1 Waitlist Management in Nova Scotia: Policy and Practice John T. Blake, Peter VanBerkel, Matthew...
-
Upload
sabina-lewis -
Category
Documents
-
view
214 -
download
1
Transcript of 1 Waitlist Management in Nova Scotia: Policy and Practice John T. Blake, Peter VanBerkel, Matthew...

1
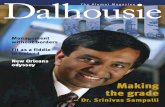
Waitlist Management in Nova Scotia:Policy and Practice
John T. Blake, Peter VanBerkel, Matthew Campbell
Department of Industrial EngineeringDalhousie University
PO Box #1000 Halifax, NS B3J 2X4CANADA

2
Nova ScotiaNova Scotia
• Canada’s 2nd smallest province (55,000 km2)
• About 950,000 people• Principle cities: Halifax
(310k) and Sydney (110k)• Principle industries:
Government services, finance, retail, manufacturing, forestry
• About 5800 km from Wroclaw
• About 60 south of Wroclaw

3
How’s The Weather?
Wroclaw - Winter 2005
www.pbase.com/tygrys50/your_favorite
Halifax - Winter 2005

4
Healthcare in Nova Scotia• 43 hospitals
– 1 adult tertiary (on two sites)– 1 paediatric– 9 regional/mid-size centres
• 2000 physicians– 700 medical residents and
interns– 60% on fee for service
• Budget of $2.6 billion ($Can)
• Provides tertiary services to patients from 3 Atlantic provinces.

5
Problem Statement
• Perception amongst docs & patients that wait times for elective procedures are long.
• There has been a lot of “buzz” around wait times in Canada in general and in Nova Scotia.
• There have been some recent rumblings in the press and policy areas about wait times.
• More recently, there has been a supreme court ruling that may (or may not) change the nature of the CHA.

6
Some Anecdotal Evidenceon Wait Lists
CBC (Online Edition): Jan 23, 2003
www.npdcaucus.ns.ca

7
The Latest Wrinkle…
• Recent supreme court ruling ties wait time to charter freedom
• Appears to allow the introduction of private insurance or services
• Could signal a major shift in Canadian health care
• Most provinces have adopted wait time or access management commissions
Canadian Medical Association June 9/05

8
Finally Some Action?Federal Advisor on Wait Times
• Under a funding “bump” in 2004, the provinces and the feds agreed to some interesting mechanisms to manage waits.
• The central idea is that research is required to understand the root causes of waits and cost-effective methods of resolution
• Areas for review include:1. Development of benchmarks for access, suitable to the Canadian context
2. Develop criteria for appropriateness
3. Identify the nature and causes of wait times, including physical capacity, process flow efficiency, spatial-geography issues, and barriers to care
4. Use operational research (!) to improve productivity and quality
5. Examine the impact of organizational design, policies, and incentives on wait times
6. Look at the impact of the media on the perception of wait times

9
So what do we know about waits?
With rare exceptions, waiting lists in Canada, as in most countries are non-standardized, capriciously organized, poorly monitored, and (according to most informed observers) in grave need of retooling
McDonald, Shortt, Sanmartin, Barer, Lewis and Sheps (1998)
As such, most of those currently in use are at best misleading sources of data on access to care, and at worst instruments of misinformation, propaganda, and general mischief

10
Rationing by Wait List:Are Waits Always Bad?
Positives• Equity: Time is more equally
distributed than cash• Broadly seen as equitable
within a societal context• Discourages consumption
where social costs outweigh social benefits
Negatives• Masks mismatches between
supply and demand• Those who receive may not
be most deserving• Efforts to stratify by need
subject to capriciousness• System can gamed; wealthy
more able to access care or bypass system
Wait times represent a non-price form of rationing healthcare

11
Summary of Canadian Wait List Initiatives
• Medical community views “wait list” initiatives as:1.Registry of patients waiting for surgery2.Prioritization scheme for ranking patients3.Management tool (i.e. data base)
• Since Canada lacks IT infrastructure to collect objective data, self-reported survey data is commonly used
• Most effort (and cash) has been expended on prioritization or triage tools
• The understanding of the need for objective data and an underlying conceptual model for wait times is just developing

12
Registry Methods: BC
0
2
4
6
8
10
12
14
16
Weeks
Dent
Opht
Gyna
Orth Urol
Card
Cance
r
Median Wait Times
0
2,000
4,000
6,000
8,000
10,000
12,000
14,000
16,000
18,000
20,000
Dent
Opht
Gyna
Orth Urol
Card
Cance
r
Patients on List
A 2005 audit found ~8,000 of 68,000 patients either redundant, double counted, dead, or no longer in need of surgery

13
More Policy QuestionsCan We Believe What we See?
• Are wait lists inherently biased?– Physician induced demand: Docs may have an incentive to
over prescribe, particularly if funded on FFS– Backwards bend supply curve: Longer wait lists seen as a
sign of prowess– Your money or your life: Inflating wait lists may be a way to
secure additional funding or hospital resources– Double counting: Patients may be double counted, dead, or
no longer in need of services– Gate keeper: Ultimately physicians, not patients, make
decision about who is/is not on wait list

14
Which Numbers are Correct?
BC Median Wait Time
0
10
20
30
40
50
60
THRTKR
Corne
aO
rthPla
stENT
Card
Catar
act
Vasc
Oph
t
Gyn
aNeu
rG
en Urol
Rad O
nc
We
eks
BC MoH
Fraser Inst

15
• Even if we spend more, there is an inconsistent relationship between spending and performance metrics
• Latent Demand (or “A built bed is a filled bed”): – As we provide more resources, barriers to entry are lowered– Wait time, typically, decreases– This allows the procedure to be more widely prescribed– Thresholds for appropriateness drop– Gradually the system returns to its congested state
• A number of Fraser Institute reports suggest that wait time is not correlated with increased spending– Increased institutional spending actually increased wait– Wait was seen to decrease with increased physician spending
• Similar findings are reported in the UK
The Dilemma: Getting bang for your Buck

16
International Experience: UK
• The UK has perennially had issues with wait time
• Over the past five years, however, wait for elective procedures has dropped
• Reductions appear to be in response to a fiat on maximum waiting times
• There is some indication that long waits have decreased, but average waits are largely unchangedSource: King’s Fund Trust

17
The Operational Research Perspective: This is an easy problem! Isn’t it?!?
• People have been studying line ups for about 100 years.• Much of the original work was done in relation to telephone
switches.• With some assumptions we can fully define the operation of a
queue with three or four pieces of data:
Arrival Rateλ (Customers/Hour)
Server Rateμ (Customers/Hour)
Number of Servers (s)
Queue Size(usually infinite)
Queue Discipline(usually FIFO)

18
Some Basic Results from OR
Queue Length vs Traffic Intensity
0
2
4
6
8
10
12
14
16
18
20
0 0.2 0.4 0.6 0.8 1
Lambda/Mu
Pat
ien
ts
Queue Length vs Number of Servers
0
0.05
0.1
0.15
0.2
0.25
0.3
0 5 10 15 20
Servers
Qu
eu
e L
en
gth
Queue Length vs Traffic Intensity and Service Variance
Sigma = 0.5Sigma = 1
Sigma = 2
0
5
10
1520
25
30
35
40
0.7 0.75 0.8 0.85 0.9 0.95 1
Traffic Intensity
Qu
eu
e L
en
gth
Queue Length vs Traffic Intensity and Queue Discipline
FIFOLIFO
LPT
SPT0
5
10
15
20
25
30
35
0.70 0.75 0.80 0.85 0.90 0.95 1.00
Traffic Intensity
Qu
eu
e L
en
gth

19
The $64k Question:Why Isn’t OR in Greater Use in Healthcare?
• Timing/Project Cycle: – Simulations typically take a long time to build and validate– Issues tend to be “front burner” for institutions
• Cost– Simulation requires specialist knowledge & software
• Data Availability:– It isn’t– IT systems are designed for clinical and administrative
purposes; patient flow hasn’t been a design issue– In the Canadian context, process management is seen as
administrative overhead.

20
Why Ask Us?
• Like most places, Nova Scotia currently lacks complete data to make an accurate determination of wait
• It does have integrated billing and discharge data and is relatively compact
• We’ve been asked to look at efficiency aspects of access
• We do have some experience in orthopaedics
• I’ll talk about some of our work in DI, surgery, and a provincial model
6682
98 0%10%
20%
0
0.2
0.4
0.6
0.8
1
Wait Time (Years)
Beds Increase in OR Time
Ortho Wait Times as a Function of Beds and OR Time
CDHA Ortho (’04)

21
Nova Scotia Access Plan
1. Invest in efficiency improvements first
2. Streamline and simplify the process
• Develop patient centred care• Reduce no-shows
3. Make DHA’s accountable for improving timely access to care
4. Adopt evidence based decision-making
5. Measure clinical and administrative outcomes
6. Manage access to services better• Standard triage tools• Centralized wait lists
7. Communicate access data with the general public
8. Invest in IT strategies9. Increase capacity only
when efficiency gains have been exploited.
10.Develop integrated health human resources plans

22
DI Issues
• Some of our contributions have been logistical in nature– Implemented better data
collection methods
– Adapted QC tools for analysis
• Some of our contributions are in the area of models– DEA analysis of providers
– A general rant on the 3rd available appointment slot(ongoing)
XmR Chart for MRIDHA XX Un-Named Regional Hospital
0
10
20
30
40
50
60
70
Dec-04
Jan-
05
Feb-0
5
Mar
-05
Apr-0
5
May
-05
Jun-
05
Jul-0
5
Aug-0
5
Sep-0
5
Oct-05
Nov-05
Dec-05
Jan-
06
Feb-0
6
Mar
-06
Wai
t
• The province now uses this tool to identify institutions that are out of control
• Results are reported back to managers and institution CEOs
• Implemented quarterly meetings with DI managers to review results

23
Diagnostic Imaging DEA Study
• There are 36 providers in NS – 2 tertiary; 9 regional; 27 rural• We run separate analysis for each band• Potential inputs include
– Budget √– Staff √– Numbers & types of machines
• Potential outputs include– Number and types of tests √– Workload units √
• We produce both efficiency scores & comparator institutions• We think we are the first people to apply DEA across DI
departments within a province• Implementation of the CCRD-I model with constant returns

24
DEA Example: RuralEfficiency
Number Include DMU Name Score Budget Techs Radiography US Workload Units1 1 Hospital 01 0.338 0.22 2.51 0.559 0.000 0.5672 1 Hospital 02 0.816 0.28 3.54 1.527 0.000 1.8573 0 Hospital 03 0.00 0.00 0.000 0.000 0.0004 1 Hospital 04 0.879 0.31 3.31 0.814 1.481 1.4855 1 Hospital 05 0.441 0.17 2.52 0.567 0.000 0.5636 0 Hospital 06 0.00 0.00 0.000 0.000 0.0007 1 Hospital 07 0.414 0.13 1.70 0.403 0.000 0.3988 1 Hospital 08 1.000 0.03 0.16 0.204 0.000 0.2249 1 Hospital 09 1.000 0.43 4.17 1.337 2.550 2.28910 0 Hospital 10 0.00 0.00 0.000 0.000 0.00011 1 Hospital 11 0.749 0.08 0.63 0.463 0.000 0.48112 0 Hospital 12 0.00 0.00 0.000 0.000 0.00013 1 Hospital 13 0.796 0.10 1.19 0.277 0.000 0.66114 1 Hospital 14 0.564 0.15 2.25 0.617 0.000 0.68615 0 Hospital 15 0.00 0.00 0.000 0.000 0.00016 1 Hospital 16 0.365 0.11 1.41 0.290 0.000 0.26117 1 Hospital 17 0.195 0.05 0.74 0.074 0.000 0.06918 0 Hospital 18 0.00 0.00 0.000 0.000 0.00019 1 Hospital 19 0.146 0.07 0.95 0.077 0.000 0.07620 1 Hospital 20 0.204 0.08 1.19 0.016 0.000 0.14121 0 Hospital 21 0.00 0.00 0.000 0.000 0.00022 1 Hospital 22 0.138 0.06 0.86 0.057 0.000 0.05423 1 Hospital 23 0.274 0.28 2.17 0.568 0.000 0.60524 1 Hospital 24 0.524 0.08 0.92 0.264 0.000 0.35225 0 Hospital 25 0.00 0.00 0.000 0.000 0.00026 1 Hospital 26 0.758 0.44 4.10 1.042 2.000 1.77127 1 Hospital 27 0.388 0.12 1.20 0.340 0.000 0.39328 1 Hospital 28 0.541 0.11 1.23 0.443 0.000 0.46729 1 Hospital 29 0.570 1.27 9.85 5.017 0.000 5.97930 0 Hospital 30 0.00 0.00 0.000 0.000 0.00031 1 Hospital 31 0.373 0.17 0.39 0.440 0.000 0.51532 1 Hospital 32 0.557 0.72 6.77 2.354 0.000 3.29533 1 Hospital 33 0.391 0.07 0.75 0.219 0.000 0.19834 0 Hospital 34 0.00 0.00 0.000 0.000 0.00035 1 Hospital 35 0.478 0.13 0.52 0.461 0.000 0.43636 0 Hospital 36 0.00 0.00 0.000 0.000 0.000
1 1 1 1 1Total Efficient DMUs 2
Data Inputs Outputs
Include Element?
Units and institutions coded

25
DEA Results
• Tertiary – not enough sites for meaningful analysis• Regional – Identified a single institution as benchmark• Rural – A bit more difficult
– We did identify two institutions in one DHA, managed by the same team that shows up as efficient on most subsets of inputs and outputs
• Implementation– Oddly, DI managers are a bit reluctant to talk efficiency – especially
in front of the province– Would really just like more money (If I’m efficient does that mean I
won’t get a new MRI machine?)– However, we are in the process of cleaning up data issues and
establishing a benchmark procedure

26
Surgical Issues
• Our contributions are largely in the area of models– Evaluation of guaranteed
waits for surgery to meet federal benchmarks
– An analysis of general surgery at the QEII (the largest hospital in the province)
– The development of a general acute care model for all hospitals in the province
DHA 4 Dispose LTC DHA 4
DHA 4
DHA 4
RegionalColchester
DHA 4
MemorialLillian Fraser
DHA 4
B ayview Memorial
InptsDispose DHA 4
0
0 . 0 6 0 . 00. 0
1. 0
0
0
0 . 0 6 0 . 00. 0
1. 0
0
0 . 0 6 0 . 00. 0
1. 0
0
0 . 0 6 0 . 00. 0
1. 0
0

27
Guaranteed Waits
• A number of ideas have been floated to deal with the impact of the supreme court ruling on waits.
• One of the more popular idea is the “guaranteed wait”• Patients would be separated into three broad bands.• After a fixed amount of time patients would be
“upgraded” into the next higher band• Some plans call for an automatic jump to the top band
• Is this likely to be an effective policy?

28
Guaranteed WaitsAvg Lost Utility (r = 0.3)
0
20
40
60
80
100
120
0.7 0.75 0.8 0.85 0.9 0.95
Rho
QA
LD
With Guarantee
Without
Simple M/M/s model with an assumed exponential decay for utility
We conclude that guaranteed waits may result in greater lost utility – should address capacity issues up front.
Guaranteed waits are particularly dangerous if ρ > 1

29
General Surgery Wait Time
• A discrete event simulation model using
– Modular design elements– Self building concepts– Excel interface to model
elements
• Data elements derived from three local sources
– Subject to a substantial level of cleaning and organizing
• Validated against a two year data sample for:
– Occupancy rate– Expected wait time– Patient LOS
Expected Wait Time for Elective Surgery
0
20
40
60
80
100
120
140
160
Date
Wai
t (da
ys)
Known Wait Time Modeled Wait TimeLinear (Modeled Wait Time)

30
General Surgery: Bottleneck Analysis
Less 15%
Current
Plus 15%
(Current) 4
145
50210
215
220
225
230
235
240
Thruput (pnts/month)
OR Time
VG Beds
Through Put (Pnts/Month)
• Two-way design to look at factors limiting patient flow
• Analysis shows that beds, rather than OR time is the limiting factor
• However, system is sensitive to reductions in OR time
• Analysis showed a number of process issues – turn around being the most obvious

31
Provincial Flow Model: ObjectivesConventional wisdom claims that the ED is backed up because inpatient beds are used by people who should be in nursing homes.
There has been a renewed call in the province for greater LTC beds
We have been asked to determine best bang for buck in terms of resources. Should we invest in:
1. Long term care beds
2. Acute care beds
3. Emergency services
4. All three
And if so, in what proportion?
Is a system wide fix required, or do local conditions dictate local approaches

32
Project Methodology
• We are developing a simulation model of the entire province
– This is probably unique in Canada• The model will runs on a DAD
abstract for 2004/05• We have detailed models of acute
care, with simple extensions for LTC and (eventually) ED
• A phased approach to model building, testing, and development will be necessary
• We have developed a Phase 1 model (right) and are now working on extensions.
• The model is based on ARENA templates to reduce coding and repetition
DHA 4 Dispose LTC DHA 4
DHA 4
DHA 4
RegionalColchester
DHA 4
MemorialLillian Fraser
DHA 4
B ayview Memorial
InptsDispose DHA 4
0
0 . 0 6 0 . 00. 0
1 . 0
0
0
0 . 0 6 0 . 00. 0
1. 0
0
0 . 0 6 0 . 00. 0
1. 0
0
0 . 0 6 0 . 00. 0
1. 0
0

33
Provincial Model: Data Items
• Of the 98,000 discharges only 2253 had any ALC days
• ~88,800 ALC days in the province out of 820,000 inpatient days
• ~138,000 days consumed by patients who ultimately end up with an ALC day
Patient Volume
0
5000
10000
15000
20000
25000
30000
Qu
e
e
n
El
i
z
a
b
e
t
h
II
He
al
t
h
Sc
i
e
n
c
e
Ce
n
tr
e
IW
K
H
ea
l
t
h
C
e
n
t
re
Ca
p
e
Br
e
t
o
n
He
a
l
t
hC
ar
e
C
o
m
pl
e
x
Va
l
l
ey
Re
g
i
o
n
a
l
H
os
pi
t
a
l
Ab
e
r
de
e
n
Ho
s
p
i
t
a
l
Co
l
c
he
s
t
e
r
R
e
gi
o
na
l
Ho
s
p
i
t
a
l
Da
r
t
mo
u
t
h
Ge
n
e
r
a
lH
os
p
i
t
al
Ya
r
m
ou
t
h
Re
g
i
o
n
a
lH
os
p
i
ta
l
.
St
Ma
r
t
h
a
'
s
R
e
g
io
n
a
l
Ho
sp
i
t
a
l
So
u
t
hS
ho
r
e
Re
g
i
o
n
a
l
Cu
m
b
er
l
a
n
d
Re
g
i
o
na
lH
e
a
lt
h
Ca
r
e
Ce
n
tr
e
In
v
e
rn
e
s
s
Co
n
s
o
l
i
d
a
t
ed
Ho
s
p
i
ta
l
So
l
d
ie
r
s
'
M
e
m
or
i
a
l
Ho
sp
it
a
l
Ha
n
t
s
Co
m
m
u
n
i
t
y
H
os
pi
t
a
l
Qu
e
e
ns
Ge
n
e
r
a
l
H
o
s
p
it
a
l
No
v
a
Sc
o
t
i
a
H
o
s
p
i
ta
l
Ro
s
e
wa
y
Ho
s
p
i
t
a
l
Vi
c
t
or
i
a
Co
u
n
t
y
M
em
or
i
a
l
H
o
s
pi
t
a
l
Li
l
l
ia
n
Fr
a
s
e
r
M
e
mo
ri
a
l
H
o
s
pi
t
a
l
Di
g
b
y
Ge
n
e
r
a
l
Ho
s
pi
ta
l
Fi
s
h
er
m
e
n
M
e
m
o
r
i
al
An
n
a
po
l
i
s
Co
m
m
u
n
it
yH
e
a
lt
h
Ce
n
t
r
e
Bu
c
h
an
a
n
Me
m
o
r
i
a
l
Ho
s
p
i
t
a
l
-
St
r
a
it
Ri
c
h
m
o
n
d
Ho
sp
i
t
a
l
Sa
c
r
ed
H
e
a
r
t
H
o
s
p
it
a
l
Ea
s
t
er
n
Sh
o
re
M
e
m
or
ia
l
H
o
sp
i
t
a
l
Gu
y
s
bo
r
o
u
g
h
Me
m
o
ri
al
Ho
s
p
i
t
al
No
r
t
h
Cu
m
b
e
r
l
a
n
d
Me
mo
r
i
a
l
H
o
sp
i
t
a
l
Tw
i
n
Oa
ks
M
e
m
o
ri
a
l
Ho
s
pi
ta
l
Mu
s
q
u
o
d
ob
o
i
t
Va
l
le
y
Me
m
o
r
i
a
l
Ho
s
p
i
t
a
l
.
St
Ma
r
y
'
s
M
e
m
o
r
i
al
Ho
s
p
i
t
a
l
Ea
s
t
er
n
Me
m
o
r
i
a
l
Ho
sp
i
t
a
l
Ba
y
v
ie
w
Me
m
o
r
i
a
l
He
al
t
h
C
e
n
t
re
So
u
t
hC
u
m
b
e
r
l
an
d
Co
m
m
un
it
y
Ca
r
e
C
e
n
tr
e
Pat
ien
ts
All Patients
ALC Patients
Institution names obscured

34
Is ALC the Only Factor?
0
5000
10000
15000
20000
25000
30000
35000
40000
SC
HIZ
OP
HR
EN
IA A
ND
OT
HE
R P
SY
CH
OT
IC
OT
HE
R F
AC
TO
RS
CA
US
ING
HE
AR
T F
AIL
UR
E
SP
EC
IFIC
CE
RE
BR
OV
AS
CU
LAR
ES
OP
HA
GIT
IS,
GA
ST
RO
EN
TE
RIT
IS
SIM
PLE
PN
EU
MO
NIA
AN
D P
LEU
RIS
Y
CH
RO
NIC
BR
ON
CH
ITIS
OT
HE
R S
PE
CIF
IED
AF
TE
RC
AR
E
MA
JOR
INT
ES
TIN
AL
AN
D R
EC
TA
L
DE
PR
ES
SIV
E M
OO
DD
ISO
RD
ER
S W
ITH
OU
T
CH
RO
NIC
OB
ST
RU
CT
IVE
DE
ME
NT
IA W
ITH
OR
WIT
HO
UT
DE
LIR
IUM
NE
ON
AT
ES
WE
IGH
T >
2500
GM
(N
OR
MA
L
GA
ST
RO
ST
OM
Y A
ND
CO
LOS
TO
MY
OT
HE
R A
DM
ISS
ION
SW
ITH
SU
RG
ER
Y
VA
GIN
AL
DE
LIV
ER
Y
DE
ME
NT
IA W
ITH
OR
WIT
HO
UT
DE
LIR
IUM
RE
SP
IRA
TO
RY
NE
OP
LAS
MS
AM
I WIT
HO
UT
CA
RD
IAC
CA
TH
To
tal D
ay
s Conservable
ALC
Expected LOS
This chart suggest that while ALC bed days are an issue, so too are “conservable” days

35
Nevertheless LTC Admissions are tight
LTC Transfers per Day
0.0000
0.2000
0.4000
0.6000
0.8000
1.0000
1.2000
DHA1
DHA2
DHA3
DHA4
DHA5
DHA6
DHA7
DHA8
DHA9
Pts
/Day Community
Hospital
Overall, only 3 patients per day can be transferred from Acute Care to LTC in NS

36
Some Interesting Notes • This is, to the best of my knowledge, the only system wide in existence in Canada or anywhere.• We are modelling at a high level, but the framework is very flexible and easily extended• The model should be seen as an evolutionary entity – we are starting simple and building up
confidence and capability in the model and its results

37
Phase 1: Model
• A single bed complement for each acute care facility
• A single patient type with a common LOS distribution
• All ALC patients transfer to LTC facilities
• Assume a single LTC facility for each DHA
• LTC facilities take admissions from community and acute care institutions
• All model widgets are “self-contained” instances of a generalized process
DHA 1 DHA 2
DHA 3 DHA 4
1Dis pos e LTC DHA
2Dis pos e LTC DHA
3Dis pos e LTC DHA
4Dis pos e LTC DHA
DHA 1
D H A 1
M em or ialFisher m ans
I np t sDis pos e DHA 1
D H A 1
Q ueens G ener al
D H A 1
RegionalSout h Shor e
D H A 2
Digby G ener alI np t s
Dis pos e DHA 2
D H A 2
Ros eway Hospit al
D H A 2
RegionalYar m out h
DHA 2
D H A 3
Cent r eCom m unit y Healt h
Annapolis
D H A 3
Soldier s M em or ial
D H A 3
Valley Regional
I np t sDis pos e DHA 3
DHA 3 DHA 4
D H A 4
RegionalColc hes t er
D H A 4
M em or ialLillian Fr aser
D H A 4
Bay v iew M em or ial
I np t sDis pos e DHA 4
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0 0
0 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0 0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0
0 . 0 6 0 . 0
0 . 0
1 . 0
0

38
Phase 1: ValidationHow do we test the model is working?
300250200150100500
Median
Mean
86420
Anderson-Darling Normality Test
Variance 420.114Skewness 5.5617Kurtosis 43.4584N 4187
Minimum 0.000
A-Squared
1st Quartile 0.097Median 0.9823rd Quartile 5.814Maximum 322.244
95% Confidence Interval for Mean
7.230
822.52
8.472
95% Confidence Interval for Median
0.848 1.086
95% Confidence Interval for StDev
20.067 20.945
P-Value < 0.005
Mean 7.851StDev 20.497
95% Confidence I ntervals
Summary for QEII LOS
• We test the averages for:- Arrival rates
- Inpatient length of stay
- Transfers to LTC
using standard statistical tests (t-test) and compare model results against samples from DAD
• We also test variance (σ2) using standard statistical techniques (χ2
test)
• We have no problem in reproducing admission numbers and appropriate lengths of stay.

39
Now for the bad news…
• Having completed a 1st model, we know our admissions are correct
• We know that the LOS is correct• However, our bed utilization
numbers are too low– In almost all instances, our
model does not show a bottleneck
• Reasons could include– Home care excluded– OR time excluded– Inadequate patient
categorization– Fluctuations in bed availability
over the year– Transfers between institutions
0
0.2
0.4
0.6
0.8
1
1.2
AB DA DDDDDDDDDDDDD D ABAAAAAAAAAAAAA ADDDDDDDDDDDDD D D AD BI D BBBBBBBBBBBBB B BD L BB A
AD
BBBBBBBBBBBBBB BD
BD

40
Patient disposition is also an issue
0
20000
40000
60000
80000
100000
120000
Nursinghome
Home care Acute Ambulatory Rehab Emerg Forensics Out of NS Out Pt Chronic Unknow n Daysurgery
Patient Days by Transfer
ALC
Conservable
PLEX
• Interestingly, 26% of ALC bed days are consumed by patients who ultimately go home.

41
Issue: Appropriate Patient Types
MED_SURG
TOTA
L_STA
Y
unknownsurgicalpregnancyneonatemental hmedical
35
30
25
20
15
10
5
0
Interval Plot of TOTAL_STAY vs MED_SURG95% CI for the Mean
• There are statistically significant differences between med/surg and all other admission types
• Mental health, in particular, has a very long LOS
• We’ve decided to eliminate neonates – triggered by maternal admissions

42
Issue: Admit Category(All significant except Mental Health)
ADMIT_CAT
TOTA
L_STA
Y
UL
13
12
11
10
9
8
7
6
5
4
95% CI for the MeanInterval Plot of TOTAL_STAY vs ADMIT_CAT (Surgical)
ADMIT_CAT
TOTA
L_STA
Y
UL
5.5
5.0
4.5
4.0
3.5
3.0
95% CI for the MeanInterval Plot of TOTAL_STAY vs ADMIT_CAT (Pregnancy)
ADMIT_CAT
TOTA
L_STA
Y
UL
50
40
30
20
10
95% CI for the MeanInterval Plot of TOTAL_STAY vs ADMIT_CAT (Mental Health)
ADMIT_CAT
TOTA
L_STA
Y
USNL
10.0
7.5
5.0
2.5
0.0
-2.5
-5.0
95% CI for the MeanInterval Plot of TOTAL_STAY vs ADMIT_CAT (Medical)

43
Issue: Transfers
G
H
B
C
D
E
F
Other
RehabNursingHome
Out ofProvince
Homecare
A

44
Phase II
• Home Care– We have added extensions to simulate
home care– We are collecting and validating capacity
and length of stay data
• Acute Care– We are implementing the model on a DHA
by DHA basis• This allows us to vet assumptions and
include local conditions
– We have added capacity for different patient types and admission categories
– We are now working to establish appropriate bed numbers and include surgical process capacity over time
• Long Term Care– One of our more difficult jobs at present is
validating LOS assumptions

45
Future Plans
• Validate acute care modules• Expand model to include ED• Expand to model specific services (i.e. Ortho)• Include a specific widget to represent OR
time and master surgical schedule• “Package” simulation widgets• Develop a platform for local use of simulation
models• Target date: January 2007