1 ACLS Pharmacology. 2 Objectives To review and obtain a better understanding of medications used in...
-
Upload
brittney-holmes -
Category
Documents
-
view
215 -
download
1
Transcript of 1 ACLS Pharmacology. 2 Objectives To review and obtain a better understanding of medications used in...

1
ACLS Pharmacology

2
Objectives
To review and obtain a better understanding of medications used in ACLS– Indications & Actions (When & Why?)– Dosing (How?)– Contraindications & Precautions (Watch
Out!)

3

4
Drug Classifications
Class I: Recommendations– Excellent evidence provides support– Proven in both efficacy and safety
Class II: Recommendations– Level I studies are absent, inconsistent or lack
power– Available evidence is positive but may lack efficacy– No evidence of harm

5
Drug Classifications
Class IIa Vs IIb– Class IIa recommendations have
Higher level of available evidenceBetter critical assessmentsMore consistency in results
– Both are optional and acceptable,– IIa recommendations are probably useful– IIb recommendations are possibly helpful
Less compelling evidence for efficacy

6
Drug Classifications
Class III: Not recommended– Not acceptable or useful and may be
harmful– Evidence is absent or unsatisfactory, or
based on poor studies Indeterminate
– Continuing area of research; no recommendation until further data is available

7
Oxygen
Indications (When & Why?)– Any suspected cardiopulmonary emergency– Saturate hemoglobin with oxygen– Reduce anxiety & further damage – Note: Pulse oximetry should be monitored
Universal Algorithm

8
Oxygen
Dosing (How?)
Device Flow Rate Oxygen %Nasal Prongs 1 to 6 lpm 24 to 44%
Venturi Mask 4 to 8 lpm 24 to 40%
Partial Rebreather Mask
6 to 10 lpm 35 to 60%
Bag Mask 15 lpm up to 100%
Universal Algorithm

9
Oxygen
Precautions (Watch Out!)– Pulse oximetry inaccurate in:
Low cardiac output VasoconstrictionHypothermia
– NEVER rely on pulse oximetry!
Universal Algorithm

10
VF / Pulseless VT
Case 3

11
VF / Pulseless VT
•Epinephrine 1 mg IV push, repeat every 3 to 5 minutesor
•Vasopressin 40 U IV, single dose, 1 time only
Resume attempts to defibrillate1 x 360 J (or equivalent biphasic) within 30 to 60 seconds
Consider antiarrhythmics:•Amiodarone (llb for persistent or recurrent VF/pulseless VT)•Lidocaine (Indeterminate for persistent or recurrent VF/pulseless VT)•Magnesium (llb if known hypomagnesemic state)•Procainamide (Indeterminate for persistent VF/pulseless VT;
llb for recurrent VF/pulseless VT)
Resume attempts to defibrillate

12
Epinephrine
Indications (When & Why?) – Increases:
Heart rateForce of contractionConduction velocity
– Peripheral vasoconstriction– Bronchial dilation
VF / Pulseless VT

13
Epinephrine
Dosing (How?)– 1 mg IV push; may repeat every 3 to 5
minutes– May use higher doses (0.2 mg/kg) if lower
dose is not effective– Endotracheal Route
2.0 to 2.5 mg diluted in 10 mL normal saline
VF / Pulseless VT

14
Epinephrine
Dosing (How?)– Alternative regimens for second dose (Class
IIb)Intermediate: 2 to 5 mg IV push, every 3 to 5
minutesEscalating: 1 mg, 3 mg, 5 mg IV push, each
dose 3 minutes apartHigh: 0.1 mg/kg IV push, every 3 to 5 minutes
VF / Pulseless VT

15
Epinephrine
Precautions (Watch Out!)– Raising blood pressure and increasing heart
rate may cause myocardial ischemia, angina, and increased myocardial oxygen demand
– Do not mix or give with alkaline solutions– Higher doses have not improved outcome &
may cause myocardial dysfunction
VF / Pulseless VT

16
Vasopressin
Indications (When & Why?)– Used to “clamp” down on vessels– Improves perfusion of heart, lungs, and brain– No direct effects on heart
VF / Pulseless VT

17
Vasopressin
Dosing (How?)– One time dose of 40 units only– May be substituted for epinephrine– Not repeated at any time– May be given down the endotracheal tube
DO NOT double the doseDilute in 10 mL of NS
VF / Pulseless VT

18
Vasopressin
Precautions (Watch Out!)– May result in an initial increase in blood
pressure immediately following return of pulse
– May provoke cardiac ischemia
VF / Pulseless VT

19
Amiodarone
Indications (When & Why?)– Powerful antiarrhythmic with substantial
toxicity, especially in the long term – Intravenous and oral behavior are quite
different – Has effects on sodium & potassium
VF / Pulseless VT

20
Amiodarone
Dosing (How?)– Should be diluted in 20 to 30 mL of D5W
300 mg bolus after first Epinephrine doseRepeat doses at 150 mg
VF / Pulseless VT

21
Amiodarone
Precautions (Watch Out!)– May produce vasodilation & shock– May have negative inotropic effects– Terminal elimination
Half-life lasts up to 40 days
VF / Pulseless VT

22
Lidocaine
Indications (When & Why?) – Depresses automaticity– Depresses excitability– Raises ventricular fibrillation threshold– Decreases ventricular irritability
VF / Pulseless VT

23
Lidocaine
Dosing (How?)– Initial dose: 1.0 to 1.5 mg/kg IV– For refractory VF may repeat 1.0 to 1.5
mg/kg IV in 3 to 5 minutes; maximum total dose, 3 mg/kg
– A single dose of 1.5 mg/kg IV in cardiac arrest is acceptable
– Endotracheal administration: 2 to 2.5 mg/kg diluted in 10 mL of NS
VF / Pulseless VT

24
Lidocaine
Dosing (How?)– Maintenance Infusion
2 to 4 mg/min
1000 mg / 250 mL D5W = 4 mg/mL– 15 mL/hr = 1 mg/min– 30 mL/hr = 2 mg/min– 45 mL/hr = 3 mg/min– 60 mL/hr = 4 mg/min
VF / Pulseless VT

25
Lidocaine
Precautions (Watch Out!)– Reduce maintenance dose (not loading
dose) in presence of impaired liver function or left ventricular dysfunction
– Discontinue infusion immediately if signs of toxicity develop
VF / Pulseless VT

26
Magnesium Sulfate
Indications (When & Why?)– Cardiac arrest associated with torsades de
pointes or suspected hypomagnesemic state– Refractory VF– VF with history of ETOH abuse– Life-threatening ventricular arrhythmias due
to digitalis toxicity, tricyclic overdose
VF / Pulseless VT

27
Magnesium Sulfate
Dosing (How?)– 1 to 2 g (2 to 4 mL of a 50% solution)
diluted in 10 mL of D5W IV push
VF / Pulseless VT

28
Magnesium Sulfate
Precautions (Watch Out!)– Occasional fall in blood pressure with rapid
administration– Use with caution if renal failure is present
VF / Pulseless VT

29
Procainamide
Indications (When & Why?)– Recurrent VF– Depresses automaticity– Depresses excitability– Raises ventricular fibrillation threshold– Decreases ventricular irritability
VF / Pulseless VT

30
Procainamide
Dosing (How?)– 30 mg/min IV infusion – May push at 50 mg/min in cardiac arrest– In refractory VF/VT, 100 mg IV push doses
given every 5 minutes are acceptable– Maximum total dose: 17 mg/kg
VF / Pulseless VT

31
Procainamide
Dosing (How?)– Maintenance Infusion
1 to 4 mg/min
1000 mg / 250 mL of D5W = 4 mg/mL– 15 mL/hr = 1 mg/min– 30 mL/hr = 2 mg/min– 45 mL/hr = 3 mg/min– 60 mL/hr = 4 mg/min
VF / Pulseless VT

32
Procainamide
Precautions (Watch Out!)– If cardiac or renal dysfunction
is present, reduce maximum total dose to 12 mg/kg and maintenance infusion to 1 to 2 mg/min
– Remember Endpoints of Administration
VF / Pulseless VT

33
PEA
Case 4

34
PEA
Atropine 1 mg IV (if PEA rate is slow),repeat every 3 to 5 minutes as needed, to a totaldose of 0.04 mg/kg
• Hypovolemia• Hypoxia• Hydrogen ion—acidosis• Hyper-/hypokalemia• Hypothermia
• Tablets (drug OD, accidents)• Tamponade, cardiac• Tension pneumothorax• Thrombosis, coronary (ACS)• Thrombosis, pulmonary (embolism)
Review for most frequent causes
Epinephrine 1 mg IV push,repeat every 3 to 5 minutes

35
Epinephrine
Indications (When & Why?) – Increases:
Heart rateForce of contractionConduction velocity
– Peripheral vasoconstriction– Bronchial dilation
Pulseless Electrical Activity

36
Epinephrine
Dosing (How?)– 1 mg IV push; may repeat every 3 to 5
minutes– May use higher doses (0.2 mg/kg) if lower
dose is not effective– Endotracheal Route
2.0 to 2.5 mg diluted in 10 mL normal saline
Pulseless Electrical Activity

37
Epinephrine
Precautions (Watch Out!)– Raising blood pressure and increasing heart
rate may cause myocardial ischemia, angina, and increased myocardial oxygen demand
– Do not mix or give with alkaline solutions– Higher doses have not improved outcome &
may cause myocardial dysfunction
Pulseless Electrical Activity

38
Atropine Sulfate
Indications (When & Why?)– Should only be used for bradycardia
Relative or Absolute
– Used to increase heart rate
Pulseless Electrical Activity

39
Atropine Sulfate
Dosing (How?)– 1 mg IV push – Repeat every 3 to 5 minutes– May give via ET tube (2 to 2.5 mg) diluted
in 10 mL of NS– Maximum Dose: 0.04 mg/kg
Pulseless Electrical Activity

40
Atropine Sulfate
Precautions (Watch Out!)– Increases myocardial oxygen demand– May result in unwanted tachycardia or
dysrhythmia
Pulseless Electrical Activity

41
Asystole
Case 5

42
AsystoleTranscutaneous pacing:
If considered, perform immediately
Epinephrine 1 mg IV push,repeat every 3 to 5 minutes
Atropine 1 mg IV,repeat every 3 to 5 minutesup to a total of 0.04 mg/kg
Asystole persistsWithhold or cease resuscitation efforts?
• Consider quality of resuscitation?• Atypical clinical features present?• Support for cease-efforts protocols in place?

43
Epinephrine
Indications (When & Why?) – Increases:
Heart rateForce of contractionConduction velocity
– Peripheral vasoconstriction– Bronchial dilation
Asystole: The Silent Heart Algorithm

44
Epinephrine
Dosing (How?)– 1 mg IV push; may repeat every 3 to 5
minutes– May use higher doses (0.2 mg/kg) if lower
dose is not effective– Endotracheal Route
2.0 to 2.5 mg diluted in 10 mL normal saline
Asystole: The Silent Heart Algorithm

45
Epinephrine
Precautions (Watch Out!)– Raising blood pressure and increasing heart
rate may cause myocardial ischemia, angina, and increased myocardial oxygen demand
– Do not mix or give with alkaline solutions– Higher doses have not improved outcome &
may cause myocardial dysfunction
Asystole: The Silent Heart Algorithm

46
Atropine Sulfate
Indications (When & Why?)– Used to increase heart rate
Questionable absolute bradycardia
Asystole: The Silent Heart Algorithm

47
Atropine Sulfate
Dosing (How?)– 1 mg IV push – Repeat every 3 to 5 minutes– May give via ET tube (2 to 2.5 mg) diluted
in 10 mL of NS– Maximum Dose: 0.04 mg/kg
Asystole: The Silent Heart Algorithm

48
Atropine Sulfate
Precautions (Watch Out!)– Increases myocardial oxygen demand
Asystole: The Silent Heart Algorithm

49
Other Cardiac Arrest Drugs

50
Calcium Chloride
Indications (When & Why?)– Known or suspected hyperkalemia (eg, renal
failure)– Hypocalcemia (blood transfusions)– As an antidote for toxic effects of calcium
channel blocker overdose– Prevent hypotension caused by calcium
channel blockers administration
Other Cardiac Arrest Drugs

51
Calcium Chloride
Dosing (How?)– IV Slow Push
8 to 16 mg/kg (usually 5 to 10 mL) IV for hyperkalemia and calcium channel blocker overdose
2 to 4 mg/kg (usually 2 mL) IV for prophylactic pretreatment before IV calcium channel blockers
Other Cardiac Arrest Drugs

52
Calcium Chloride
Precautions (Watch Out!)– Do not use routinely in cardiac arrest– Do not mix with sodium bicarbonate
Other Cardiac Arrest Drugs

53
Sodium Bicarbonate
Indications (When & Why?)– Class I if known preexisting hyperkalemia– Class IIa if known preexisting bicarbonate-
responsive acidosis– Class IIb if prolonged resuscitation with effective
ventilation; upon return of spontaneous circulation– Class III (not useful or effective) in hypoxic lactic
acidosis or hypercarbic acidosis (eg, cardiac arrest and CPR without intubation)
Other Cardiac Arrest Drugs

54
Sodium Bicarbonate
Dosing (How?)– 1 mEq/kg IV bolus– Repeat half this dose every 10 minutes
thereafter– If rapidly available, use arterial blood gas
analysis to guide bicarbonate therapy (calculated base deficits or bicarbonate concentration)
Other Cardiac Arrest Drugs

55
Sodium Bicarbonate
Precautions (Watch Out!)– Adequate ventilation and CPR, not
bicarbonate, are the major "buffer agents" in cardiac arrest
– Not recommended for routine use in cardiac arrest patients
Other Cardiac Arrest Drugs

56
Acute Coronary Syndromes
Case 6

57

58
Acute Coronary Syndromes
Immediate assessment (<10 minutes)• Measure vital signs (automatic/standard BP cuff)• Measure oxygen saturation• Obtain IV access• Obtain 12-lead ECG (physician reviews)• Perform brief, targeted history and physical exam;
focus on eligibility for fibrinolytic therapy• Obtain initial serum cardiac marker levels• Evaluate initial electrolyte and coagulation studies• Request, review portable chest x-ray (<30 minutes)
Chest painsuggestive of ischemia
Immediate general treatment• Oxygen at 4 L/min• Aspirin 160 to 325 mg• Nitroglycerin SL or spray• Morphine IV (if pain not relieved with
nitroglycerin)
Memory aid: “MONA” greetsall patients (Morphine, Oxygen, Nitroglycerin, Aspirin)
EMS personnel canperform immediateassessment and treat-ment (“MONA”),including initial 12-lead
ECG and review forfibrinolytic therapyindications andcontraindications.
Assess initial 12-lead ECG

59
Aspirin
Indications (When & Why?)– Administer to all patients with ACS,
particularly reperfusion candidatesGive as soon as possible
– Blocks formation of thromboxane A2, which causes platelets to aggregate
Acute Coronary Syndromes

60
Aspirin
Dosing (How?)– 160 to 325 mg tablets
Preferably chewedMay use suppository
– Higher doses may be harmful
Acute Coronary Syndromes

61
Aspirin
Precautions (Watch Out!)– Relatively contraindicated in patients with
active ulcer disease or asthma
Acute Coronary Syndromes

62
Nitroglycerine
Indications (When & Why?)– Chest pain of suspected cardiac origin– Unstable angina– Complications of AMI, including congestive
heart failure, left ventricular failure– Hypertensive crisis or urgency with chest
pain
Acute Coronary Syndromes

63
Nitroglycerin
Indications (When & Why?)– Decreases pain of ischemia– Increases venous dilation– Decreases venous blood return to heart – Decreases preload and cardiac
oxygen consumption– Dilates coronary arteries– Increases cardiac collateral flow
Acute Coronary Syndromes

64
Nitroglycerine
Dosing (How?)– Sublingual Route
0.3 to 0.4 mg; repeat every 5 minutes– Aerosol Spray
Spray for 0.5 to 1.0 second at 5 minute intervals– IV Infusion
Infuse at 10 to 20 µg/minRoute of choice for emergenciesTitrate to effect
Acute Coronary Syndromes

65
Nitroglycerine
Precautions (Watch Out!)– Use extreme caution if systolic BP <90 mm Hg– Use extreme caution in RV infarction
– Suspect RV infarction with inferior ST changes
– Limit BP drop to 10% if patient is normotensive– Limit BP drop to 30% if patient is hypertensive– Watch for headache, drop in BP, syncope,
tachycardia– Tell patient to sit or lie down during administration
Acute Coronary Syndromes

66
Morphine Sulfate
Indications (When & Why?)– Chest pain and anxiety associated with AMI
or cardiac ischemia– Acute cardiogenic pulmonary edema (if
blood pressure is adequate)
Acute Coronary Syndromes

67
Morphine Sulfate
Indications (When & Why?)– To reduce pain of ischemia– To reduce anxiety– To reduce extension of ischemia by reducing
oxygen demands
Acute Coronary Syndromes

68
Morphine Sulfate
Dosing (How?)– 1 to 3 mg IV (over 1 to 5 minutes) every 5 to
10 minutes as needed
Acute Coronary Syndromes

69
Morphine Sulfate
Precautions (Watch Out!)– Administer slowly and titrate to effect– May compromise respiration; therefore use
with caution in acute pulmonary edema– Causes hypotension in volume-depleted
patients
Acute Coronary Syndromes

70
Acute Coronary Syndromes
• ST elevation or new or presumably new LBBB:
strongly suspicious for injury
• ST-elevation AMI
• ST depression or dynamicT-wave inversion:
strongly suspicious for ischemia
• High-risk unstable angina/non–ST-elevation AMI
• Nondiagnostic ECG:absence of changes in ST segment or T waves
• Intermediate/low-riskunstable angina

71
ST Elevation

72
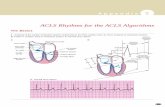
Recognition of AMI
Know what to look for—– ST elevation >1 mm– 3 contiguous leads
Know where to look– Refer to 2000 ECC
HandbookPR baseline
ST-segment deviation= 4.5 mm
J point plus0.04 second

73
ST Elevation
Baseline
Ischemia—tall or inverted T wave (infarct),ST segment may be depressed (angina)
Injury—elevated ST segment, T wave may invert
Infarction (Acute)—abnormal Q wave,ST segment may be elevated and T wavemay be inverted
Infarction (Age Unknown)—abnormal Q wave,ST segment and T wave returned to normal

74
Beta Blockers
Indications (When & Why?)– To reduce myocardial ischemia and damage
in AMI patients with elevated heart rates, blood pressure, or both
– Blocks catecholamines from binding to ß-adrenergic receptors
– Reduces HR, BP, myocardial contractility – Decreases AV nodal conduction – Decreases incidence of primary VF
Acute Coronary Syndromes

75
Beta Blockers
Dosing (How?)– Esmolol
0.5 mg/kg over 1 minute, followed by continuous infusion at 0.05 mg/kg/min
Titrate to effect, Esmolol has a short half-life (<10 minutes)
– Labetalol 10 mg labetalol IV push over 1 to 2 minutes May repeat or double labetalol every 10 minutes to a
maximum dose of 150 mg, or give initial dose as a bolus, then start labetalol infusion 2 to 8 µg/min
Acute Coronary Syndromes

76
Beta Blockers
Dosing (How?)– Metoprolol
5 mg slow IV at 5-minute intervals to a total of 15 mg
– Atenolol 5 mg slow IV (over 5 minutes) Wait 10 minutes, then give second dose of 5 mg slow IV
(over 5 minutes)
– Propranolol 1 to 3 mg slow IV. Do not exceed 1 mg/min Repeat after 2 minutes if necessary
Acute Coronary Syndromes

77
Beta Blockers
Precautions (Watch Out!)– Concurrent IV administration with IV calcium
channel blocking agents like verapamil or diltiazem can cause severe hypotension
– Avoid in bronchospastic diseases, cardiac failure, or severe abnormalities in cardiac conduction
– Monitor cardiac and pulmonary status during administration
– May cause myocardial depression
Acute Coronary Syndromes

78
Heparin
Indications (When & Why?)– For use in ACS patients with Non Q wave MI
or unstable angina– Inhibits thrombin generation by factor Xa
inhibition and also inhibit thrombin indirectly by formation of a complex with antithrombin III
Acute Coronary Syndromes

79
Heparin
Dosing (How?)– Initial bolus 60 IU/kg
Maximum bolus: 4000 IU
– Continue at 12 IU/kg/hr (maximum 1000 IU/hr for patients < 70 kg), round to the nearest 50 IU
Acute Coronary Syndromes

80
Heparin
Dosing (How?)– Adjust to maintain activated partial thromboplastin
time (aPTT) 1.5 to 2.0 times the control values for 48 hours or angiography
– Target range for aPTT after first 24 hours is between 50 & 70 seconds (may vary with laboratory)
– Check aPTT at 6, 12, 18, and 24 hours– Follow Institutional Heparin Protocol
Acute Coronary Syndromes

81
Heparin
Precautions (Watch Out!)– Same contraindications as for fibrinolytic
therapy: active bleeding; recent intracranial, intraspinal or eye surgery; severe hypertension; bleeding disorders; gastroinintestinal bleeding
– DO NOT use if platelet count is below 100 000
Acute Coronary Syndromes

82
Glycoprotein IIb/IIIa Inhibitors
Indications (When & Why?)– Inhibit the integrin glycoprotein IIb/IIIa
receptor in the membrane of platelets, inhibiting platelet aggregation
– Indicated for Acute Coronary Syndromes without ST segment elevation
Acute Coronary Syndromes

83
Glycoprotein IIb/IIIa Inhibitors
Indications (When & Why?)– Abciximab (ReoPro)
Non Q wave MI or unstable angina with planned PCI within 24 hours
Must use with heparin– Binds irreversibly with platelets– Platelet function recovery requires 48 hours
Acute Coronary Syndromes

84
Glycoprotein IIb/IIIa Inhibitors
Indications (When & Why?)– Eptifibitide (Integrilin)
Non Q wave MI, unstable angina managed medically, and unstable angina / Non Q wave MI patients undergoing PCI
Platelet function recovers within 4 to 8 hours after discontinuation
Acute Coronary Syndromes

85
Glycoprotein IIb/IIIa Inhibitors
Indications (When & Why?)– Tirofiban (Aggrastat)
Non Q wave MI, unstable angina managed medically, and unstable angina / Non Q wave MI patients undergoing PCI
Platelet function recovers within 4 to 8 hours after discontinuation
Acute Coronary Syndromes

86
Glycoprotein IIb/IIIa Inhibitors
Dosing (How?)– NOTE: Check package insert for current
indications, doses, and duration of therapy.
Optimal duration of therapy has NOT been established.
Acute Coronary Syndromes

87
Glycoprotein IIb/IIIa Inhibitors
Dosing (How?)– Abciximab (ReoPro)
ACS with planned PCI within 24 hours– 0.25 mg/kg bolus (10 to 60 minutes before
procedure), then 0.125 mcg/kg/min infusionPCI only
– 0.25 mg/kg bolus– Then 10 mcg/min infusion
Acute Coronary Syndromes

88
Glycoprotein IIb/IIIa Inhibitors
Dosing (How?)– Eptifibitide (Integrilin)
Acute Coronary Syndromes– 180 mcg/kg IV bolus, then 2 mcg/kg/min
infusionPCI
– 135 mcg/kg IV bolus, then begin 0.5 mcg/kg/min infusion, then repeat bolus in 10 minutes
Acute Coronary Syndromes

89
Glycoprotein IIb/IIIa Inhibitors
Dosing (How?)– Tirofiban (Aggrastat)
Acute Coronary Syndromes or PCI– 0.4 mcg/kg/min infusion IV for 30 minutes– Then 0.1 mcg/kg/min infusion
Acute Coronary Syndromes

90
Glycoprotein IIb/IIIa Inhibitors
Precautions (Watch Out!)– Active internal bleeding or bleeding disorder
within 30 days– History of intracranial hemorrhage or other
bleeding– Surgical procedure or trauma within 1 month– Platelet count > 150 000/mm3
Acute Coronary Syndromes

91
PTCA

92
Fibrinolytics
Indications (When & Why?) – For AMI in adults
ST elevation or new or presumably new LBBB; strongly suspicious for injury
Time of onset of symptoms < 12 hours
Acute Coronary Syndromes

93
Fibrinolytics
Indications (When & Why?) – For Acute Ischemic Stroke
Sudden onset of focal neurologic deficits or alterations in consciousness
Absence of subarachnoid or intracerebral hemorrhage
Alteplase can be started in less than 3 hours of symptom onset
Acute Coronary Syndromes

94
Fibrinolytics
Dosing (How?)– For fibrinolytic use, all patients should have
2 peripheral IV lines1 line exclusively for fibrinolytic administration
Acute Coronary Syndromes

95
Fibrinolytics Dosing for AMI Patients (How?)
– Alteplase, recombinant (tPA) Accelerated Infusion
– 15 mg IV bolus– Then 0.75 mg/kg over the next 30 minutes
Not to exceed 50 mg– Then 0.5 mg/kg over the next 60 minutes
Not to exceed 35 mg 3 hour Infusion
– Give 60 mg in the first hour (initial 6 to 10 mg is given as a bolus)
– Then 20 mg/hour for 2 additional hours
Acute Coronary Syndromes

96
Fibrinolytics Dosing for AMI Patients (How?)
– Anistreplase (APSAC) Reconstitute 30 units in 50 mL of sterile water 30 units IV over 2 to 5 minutes
– Reteplase, recombinant Give first 10 unit IV bolus over 2 minutes 30 minutes later give second 10 unit IV bolus over 2
minutes– Streptokinase
1.5 million IU in a 1 hour infusion– Tenecteplase (TNKase)
Bolus 30 to 50 mg
Acute Coronary Syndromes

97
Fibrinolytics
Adjunctive Therapy for AMI Patients (How?)– 160 to 325 mg aspirin chewed as soon as
possible– Begin heparin immediately and continue for
48 hours if alteplase or Retavase is used
Acute Coronary Syndromes

98
Fibrinolytics
Dosing for Acute Ischemic Stroke (How?)– Alteplase, recombinant (tPA)
Give 0.9 mg/kg (maximum 90 mg) infused over 60 minutes
– Give 10% of total dose as an initial IV bolus over 1 minute
– Give the remaining 90% over the next 60 minutes
– Alteplase is the only agent approved for use in Ischemic Stroke patients
Acute Coronary Syndromes

99
Fibrinolytics
Precautions (Watch Out!)– Specific Exclusion Criteria
Active internal bleeding (except mensus) within 21 days
History of CVA, intracranial, or intraspinal within 3 months
Major trauma or serious injury within 14 daysAortic dissectionSevere uncontrolled hypertension
Acute Coronary Syndromes

100
Fibrinolytics
Precautions (Watch Out!)– Specific Exclusion Criteria
Known bleeding disordersProlonged CPR with evidence of thoracic traumaLumbar puncture within 7 daysRecent arterial puncture at noncompressible siteDuring the first 24 hours of fibrinolytic therapy for
ischemic stroke, do not give aspirin or heparin
Acute Coronary Syndromes

101
ACE Inhibitors
Indications (When & Why?)– Reduce mortality & improve LV dysfunction
in post AMI patients– Help prevent adverse LV remodeling, delay
progression of heart failure, and decrease sudden death & recurrent MI
Acute Coronary Syndromes

102
ACE Inhibitors
Indications (When & Why?)– Suspected MI & ST elevation in 2 or more
anterior leads– Hypertension– Clinical signs of AMI with LV dysfunction– LV ejection fraction <40%
Acute Coronary Syndromes

103
ACE Inhibitors
Indications (When & Why?)– Generally not started in the ED but within
first 24 hours after:Fibrinolytic therapy has been completedBlood pressure has stabilized
Acute Coronary Syndromes

104
ACE Inhibitors
Dosing (How?)– Should start with low-dose oral
administration (with possible IV doses for some preparations) and increase steadily to achieve a full dose within 24 to 48 hours
Acute Coronary Syndromes

105
ACE Inhibitors
Dosing (How?)– Enalapril
2.5 mg PO titrated to 20 mg BIDIV dosing of 1.25 mg IV over 5 minutes, then
1.25 to 5 mg IV every six hours
– CaptoprilStart with 6.25 mg POAdvance to 25 mg TID, then to 50 mg TID as
tolerated
Acute Coronary Syndromes

106
ACE Inhibitors
Dosing (How?)– Lisinopril (AMI dose)
5 mg within 24 hours onset of symptoms10 mg after 24 hours, then 10 mg after 48 hours,
then 10 mg PO daily for six weeks
– RamiprilStart with single dose of 2.5 mg POTitrate to 5 mg PO BID as tolerated
Acute Coronary Syndromes

107
ACE Inhibitors
Precautions (Watch Out!)– Contraindicated in pregnancy– Contraindicated in angioedema– Reduce dose in renal failure– Avoid hypotension, especially following initial
dose & in relative volume depletion
Acute Coronary Syndromes

108
Bradycardias
Case 7

109
BradycardiaBradycardia
•Slow (absolute bradycardia = rate <60 bpm)or
•Relatively slow (rate less than expected relative to underlying condition or cause)
• Assess ABCs• Secure airway noninvasively• Ensure monitor/defibrillator is available
Primary ABCD Survey
Secondary ABCD Survey• Assess secondary ABCs (invasive airway management
needed?)• Oxygen–IV access–monitor–fluids• Vital signs, pulse oximeter, monitor BP• Obtain and review 12-lead ECG• Obtain and review portable chest x-ray• Problem-focused history• Problem-focused physical examination• Consider causes (differential diagnoses)

110
Bradycardia
Intervention sequence• Atropine 0.5 to 1.0 mg• Transcutaneous pacing if available• Dopamine 5 to 20 µg/kg per minute• Epinephrine 2 to 10 µg/min• Isoproterenol 2 to 10 µg/min
Serious signs or symptoms?Due to bradycardia?
Type II second-degree AV blockor
Third-degree AV block?
Observe • Prepare for transvenous pacer• If symptoms develop, use
transcutaneous pacemaker until transvenous pacer placed
No Yes
YesNo

111
Atropine Sulfate
Indications (When & Why?)– First drug for symptomatic bradycardia
Increases heart rate by blocking the parasympathetic nervous system
Bradycardias

112
Atropine Sulfate
Dosing (How?)– 0.5 to 1.0 mg IV every 3 to 5 minutes as
needed– May give via ET tube (2 to 2.5 mg) diluted
in 10 mL of NS– Maximum Dose: 0.04 mg/kg
Bradycardias

113
Atropine Sulfate
Precautions (Watch Out!)– Use with caution in presence of myocardial
ischemia and hypoxia– Increases myocardial oxygen demand– Seldom effective for:
Infranodal (type II) AV block Third-degree block (Class IIb)
Bradycardias

114
Dopamine
Indications (When & Why?)– Second drug for symptomatic bradycardia
(after atropine)– Use for hypotension (systolic BP 70 to 100
mm Hg) with S/S of shock
Bradycardias

115
Dopamine
Dosing (How?)– IV Infusions (Titrate to Effect)
– 400 mg / 250 mL of D5W = 1600 mcg/mL– 800 mg/ 250 mL of D5W = 3200 mcg/mL
Bradycardias

116
Dopamine
Dosing (How?)– IV Infusions (Titrate to Effect)
Low Dose “Renal Dose"– 1 to 5 µg/kg per minute
Moderate Dose “Cardiac Dose"– 5 to 10 µg/kg per minute
High Dose “Vasopressor Dose"– 10 to 20 µg/kg per minute
Bradycardias

117
Dopamine
Precautions (Watch Out!)– May use in patients with hypovolemia but only after
volume replacement– May cause tachyarrhythmias, excessive
vasoconstriction– DO NOT mix with sodium bicarbonate
Bradycardias

118
Epinephrine
Indications (When & Why?) – Symptomatic bradycardia: After atropine,
dopamine, and transcutaneous pacing (Class IIb)
Bradycardias

119
Epinephrine
Dosing (How?)– Profound Bradycardia
2 to 10 µg/min infusion (add 1 mg of 1:1000 to 500 mL normal saline; infuse at 1 to 5 mL/min)
Bradycardias

120
Epinephrine
Precautions (Watch Out!)– Raising blood pressure and increasing heart
rate may cause myocardial ischemia, angina, and increased myocardial oxygen demand
– Do not mix or give with alkaline solutions
Bradycardias

121
Isoproterenol
Indications (When & Why?)– Temporary control of bradycardia in heart
transplant patients– Class IIb at low doses for symptomatic
bradycardia– Heart Transplant Patients!
Bradycardias

122
Isoproterenol
Dosing (How?)– Infuse at 2 to 10 µg/min– Titrate to adequate heart rate
Bradycardias

123
Isoproterenol
Precautions (Watch Out!)– Increases myocardial oxygen requirements,
which may increase myocardial ischemia– DO NOT administer with poison/drug-
induced shockException: Beta Blocker Poisoning
Bradycardias

124
Stable Tachycardias
Case 9

125
Diltiazem
Indications (When & Why?)– To control ventricular rate in atrial fibrillation
and atrial flutter– Use after adenosine to treat refractory PSVT
in patients with narrow QRS complex and adequate blood pressure
– As an alternative, use verapamil
Stable Tachycardias

126
Diltiazem
Dosing (How?)– Acute Rate Control
15 to 20 mg (0.25 mg/kg) IV over 2 minutesMay repeat in 15 minutes at 20 to 25 mg (0.35
mg/kg) over 2 minutes
– Maintenance Infusion5 to 15 mg/hour, titrated to heart rate
Stable Tachycardias

127
Diltiazem
Precautions (Watch Out!)– Do not use calcium channel blockers for
tachycardias of uncertain origin– Avoid calcium channel blockers in patients with
Wolff-Parkinson-White syndrome, in patients with sick sinus syndrome, or in patients with AV block without a pacemaker
– Expect blood pressure drop resulting from peripheral vasodilation
– Concurrent IV administration with IV ß-blockers can cause severe hypotension
Stable Tachycardias

128
Verapamil
Indications (When & Why?)– Used as an alternative to diltiazem for
ventricular rate control in atrial fibrillation and atrial flutter
– Drug of second choice (after adenosine) to terminate PSVT with narrow QRS complex and adequate blood pressure
Stable Tachycardias

129
Verapamil
Dosing (How?)– 2.5 to 5.0 mg IV bolus over 1to 2 minutes– Second dose: 5 to 10 mg, if needed, in 15 to
30 minutes. Maximum dose: 30 mg– Older patients: Administer over 3 minutes
Stable Tachycardias

130
Verapamil
Precautions (Watch Out!)– Do not use calcium channel blockers for
wide-QRS tachycardias of uncertain origin– Avoid calcium channel blockers in patients
with Wolff-Parkinson-White syndrome and atrial fibrillation, sick sinus syndrome, or second- or third-degree AV block without pacemaker
Stable Tachycardias

131
Verapamil
Precautions (Watch Out!)– Expect blood pressure drop caused by
peripheral vasodilation– IV calcium can restore blood pressure, and
some experts recommend prophylactic calcium before giving calcium channel blockers
– Concurrent IV administration with IV ß-blockers may produce severe hypotension
Stable Tachycardias

132
Adenosine
Indications (When & Why?)– First drug for narrow-complex PSVT– May be used diagnostically (after lidocaine)
in wide-complex tachycardias of uncertain type
Stable Tachycardias

133
Adenosine
Dose (How?)– IV Rapid Push– Initial bolus of 6 mg given rapidly over 1 to 3
seconds followed by normal saline bolus of 20 mL; then elevate the extremity
– Repeat dose of 12 mg in 1 to 2 minutes if needed
– A third dose of 12 mg may be given in 1 to 2 minutes if needed
Stable Tachycardias

134
Adenosine
Precautions (Watch Out!)– Transient side effects include:
Facial FlushingChest painBrief periods of asystole or bradycardia
– Less effective in patients taking theophyllines
Stable Tachycardias

135
Beta Blockers
Indications (When & Why?)– To convert to normal sinus rhythm or to slow
ventricular response (or both) in supraventricular tachyarrhythmias (PSVT, atrial fibrillation, or atrial flutter)
– ß-Blockers are second-line agents after adenosine, diltiazem, or digoxin
Stable Tachycardias

136
Beta Blockers
Dosing (How?)– Esmolol
0.5 mg/kg over 1 minute, followed by continuous infusion at 0.05 mg/kg/min
Titrate to effect, Esmolol has a short half-life (<10 minutes)
– Labetalol 10 mg labetalol IV push over 1 to 2 minutes May repeat or double labetalol every 10 minutes to a
maximum dose of 150 mg, or give initial dose as a bolus, then start labetalol infusion 2 to 8 µg/min
Stable Tachycardias

137
Beta Blockers
Dosing (How?)– Metoprolol
5 mg slow IV at 5-minute intervals to a total of 15 mg
– Atenolol 5 mg slow IV (over 5 minutes) Wait 10 minutes, then give second dose of 5 mg slow IV
(over 5 minutes)
– Propranolol 1 to 3 mg slow IV. Do not exceed 1 mg/min Repeat after 2 minutes if necessary
Stable Tachycardias

138
Beta Blockers
Precautions (Watch Out!)– Concurrent IV administration with IV calcium
channel blocking agents like verapamil or diltiazem can cause severe hypotension
– Avoid in bronchospastic diseases, cardiac failure, or severe abnormalities in cardiac conduction
– Monitor cardiac and pulmonary status during administration
– May cause myocardial depression
Stable Tachycardias

139
Digoxin
Indications (When & Why?)– To slow ventricular response in atrial
fibrillation or atrial flutter– Third-line choice for PSVT
Stable Tachycardias

140
Digoxin
Dosing (How?)– IV Infusion
Loading doses of 10 to 15 µg/kg provide therapeutic effect with minimum risk of toxic effects
Maintenance dose is affected by body size and renal function
Stable Tachycardias

141
Digoxin
Precautions (Watch Out!)– Toxic effects are common and are frequently
associated with serious arrhythmias– Avoid electrical cardioversion unless
condition is life threateningUse lower current settings (10 to 20 Joules)
Stable Tachycardias

142
Amiodarone
Indications (When & Why?)– Powerful antiarrhythmic with substantial
toxicity, especially in the long term – Intravenous and oral behavior are quite
different
Stable Tachycardias

143
Amiodarone
Dosing (How?)– Stable Wide-Complex Tachycardias
Rapid Infusion– 150 mg IV over 10 minutes (15 mg/min)– May repeat
Slow Infusion– 360 mg IV over 6 hours (1 mg/min)
Stable Tachycardias

144
Amiodarone
Dosing (How?)– Maintenance Infusion
540 mg IV over 18 hours (0.5 mg/min)
Stable Tachycardias

145
Amiodarone
Precautions (Watch Out!)– May produce vasodilation & shock– May have negative inotropic effects– May prolong QT Interval
DO NOT administer with other drugs that may prolong QT Interval (Procainamide)
– Terminal eliminationHalf-life lasts up to 40 days
Stable Tachycardias

146
Amiodarone
Precautions (Watch Out!)– Contraindicated in:
Second or third degree A-V blockSevere bradycardiaPregnancyCHFHypokalaemiaLiver dysfunction
Stable Tachycardias

147
Lidocaine
Indications (When & Why?) – Depresses automaticity– Depresses excitability– Raises ventricular fibrillation threshold– Decreases ventricular irritability
Stable Tachycardias

148
Lidocaine
Dosing (How?)– For stable VT, wide-complex tachycardia of
uncertain type, significant ectopy, use as follows:
1.0 to 1.5 mg/kg IV pushRepeat 0.5 to 0.75 mg/kg every 5 to 10 minutes;
maximum total dose, 3 mg/kg
Stable Tachycardias

149
Lidocaine
Dosing (How?)– Maintenance Infusion
2 to 4 mg/min
Stable Tachycardias

150
Lidocaine
Precautions (Watch Out!)– Reduce maintenance dose (not loading
dose) in presence of impaired liver function or left ventricular dysfunction
– Discontinue infusion immediately if signs of toxicity develop
Stable Tachycardias

151
Magnesium Sulfate
Indications (When & Why?)– Torsades de pointes with a pulse– Wide-complex tachycardia with history of
ETOH abuse– Life-threatening ventricular arrhythmias due
to digitalis toxicity, tricyclic overdose
Stable Tachycardias

152
Magnesium Sulfate
Dosing (How?)– Loading dose of 1 to 2 grams mixed in 50 to
100 mL of D5W IV push over 5 to 60 minutes
Stable Tachycardias

153
Magnesium Sulfate
Dosing (How?)– Maintenance Infusion
1 to 4 g/hour IV (titrate dose to control the torsades)
Stable Tachycardias

154
Magnesium Sulfate
Precautions (Watch Out!)– Occasional fall in blood pressure with rapid
administration– Use with caution if renal failure is present
Stable Tachycardias

155
Procainamide
Indications (When & Why?)– Depresses automaticity– Depresses excitability– Raises ventricular fibrillation threshold– Decreases ventricular irritability– Atrial fibrillation with rapid rate in Wolff-
Parkinson-White syndrome
Stable Tachycardias

156
Procainamide
Dosing (How?)– Perfusing Arrhythmia
20 mg/min IV infusion until:– Hypotension develops– Arrhythmia is suppressed– QRS widens by >50%– Maximum dose of 17 mg/kg is reached
In refractory VF/VT, 100 mg IV push doses given every 5 minutes are acceptable
Stable Tachycardias

157
Procainamide
Dosing (How?)– Maintenance Infusion
1 to 4 mg/min
Stable Tachycardias

158
Procainamide
Precautions (Watch Out!)– If cardiac or renal dysfunction
is present, reduce maximum total dose to 12 mg/kg and maintenance infusion to 1 to 2 mg/min
– Remember Endpoints of Administration
Stable Tachycardias

159
Acute Ischemic Stroke
Case 10

160
Acute Ischemic Stroke
Immediate assessment: <10 minutes from arrival• Assess ABCs, vital signs• Provide oxygen by nasal cannula• Obtain IV access; obtain blood samples (CBC,
electolytes, coagulation studies)• Check blood sugar; treat if indicated• Obtain 12-lead ECG, check for arrhythmias• Perform general neurological screening assessment• Alert Stroke Team: neurologist, radiologist,
CT technician
Immediate neurological assessment: <25 minutes from arrival• Review patient history• Establish onset (<3 hours required for fibrinolytics)• Perform physical examination• Perform neurological examination:
Determine level of consciousness (Glasgow Coma Scale) Determine level of stroke severity (NIH Stroke Scale or
Hunt and Hess Scale)• Order urgent noncontrast CT scan
(door-to–CT scan performed: goal <25 minutes from arrival)• Read CT scan (door-to–CT read: goal <45 minutes from arrival)• Perform lateral cervical spine x-ray (if patient comatose/history
of trauma)
EMS assessments and actions
Immediate assessments performed by EMSpersonnel include• Cincinnati Prehospital Stroke Scale
(includes difficulty speaking, arm weakness, facial droop)
• Los Angeles Prehospital Stroke Screen• Alert hospital to possible stroke patient• Rapid transport to hospital
Suspected Stroke
DetectionDispatchDeliveryDoor

161
Nitroprusside
Indications (When & Why?)– Hypertensive crisis
Acute Ischemic Stroke

162
Nitroprusside
Dosing (How?)– Begin at 0.1 mcg/kg/min and titrate upward
every 3 to 5 minutes to desired effectUp to 0.5 mcg/kg/min
– Action occurs within 1 to 2 minutes
Acute Ischemic Stroke

163
Nitroprusside
Dosing Precautions (How?)– Use with an infusion pump; use
hemodynamic monitoring for optimal safety– Cover drug reservoir with opaque material
Acute Ischemic Stroke

164
Nitroprusside
Precautions (Watch Out!)– Light-sensitive; therefore, wrap drug
reservoir in aluminum foil– May cause hypotension and CO2 retention– May exacerbate intrapulmonary shunting– Other side effects include headaches,
nausea, vomiting, and abdominal cramps
Acute Ischemic Stroke

165
Drugs used in Overdoses

166
Calcium Chloride
Indications (When & Why?)– As an antidote for toxic effects of calcium
channel blocker overdose
Drugs Used in Overdoses

167
Calcium Chloride
Dosing (How?)– 8 to 16 mg/kg (usually 5 to 10 mL) IV for
hyperkalemia and calcium channel blocker overdose
Drugs Used in Overdoses

168
Calcium Chloride
Precautions (Watch Out!)– Do not use routinely in cardiac arrest– Do not mix with sodium bicarbonate
Drugs Used in Overdoses

169
Flumazenil
Indications (When & Why?)– Reduce respiratory depression and sedative
effects from pure benzodiazepine overdose
Drugs Used in Overdoses

170
Flumazenil
Dosing (How?)– First Dose
0.2 mg IV over 15 seconds– Second Dose
0.3 mg IV over 30 seconds– Third Dose
0.4 mg IV over 30 seconds– Maximum Dose
3 mg
Drugs Used in Overdoses

171
Flumazenil
Precautions (Watch Out!)– Effects may not outlast effects of
benzodiazepines– Monitor for recurrent respiratory depression– DO NOT use in suspected tricyclic overdose– DO NOT use in seizure-prone patients– DO NOT use if unknown type overdose or
mixed drug overdose with drugs known to cause seizures
Drugs Used in Overdoses

172
Naloxone Hydrochloride
Indications (When & Why?)– Respiratory and neurologic depression due
to opiate intoxication unresponsive to oxygen and hyperventilation
Drugs Used in Overdoses

173
Naloxone Hydrochloride
Dosing (How?)– 0.4 to 2 mg IVP every 2 minutes– Use higher doses for complete narcotic
reversal– Can administer up to 10 mg in a short time
(10 minutes)
Drugs Used in Overdoses

174
Naloxone Hydrochloride
Precautions (Watch Out!)– May cause opiate withdrawal– Effects may not outlast effects of narcotics– Monitor for recurrent respiratory depression
Drugs Used in Overdoses

175
Review of Infusions

176
Dobutamine
Indications (When & Why?)– Consider for pump problems (congestive
heart failure, pulmonary congestion) with systolic blood pressure of 70 to 100 mm Hg and no signs of shock
– Increases Inotropy
Review of Infusions

177
Dobutamine
Dosing (How?)– Usual infusion rate is 2 to 20 µg/kg per
minute– Titrate so heart rate does not increase by
more than 10% of baseline– Hemodynamic monitoring is recommended
for optimal use
Review of Infusions

178
Dobutamine
Precautions (Watch Out!)– Avoid when systolic blood pressure <100
mm Hg with signs of shock– May cause tachyarrhythmias, fluctuations in
blood pressure, headache, and nausea– DO NOT mix with sodium bicarbonate
Review of Infusions

179
Dopamine
Indications (When & Why?)– Second drug for symptomatic bradycardia
(after atropine)– Use for hypotension (systolic BP 70 to 100
mm Hg) with S/S of shock
Review of Infusions

180
Dopamine
Dosing (How?)– IV Infusions (Titrate to Effect)
Low Dose “Renal Dose"– 1 to 5 µg/kg per minute
Moderate Dose “Cardiac Dose"– 5 to 10 µg/kg per minute
High Dose “Vasopressor Dose"– 10 to 20 µg/kg per minute
Review of Infusions

181
Dopamine
Precautions (Watch Out!)– May use in patients with hypovolemia but only after
volume replacement– May cause tachyarrhythmias, excessive
vasoconstriction– DO NOT mix with sodium bicarbonate
Review of Infusions

182
Epinephrine
Indications (When & Why?) – Symptomatic bradycardia: After atropine,
dopamine, and transcutaneous pacing (Class IIb)
Review of Infusions

183
Epinephrine
Dosing (How?)– Profound Bradycardia
2 to 10 µg/min infusion (add 1 mg of 1:1000 to 500 mL normal saline; infuse at 1 to 5 mL/min)
Review of Infusions

184
Epinephrine
Precautions (Watch Out!)– Raising blood pressure and increasing heart
rate may cause myocardial ischemia, angina, and increased myocardial oxygen demand
– Do not mix or give with alkaline solutions– Higher doses have not improved outcome &
may cause myocardial dysfunction
Review of Infusions

185
Norepinephrine
Indications (When & Why?)– For severe cardiogenic shock and
hemodynamic significant hypotension (systolic blood pressure < 70 mm/Hg) with low total peripheral resistance
– This is an agent of last resort for management of ischemic heart disease and shock
Review of Infusions

186
Norepinephrine
Dosing (How?)– 0.5 to 1 mcg/min titrated to improve blood
pressure (up to 30 mcg/min)– DO NOT administer is same IV line as
alkaline infusions– Poison/drug-induced hypotension may
higher doses to achieve adequate perfusion
Review of Infusions

187
Norepinephrine
Precautions (Watch Out!)– Increases myocardial oxygen requirements– May induce arrhythmias– Extravasation causes tissue necrosis
Review of Infusions

188
Calculating mg/min
dose X gtt factor
Solution Concentration
2 mg X 60 gtt/mL
4 mg
Using a 60 gtt set: 30 gtt/min = 30 cc/hr
= 30 gtts/min
= gtts/min

189
Calculating mcg/kg/min
dose X kg X gtt factor
solution concentration
5 mcg/min X 75 kg X 60 gtt/mL
1600 mcg/cc
Using a 60 gtt set: 18.75 cc/hr = 18.75 gtts/min
= 18.75 cc/hr
= cc/hr

190
Furosemide
Indications (When & Why?)– For adjuvant therapy of acute pulmonary
edema in patients with systolic blood pressure >90 to 100 mm Hg (without S/S of shock)
– Hypertensive emergencies– Increased intracranial pressure

191
Furosemide
Dosing (How?)– 20 to 40 mg slow IVP– If patient is taking at home, double their daily
dose

192
Furosemide
Precautions (Watch Out!)– Dehydration, hypovolemia, hypotension,
hypokalemia, or other electrolyte imbalance may occur

194
Summary
To obtain a full understanding of ACLS pharmacology requires constant review of:– Indications & Actions (When & Why?)– Dosing (How?)– Contraindications & Precautions (Watch
Out!)

195
Thank You!