10 Key ASCO 2014 Presentations in Lung Cancer
-
Upload
h-jack-west -
Category
Health & Medicine
-
view
8.960 -
download
2
description
Transcript of 10 Key ASCO 2014 Presentations in Lung Cancer

10 Key ASCO 2014 Presentations in Lung Cancer: NSCLC and SCLC
H. Jack West, MD

• With space to prioritize just 10 key presentations, multiple important trials that have already been reported in press releases as negative were not included.
• Trials that provided longer follow up or convey variations of results already presumed or known were not prioritized.
• Accordingly, even though there will be several immunotherapy trials with several previously identified and some new immune checkpoint inhibitor agents, none really breaks new ground. Immunotherapy hasn’t lost any momentum, but the story is still being written.
Introductory comments on some notable omissions

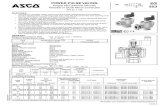
Tarceva (Erlotinib) +/- Avastin (Bevacizumab)In EGFR Mutation-Positive Adv NSCLC
Kato, Abstract #8005 Oral Session, Monday, June 2
154 Japanese EGFR Mutation-Pos Pts,
Advanced NSCLCPreviously Untreated
RAND Tarceva 150 mg by mouth daily
Tarceva 150 mg by mouth daily +Avastin 15 mg/kg IV every 3 weeks
• Key results:– Median PFS* 16.0 mo w/combo vs. 9.7 mo for Tarceva (HR^ = 0.54)– Differences by EGFR mutation subtype
• Exon 19: Median PFS 18.0 vs. 10.3 mo• Exon 21: Median PFS 13.9 vs. 7.1 mo
• Overall Survival not reported, but remarkable improvement in PFS for Tarceva/Avastin in EGFR Mut+ NSCLC, & differences between exon 19 and exon 21 mutations
*Progression-Free Survival ^Hazard Ratio

Combined Analysis of Afatinib vs. Chemoin EGFR Mutation-Positive Adv NSCLC
• Pooled analysis shows significantly longer overall survival benefit with afatinib, 27.3 vs. 24.3 mo (HR = 0.81)
• OS benefit with afatinib is actually seen entirely in exon 19 patients (HR 0.59), while there is actually no benefit (and trend in detrimental direction) in exon 21 patients (HR 1.25)
Yang, Abstract #8004 Metastatic NSCLC Oral Session, Monday, June 2
631 pts w/exon 19 or 21 EGFR mut’n, combined from 2 trials
(LUX-Lung-3, LUX-Lung-6)
RAND
Cisplatin/Pemetrexed (LUX-Lung-3)or
Cisplatin/Gemcitabine (LUX-Lung-6)
Afatinib 40 mg by mouth

AZD9291 for EGFR Mutation-Positive Patients with Acquired Resistance to EGFR TKI Therapy
Janne, Abstract #8009Clinical Science Symposium, Saturday, May 31
199 EGFR Mut’n-Pos Pts, Advanced NSCLC
Prior Progression onEGFR Tyrosine Kinase
Inhibitor (TKI)132 w/centrally confirmed
T790M mutation status
Dose escalation of oral AZD9291 from 20-240 mg/d57 Rx’d with free base formulation up to 900 mg 2x/d
31 Rx’d with HBr formulation to to 1000 mg 2x/d10 transitioned from free base to HBr formulation
• RR 51% among 177 evaluable patients, including brain metastases– responses lasting up to 8 months and ongoing
• RR 64% among T790M+, 23% among T790M-
• Most side effects grade 1: diarrhea, rash, nausea, though 5 cases of interstitial lung disease (ILD) being evaluated

Sequist, Abstract #8010 Clinical Science Symposium, Saturday, May 29
88 EGFR Mut’n Pos Pts, Advanced NSCLC
Prior progression onEGFR TKI
2/3 have T790M mutation
Dose escalation of CO1686 twice daily57 Rx’d with free base formulation up to 900 mg 2x/d
31 Rx’d with HBr formulation to to 1000 mg 2x/d10 transitioned from free base to HBr formulation
CO1686 for EGFR Mutation-Positive Patients with Acquired Resistance to EGFR TKI Therapy
• Optimal dosing selected as 750 mg HBr, which was 3-fold higher exposure to drug than free base formulation
• Leading side effects were nausea, fatigue, and high blood sugar (each in 20-25% of patients)
• Responses seen in T790M+ pts treated w/free base 900 mg 2x/d • Responses being seen w/free base, but most too early

Camidge, Abstract #8001
16 patients w/adv NSCLCenrolled, limited to 13 positive for c-MET amplification by FISH
(1 low; 6 intermed; 6 high)
Crizotinib 250 mg by mouth twice dailyContinue until disease progression or
prohibitive side effects
Metastatic NSCLC Oral Session, Monday, June 2
• XALKORI was originally developed as MET inhibitor but was diverted as “accidental” ALK inhibitor
XALKORI (Crizotinib) for c-MET-PositiveAdvanced NSCLC
• Among 12 patients evaluable for response, 4 responses (33%)– 0 of 1 low, 1 (20%) w/intermediate, 3 (50%) w/high amplification
• Median duration of response 35 weeks (8 months)
• Most common side effects: diarrhea (50%), nausea (31%), vomiting (31%), peripheral edema (25%) visual impairment (25%).

Perol, Abstract #LBA8007Metastatic NSCLC Oral Session, Monday, June 2
~1200 pts with adv NSCLC, Squamous & non-squamous
Prior platinum-doublet chemo
RAND
Taxotere (docetaxel) IV every 3 weeks &Ramucirumab IV every 3 weeks
Taxotere (docetaxel) IV every 3 weeks &Placebo IV every 3 weeks
• Ramucirumab, now marketed as Cyramza for gastric cancer, is an anti-angiogenic monoclonal antibody inhibitor of VEGF-R2 (similar to Avastin)
• Late-breaking abstract, so no details yet provided, but press release in February reports trial is positive for significant progression-free and overall survival benefit
• Positive result of targeted therapy combined with second line chemo; also a rare positive trial for pts. w/squamous NSCLC
Ramucirumab for Second Line Treatment of Advanced NSCLC: The REVEL Trial

SQUIRE Trial: Necitumumab + Cis/Gem Chemo Leads to Survival Benefit in Squamous NSCLC
• Necitumumab is humanized anti-EGFR monoclonal antibody (same mechanism of action as Erbitux (cetuximab))
Thatcher, Abstract #8008Metastatic NSCLC Oral Session, Monday, June 2
1093 pts advanced Squamous NSCLC
Previously untreated
RAND
Cisplatin/Gemcitabine every 3 wks x 6 & Necitumumab d1,8 IV every 3 wks
Cisplatin/Gemcitabine every 3 wks x 6
• Statistically significant (but not necessarily clinically significant) improvement in overall survival, progression-free survival
Necitumumabuntil progression
• Absolute differences: median OS 11.5 vs. 9.9 mo; median OS 5.7 vs. 5.5 months, Response rate 31% vs. 29%

Prophylactic Cranial Irradiation (PCI) for Resected Stage IIIA N2 NSCLC
• Closed early due to slow accrual• Disease-free survival (DFS) significantly favors PCI:– Median DFS 28.5 vs. 21.2 mo (HR 0.67, p = 0.37); – 5 yr DFS 29.8 vs 18.5%
• 5 yr brain relapse rate 13.6 vs. 41.3% (P<0.0001)• Median OS 31.2 vs. 27.4 mo (NS)• PCI Side effects: nausea, headache, fatigue, usually mild• Small numbers, but huge differences
Wang, Abstract #7508Stage I-III NSCLC & SCLC Poster Highlights Session, Sunday, June 1
156 pts w/resected st IIIA N2NSCLC, rec’d post-op chemo
No evidence of disease
RAND Observation
PCI (30 Gy over 10 fractions)

Seto, Abstract #7503Stage I-III NSCLC & SCLC Oral Session, Monday, June 2
Planned enrollment of 330 ptsw/ES-SCLC and any response
to first line chemotherapyStopped early, after 163 pts
After futility analysis
RAND Observation
PCI (25 Gy over 10 fractions)
• PCI led to survival benefit in European trial of patients with ES-SCLC, but no brain imaging done before study entry
• Was benefit actually from treating brain metastases?
• Though PCI significantly reduced risk of brain metastases (58% vs. 32.4% at 12 mo, p < 0.001), it was associated with a 38% decline in survival (median OS 10.1 vs. 15.1 mo) vs. observation
Harmful Effect of Prophylactice Cranial Irradiation (PCI) for Extensive-Stage (ES-)SCLC

“Consolidation” Thoracic Radiation Therapy (TRT) for Residual Chest Disease in ES-SCLC
• All patients also received PCI
Slotman, Abstract #7502
498 pts with ES-SCLCAny response after 4-6
cycles chemo
RAND Observation
Thoracic Radiation Therapy (30 Gy over 10 fractions)
• Significant improvement in prog-free survival (HR 0.73, p = 0.001).
• Overall survival curves overlap for first 9 months, then separate to favor TRT; no difference in 1 yr survival, but 2 year survival diff is 13% vs. 3% (p = 0.004)
• Given results on PCI for ED-SCLC in Japan (Seto abstract), would survival have been better without PCI given to all patients?
Stage I-III NSCLC & SCLC Oral Session, Monday, June 2
88% had residual thoracicdisease

For questions, comments, and further information, check out
CancerGRACE.org