1 Splenic marginal zone lymphoma BLOOD 1 APRIL 2003 VOLUME 101, NUMBER 7.
-
Upload
ashlee-wilkinson -
Category
Documents
-
view
214 -
download
0
Transcript of 1 Splenic marginal zone lymphoma BLOOD 1 APRIL 2003 VOLUME 101, NUMBER 7.

1
Splenic marginal zone lymphoma
BLOOD 1 APRIL 2003 VOLUME 101, NUMBER 7

2
Clinical features(1)Incidence
The real incidence of SMZL has never been exactly calculated, even if it has been estimated as less than 1% of non-Hodgkin lymphoma (NHL).
SMZL constitutes 8% to 14% of lymphoma in surgically removed spleens involved by lymphoproliferative disorders.
Median age of patients is 68 years (range, 22-79 years)
Male-to-female ratio 1:1.8.

3
Clinical features(2)Clinical presentation
Almost all patients present moderate-to-massive splenomegaly that can cause discomfort in the left hypochondrium.
Hepatomegaly can be sometimes observed, Lymphadenopathy is extremely rare. B symptoms such as fever and night sweats
are rare.

4
Clinical features(3)laboratory findings
Nonspecific symptoms relating to moderate anemia are reported in up to 64% of cases.
Thrombocytopenia is sometimes seen, but it is severe only in 15% of cases.
Mild neutropenia is commonly observed, but only 5% of patients present neutropenia below 1×109/L.

5
Clinical features(4)laboratory findings
Absolute lymphocytosis is reported in 75% of patients.
Lymphocytosis can ensue in the course of the disease after diagnosis.
A frequent rise in lymphocyte count is observed after splenectomy.

6
Clinical features(5)laboratory findings
The presence of a small M band, IgM or IgG, usually less than 30 g/L, can be documented in up to 50% of patients.
Alterations in levels of serum albumin, lactic dehydrogenase (LDH), and 2-microglobulin may be seen in variable percentages.
Occasionally diagnosis can be made on splenectomy specimens for traumatic or spontaneous rupture.

7
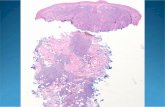
Pathologic features(1)
Spleen
The spleen is enlarged, weighing from 270 to 5500 g with a median of 1750 g.
The cut surface generally shows multiple, small-to-moderate gray-tan nodules throughout the parenchyma

8
Pathologic features(2)
the splenic architecture can be retained in initial phases. Hyperplastic white pulp shows expansion of marginal zones with frequent merging and coalescence.
In advanced phases,no residual follicular structures can be identified.
Involvement of splenic sinuses is typical.

9
Pathologic features(3)
Bone marrow Bone marrow is invariably involved. Different types of infiltration have been
described, namely, intrasinusoidal, interstitial, nodular, and even paratrabecular.
Different patterns of infiltration could be an expression of different phases of the disease.

10
Pathologic features(4)
Peripheral blood In obvious peripheral blood involvement,
numerous mature B lymphocytes with pale cytoplasm, irregular cytoplasmic borders, and villous projections can easily be recognized
Larger cells with prominent nucleoli can be seen in the aggressive variant.

11
Pathologic features(5)
lymph node Involvement of hilar splenic lymph nodes is
commonly observed in SMZL. Peripheral lymph nodes can be involved as
well, but to a lesser extent.

12
Pathologic features(6)
Liver The liver is involved in almost 90% of cases
prevalently showing nodular infiltration of portal tracts.
Lobular invasion is reported to a lesser extent. Liver biopsies show an invariable sinusoidal
infiltration together with lymphoid nodules in portal tracts.

13
Pathologic features(7)
Other organsRarely(6.6%) are nonhematolymphoid organs massively involved, at least at presentation.Cutaneous involvement showing dermal tumoral infiltration located around cutaneous appendages and blood vessels with some degree of epidermotropism.

14
Pathologic features(8)
Pleura localization is seen in 5% of cases in a large series.
Sporadic soft-tissue involvement ,such as thoracic 、 perirenal area.
Meningeal involvement has also been reported and can induce altered mental status and seizures.

15
ImmunophenotypePositivity
CD20, CD45RA, CD45RB, CD79a, PAX5/BSAP, IgM, and bcl-2Negativity
CD43, CD23, CD10, bcl6,cyclin D1T-cell antigens are always negative.
the absence of telomerase activity

16
Cytogenetics and molecular biology(1)
Few genetic alterations have been reported in association with SMZL.
t(6;14)
t(9;14)(p13;q32) translocation was reported in cases of SMZLs.
Rearrangement of bcl-6 was identified in some marginal zone lymphomas.

17
Cytogenetics and molecular biology(2)
7q Alterations of chromosome 7q, mainly allelic loss,
are frequently observed in splenic lymphoma. With subsequent dysregulation of cyclin-
dependent kinase 6 (CDK6) gene, possibly playing a role in the pathogenesis of SMZL and SLVLs.
7q deletion may play an alternative role in the inactivation of p53 pathway for tumor progression.

18
Cytogenetics and molecular biology(3)
Translocations t(2;8)(p12;q24) and t(14;18)(q32;q21) were reported in a case of an aggressive variant of SMZL.Complex chromosome defects including 6q, 11q, 12, and 17p were usually associated with switching into high-grade histologymainly involving 7q and 17p, were associated with shorter survival.

19
Differential diagnosis(1)Hairy cell leukemiaBone marrow: “dry taps” . patchy infiltration with progressive replacement of normal hematopoietic series and low cellular density.Neoplastic infiltration is characteristically intermingled with extravasated red cells. Spleen: white pulp is atrophied.tartrate-resistant acid phosphatase(TRAP)CD25 and CD103Ultrastructural analysis : ribosomelamella complex.

20
Differential diagnosis(2)B-CLL
Morphology: small mature lymphoid cells, with high nuclear-to-cytoplasm ratio, scant cytoplasm, and round nuclei with highly condensed chromatin and inconspicuous nucleolus.
Admixed with prolymphocytes and paraimmunoblasts, characterized by larger size and prominent nucleoli.
Bone marrow : the pattern of infiltration never intrasinusoidal.
a lower expression of CD20 and positivity for CD23.

21
Differential diagnosis(3)Mantle cell lymphoma
high frequency of peripheral lymphadenopathy.
Neoplastic cells are small to medium sized with irregular nuclei, morphologically resembling centrocytes/cleaved follicular center cells, but with less irregular nuclear contours.
The bone marrow infiltration has never been intrasinusoidal.
characteristically CD5, CD43, and cyclin D1.

22
Prognostic Factors(1)
SMZL is universally considered a low-grade lymphoma with an indolent clinical course.The 5-year overall survival rate ranges from 65% to 78%. Even in the absence of treatment or complete response, the time to progression exceeds 5 years.

23
Prognostic Factors(2)
4 factors associated with poorer survival. Failure to obtain complete remission involvement of nonhematopoietic sites at
diagnosis high performance status scores p53 expression

24
Prognostic Factors(3)
Thieblemont etal presence of M component elevated 2-microglobulin level Leukocyte count more than 20 ×109 /L, and
lymphocytes more than 9 ×109 /L.

25
Prognostic Factors(4)
Blastic transformation occurred in 13% of cases. Response to treatment and survival after
transformation are poor. patients who died from lymphoma had a
median survival time of less than 2 years.

26
Treatment (1)
No treatment---- “wait and see” policy. Patients with favorable prognostic factors. Patients with mild lymphocytosis and no
cytopenia In untreated patients the 5-year overall
survival rate is 88%.

27
Treatment (2)
Splenic irradiation Even low-dose radiotherapy (4 Gy) may be
effective, producing a dramatic reduction in circulating villous lymphocytes, regression of splenomegaly, and improvement of cytopenias.
SLVL when splenectomy is contraindicated and/or when pancytopenia is present and likely to give rise to excessive toxicity when chemotherapy is administered.

28
Treatment (3)
Chemotherapy first-line treatment in patients with more
advanced disease. There is no univocal convergence when and
how to use chemotherapy.

29
Treatment (3)
The role of alkylating agents is marginal. In cases of disease progression, especially after splenectomy, may achieve good response, but seldom complete remission.
Mean duration of response in patients treated with
alkylating agents alone or in combination with other drugs is 6 months, whereas the 5-year overall survival rate is 64%.

30
Treatment (3)
Purine analogues,such as 2-deoxycoformycin is more promising, but only tested in relatively few patients.
Good responses with 2- chlorodeoxyadenosine have been also reported, whereas in other cases only partial responses with high frequency of relapses were obtained.
Some complete remissions have been achieved with fludarabine as first- or second-line therapy.

31
Treatment (4)
Splenectomy
A huge symptomatic splenomegaly or a severe cytopenia or both are the main indications.

32
Treatment (4)
Advantage Long and sustained improvement of cytopenia Relief of abdominal discomfort
Disadvantage cannot reduce extrasplenic lymphomatous infiltrations. changes in bone marrow infiltration, probably through
the lack of microenvironmental homing factors on circulating B cells.

33
Treatment (5)
Other modalities Single-agent rituximab are under investigation. Interferon-alfa ribavirin