360 -- Summer 2015
-
Upload
cincinnati-childrens-hospital-medical-center -
Category
Documents
-
view
214 -
download
1
description
Transcript of 360 -- Summer 2015

F O R T H E E M P L O Y E E S O F C I N C I N N AT I C H I L D R E N ’ S
SUMMER 2015
THE SYMBIOTIC EFFECT WHAT’S INSIDE
3 New Plan Advances Our Mission
4 Why Putting Employees First Is Good for Our Patients
7 We Did It!
8 Holistic Approach Calms Patients and Caregivers
10 Schwartz Center Rounds Support Employees Through the Hard Stuff
SP20Look inside!

What came first? The chicken or the egg? You could ask the same question about the patient and employee experience. One is contingent on the other. We feel good when we make a positive difference in a patient’s life—directly or indirectly. And patients feel good when our interactions with them are competent and compassionate. In fact, some patients are so inspired by their experience here that they return as employees in their adult life, eager to give to others what was given to them.
In this issue, we look at the link between patients and employees and how important it is to support both. We also give you a glimpse of our 2020 Strategic Plan: Changing the Outcome Together (see insert). SP20 clearly recognizes the role all of us play in improving the health of children—whether we are at the bedside, in an office, a laboratory or a shuttle bus—and empowers us to be active contributors. It’s no surprise then that SP20 emphasizes the patient/employee experience through two of its five strategies—“Care” and “People.”
None of us work in a vacuum. Everything we do touches someone else. Our aim is to be more intentional in our actions to foster stronger, more productive connections that make everyone’s experience a more deeply satisfying one.
Cindy Duesing, editor
Volume 3, Issue 3 | 360° is an employee
publication of Cincinnati Children’s Hospital
Medical Center, produced by the Department
of Marketing and Communications, MLC 9012,
Cincinnati Children’s Hospital Medical Center,
3333 Burnet Avenue, Cincinnati, OH
45229-3026, 513-636-4420.
To give us your feedback or request additional
or fewer copies of this newsletter, email us at
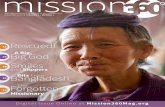
O N T H E C O V E R :
The patient/employee experience is closely
intertwined, and when all the pieces come
together in the right way, it creates a total
picture of excellent care.
Editor: Cindy Duesing
Contributors: Karyn Enzweiler,
Kate Harold, Bea Katz and Molly Vargo
Senior Art Director: Anna Diederichs
Designers: Elyse Balster and Gina Johnston
Contributing Photographers: Cindy Duesing,
Karyn Enzweiler, Tine Hofmann, Ryan Kurtz
and Mark Lyons
10202-51285 0715
THE SYMBIOTIC EFFECT

Changing the Outcome Together—that’s the name of our new 2020 Strategic Plan, which officially launched this month. The choice to use the word “changing” instead of “change” marks a subtle but important difference from our current tagline. It signifies the active collaboration we engage in every day to make Cincinnati Children’s the best it can be. The word
“together” recognizes one of the most powerful aspects of how we work and who we are. It reflects our unique “Cincinnati Children’s way,” whether this be in our interactions with colleagues, with patients and families, or with our many diverse partners internal and external to Cincinnati Children’s. It emphasizes that everyone has a vital role to play in living our vision, mission and values and that no one does this alone. Compared to where we were five years ago, we have evolved and grown as an organization and believe the new plan reflects this progress as well as our aspirations for the future.
SP20—Changing the Outcome Together builds on the strengths and successes of SP15. We asked for and received a lot of input from many of you across the medical center—faculty, research, clinical and administrative staff—as we developed it. You told us you wanted a cohesive plan that everyone could feel connected to and a concise plan that clearly identifies our priorities. We hope you will agree that this framework delivers.
In this issue, you’ll find a special insert that summarizes our plan—its five pillars and three enablers that will help us achieve our goals. Please know that there is a lot of depth and richness behind each aspect. You will learn more from your manager about the details as they pertain to you and your role. You can also find more information on CenterLink.
It’s an exciting time for Cincinnati Children’s, and each of you are an integral part of this amazing organization. You have done outstanding work to get us to this point. We hope you will feel inspired to continue exploring ways we can make a difference for patients, families, our community and the world, as we collaborate to improve health and transform care for children everywhere. Thank you!
The Performance Leadership Team
New Plan Advances Our Mission
3
Michael Fisher
Brian Coley, MD
Jennifer Dauer
Jane Garvey
Tracy Glauser, MD
Peggy Hostetter, MD
Cheryl Hoying, PhD, RN
Marianne James
Bill Kent
Uma Kotagal, MBBS, MSc
Dean Kurth, MD
Mark Mumford
Fred Ryckman, MD
Jim Saporito
Beth Stautberg
Derek Wheeler, MD
Jeffrey Whitsett, MD

At Cincinnati Children’s, our mission is to provide the best medical and quality of life outcomes, the best patient and family experience and the best value. We center our care around
patients and families, and if you ask employees why they work here, the majority of them will say they want to make a difference in the lives of those we serve.
In light of such selflessness and dedication, it may seem like heresy to say that when prioritizing between patients and employees, employees come first. But research shows that employees who enjoy a positive work experience take better care of patients and families. Conversely, bad employee experiences translate into poorer patient
outcomes. For example, hospitals with the lowest levels of employee engagement incurred an average of
$1,120,000 more in malpractice claims per year than hospitals
with the highest employee engagement, according to
one Gallup report.
“Employees are our greatest asset,” says Anne Boat, MD, patient experience officer. “They
are the single biggest driver for delivering exceptional care.”
Delivering exceptional, safe and affordable care for every child and every family, every day is one of the five pillars of the new 2020 Strategic Plan. So is realizing our full potential by engaging, inspiring and enabling all employees to make a difference. “The employee and patient experience are inextricably connected,” says
360°

5
Boat. “We need to take care of employees so they can deliver on the promise of care. We do this by empowering the people on the front lines, by setting them up for success and by removing barriers and obstacles as we discover them.”
Amy Stoll, director of management and leadership development in Human Resources, paints a picture of how employees are feeling these days, based on the most recent employee satisfaction survey and monthly pulse surveys.
“People feel as passionate as ever about working here. They are drawn to the mission, and it drives them to do great things,” she says. “But they are under more pressure than ever before. The words they use most often to describe their experience are ‘stressful,’ ‘busy,’ ‘challenging’ and ‘frustrating.’”
Our challenges include a prolonged high census; a larger number of high-acuity patients; new technology; physical space changes; organizational growth and complexity; and caring for more patients from different cultures. The management of these factors collectively stress the system.
K E E P I N G I T S I M P L EThe 2020 Strategic Plan aims to clarify our objectives and help employees take ownership of their role in achieving them. “The Care pillar needed to be really simple, so we asked what families actually want when they come here,” explains Fred Ryckman, MD, senior vice president, Medical Operations. “We narrowed it down to three things: the right care from the right team delivered in a way that’s cost-effective. This means standardizing care so we’re not doing more or less than what is needed. We have evidence-based, best-in-class practices to help us determine what the right care is. When we have these standards to guide us, we should use them. And when we don’t, we have the best expertise and skill to help us figure it out.”
Standardizing processes also means retaining tasks that add value and eliminating those that don’t. Some employees see standardization as a negative, a loss. But it’s also a plus. For example, if a nurse routinely asks each patient 10 questions in clinic and only needs the answers to five, it would save time and aggravation to just ask five questions.Says Boat, “If we can drive the unnecessary tasks out of
the system, we can spend more time interacting with patients and each other. Standardization at the highest level frees up staff to customize care for individuals.”
The past strategic plan contained measures for safety, productivity, flow, value and more. Each one was its own silo, with numerous quality improvement initiatives that overwhelmed employees.
SP20 integrates all of these individual aspects of care, which will ultimately create less work for frontline staff.
“Safety, flow and the others are still our priority,” Boat explains. “But we’re thinking of them in a more holistic way.”
O U R VA L U E S I N A C T I O NGood relationships between patients and providers contribute to overall satisfaction. Says Ryckman, “Patients and families should know their care team, whether they’re here frequently for a chronic condition or once for appendicitis. They need to feel comfortable with us and know who to call if they have a problem. Likewise, we, as providers, need to know who our patients are, to be able to track their care and do appropriate follow-up.”
Relationships between team members are even more critical.
“One of the best things we’ve done to improve the employee experience is to revamp our Core Values to make them as relatable for how we treat each other as they are for how
5
“People feel as passionate as ever
about working here. They are drawn
to the mission, and it drives them to
do great things.”

we treat patients and families,” says Stoll. “They are our guideposts. If I need to be transparent in a dif f icult situation, and I’m struggling with how to do that, the Core Values remind me to rise above the fray and do the right thing. They enable each of us to be leaders in tending to our cultural health, to say this is how we want to be as a workforce.”
Much work has been done to foster respect and professionalism over the past two years. “We are building inter-professional teams made up of doctors, nurses, dietitians, respiratory therapists, social workers and many more,” says Ryckman. “We work side by side, each of us with a different set of skills. When you do this, the hierarchy flattens out and everyone’s voice is heard. We work in a stressful environment. People get in difficult situations where, on occasion, they act poorly. But in the absence of mutual respect, we won’t make progress. So our stance is, you can’t behave disrespectfully here anymore and get away with it.” Empowerment is a critical component of SP20. “We as an institution must be clear about what we expect of employees and provide coaching and mentoring to help them be successful,” says Boat. “After that, we must trust them to do an excellent job of representing Cincinnati Children’s and not micromanage.”
As an example, Boat cites a service recovery program piloted by Same Day Surgery and the Post Anesthesia Care Unit. Staff are trained to work with dissatisfied patients and families to mitigate problems at the point they occur to avoid escalation. They are equipped with a toolkit containing meal cards for the cafeteria, gift cards for the Gift Shop, valet parking vouchers and more to give to families who’ve had an unpleasant experience.
Similarly, Guest Services has implemented an empowerment initiative where staff can offer families meal cards, a snack pack or a gift box for parents who have an unplanned overnight stay at the hospital.
“A mother was dealing with a cranky child who had endured a long wait during a sibling’s surgery,” says Boat. “A staff member offered her a snack pack for her child to stave off a meltdown. The mother said it made all the difference in the world.
“Our message to staff is that we trust your judgment to know what patients and families need, and we’re giving you the tools to address it. What’s terrible is if you see the crying toddler and have nothing to offer.”
Employees must also be empowered to meet their own needs.
“If you see a situation that needs changing, speak up,” says Stoll. “Talk with your manager. It can be hard to tell someone that something is broken. But not addressing a problem can lead to added stress. Even if you don’t care for patients directly, your bad day spreads to someone else, and that can potentially affect a patient somewhere down the line.”
Boat and her team are preparing to launch the Care Promises, a four-hour training for patient-facing employees. The promises originated from a retreat with 80 employees from across the medical center and 50 patient/family members who distilled their experiences, good and bad, into a prescribed set of behaviors that define exceptional care.
Says Boat, “I’m very optimistic about our ability to improve the patient and employee experience. Our staff is great. They have a lot of heart and want to make a difference. We have the right people. We just need to unleash their talent.”
360°
Studies show that employees who enjoy a positive work experience take better care of patients and families.

7
Our 2015 Strategic Plan yielded multiple success stories, thanks to the
purposeful and hard work of many dedicated teams. Here is a sampling
of our achievements over the past five years:
Sustained the longest run of zero Serious Safety Events in our history
Launched the Health Network by Cincinnati Children’s—now serving 37,000 children and demonstrating medical cost more than 10 percent below comparable populations
Helped reduce infant mortality by 15 percent in Hamilton County
Increased our research funding more than 46 percent (since FY09), even as NIH budgets tightened
Landed #1 US News specialty rankings for cancer, perinatal and pulmonary care
Earned Magnet re-certification
Managed a record patient census
Built and opened the new Clinical Sciences Pavilion, which will promote collaboration
and translational research
Experienced more than 20 percent growth in destination patients each year since 2010
Realized extraordinary financial success in a period of economic uncertainty
We Did It!

Emotions ran high at the graduation ceremony. There were smiles and tears as the nurses spoke about what the intensive, 16-week course in pediatric holistic nursing meant to them.
The 29 nurses in this pilot program were drawn to the course by a
desire to be more effective nurses. They were able to transform their nursing approach to care for patients and families with holistic therapeutic presence.
They had learned to think holistically about their patient’s
many needs—physical, emotional, spiritual, social, cultural and more—so
they can help patients and their families achieve a sense of wholeness and well-being.
They had explored techniques that reduce stress and distractions, and promote relaxation and
comfort, for their patients and themselves.
In a world where stress is a way of life and nurses are increasingly focused on technical skills and high-tech equipment, they had invested time in learning more about themselves and their own needs as people and caregivers, so that they can focus more intensely on their patients.
And they had applied what they learned by completing a project on their units, and by incorporating new approaches into their day-to-day clinical practice.
The course touched them deeply. “It was inspirational,” says Nishi Jani, BSN, RN, Lindner Center of Hope, who felt a sense of peace at the end of each class.
F U N D A M E N TA L S O F H O L I S T I C N U R S I N GHolistic nursing has been recognized by the American Nurses Association as a nursing specialty since 2006.
The Division of Child Life and Integrative Care includes a holistic care team, with certified holistic nurses, licensed massage therapists and other highly trained holistic health specialists.
“Ours is a unique program,” says Lois Bogenschutz, RN, BSN, clinical manager of Integrative Care. “While integrative care is becoming more common in inpatient settings, Cincinnati Children’s has the most extensive inpatient pediatric integrative care program.“
Nishi Jani, BSN, RN, Lindner Center of HOPE, shows social worker Megan Miller how to perform a yoga breathing technique to relieve anxiety.
360°

Many patients (including the tiny ones) respond well to a gentle touch.
The goal of the course, Foundations of Holistic Pediatric Nursing, was to spread knowledge of these approaches more broadly within the institution, and at the same time, to provide a work environment that is more fulfilling and balanced for nurses, explains Susie Allen, PhD, RN-BC, assistant vice president, Center for Professional Excellence.
The course was taught by Wendy Rolf, MSN, RN, CHTP, HTCP, AHN-BC, holistic health specialist III, a founding member of the holistic care team at Cincinnati Children’s. It was offered in partnership with Xavier University and met the requirements to pursue board certification as a holistic health nurse through the American Holistic Nurses Credentialing Corporation.
The 29 participants were selected from a large number of applicants. “We were looking for nurses with an interest in holistic approaches, who could be leaders in spreading the knowledge to their coworkers,” says Bogenschutz.
A D O P T I N G H O L I S T I C P R A C T I C E SMarla Layne, MSN, RN, CPN, Specialty Resource Unit, has adopted approaches that she learned in the course into her clinical practice. “We’re not certified massage therapists, but our license permits nurses to touch, and I do,” she says. She finds that her patients respond to gentle stroking, a touch to share energy, a focus on breathing.
She also has adopted practices that help her center herself. For example, she has turned the routine of
handwashing before seeing a patient into a moment of “sacred handwashing.” She explains, “I use
the time to set my mind to the task and the interaction with the patient.” Taking that moment to pay attention to her breathing and to reflect on what she’s going to do helps her feel better and prepare for her work with the patient.
“Holistic nursing is not just another added thing we do, like massage or music therapy,” Layne says. “It’s not what we do, but who we are.”
For Jani, who says she was blessed to be part of a family that’s interested in yoga and other alternative practices, the holistic nursing course validated and intensified an approach that has always been part of her life.
As a nurse at the Lindner Center of HOPE, she works with teens who may have eating disorders, depression, anxiety and negative thinking. She applied for the course because she wanted to learn new approaches for helping them.
“The medicines we give take a long time to work, and I noticed that the coping and distraction skills we were using with our patients weren’t working very well.”
She now teaches patients ancient Japanese and Indian healing practices to give them tools they can use to calm themselves when they feel anxious. One is jin shin jyutsu finger holding, a simple type of acupressure. Another is bhramri pranayam, a yoga breathing technique done while putting gentle pressure on facial nerves.
Jani has offered in-service training for her colleagues in these techniques and uses them herself when she needs to calm herself or restore her energy during a long shift.
“If I’m not taking care of myself, I’m not as effective taking care of my patients,” she says.
Having graduated from the 16-week course on April 30, the nurses are beginning to prepare for the certification exam in the Fall. Jani and Layne see themselves as instruments for spreading knowledge of holistic nursing to their colleagues and are enthusiastic about learning more.
“The things we learned are just the tip of the iceberg,” Jani says. “The course made me hungry for more knowledge.”
9
(Right) Marla Layne, MSN, RN, CPN, Specialty Resource Unit, connects with Jazaria Hughes, age 19 months, using holistic methods.

The team that brought Schwartz Center Rounds to Cincinnati Children’s recently hit a milestone: one year of putting on rounds for all employees that are focused not on the medical side of
healthcare, but on the human side. (Ed. note: Schwartz Center Rounds are a program of the Schwartz Center for Compassionate Healthcare, a national nonprofit dedicated to strengthening the relationship between patients and caregivers, i.e., everyone who cares for a patient in any way.)
A year ago in April, the first Schwartz Center Rounds session was held at the medical center on the topic of experiencing the death of a patient. At that time, the committee that put together the program was hopeful, but hesitant. “We didn’t know what to expect. We didn’t know if it would take hold,” says Rajit Basu, MD, assistant professor, Critical Care Medicine, and a member of the planning committee.
It has definitely taken hold. Over the past year, the monthly Schwartz Center Rounds have regularly packed the Sabin Auditorium to overflowing, averaging about 125 –175 attendees per session.
A S PA C E T O S H A R ESchwartz Center Rounds provide a forum for employees to share experiences with the aim of increasing understanding and compassion among employees. If you haven’t been, you’re welcome—and encouraged—to come. This isn’t like Grand Rounds where medical problems and treatments are discussed. It’s a safe place where all employees are invited to air their thoughts and gain insights from others.
“The reason for Schwartz Center Rounds is to increase compassion for patients and families, to increase understanding and support for one another, and to increase our ability to receive support so we don’t feel isolated in what we’re
doing,” says committee member Judy Ragsdale, MDiv, PhD, director, Pastoral Care.
At each session, a group of panelists speaks on a set topic. Then the floor
opens up, and attendees can share their experiences. A wide variety of topics have
been covered so far: What Haunts You?, Working with Difficult Families, and Simple Acts of Kindness are just a few.
360°
Shanti Smith, RN, application coordinator II, Information Services (l), and Isis Chesko,
RPh, pharmacist I, Investigational Pharmacy, appreciate the bonds that Schwartz Center
Rounds help foster among staff.

11
11
Attendees have been positive with their feedback:• I thought the panel was excellent, and I applaud their
honesty and openness. The insight their stories provided is so valuable to ALL employees because it is a reminder that we are all human and reinforces why we are here—for the kids!
• Following the intimate and emotional stories shared during today’s discussion, I feel more comfortable and able to relate to my colleagues from other disciplines, as this made them seem more vulnerable and approachable.
• I think Schwartz Rounds is one of the most meaningful investments the hospital has made to support staff in a long time. To normalize and validate our experiences as caregivers creates a natural opportunity to talk about the same issues at other times and in other ways.
L U N C H E O N H O N O R S PA R T I C I PA N T SA luncheon was held on April 20 to honor participants from the past year, both the panelists and those on the planning committee. Anna Sheets, RN, clinical director, Otolaryngology, is a committee member and one of those instrumental in bringing Schwartz Center Rounds to Cincinnati Children’s. “You’ve made a difference in the stories you’ve shared,” she told the participants. “The hope is that the conversation continues after rounds.”
To drive home that idea of the conversation continuing, each participant was given a pebble, symbolizing the ripple effect that Schwartz Center Rounds topics can have around the medical center.
The ultimate goal of these rounds is to spread compassion. That’s a lofty goal in a world where measurements are king and results are based on numbers and data. But the stories coming out of these rounds show that they’re having an influence.
Deanna Best, RN, is a quality outcomes manager with the Cancer and Blood Diseases Institute (CBDI). She was a panelist who spoke on the topic of “Running on Empty” last December. All these months later, she still remembers what resonated with her most. A coworker of hers was also a panelist. “I heard her story and remember thinking, ‘How can I work with her so much and never have known this about her?’” Best says. “It was a good example of how Schwartz Center Rounds can impact everyone.”
Best also noticed the effect the panelists’ stories had on the audience. “Once the panelists opened up, it really got others to want to open up too. I definitely want to come back,” she says. “The topics are very engaging both from a bedside perspective and non-bedside.”
W H AT ’ S T O C O M EGoing forward, the planning committee aims to continue bringing thought-provoking topics to Schwartz Center Rounds. They’ll continue to solicit topics from the crowd and address issues that affect the people who work here, with the goal of preserving and protecting the human connection in healthcare.
Explains Basu, “In order to treat human beings, we have to be human beings. Compassionate care is at the heart of caring for children. With all the pressures that are put on the workers in the hospital, addressing their emotional health is important. If we demonstrate compassion to each other, care will improve.”
(L-r) Judy Ragsdale, MDiv, PhD, director, Pastoral Care; Anna Sheets, RN, clinical director, Otolaryngology; and Derek Wheeler, MD, chief of staff, have been pleased by the way employees have embraced the opportunity to listen to and support each other via Schwartz Center Rounds.
Your next opportunity to participate in Schwartz Center Rounds is coming up soon. Continuing education credits are given, and lunch is provided for the first 120 attendees. Rounds are held in the Sabin Auditorium. All employees are welcome. The next topic will be:
August 25 – The Legendary Patient: How Memorable Patients Leave a Legacy for Caregivers
If you would like to help on the planning committee or have an idea for an upcoming topic, contact Anna Sheets, 6-7715; Judy Ragsdale, 6-8913;or Raj Basu, 6-4259.

360°360°
thebuzz
I AM
HAPPIEST AT MY JOB
WHEN…
“I can be part of a great team,
who keeps me smiling and
feeling accomplished.”
Miranda Cornett, administrative
assistant, Pediatric Rehabilitation
“I’ve helped someone and made
their day easier.”
Erica Mason, administrative assistant,
Pediatric Ophthalmology
“I’m interacting with the
patients’ families.”
Ruth Foertsch, coordinator, Gift Shop
“I know I’ve helped a family
and made a positive impact on
someone’s day.”
Ali Snow, senior scheduling agent,
Developmental and Behavioral
Pediatrics
“I am meeting and interacting
with the amazing patients and
families we serve.”
Drew Reeder, social media
coordinator, Marketing &
Communications
“I see and hear that the
research we do helps solve
medical problems.”
Paul Speeg, veterinary research
assistant, Ophthalmology

snapshots
Department Behavioral
Medicine and Clinical
Psychology
Role Pediatric psychologist,
specializing in pediatric
chronic pain
What I love most about what
I do is working with
multidisciplinary teams to help
kids and teens with pain
improve their quality of life.
When I’m not here, you can
usually find me outside,
spending time with my two
daughters and husband.
A phrase that describes me
Balanced
What I love about CCHMC
is the collaboration, innovation
and energy among my patients
and colleagues.
I was born in the middle of a
blizzard.
The guiding principle of my
life is Work smarter, not harder.
Person I admire most
My mother
People would never guess
that I am artistic (inherited
from my father, an artist).
What’s on my bucket list
Traveling to all the major US
national parks
Department Materials
Management
Role Receiving docks
supervisor
What I love most about what
I do is making a difference for
children through collaboration
and problem-solving.
When I’m not here, you can
usually find me mowing the
lawn, taking care of my flowers,
searching YouTube for
home-repair videos.
A phrase that describes me
Reliable, hard-working and
wants to win
What I love about CCHMC
is meeting people whose skills
and talent make it a great place
to work.
I was born in Cincinnati and
raised with tough love.
The guiding principle of my
life Do unto others as you
would have them do unto you.
Person I admire most
My mother. She was an
evangelist who visited prisons,
nursing homes—anywhere
people needed help.
People would never guess
that I am afraid of cats, but I
love large dogs.
What’s on my bucket list
To a) find a way to update
everyone’s Centerlink profile
when they move to a new
location, and b) buy a motor
home and travel.
Department Transport Team
Role Respiratory therapist
What I love most about what
I do is traveling throughout the
country to get kids, the unknown
from one run to the next, and
the great team I work with.
When I’m not here, you can
usually find me relaxing with
my family, at the fire department
or the airport.
A phrase that describes me
A go-getter
What I love about CCHMC
is the pride that every employee
exhibits.
I was born in Virginia and have
lived all over the world.
The guiding principle of my
life is The Golden Rule.
Person I admire most
James Mattis—He’s a
no-nonsense kind of guy.
People would never guess
that I have a pet unicorn that
only eats rainbow sherbet.
What’s on my bucket list
I’ve completed my bucket list.
It was a very short list. I’ve
checked every box.
Department Outpatient GI,
Cincinnati Center for
Eosinophilic Disorders
Role Licensed practical nurse
What I love most about what
I do is continuing the
relationship with patients, most
of whom come from across the
country and travel here often
for repeated procedures every
few months.
When I’m not here, you can
usually find me spending time
with my family and friends.
A phrase that describes me
Laughter is the best medicine.
What I love about CCHMC
is our reputation for being the
best!
I was born in West Memphis,
AR.
The guiding principle of my
life is Respect people: Treat
them as you would like to be
treated.
People would never guess
that I watch more football than
my husband.
What’s on my bucket list
To attend a Super Bowl game.
13

360°
Kathy Graue, Child Life and Integrative Care
Thomas Kimball, MD, The Heart Institute
Charles Myer III, MD, Otolaryngology
Joan Nelson, Customer Service
Holly Odom, A6 North/Adolescent Medicine
Jennifer Pfeffer, Microbiology
Elizabeth Schorry, MD, Human Genetics
Vicki Schum, RN, Information Services
Susan Spear, RN, Liaison Resources
Michelle Stultz, RN, Medical Staf f Services
Maureen Switzer, RN, General and Community Pediatrics
Carolyn Wohl, RN, International Adoption Center
Damita Allen, Access Services
Raouf Amin, MD, Pulmonary Medicine
Phillip Autry, Protective Services
John Ball, Clinical Engineering
Karen Barnes, Patient Services
Jorge Bezerra , MD, Gastroenterology
Ann Bowling , RN, A3 North
Connie Brady, Behavioral Medicine/Clinical Psychology
Kelly Christian, RN, Same Day Surgery
Michelle Dickey, RN-CNP, Infectious Diseases
Eileen Fiedler, RN, Pediatric Urology
Pamela Fiorini, RN, Outpatient Administration
Mary Frey, RN, Emergency Medicine
Kathleen Friend, RN, Liberty Campus/Same Day Surgery
Victor Garcia , MD, Pediatric Surgery
James Heubi, MD, Gastroenterology
Judy Knapp, RPh, Pharmacy
Deborah Seider, RN, Allergy and Immunology
Virginia Bossman, RN, A6 Central
Deborah Floyd, Nutrition Therapy
Carol Hill, APRN-CNP, Pre-anesthesia Consultation Clinic
John Hingl, RPh, Pharmacy
Jeanne Hubbard, RN, Same Day Surgery
Karen Kalinyak , MD, Hematology
Uma Kotagal, MBBS, MSc, Anderson Center
Tonette McKimm, RN, Liberty Campus/Surgery
John Reuter, MD, Neonatology and Pulmonary Biology
Brenda Robb, Critical Care
Robin Walker, Food Services
Julie Ballweg , RN, Orthopaedics Center
Brenda Bell, B1/Emergency Department
Laurie Clark , APRN-CNP, Pre-anesthesia Consultation Clinic
Lynn Daum, RN, Patient Services
milestones
25
Congratulations to the fol lowing employees who celebrate milestone service anniversaries in J U LY, A U G U S T and S E P T E M B E R!
35
30
Very few employees reach the 50-year service anniversary milestone at Cincinnati Children’s. Beatrice Lampkin, MD, joined the Division of Hematology/Oncology in 1965 and directed the division for 18 years (1973–1997). She was the first female director of a hematology/oncology division in the United States and has made important contributions to the development of chemotherapy regimens that improved outcomes for children with leukemia.
40
50

15
20
Lorrie Gates, RN, A6 South
Michael Gelfand, MD, Radiology
Stuart Handwerger, MD, Endocrinology
Amy Heikkila , Liberty Campus/Surgery
Donna Hillman, RN, Post Anesthesia Care Unit
Emily Hoffman, RN, Plastic Surgery
Sonya Holston, Managers of Patient Services
Heidi Kalkwarf, PhD, General and Community Pediatrics
Suhas Kallapur, MD, Neonatology and Pulmonary Biology
Holly Kuhl, RN, Allergy and Immunology
Jennifer Lohrer, RN, Clinical Translational Research Center
Teresa Marcus, Outpatient Registration
Colleen McGuire, Protective Services
Mary Miller, APRN-CNP, Advanced Practice Nurses
Mark Naugle, Neurology
Debra Norman, Scheduling Center
Cathy Patterson, RN, A6 North/Adolescent Medicine
Cheryl Reynolds, Information Services
Lynn Sanner, Child Life and Integrative Care
Scott Schappacher, PharmD, Pharmacy
Sherri Schoo, Pharmacy
Kimberly Sears, RN, Nephrology
Michael Sorter, MD, Psychiatry
Laurie Tate, Hospital Bill ing
Laura Weber, Child Life and Integrative Care
Betsy Adler, APRN-CNP, Heart Institute
Julianne Badylak , Occupational Therapy/Physical Therapy
Kathleen Baumhardt, Occupational Therapy/Physical Therapy
Audra Birri, Human Genetics
Jasenka Black , LISW, Psychiatry
Maria Britto, MD, MPH, Adolescent Medicine
Alan Brody, MD, Radiology
Richard Campbell, DMD, Dentistry
Tracey Carraher, RN, Drug and Poison Information Center
Tammy Cook , RRT, Respiratory Care
Jennifer Detzel, APRN-CNP, Advanced Practice Nurses
Renee Dey, RRT, Respiratory Care
Jennifer Donohue, Radiology
Alexandra Falcone, Transgenic Core
Amanda Fitz, Audiology
Sheila Ford, RN, Psychiatric Resource Unit
Jill Baumann Freudenberg , RN, Liberty Campus/Emergency
Department
Rebecca Haehnle, RN, General and Community Pediatrics
Kathleen Zink Hass, RN, LMT, Child Life and Integrative Care
Julie Hausfeld, RN, A6 North/Adolescent Medicine
Kelly Hicks, RN-CNS, Advanced Practice Nurses
Ajay Kaul, MD, Gastroenterology
Laura Kelly, RN, Allergy and Immunology
Lynne Lane, Orthopaedics
Denise Leonard, RN, Pulmonary Medicine
Teresa Louis, Hospital Bill ing
Aimee Maas, LISW, Social Services
Charles Mehlman, DO, MPH, Orthopaedics
Kenneth Morency, Materials Management
Laura Olexa , RN, Hopple Street
Karen Padgett, Speech Pathology
Wendy Pomerantz, MD, Emergency Medicine
Andrea Powers, LISW, Social Services
Terri Roberts, Accounting
Lora Schmidt, Human Genetics
Lisa Schwetschenau, Emergency Services
Molly Shewmaker, A4 Central/Psychiatry
William Sirbu, PhD, Behavioral Medicine/Clinical Psychology
Carolina Sprinkle, RRT, Respiratory Care
Sara Valentine, Speech Pathology
Sara Welch, Human Genetics
Vivian Wolfe, Critical Care
Hector Wong , MD, Critical Care
Daniella Woodberry, Cancer and Blood Diseases Institute
Katherine Yutzey, PhD, Molecular Cardiovascular Biology
See a complete l ist of milestone service anniversaries online
in this week’s edition of CenterNews.

3333 Burnet Avenue, MLC 9012
Cincinnati, OH 45229-3026
a moment in history 1930s
In 1939, a boy in an iron lung joins other children in a playroom at Cincinnati Children’s as they listen to the Cincinnati Reds play in a World Series game (they won the championship). Iron lungs were respirators used to treat patients with severe lung disease due to polio. This same year, Albert Sabin, MD, arrived in Cincinnati, where in his CCHMC research laboratory, he ultimately developed the oral vaccine that would conquer polio around the world.
I became a member of the Cincinnati Children’s community at 8 years old
when my older sister was diagnosed with juvenile diabetes. I remember tagging along to numerous doctors’ visits here and hanging out in the play area with her until she was swept away by her friendly nurse to see the doctor. Having to watch the person I looked up to most endure the pain of being stuck with a needle every day and constantly struggling to balance this
huge weight that had been thrust on her (and my parents’) shoulders marked
the first time I ever thought about more than just myself. That’s when I informed my
parents that I was going to find the cure for my older sister at Cincinnati Children’s. That moment
sparked the fire behind my love for science, research and the medical center.
As I got older, my love for all things science did not waver, nor did my memories of the phenomenal care that Cincinnati Children’s offered my sister. Throughout my undergraduate and graduate years, I never stopped working toward my goal of becoming a part of the Cincinnati Children’s family. And although I never found the cure for diabetes, today I am lucky enough to be a part of an amazing team here that focuses on the research of pediatric brain tumors.
I credit those childhood experiences to opening my eyes to the wonderful family that is Cincinnati Children’s, to the amazing work that is accomplished here and leading me to where I am today. Being a part of something that is constantly moving forward, where everyone holds so much pride for what they do and what this organization stands for allows me to say that I could not be prouder to be a Cincinnati Children’s employee!
—Amanda Smith, research assistant III, Oncology
Why Am I Here? Amanda Smith