1.1c Implantation & Placental Development
Click here to load reader
-
Upload
bei-samonte -
Category
Documents
-
view
218 -
download
2
description
Transcript of 1.1c Implantation & Placental Development

`
Page 1 of 5
1.1C IMPLANTATION & PLACENTAL DEVELOPMENT
OBSTETRICS
DECIDUA
Endometrium of PREGNANCY
- Essential for HEMOCHORIAL PLACENTATION
Decidualization - dependent on : Estrogen, progesterone &
other factors secreted by blastocyst
During the course of pregnancy, decidual transformation is
from thick to thin.
DECIDUAL STRUCTURE
3 layers
- Zona Compacta Zona Functionalis
- Zona Spongiosa
- Zona Basalis - Remains after delivery, gives rise to new
endometrium
DECIDUAL BLOOD SUPPLY
As a consequence of implantation, blood supply to the decidua
capsularis is lost as the embryo-fetus grows.
Decidua parietalis - spiral arteries
Decidua basalis & intervillous space - invaded by
cytotrophoblasts
Uteroplacental vessels - not responsive to vasoactive agents
Fetal chorionic vessels - transports blood between the placenta
and the fetus
- Contains smooth muscle; doesn't respond to vasoactive
agents
DECIDUAL REACTION
Completed only by blastocyst implantation
Commences mid-luteal phase
DECIDUAL HISTOLOGY
Zona Spongiosa glands
- Cylindrical -> Cuboidal & flat -> Degenerate & Slough off ->
Disappear
Placental Basal Plate (Decidua Basalis)
1. Spongiosa
- Arteries & dilated veins
- Disappeared glands
2. Cell invasion
- Interstitial trophoblast cells
- Trophoblastic giant cells
Normal Decidual Necrosis: 1st to 2nd trimester
Cell types:
- True decidual cells
- Maternal bone marrow - derived cells
- NK cells
- Trophoblast invasion
- Vasculogenesis
PERIPHERAL NK CELLS DECIDUAL NK CELLS
10% Cytokine secretion
90% Cytolytic
95 % Cytokine secretion
50 % Angiogenic
DECIDUAL PROLACTIN
↑↑ in AMNIOTIC FLUID
Paracrine function between maternal & fetal tissues
Same gene that encodes pituitary PRL
- Alternative Promoter - different regulation
Regulation
- Pituitary regulators do not affect decidual PRL
DECIDUAL PROLACTIN ROLES
Amniotic fluid
- Transmembrane solute & water transport
- Fluid volume maintenance
Regulate immunologic functions in pregnancy
- Stimulate T-cells
Protective function
- Repress expression of detrimental genes to pregnancy
IMPLANTATION & FERTILIZATION
IMPLANTATION
Occurs within 6-7 days post fertilization
Must be on 20-24of the endometrial - ovarian cycle
If it doesn't occur within this period: Failure of implantation
o Placenta Previa or Ectopic pregnancy in the cervical wall
o Apposition is the 1st step of implantation
Progestins
Cyclic AMP
Endothelin 1
IL 1
IL 2
EGF

Page 2 of 5
1.1C IMPLANTATION & PLACENTAL DEVELOPMENT
Obstetrics
FERTILIZATION
With ovulation, the oocyte is engulfed by the fallopian tube
infundibulum. Transport through the tube is by movement of
cilia and tubal peristalsis.
Fertilization, occurs in oviduct in few hours. Spermatozoa must
be present in the tube at the time of oocyte arrival.
Spermatozoa passes between follicular cells; through the zona
pellucida (glycoprotein layer surrounding oocyte Cell
Membrane) and into the oocyte cytoplasm.
Fusion of two nuclei, intermingling of maternal and paternal
chromosomes creates the zygote.
CHORION & DECIDUA DEVELOPMENT
During Early Pregnancy
1. Villi in the entire periphery (chorionic membrane)
2. Blastocysts expand to form DECIDUA (endometrial cavity)
3. Villous trophoblast & anchoring cytotrophoblast, PLACENTA
4. Chorionic villi (Decidua Basalis) form Chorion Frondosum
“Fetal Development of Placenta”
5. Avascular fetal membrane abuts Decidua Parietalis -> Chorion
laeve
End Of 3rd Month
1. Chorion laeve separated from amnion by EXOCOELOMIC
CAVITY
2. Intimate contact to form AVASCULAR AMNIOCHORION
TROPHOBLAST
The peripheral cells of the Blastocyst, which attach the zygote
(fertilized ovum) to the uterine wall and become the placenta
and the membranes that nourish and protect the developing
organism.
FATE OF TROPHOBLAST
During implantation into the uterine wall at 8th day the trophoblast differentiates itself into two layers: o Syncytiotrophoblast (ST)
outer multinucleated syncytium has an amorphous cytoplasm without cell borders has nuclei that are multiple and diverse in size and
shape has a continuous syncytial lining
o Cytotrophoblast (CT)
inner layer of primitive mononuclear cells
germinal cells for the syncytium
has a well-demarcated cell border
has a single nucleus
has the ability to undergo DNA synthesis and mitosis
1 Syncytiotrophoblast (ST)
2 Cytotrophoblast (CT)
3 Epiblast
4 Hypoblast
5 Blastocyst cavity
6 Maternal blood capillary
7 Amniotic cavity
10th day, - the blastocyst becomes
totally encased within the
endometrium
Embryo enlarges - more maternal
decidua basalis is invaded by syncytiotrophoblast
Trophoblastic Lacunae- a system of intercommunicating
channels that permeates syncytiotrophoblast
Lacunae - become filled with maternal blood
FETAL & MATERNAL BLOOD CIRCULATION IN MATURE PLACENTA
MATERNAL CIRCULATION
Physiologic maternal-placental circulation
- Maternal blood thru the basal plate and driven high up to the
chorionic plate
- Blood flows back down as it baths the microvillous surface
- Maternal blood drains back to the venous orifices

Page 3 of 5
1.1C IMPLANTATION & PLACENTAL DEVELOPMENT
Obstetrics
FETAL CIRCULATION
Deoxygenated blood flows through 2 umbilical arteries
Umbilical vessels branch repeatedly beneath the amnion and
diving villi
Blood with a higher 02 content passes thru the umbilical vein
Placental Surface / Chorionic vessels
- Umbilical vessels along the fetal surface of the chorionic plate
- Responsive to vasoactive substances
- Arteries always cross over the veins
Truncal arteries
- Perforating branches of the surface arteries
- Each supply one cotyledon
- Decrease amount of smooth muscle but has increase in
caliber
AMNION
Provides almost all tensile strength of the fetal membranes
Preterm rupture of fetal membrane - major cause of preterm
delivery
5 separate amnion layers:
> Inner surface - bathed by amnionic fluid, uninterrupted single
layer of cuboidal epithelium
> Basement membrane
> Acellular compact layer - composed primarily of interstitial
collagens
> Outer side of the compact layer - row of fibroblast-like
mesenchymal cells
> Outermost amnion layer - acellular zona spongiosa -
contiguous with the second fetal membrane, the chorion laeve.
DEVELOPMENT
Amniogenic cells - precursor of amnionic epithelium
Growth of amnion eventually engulfs the embryo & prolapses
into the cavity
End of the 1st trimester - apposition of the mesoblast of the
chorion and mnion
AMNION EPITHELIAL CELLS
May respond to signals derived from the fetus of the mother
Responsive to various endocrine or paracrine modulators
Metabolically active:
> Inhibits metalloprotinase-1 synthesis
> Produce PGE2 and fetal fibronectin
> Site of prostaglandin production
> Synthesis of vasoactive peptides
AMNION MESENCHYMAL CELLS
Synthesis of interstitial collagens that compose the compact
layer of the amnion.
Synthesize cytokines that include IL-6, IL-8 and monocyte
chemoattractant protein-1.
Greater source of PGE2 compared to epithelial cells
AMNION TENSILE STRENGTH
Resides almost exclusively in the compact layer
Regulated in part by fibrillar collagen interacting with
proteoglycans such as decorin.
Decorin - promotes tissue strength.
Compact layer:
> Cross linked interstitial collagens I and III
> Lesser amounts of collagens V and VI
Collagen I is the major interstitial collagen in tissues
characterized by great tensile strength, such as bone and
tendon.
Collegen III is believed to contribute to tissue integrity and
provides both tissue extensibility and tensile strength.
THE UMBILICAL CORD
DEVELOPMENT
By middle of the 3rd month, the exocoelom (primitive yolk sac)
is obliterated due to expanding amnion
The amnion fuses with the chorion laeve (non-placental part of
the chorion), and covers the bulging placental disc and the
lateral surface of the body stalk.
This covered body stalk becomes the Umbilical Cord or funis
STRUCTURE & FUNCTION
Dull white in color, is a part of the fetal membranes
Extends from the fetal surface of the placenta to the fetal
umbilicus
Contains three vessels within
Two Arteries and One Vein
Flow into the umbilical vein passes two routes through the
ductus venosus into the inferior vena cava as well as hepatic
circulation
The flow then leaves through the two umbilical arteries

Page 4 of 5
1.1C IMPLANTATION & PLACENTAL DEVELOPMENT
Obstetrics
These vessels twist within cord, dextral (Right) or sinistral (left)
> It is theorized that crimping of the cord is prevented by
twisting
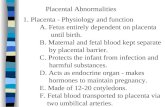
PLACENTAL HORMONES
BIOLOGIC FUNCTIONS OF hCG
Rescue and maintenance of the corpus luteum
Stimulation of fetal testosterone secretion
Stimulation of the maternal thyroid gland
Relaxin secretion of the corpus luteum
Promotion of uterine vascular vasodilation
Myometrial smooth muscle relaxation
Regulation of expansion of uterine natural killer cell numbers
→ Glycoprotein with a biological activity same to LH
→ Produced almost exclusively by the placenta, however low
levels are also synthesized in the kidney
METABOLIC ACTIONS
Promotes maternal lipolysis
Inhibits leptin secretion
Maternal adaptation to fetal energy requirements
Increase maternal beta cell proliferation to augment insulin
secretion (with prolactin)
Angiogenic -> function in fetal vasculature
→ Lactogenic
→ Growth-hormone like
→ Immunochemical
→ Concentrated in the syncitiotrophoblast
→ Detected as early as 2-3 weeks after fertilization
→ Secreted in the maternal circulation
→ And has low concentrations in the urine
→ Similar with hGH
→ There are five genes in the growth hormone–placental lacto-
gen gene cluster that are linked and located on chromosome
17. Two of these—hPL2 and hPL3—encode hPL, and the
amount of mRNA in the term placenta is similar for each.
→ Within 5 to 10 days after conception, hPL is demonstrable in
the placenta and can be detected in maternal serum as early
as 3 weeks. Maternal plasma concentrations are linked to pla-
cental mass, and they rise steadily until 34 to 36 weeks’ gesta-
tion. The hPL production rate near term—approximately 1 g/
day—is by far the greatest of any known hormone in humans.
The half-life of hPL in maternal plasma is between 10 and 30
minutes. In late pregnancy, maternal serum concentrations
reach levels of 5 to 15 μg/mL.
→ hPL concentration is proportional to placental mass, because
the levels of mRNA for hPL is relatively constant throughout the
pregnancy
→ Energy source for maternal metabolism and fetal nutrition
OTHER PLACENTAL HORMONES
Protein/peptide hormones, analogous to hypothalamic or pituitary
hormone, differ in terms of feedback inhibition.
1. Chorionic Adrenocorticotropic Hormone (ACTH):
Product of Pro-opiomenanocortin.
Placental CRH → Chorionic ACTH, important in fetal
lung maturation and parturition timing.
Promotes glucocorticoid production.
2. Growth Hormone Variant (hGH-V)
GH, synthesized in the syncytium by 21- 26 week’s
of gestation but not expressed in Pituitary.
Growth Promoting and antilipogenic function similar
to hGH but has reduced diabetogenic and lactogenic
actions. Mediates Pregnancy Insulin Resistance.
3. Hypothalamic Releasing Hormones
Analogous of Hypothalamic releasing or inhibiting
hormones.
4. GnRH
Found in cytotrophoblast but not in
cyncytiotrophoblast
Regulates trophoblast hCG production.
5. CRH Related Peotides:
CRH, Ucoroctin, Ucoroctin II and III
CRH level surges (upto 100pmol/L) in third trimester.
Increases trophoblast ACTH secretion. In maternal
plasma CRH binds to CRH-binding protein and
remains inactive.
Induces smooth muscle relaxation in vascular and
myometrial tissues and immunosuppression.
Glucocorticoids stimulates CRH production.
6. GHRH (Grhelin)
Regulator of hGH secretion produced by placental
tissue.
Peaks at midpregnancy and plays role in regulating
hGH-V
7. Relaxin:
Similar to Insulin and IGF-, expressed in Corpus
luteum, decidua and placenta.
Act on myometrium with progesterone to promote
relaxation and quiescence of early pregnancy.
Also plays role in postpartum. extracellular
degradation
8. Parathyroid Hormone Related Hormone (PTH-rP)
Regulate transfer of calcium and other solutes and
fetal mineral homeostasis in bone, amnionic fluid and
circulation.
9. Leptin :
Plays role in birthweights, fetal development and
growth, inhbitis apotosis and promotes trophoblast
proliferation.

Page 5 of 5
1.1C IMPLANTATION & PLACENTAL DEVELOPMENT
Obstetrics
10. Neuropeptide Y
Expressed in cytotrophoblast, plays role in CRH
release.
11. Inhibin and Activin.
Inhibin produced by trophoblast inhibit pituitary FSH
release thereby inhibiting ovulation during pregnancy
also regulates placental hCG synthesis via GnRH
Activin is expressed in placenta and amnion.
FETAL ADRENAL GLANDS
• At term, it weigh the same as those of the adult.
• More than 85 percent of the fetal gland is composed of a
unique fetal zone
• Daily steroid production of fetal adrenal glands near term is 100
to 200 mg/day.
• The fetal zone is lost in the first year of life and is not present in
the adult.
• In addition to ACTH, fetal adrenal gland growth is influenced by
factors secreted by the placenta.
FETAL ADRENAL HORMONES
PLACENTAL ESTRIOL
SYNTHESIS
FETAL ADRENAL STEROID
PRECURSOR
• Estradiol- primary placental
estrogen secretory product at
term.
• High levels of fetal hepatic 16-
hydroxylase act on adrenal
derived steroids.
• 16-OHDHEA, were converted
to estriol by placental tissue.
• Most placental estrogens are
released into the maternal
circulation.
• Maternal estriol and estetrol
are produced by fetal steroid
precursors.
• There is a severe deficiency
in the expression of 3HSD in
adrenal fetal zone cells
• But there is a very active
steroid sulfotransferase
activity in the fetal adrenal
glands.
The precursor for fetal
adrenal steroidogenesis is
cholesterol.
Fetal adrenal glands
synthesize cholesterol from
acetate.
Enzymes involved in
cholesterol synthesis are
elevated compared with
adult.
It is still insufficient to
account for the steroids
produced by these glands.
Fetal glands take up
lipoproteins as a source of
cholesterol for
steroidogenesis.
LDL was most effective,
HDL was much less, and
VLDL was devoid of
• The principal secretory
products of the fetal adrenal
glands are pregnenolone
sulfate and DHEA-S.
• Cortisol arises primarily in the
neocortex and transitional
zone of the fetal adrenal
glands
stimulatory activity.
Fetal adrenal glands are
highly dependent on
circulating LDL as a source
of cholesterol for optimum
steroidogenesis
The low level of LDL
cholesterol in fetal plasma
results from the rapid use of
LDL by the fetal adrenal
glands for steroidogenesis