21 Disorders of the external breathing I breathing_I_PR... · External breathing ~: O 2 and CO 2...
Transcript of 21 Disorders of the external breathing I breathing_I_PR... · External breathing ~: O 2 and CO 2...

Disorders of the
external breathing I.
Roland Psader DVM
SZIU

External breathing
� ~: O2 and CO2 exchange between blood and
atmosphere
� Respiratory tract
� Gas transport system
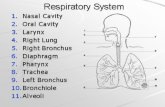
� Conducting system: nasal cavity, larynx, trachea, bronchi
� Transitional system: bronchioles
� Gaseous exchange system: alveolar ducts, alveoli

Schematic diagram of airways

Structure
� Conducting system: pseudostratified, ciliated
columnar cells, secretory goblet cells (mucus), secretory cells
� Transitional s.: disappearance of cilia, lack of
goblet cells, neuroendocrine and Clara cells(detoxification of xenobiotics)
� Gas exchange s.: type I. pneumocytes
(membranous) and type II. pneumocytes (granular)


The blood-air barrier
� Type I. pneumocytes:� Cytoplasm thin
� Tight intercellular junctions
� Type II. pn.: � Precursors of type I.
� Surfactant (reduce surfacetension)
� Thin basement membrane
� Capillaries
� Small amount of collagenand elastin

Pulmonary lymph
� Arises from alveolar capillary
� Lymphatic capillaries are not present in the alveolarwall, but are present within the walls of resp. bronchioles
� Higher protein content compared with other tissues (3,5 g/100 ml,
other t.: 2g/100ml)
� Alveoli are kept dry, lymph is rapidly removed:� Pumping action of the lymphatics
� Relative impermeability of alveolar epithelial cells

Defense mechanisms ofrespiratory tract
� Sneezing, reverse sneezing, coughing and
reflex bronchoconstriction
� Mucociliary clearance and phagocytosis
� Immunologic defense

Defense mechanisms
Mucociliary
clearance
nose
larynx
trachea
bronchi
bronchioles
alveoli
sneezing
coughing
bronchoconstriction
phagocytosis
IgA
IgG
C
E
L
L
-
M
E
D
I
A
T
E
D

� Sneezing: subepithelial myelinated trigeminal
nerve endings in nasal mucosa, exspiratory effortthrough the nares
� Reverse sneezing: nasopharyngeal irritation,
extreme inspiratory effort
� Bronchoconstriction: n. vagus, increase in
airway resistance, prevent further penetration ofmechanical or chemical irritants

Cough pathway
Cough stimulus (mechanical, chemical, inflammatory)
Cough receptors (rapid
stretch receptors,
bronchial and pulmonary
C-fibers)
Vagus nerve
Mediators
(tachykinins, substance P)
Central coughcenter(Brainstem, pons)
Cortex
Cough

Cough receptors
Stretch receptors:
� Mechanical stimulus
C-fibers:
� Chemical stimulus >>mechanical
Proximal airways: mechanical >>> chemical
Bronchi, bronchioles: chemical >>> mechanical

Mucociliary clearance
� Two-phase fluid layer (inner sol phase, outer viscousgale phase)
� Goblet cells, serous cells, submucosal glands
� Cilia beat synchronously, removal deposited particlesand dissolved gasses
� Nasal cavity back to the pharynx, trachea upto the pharynx

Changes in clearance activity
� Activity of cilia:� increasing up to 39 0C and then decreasing
(fever)
� low air temperature ↓, some drugs, viruses ↓
� Amount and composition of mucus:� increased viscosity: hot, dry atmosphere→ tearing
of mucus and exposure of mucosa → bacterialcolonisation
� serous fluid production: acute inflammation, thickened fluid layer → reducing movement

Immunologic defense
� All class of immunoglobulins but IgApredominates in the upper resp. tract and
IgG in the lower tract
� Cell-mediated immunity: BALT (bronchial-
associated lymphoid tissue), B and T
lymphocytes, macrophages, M cells, dendritic
cells, other antigen presenting cells

Defense mechanisms ofexchange system (alveoli)
� Lack of mucociliary clearance and coughing reflex doesn’t cause increased velocity of airflow in the
alveoli
� 2 µm > particles (asbestos 200 µm large but slenderfiber!)
� Alveolar macrophags, intravascularmacrophages, opsonizing antibodies, surfactant,
antioxidants

Impairment of defensemechanisms
� Viral infections: influenza virus in pigs and horses, PI-3
and BHV-1 (bovine herpes v.) in cattle, distemper in dogs, multiple
mechanism, change in mucociliary clearance, 5-7 days after a
viral inf. the phagocytic function is impaired
� Toxic gases: ammonia, hydrogen sulfide, smooke
inhalation
� Immunodeficiency: PRRS, FIV, AIDS → increased
susceptibility to secoundary bacterial infections

Bacterial retention in the lung

Alveolar hyperplasia andepithelization
� Common and non-specific respons to many stimuli
� Directly acting stimuli: toxic gases (nitrogen dioxid, pure
oxygen, ozone), chemicals (phenols, ethylene dibromide,
pyrrolizidine alkaloids), viruses
� Indirectly acting s.: pulmonary edema and fibrosis
Thickening of blood-air barrier + decreased„stretchability” of the alveolar wall → restrictiverespiratory failure

Normal respiratory function
O2 and CO2 exchange between blood and air is
achieved by combination of:
� Ventilation (V)� Perfusion
� Distribution
� Diffusion

Ventilation (V)
� ~: is the process by wich air is moved into the alveoli
� 2/3 of inspired air reaches the alveoli, remainder 1/3occupies the dead space (in the trachea, bronchi, bronchioles)
� Alveolar ventilation (VA): the volume of air entering the alveoli each
minute
� Partial pressure of arterial carbon dioxid (P a,CO2) is utilized to determine the ventilatory status of patient

VA and P a,CO2 / P a,O2
� VA is inversely proportional to the P a,CO2
� If VA is reduced P a,CO2 increases, and if VA is increased P a,CO2 decreases
� In contrast , increasing the VA of normal lung doesnot increase the partial pressure of oxygen, because the blood leaving the well ventillated alveoli is already fullyoxygenated
� Normal range of P a,CO2 : 35-45 Hgmm in dog and 30-40 Hgmm in cat

Control of breathing
� Central neuronal control
Medullary respiratory center, apneustic and pneumotaxic center in pons: H+ concentration in CSF, decrease in pH increases ventilation
(determined by P a,CO2 )
� Peripheral control
� Chemoreceptors in the aortic and carotid bodies: largely
arterial hypoxemia >> fall in pH, increase in P a,CO2
� Stretch receptors in the lung, baroreceptors in the carotid and aortic sinuses,
other receptors

Respiratory volumes
IC
VC
FRC RV
TLC
ERV
V T
IRV
TLC = Total lung capacity
FRC = Functional residual capacity
RV = Residual volume
VC = Vital capacity
VT = Tidal volume-normal resp.
IC = Inspiratory capacity
ERV = Expiratory reserve volume
(supplemental air)
IRV = Inspiratory reserve volume
(complemental air)

Normal respiratory function
� Ventilation (V)
� Perfusion (Q)� Distribution
� Diffusion

Perfusion of the lung withblood (Q)
� Lung is perfused by the output of the right
ventricle, but not uniformly!
� Gravitation! Ventral portions of the lung have a much greater
blood flow than dorsal regions. In laterally recumbent animals the„downside” lung suffers overperfusion. Large animals and largedeep-chested dogs.
� Pathologic overperfusion: left-sided heart
failure + gravitation→ pulmonary edema

Normal respiratory function
� Ventilation (V)
� Perfusion (Q)
� Distribution (V/Q)� Diffusion

Distribution (V/Q)
� Distibution of air in the lung is not uniform, but the differences are
not as marked as perfusion differences!
� Ideally ventilation/ perfusion ratio in an alveolus: V/Q=1
� Little or no ventilation (bronchitis): V/Q < 1 to zero → venous
blood cannot be oxygenated! This area of lung is acting as right to left
shunt
� Ventilated but not perfused alveolus (thrombosis): V/Q >1 →this alveoli act as dead space

Accomodation of perfusion (P) toimpaired ventilation (V)

Normal respiratory function
� Ventilation (V)
� Perfusion (Q)
� Distribution (V/Q)
� Diffusion

Diffusion
� The diffusion of O2 and CO2 across the alveolar wall is
dependent on:
� Surface area: large!
� Differences in partial pressure: O2: 100Hgmm and 40Hgmm,
Co2: 40Hgmm and 46Hgmm
� Thickness of the tissue: extremely thin normally
� Contact time: large functional reserve! Equilibration occurs only
1/3 of the way along an alveolar capillary!
� Solubility and diffusibility of the gas CO2 20x more
diffusible than O2!

� Diffusion of oxygen inhibited by:
� Decrease in alveolar Po2
� Increase in alveolar wall thickness
� CO2:
� Much more diffusible→ increase in the thicknessof alveolar wall does not generally result in
increased Pa,CO2

Respiratory failure
~:Inability of the lungs maintain the arterial
levels of O2 and CO2 within defined limits.
When arterial O2 levels fall from 90-100 to 60-70Hgmm and CO2 rises from 40 to 50 Hgmm, the animal is in respiratory failure

Causes of hypercapnia
� Neurogenic hypoventilation� Neuromuscular disorder
� Medullary dysfunction (anesthesia, intracranial disease)
� Cervical disease, neuromuscular disease
� Airway obstruction� Large airway (laryngeal paralysis, tracheal collapse)
� Small airway obstruction (chronic airway disease, bronchoconstruction)
� Thoracic wall problems� Open PTX
� Flail chest wall
� Anterior displacement of the diaphragm
� Pleural space filling disorder (air, blood, diaphragmatic hernia, etc.)
� Pleural fibrosis
� Pulmonary parenchymal disease� Compensation for metabolic acidosis� Malignant hyperthermia� Inappropriate ventilator settings� Dead space rebreathing� Recent bicarbonate therapy in ventilatory compromised patients

Causes of hypoxia
� Low inspired oxygenconcentration
� Inadequate supply of oxygento the breathing circuit
� Dead space rebreathing� Neurogenic hypoventilation
(see before)� Venous admixture� Low V/Q� Bronchospasm� Airway narrowing due to
fluid/exudate accumulation� Small airway/alveolar collapse� Positional stasis especially
with hypoventilation
� Increased surface tension dueto fluid/exudate accumulation
� External compression of thelung
� Diffusion defect� Inhalation injury� Anatomic shunt� Any heart dysfunction� Hypovolemia� Anemia� High oxygen consumption� Hyperthermia� Muscular activity

Starting point:
O2 demand increases / O2 supply decreases
↓↓↓↓
Compensation
Breathing rate increases Depth (amplitude) and rate of
(frequency of breathing) breathing increases
(tachypnea, polypnea) (hyperventilation, hyperpnea)
Limits: only the pCO2 decreases �
dead space activity of the
is ventilated respiratory centre
(panting) decreases
hypoventilaton
There are limits in increasing the frequency and the intensity of breathing, similarly
to limits of increasing efficacy of cardiac function.
Increase in efficiacy ofrespiration – ways of adaptation

Thank you for your attention!