600: Impact of number of cesareans on placental abnormalities and maternal morbidity: a systematic...
-
Upload
nicole-marshall -
Category
Documents
-
view
216 -
download
1
Transcript of 600: Impact of number of cesareans on placental abnormalities and maternal morbidity: a systematic...

lwiwg
lrapwAcL
agldg
G
o
C
o
lwiwp
(cw0vC
os
C
a
l
nnTdwoc
bemistp
www.AJOG.org Epidemiology, Global Maternal-Fetal Public Health, Infectious Disease, Intrapartum Fetal Assessment, Operative Obstetrics Poster Session IV
STUDY DESIGN: This is a retrospective cohort study of birth recordsinked to hospital discharge data for all live born singleton infants �37eeks gestation born to African American or Caucasian Missouri res-
dents from 2000-2006. We excluded major congenital anomalies andomen with diabetes or chronic hypertension. Gestational weightain categories were chosen as �10 lbs and �40 lbs as these amounts
are outside of the 2009 Institute of Medicine guidelines for weight gainin pregnancy. GWG of 10-40 lbs served as the referent category.RESULTS: There were 625,745 births meeting study criteria. GWG �40bs was associated with an increased incidence of fetal macrosomia,egardless of race or maternal BMI (table). GWG �10 lbs was associ-ted with an increased risk of low birth weight and GWG �40 wasrotective against LBW for both Caucasian and African Americanomen of all BMI. Overweight and obese Caucasian women, but notfrican American women, with GWG � 10 lbs had significantly de-reased risk of fetal macrosomia and significantly increased risk ofBW.
CONCLUSIONS: Weight gain during pregnancy is significantly associ-ted with BW. All women, including normal weight women, whoained more than 40 lbs during pregnancy were significantly moreikely to deliver macrosomic infants. Further studies are needed toetermine the ideal weight gain during pregnancy for optimal fetalrowth.
Table. Risk of macrosomia for women who gain<10 lbs or > 40 lbs across BMI categories
Caucasian African AmericancOR (95% CI) cOR (95% CI) aOR
†(95% CI)
WG �10 lbs.................................................................................................................................................................................
18.5-24.9* 1.00 (0.54, 1.88) 5.18 (2.05, 16.46) 0.44 (0.38, 0.50).................................................................................................................................................................................
25-29.9* 0.41 (0.26, 0.65) 0.56 (0.14, 2.3) 0.48 (0.42, 0.54).................................................................................................................................................................................
� 30* 0.34 (0.27, 0.44) 0.36 (0.13, 1.00) 0.46 (0.40, 0.53)..........................................................................................................................................................................................
GWG �40 lbs.................................................................................................................................................................................
18.5-24.9* 2.95 (2.71, 3.20) 5.47 (3.62, 8.28) 0.48 (0.43, 0.53).................................................................................................................................................................................
25-29.9* 2.64 (2.41, 2.89) 3.97 (2.90, 5.42) 0.51 (0.46, 0.57).................................................................................................................................................................................
� 30* 2.18 (1.96, 2.42) 2.23 (1.57, 3.17) 0.49 (0.45, 0.54)..........................................................................................................................................................................................
* BMI (kg/m2)† Adjusted for maternal age, average education, nulliparous, Medicaid, adequate prenatal
care, smoking, maried, male gender, prior C-section, primary elective C-section.
599 The effect of race and maternalbesity on perinatal outcome
Nicole Marshall1, Camelia Guild2, Yvonne W.heng3, Aaron Caughey1, Donna Halloran2
1Oregon Health & Science University, Portland, OR, 2Saint Louis University,Saint Louis, MO, 3University of California, San Francisco, San Francisco, CAOBJECTIVE: To determine the effect of race and obesity on perinatal
utcomes.STUDY DESIGN: This is a retrospective cohort study of birth recordsinked to hospital discharge data for all live born singleton infants �37eeks gestation born to African American or Caucasian Missouri res-
dents from 2000-2006. We excluded major congenital anomalies andomen with diabetes or chronic hypertension. Obesity was defined asre-pregnancy body mass index � 30 kg/m2.
RESULTS: There were 625,745 births meeting study criteria. 28.1%25,727) of African American mothers and 20.0% (111,596) of Cau-asian mothers were obese. Infants of obese African American womenere significantly less likely to be macrosomic (1.2% vs. 2.5%, aOR.39, 95% CI 0.34, 0.45) and more likely to be low birth weight (3.4%s. 1.8%, aOR 2.26, 95% CI 2.14, 2.38) compared to infants of obeseaucasian women (table).
CONCLUSIONS: Obesity-related maternal and neonatal complicationsf pregnancy, especially birth weight, vary by race and should be con-
idered in counseling obese pregnant women.Supplem
Table. Obstetric outcomes in obese women by race
AfricanAmerican CaucasianN % N % aOR
†(95% CI) p-value
esarean delivery 8294 32.2 41730 37.4 1.02(0.98, 1.05) 0.3953..........................................................................................................................................................................................Preeclampsia 1952 7.6 9163 8.2 1.11 (1.06, 1.16) �.0001..........................................................................................................................................................................................Macrosomia 309 1.2 2809 2.5 0.39 (0.34, 0.45) �.0001..........................................................................................................................................................................................Low Birth Weight 880 3.4 2006 1.8 2.26(2.14, 2.38) �.0001..........................................................................................................................................................................................Birth Trauma 430 1.7 2065 1.8 0.89 (0.83, 0.96) 0.0026..........................................................................................................................................................................................Hypoglycemia 367 1.4 1770 1.6 0.80 (0.70, 0.91) 0.0008..........................................................................................................................................................................................Length of stay� 5 days
2663 10.3 10779 9.7 1.07 (1.03, 1.10) 0.0003
..........................................................................................................................................................................................Low Apgar 266 1.0 713 0.6 1.47 (1.31, 1.62) �.0001..........................................................................................................................................................................................
† Adjusted for maternal age, average education, nulliparous, Medicaid, adequate prenatalcare, smoking, married, male gender, prior C-section, primary elective C-section.
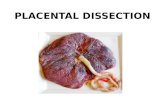
600 Impact of number of cesareans on placentalbnormalities and maternal morbidity: a systematic review
Nicole Marshall1, Jeanne-Marie Guise1
1Oregon Health & Science University, Portland, OROBJECTIVE: To determine the impact of number of prior cesarean de-iveries upon placental abnormalities and maternal outcomes.
STUDY DESIGN: This study was performed as part of a systematic re-view conducted to inform the 2010 NIH Consensus DevelopmentConference on Vaginal Birth After Cesarean: New Insights. Publishedstudies were identified from searches of MEDLINE®, Cochrane Da-tabase of Systematic Reviews, National Centre for Reviews and Dis-semination (1980 to September 2009), reference lists, and nationalexperts. English language,general population studies from developedcountries of women with one or more prior cesarean were included.RESULTS: Women with a prior cesarean delivery had a statistically sig-
ificant increased risk of placenta previa compared with women witho prior cesarean at a rate of 12 per 1,000 (95% CI: 8 to 15 per 1,000).he incidence increased with increasing number of prior cesareaneliveries (Table). Similarly, the odds of adverse outcomes increasedith increasing number of cesareans: Hysterectomy OR 3.8-18.6 for 2r more cesareans compared with 1; adhesions OR 2.5 with 2 or moreompared with none.
CONCLUSIONS: Women with multiple cesareans suffer increasing mor-idity with increasing numbers of cesareans. Women consideringlective or repeat cesarean need to be counseled about the risks ofultiple cesareans. This increased morbidity is particularly concern-
ng for rural providers who may not have the resources (e.g. bloodupply and surgical staff) to respond to these life threatening condi-ions, yet according to limited evidence this is the very group who areerforming fewer VBACs.
Considerations Rate
Placenta Previa..........................................................................................................................................................................................
General population 800/100,000..........................................................................................................................................................................................
1 Prior Cesarean 1,000/100,000..........................................................................................................................................................................................
2 Prior Cesareans 1,700/100,000..........................................................................................................................................................................................
3 or more Prior Cesareans 2,700/100,000..........................................................................................................................................................................................
Placenta Accreta..........................................................................................................................................................................................
General population 240/100,000..........................................................................................................................................................................................
1 Prior Cesarean 319/100,000..........................................................................................................................................................................................
2 Prior Cesareans 570/100,000..........................................................................................................................................................................................
3 or more Prior Cesareans 2,400/100,000..........................................................................................................................................................................................
ent to JANUARY 2011 American Journal of Obstetrics & Gynecology S239