384: Chorioamnion membrane separation at the cervical os (moon sign) and risk of preterm premature...
Transcript of 384: Chorioamnion membrane separation at the cervical os (moon sign) and risk of preterm premature...
l
N
vtCuiet
ctuWu1
oof
J
OA
(a
sogtsPws
(ttPtp317pwCa(P
Poster Session II Clinical Obstetrics, Diabetes, Labor, Medical-Surgical-Disease, Physiology/Endocrinology, Prematurity www.AJOG.org
characteristics, including age, race, and gestational age at screening.Women with previous term deliveries had a longer mean CL in thesecond trimester compared to nulliparous women (Table, p�0.03).The incidence of short CL, however, was comparable between thegroups (p�0.99). The mean CL for women with a short cervix differedbetween the groups, but not significantly (p�0.09). Short CL re-mained comparable between the groups when defined as CL � 20mm(p�0.53).CONCLUSION: Although mean CL was slightly longer in women withprevious term deliveries, a previous term delivery is associated with asimilar incidence of short cervix in the second trimester, compared tonulliparous women. Universal CL screening for preterm birth preven-tion is reasonable even in women with previous term deliveries.
383 Can transabdominal imaging effectively screenow-risk patients for shortened cervical length?
Shirlee Jaffe Lifshitz1, Stephen Chasen1
1NY Presbyterian–Weill Cornell Medical College, Obstetrics & Gynecology,ew York, NY
OBJECTIVE: Although routine transvaginal ultrasound to measure cer-ical length is not currently recommended, there are interventionshat may improve the outcomes of pregnancies with a short cervix.urrent practice in many institutions is to perform a transvaginalltrasound (TVS) on low-risk patients only if the transabdominal
maging raises suspicion of short CL. Our objective was to assess thefficacy of abdominal ultrasound in screening for a short cervix at theime of the 2nd trimester anatomical survey.
STUDY DESIGN: We performed a prospective study of women present-ing for their anatomical survey between October 2011 and April 2012in one large academic center. Consenting patients underwent TVS forCL measurement after their cervix was imaged transabdominally.Sonographers recorded their impression of whether or not the cervixappeared short based on abdominal images prior to TVS. Sensitivityand specificity of transabdominal ultrasound were calculated for CLof 25mm, 20mm, and 15mm, which have been suggested as cutoffs forinterventions.RESULTS: 435 women consented to participate in the study. In 4.6% ofases, the sonographer indicated that the cervix appeared short based onransabdominal imaging. Sensitivity and specificity of transabdominalltrasound in detecting CLs of 25, 20, and 15mm are given in the Table.hile all patients with CL of 15mm or less would have been detected
sing transabdominal imaging as a screening test, only 3 of 9 with CL of6-25mm had a cervix that appeared short transabdominally.
CONCLUSION: Based on our data, most cases with a short cervix can besuspected based on transabdominal imaging at the time of routineanatomical survey, avoiding transvaginal ultrasound in most patients.If intervention would be offered at a CL above 15mm, however, trans-vaginal ultrasound may be warranted.
Table
S168 American Journal of Obstetrics & Gynecology Supplement to JANUARY 2
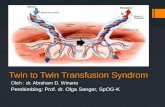
384 Chorioamnion membrane separation at the cervicals (moon sign) and risk of preterm premature rupturef membranes (PPROM) after operative fetoscopyor twin-twin transfusion syndrome (TTTS)
Shivani Patel1, Lisa Korst1, Arlyn Llanes1, Richard Lee1,oseph Ouzounian1, Ramen Chmait1
1Keck School of Medicine, University of Southern California, Department ofbstetrics and Gynecology, Division of Maternal-Fetal Medicine, Losngeles, CA
OBJECTIVE: To determine if chorioamniotic membrane separationMS) from the internal cervical os, the so-called moon sign, is associ-ted with an increased risk of PPROM after laser surgery for TTTS.
STUDY DESIGN: The study included all TTTS patients treated with laserurgery (2006-2012). MS was diagnosed by review of pre- and post-perative endovaginal ultrasound images. The degree of MS wasraded (Grade I: only over the internal os; Grade II: within 2 cm fromhe os; Grade III: beyond 2 cm from the os). MS before and afterurgery was tested against any PPROM, PPROM within 7 days, andPROM within 21 days. Because intrauterine fetal demise (IUFD) waseakly associated with PPROM (p�0.08), these patients underwent a
eparate analysis.RESULTS: 244 of 303 patients (80.5%) did not experience an IUFD. 3313.5%) of these had pre-operative MS, 32 (13.1%) had post-opera-ive MS, and 26 (10.7%) of these had MS both pre- and post-opera-ively. Among those with pre-operative MS, there was no difference inPROM, PPROM within 7 days, or PPROM within 21 days compared
o those without pre-operative MS. Among those with and withoutost-operative MS, the proportion with any PPROM was 34.4% (11/2) vs. 27.4% (58/212) (P�0.4067), with PPROM within 21 days was5.6% (5/32) vs. 5.2% (11/212) (P�0.0428), and with PPROM withindays was 9.4% (3/32) vs. 4.7% (10/212) (P�0.3875). Patients withost-operative MS were three times more likely to have PPROMithin 21 days of surgery (OR 3.38, 95%CI 1.09-10.48, P �0.0346).hange in grade of MS from pre- to post-operative state was notssociated with PPROM. Among patients who experienced an IUFDN�59), neither pre- nor post-operative MS were associated withPROM at any time.
CONCLUSION: In this large series, the pre-operative moon sign was notassociated with PPROM. However, post-operatively this finding wasassociated with PPROM at 21 days.
Grade III chorioamnion membraneseparation (moon sign)
013

![Minimally invasive implantable fetal micropacemaker ... · ing using ultrasound or fetoscopy [23]. Fetuses with hydrops develop fluid collections in the pleural and per-icardial spaces,](https://static.fdocuments.in/doc/165x107/5f2d761c9172f467120f31f8/minimally-invasive-implantable-fetal-micropacemaker-ing-using-ultrasound-or.jpg)