1.3b Stomach
-
Upload
jennifer-bea-marie-samonte -
Category
Documents
-
view
217 -
download
0
Transcript of 1.3b Stomach
-
8/18/2019 1.3b Stomach
1/7
`
BEI SAMONTE ☺ Page 1 of
1 3B STOMACH
SURG RY
STOMACH
• STORES ingested food
• DIGEST and ABSORB ingested food
• REGULATE appetite
• Has digestive, nutritional, and endocrine functions
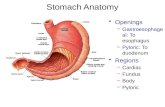
ANATOMY
• The stomach is a dilated part of the alimentary canal between
the esophagus and the small intestine.
• It is a muscular sac.• It occupies the left upper quadrant, epigastric, and umbilical
regions, and much of it lies under cover of the ribs.
• Stomach located at level of T10 and L3 vertebral.
• Position of the stomach varies with body habitués.
The stomach is divided into four regions:
1. The cardia, which surrounds the opening of the esophagus
into the stomach.
2. The fundus of stomach, which is the area above the level of
the cardial orifice.
3. The body of stomach, which is the largest region of the
stomach.
4. The pyloric part, which is divided into the pyloric antrum an
pyloric canal and is the distal end of the stomach.
• Openings:
– Gastroesophageal: To esophagus
– Pyloric: To duodenum
BLOOD SUPPLY
Arterial blood supply:
• 3 Branches
• Left Gastric Artery
- Supplies the cardia of the stomach and distal
esophagus
• Splenic Artery
- Gives rise to 2 branches which help supply the
greater curvature of the stomach
Left Gastroepiploic
Short Gastric Arteries
• Common Hepatic or Proper Hepatic Artery
- 2 major branches
Right Gastric- supplies a portion of the lesser
curvature
Gastroduodenal artery
→ Gives rise to Right Gastroepiploic artery
→ Helps supply greater curvature in
conjunction with Left Gastroepiploic Artery
LYMPHATIC DRAINAGE
-
8/18/2019 1.3b Stomach
2/7
BEI SAMONTE☺ Page 2 of
1 3B STOMACH Surgery
• Lymph from the proximal portion of the stomach drains along
the lesser curvature first drains into superior gastric lymph
nodes surrounding the Left Gastric Artery.
• Distal portion of lesser curvature drains through the
suprapyloric nodes.
• Proximal portion of the greater curvature is supplied by the
lymphatic vessels that traverse the pancreaticosplenic nodes.• Antral portion of the greater curvature drains into the subpyloric
and omental nodal groups.
INNERVATIONS
• The main innervations are Left and Right Vagus Nerves.
• Parasympathetic innervation of Stomach- Vagus Nerve
- 90% of fiber in vagal trunk is afferent (info
transmitting from stomach to CNS)
• Sympathetic innervation of Stomach- Splanchnic Nerve
- Derived from spinal segement T5-T10
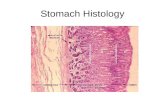
HISTOLOGY
PHYSIOLOGY
• To store food and facilitate digestion by
- Secretory functions
Production of acid, pepsin, intrinsic factor
mucus, and a variety of GI hormones
- Motor functions
Food storage (receptive relaxation and
accomodation), grinding and mixing,
controlled emptying of ingested food, and
periodic interprandial "housekeeping."
IDENTIFYING THE DISEASE
SIGNS AND SYMPTOMS
• Abdominal pain, weight loss, early satiety, anorexia, nausea,
vomiting, bloating, and anemia
• Complete and thorough history and PE
DIAGNOSTIC TESTS
• Esophagogastroduodenoscopy
- 45 years old and above
- Or if with the ff:
Recurrent vomiting
Bleeding
Anemia
Weight loss
Dysphagia
• Radiographic tests - SFA, UGIS with contrast
• CT scan, MRI, arteriography
• Endoscopic ultrasound
• Gastric secretory analysus, H.Pylori Test
• Scintigraphy
• Antroduodenal motility testing and EGG
ENDOSCOPIC ULTRASOUND
1. Superficial mucosa2. Deep mucosa
3. Submucosa
4. Muscularis propria
5. Serosa
PEPTIC ULCER DISEASE
• Focal defects in the gastric or duodenal mucosa that extend
into the submucosa or deeper
• Due to an imbalance between mucosal defenses and
acid/peptic injury
• Caused by:
- Gastrinoma, antral G-cell hyperfunction and/or
hyperplasia, systemic mastocytosis, trauma, burns
and major physiologic stress
- Drugs (all NSAIDS, aspirin, and cocaine), smoking
and psychologic stress
• Helicobacter pylori
• Possess the enzyme urease
Converts urea into ammonia and
bicarbonate
• Ammonia is damaging to the surface epithelial cells
-
8/18/2019 1.3b Stomach
3/7
BEI SAMONTE ☺ Page 3 of
1 3B STOMACH Surgery
Aggression Defense Repair
Acid
Pepsin
NSAIDS
H.Pylori
Bicarbonate
Blood flow
Mucus
Cell junctions
Apical resistance
Restitution
Mucoid cap
Proliferation
Growth factors
SIGNS & SYMPTOMS
• Burning, non radiating epigastric pain
• Duodenal ulcer - after a meal, at night
• Gastric ulcer - occurs with eating
• Nausea, bloating, weight loss, stool positive for occult blood,
and anemia
DIAGNOSTIC TESTS
• EGD with or without biopsy• H.Pylori test
COMPLICATIONS
• Bleeding
• Perforation
• Obstruction
TREATMENT
• Lifestyle modification
• Medical
• Surgical
JOHNSONS CLASSIFICATION
PATIENTS TAKING NSAIDS OR ASPIRIN NEED CONCOMITANT ACI
SUPPRESSING MEDICATION IF ANY OF THE FF RISK FACTORS IS
PRESENT
• Age over 60
• History of acid/ peptic disease
• Concurrent steroid intake
• Concurrent anticoagulant intake
• High-dose NSAID or acetylsalicylic acid
-
8/18/2019 1.3b Stomach
4/7
BEI SAMONTE☺ Page 4 of
1 3B STOMACH Surgery
VAGOTOMY
HSV TV
DRAINAGE
Gastrojejunostomy Pyloroplasty
ZOLLINGER ELLISON SYNDROME
• Uncontrolled secretion of abnormal amounts of gastrin by a
duodenal or pancreatic neuroendocrine tumor (i.e.,
gastrinoma).
• 80% are sporadic (mid life 40-50's)
• 20% are inherited (young 20-30's)
• Associated with multiple endocrine neoplasia type I
(MEN I), which consists of parathyroid, pituitary, and
pancreatic (or duodenal) tumors.
SIGNS & SYMPTOMS
• Epigastric pain, GERD, diarrhea
DIAGNOSTIC TESTS
• EGD - atypical ulcer location (distal duodenum, jejunum, or
multiple ulcers)
• Secretin stimulation test
• BAO testing
• Serum calcium
• Parathyroid hormone levels
• Somatostatin receptor scintigraphy (octreotide scan)
• Endoscopic ultrasound, CT scan or MRI
TREATMENT
• PPIs
• Exploratory laparotomy with curative intent
• Chemotherapy
GASTRITIS AND STRESS ULCER
GASTRITIS
• Gastritis = mucosal inflammation
• H.Pylori - most common cause
• Others: Alcohol, NSAIDS, Crohn's disease, TB, and bile reflux
• Infectious and inflammatory causes result in immune cell
infiltration and cytokine production which damage mucosal
cells
• Chemical agents (alcohol, aspirin, and bile) disrupt the mucos
barrier, allowing mucosal damage by back diffusion of luminalhydrogen ions
• Diagnosis is made clinically and with EGD with biopsy
STRESS GASTRITIS
• Due to inadequate gastric mucosal blood flow during periods o
intense physiologic stress
• Mucosal breakdown occurs
• Seen in ICU patients
• Medical treatment: Acid suppression
• Bleeding: Angiographic embolization or endoscopic hemostat
treatment, surgery
MALIGNANT NEOPLASM - ADENOCARCINOMA
• 95% of gastric malignancies
• Elderly
• Younger patients
- Tend to be diffuse, large, aggressive, poorly
differentiated, sometimes infiltrating the entire
stomach (linitis plastic)
• Higher incidence in groups of lower socioeconomic status
FACTORS INCREASING OR DECREASING THE RISK OF GASTRIC
CANCER
• Increase risk
- Family history
- Diet (high in nitrates, salt, fat)
- Familial polyposis
- Gastric adenomas
- Hereditary nonpolyposis colorectal cancer
- Helicobacter pylori infection
Atrophic gastritis, intestinal metaplasia,
dysplasia
- Previous gastrectomy or gastrojejunostomy (>10y
ago)- Tobacco use
- Menetrier's disease
• Decrease risk
- Aspirin
- Diet (high fresh fruit & vegetable intake)
- Vitamin C
-
8/18/2019 1.3b Stomach
5/7
BEI SAMONTE ☺ Page 5 of
1 3B STOMACH Surgery
SIGNS& SYMPTOMS
• Abdominal pain, weight loss, anorexia, early satiety, nausea,
vomiting, bloating
• Chronic occult bleeding > acute massive bleeding
• Palpation of mass is rare and if present the stage is most likel
advanced
• Virchow's node, Sister Joseph's nodule
• (+) nodules in the rectal shelf - drop metastasis
DIAGNOSTIC EVALUATION
• EGD with biopsy
• Abdominopelvic CT scan with IV and oral contrast, EUS
• PET scanning
• Staging laparoscopy
TREATMENT
• Perioperative chemotherapy and curative gastric resection wit
lymphadenectomy
• Palliative gastrectomy for stage IV
– Endoscopic removal
< 2cm in sixe
Node negative
Confined to the mucosa on EUS
No other gastric lesions
MALIGNANT NEOPLASMS - LYMPHOMA
• 4% of gastric malignancies
• Most are B-cell type, thought to arise in mucosa associated
lymphoid tissue (MALT)
• 50% are high grade, 50% are low grade
• The normal stomach = no lymphoid tissue
• However, chronic gastritis = acquires MALT -> malignant
degeneration
• H.Pylori = culprit
• Low-grade MALT lymphoma can degenerate
• into high-grade lymphoma
• Remarkably, when the H. pylori is eradicated and the gastritis
improves, the low-grade MALT lymphoma often disappears.
Thus, low- grade MALT lymphoma is not a surgical lesion.
SIGNS & SYMPTOMS
• Obstruction, bleeding, fever, weight loss, night sweats,
lymphadenopathy
DIAGNOSTIC TESTS
• EGD with biopsy, CT scan of abdomen, pelvis and chest,
bone marrow biopsy, endoscopic ultrasound
TREATMENT
• H. pylori regimen
• radiotherapy (early stage) or chemotherapy with or without
radiation (advanced)
• Surgery: tube jejunostomy, gastrectomy (definitive, palliative
MALIGNANT NEOPLASMS - GIST
• GIST – gastrointestinal stromal tumor
• Arise from interstitial cells of Cajal (ICC)
-
8/18/2019 1.3b Stomach
6/7
BEI SAMONTE ☺ Page 6 of
1 3B STOMACH Surgery
• Prognosis depends mostly on tumor size and mitotic count
• Metastasis is by the hematogenous route
• Any lesion >1 cm can behave in a malignant fashion and may
recur
• Almost all express c-KIT (CD117) or the related PDGF receptor
A, as well as CD34
• Low grade – 80% survival in 5 years• High grade – 30% survival in 5 years
• Submucosal tumors that are slow growing
SIGNS & SYMPTOMS
• Small lesions: asymptomatic or impressive bleeding
• Larger lesions: weight loss, abdominal pain, fullness, early
satiety, bleeding, palpable abdominal mass
DIAGNOSTIC TESTS
• EGD with biopsy and IHC staining, CT scan (abdomen, chest
and pelvis)
TREATMENT
• Wedge resection with clear margins is adequate surgicaltreatment.
• If there is invasion of adjacent structure, en bloc removal is
done.
• Chemotherapy: Imatinib (gleevec) 400mg once a day for 3
years for high risk of recurrence
MALIGNANT NEOPLASMS - CARCINOID
• Rare
• Arise from gastric enterochromaffin-like (ECL) cells and some
have malignant potential
• 3 types:
– Type I
Most common, 75%
Occur in patients with chronic hypergastrinemia
secondary to pernicious anemia or chronic
atrophic gastritis
More frequent in women
Often multiple and small
Low malignant potential (2 cm)
More commonly in men
Not associated with hypergastrinemia
Most patients have nodal or distant metastases
at the time of diagnosis, and some present with
symptoms of carcinoid syndrome.
30% survival in 5 years
DIAGNOSTIC TESTS
• EGD and biopsy
• If small, EUS and biopsy
• CT scan and octreotide scan for staging
TREATMENT
• If small (type I and II) and
-
8/18/2019 1.3b Stomach
7/7
BEI SAMONTE ☺ Page 7 of
1 3B STOMACH Surgery
MASSIVE UPPER GI BLEEDING
• Acute bleeding proximal to the ligament of Treitz which
requires blood transfusion
• Most common source - stomach and proximal duodenum
• Causes:
• Peptic ulcer, gastritis, Mallory-Weiss tear, and
esophagogastric varices, neoplasm, angiodysplasia,
Dieulafoy’s lesion, portal gastropathy,ie’s disease, and
watermelon stomach, arterioenteric fistula
• IMPORTANT: resuscitation and risk stratification
A. What is the magnitude and acuity of the hemorrhage? Does
the patient have signs and symptoms that suggest that large
blood loss has occurred over a short period of time?
B. Does the patient have significant chronic disease which
compromises physiologic reserve?
C. Is the patient anticoagulated, or immunosuppressed?
D. On endoscopy, is the patient bleeding from varices, or is
there active bleeding, or is there a visible vessel, or is there
a deep ulcer overlying a large vessel? Could the patient be
bleeding from an Arterio enteric fistula?
• NO: low risk
• Most patients will stop bleeding
• supportive treatment
• IV PPI
• Selected patients may be discharged from the emergency
room and managed on an outpatient basis.
UPPER GI BLEEDING
• YES: high risk
• Type and cross-match for blood transfusion
• Admit to ICU
• Consult surgeon and gastroenterologist.
• Resuscitate and correct coagulopathy
• Medical vs. Surgical therapy
DIEULAFOY'S LESION
• Congenital AVM of a submucosal artery
• Usually 6cm from GEJ at lesser curvature
• Middle-aged or elderly men
• More common in patients with liver disease
SIGNS & SYMPTOMS
• Recurrent/intermittent melena, hematemesis, hematochezia
• EGD: Pulsatile bleeding
DIAGNOSTIC TESTS
• Angiography/RBC tagging – if no active bleeding on
TREATMENT
• Endoscopic hemostatic therapy
• Angiographic embolization
• Oversewing/resection
BEZOAR
• Concretions of indigestible matter
– Trichobezoars (hair)
– Phytobezoars (vegetable)
SIGNS & SYMPTOMS
• Obstruction,
• Ulceration, bleeding
DIAGNOSTIC TESTS
• UGIS, EGD, CT scan
TREATMENT
• Enzyme therapy (papain, cellulase, acetylcysteine)
• Endoscopic disruption and removal
• Surgical removal
MALLORY WEISS LESION
• Longitudinal tear in the mucosa of the GE junction
• Caused: forceful vomiting &/or retching
• Commonly seen in alcoholics
• Boehaave’s syndrome (esophageal rupture): vomiting, ches
pain, subcutaneous emphysema
• EGD: confirm diagnosis and
• Control bleeding
• 90% of patients stop bleeding spontaneously
• Other options:
– Balloon tamponade
– Angiographic embolization
– Selective infusion of vasopressin
– Systemic vasopressin, and operation
– Surgery: oversew
_________________________________________________________
END OF TRANX