4 hemoglobin disorder
-
Upload
nayeem-ahmed -
Category
Health & Medicine
-
view
226 -
download
10
Transcript of 4 hemoglobin disorder

HEMOGLOBIN DISORDER

IRON-DEFICIENCY ANEMIA
Iron-deficiency anemia (or iron-deficiency anaemia) is a common anemia (low red blood cell level) caused by insufficient dietary intake and absorption of iron, and/or iron loss from intestinal bleeding.
Anemia occurs when a person's blood contains insufficient red blood cells. This could result if: The body does not make enough red blood cells Bleeding causes loss of red blood cells more
quickly than they can be replaced

Iron deficiency anemia:
Other name: microcytic hypochromic anemiaMost commonest form of anemia in underdeveloped countryHigh incidence of iron deficiency anemia occurs in women during the reproductive life
Etiology/cause:
Iron deficiency anemia may result from:•Inadequate iron intake•Impaired absorption of iron•Loss of blood/chronic blood loss•An increase physiological demand for iron

1.In adult males and post-menopausal women (pathological blood loss)Hookworm infestationBleeding peptic ulcerCancer of stomachBleeding pilesColon cancer
2.In female in reproductive period of lifeMenstruation (excessive menstrual bleeding)Frequent pregnancyLactation
3.Infant and children Dietary deficient in proportion to body
requirement

Megaloblastic anemia:
Megaloblastic anemia is characterized by formation of morphologically abnormal nucleated red cell precussor called megaloblasts in the bone marrow due to megaloblastic erythropoiesis Cause:
1. Deficiency of VitB12 2. Deficiency of folic acid

Cause of VitB12 deficiency
1. Inadequate intake of VitB12 (nutritional deficiency): it occurs among strict vegetarian
2. Decrease absorption: a.Gastric cause: Due to deficiency of intrinsic factor I. Gastric atrophy: Occurs as in Addisonian
pernicious anemia II.After gastrectomy b. Intestinal cause
I.Tropical sprue II.Celiac disease II.Lesion of small intestine
3.Drugs: (Rare)Paraminosalicyclic acidMetformin

Cause of folic acid deficiency:
1.Inadequate intake (nutritional deficiency): Common in poor, pregnant women
2.Increased requirement: DuringPregnancyPuerperiumCarcinoma (malignancy)Leukemia
3.Impaired absorptionTropical sprueCeliac disease
4.Hepatic cirrhosis
5.Drugs: Drugs like folate antagonistPhenytoinTrimethprim

Cardinal manifestation of
1.VitB12 deficiency:Macrocytic (megaloblastic) anemiaGlossitisSubacute combined degeneration of spinal cord and peripheral
neuropathy
2.Folic acid deficiency:
Macrocytic (megaloblastic) anemiaGlossitisPeripheral neuropathy (occasional) (subacute combined
degeneration of spinal cord does not occur)

Pernicious anemia
Addisonian pernicious anemia is a VitB12 deficiency megaloblastic anemia Pathogenesis:
Pernicious anemia occurs due to failure of secretion of intrinsic factor (IF) by the stomach due to permanent gastric atrophy
Deficiency/absence of intrinsic factor
VitB12 present in food is not absorbed
VitB12 deficiency
C/F of megaloblastic anemia

Aplastic anemiaAplastic anemia is a condition where bone marrow does not produce sufficient
new cells to replenish blood cells. The condition, as the name indicates, involves both aplasia and anemia. Typically, anemia refers to low red blood cell counts, but aplastic anemia patients have lower counts of all three blood cell types: red blood cells, white blood cells, and platelets, termed pancytopenia.
Classification: 1.Primary or idiopathic aplastic anemia: Cause unknown 2.Secondary aplastic anemia:
Cause: Drugs: Which cause bone marrow depression
Cytotoxic drugsPhenylbutazoneChloramphenicol
Chemicals: Hairdye, benzene, DDTIonizing radiation: Radiotherapy, diagnostic radiologyViral hepatitis
3.Other types of aplastic anemia a. Fanconi’s anemia: A familial aplastic anemia b.Pure red cell aplasia

Clinical feature:
Clinical feature is aplastic anemia comprises the features of anemia, neutropenia, thrombocytopeniaAnaemia
Thrombocytopenia: Bleeding manifestations Cerebral hemorrhage is cause of death
Neutropenia: Infection Pneumonia and septicemia is cause of death

Pancytopenia:
Pancytopenia is the state where all three formed elements of blood are reduced i.e. there is anemia, leukopenia, thrombocytopenia Cause:
Aplastic anemiaCytotoxic agentsRadiotherapyOverwhelming infectionBone marrow infiltration: in disease like lymphoma, metastatic
carcinoma of bone, multiple myelomaHyperspleenismMegaloblastic anemia

Hemolytic anemia:
Hemolytic anemia result from an increase in the rate of red cell destruction Normal life span of red cell is 120 days In hemolytic anemia life span may be shortened to 2-3 days in extreme cases
Classification: Hemolytic anemia are classified on the basis of factors that causes hemolysis
1.Intracorpuscular cause: if the factors that cause hemolysis are inside the red cell 2.Extracorpuscular cause : if the factors that cause hemolysis are outside the red cell

Intracorpuscular defect:
When the factors causing hemolysis of red cell is inside the cell
A.Hereditary
1.Due to defect in membraneHereditary spherocytosisHereditary elliptocytosis
2. Due to defect in hemoglobin synthesis Thalassemia: Due to reduced synthesis of alpha or beta chain of globin
Haemoglobinopathies: Due to synthesis of structurally abnormal globin, HbS, HbC, HbD 3.Due to deficiency of enzyme in red cell
Deficiency of glucose-6-phosphate dehydrogenase enzymeDeficiency of enzyme of Embden-Meyerhoff pathway (pyruvate kinase)
B.Acquired: Membrane defect. E.g. paroxysmal nocturnal hemoglobunuria (PNH)

Extracorpuscular defect:
When the factor causing hemolysis of red cell is outside the cell
1. Immune dependent:a.Autoimmune hemolytic anemiab.Hemolytic disease of new born (erythroblastosis foetalis)c.Incompatible blood transfusiond.Drug induce hemolytic anemia
2.Non-immune dependent a.Mechanical hemolytic anemia
Cardiac hemolytic anemia: Prosthesis valueMicroangpathic hemolytic anemiaMarch hemoglobuinuria
b. Infection e.g. malarial parasite c. Sever burn, shake, and spider bite d. Drug and chemical e.g. lead poisoning

Disorders of hemoglobin
Hemoglobin disorders are genetically determined disorders
Thalassaemias: These occur due to reduction in the rate of synthesis of one or more types of polypeptide chain of hemoglobin
Haemoglobinopathies: These are disorders in which structurally abnormal hemoglobin are produced

Thalassaemias: These are inherited disorder in which there is inadequate production of chains or chains (polypeptide) of hemoglobin
Types
A. -thalassaemia: There is inadequate production of -chain and thereby reduction of Hb A
Classification of thalassaemia:
1.On extend of reduction of chain synthesis a. thalassaemia: There is complete absence of -chain synthesis b.+ thalassasemia: There is incomplete reduction of -chain synthesis 2.On the basis of clinical manifestation:
a. thalassasemia major:There is total suppression of chain synthesisIt is homozygous stateIt is usually a severe disease
Death may occur during childhood b. thalassasemia minor:
Suppression of chain synthesis is much less severe It is a heterozygous state It is mild or asymptomatic condition
c. thalassasemia intermedia:

Clinical feature of thalassasemia
Mongoloid faciesHepatomegalySplenomegalySlow growth in childhoodAnemiaRecurrent infectionSkin pigmentation

B. thalassasemia:
There is defective synthesis of chain with reduction in amount of HbA, HbA2, and HbF
Types of thalassasemia
1. thalassasemia trait: It is asymptomatic
2.Hemoglobin-Bart’s Hydrop foetalis In fetus an excess production of chain is produced (absence of chain)
4 called Hb-Bart’sAffected infants are either born dead or die within few hours of birthGross edema, ascites, and hepatosplenomegaly are present
3.Hemoglobin-H disease: In adult an excess production of chain occurs (absence of chain) form
4 called Hb-H. There is moderate to severe anemia

Hemoglobinopathies:
These are condition associated with abnormal hemoglobin
The common abnormal hemoglobin HbS: (tropical Africa)-------- α2 β2 6 glu--------val HbE: (south east Asia)------ α2 β2 26 glu--------lys HbC: (tropical Africa) ------ α2 β2 6 glu-------- lys HbD Punjab: (India)--------- α2 β2 121 glu--------gln Glu: glutamic acid, val: valine, lys: lysine, gln:glutamine

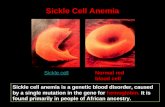
SICKLE CELL ANEMIA

DEFINITIONSickle Cell Disease:
A genetic hemoglobinopathy
Results in deformation, increased rigidity, and destruction of RBCs
Vasocclusive and pro-inflammatory disease process
Chronic multiorgan system disease Severe morbidity and early mortality

What is Sickle Cell Anemia (SCA)? First described in Chicago in
1910 by James Herrick as an inherited condition that results in a decrease in the ability of red blood cells to carry oxygen throughout the body
Sickle red blood cells become hard and irregularly shaped (resembling a sickle)
Become clogged in the small blood vessels and therefore do not deliver oxygen to the tissues.
Lack of tissue oxygenation can cause excruciating pain, damage to body organs and even death.

DEFINITION Autosomal recessive genetic disease:
β-globin gene (chromosome 11q) mutation GAGGTG at 6th codon
Glutamic Acid Valine at the 6th amino acid along the β-globin chain
α2β2 = normal hemoglobin
α2βS = heterozygote = Sickle trait
α2S2 = homozygous recessive = Sickle cell disease

HISTORY OF SICKLE CELL DISEASE Known by many African tribes for centuries Earliest historical report -- 1670 in Ghana African cultures often named illness to describe the
sounds of moaning made by the victims Tribal names:
Ahututua – Twi tribe Chwecheechwe – Ga tribe Nuidudui – Ewe tribe “Obanje” – “Children who come and go”

PATHOPHYSIOLOGY Inheritance of mutated hemoglobin β-globin chain Mutation GAG GTG at 6th codon Glutamic acid Valine at 6th AA α2βS = heterozygote = Sickle trait α2S2 = homozygote recessive = Sickle cell disease
Additional variants: Hgb S - β+ thalassemia Hgb S - β0 thalassemia Hgb S - α thalassemia Hgb SC Hgb SD Hgb SE Hgb S-HPFH (Hereditary Persistance of Fetal Hgb)

PATHOPHYSIOLOGY
1. Deoxygenation HgbS protein conformational change
2. Hydrophobic Valine exposed at molecular surface
3. Val6 of B2 chain of 1st Hgb S chain forms hydrophobic bond with Phe85 and Leu88 of a 2nd Hgb S B1 chain
4. Pairing Hgb S monomers polymerize to form Hgb S chains
5. Hgb S polymers precipitate in RBCs as long, rigid fibers
Sickling Mechanism

PATHOPHYSIOLOGY
HgbS fibers are rigid
Hgb S fibers deform RBC membranes
Membrane disruption exposes transmembrane proteins and lipids that are pro-inflammatory
Progressive sickling makes cells dense and inflexible

Sickle Cell Formation Microvascular vasoocclusion Chronic Inflammation Multiorgan System Disease
Hallmarks of Hallmarks of Sickle Cell PathophysiologySickle Cell Pathophysiology

PATHOPHYSIOLOGYFactors that Promote Hgb S polymerization:
Low pO2 / Hypoxia
Prolonged “Delay Time” – time RBC spends in microcirculation
Low pH
High Hgb S concentration Genotype-dependent Cellular “Dehydration”
Volume depletion (total body) Sickling Activation K+ / Cl- cotransporter and Gardos Ca2+- activated K+ efflux channels ion and water efflux
Low Hgb F concentration αα22γγS:S: gamma globin chains bind Hgb S chains and inhibit Hgb S polymerization, thus countering sickling process

PathophysiologyPathophysiology

Sickle cell anemia: (Summary)
In sickle cell anemia RBC contains Hb S
•Sickle cell anemia is present in 0.3-1% of West Africans and American blacks
•When Hb S is exposed to low concentration of oxygen it precipitates into long crystal inside red blood cell. This crystal elongates the cell and gives it the appearance of being sickle rather than a biconcave disc.•The precipitated hemoglobin also damages the red cell membrane , so that the cell becomes highly fragile Sickle of red cells is initially reversible when oxygenation occurs but later become permanent irreversibly sickle due to membrane damage
•Red cell will begin to sickle at an oxygen tension of 50-60 mmHg, which is usually found in microcirculation but it the flow is rapid, they resume normal shape when they are swept back to area of circulation where the oxygen tension is higher
•But if the flow rate is slow and the cells are delayed in areas where oxygen tension is low, the cell sickle and this sickle cell greatly increase blood viscosity with further slowing of circulation

Effect: These sickle cells cause great
increase in blood viscosity and block small blood vessels impairing flow and causing ischaemia and infarction of tissue
Repeated sickling-unsickling of red cell cause loss of fragment of red cell membrane, which cause red cell to be fragile, so easy hemolysis occurs
leading to anemia

Effect of anemia
A. In anemia viscosity of blood decrease (due to decrease in red cells)
Decrease viscosity
Decrease the resistance to blood flow in peripheral vessels
Increase quantity of blood flow to tissue
This increases quantity of blood is returning to heart from these tissues

B.Anemia cause hypoxia to tissue
Decrease amount of oxygen transported by blood to tissue
Hypoxia
Dilates peripheral blood tissue
Increase flow of blood to tissue
Increase venous return (blood to heart)
Thus these two effects cause
Increase venous return to heart
Increase cardiac output
i.e. increase workload on the heart

Polycythemia: Increase in number of red cells above normal range per unit volume of
blood Classification: 1. True or absolute polycythemia 2. Relative polycythemia

1.True or absolute polycythemia: There is an increase in total red cell volumeTypes
A.Polycythemia Vera (erythremia): When there is pathological proliferation of red cell without erythropoietin stimulus, then it is called polycythemia vera Red cell count may be 7-8 million and hematocrit 60-70% Causes:
Bone marrow tumorX-ray radiation
Here WBC and platelet production also increase
B.Secondary polycythemia (erythrocytosis): When the polycythemia occurs in response to increase erythropoietin production. Cause of increase erythropoietin production
I .Secondary to hypoxiaHigh altitudeCongenital heart diseaseChronic pulmonary disease like emphysema, pulmonary fibrosis
II.Other factors that cause increase erythropoietin productionNon-neoplastic kidney disease: Renal cystTumors: Kidney, liverOvarian tumor
C.Benign familial polycythemia

2.Relative polycythemia:
Here total red cell volume is within normal range. But there is increase in RBC conc or increase hematocrit due to hemoconcentration (loss of plasma portion)
Cause:DehydrationRedistribution of body fluidAdrenal insufficiency: Increase loss of electrolyte—increase loss
of fluid

Effect of polycythemia
1.On circulatory systema. Due to increase in viscosity of blood in polycythemia
Blood flow through blood vessels is sluggish
Decrease venous return to heart
b.On the other hand, polycythemia increases volume of blood
Increase venous return
So actually cardiac output in polycythemia is not far from normal because these two factors more or less neutralize each other
2.On arterial blood pressure: Arterial pressure is normal in most people with polycythemia although in about 1/3 of them pressure increase Cause:
Because blood pressure regulating mechanism can maintain it up to certain limits

3.On skin color:
Color of skin depends to great extent on quantity of blood in subpapillary venous plexus
In polycythemia vera, quantity of blood in this plexus is greatly increasedBecause the blood passes sluggishly through skin capillaries before entering the venous plexus, a larger than normal quantity of Hb is deoxygenated before the blood enters the plexus. The blue color of deoxygenated Hb masks the red color of oxygenated Hb.
Therefore person with polycythemia vera ordinarily has a ruddy complexion with a bluish (cyanotic) tint to skin
Polycythemia vera Secondary polycythemia
Increased red cells, increase WBC, increased platelets
Increased only red cells
Erythropoietin concentration in blood is normal
Erythropoietin concentration in blood is increased

Jaundice:
Jaundice is defined as yellow discoloration of skin, mucous membrane and sclera due to increase bilirubin concentration in the body fluid above normal
Serum bilirubin:Normal: 0.3-1 mg/dl (5-17 umol/l)
Classification of jaundice:
1.Latent jaundice: Clinically, there is no jaundice but serum bilirubin is more than normal but less then 3 mg/dl
2.Clinical jaundice: Jaundice is clinically seen as yellow coloration of skin, mucous membrane, and skin when bilirubin exceeds 3 mg/dl (50 umol/l)

Types of jaundice:
1. Hemolytic or prehepatic2. Hepatocellular or hepatic3. Obstructive or cholestatic or posthepatic
Site where jaundice can be seen:
1.Sclera or eye2.Mucous membrane of mouth3.Skin4.Crease of palm and sole

Jaundice may develop due to any one of the following conditions
1.When there is excess production of bilirubin
2.When there is decrease uptake of bilirubin by liver cell
3.Impaired conjugation of bilirubin in hepatocytes
4.Impaired excretion of conjugated bilirubin through bile canaliculi

1.Hemolytic jaundice:
Hemolytic jaundice occurs due to increased breakdown of red cells which lead to increase in production of bilirubin Cause:
Hemolytic anemiaIneffective erythropoiesis: E.g. thalassaemia, pernicious anemia
Jaundice is usually mild as normal liver can excrete 6 times the bilirubin that is normally formed Bilirubin is mainly unconjugated bilirubin
2.Hepatocellular jaundice/Hepatic jaundice: This type of jaundice develops due to failure of liver to transport bilirubin into bile as a result of liver cell damage
Cause:Viral hepatitisDrugsChronic alcoholic hepatitisCirrhosis
In Hepatocellular jaundice both unconjugated and conjugated bilirubin increase

3.Obstructive or cholestatic jaundice/posthepatic jaundice:
It occurs due to obstruction of bile flow obstructive may be intrahepatic or extrahepatic
A.Intrahepatic obstruction:
Cause:Viral hepatitisDrugsAlcoholic hepatitisCirrhosisPregnancy
B.Extrahepatic obstruction: Obstruction in biliary tract. The obstruction may be in lumen, in wall, or outside the wall
In the lumen: Gallstone, wormIn the wall: Cholingitis, tumor, atresia, strictureOutside the wall: Carcinoma of head of pancreas, subhepatic abscess,
enlarged lymph node The bilirubin in serum is conjugated

Unconjugated Conjugated
Water insoluble Water soluble
Lipid soluble Lipid insoluble
Present in blood of normal healthy person
Absent in blood of normal healthy individual
Cannot pass in urine as it is not water soluble
Can pass in urine as it is water soluble
Vanden Bergh reaction indirect positive
Vanden Bergh reaction direct positive

THANK YOU!!