15 Immunodeficiency
Transcript of 15 Immunodeficiency

Immunodeficiency
Francis Ian L. Salaver, RMT
Aileen Grace L. Ang, RMT, MAST-Bio

Definition
• A group of disorders characterized by an impaired ability to produce normal immune response. Most of these disorders are caused by mutations in genes involved in the development and function of immune organs, cells, and molecules.

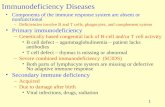
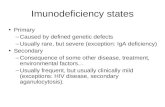
Origins of Immunodeficiency
• Primary or Congenital– Inherited genetic defects in immune cell
development or function, or inherited deficiency in a particular immune molecule
• Secondary or acquired– A loss of previously functional immunity
due to infection, toxicity, radiation, splenectomy, aging, malnutrition, etc.

44
Types of immunodeficiency disorders:
1- Primary: Causes in immune system component:a. According of component:
i. Complements.
ii. Phagocytic.
iii. B cells.
iv. T Cells.
b. According to the etiology:
i. Congenital (X-linked disease)
ii. Acquired (AIDS)
iii. Embryogenesis (DiGeorge syndrome).
iv. Idiopathic

55
Types of immunodeficiency disorders:
2- Secondary: Non Immunogenic causes:a. Prematurity
b. Mal nutrition.
c. Hodgkin`s and others malignancy.
d. Injury, Burns, Splenectomy.
e. Drugs.

Common variable immunodeficiency (CVID) X-linked agammaglobulinemia (XLA) Selective IgA deficiency (SIgAd) Selective IgG subclass deficiency (SIgGsd) Hyper IgM syndrome (HIgM) Transient hypogammaglobulinemia of Infancy (THI)
Antibody deficiencies include:

Severe combined immunodeficiency (SCID) Ataxia-Telangiectasia syndrome (AT) Wiskott-Aldrich syndrome (WAS) DiGeorge syndrome Chronic mucocutaneous candidiasis (CMCC)
Cellular deficiencies include:

Chronic granulomatous disease (CGD) Leukocyte adhesion defect (LAD) Chediak-Higashi syndrome (CHS) Swhachman syndrome (Swh.S) Hyper IgE syndrome (Job syndrome)
Complement deficiencies
Phagocytic disorders include:

Infectious Consequences of Immunodeficiency
• Antibody deficiency, Phagocyte deficiencies, or Complement protein deficiencies are associated with recurrent infections with extracellular pyogenic bacteria (pneumonia, otitis media, skin infections)
• Deficiency in Cell-mediated immunity is associated with recurrent or chronic viral, fungal, or protozoal diseases.

Infectious Consequences of Immunodeficiency
• T-cell problems often also result in B-cell problems, due to T-dependent Ag’s.
• Both, or all- bacterial, viral, problems with commensals, etc.
• Patients with immunodeficiency are also susceptible to certain types of cancer

Type of the infecting organism
• Recurrent viral, fungal, mycobacterial, or opportunistic infections suggest T-cell defects.
• Recurrent infections with invasive encapsulated bacteria (e.g: pneumococcus) suggest B-cell defects.
• Recurrent infections with bacteria of low virulence (e.g: staph) suggest a neutrophil abnormality.
• Recurrent Neisseria infections suggest terminal complement defect.

Primary Immunodeficiency: Frequency
Phagocytic18%
Antibody50%
Combined20%
Cellular10%
Complement2%
The overall prevalence of PID is about 1:2000

B Plasma IgM
B Plasma IgA
IgA
IgM
B Plasma IgG
IgG
B Plasma IgE
IgE
CD19+
CD20 +
SLSC
ProBCFU
MØPMNPletRBC
PreB
PT T
THYRUM Epi.
BMCD3+
CD8+
CD4+ TH1
TH2CTL
IFN-γ、 IL-2
IL-4 、 5 、 8 、 9、 10 、 13
Development of Immune cell




B cell Deficiencies
• X-linked Agammaglobulinemia• B cell defect
» Defect in kinase that keeps B cells in pre-B stage with H chains rearranged but L chains not
• Low levels of IgG and absence of other classes
• Recurrent bacterial infections
• Symptoms at 9 mo. to 2 yr of age
• Treat with intravenous immunoglobulin (IVIG)

X-linked Agammaglobulinemia• It is failure of B-cells to mature beyond the
pre-B cell stage in the bone marrow
• Failure is caused by mutations or deletions in the gene encoding an enzyme called B-cell tyrosine kinase (Btk)
• Btk is involved in transducing signals from the pre- B cell receptor required for continued maturation of the cells

Molecular Defects in Lymphocyte Maturation

—Bruton disease
— mutations in btk
—maturation disorder
of pre-B cell

Immunoglobulin Levels vs. Age

Antibody DeficienciesX-Linked Agammaglobulinemia
Age of onset of symptoms
4-12 months of age
Inheritance X-linked
Pathogenesis Mutations in the gene for Btk arrest in dev’t of B cells (pre-B stage) decreased number of circulating B cells and absent or very low levels of all Ig classes
Symptoms Well during the 1st 6-9 months of life because of maternally transmitted IgG antibodies. Chronic or recurrent pyogenic bacterial sinopulmonary or gastrointestinal infections;

B cell Deficiencies
• Common Variable Immunodeficiency– is a disorder that involves the following: (1) low levels
of most or all of the immunoglobulin (Ig) classes, (2) a lack of B lymphocytes or plasma cells that are capable of producing antibodies, and (3) frequent bacterial infections.

B cell Deficiencies
• Common Variable Immunodeficiency– One study showed that, when B lymphocytes were
stimulated with pokeweed mitogen in vitro, plasma cells failed to differentiate, even in the presence of normal T cells. This finding suggests a defect in B-cell expression in surface molecules.

B cell Deficiencies
• Transient hypogammaglobulinemia of infancy– Primarily due to delayed maturation of T cells– As the child ages, the number and condition of T-
helper cells improves and this situation corrects itself. Hypogammaglobulinemia is characterized by low levels of gammaglobulin (antibodies) in the blood.

B cell Deficiencies
• X-linked Hyper-IgM Syndrome• Deficiency of IgG, IgE, IgA but elevated levels of
IgM
• Defect in T cell surface marker CD40L» This is needed for interaction between TH and B cell
for class switching for T-dependent antigens
» T independent antigens???


Molecular Defects In Lymphocyte Activation and Function

Antibody DeficienciesHyper-IgM Syndrome
Age of onset of symptoms
1-2 years of age
Inheritance Genetically heterogenous
Pathogenesis Mutation in the gene for CD154(40L) on T cells, which is the ligand for CD40 on B cells inability to signal B cells to undergo isotype switching B cells produce only IgM.
Clinical Manifestations X-linked Hyper IgM: small tonsils, no palpable lymph nodes; recurrent pyogenic infections

B cell Deficiencies
• Hyper-IgE Syndrome (Job syndrome)• Autosomal dominant
• Skin abscesses, pneumonia, eczema, facial abnormalities
• High # of eosinophils and IgE

B cell Deficiencies
• Hyper-IgE Syndrome (Job syndrome)• Imbalance of TH 1 and TH 2 responses, decreased
production/expression of interferon (IFN)-γ
• Elevated production/expression of interleukin (IL)-4
• Defects in IFN-γ and IL-12 pathways, underexpression of certain chemokines and adhesion molecules
• Reduced expression of transforming growth factor β (TGF-β) and IFN-γ messenger RNA (mRNA) in circulating activated T cells

B cell Deficiencies
• Selective Deficiences of Immunoglobulin Classes
• IgA deficiency is most common– Can be caused by problems in class switching, deletion of
IgA mRNA during processing,
– Recurrent respiratory and urinary tract infections, intestinal problems
– Associated with autoimmune disorders and allergic reaction

B cell Deficiencies
• Selective Deficiences of Immunoglobulin Classes
• IgA deficiency is most common– Associated with one type of transfusion reaction
– Selective IgA deficiency is an inherited disease, resulting from a failure of B-cells to switch from making IgM, the early antibody, to IgA. Although the B-cell numbers are normal, and the B-cells are otherwise normal (they can still make all other classes of antibodies), the amount of IgA produced is limited. This results in more infections of mucosal surfaces, such as the nose, throat, lungs, and intestines.

B cell Deficiencies
• Selective Deficiences of Immunoglobulin Classes
• IgG deficiencies are rare– Selective IgG subclass deficiencies is a group of genetic
diseases in which some of the subclasses of IgG are not made.
– There are four subclasses in the IgG class of antibodies. As the B-cell matures, it can switch from one subclass to another.
– In these diseases there is a defect in the maturation of the B-cells that results in a lack of switching.

Immunoglobulin levelsin adults
• IgA – 80-350 mg/dL
• IgG – 620-1400 mg/dL
• IgM – 45-250 mg/dL
• IgD – O.3-3 mg/dL
• IgE – 0.02 – 0.2 mg/dL

Reference range for serum immunoglobins based on age
AgeAge IgG IgG (mg/dL)(mg/dL) IgA IgA (mg/dL)(mg/dL) IgMIgM (mg/dL)(mg/dL)
0-1 mo0-1 mo 700-1300700-1300 0-110-11 5-305-30
1-4 mo1-4 mo 280-750280-750 6-506-50 15-7015-70
4-7 mo4-7 mo 200-1200200-1200 8-908-90 10-9010-90
7-13 mo7-13 mo 300-1500300-1500 16-10016-100 25-11525-115
13-36 mo13-36 mo 400-1300400-1300 20-23020-230 30-12030-120
3-6 yr3-6 yr 600-1500600-1500 50-15050-150 22-10022-100
6 yr-adult6 yr-adult 639-1344639-1344 70-31270-312 56-35256-352
From the laboratories of Children’s Hospital, Boston, Mass.

T Cell Deficiencies
• “Pure” T Cell Deficiencies:• DiGeorge syndrome
• T cell receptor deficiencies
• Zap 70 deficiency

DiGeorge Syndrome
• Conotruncal cardiac malformation• Hypoparathyroidism• Thymic hypoplasia leading to variable immunodeficiency• The result of common 22q11.2 deletion is a developmental field
defect involving the third and fourth pharyngeal pouches leading to defective migration of the neural crest cells during the fourth week of embryogenesis. Portions of the heart, head and neck, thymus, and parathyroids derive from these pouches.
• Other features:• Characteristic facies• Deletion in 22q11 in > 80%• Affected gene(s) is a transcription factor in the T-box family called Tbx1

Velo-cardio-facial syndrome
• Thymus• DiGeorge Syndrome – decreased or absent thymus
» Results from deletion of region on chromosome 22 in developing embryo, developmental anomaly
» Lowered T cell numbers, results in B cells not producing sufficient Abs

Cardiac defectsAbnormal faciesThymic hypoplasiaCleft palateHypocalcaemia resulting from 22q11 deletions.



Primary Immunodeficiency of B and T cells

Severe Combined Immunodeficiency
• X-linked SCID:
• Swiss-Type SCID
• Bare Lymphocyte syndrome
• Purine nucleoside phosphorylase deficiency
• Omenn syndrome

Severe Combined Immunodeficiency
• Bare Lymphocyte syndrome– Rare recessive genetic condition in which a
group of genes called major histocompatibility complex class II (MHC class II) are not expressed.
– Problems with activators of MHC Class II gene transcription (transcription factor RFX (RFX-B, RFX5, and RFXAP) and the class II transactivator CIITA)



Severe Combined Immunodeficiency
• X-linked SCID:– X-linked recessive trait, stemming from a
mutated (abnormal) version of the IL2-receptor gene located at xq13.1 on the X-chromosome, which is shared between receptors for IL-2, IL-4, and IL-7.
– Body produces very little T cells and NK cells




Severe Combined Immunodeficiency
• Swiss-Type SCID– Adenosine deaminase deficiency– Autosomal recessive– ADA deficiency is due to a lack of the enzyme adenosine
deaminase. This deficiency results in an accumulation of deoxyadenosine

Severe Combined Immunodeficiency
• Swiss-Type SCID– a build up of dATP in all cells, which inhibits ribonucleotide
reductase and prevents DNA synthesis, so cells are unable to divide. Since developing T cells and B cells are some of the most mitotically active cells, they are highly susceptible to this condition.
– an increase in S-adenosylhomocysteine since the enzyme adenosine deaminase is important in the purine salvage pathway; both substances are toxic to immature lymphocytes, which thus fail to mature.


ADA & PNP deficiency
deaminization
inosine↓ ADAdeficiency
deoxyadenosine↑ dAMP↑
dADP↑
dATP↑dATP↑
ribonucleotide reductase↓
DNA synthsize↓blood
urineUric acid ↓
dGTP↑dGTP↑
dGDP↑
dGMP↑ deoxyguanosine ↑ PNP
deficiencyuridine↓
T/B cell mature compromised


Severe Combined Immunodeficiency
• Purine nucleoside phosphorylase deficiency– Autosomal recessive– Impairment of this enzyme causes elevated dGTP levels
resulting in T-cell toxicity and deficiency– In contrast to adenosine deaminase deficiency (another
deficiency of purine metabolism), there is minimal disruption to B cells.

Severe Combined Immunodeficiency
• Omenn syndrome– Autosomal recessive– Associated with mutations in the recombination
activating genes (RAG1 and RAG2), affecting circulating levels of both B-cells and T-cells

Severe Combined Immunodeficiency
• Artermis/DCLRE1C– Protein that in humans is encoded by the DCLRE1C
(DNA cross-link repair 1C) gene– Without the gene, children's bodies are unable to repair
DNA– This gene encodes a nuclear protein that is involved in
V(D)J recombination and DNA repair

Severe Combined Immunodeficiency
• Artermis/DCLRE1C– Protein that in humans is encoded by the DCLRE1C
(DNA cross-link repair 1C) gene– Without the gene, children's bodies are unable to repair
DNA– This gene encodes a nuclear protein that is involved in
V(D)J recombination and DNA repair

Severe Combined Immunodeficiency
• Reticular Dysgenesis– Caused by mutations in the AK2 gene (1p34). The
resulting deficiency in adenylate kinase 2 causes increased apoptosis of myeloid and lymphoid precursors.

Severe Combined Immunodeficiency
• JAK 3 deficiency


Wiskott-Aldrich Syndrome
• X-linked recessive disease characterized by eczema, thrombocytopenia and immune deficiency
• Defect in the WASP gene• WAS gene mutations impair WASP's role in cell signaling
and disrupt the function of the actin cytoskeleton in certain immune cells and blood cells. Immune cells that lack WASP function tend to have trouble responding to factors that trigger cell growth and division (proliferation).


Ataxia-telangiectasia
• Caused by a defect in the ATM gene,which is responsible for managing the cell’s response to multiple forms of stress including double-strand breaks in DNA. (autosomal recessive)
• In simple terms, the protein produced by the ATM gene recognizes that there is a break in DNA, recruits other proteins to fix the break, and stops the cell from making new DNA until the repair is complete.

Ataxia-telangiectasia
• Mutations in the ATM gene reduce or eliminate the function of the ATM protein. Without this protein, cells become unstable and die.
• Cells in the part of the brain involved in coordinating movements (the cerebellum) are particularly affected by loss of the ATM protein.
• The loss of these brain cells causes some of the movement problems characteristic of ataxia-telangiectasia.

Ataxia

Phagocyte Deficiencies
• Chronic Granulomatous Disease– NADPH oxidase defect
• Chediak -Higashi Syndrome– Abnormal lysosome formation
• Leukocyte Adhesion Deficiency– Absence of leukocyte adhesion molecules

Phagocyte Deficiencies
• Chronic Granulomatous Disease– NADPH oxidase defect– An inherited disorder of phagocytic cells,
results from an inability of phagocytes to produce bactericidal superoxide anions (O2-).


Bacteria
phagosome
Bacteria
Phagosome
Neutrophil
NADPH H+NADPH H+
e- +O2
O2-
H+
H2O2
Normsal phagocyte Dysfunction of phagocyte
Chronic granulomatous disease

Nitroblue tetrazolium test
• The panel on the right demonstrates that neutrophils ingest the dye, nitroblue tetrazolium, and in the presence of reactive oxygen species, the yellow colored NBT compound is converted to the purple-blue formazan compound.

Dihydrorhodamine Flow Cytometry based assay
• This test is based on the principle that nonfluorescent DHR (dihydrorhodamine) 123 when phagocytosed by normal activated neutrophils (after stimulation with PMA – phorbol myristate acetate) can be oxidized by hydrogen peroxide, produced during the activated neutrophil respiratory oxidative burst, to rhodamine 123, a green fluorescent compound, which can be detected by flow cytometry.


Phagocyte Deficiencies
• Chediak -Higashi Syndrome– Abnormal lysosome formation
– Autosomal recessive disorder that arises from a microtubule polymerization defect which leads to a decrease in phagocytosis.
– Caused by mutations in the LYST gene which provides instructions for making a protein known as the lysosomal trafficking regulator. Researchers believe that this protein plays a role in the fusion of phagosome and lysosome

Phagocyte Deficiencies
• Chediak -Higashi Syndrome– Also involves problem with skin pigmentation albinism

Phagocyte Deficiencies
• Leukocyte Adhesion Deficiency– Absence of leukocyte adhesion molecules– Results from an impaired step in the
inflammatory process, namely, the migration of leukocytes from the blood vessels to sites of infection, which requires adhesion of leukocytes to the endothelium.

Phagocyte Deficiencies
• Leukocyte Adhesion Deficiency– LAD-I is caused by mutations in the ITGB2
gene (21q22.3), encoding the beta-2-integrin CD18.
– LAD-II results from mutations in the SLC35C1 gene (11p11.2), encoding the guanosine 5'-diphosphate (GDP)-fucose transporter.


Complement Deficiencies
• Single component deficiencies– Example: C3 deficiency
• Hereditary Angioedema– C1 Inhibitor deficiency
• C5,C6,C7,C8, or C9 deficiency– Recurrent bacterial meningitis due defective
membrane attack complex

Causes of Acquired Immunodeficiency
• Cancer (immunoproliferative diseases)
• Cytotoxic drugs or radiation
• Malnutrition
• Splenectomy
• Immunosuppressive therapies
• Stress/emotions
• Aging (thymic atrophy)
• Infection

Immunodeficiency Syndromes

Immunodeficiency Syndromes

Immunodeficiency Syndromes