2 The Anatomy and Physiology of the Stomach
Transcript of 2 The Anatomy and Physiology of the Stomach

111234567891011123456789201112345678930111234567894011123456789501112311
17
2The Anatomy and Physiology of the StomachIan R. Daniels and William H. Allum
Aims
To detail the anatomy and physiology of thestomach.
IntroductionThe stomach is the most dilated part of thedigestive tube, having a capacity of 1000–1500ml in the adult. It is situated between the end of the oesophagus and the duodenum – thebeginning of the small intestine. It lies in theepigastric, umbilical, and left hypochondrialregions of the abdomen, and occupies a recessbounded by the upper abdominal viscera, theanterior abdominal wall and the diaphragm. Ithas two openings and is described as having twoborders, although in reality the external surfaceis continuous. The relationship of the stomachto the surrounding viscera is altered by theamount of the stomach contents, the stage thatthe digestive process has reached, the degree ofdevelopment of the gastric musculature, and thecondition of the adjacent intestines. However,borders are assigned by the attachment of theperitoneum via the greater and lesser omentum,thus dividing the stomach into an anterior andposterior surface.
The principal function of the stomach is to mix the food with acid, mucus and pepsin and then release the resulting chyme, at a con-trolled rate into the duodenum for the process
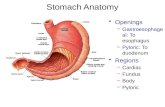
of absorption. Gastric motility is controlled byboth neural and hormonal signals. Nervous control originates from the enteric nervous sys-tem as well as the parasympathetic (predomi-nantly vagus nerve) and sympathetic systems. A number of hormones have been shown toinfluence gastric motility – for example, bothgastrin and cholecystokinin act to relax theproximal stomach and enhance contractions in the distal stomach. Other functions of thestomach include the secretion of intrinsic factornecessary for the absorption of vitamin B12(Figure 2.1).
Anatomy
EmbryologyTowards the end of the fourth week of embry-onic development, the stomach begins to differ-entiate from the primitive foregut – a midlinetube, separated from the developing peri-cardium by the septum transversum and dor-sally to the aorta. Initially a fusiform dilationforms, beyond which the midgut opens into theyolk sac. The foregut, owing to the presence ofthe pleuroperitoneal canals on either side, isconnected to the dorsal wall by a mesentery that is continuous with the dorsal mesentery ofthe mid- and hindguts. Thus a primitive mesen-tery extends from the septum transversum tothe developing cloaca. The liver and ventralpancreas (uncinate process) develop from the

ventral aspect of the foregut and grow into theseptum transversum, thus forming a ventralmesentery – the ventral mesogastrium. As theembryonic period continues the growth of thetwo “borders” becomes notably altered and the curvature of the stomach becomes apparent(Figure 2.2). The distal end rotates ventrally andwith the increased growth of the dorsal borderthe concavity of the lesser curvature becomesapparent. With further increasing growth of the entire gut and the return of the gut to theabdominal cavity the stomach becomes rotatedalong its cranial-caudal plane so that the“stomach sac” rotates and the original rightsurface becomes dorsal and the left ventral. Theposition of the dorsal and ventral mesogastriumis affected by the rotation (Figure 2.3).
As the dorsal mesogastrium becomes in-creased in length, it folds upon itself forming thelesser omentum. This lies transverse rather than
2 · UPPER GASTROINTESTINAL SURGERY
18
1111234567891011123456789201112345678930111234567894011123456789501112311
18
Duodenum
Lesser curvature
Cardia
Oesophagus
Fundus
Body (Parietal cells: HCL Intrinsic factor Chief cells: Pepsinogen)
Greatercurvature
Antrum(gastrin)Pylorus
Figure 2.1. The regions and functions of the stomach. (Withpermission from Review of Medical Physiology, WF Ganong,13th edition, Lange Medical Press, 1987.)
a bGreatercurvaturePylorus
Anteroposterioraxix
Oesophagus
Lessercurvature
Cardia
Greatercurvature
Figure 2.3. The rotation of the stomach along its anteroposterior axis. (With permission from Langman’s Medical Embryology, 5thedition, Williams & Wilkins, Baltimore, 1985.)
Stomach
Longitudinalrotation axiis
Duodenum
Lessercurvature
Greatercurvature
a b c
Figure 2.2. a–c The rotation of the stomach along its longitudinal axis.

anteroposterior and leads to the formation ofthe lesser sac. This lies between the stomach andposterior abdominal wall, bounded laterally onthe left by the dorsal mesogastrium, anteriorlyby the stomach and laterally on the right by thedeveloping liver. The foramen of Winslow is theonly opening into the space and formed by the free border of the lesser omentum, betweenthe stomach and liver (Figure 2.4).
With the rotation of the stomach, the duo-denum is carried to the right. Initially the duodenum is fixed by a thick mesentery to the posterior abdominal wall. However, withthis rotation the duodenum comes to lie on the posterior abdominal wall and the primitivemesentery disappears. This results in the duodenum coming to lie retroperitoneally. Sim-ilarly the bilary ducts and pancreas come to liewithin the concavity of the duodenum, the bileduct having passed behind its proximal part.
Within the folds of the dorsal mesogastriumthe spleen develops and this remains intimatelyattached to the stomach.
Congenital Abnormalities
Pyloric Atresia
Almost all cases of gastric atresia occur in thepyloric region and may present as a membraneoccluding the lumen, as a gap in continuity, oras a fibrous cord intervening between patentportions at the gastroduodenal junction. Thereis a reported association with epidermolysisbullosa. Clinically the condition presents asupper abdominal distension and bile-free vom-iting in the newborn. Maternal hydramniosoccurs in approximately 50% of cases.
DuplicationsTrue or complete duplication of the stomach isexceedingly rare. More common (but also rare)
incomplete duplications may be defined asspherical or tubular enteric formations which liein contiguity with the normal alimentary tractand which share with it a common blood supply,and usually a common muscle coat. These cyst-like structures, or duplication cysts, usually donot communicate with the normal lumen. Theymay have a mucosal lining and may be pedun-culated. A duplication cyst of the stomach is a communicating or non-communicating cyst lined by gastric, intestinal or pancreaticepithelium, and usually located along thegreater curvature. Occasionally it may be situ-ated in the wall of the pyloric region; in suchcases encroachment on the lumen may producegastric outlet obstruction, or an appearanceresembling infantile hypertrophic pyloric steno-sis. In non-communicating duplication cysts,accumulation of acid and pepsin may producea local inflammatory reaction, perforation,abscess formation and peritonitis.
Congenital Double Pylorus, PyloricMembrane, Web or DiaphragmCongenital double pylorus is an extremely rarecondition. A pyloric membrane is defined as athin, circumferential mucosal septum in thepyloric region, projecting intraluminally per-pendicular to the long axis of the “antrum”. Itis composed of two layers of gastric mucosa,with a central core of submucosa and muscu-laris mucosae. It is generally regarded as a con-genital anomaly and is usually associated withsymptoms and signs of gastric outlet obstruc-tion.
Ectopic Pancreatic TissueAberrant pancreatic nodules have beenreported in the upper gastrointestinal tract.Although usually in the duodenum they havebeen reported in the stomach near the pylorus.
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
19
111234567891011123456789201112345678930111234567894011123456789501112311
19
Dorsal mesogastrium Omental bursa
Stomach
Ventralmessogastriuma b c
FFigure 2.4.a–c The effect of rotation on the ventral and dorsal mesogastrium (a, b) and the formation of the lesser sac (omentalbursa) (c). (With permission from Langman’s Medical Embryology, 5th edition, Williams & Wilkins, Baltimore, 1985.)

Macroscopic AnatomyThe stomach has two openings, two curvatures,two surfaces and two omenta.
Openings
Gastro-oesophageal JunctionThe oesophagus communicates with the stom-ach via the cardiac orifice, which is situated onthe left of the midline at the level of T10. The intra-abdominal oesophagus (antrum car-diacum) is short and conical. After passingthrough the diaphragm it curves sharply to theleft, and becomes continuous with the cardiacorifice of the stomach. The right margin of theoesophagus is continuous with the lesser curva-ture of the stomach, while the left margin joinsthe greater curvature at an acute angle (incisuracardiaca).
Gastroduodenal JunctionThe pylorus forms the gastric outlet and com-municates with the duodenum. It lies to theright of the midline at the level of the upperborder of L1 and may be identified on thesurface of the stomach by a circular groove(duodeno-pyloric constriction). There has longbeen disagreement about various aspects of thestructure and function of the “gatekeeper”(Greek pyloros, from pyle = gate and ouros =guard). Willis (1682) introduced the term“antrum pylori” (Greek antron = cave) to indi-cate the part of the stomach adjoining thepylorus; no further demarcation was given.
Curvatures
Lesser Curvature (CurvaturaVentriculi Minor)This extends from the cardiac to the pyloric ori-fices, thus forming the right or posterior borderof the stomach. It is a continuation of the rightborder of the oesophagus and lies in front of the right crus of the diaphragm. It crosses thebody of L1 and ends at the pylorus. A well-demarcated notch, the incisura angularis, is seendistally although its position varies with the stateof distension of the stomach. Attached to thelesser curvature are the two layers of the hepato-gastric ligament (lesser omentum). Betweenthese two layers are the left gastric artery and theright gastric branch of the hepatic artery.
Greater Curvature (CurvaturaVentriculi Major)This is directed mainly forward, and is four tofive times longer than the lesser curvature. Itstarts from the incisura cardiaca and archesbackward, upward, and to the left; the highestpoint of the convexity is on a level with the sixthleft costal cartilage. It then descends downwardsand forwards, with a slight convexity to theleft as low as the cartilage of the ninth rib, before turning to the right, to end at the pylorus.Directly opposite the incisura angularis of the lesser curvature, the greater curvature pre-sents a dilatation, which is the left extremity of the pyloric part; this dilatation is limited on theright by a slight groove, the sulcus intermedius,which is about 2.5 cm, from the duodenopyloricconstriction. The portion between the sulcusintermedius and the duodenopyloric constric-tion is termed the pyloric antrum. At its com-mencement the greater curvature is covered atits origin by peritoneum continuous with thatcovering the front of the organ. The left part ofthe curvature gives attachment to the gastros-plenic (lineal) ligament, while to its anteriorportion are attached the two layers of the greateromentum, separated from each other by theright and left gastroepiploic vessels.
Surfaces
These change with the degree of gastric disten-sion. When the stomach is empty they may bedescribed as anterior and posterior surfaces, butwith distension become anterosuperior andpostero-inferior.
Anterosuperior SurfaceThis surface is covered by peritoneum and liesin contact with the diaphragm, which separatesit from the base of the left lung, the pericardium,the seventh–ninth ribs, and the intercostalspaces of the left side. The right half lies in rela-tion to the left and quadrate lobes of the livertogether with the anterior abdominal wall. Thetransverse colon may lie on the front part of thissurface when the stomach is collapsed.
Postero-inferior SurfaceThis surface is covered by peritoneum, exceptover a small area close to the cardiac orifice; thisarea is limited by the lines of attachment of thegastrophrenic ligament, and lies in apposition
2 · UPPER GASTROINTESTINAL SURGERY
20
1111234567891011123456789201112345678930111234567894011123456789501112311
20

with the diaphragm, and frequently with theupper portion of the left suprarenal gland. Otherrelations are to the upper part of the front of the left kidney, the anterior surface of the pan-creas, the left colic flexure, and the upper layerof the transverse mesocolon. The transversemesocolon separates the stomach from the duodenojejunal flexure and small intestine.Thus the abdominal cavity is divided into supra-and infra-colic compartments.
The anterior boundary of the lesser sac(omental bursa) is formed by this surface. Thispotential space can be accessed via an openingon the free border of the lesser omentum, which contains the common hepatic artery, the common bile duct and the portal vein (theforamen of Winslow).
Parts of the Stomach
The stomach is divided into a pyloric part andbody by a plane passing through the incisuraangularis on the lesser curvature and the leftlimit of the opposed dilatation on the greatercurvature. The body is further subdivided intothe fundus and cardia by a plane passing hori-zontally through the cardiac orifice. Distally aplane passing from the sulcus intermedius atright angles to the long axis of this portionfurther subdivides the pyloric portion. To theright of this plane lies the pyloric antrum. Atoperations, a slight groove may be seen in theserosal surface at the gastroduodenal junction.A small, superficial subserosal vein, lying withinthis groove and vertically across the front of thegut may be evident. This is the prepyloric vein(of Mayo) and drains into the right gastric vein.At operation, palpation of this area reveals the pyloric ring between the thick walls of thepyloric region and the thin walls of the duode-num.
Omenta
Lesser OmentumThis extends from the inferior and posteriorsurfaces of the liver to the stomach and proxi-mal 3.0 cm of the duodenum. The free border ofthe lesser omentum between the porta hepatisand the duodenum contains the hepatic artery,the portal vein, the common bile duct, lymphglands, lymph vessels and nerves. Behind thisfree edge is the opening into the lesser sac or
epiploic foramen (of Winslow). The remainderof the lesser omentum, extending from the leftend of the porta hepatis to the lesser curvature,contains the right and left gastric arteries andthe accompanying veins, as well as lymphglands, lymph vessels and branches of the ante-rior and posterior vagus nerves.
Greater OmentumThis is formed along the greater curvature of thestomach by the union of the peritoneal coats of the anterior and posterior gastric surfaces.On its left it shortens into the gastrosplenicomentum, containing the short gastric branchesof the splenic artery between its two layers. Onthe right it is continued for 3.0 cm along thelower border of the first part of the duodenum.From its origin the greater omentum hangsdown in front of the intestines as a loose apron,extending as far as the transverse colon, whereits two layers separate to enclose that part of thecolon. The upper part of the greater omentumcontains the greater part of the right and leftgastroepiploic arteries and their accompanyingveins, lymph vessels, lymph glands, nerve fila-ments, fat and areolar tissue.
Blood supply
Arterial Supply (Figure 2.5)
The coeliac artery, the artery of the foregut, sup-plies the stomach by its three branches. It arisesfrom the front of the aorta between the crura of the diaphragm and is a short wide trunk, surrounded by the coeliac lymph nodes andflanked by the coeliac ganglia of the sympatheticsystem. The main branches are the left gastricartery, the hepatic artery and the splenic artery.
The Left Gastric Artery.This runs to the left, gives off an ascendingoesophageal branch, and supplies the upperpart of the stomach. However, it may arisedirectly from the aorta (5–6.7%), and mayprovide one or both of the inferior phrenicarteries or a common trunk for the two. Dupli-cate arteries have been reported and sometimesan enlarged (accessory) branch (8–25% of indi-viduals) is found. This branch may replace theleft hepatic artery (11–12% of individuals). Theleft gastric artery turns downwards between the layers of the lesser omentum and runs to the
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
21
111234567891011123456789201112345678930111234567894011123456789501112311
21

right along the lesser curvature. Having dividedinto two parallel branches, these divide furthersupplying the anterior and posterior gastricwalls. These vessels anastomose freely witharteries from the greater curvature. Around theincisura angularis, the two main branches thenanastomose with the two branches of the rightgastric artery. The hepatic artery may arisedirectly from the left gastric.
The Hepatic ArteryThis is the second branch of the coeliac trunkand passes downwards as far as the first part ofthe duodenum. At the opening into right borderof the lesser sac it turns forwards (epiploic fora-men) and curves upwards between the two lay-ers of the lesser omentum towards the portahepatis, to supply the liver. The gastroduodenaland right gastric arteries are given off as it turnsinto the lesser omentum. The right gastric arterypasses to the left between the two layers of thelesser omentum, and runs along the lesser cur-vature of the stomach before dividing into twobranches that anastomose with the branches ofthe left gastric artery. It also gives off branches to
the anterior and posterior gastric walls, anasto-mosing with branches from the right gastro-epiploic artery. The gastroduodenal arterydescends behind the first part of the duodenum,which it supplies by multiple small branches.The terminal divisions are the superior pancre-aticoduodenal artery, supplying the second partof the duodenum and head of the pancreas, andthe right gastroepiploic artery. The right gas-troepiploic artery passes along the greater cur-vature of the stomach between the layers of thegreater omentum and gives off branches to the anterior and posterior gastric walls before anastomosing with the left gastroepiploic artery.
The Splenic ArteryThis passes to the left along the upper border ofthe pancreas, behind the peritoneum and thestomach, to supply the spleen. Division into the terminal branches close to the spleen iscalled a magistral splenic (~1–2 cm from thehilum), but earlier division is called a distribut-ing splenic. During its course it gives offbranches to the pancreas; just before enteringthe splenic hilum it gives off the short gastric
2 · UPPER GASTROINTESTINAL SURGERY
22
1111234567891011123456789201112345678930111234567894011123456789501112311
22
Oesophageal branchesOesophageal hiatus of diaphragm
Right gastric arteryShort gastric arteries
Splenic artery
Left gastroepiploic artery
Right gastroepiploic arterySuperior pancreaticoduodenal artery
Gastroduodenal artery
Hepatic artery
AortaDoeliac artery
Left gastric artery
Figure 2.5. The arterial supply of the stomach. (With permission from Clinical Anatomy for Medical Students, 6th edition, RS Snell,p. 207, Fig. 5–14, Lippincott Williams & Wilkins, Philadelphia, 2000.)

arteries supplying the gastric fornix, and the leftgastroepiploic artery. The latter passes down-wards and to the right along the greater curva-ture of the stomach, between the two layers ofthe greater omentum, to anastomose with theright gastroepiploic artery at the mid-portion of the greater curvature. It gives off branches tothe anterior and posterior gastric walls, whichanastomose with branches of the gastric arter-ies along the lesser curvature. These arterialarcades ramify through the submucosa, forminga rich arterial network from which branchesarise to supply the mucous membrane. There-fore the mucosa is not supplied by end arteries,with the possible exception of the mucosa alongthe lessercurvature, which appears to receive itsarterial supply directly from branches of theright and left gastric arteries.
Multiple variations of the splenic artery arereported. Commonly it may divide into twobranches that reunite with the splenic veinpassing through the loop thus formed. It maygive rise to branches normally derived fromother vessels, such as the left gastric, middlecolic and left hepatic. The short gastric arteriesmay arise from the gastroepiploic artery, thesplenic artery proper, the splenic branches ofthe splenic artery, or any combination thereof.Similarly the left gastroepiploic artery may orig-inate from one of the splenic branches. In athird of cases the dorsal pancreatic artery mayalso arise from the splenic artery.
Multiple small branches from the hepatic andgastroduodenal arteries supply the first 2 cm of the duodenum. This part of the duodenumoccupies the embryological transition zonebetween the coeliac and superior mesentericvascular supplies, and the vessels, which supplyit vary considerably in their size and mode oforigin. This variation in blood supply maypartly account for the frequency of ulceration.
The coeliac trunk may lack one or more of itsmain branches. These may arise from the aortaor the superior mesenteric, either indepen-dently or in conjunction with another branch.The following variations have been reported:
1. Hepatosplenogastric trunk2. Hepatosplenic trunk (hepatic and
splenic)3. Hepatosplenomesenteric trunk (hepatic,
splenic and superior mesenteric)
4. Hepatogastric trunk (hepatic and leftgastric)
5. Splenogastric trunk (splenic and leftgastric)
6. Coeliacomesenteric trunk (superiormesenteric in conjunction with hepato-splenogastric trunk)
7. Coeliacocolic trunk (middle or accessorymiddle colic arising from the coeliactrunk is extremely rare).
A posterior gastric artery, a branch of thesplenic, is reported to be present in 48–68% ofindividuals and forms another source of theblood supply to the superior portion of the pos-terior gastric wall. It may also supply a superiorpolar artery to the spleen. These vessels have a“hidden” posterior location and may be over-looked, leading to the possibility of dangerousbleeding if damaged.
Venous Drainage
The gastric veins are similar in position to that of the arteries along the lesser and greatercurvatures. These veins drain either directly or indirectly into the portal system. The majorveins are:
1. Left gastric vein. This runs to the leftalong the lesser curvature, receiving theoesophageal veins below the oesophagealhiatus in the diaphragm. It usually drainsdirectly into the portal vein at the supe-rior border of the pancreas.
2. Right gastric vein. This runs along thelesser curvature to the right towards the pylorus. Posterior to the first part ofthe duodenum it joins the portal vein. Italso receives the prepyloric vein whichreceives the veins from the first 2 cm ofthe duodenum.
3. Left gastroepiploic vein. This passes tothe left along the greater curvature andwith the short gastric veins drains intothe splenic vein or its tributaries. Thesplenic vein is joined with tributariesfrom the pancreas as well as the inferiormesenteric vein; these ultimately formthe portal vein with the superior mesen-teric vein.
4. Right gastroepiploic vein. This runs tothe right as far as the head of the pan-
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
23
111234567891011123456789201112345678930111234567894011123456789501112311
23

creas. Usually it joins the superiormesenteric vein and thus drains into the portal vein. However, considerablevariations may occur and the right gas-troepiploic may enter the portal veindirectly, or it may join the splenic vein.There is no gastroduodenal vein.
Lymphatic DrainageThe gastric lymphatics arise in the subepithelialinterglandular tissue of the mucosa. They passoutwards between the glands to communicatewith each other in the periglandular plexus and from here the channels proceed into thesubglandular plexus between the glands andmuscularis mucosae. Short vessels passingthrough the muscularis mucosae form the submucous plexus. Larger vessels draining thisplexus then pass through the muscular coatsbefore communicating with the networksamong the muscle fibres, and opening into thesubserous plexus. From this subserosal plexus,valved collecting vessels radiate to the curva-tures of the stomach to enter the omenta.
The lymphatics of the stomach can be dividedinto three systems:
1. Intramural. This consists of three net-works; submucosal, intermuscular andsubserosal. The submucosal lymphaticchannels communicate freely through-out the submucosa of the stomach and to a lesser degree with the submucosallymphatics of the duodenum; they alsocommunicate freely with the intermus-cular and subserosal networks.
2. Intermediary. This consists of numeroussmall channels between the subserosalnetwork and the extramural collectingsystems.
3. Extramural. This consists of four majorzones of lymphatic drainage, corre-sponding to the arterial supply of thestomach. Ultimately all zones drain intothe coeliac nodes around the coeliacarterial trunk on the anterior aspect ofthe aorta.
The lymphatic drainage of the stomach can bedivided into four zones [1]. (Figures 2.6 and 2.7):
• Zone 1. This comprises the upper two-thirds of the lesser curvature and a large
part of the body of the stomach. Thesedrain into the left gastric nodes lyingalong the left gastric artery. These nodesare joined by lymphatics coming downfrom the lower part of the oesophagus,and their efferents proceed to the coeliacnodes.
• Zone 2. This is from the distal part of the lesser curvature, including the lessercurvature of the pyloric region, to thesuprapyloric nodes along the rightgastric artery. Efferent channels from thesuprapyloric nodes drain to the hepaticand ultimately to the coeliac and aorticnodes.
• Zone 3. This zone includes the pyloricpart of the stomach as well as the righthalf of the greater curvature. The lym-phatics from these areas drain into theright gastroepiploic nodes in the gastro-colic ligament, lying along the right gas-troepiploic vessels, and into the pyloricnodes on the anterior surface of the headof the pancreas. The direction of lymphflow is from above downwards, towardsthe pylorus and the nodes between thehead of the pancreas and second part ofthe duodenum. From these groups, col-lectively called the subpyloric glands
2 · UPPER GASTROINTESTINAL SURGERY
24
1111234567891011123456789201112345678930111234567894011123456789501112311
24
Zone 1
Zone 2
Zone 3
Zone 4
Figure 2.6. Zonal drainage of the gastric lymphatics. (Withpermission from Last’s Anatomy, 10th edition, p. 245, Fig. 5.27,CS Sinnatamby (ed), Churchill Livingstone, London, 2001.)

(which also drain the first part of theduodenum), efferent vessels pass alongthe gastroduodenal artery to the hepaticnodes along the hepatic artery, andthence to the coeliac nodes.
• Zone 4. This comprises the left half ofthe greater curvature and the gastricfornix. The lymph vessels from here pass to the left gastroepiploic nodes,lying along the left gastroepiploic artery.These drain to the pancreatico-lienalnodes along the splenic artery, beforeterminating in the coeliac nodes.
NervesThe autonomic nervous system consists of twocomponents, cholinergic – mostly parasympa-thetic, and adrenergic – mostly sympatheticnerves. However, a third component of theautonomic system, which is neither cholinergicnor adrenergic, has been recognised within thegastrointestinal tract – the peptidergic system.They release a purine nucleotide as the activesubstance. An increasing number of peptidesthat are released have been recognised and this
has led to the concept of a three-part autonomiccontrol system consisting of cholinergic, adren-ergic and peptidergic nerves. These peptides areunique with a dual localisation in endocrinecells and peripheral nerves in the walls of thegastrointestinal tract.
Parasympathetic Nerve Supply
The anterior and posterior vagal trunks andtheir branches form the parasympathetic nervesupply to the stomach. Afferent fibres are alsopresent in the vagi.
Anterior VagusThis is derived mainly from the left vagus nerve but also includes fibres from the rightvagus and also some sympathetic fibres fromthe splanchnic nerves. It enters the abdominalcavity through the oesophageal hiatus in thediaphragm. It is usually single but may bedivided into multiple trunks. Having given offseveral fine branches to the lower end of theoesophagus and cardiac part of the stomach, theanterior trunk breaks up into its main branches.Latarjet’s classic description of the nerves is that
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
25
111234567891011123456789201112345678930111234567894011123456789501112311
25
Lymphatics from lower third of oesophagus
Left gastric nodes
Right gastric nodes
Coeliac nodes
Hepatic nodes
Gastroduodenal nodes
Right gastroepiploic nodes
Left gastroepiploic nodes
Splenic nodes
‘Short gastric’ nodes
Figure 2.7. The nodal lymphatics. (With permission from Clinical Anatomy for Medical Students 6th edition, RS Snell, p. 207, Fig.5–15, Lippincott Williams & Wilkins, Philadelphia, 2000.)

three main sets of branches are present [2](Figure 2.8) These are:
• Set 1. This consists of four to five directbranches, emanating “one below theother” to supply the upper part of the lesser curvature. These nerves do notform a plexus. A few filaments from thesympathetic supply join these directbranches via the coeliac plexus. One ofthe branches in this group is very distinctand Latarjet called it the “principal ante-rior nerve of the lesser curvature”. Itinnervates the area from the cardia to the pylorus.
• Set 2. Branches from the vagal supply tothe liver. There are usually three to fivenerves and they descend in the lesseromentum, on to the superior margin ofthe pylorus and first part of the duode-num.
• Set 3. These consist of vagal filamentsfrom the hepatic branches. These accom-pany the sympathetic nerves along theright gastroepiploic artery and providevagal fibres to the inferior margin of thepylorus.
Latarjet divided the nerves of the anteriorvagus into two distinct functional divisions. Thefirst division, consisting of the direct branches,supplies the fornix and body, i.e. the “reservoir”
part of the stomach. The second division,through the hepatic branches, supplies thepylorus and first part of the duodenum, i.e. the “sphincteric” part of the stomach.
Posterior VagusThis is mainly formed by fibres from the rightvagus nerve and enters the abdomen posteriorto the oesophagus. After entering the abdomenit divides into two main branches: the coeliacand the posterior gastric. It then continuesalong the lesser curvature innervating the pos-terior gastric wall although only extending tothe incisura angularis. The lowest branch issometimes referred to as “the posterior nerve ofLatarjet”. These nerves do not innervate thepylorus and prepyloric region.
Sympathetic Nerve Supply
This is derived almost entirely derived from the coeliac plexus. The gastric branches of thecoeliac plexus accompany the vessels supplyingthe stomach – the left gastric, hepatic andphrenic arteries. Others accompany the splenic,right gastric and gastroepiploic vessels. Fibresfrom the coeliac plexus accompany the left infe-rior phrenic artery, pass anterior to the loweroesophagus and communicate with the anteriorvagus before being distributed to the cardia andfornix. Other fibres travel with the left gastricartery and divide into three groups:
1. Those passing with the oesophageal andsuperior branches of the left gastricartery to the cardia and proximal part ofthe body of the stomach. These commu-nicate with branches of the anterior andposterior vagal trunks.
2. Those passing with the main branch ofthe left gastric artery along the lesser cur-vature to supply the anterior and poste-rior surfaces of the body of the stomachand antrum.
3. Those passing through the lesseromentum towards the porta hepatis.These communicate with hepaticbranches of the anterior vagal trunk
Fibres from the coeliac plexus pass along thehepatic artery and are distributed with itsbranches. They reach the pyloric region of the stomach with the right gastric and right gastroepiploic arteries.
2 · UPPER GASTROINTESTINAL SURGERY
26
1111234567891011123456789201112345678930111234567894011123456789501112311
26
Anterior vagaltrunk
Posterior vagaltrunk
Coeliac branch
Hepaticbranch
Pyloricbranch
Figure 2.8. The anatomy of the nerves of Laterjet. (Withpermission from Clinical Anatomy for Medical Students, 6thedition, RS Snell, p. 246, Fig. 5–28, Lippincott Williams & Wilkins,Philadelphia, 2000.)

Preganglionic sympathetic fibres end in thecoeliac ganglia. The efferent fibres emergingfrom the coeliac ganglia to accompany the arter-ies are postganglionic. Afferent visceral fibresfrom the stomach travel the same course inreverse, to ganglion cells in the posterior spinalnerve roots. However, these do not synapse inthe sympathetic ganglia.
Peptidergic SystemPeptidergic cells are derived embryologicallyfrom neuroectoderm and are referred to asAPUD cells because they synthesize monoa-mines through a process of amine precursoruptake and decarboxylation (APUD). They arealso referred to as neuroendocrine cells. A large number of biologically active peptideshave been detected in these APUD cells withinthe gut. These peptides include gastrin, vasoac-tive intestinal peptide (VIP), somatostatin,enkephalin, neurotensin and substance P.
Most of these monoamines have several mol-ecular forms or sizes, e.g. gastrin-14, gastrin-17,gastrin-34. Some are released into the circula-tion, producing their biological effects in distanttarget organs (endocrine), whilst others actlocally in the vicinity of their site of origin(paracrine) and some function as neurotrans-mitters (neurocrine).
Microscopic AnatomyThe wall of the stomach and the proximal 3.0 cm of the duodenum are composed of fourcoats. From without inwards these are theserous, muscular, submucous and mucouscoats. The mucous coat is separated from theluminal contents by a layer of gastric mucus.
Serous Coat (Adventitia)This is formed by the peritoneum, which is athin layer of loose connective tissue coveredwith mesothelium. It is attached to the muscu-lar coat, except at the greater and lesser curva-tures, where it is continuous with the greaterand lesser omentum respectively. Owing to itsperitoneal attachments the proximal 3.0 cm ofthe duodenum, i.e. the proximal half of the firstpart of the duodenum, the duodenal bulb, ismobile. It shares the peritoneal covering of thepyloric region of the stomach and is unlike the remainder of the duodenum, which isretroperitoneal.
Muscularis Externa
Since the time of Willis (1682), there has beendisagreement about the muscular layers of thestomach. The muscularis externa is composedof smooth, unstriped or involuntary fibres andis made up of three layers: an external longitu-dinal, middle circular, and an inner obliquelayer. These inner oblique fibres are arranged ininverted U-shaped bundles over the anteriorand posterior gastric walls. They loop over thefornix and extend as far as the incisura angu-laris. Hence these fibres have no effect on the distal stomach. In this area, including thepyloric region, the muscularis externa is com-posed of outer longitudinal and inner circularlayers.
Submucous Coat
This is a layer of loose areolar tissue with someelastic fibres that lies between the muscularismucosae and the muscularis externa. It is rich in mast cells, macrophages, lymphocytes,eosinophilic leucocytes and plasma cells.Within this layer the vessels and nerves dividebefore entering the mucous membrane. It con-tains arteries, veins, lymphatics and Meissner’snerve plexuses. These plexuses form part of theautonomic nervous system and contain post-ganglionic sympathetic fibres as well as pre- andpostglanglionic parasympathetic fibres.
Unlike the duodenum (glands of Brunner), inthe stomach the submucous layer does notcontain any glands. However, it is wider thanthat of the duodenum and extends into therugae of the stomach, forming the core of eachmucosal fold.
Mucosa
This consists of three components, the muscu-laris mucosae, the lamina propria, and theepithelial lining.
Muscularis MucosaeThis is a thin layer of smooth muscle that formsthe border between the mucosa and submucosa.It has outer longitudinal and inner circularfibres and fibres extend from the inner layerthrough the lamina propria around the gastricglands and toward the gastric lumen. These maycompress the glands and aid their emptying.
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
27
111234567891011123456789201112345678930111234567894011123456789501112311
27

Lamina PropriaThis layer consists of a delicate network of col-lagenous and reticular fibres and a few fibrob-lasts or reticular cells. It lies between themuscularis mucosae and the surface epithelialcells with their glands and extends into the areabetween the necks of the glands forming abasement membrane. It is thin in the fundusand body, where the gastric glands are numer-ous and closely packed, but is more prominentin the cardiac and pyloric zones. It also containsplasma cells, mast cells, eosinophilic leucocytesand lymphocytes. Local accumulations of lym-phocytes may occur in the cardiac and pyloricregions. Strands of smooth muscle from themuscularis mucosae traverse this layer, whichalso contains fine capillaries, lymphatic vesselsand nerve fibres.
Epithelial LiningA layer of simple columnar cells covers theentire luminal surface of the mucosa. However,the surface contains numerous tubular invagi-nations – gastric pits or foveolae. The pits aredeeper in the pyloric region than elsewhere inthe remainder of the stomach, extending at leasthalfway to the muscularis mucosae. They are V-shaped, tapering off into the glands that openinto them.
The mucus-secreting columnar cells liningthe luminal surface and the pits are joined bytight junctions. This may act as one of the mech-anisms to protect the underlying layers againstluminal acid. The supranuclear portions of thecells contain dense, homogeneous, spherical orovoid granules consisting of a type of mucigen,which upon release into the lumen gives rise tothe layer of mucus that covers the luminalsurface of the mucosa. In the cells of the gastricpits, the granules become progressively lessabundant at deeper levels, and in the bottom ofthe pits they form only a thin layer immediatelybeneath the cell surface. These cells continueinto the necks of the gastric glands. Under phys-iological conditions, the surface mucous cellsare continuously desquamated into the lumenand are completely replaced every 3 days. Newlyformed cells appear in the deeper parts of thefoveolae and in the necks of the glands; theseare slowly displaced upward and continuallyreplace those lost on the surface.
Mucosal Zones
The mucous membrane of the entire stomach islined by glands that open into the gastric pits.The blind ends of the glands extending into the mucosa are slightly expanded and coiled,sometimes dividing into two or three branches(Figure 2.9). The gastric mucosa can be dividedinto three zones, based on the predominant celltypes within the glands (Tables 2.1 and 2.2).
2 · UPPER GASTROINTESTINAL SURGERY
28
1111234567891011123456789201112345678930111234567894011123456789501112311
28
Surfacemucous cells
Gastric pit
Laminapropria
Mucousneck cells
Parietal cells
Chief cells
Argentaffin cell
Figure 2.9. The gastric glands. (Reproduced with permissionfrom Applied Physiology for Critical Care, MA Glasby, CL-HHuang, 1st Edition, 1995, Fig. 34.1, p. 337, ButterworthHeinemann Oxford.)

Cardiac Zone
This is a narrow, ring-shaped area around the gastro-oesophageal junction, containing thecardiac glands. These glands have wide luminaand shallow pits and are composed of mucus-secreting cells. This zone may contain a fewAPUD cells that synthesise monoamines. In thetransitional area, where this zone is continuouswith the oxyntic zone, a few parietal cells maybe present. The glands of the cardiac zonesecrete mucus.
Oxyntic Zone
This comprises the proximal two-thirds or more of the stomach. The glands are known asfundic glands, proper gastric glands or princi-pal gastric glands. One of their most importantproperties is the secretion of gastric acid. Theterm oxyntic (Greek: acid- forming) is also usedas an indicator of this glandular zone. Themucosa here is much deeper than in the cardiaczone and contains a greater number of glands.The pits are shallow, but the glands extendingfrom the bottoms of the pits are longer than thepits are deep.
Each principal gastric gland is composed offour kinds of cells:
1. Chief, zymogenic or peptic cells. Theirsecretory granules contain the precur-sors of pepsin.
2. Parietal or oxyntic cells. These are mostnumerous in the necks of the glands, butdo not border directly onto the lumen,being separated from it by the pepticcells. They are triangular in shape, withthe apex projecting towards the lumenbetween the sides of two peptic cells.These cells are intensely acidophilic, andcontain the gastric proton pump mecha-nism that produces the hydrochloricacid. They may also contain intrinsicfactor.
3. Neck mucous cells. These cells resemblethe mucous cells of the cardiac andpyloric zones. They lie between the pari-etal cells in the necks of the glands but aresmaller than the surface mucous cells.Their mucigen granules are larger andless dense than those of the surface cells.
4. Neuroendocrine cells. These are small,granulated cells that occur sporadicallywithin the gastric mucosa. They synthe-sise and store serotonin (5-hydroxy-tryptamine, 5-HT). They are much morenumerous in the pyloric zone.
Pyloric ZoneThis comprises the distal third of the stomachand extends further along the lesser curvaturethan the greater. The pits are the deepest withinthe stomach and extend into the mucous mem-brane for half its thickness. These glands branchmore extensively and the tubules are coiled.They contain the following types of cells:
1. Mucous cells. These are similar to theneck mucous cells of the oxyntic glandsand constitute the majority of cells in the pyloric glands. They have a pale cyto-plasm containing indistinct granules, the nucleus is often flattened against thebase of a cell, and short microvillicovered by a layer of mucus are presenton the luminal surface.
2. Parietal cells. A few isolated parietal cellsmay be present among the mucous cells. Parietal cells also occur in the tran-sitional region between the pyloric andoxyntic zones.
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
29
111234567891011123456789201112345678930111234567894011123456789501112311
29
Table 2.1. Summary of the mucosal zones
Oxyntic zone These glands produce nearly all theenzymes and hydrochloric acid secreted inthe stomach as well as producing mucus
Cardiac zone These glands secrete mucusPyloric zone These glands secrete mucus. They also
produce endocrine, paracrine or neurocrineregulatory peptides by virtue of the APUDcells contained in their glands
Table 2.2. The secretory epithelial cells and their roles
Four major types of secretory epithelial cells cover thesurface of the stomach and extend down into gastric pits and glands:
Mucous cells: secrete alkaline mucus that protexts the epithelium against shear stress and acid
Parietal cells: secrete hydrochloric acid
Chief cells: secrete pepsin, a proteolytic enzyme
G cells: secrete the hormone gastrin

3. Neuroendocrine cells. These cells aremuch more numerous in the pyloric than in the cardiac and oxyntic zonesalthough when compared with themucous cells they are still relatively fewin number. With light microscopy theyhave been called enterochromaffin cells.With electron microscopy their cyto-plasmic granules are clearly visible afterstaining with chromium or silver salts.On the basis of their staining reactions,the cells have been divided into twotypes: argentaffin cells, in which thegranules reduce silver without pretreat-ment, and argyrophilic cells, in which areducing substance is required beforethe granules will react with silver.
The mucosal zones of the stomach are notsharply defined, the glands of one region minglewith those of the adjoining region and interme-diate glands may be present between themucosal zones.
PhysiologyGastric SecretionsThe cells of the gastric glands secrete about 2500ml of gastric juice daily. This contains a varietyof substances and gastric enzymes, whose roleis to kill ingested bacteria, aid protein digestion,stimulate the flow of bilary and pancreatic juicesand provide the necessary pH for pepsin tobegin protein degradation (Table 2.3).
Mucus Secretion
The most abundant epithelial cells are mucus-secreting columnar cells, which cover the entireluminal surface and extend down into theglands as “mucous neck cells”. These cellssecrete bicarbonate-rich mucus that coats andlubricates the gastric surface, and serves an
important role in protecting the epitheliumfrom acid and other chemical insults. It is madeup of glycoprotein subunits bound by disul-phide bonds and forms a water-insoluble gelthat is impermeable to H+ ions. Production isstimulated by luminal acid and vagal activity,and is increased by prostaglandins. Thereforeaspirin non-steroidal anti-inflammatory drugs(NSAIDs) increase the damage to the stomachby inhibiting prostaglandin formation as well as by crystallising out in the gastric cells.Bicarbonate is also secreted from parietal cells. These epithelial barrier cells are veryadherent due to tight junctions between them.After epithelial disruption the cells migratealong the exposed basement membrane to fill in the defect and then stick tightly together.Gastric cells also can turn over rapidly inresponse to injury, as there is a rich mucosalblood flow providing oxygen, bicarbonate andnutrients and removing acid. Blood flow is normally increased simultaneously with acidsecretion and is reduced by aspirin and alcohol.
Pepsinogen SecretionThe chief cells secrete pepsinogens, contained inzymogen granules. These are the precursors ofthe pepsins (proteases) in gastric juice. Oncesecreted, pepsinogen I is activated by the pres-ence of gastric acid into the active proteasepepsin. This is an endopeptidase that is largelyresponsible for the initiation of protein diges-tion into smaller peptides and polypeptides. Itsplits the long amino acid chains in the regionof peptide bonds containing aromatic aminoacids. It acts at pH 1.5–2.5 and above pH 5.4 isinactivated. It is released mainly by vagal stim-ulation but also by histamine gastrin secretion,alcohol, cortisol, caffeine and acetazolamide.Pepsinogen release may also occur duringperiods of hypoglycaemia and prolongedincreased intracranial pressure.
Hormone SecretionThe principal hormone secreted from thegastric epithelium is gastrin, a peptide that isimportant in control of acid secretion andgastric motility (see below).
Other SecretionsGastric epithelial cells secrete a number of otherenzymes, including an acid-resistant lipase and
2 · UPPER GASTROINTESTINAL SURGERY
30
1111234567891011123456789201112345678930111234567894011123456789501112311
30
Table 2.3. Contents of normal (fasting) gastric juice
Cations: Na+, K+, Mg2+, H+
Anions: Cl–, HPO42–, SO4
2–
Pepsins: I–IIIGelatinaseMucusIntrinsic factorWater

gelatinase. The lipase hydrolyses triglycerides of medium- and short-chain fatty acids intoglycerol and free fatty acids.
Intrinsic factor, a glycoprotein secreted byparietal cells, is necessary for intestinal absorp-tion of vitamin B12. It acts by combining withthe vitamin B12 and is necessary for its attach-ment to receptors in the terminal ileum. Lack ofintrinsic factor due to reduction in parietal cellmass following gastric surgery, or the produc-tion of antibodies to the cells, called perniciousanaemia, leads to megaloblastic anaemia.Secretion of intrinsic factor occurs followingvagal, gastrin or histamine stimulation of theparietal cells.
The Formation and Secretion ofGastric AcidStimulation of the parietal cells results in acidsecretion (Figure 2.10). These cells contain multiple tubulovesicular structures within theircytoplasm that on stimulation move to themucosal membrane and fuse with it, producinga microvillous appearance that increases thesurface area. This results in the presence of the H+-K+ ATPase that transports the H+ ontothe luminal surface. This secretion is isotonicwith other fluids and its pH is <1.
The H+ is obtained from the ionisation ofwater, which is then actively transported intothe gastric lumen in exchange for K+ that hasbeen recycled from the membrane. Chlorideions are also actively transported into thegastric lumen. The resulting OH– ion is neu-tralised by the carbonic acid buffer system toform a bicarbonate ion that diffuses into theinterstitium to be replaced by a further Cl– ion.There is a HCO3
––Cl– exchange mechanismwithin the interstitium, but Cl– also enters thecell with Na+. The carbonic acid is replenishedby the hydration of CO2, which is produced by cellular metabolism from the abundance ofcarbonic anhydrase within the mucosa. After ameal this results in the development of a nega-tive respiratory quotient; thus arterial CO2 ishigher than venous and the gastric venousreturn is alkaline with a high HCO3
– content.
Gastric Hormones
Gastrin
Experiments in the early twentieth centuryusing injected extract of pyloric mucosa stimu-lated secretion of gastric acid and pepsinogen.This action was thought to be hormonal inorigin and the active substance was calledgastrin [3]. However, this theory was initiallydisputed because this action was similar to thatof histamine and the isolation of gastrin was notperformed until the late 1960s when two relatedheptadecapeptides were identified from hogantral mucosa. These heptadecapeptides wereisolated in the pyloric zone. The highest densityof gastrin-producing G cells occurs in the distal3.0 cm of the stomach, where the concentrationof gastrin is 500 times higher than in the bodyof the stomach. The first part of the duodenumalso contains a significant level of G cells. Thesecells originate from neuroectoderm togetherwith other cells of the APUD series.
Microscopically they are piriform in shapeand located in the mid and deep zones of thepyloric mucosal glands. Electron microscopyshows that they possess microvilli extendinginto the lumen and that secretory granules arepresent in the basal parts of the cells. This allowsfor secretion of hormone into the bloodstreamin response to luminal stimuli.
There are two main types of gastrin, gastrin Iand gastrin II, produced predominantly by the
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
31
111234567891011123456789201112345678930111234567894011123456789501112311
31
Interstitialfluid
Gastricjuice
Carbonicanhydrase
Cl– Cl–
A
HCO3
H+ H+ OH–
K+ H+ + HCO3–
H2O + CO3
H2O
Parietal cell
H2 CO3
Figure 2.10. Hydrochloric acid production from the parietal cell.

G cells of the pyloric mucosal zone. Othersources are the duodenal G cells, D cells in theislands of Langerhans in the pancreas, and iso-lated G cells in the proximal-acid-producingregion of the fornix and body of the stomach.
Gastrin 17 (17 amino acids) is the predomi-nant form in the pyloric antrum, and is furthersubdivided into a non-sulphated gastrin I and asulphated gastrin II form. There is also a “big”gastrin (G34) containing 34 amino acids and a“big big” gastrin with many more amino acids.“Mini” gastrin containing 14 amino acids canalso be isolated, but is less active than G17. The common factor in all the molecules is theC-terminal tetrapeptide Tyr-Met-Asp-Phe-NH2.
Fasting levels of gastrin are increased by achlorhydria associated with perniciousanaemia, any form of surgical vagotomy,Zollinger–Ellison syndrome (gastrinoma),chronic renal failure and massive small bowelresection.
Its physiological and pharmacological effectsare summarised in Table 2.4.
Somatostatin
Somatostatin is a tetradecapeptide that was initially found to inhibit the release of growthhormone (GH) from the pituitary gland.However, it has subsequently been identifiedwidely in the central nervous system, the gas-trointestinal tract and other organs, with thehighest concentration being found in the pan-creas. In the stomach it is found in the pyloricand oxyntic mucosal zones but not in thecardiac zone. Within the pancreas it is isolatedfrom the islet D cells.
Although initially thought only to suppressthe secretion of growth hormone, it also pos-sesses a wide variety of inhibitory actions onother pituitary and extrapituitary secretions. Itsuppresses the release of thyroid-stimulatinghormone by the pituitary, the release of gluca-gon, insulin and exocrine secretions by the pancreas, the secretion of cholecystokinin,motilin and secretin by the intestine, and thesecretion of gastrin, gastric acid and pepsin bythe stomach.
Somatostatin suppresses gastric acid secre-tion by direct action on the parietal cells of thecardiac and oxyntic mucosal zones. Thus bylowering the pH, it also inhibits the secretion ofgastrin through a feedback loop of low pH sup-pressing both gastric acid and gastrin secretion.
Vasoactive Intestinal Peptide (VIP)
Vasoactive intestinal peptide (VIP) is a polypep-tide with strong vascular effects isolated fromsmall intestine. It has been subsequentlydemonstrated in central and peripheral neu-rones, suggesting a neurotransmitter function.In the peripheral autonomic system VIP nerves occur in various regions, including thesuperior and inferior mesenteric ganglia, andthe submucous (Meissner’s) and myenteric(Auerbach’s) plexuses of the intestinal wall.Structures believed to exert a sphincteric func-tion receive a particularly rich supply of VIPnerves, more so than the smooth muscle of adjacent regions. Among these are the oesoph-agogastric junction, the pyloric “sphincter”,sphincter of Oddi, internal anal sphincter, andthe openings of the ureters and urethra into thetrigonum of the bladder.
In the stomach these nerves are found aroundoxyntic and pyloric mucosal glands. In the duo-denum VIP (and substance P) is present innerves in the villi and muscularis mucosae andaround blood vessels and between the lobules ofBrunner’s glands. Its actions include vasodilata-tion, thus lowering blood pressure, increasedcardiac output, glycogenolysis and relaxation ofsmooth muscle. In the stomach there is signifi-cant inhibition of gastric secretion associatedwith VIP release. It probably acts as a neuro-transmitter in a paracrine, rather than in anendocrine, way. The VIP neurones have beenshown to be under dual (both vagal andsplanchnic) control of the autonomic system.
2 · UPPER GASTROINTESTINAL SURGERY
32
1111234567891011123456789201112345678930111234567894011123456789501112311
32
Table 2.4. The physiological and pharmacological effects ofgastrin
Gastrin causes: Parietal cells to stimulate acid secretionPepsin and intrinsic factor secretionIncreased mitotic activity in the stomachand small bowel mucosaContraction of the lower oesophagealsphincterThe release of insulin, glucagon andcalcitoninPancreatic stimulation and bile flowSmall bowel secretionGastric and small bowel motility toincreaseThe gastrocolic reflex

Substance P
In the gastrointestinal tract nerve fibres andneurones containing substance P (11-amino-acid peptide) are encountered along its entirelength. However, they are least prominent in theoesophagus and upper part of the stomach, butthe highest concentrations occur in the duode-num. These neurones are located mainly in themyenteric plexuses. Here the nerve fibres richlyinnervate the circular musculature. However,the longitudinal muscle contains only a sparsenetwork of fibres. Substance P may also bevasoactive as the nerve fibres are also found inclose contact with blood vessels.
In the stomach substance P is found in theoxyntic zone in a few, thin fibres only and infibres interconnecting in the pyloric antrum. Inthe duodenum substance P (and VIP) is presentin nerve networks in the villi as well as in themuscularis mucosae and around blood vessels.It has been found to cause contraction of themuscularis mucosae.
Other Gastric Hormones
EncephalinThese are endogenous opiate-like compoundsforming two pentapeptides, endorphin andenkephalin. They can be isolated throughout the gastrointestinal tract, although the highestconcentration is found in the pyloric antrum.The role of these peptides is not clear.
GalaninGalanin may act as a regulatory factor in thecontrol of gastrointestinal motility. It is usuallyfound in close association with VIP-containingnerves.
NeurotensinThis is secreted by N cells in ileal mucosa.However, small traces occur in the pyloricmucosal zone. The neurotensin level rises aftera meal, but its function is still unclear. It mayinhibit pentagastrin-stimulated gastric acid andpepsin secretion after a meal as well as delayinggastric emptying, resulting in the controlledrelease of chyme into the small intestine.
Absorption from the StomachThe stomach absorbs very few substances. Fatsare not absorbed. Polypetides are absorbed only
slightly. Sugars are absorbed to an extent andthis varies with the sugar and its concentration.Galactose is most readily absorbed followed byglucose, lactose, fructose and finally sucrose.Low concentrations of sugars are absorbed veryslowly. Ethyl alcohol is absorbed fairly rapidlyas are other lipid-soluble compounds includingaspirin and other NSAIDs. These substances arealso well-recognised causes of gastric irritationand their use (especially overuse) is commonlyassociated with development of gastritis andgastric ulcers. The stomach absorbs waterreadily with half the ingested volume absorbedin about 20 minutes.
Regulation of Gastric Secretionand MotilityGastric function is classified into three phases inwhich secretory and motor activities are closelylinked.
Control of Gastric Acid Secretion
Acid secretion may be divided into two phases interprandial, when acid secretion is 1–5 mmol/h, and stimulated where acid secre-tion is maximally 20–35 mmol/h. This is furthersubdivided into cephalic, gastric and intestinalphase. Normal subjects maximally secrete 0.5 mmol/h/kg body weight)
InterprandialResting secretion occurs in the absence of allintestinal stimulation. However, to abolish all gastic acid secretions, a bilateral vagotomy(truncal) and excision of the pyloric antrumwould be necessary.
Stimulated SecretionThe Cephalic Phase (Figure 2.11). The cephalicphase is initiated by seeing, smelling and antic-ipating food. These influences act on the limbicsystem and hypothalamus and these nucleistimulate the dorsal motor nucleus of the vagus.This stimulus is transmitted thought the vagusnerve to the enteric nervous system, resulting inrelease of acetylcholine in the vicinity of G cellsand parietal cells. Binding of acetylcholine to its receptor on G cells induces secretion of thehormone gastrin, which, in concert with acetyl-choline and histamine, stimulates parietal cellsto secrete small amounts of acid. Additionally,a low level of gastric motility is induced.
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
33
111234567891011123456789201112345678930111234567894011123456789501112311
33

The release of acetylcholine and bombesin(gastrin-releasing peptide) initiates gastrinrelease from the G cells. The gastrin passes viathe portal circulation to stimulate the parietalcells. It potentiates the effect of vagal stimula-tion, thus resulting in increased acid secretion.The parietal cells also have H2 receptors (hista-
mine) stimulated by the release of histaminefrom mast cells close to the parietal cells. Thehistamine sensitises the parietal cell to theaction of gastrin and acetylcholine. The H2receptor blockers (cimetidine and ranitidine)act on these receptors, thus reducing acid secretion.
2 · UPPER GASTROINTESTINAL SURGERY
34
1111234567891011123456789201112345678930111234567894011123456789501112311
34
ThoughtSightSmellTaste
of food
G cell
Gastrin
Parietalcell
HCl
ACh (N)
ACh (M)GRP
ACh(M)
ACh(N)
a
b HCl
X (vagus)
X (vagus)
X (vagus)
X (vagus)
X (vagus)
X (vagus)
Gastrin
G cell
Amino acids
Parietalcell
Distension ofpyloric antrum
Distensionfundus and body of stomach
SMP
SMP
MP
MP
Figure 2.11. The cephalic (a) and gastric phases (b) of acid secretion. X, vagus; ACh (N), acetylcholine (nicotinic receptor); ACh (M),acetylcholine (muscarinic receptor); GRP, gastrin-releasing peptide; SMP, submucous plexus; MP, myenteric plexus. (Reproduced withpermission from Applied Physiology for Critical Care, MA Glasby, CL-H Huang, 1st edition, 1995, Fig. 34.3, p. 340, ButterworthHeinemann, Oxford.)

The Gastric Phase (Figure 2.11). When foodenters the stomach several additional factorscome into play, foremost among them beingdistension and mucosal irritation. Distensionexcites stretch receptors and irritation activateschemoreceptors in the mucosa. These events aresensed by enteric neurones, which secrete addi-tional acetylcholine, further stimulating both Gcells and parietal cells. Gastrin from the G cellsfeeds back to the parietal cells, stimulating iteven further, mediated by vagovagal reflexesthrough the dorsal motor nucleus. Additionally,activation of the enteric nervous system andrelease of gastrin cause vigorous smooth musclecontractions. The net result is that secretory andmotor functions of the stomach are fully turnedon – acid and pepsinogen are secreted, pepsino-gen is converted into pepsin and vigorousgrinding and mixing contractions take place.
However, acid secretion may be inhibitedduring the gastric phase by local mechanisms.If the antral pH falls to 1–1.5, inhibition ofgastrin release occurs. This is mediated by twomechanisms – the effect of luminal acid on themicrovilli of the G cell and the stimulation ofsomatostatin from D cells in the antrum, whichacts inhibits directly on the G cells and parietalcells by a local paracrine effect.
The Intestinal Phase. As chyme is emptied intothe small intestine control is necessary to limitgastric empting. This probably allows the duo-denum time to neutralize the acid and efficientlyabsorb incoming nutrients. Hence, this phase ofgastric function is dominated by the small intes-tine sending inhibitory signals to the stomachto slow secretion and motility. Two types ofsignals are used: nervous and endocrine. Dis-tension of the small intestine, as well as chemi-cal and osmotic irritation of the mucosa, istransduced into gastric-inhibitory impulses in the enteric nervous system – this nervouspathway is called the enterogastric reflex. Fatand carbohydrate in the chyme cause the releaseof GIP (gastric inhibiting peptide), whichinhibits gastrin secretion. Secondly, enteric hor-mones such as cholecystokinin and secretin arereleased from cells in the small intestine andcontribute to suppression of gastric activity.Gastrin also causes the release of calcitoninfrom the C cells of the thyroid gland, whichinhibits further release of gastrin via a feedbackloop.
Collectively, enteric hormones and theenterogastric reflex put a strong brake on gastricsecretion and motility. As the ingesta in thesmall intestine is processed, these stimulidiminish, the damper on the stomach isreleased, and its secretory and motor activitiesresume.
Gastric Motility and Hunger Contraction
Resting Electrical Activity Within theStomachA pacemaker in the longitudinal muscle close tothe greater curve of the cardia controls the fre-quency of contractions. It depolarises at a rateof 3/minute, and each wave – the gastric slowwave (or basal electrical rhythm) – increasessodium permeability across the cell membraneand the impulse spreads through the longitudi-nal and circular muscles via low resistance junc-tions. These junctions make up about 12% of themembrane surface.
In the empty stomach (approximately 50 mlvolume), the resting potential is low (–50 mV)and although the waves pass at a rate of3/minute, not all of these waves are equal inamplitude and do not set off an action poten-tial. However, when the critical firing level ispassed the resulting action potential sets off anexcitation–contraction coupling and a contrac-tion spreads throughout the stomach.
Intragastric PressureIntragastric pressure remains relatively con-stant at 5 mmHg (0.7 kPa) because as foodpasses into the stomach, the musculature of thefundus and body relaxes via a feedback loop –receptive relaxation. In addition, as wall tensionrises so does the radius, thus keeping the intra-gastric pressure constant (law of Laplace).However, above 1000 ml, the radius cannotincrease in size so the wall tension and intra-gastric pressure rises.
Thus volumes above 1000 ml lead to stimula-tion of stretch receptors within the stomachwall.
Gastric ToneIn most instances gastric hypotonicity is of idiopathic origin and presumably of little clini-cal significance. More severe degrees, some-times progressing to acute gastric dilatation,may occur in a variety of conditions, e.g. post-
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
35
111234567891011123456789201112345678930111234567894011123456789501112311
35

operatively, after severe trauma and in elec-trolyte disturbances.
A short, transversely situated, “steerhorn”stomach, on the other hand, is now known to bethe result of gastric hypertonicity. In these casesimmediate emptying of liquid barium usuallycommences in the erect position, before theonset of peristalsis or cyclical contractions ofthe pyloric sphincteric cylinder.
Control of Gastric Motility
As the volume of the stomach passes 1000 mlthe intragastric wall tension rises. This activatesstretch receptors, again through a vagovagalreflex arc, which cause depolarisation in thelongitudinal and circular smooth muscles.However, this leads to every slow wave beingabove the critical firing level. An action poten-tial is therefore propagated with each slow waveand a contraction passes from the fundusthrough the body to the pyloric antrum. Thesenow occur three times per minute and the forceof the contraction also increases along thestomach. Initially low in the fundus, where the muscular layer is thinnest, at the pylorusintragastric pressure may reach 40–50 mmHg(5.3–6.7 kPa).
The pyloric sphincter is not a high-pressurezone and is open in the resting phase. As a con-traction wave arrives it contracts. However,since the canal was open before the rise in intra-gastric pressure some of the chyme passesthrough the pylorus (5–15 ml) before the gastricslow wave reaches it. When the slow wavereaches the antrum and pylorus they contracttogether – terminal contraction, and the pyloruscloses. This phase of the contraction acts torecirculate or “churn” the gastric contents. Onlywhen duodenal pressure drops due to relaxationdoes the pyloric pressure drop.
Factors Modifying Gastric MotilityBoth vagal stimuli and gastrin increase antralmotility and influence emptying. However, aftera truncal vagotomy, the force of the antral pumpis reduced and gastric emptying time is pro-longed, hence the need for a drainage procedureafter a truncal vagotomy.
The force of the pump is also moderated bythe volume and composition of the chyme.Hormonal and neuronal mechanisms also reg-ulate gastric emptying. These include duodenal
distension – via a vagal feedback loop, increasedduodenal osmolarity – via osmoreceptors, thepresence of acid in the duodenum – via a localenteric neuronal pathway, and the release of GIPand chalesystokinin by fat in the duodenum.
In addition, sympathetic stimuli reducegastric emptying via the limbic and hypothala-mic nuclei.
Hunger ContractionsWhen the stomach is empty there can be periodsof increased gastric motility several hours after a meal. With stimulation of the hypothalamusthe individual feels hungry. This leads in a rise in vagal stimulation and causes increasedgastric motility. Contraction of the empty stom-ach leads to a rise in intragastric pressure thatcan stimulate tension and pain receptors in thegastric wall, simulating mild pain or discomfort.
Changes in Physiology andFunction Related to Disease
Nausea, Retching and Vomiting
The mechanism of vomiting in mammals iscomplex and in spite of experimental studiessome aspects are still not fully understood. It isusually accepted that the vomiting sequenceconsists of three successive phases: nausea ini-tially, followed by retching, often leading toforcible expulsion of gastric contents throughthe mouth, i.e. ejection or vomiting. Duringthese stages a coordinated sequence of move-ments occurs, involving, amongst others, theupper small bowel, stomach, oesophagus,diaphragm, voluntary abdominal muscles andglottis. The complex movements of the ejectionphase occur with extreme rapidity. The action iscontrolled by the vomiting centre present bilat-erally in the medulla oblongata at the level ofthe olivary nuclei, and close to the tractus soli-tarius at the level of the dorsal vagal nuclei. Acomplex pathway mediated via efferents in thefifth, seventh, ninth, tenth and twelfth cranialnerves leads to contraction of the intercostalmuscles, diaphragm and abdominal muscles.Afferent impulses pass via the vagus (tenthcranial nerve) and sympathetic nerves to thevomiting centre. However, other impulses reachvia the labyrinth, the limbic system and thechemoreceptor trigger zone. This is situated inthe lateral wall of the fourth ventricle.
2 · UPPER GASTROINTESTINAL SURGERY
36
1111234567891011123456789201112345678930111234567894011123456789501112311
36

Nausea is the conscious recognition of thesubconscious excitation of an area known as the medulla oblongata closely associated withthe vomiting centre and can be initiated byimpulses from the gastrointestinal tract, thelower brain in association with motion sicknessor cortical impulses. Vomiting without the pro-dromal phase of nausea can occur, indicatingthat only certain portions of the vomiting centreare associated with it.
The Process of VomitingIf the upper gastrointestinal tract becomesexcessively irritated, over-distended or over-stimulated, vomiting may occur. Initially anti-peristaltic waves begin and may occur as fardown as the ileum. These waves travel at 2–3cm/s; thus within a few minutes a large volumeof intestinal contents may be pushed back intothe stomach and duodenum causing distension.This may result in retching.
Retching PhaseThe retching phase is characterized by a seriesof violent spasmodic abdomino-thoracic con-tractions with the glottis closed. During thistime the inspiratory movements of the chestwall and diaphragm are opposed by the expira-tory contractions of the abdominal muscula-ture. At the same time movements of thestomach and its contents take place. Whereas apatient will complain of disagreeable sensationsduring nausea, speech is not possible duringretching. The characteristic movements furnisha ready diagnostic sign of the retching phase.
The Vomiting ActOnce the act of vomiting has been triggered, adeep inspiratory movement occurs, with eleva-
tion of the hyoid bone, which opens the upperoesophageal sphincter and closes the glottis, thesoft palate rises to close the posterior nares andthen a downward contraction of the diaphragmwith simultaneous contraction of the abdominalwall muscles raises intragastric pressure. Withthe sudden relaxation of the lower oesophagealsphincter, expulsion occurs.
Questions
1. Outline congenital abnormalities.2. Describe lymph drainage of stomach and
relate this to surgical excision.3. Describe nerve supply.4. Name cells of the gastric wall and their
functions.
References1. Eker R. Carcinomas of the stomach: investigation of the
lymphatic spread from gastric carcinomas after totleand partial gastrectomy. Acta Chir Scand 1951;101:112–26.
2. Latarjet A, Wertheimer P. L’énervation gastrique.Données expérimentales. Déductions cliniques. J MédLyon 1921;36:1289–302.
3. Edkins J. The chemical mechanism of acid secretion. J Physiol 1906;34:133–44.
Further ReadingSinnatamby CS (ed). Last’s anatomy. Regional and applied.
10th edn. London: Churchill Livingstone, 2001.Snell RS Clinical anatomy for medical students. 6th ed.
Philadelphia: Lippincott Williams & Wilkins, 2000.
THE ANATOMY AND PHYSIOLOGY OF THE STOMACH
37
111234567891011123456789201112345678930111234567894011123456789501112311
37