324.full
-
Upload
anthony-chandra -
Category
Documents
-
view
6 -
download
1
description
Transcript of 324.full

Journal of Epidemiology and Community Health, 1989, 43, 324-329
Cryptorchidism: a registry based study in Sweden onsome factors of possible aetiological importanceMATS HJERTKVIST,' JAN-ERIK DAMBER,2 AND ANDERS BERGH3From the Departments of'Surgery, 2Urology andAndrology, and3Pathology, University ofUmecl, Umecl, Sweden.
ABSTRACTStudy objective: To examine the epidemiological characteristics of boys with crypt-orchidism.Design: Cohort survey using the Swedish personal identification code and Medical Birth Registry tolink cryptorchid boys with their pregnancy and delivery data. They were compared with the totalpopulation of male births during the same period.Subjects: 2861 cryptorchid boys born in Sweden between 1973 and 1982 were identified. Of these 437could not be linked with their Medical Birth Registry information for various reasons, or were
excluded because they were under 1 year of age at the end of 1982, leaving 2424 cases for study. Thereference population comprised all boys born in Sweden during the same period (n=458 601).Measurements and main results: For each study variable, the observed number of cases among boyswith cryptorchidism was compared with the expected number calculated from the whole population.A significant increase in intensity ratio for cryptorchidism was found with the first birth, caesarean
section, toxaemia of pregnancy, and certain congenital abnormalities (hypospadias and subluxationof the hip). It was also more common in small for dates infants. There was a seasonal variation incryptorchidism, with increased incidence in January-March.Conclusions: Cryptorchidism may be caused by hormonal influences during pregnancy, which couldbe affected by utero-placental factors involving placental dysfunction or by daylight hours, throughpineal activity.
Cryptorchidsm is one of the most common congenitalmalformations in males. There are reports' 2 showingan increase in incidence. The close association betweencryptorchidism and testicular malignancy3-5 andinfertility6 makes the condition clinically important.However, the aetiology of this disorder is littleunderstood. Testicular descent is believed to takeplace in two phases.7 During the first phase, occurringduring the first trimester, the testes descend from theirintra-abdominal position to the groin and this phase isbelieved to be independent of androgens. The secondphase occurs during the third trimester, when thetestes descend to the scrotal sac. It is believed that thissecond phase of descent is androgen dependent.7Theoretically, any condition in the mother or in thefetus causing disturbed androgen production maylead to cryptorchidism, although such conditions arehard to define. Previous studies have suggested somerisk factors which might be associated with theaetiology of cryptorchidism, such as impairment ofthe placental function,8 abnormal chorionic
gonadotrophin (hCG) secretion,' exposure tooestrogens,8 and breech presentation in labour.9 Thesefactors may cause an impairment of testicularandrogen production in the fetus. The present studywas designed to investigate characteristics of themother and/or the child which are possibly related tocryptorchidism and are perhaps aetiological factorsfor this malformation. This was done by use of anationwide public health registry.
Methods
Since 1973, a Medical Birth Registry in Sweden hascollected medical information on all births. It is basedon a standardised record form used in the wholecountry (with a local variant in one county) formedical care in maternity health centres (which nearlyevery pregnant woman attends), delivery units(practically all deliveries occur in hospitals), and atexamination of the newborn infant (nearly all infantsare examined by a qualified paediatrician). The form is
324

Registry based study of cryptorchidism
used for information exchange between maternityhealth centres, delivery units and child health centres.A copy of the form goes to the National Board ofHealth and Social Welfare and forms the basis for theregistry. It contains among other things some socialdata, data on the pregnancy and the newborn infant,and diagnoses referring to pregnancy, delivery and thenewborn. Such diagnoses are submitted in a codedform, using the Swedish modification of the ICD8classification. 10Another registry, The Hospital Discharge Registry,
contains information on all patients discharged fromhospitals, including discharge diagnoses (coded asICD8) and operation codes. This registry does notcover the whole country, as only approximately 70%of the counties participate.
In both registries, each individual is identified by theunique personal identification code which everySwedish citizen gets soon after birth. This makes itpossible to link the two registries to each other.
All boys over the age of one year in the HospitalDischarge Registry with the diagnosis ofcryptorchidism and/or who had received anorchidopexy were identified. During the periodstudied (1973-1982) nearly all boys with this conditionwere treated surgically. A total of 2861 cases wereidentified. By linkage to the Medical Birth Registry(1973-1981), information concerning pregnancy,delivery and the conditions in the neonatal period werelinked to each case. No linkage was possible in 437cases, either because their identification numbers wereincomplete or wrong in either file, or because theywere not born in Sweden but had immigrated. In thesecases it was not possible to compare variables with thegroup in which linkage was achieved. Infants born in1982 were excluded because this cohort had not yetreached the age of 1 year at the end of 1982. Thediagnosis is not accepted under 1 year of age becauseof the known possibility of spontaneous testiculardescent during the first year of life. This left 2424 casesfor further study.As a comparison group, all 458 601 boys born in
1973-1981 and registered in the Medical BirthRegistry were used. The table presents the annualnumber of cases and total male births in each year.
Statistical methods
For each study variable, the observed number of casesamong the boys with cryptorchidism was compared tothe expected number, calculated from the total group.This comparison was often made after stratificationfor different variables, eg, year of birth, maternal ageand/or parity, delivery unit. The ratio between theobserved and expected number is called intensity ratio,a neutral term which does not imply causality. The
325
Table The number of cases of cryptorchidism born 1973-81and operated on at I year ofage or older 1974-82 and all malesborn per year 1973-81.
Year of Cases All malesBirth born
1973 594 55 8761974 521 56 2691975 441 52 8601976 303 50 2501977 240 49 2741978 167 47 5801979 86 49 0291980 46 49 7181981 26 47 745
statistical significance of an intensity ratio wasevaluated with x2 statistics when the expected numberexceeded 5, and the approximate 95% confidenceinterval (CI) was determined with Miettinen'sapproximation. " When the expected number was 5 orless, a Poisson model was applied instead. Seasonalitywas studied with the use of Edward's model'2 wherethe expected number ofcases each calender month wasadjusted for variations in total number of births thatyear and month.
*1 1-
0
a'rcoL._
4-
1-U-
O.81J F MA MJJASND
1-2
0984078 / N
0-.7 / , .. . . . . . .
Month of birth
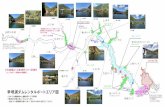
Fig 1 Intensity ratios (IR) for cryptorchidism in differentmonths of the year. The upper panel shows the curve for thewhole ofSweden and the lowerfor different geographic regions(south, middle and north).
v,- i . .i A r. i . A i 6 . 6

Mats Hjertkvist, Jan-Erik Damber, and Anders Bergh
Results
SEASONALITY:A seasonal variation in the intensity ratio of birth ofboys with cryptorchidism was found. There was amaximum intensity ratio from January to March anda minimum in November. Figure 2 shows the intensityratio for cryptorchidism in the whole ofSweden and indifferent geographical areas, after adjustment for theseasonal variations in the number of births. Edward'sformula'2 gives x2 = 25-9 at 2 df for the total material,p<0 001. For each one of the three areas, acorresponding calculation gives: south, X2= 110(p<0 01); middle, x2=4 5 (p>0 05); and north,%2 = 6-2 (p < 0.05). The seasonality in the middle areathus does not reach statistical significance, but allthree areas may show random variation from the sameseasonality.
1-2
1-X1\10
.Da
0- 4+Parity
Fig 2 Intensity ratios (IR) for cryptorchidism in relation toparity (with 95% confidence intervals).
CAESAREAN SECTION:Among the cryptorchid boys, 264 (10 9%) were
delivered by caesarean section. The expected number,after standardisation for year of birth and deliveryunit, was 197-6, intensity ratio= 1 33, p<0 001, 95%CI= 1-l8-1-51. The expected number afterstandardisation for birthweight and year of birth was202-6, intensity ratio = 1 30, p < 0-001, 95% CI = 1-15-1-47.
MATERNAL FACTORSParity-Figure 2 shows the intensity ratio ofcryptorchidism in relation to parity after adjustmentfor year of birth, birth weight and age ofthe mother. Itwas found that there was an increased intensity ratiofor cryptorchidism in the first born child and that therewas no difference in subsequent births. The intensity
ratio for first births v higher order births was [ 11,p<0-001, with a 95% CI of 105-1 18.Maternalage-When adjusted for parity, year of birthand birthweight there was no significant effect ofmaternal age on the intensity ratio for cryptorchidism,as seen in fig 3. When calculated without adjustmentthere was an increased intensity ratio ofcryptorchidism in cases born to younger mothers butthis was secondary to the effect of parity.
12
.2
098
15 20 25 30 35 40 45 50
Maternal age (years)
Fig 3 The intensity ratios (IR)for cryptorchidism in relationto maternal age (with 95% confidence intervals).
Maternal illness-In 14 cases the mother was found tohave diabetes mellitus. When compared to theexpected number (8 14), this gives an intensity ratio of1-7 (p < 0-05). Pregnancy toxaemia occurred in 275mothers. The expected number when adjusted fordelivery unit, maternal age and parity was 50, givingan intensity ratio of 5-4 (p< 0001). Pregnancyhyperemesis occurred in 12 cases, the expected numberbeing 8-8. This gives an IR of 1-4, which was notstatistically significant.Length ofgestation-Figure 4 shows the relationshipbetween length of gestation and cryptorchidism.Adjustment has been made for the age of the mother,parity and year of birth. Calculation of pregnancyduration is based on the date of the last menstrualperiod, or if not available or clearly wrong, on thegestational assessment made by the hospital. It wasfound that there was no significant influence ofgestational age on intensity ratio for cryptorchidismdiagnosed at or after one year of age.
CHILD FACTORSBirth weight-The distribution of cryptorchidism inbirth weight groups, divided into 500g bands, is shownin fig 5. Adjustment was made for year of birth, age ofthe mother and parity. There was an intensity ratio of
, 1-0- 11
0.9-
1n-R
326

Registry based study of cryptorchidism
4-1~
-1.0-
0*50
0
26 30 34 348
Gestational duration (weeks)
Fig 4 The intensity ratios (IR)for cryptorchidism in relationto gestational duration (with 95% confidence intervals).
15 (95% CI= 1.3-1.8) for birth weights between 15and 2 5 kg (p< 0-001) but there was also a significantlyincreased risk for the 1 0-1 5 and 2-5-3 0 kg classes.
30
205-
2.0
15
10
01 2 3 4 5
Birthweight (1000 g)
Fig 5 The intensity ratios (IR)for cryptorchidism in relationto birth weights (with 95% confidence intervals).
When birth weight and length of gestation wereconsidered together (figs 4 and 5) there was anincreased intensity ratio for cryptorchidism in boyswith subnormal birth weight but not in those withsubnormal gestation. This means that these boys weresmall for dates, irrespective of their length ofgestation.Congenital malformations-Only 30% ofthe cases hada diagnosis of cryptorchidism in the newborn period.This is close to the figure of 34% given in reference 1.The distribution of congenital malformations ininfants with cryptorchidism deviated from thatexpected from the total population with respect to
327
only three groups: (1) The observed number of heartmalformations was 16 and the expected number was14-2. This difference may be random. (2) Hypospadiaswas observed in 12 cases and the expected number was4 5, which gives an intensity ratio of2-7(p < 0-01), 95%CI =1 4-47. (3) Dislocation or subluxation of the hipwas observed in 22 cases and the expected number,after adjustment for delivery unit and year of birth,was 8-9 which gives an intensity ratio of 2 5 (< 0-001),95% CI= 17-3-7.
Discussion
In this study we observed a seasonal variation in theincidence of cryptorchidism in Sweden. An increasedincidence was found in boys born in March and adecreased incidence in boys born in November. In themiddle area, seasonality was not statisticallysignificant, perhaps due to small numbers. A similarseasonal variation has been reported both in Hungaryand in Britain.'3 14 The incidence oftwo other diseasesin the male reproductive system, hypospadias andtesticular cancer, both show a similar seasonalvariation.15 16 The reason for this seasonal variation isunknown and difficult to explain (see Kallen'7 fordiscussion). However the sexual differentiation of thefetus, including testicular descent, is controlled byhormones,7 and seasonal differences in daylight length(via effects on the pineal gland) are known to influenceovarian hormonal activity in man.18 The seasonalvariations in daylight are pronounced in Sweden,particularly in the northern part.'8 Moreover, inexperimental animals it has been shown thatinterference with pineal function in the pregnantmother influences testicular function in the maleoffspring.'9 On the other hand our findings ofa similarseasonal variation in southern and northern Swedendespite large differences in daylight hours mayindicate that factors other than light could beinvolved. One possible example could be seasonaloccurrence of certain infectious diseases impairingplacental function and thus disturbing sexualdevelopment ofthe fetus. Impaired placental function,with general effects on fetal health and possiblyreduced secretion of hCG and, as a consequence, areduced production of testosterone and othertesticular hormones in the male fetus, has beensuggested as an aetiological factor for testicularmaldescent.78 Some observations in this and otherstudies are in favour of this hypothesis:
(1) Placental insufficiency or breech labour are themost common reasons for caesarean sections inSweden, and caesarean section was found to be morecommon in the cryptorchid than the control group.Breech labour as such was not associated with

328
cryptorchidism and it is thus unlikely that caesareansection protects against a risk caused by breech labouras suggested by Swerdlow et al.9
(2) The intensity ratio for cryptorchidism wasincreased in boys born "small for date", a conditionwhich may be due to placental insufficiency or to thefetus being unhealthy from some other cause. Earlierstudies on the duration of gestation and birth weightshowed an increased risk of cryptorchidism whenthese were subnormal.2 20 However, when comparingthe effects ofgestational length and birth weight in ourstudy, we found that the intensity ratio forcryptorchidism was increased by low birth weightwhen the child was "small for date" but not when itwas born preterm. Thus the mechanisms controllingtesticular descent may operate normally after birthprovided that the child is otherwise healthy. Up to 3years after delivery cryptorchid boys are twice as likelyas controls to have reported illnesses of some kind(other than minor colds).8 Thus some data suggestthat the cryptorchid individual is somewhat unhealthyboth in utero and later.
(3) Bleeding and spotting during the last trimester2'and threatened abortion8 have been reported as riskfactors for cryptorchidism.
High levels of unbound oestrogens duringpregnancy, as are found in toxaemia,3 20 have beensuggested as a cause of cryptorchidism, possibly byimpairing testicular hormone secretion.22 Someobservations in this study support this hypothesis. (1)The study confirms that toxaemia is a risk factor forcryptorchidism (see also Kallen23). (2) The incidenceof cryptorchidism is increased in first born boys(irrespective of the age of the mother, see above) andpossibly oestrogen levels may be higher in the firstthan in subsequent pregnancies.24 (3) Hypospadiasand malformations of the hip were considerably morecommon in the cryptorchid than in the control groupand it has been suggested that both thesemalformations are associated with increasedoestrogen levels.20 22 25 26. However, recently Burtonet a127 showed that the mothers of cryptorchid boyshad reduced rather than increased oestradiol levelsduring pregnancy, and Beard et at2' did not observeany increase in the incidence ofcryptorchidism in boysexposed to exogenous oestrogens in utero.
Diabetes mellitus in the mother is a risk factor forcryptorchidism. The reason for this is unknown butthis condition probably influences placental functionand most interestingly Leydig cells are hyperplastic innewborn infants of diabetic mothers, possibly due tosupranormal placental hCG secretion.28 Increasedmaternal hCG secretion is also observed in pregnancytoxaemia and intrauterine growth retardation,29suggesting that the relationship between placental
Mats Hjertkvist, Jan-Erik Damber, and Anders Bergh
insufficiency and cryptorchidism is not necessarilyexplained by reduced but perhaps by supranormaltesticular function.
In conclusion, this epidemiological study confirmsseveral previous studies showing that diabetesmellitus, pregnancy toxaemia and caesarean sectionare risk factors for cryptorchidism and that theincidence of this disease is related to the month ofbirth. In some aspects it extends previous findings;decreased gestational length as such is not a riskfactor, but a subnormal birth weight is, both at normaland subnormal gestational length. That means thatthese cases have retarded intrauterine growth. Firstborn males have an increased incidence ofcryptorchidism but the age of the mother is notimportant. The incidence of hip malformations isconsiderably increased among cryptorchid boys.However, it is worth remembering that only 30% ofcryptorchid boys are diagnosed at birth.The aetiology of cryptorchidism remains largely
unknown but the present findings support thehypothesis that placental dysfunction causinghormonal or other disturbances in fetal health couldbe involved.
This work was supported by grants nos 5653 and 5935from the Swedish Medical Research Council.The authors are most grateful to Professor Bengt
Kiillen, Department of Embryology, University ofLund, for valuable methodological help andsuggestions. Also the assistance of Anders Ericson,National Board of Health and Welfare, and AnitaSandstrom, Department of Epidemiology, Universityof Umea, is gratefully acknowledged.
Address for correspondence and reprints: MatsHjertkvist, Department of Surgery, University ofUmea, S-901 87 Umea, Sweden.
References
I John Radcliffe Hospital Study Group. Cryptorchidism: anapparent substantial increase since 1960. Br Med J 1986;ii: 1401-4.
2Chilvers C, Pike MC, Forsman D, Fogelman K,Wadsworth MEJ. Apparent doubling of frequency ofundescended testis in England and Wales in 1962-81.Lancet 1984; ii: 330-2.
Henderson BE, Benton B, Jing J, Yu MC, Pike MC. Riskfactors for cancer of the testis in young men. Int J Cancer1979; 23: 598-602.
4Pottern LM, Brown LM, Hoover RN, et al. Testicularcancer risk among young men: Role of cryptorchidismand inguinal hernia. J Nati Cancer Inst 1985; 74: 377-81.
5 Krabbe S, Berthelsen JG, Volsted P, et al. High incidenceof undetected neoplasia in maldescended testes. Lancet1979; i: 999-1000.
6 Hadziselimovic F, Herzog B, Girard J. Cryptorchidism:Histology, fertility and treatment. Prog Reprod Biol Med1984; 10: 1-15.

Registry based study of cryptorchidism7 Hutson JM. A biphasic model for hormonal control of
testicular descent. Lancet 1985; ii: 419-21.8Davies TW, Williams DRR, Whitaker RH. Risk factors
for undescended testis. Int JEpidemiol 1986; 15: 197-201.9 Swerdlow AJ, Wood KH, Smith PG. A case-control study
of cryptorchidism. J Epidemiol Community Health 1983;37: 238-44.
10 International Statistical Classification of Diseases, Injuriesand Causes of Death; 1965 revision adapted for indexingof hospital records and morbidity statistics (in Swedish).Stockholm, 1968.
l Miettinen OS. Simple interval estimation of risk ratio. AmJ Epidemiol 1974; 100: 515-6.Edwards JH. The recognition and estimation of cyclictrends. Ann Hum Genet 1961; 25: 83-7.
3 Czeizel A. Aetiological studies of isolated commoncongenital abnormalities in Hungary. Budapest:Akademiai Kiado, 1984.
14Jackson MB, Swerdlow AJ. Seasonal variations incryptorchidism. J Epidemiol Community Health 1986; 40:210-3.
5 Knox EG, Cummins C. Birth dates ofmen with cancer ofthe testis. J Epidemiol Community Health 1985; 39:237-43.
16 Kallen B, Bertollini B, Castilla E, et al. A jointinternational study on the epidemiology of hypospadias.Acta Paediatr Scand (Suppl) 1986; 324.
17Kalln B. Epidemiology of human reproduction. BocaRaton, Florida: CRC Press, 1988; 177-8.
Kauppila A, Kivela A, Pakarinen A, Vakkuri 0. Inverserelationship between melatonin and ovarian activity in aregion with a strong seasonal contrast in luminosity. JClin Endocrinol Metab 1987; 65: 823-8.
19Jarrige JF, Tlemcani 0, Boucher D. Gonadal function inmale offspring of pinealectomized female rats. ActaEndocrinol 1987; 116: 247-52.
32920 Depue RH. Maternal and gestational factors affecting the
risk of cryptorchidism and inguinal hernia. Int JEpidemiol 1984; 13: 311-7.
21 Beard M, Melton LJ, O'Fallon WM, Noller KL, BensonRC. Cryptorchidism and maternal estrogen exposure.Am J Epidemiol 1984; 120: 707-16.
22 Hadziselimovic F. Cryptorchidism. Management andimplications. Berlin: Springerverlag, 1983.
23 Kallen B. Hyperemesis during pregnancy and deliveryoutcome: a registry study. Eur J Obstet Gynecol ReprodBiol 1987; 26: 291-302.
24 Swerdlow AJ, Huttly SRA, Smith PG. Prenatal andfamilial associations of testicular cancer. Br J Cancer1987; 55: 571-7.
25Svensson J. Male hypospadias. 625 cases, associatedmalformations and possible aetiological factors. ActaPediatr Scand 1979; 68: 587-92.
26Andren L. Pelvic instability in newborns with specialreference to congenital dislocation of the hip andhormonal factors. Acta Radiol (Suppl) (Stockh) 1962;212.
27 Burton MH, Davies TW, Raggatt PR. Undescended testisand hormone levels in early pregnancy. J EpidemiolCommunity Health 1987; 41: 127-9.
28 Barbieri RL, Saltzman D, Phillippe M, et al. Elevatedn-human chorionic gonadotropin and testosterone incord serum of male infants of diabetic mothers. J ClinEndocrinol Metabol 1985; 61: 976-9.
29 Heikinheimo M, Seppala M. Amniotic fluid humanchorionic gonadotropin in late pregnancy; elevated levelsin toxemia with intrauterine growth retardation. Am JObstet Gynecol 1983; 146: 766-75.
Acceptedfor publication April 1989