiNThttp://answers.yahoo.com/question/?qid=20080503195058AAimEt9 -
7/24/2019 93493980 Degenerative Myopia
33/49
:)ay, so, my doctor said % have degenerative spine. Two people have T;%1 to eplain what it is,
but they use big words that mean nothing to me. Dive me a brea), % only too) one semester of high
school medical terminology. /ould you eplain in %M361 terms what8s going on with my bac),and why he said there were (two little wing loo)ing things coming off the base( of my spineP hy
are they thereP lso, is there any way to ma)e my tailbone T:3 hurtingP 3lease help. Than) you.
**********
Do here"
http"QQwww.la!ollaspine.comQsdds.shtml #V info$
& there any way to red#e the power(myopia in the eye withot rgery%
% really can8t undergo surgery. ut % want to )now if there is any way of reducing this eye
defect#myopia$ without surgery.
**********
%t8s posible but unfortunatly most people are too la&y and don8t believe in self healing. % have a reada boo) with studies where people ranging in different ages had their eye sight fied by !ust
eerci&ing their eyes. Cou )now the table with the lettersP 6oo) at the line where it already getsblurry. 9eep on loo)ing at it, blin)ing, tryng to see the letters. hen you see the letter are getting
bette, stop. o this for about K mins. > times a dayP on8t stress urself. 9eep on wro)ing on that
one line until you see it crearly from the start of the 8wor)out8. Then, go onto the net line. %t isn8tsilly. %t :;9 because the eyes contain muscles that contract and lenses that )eep on ad!usting.
#1ample" ;unning builds up muscles and breathing so after running many times you won8t havebreathing problems*$
Cou always have to persuate yourself that C:U /N fi your eye sight. % )now some people whowere able to do it. Try it. Ta)e some time. M:st people are la&y and won8t do it. :thers lac) belief
in self healing. This is the only way % )now without an operation. [ good luc)Z #V info$
hat "ind of profeion i mot itab)e for peop)e with high degree of myopia%
hat )ind of profession is most suitable for people who suffer from high degrees of myopia
#nearsightedness$ or what )ind of wor) they should perform in order not to hurt their eyesP**********
ell this optometrist gets to *=J.2K in the worst meridian of my worst eye.
%t8s given me some insight #sorry$ and empathy with at least my high myope patients.
%t8s a 5uestion better tac)led from the other end.
'igh myopes are marginally more prone to retinal detachment, so occupations eposed to vibration
or shoc)s are to be avoided" pneumatic drills, driving heavy machinery...
'igh diver, professional football player #U$
ome occupations re5uire good vision without glasses or contact lenses... principally branches of
http://answers.yahoo.com/question/?qid=20060611224144AA0iSG8http://answers.yahoo.com/question/?qid=20080229084658AAMN2Wwhttp://answers.yahoo.com/question/?qid=20060611224144AA0iSG8http://answers.yahoo.com/question/?qid=20080229084658AAMN2Ww -
7/24/2019 93493980 Degenerative Myopia
34/49
the military and the fire service, but heavy goods vehicle driving is also legally barred from high
myopes on grounds of a minimum vision without glasses re5uirement in most countries.
:therwise go for itZ
)i instructor, if you are happy in contacts
#glasses steam upZ$ #V info$
.)aifi"ai myopia berdaar"an bearnya dera/at refra"i anoma)y, antara lain "
=. Myopia ringan " pheris * 0.2K ioptri sQd pheris * >.00 ioptri
2. Myopia sedang " peris * >.2K ioptri sQd pheris * ?.00 ioptri
>. Myopia tinggi " lebih dari pheris * ?.2K ioptri
.)aifi"ai berdaar"an )a/ perbahan bearnya dera/at anoma)y e#ara ")ini", antara lain "
Myopia imp)e"0taioner0fiio)ogi"
Myopia simple) biasanya timbul pada usia yang masih muda )emudian a)an berhenti. Tetapi dapat
!uga nai) sedi)it )emudian berhenti. apat !uga nai) sedi)it pada masa puber sampai se)itar umur
20 tahun. esar dioptrinya )urang dari *K.00 ioptri atau *?.00 ioptri. Tetapi )alau di)ore)si
dengan lensa yang sesuai dapat mencapai normal yaitu ?Q? atau 20Q20.
Myopia progreif
Myopia ini ditemu)an pada segala umur. 3ada )eadaan ini a)an ter!adi )elainan fundus yang )has
untu) myopia tinggi # myopia lebih dari peris *?.00 ioptri $
Myopia ma)igna
Myopia ini disebut !uga dengan myopia patologisQdegeneratif )arena disertai penuaan dari )oroid
dan bagian lain dalam bolamata # lensa, )oroid, badan siliar $.
Myopia berdasar)an fa)tor penyebab dapat dibeda)an men!adi dua, yaitu "
Myopia a1ia)
Myopia aial ini dapat ter!adi se!a) lahir oleh )arena fa)tor hereditas, )ompli)asi penya)it lainseperti gondo), T/, dan campa) maupun )arena )onginetal. elain itu !uga dapat )arena ana)
biasa membaca dalam !ara) yang selalu de)at sehingga mata luar dan polus posterior yang paling
lemah dari bolamata meman!ang. :rang yang berwa!ah lebar a)an menyebab)an )onvergensiberlebihan saat mela)u)an pe)er!aan de)at, )arena peradangan atau melemahnya lapisan yang
mengelilingi bolamata disertai te)anan yang tinggi. Myopia ini dapat bertambah terus sampai
dewasa.
http://answers.yahoo.com/question/?qid=20070821080916AAcDypOhttp://answers.yahoo.com/question/?qid=20070821080916AAcDypO -
7/24/2019 93493980 Degenerative Myopia
35/49
Myopia aial merupa)an suatu )eadaan dimana !ara) fo)us media refra)ta lebih pende)
dibanding)an sumbu orbitnya. alam hal ini !ara) fo)us media refra)ta normal 22,? mm
sedang)an !ara) sumbu orbitnya adalah \ 22,? mm.
Myopia refra"tif
Myopia refra)tif merupa)an suatu )eadaan dimana !ara) fo)us media refra)ta lebih pende)
ddibanding)an sumbu orbitnya. Namun dalam hal ini sumbu orbit normal 22,? mm sedang)an
!ara) fo)us media refra)ta ] 22,? mm
umber" http"QQid.shvoong.comQmedicine*and*healthQophthalmologyQ2=7JLJ A /omplications of Dlaucoma urgery and Their Management
. %66%M :C61
M. +;N M%T'
%NT;:U/T%:N
%n the ideal world, surgery proceeds smoothly and outcomes are uncomplicated. Unfortunately, inthe real world, despite a surgeonOs best efforts, complications may occur. This is especially true in
the field of glaucomaSglaucoma surgery, unli)e many other ocular procedures, is not particularly
FforgivingG in nature. Nonetheless, good final outcomes may often be achieved in spite of theoccurrence of complications. The )ey to success is for the surgeon to be alert and be able to
identify and address any problems promptly.
+%6T;T%:N U;D1;C
efore the discussion of complication management in filtration surgery, it is worth repeating an
old surgical aiom. ithout a doubt, the best surgical complication management is avoidance ofthe complication in the first place. 3reoperatively, ensure that the patient stops the inta)e of all
aspirin*li)e products, and discontinue topical epinephrine #adrenaline$ compounds to decrease the
5uantity of superficial bleeding. /onsider the use of preoperative topical antibiotics.%ntraoperatively, meticulous attention to detail is important, especially if antimetabolites are being
used. %t is imperative to handle the con!unctiva gently. hen the partial*thic)ness trabeculectomy
http://id.shvoong.com/medicine-and-health/ophthalmology/2174948-klasifikasi-myopia/#ixzz1towVNYVjhttp://id.shvoong.com/medicine-and-health/ophthalmology/2174948-klasifikasi-myopia/#ixzz1towVNYVjhttp://id.shvoong.com/medicine-and-health/ophthalmology/2174948-klasifikasi-myopia/#ixzz1towVNYVjhttp://id.shvoong.com/medicine-and-health/ophthalmology/2174948-klasifikasi-myopia/#ixzz1towVNYVj -
7/24/2019 93493980 Degenerative Myopia
36/49
flap is being closed, consider using etra, releasable*style sutures. %f intraocular pressure #%:3$ is
too high postoperatively, a stitch may be pulled easily. ut if too much drainage occurs
postoperatively, an insidious cycle of overdrainage may be establishedSand this cannot always becorrected readily.
Nonetheless, complications intermittently occur. +iltration surgery complications are most easilycategori&ed as intraoperative, early postoperative, and late postoperative.
%ntraoperative /omplications
/:NUN/T%46 UTT:N':61.
%n no other situation is the aiom given before more appropriateSthe best complication
management of the buttonhole is initial avoidance of the complication. Toothed forceps are the
problem hereSthey should not be on the glaucoma tray. ishop*'armon or suture*tying forceps
are preferable when con!unctiva is handled. etter yet, the use of a dry cellulose sponge, with its
tip cut off, to stretch con!unctiva up and away from the area of interest is safe. %f a buttonholeoccurs anyway, management re5uires patient, complete hole closure if successful surgery is to
ensue. %f a buttonhole cannot be closed in a watertight fashion and detection of the hole hasoccurred early in the surgery, consideration must be given to rotation of the site of the
trabeculectomy flap to a different area, away from the hole. lso, if antimetabolite use was
planned but not initiated prior to discovery of the buttonhole, the surgeon must consider noeposure, or limited eposure, to antimetabolite, applied well away from the buttonhole.
/losure techni5ue for a con!unctival buttonhole depends on its location, si&e, and shape. The most
easily closed buttonhole
+igure 2J>*= ;epair of buttonhole close to limbus.
+igure 2J>*2 Two*layer closure of intraoperative buttonhole in central bleb &one. +ollowing
TenonOs layer closure, con!unctiva is closed.
is the short limbal tear, which may be closed with a hori&ontal mattress suture of double*armed =0*0 nylon. /ornea !ust anterior to the tear is deepitheliali&ed. :ne arm of the suture is passed to one
side of the hole, through con!unctiva and partial*thic)ness anterior TenonOs layer, and into the
cornea in front of the tear. The other needle of the double*armed suture is passed similarly on theother side of the hole. hen the two ends are tied, con!unctiva is pulled safely down, with
-
7/24/2019 93493980 Degenerative Myopia
37/49
considerable overlap, onto clear cornea. The deepitheliali&ed cornea 5uic)ly heals to the underside
of the overlapped con!unctiva # +ig. 2J>*= $.
6inear tears of con!unctiva away from the limbus are probably best closed in two layers with arunning suture. n *2 $. imilarly,
small, round holes can be closed using a two*layer techni5ue and purse*stringing the suture aroundthe hole.
=?==
+igure 2J>*> 3eripheral intraoperative buttonhole closure. ;epair by inclusion in con!unctivalincision closure.
+inally, linear tears in con!unctiva near a forni incision are fre5uently best addressed by
incorporation of the tear into the final incision closure #see +ig. 2J>*> $.
fter buttonhole repair, it is essential that watertightness be tested before proceeding further.alanced salt solution may be s5uirted vigorously at one side of the closure and any seepage
through to the other side carefully sought. lso, after final incision closure, it is best to rechec) for
lea)age using fluorescein dye. %nflation of the bleb with balanced salt solution through the cornealparacentesis and application of fluorescein dye is a simple way to mar) any lea)s. The time to
address such lea)s is while the patient has good anesthesia and is still in the operating room.
3ostoperatively, when inflammation occurs and the con!unctiva has become thinned because of
a5ueous flow, definitive surgical repair may not be possible.
T;1/U61/T:MC /61;6 +63 T1;Q%%N1;T%:N.
:ccasionally, despite the surgeonOs attempt to dissect up a sufficiently thic) #about two thirds of
the total scleral thic)ness$ scleral flap, tissues are such that a FrattyG flap is produced. These flaps
tend to tear or disinsert. %f the tear is found early and is small enough, direct suture closure using
=0*0 nylon may be attempted. imilarly, if the flap base is disinserted partially, an attempt may bemade to reposit the flap using a double*armed hori&ontal mattress suture eternali&ed through clear
cornea # +ig. 2J>*J $. ome surgeons have reported successful reposition of a totally disinsertedflap using two =0*0 nylon sutures through the flap base and out the peripheral cornea.H=I 'owever,
total disinsertion and large tears are usually a reflection of eceptionally poor 5uality #ratty$ scleraE
such flaps do not tolerate sutures well and tend to Fcheesewire,G which results in larger defects.
;ather, this complication may be best addressed by placement of an additional cover over theproblem flap.
-
7/24/2019 93493980 Degenerative Myopia
38/49
TenonOs tissue is readily available in all eyes. The surgeon may choose to ecise a J _ >Pmm piece
of redundant TenonOs tissue from up in the superior forni near the incision or alternatively from
the inferior forni if ecess tissue is not present superiorly. This ecised rectangular piece of tissuemay be sutured at its four corners over the full*thic)ness sclerotomy. H2I %f ecess lea)age is noted
after anterior chamber reformation, additional sutures may be placed. :ther choices of coverage
material are donor sclera,H>I dura, pericardium, or even fascia lata.HJI Most operating rooms haveat least one of these materials present in a convenient prepac)aged form. The material is hydrated
in balanced salt solution, a rectangle of material #approimately 2Pmm larger and wider than the
trabeculectomy flap$ is cut out, and the cover is sutured into place, with at least one =0*0 nylonsuture to each corner of the material. 3ostoperatively, these sutures may be lysed using an argon
laser to increase drainage as desired, so secure closure on the operating table is warranted # +ig.
2J>*K $.
4%T;1:U 6:.
1specially in pseudopha)es after complicated cataract etraction or in apha)es, the surgeon may
encounter vitreous prolapse after the iridectomy. /areful clearance
+igure 2J>*J ;epair of disinserted flap.
+igure 2J>*K onor dura flap to replace disinserted flap.
from the sclerotomy of all vitreous is )ey because vitreous is a very effective sclerotomy plug.
limited vitrectomy with a combination of scissors dissection, cellulose sponge, and automated
vitrector should be performed. The goal is no vitreous present at the sclerotomy when chec)edusing a cellulose sponge. 1tra care is re5uired in these eyes to avoid a postoperative shallow
anterior chamber because this may bring further vitreous forward to bloc) the sclerotomy.
Therefore, consider the placement of etra releasable sutures #or sutures that may be lasered$ to
prevent early overdrainage.
%NT;:31;T%41 611%ND.
1cess bleeding from the iris root andQor ciliary body after iridectomy must be addressed because
blood may also cause sclerotomy bloc)age. /old balanced salt solution, dripped slowly over
several minutes, with or without low*concentration epinephrine added, usually results in stoppageof the bleeding. lternatively, a monopolar wet*field 2>gauge cautery may be applied carefully to
the bleeding vessel if the site can be visuali&ed. %t is rare for these areas to rebleed postoperatively,
but if they do, it is usually in situations with hypotonyE again, a tight closure with etra releasable
-
7/24/2019 93493980 Degenerative Myopia
39/49
sutures is considered. 4iscoelastic material can be left in the eye at the conclusion of surgery to act
as a FtamponadeG and also to help avoid postoperative hypotony.
uprachoroidal hemorrhage #/'$ is the other type of intraoperative bleeding. %n these cases theeye should be closed as 5uic)ly as possible. voidance is paramount because an epulsive
=?=2
/' is disastrous. 3reoperative intravenous mannitol #=00Pml of 20- solution over =K minutes$,
with +oley catheter placement, may be considered in eyes that undergo trabeculectomy with apreoperative %:3 \J0Pmm'g #K.>P)3a$. Theoretically, less chance eists of /' if eye pressure at
the time of internal sclerotomy does not suddenly drop from JKPmm'g #?.0P)3a$ to &ero. %n
addition, the paracentesis may be performed earlier to decompress the eye gradually prior to
internal bloc) removal.
/':;:%6 1++U%:N.
Usually effusions develop postoperatively, not intraoperatively. 'owever, patients who have
turge*eber syndrome or mar)edly elevated episcleral venous pressure may develop effusions
intraoperatively. Their occurrence is signaled by sudden anterior chamber shallowing.Management consists of drainage via inferior linear sclerotomies, located KA?Pmm from the
limbus. %f the plan is to carry out surgery on the second eye of a patient who has developed
intraoperative choroidal effusions in the first eye #the disease is bilateral$, placement of apreliminary posterior sclerotomy prior to internal bloc) removal may be considered.
1arly 3ostoperative /omplications
UN1;;%ND1.
%n the early postoperative period, initial underdrainage, not associated with sclerotomy bloc)age, is
addressed effectively by se5uential release of scleral flap sutures. %f so*called permanent sutureshave been placed, the =0*0 nylon may be lysed with the argon laser and a 'os)ins #or ;itch$ lens.
HKI 9rypton red #or blue*green argon$, K0PWm spots, at >00Pm are usually effective. ;arely, a
nylon suture cannot be visuali&ed, secondary to overlying subcon!unctival hemorrhage or thic)
TenonOs tissue. To avoid this occurrence, place at least half of the scleral flap sutures using aFreleasableG*suture techni5ue. H?I This involves tying the suture with a slip )not that may be
released easily with a pull on the corneali&ed free suture end # +ig. 2J>*? $. ecauseendophthalmitis has been reported to develop from a freely moving, corneali&ed releasable suture,the eternali&ed suture end must be buried in clear cornea.H7I The superficial unburied segment of
the suture is epitheliali&ed 5uic)ly, which decreases ris) of endophthalmitis and still allows the
surgeon easy assess.H
-
7/24/2019 93493980 Degenerative Myopia
40/49
ali5uot of a5ueous, which lowers %:3. Donioscopy is recommended to chec) that the internal
sclerostomy is not bloc)ed by vitreous, iris, and so forth.
bloc)ed sclerotomy is handled differently. %f fibrin or blood bloc)s outflow, tissue plasminogenactivator may be helpful.HLI H=0I
+igure 2J>*? ;eleasable sutures #arrow$.
oses of ?A2KPWl have been in!ected into the anterior chamber safely, with resumption of flow
through the sclerotomy. ecause recurrent bleeding is a ris) with tissue plasminogen activator use,lower doses, ?A=2PWl, are now recommended. lso, fibrin fre5uently recurs unless high*dose
corticosteroids, topical, subcon!unctival, andQor oral, are used to reduce inflammation.
T'1 '66: NT1;%:; /'M1;.
%f a shallow anterior chamber is present, the reason for shallowingSoverdrainage or some otherprocessSmust be ascertained. :verdrainage is associated with low %:3, which usually results
from inade5uate scleral flap closure #with a high bleb present$ or from a bleb lea) #no or low bleb
present$.
:verdrainage with no bleb lea) can be tedious to manage. %f the bleb is high and no corneal*lenstouch or F)issingG choroidal effusion occurs, observation with cycloplegic prescription is
appropriate. 'owever, if anterior chamber shallowing is progressive, early placement of an
oversi&ed, bandage soft contact lens may help to prevent later, more difficult problems.H==I H=2Iuch lenses seem to limit ecessive bleb etension andQor ecess bleb transcon!unctival a5ueous
flow # +ig. 2J>*7 $. Usually, their use may be discontinued after =A2 wee)s. lternatively, a
immonOs shell may be applied to the eye. The shell has a plate that can be positioned over the
sclerotomy site for maimum tamponade. 'owever, patients may tolerate it poorly, and dailyocular eamination is re5uired. lso, corneal epithelial defects occur fre5uently.
nother option some surgeons use in these cases is gentle pressure patching, in which pressure is
applied directly over the trabeculectomy flap to limit outflow. :ne concern with this option is that,
when the patient loo)s up #or ehibits ellOs phenomenon, with sleep$, the pressure patch maytransfer pressure over the cornea, which results in lens*corneal touch. ometimes, in!ection of
viscoelastic material into the anterior chamber may provide sufficient time #2JAJ< hours$ to allowthe eye to Fcatch upG with itself.H=>I e have found greater viscosity viscoelastic to be particularlyuseful in such cases. This is best attempted early, rather than late, in the course. +inally, if
overdrainage continues with the development of choroidal effusions that touch, or of lens*corneal
touch, the surgeon may need to return the patient to the operating room for further flap closure,anterior chamber reformation, and effusion drainage.
-
7/24/2019 93493980 Degenerative Myopia
41/49
%nitial overdrainage with bleb lea) is fre5uently the result of a buttonhole missed at the time of
surgery. 3ostoperatively, a buttonhole is far more difficult to manage. s already noted, suture
repair at this time is often ineffective, especially if intraoperative antimetabolites were used andQorthe con!unctiva is cystic or ecessively thinned. uturing at this time may result in a larger hole.
3atching, bandage soft contact lenses, and immonOs shell may be used, with variable results. The
surgeon must watch the bleb carefully because the preceding FsolutionsG often fail to
+igure 2J>*7 =7Pmm contact lens compresses an overdraining bleb. 1dge of bandage contact
lens indicated by arrows.
=?=>
seal the lea) and only act to eacerbate episcleralQcon!unctival healing and adhesion. :theralternatives include autologous fibrin tissue glue,H=JI autologous blood in!ection #see +ig. 2J>*< $,
H=KI H=?I H=7I and cyanoacrylate glue with contact lens application. H=
-
7/24/2019 93493980 Degenerative Myopia
42/49
pupillary bloc) be ruled out. :nce pupillary bloc) is ecluded, the surgeon must eamine for the
presence of an /', which is more li)ely to occur in elderly, vitrectomi&ed, apha)ic, hypotonous
eyes. Usually, diagnosis is made easily by indirect ophthalmoscopy, with observation of thecharacteristic dar) choroidal swellings and the patientOs history of pain, nausea, and vomiting. %f
ophthalmoscopy is impossible, a *scan ultrasound eamination is carried out # +ig. 2J>*L $. %f
/' is diagnosed, therapeutic options include observation and corticosteroid prescription if thepatient is not too uncomfortable and there is no choroidal or lens*corneal touch. gain, K*
fluorouracil in!ections may be considered to prevent scarring of the sclerotomy while the /'
resolves. :therwise, it may be best to return the patient to the operating room for evacuation of the/'. This is best accomplished no sooner than postoperative day 7A=0, at which time clot lysis
has usually begun, which allows easier /' drainage.
nother cause of a shallow anterior chamber, with associated high %:3, is a5ueous misdirection.
:nce called malignant glaucoma, it is indeed a malignant process to treat. 5ueous misdirection
+igure 2J>*< 3eribleb autologous blood in!ection for lea).
#as discussed in /hapter 22L $ is the syndrome characteri&ed by mar)ed anterior displacement of
the lens*iris diaphragm with a high %:3, presumably as a result of trapped misdirected posterior
a5ueous. %f prompt treatment is initiated, perhaps K0- of mild cases resolve with intensivecycloplegic therapy #i.e., atropine =-, one drop every K minutes for a total of three drops, four
times a day$. lso, to relieve the buildup of what is believed to be misdirected a5ueous trapped
behind the vitreous face, many surgeons recommend a5ueous suppressants andQor osmotics. :ther
useful medical ad!uncts include phenylephrine 2.K- four times a day and prednisolone acetateevery 2 hours for inflammation. %f this is unsuccessful and the patient is apha)ic or pseudopha)ic,
laser therapy is an option.
+inally, although rare, anterior ring choroidal effusion has been described as a cause of shallowanterior chamber associated with high %:3.H=LI *scan confirms this diagnosis.
/':;:%6 1++U%:N.
lthough classical posterior choroidal effusions often occur in con!unction with a shallow anterior
chamber and low %:3, they may also occur in eyes that have full*depth chambers and low %:3s.
Management usually consists of cycloplegia, topical corticosteroids, and observation. s long asthe effusions do not touch, drainage is not re5uired. %f touch does occur centrally, because of the
danger of retinal adhesion formation, many surgeons choose to perform effusion drainage via
posterior sclerotomies inferiorly. The scleral flap may be revised at the time of choroidal drainageto prevent further hypotony and a recurrence of the effusions. everal permanent or releasable
sutures may be enough to reduce lea)age in the short term.
/:;N16 13%T'16%:3T'C.
-
7/24/2019 93493980 Degenerative Myopia
43/49
%n this era of antimetabolite use, an increased incidence of corneal epithelial toicity and even
defects occurs after K*fluorouracil in!ections. 4ery early temporary punctal occlusion using
collagen plugs optimi&es the corneal wetting. 3reservative*free tears are helpful. :ne group alsoreported that bandage contact lens application increased comfort and decreased inflammation.H20I
6ate 3ostoperative /omplications
6T1 61 +%6U;1.
6ate bleb failure may result from heavy vasculari&ation and healing around the bleb. igital
pressure applied by the patient to the inferior globe through the inferior lid may be useful in suchcases, as this helps maintain flow through the drain and )eeps the subcon!unctival space epanded.
%f this is insufficient, needling revision of the bleb may reestablish effective filtration. The needling
process alone rarely establishes long*term filtration in eyes not eposed to antimetabolites.'owever, if needling is followed with K*fluorouracil in!ections,
+igure 2J>*L *scan of suprachoroidal hemorrhage following trabeculectomy.
=?=J
+igure 2J>*=0 Neodymium"yttrium*aluminum*garnet laser bleb remodeling for bleb lea).
#/ourtesy of Mary 6ynch, M.$
up to an
-
7/24/2019 93493980 Degenerative Myopia
44/49
6T1 61 619.
%nitial management of these lea)s involves patching, a5ueous suppressants, and antibiotics.
dditional management includes modalities already referred to, such as bandage contact lenses,autologous fibrin or blood, and glue. Trichloroacetic acid application and carefully applied
cryotherapy may also be attempted. %f these modalities fail and further management is feltnecessary, neodymium"yttrium*aluminum*garnet laser bleb remodeling may be tried.H2>I The laser
is tuned to the continuous*wave multimode, carefully retrofocused =.0Pmm behind the bleb to theunderlying sclera, and then applied in a grid pattern #>.0PQshot$ over the bleb area # +ig. 2J>*=0 $.
%nflammation and discomfort may be intense, but up to *== $. The )ey here isanalysis of the vitreous response. %f the vitreous is 5uiet, prompt treatment with hourly topical
antibiotics may save the bleb and the eye. Topical corticosteroids after J< hours of treatment are
useful to treat the inflammation. 'owever, if endophthalmitis is diagnosed with vitreousinvolvement, intravitreal cultures and antibiotics are re5uired and eye
+igure 2J>*== lebitis.
+igure 2J>*=2 %ntrableb in!ection of autologous blood for hypotony.
salvage is rare. :rganisms fre5uently seen in these eyes include hemophilus, streptococci, andstaphylococci. Thus, coverage is best initiated with fortified topical cefa&olin or vancomycin and
tobramycin. lternatively, topical fluoro5uinolones, perhaps in combination with systemicfluoro5uinolone prescription, may cover many of these cases. %ntravitreal antibiotic in!ections of
choice are vancomycin and ami)acin.
6T1 'C3:T:NC.
-
7/24/2019 93493980 Degenerative Myopia
45/49
ntimetabolites have introduced a somewhat new entity, late hypotony, to the list of late
postoperative trabeculectomy complications. hereas an %:3 ]KPmm'g #]0.?7P)3a$ on a long*
term basis used to be unheard of, now such eyes are not infre5uent. Most commonly, the history isof high*dose mitomycin use with loose scleral flap closure, although this entity has also been seen
after K*fluorouracil in!ections. /haracteristically, vision is decreased, the eyes are soft, blebs are
large, thin, and totally avascular, retinal folds are seen in the macula #with or without the aid offluorescein angiography$, retinal vessels are tortuous, and the nerve head may be swollen. Useful
treatments, as with bleb lea)s, include intrableb autologous blood in!ectionH2?I # +ig. 2J>*=2 $ and
neodymium"yttrium*aluminum*garnet bleb treatment.H2>I ometimes, a return to the operatingroom to revise the thin bleb andQor resuture the flap is indicated. donor FcoverG #as already
discussed$ may be necessary to limit a5ueous egress. lternatively, if a symptomatic cataract is
present, the cataract etraction*associated inflammation fre5uently slows filtration through bleb
healing and resolves the hypotony.H27I ome surgeons
=?=K
+igure 2J>*=> 1posure of tube in drainage seton #arrow$.
have epressed concern that if such eyes are left untreated for many months, the retinal folds maynot resolve, even after successful pressure ad!ustment. :ne report eists of such an eye, finally
successfully treated with pars plana vitrectomy and li5uid perfluorocarbon li5uid.H2*=> $, and intraocular rotation
of the tube anteriorly into cornea. Melting of the graft may be monitored if con!unctival coverage
is maintained. %f not maintained, a new graft must be placed and con!unctiva mobili&ed to cover it.The other problem, tube migration, is especially common in children and young adults. t the first
hint of corneal compromise #endothelial cell counts may be helpful$, the tube is repositioned more
posteriorly to avoid corneal failure.
-
7/24/2019 93493980 Degenerative Myopia
46/49
;1+1;1N/1
=. ;iley +, mith T, immons ;. ;epair of a disinserted scleral flap in trabeculectomy.
:phthalmic urg. =LL>E2J">JLAK0.
2. rown 4. Management of a partial thic)ness scleral flap buttonhole during trabeculectomy.
:phthalmic urg. =LLJE2K"7>2A>.
>. ;iley +, 6ima +6, mith T, immons ;. Using donor sclera to create a flap in glaucomafiltering procedures. :phthalmic urg. =LLJE2K"==7A=0>AL.
?. 9ol)er 1, 9ass M, ;ait 6. Trabeculectomy with releasable sutures. rch :phthalmol.
=LLJE==2"?2A?.
7. urchfield /, 9ol)er 1, /oo) D. 1ndophthalmitis following trabeculectomy with releasable
sutures HletterI. rch :phthalmol. =LL?E==J"7??.
-
7/24/2019 93493980 Degenerative Myopia
47/49
=0. Tripathi ;/, Tripathi , 3ar) 9, et al. %ntracorneal tissue plasminogen activator for
resolution of fibrin clots after glaucoma filtering procedure. m :phthalmol. =LL=E==="2J7A?A7.
=7. mith M+, Magauran ;D, oyle , etch)el . Treatment of postfiltration bleb lea)s with
autologous blood. :phthalmology. =LLKE=02"
-
7/24/2019 93493980 Degenerative Myopia
48/49
=L. ugel 3U, 'euer 9, Thach , et al. nnular peripheral choroidal detachment simulating
a5ueous misdirection after glaucoma surgery. :phthalmology =LL7E =0J"J>LAJJ
20. ec)man ;6, olins)i , Dreff 6, et al. andage contact lens augmentation of K*fluorouraciltreatment in glaucoma filtration surgery. :phthalmic urg. =LL=E 22"K?>AJ.
2=. hin ', u&ych M, 9latana 9, et al. Needling revision of failed filter blebs with ad!unctive
K*fluorouracil. :phthalmic urg. =LL>E2J"2J2A"=700AK.
2J. ilson M;, 9otas*Neumann ;. +ree con!unctival patch for repair of persistent late bleb lea).
m :phthalmol. =LLJE==7"K?LA7J.
2K. uton N, 6avery 9T, 6iebmann M, et al. ;econstruction of filtering blebs with free
con!unctival autografts. :phthalmology. =LLJE=0="?>KAL.
2?. ise . Treatment of chronic postfiltration hypotony by intrableb in!ection of autologous
blood. rch :phthalmol. =LL>E==="0.
27. oyle , mith M+. 1ffect of phacoemulsification surgery on hypotony following
trabeculectomy surgery. rch :phthalmol. 2000E==
-
7/24/2019 93493980 Degenerative Myopia
49/49
2