Endocrine Physiology The Endocrine Pancreas Dr. Khalid Al-Regaiey.
18. endocrine pancreas
-
Upload
nasir-koko -
Category
Health & Medicine
-
view
3.959 -
download
7
Transcript of 18. endocrine pancreas

The Endocrine Pancreas


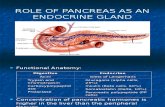
The endocrine cells of the pancreas are localized in the islets ofLangerhans and constitute only 2% of the mass of the pancreas. Thehuman pancreas contain about 1 million islets of Langerhans whichare distributed throughout the organ, but more commonly found in
the tail.

The islets are composed of:
•A or α cells (~20%), located at the periphery of the islet and secret glucagon•B or β cells (~75%), generally located at the center of the islet and secret insulin•D or δ cells (~5%), located around the periphery and release somatostatin, a paracrine inhibitor of both insulin and glucagon secretion•F cells (<2%) produce pancreatic polypeptide

Insulin
•Insulin consists of two peptide chains linked by two disulphide bonds•Insulin is released from the β cells by exocytosis in response to an increase in blood glucose•“half-life” of insulin in circulation is about 5 minutes•Insulin maintains blood glucose levels close to 5mmol/L under fasting conditions, but may temporarily rise as high as 8 mmol/L after a meal•Overweight and obese people show higher basal levels of insulin

Regulation of secretionRegulation of secretion•Elevation of plasma glucose concentration directly stimulates: - a rapid rise of insulin secretion - there is an increase in inreacellular Ca, which is responsible for releasing insulin (entry of glucose into β cells does not depend on presence of insulin)•Insulin secretion by β cells as glucose levels decline•Increased amono acid concentrations in plasma insulin secretion•Stimulation of right vagus nerve insulin secretion•Sympathetic stimulation release of insulin (α-receptor mechanism)•Gastrointestinal hormones (glucagon, gastrin, secretin and gastric inhibitory peptide) insulin release•Keto acids insulin secretion•Somatostatin, secreted by δ cells insulin secretion•Drugs (orally active) - sulphonylureas (e.g. tolbutamide) insulin secretion - glibizide/gliburide insulin secretion and promotes its action at cellular level - biguanides (e.g. phenformin) act by increasing glucose catabolism glucose absorption in the intestine - thiazide diuretics insulin secretion - diazxide (used in the treatment of hypertension) insulin secretion•Leptin basal and glucose-stimulated insulin release

Actions of InsulinActions of Insulin•Insulin binds to specific membrane receptors and triggers changes in the activity of both membrane transport proteins and intracellular enzymes•Insulin receptor number in starvation and in obesity and acromegaly•Affinity of insulin receptors in adrenocortical insufficiency but when exposed to high glucocorticoid levels

•Insulin blood glucose by facilitating glucose uptake in muscles and adipose tissue•Brain, liver, kidneys, red blood cells & intestinal mucosa are exceptions•Insulin glycogen synthesis (glycogenesis) in the liver & glycogen breakdown (glycogenolysis)•Insulin is an anabolic hormone & promotes the rate of protein synthesis by: - stimulating amino acid uptake in the liver and skeletal muscle - inhibiting protein breakdown - inhibiting conversion of amino acids to glucose (gluconeogenesis)•Insulin promotes storage of fat and decreases its utilization by: - inhibiting the breakdown of stored lipid (by hormone-sensitive lipase) free fatty acid levels in circulation - stimulating fatty acid synthesis from glucose in the liver - promoting glycerol synthesis in lipid cells - promoting carbohydrate utilization so that fat is spared (resting muscle normally oxidizes fatty acids for energy)•Insulin plasma levels of K ( cellular uptake)


Clinical•Inadequate insulin effect leads to the clinical syndrome of diabetes mellitus•A primary deficiency of insulin is classified as: type 1/insulin dependent (IDDM/juvenile onset diabetes - insulin is possibly due to autoimmune destruction of ß cells•In type 2/non-insulin dependent (NIDMM)/maturity onset diabetes: - insulin secretion is relatively unimpaired - insulin effect on the cells are inhibited/insulin resistance - mostly found in elderly, overweight patients•Occasionally, diabetes mellitus is secondary to excess secretion of a diabetogenic hormone, e.g. cortisol, growth hormone or very rarely, glucagon.

Symptoms and biochemical abnormalities
•Hypergycemia - decreased glucose uptake & utilization plasma glucose level•Glucosuria - plasma glucose ~11 mmol/L crosses renal Tmax limit excreted in urine•Polyuria - glucose within the renal tubules osmotic retention of H2O urine production (osmotic diuresis)•Polydipsia - polyuria dehydration thirst and drinking•Reduction in amino acid uptake protein synthesis negative nitrogen balance impaired growth (in children)/muscle wasting & weight loss (in adults)•Lipid mobilization plasma free fatty acid levels weight loss•Ketosis - ß-oxidation of fatty acid ketone bodies metabolic acidosis•Increased ventilation - respiratory compensation of acidosis

Treatment
•If the patient remain untreated, diabetes mellitus will eventually lead to ketotic coma and death from dehydration and acidosis - recombinant insulin treatment can lead to a good control of glucose levels.
•Cases in which hyperglycemia is associated with obesity, diet alone or diet in combination with physical exercise may be adequate
•Excess insulin hypoglycemia sympathetic activity tremor, sweating, heart rate, anxiety, may coma, could reversed by intravenous glucose/glucagon

Glucagon•Glucagon is a catabolic peptide hormone secreted by α cells of the pancreatic islets
Regulation of secretion•Glucagon secretion is directly stimulated by: - low blood glucose concentration - high levels of circulating amino acids•Somatostatin glucagon secretion•Insulin & secretin glucagon secretion•Sympathetic stimulation glucagon secretion (ß-receptor mechanism)•Vagal stimulation glucagon secretion•All forms of physical stress glucagon secretion


Actions of glucagon
•Glucagon effects oppose those of insulin, most pronounced in the liver to safeguard against hypoglycemia•Glucagon increases blood glucose levels by: - glycogenolysis in the liver ( phosphorylase) - protein breakdown in muscle - protein synthesis in the liver - formation of glucose from amino acids and glycerol ( gluconeogenesis) - fat mobilization ( hormone-sensitive lipase activity) free fatty acids in blood ( ß-oxidation) keto acid formation

Somatostatin•Somatostatin is a peptide hormone secreted by δ cells of the pancreatic islets (also produced in the hypothalamus) in response to: - blood glucose - plasma amino acids - fatty acids
•Somatostatin decreases gastrointestinal functions by: - motility - secretion - absorption •Somatostatin splanchnic blood flow
•Somatostatin release of: - insulin - glucagon

Amylin
•A pancreatic hormone, is stored in the ß cells and released together with insulin
•Amylin is a potent inhibitor of gastric emptying
•Amylin insulin secretion
•It can induce insulin resistance