013 Am09 Presentations Harris
-
Upload
simon-prince -
Category
Business
-
view
873 -
download
4
description
Transcript of 013 Am09 Presentations Harris

RPA 2009 Annual MeetingRPA 2009 Annual Meeting
Jeffrey P. Harris, MD, FACPJeffrey P. Harris, MD, FACPJeffrey P. Harris, MD, FACPJeffrey P. Harris, MD, FACP
Patient Centered Medical Home Patient Centered Medical Home
March 23, 2009March 23, 2009

Three Commonly Posed Questions:
1. Why does the ACP, with nearly equal numbers of general internists and subspecialty internists members, advocate for a system that appears more beneficial to primary care physicians?
2. How will my practice and my patients' experiences change?
3. Why should subspecialists support this model?

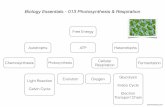
PCMH/The Central Hub of Care
• why is it needed
• what must it provide
• how might it be funded
• where should it be

Escalating CostsInternational Comparison of Spending on Health, 1980–2004
0
1000
2000
3000
4000
5000
6000
7000
1980
1982
1984
1986
1988
1990
1992
1994
1996
1998
2000
2002
2004
United StatesGermanyCanadaFranceAustraliaUnited Kingdom
Data: OECD Health Data 2005 and 2006.
0
2
4
6
8
10
12
14
16
United StatesGermanyCanadaFranceAustraliaUnited Kingdom
Average spending on healthper capita ($US PPP)
Total expenditures on healthas percent of GDP
Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006
EFFICIENCY
4

Total outlays in billions
$454 $486 $514$567 $568
$636 $681$729
$814 $850 $887
$0
$200
$400
$600
$800
$1,000
2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018
Projected Medicare Outlays, 2008-2018
NOTE: Numbers have been rounded to nearest whole number. SOURCE: Kaiser Family Foundation, based on Congressional Budget Office, The Budget and Economic Outlook: An Update, January 2008.
16% 16% 16% 17% 17% 18% 18% 19% 20% 20% 20%
3% 3% 3% 3% 3% 3% 4% 4% 4% 4% 4%
Share of:Federal BudgetGross
Domestic Product

Medicare Beneficiaries and The Number of Workers Per Beneficiary
79
62
47
19
40
34
20
1966 1970 1990 2000 2010 2020 2030
Millions of beneficiaries
4.0
2.4
2.9
3.7
2000 2010 2020 2030
Number of workers per beneficiary
SOURCE: Kaiser Family Foundation, based on 2001 and 2008 Annual Reports of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds.

USA: LESS EFFICIENTAdministrative and Insurance Costs as %
of National Health Expenditures 2003
2.60%
5.60%
4.80%4.20%
4.00%3.30%
2.10%
7.30%
1.90%
0.0%
1.0%
2.0%
3.0%
4.0%
5.0%
6.0%
7.0%
8.0%
FR
JA
P
CA
N
UK
NT
H
AU
ST
SW
Z
GE
R
US
A
Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. www.commonwealthfund.org

Life Expectancy at Birth in 2005Life Expectancy at Birth in 2005
77.8 77.9
79 79 7979.4 79.4
80.2 80.3
80.9
81.3
82
75
76
77
78
79
80
81
82
USA DEN GER UK NZ BEL NETH CAN FR AUST SWZ JAP
Source: OEDC Data, 2007

CriteriaCriteria: Overall Mission to Achieve Long, Healthy : Overall Mission to Achieve Long, Healthy and Productive Livesand Productive Lives
Infant Mortality per 1000 Births (2005)
3.6 3.7 3.9 4.2 4.45 5.1 5.1
6.8
4.9
2.8
0
2
4
6
8
JAP
FR
BEL
GER
SW
Z
DEN
NET
H
AU
ST
NZ
UK
USA
Source: OEDC Data, 2007

USA: MORE ERRORSUSA: MORE ERRORSDeaths Due to Surgical or Medical Mishaps Deaths Due to Surgical or Medical Mishaps
per 100,000 Population in 2004per 100,000 Population in 2004
0.7
0.6
0.5 0.5 0.5
0.4 0.4
0.2 0.2
0.0
0.1
0.2
0.3
0.4
0.5
0.6
0.7
0.8
United
States
Germany Canada France United
K ingdom
Australia OECD
Median
J apan Netherlands
a2003b2002
ab
b
bb
b
Source: The Commonwealth Fund, calculated from OECD Health Data 2006. Cylus J and Anderson GF. Multinational Comparisons of Health Systems Data, 2006


Buyers’ remorseBuyers’ remorse
Statement of Peter R. Rosa. Director, Growth in Health Care Costs, Congressional Budget Office, before the Committee on the Budget
United States Senate, January 31, 2008
www.cbo.gov/ftpdocs/89xx/doc8948/01-31-HealthcareSlides.pdf

Primary Care Associated with Primary Care Associated with Decreased CostsDecreased Costs
• According to the According to the Center for Evaluative Clinical Center for Evaluative Clinical Sciences at DartmouthSciences at Dartmouth, for patients with severe , for patients with severe chronic diseases, those who live U.S. states that chronic diseases, those who live U.S. states that relied more on primary care have:relied more on primary care have:– Lower Medicare spending (inpatient reimbursements and Part Lower Medicare spending (inpatient reimbursements and Part
B payments)B payments)– Lower resource inputs (hospital beds, ICU beds, total Lower resource inputs (hospital beds, ICU beds, total
physician labor, primary care labor, and medical specialist physician labor, primary care labor, and medical specialist labor)labor)
– Lower utilization rates (physician visits, days in ICUs, days in Lower utilization rates (physician visits, days in ICUs, days in the hospital, and fewer patients seeing 10 or more the hospital, and fewer patients seeing 10 or more physicians)physicians)
– Better quality of care (fewer ICU deaths and a higher Better quality of care (fewer ICU deaths and a higher composite quality scorecomposite quality score
Dartmouth Atlas of Health Care, Variation among States in the Management of Severe Chronic Illness, 2006

States with red circles have PC/Specialty Ratio of < 1.0States with green circles have PC/Specialty Ratio of >1.45
[In the last two years of life]
Dartmouth atlas
Quality/Cost Impact

Primary Care Score vs Health Care Expenditures 1997
Source: The Commonwealth Fund, Data from B. Starfield, “Why More Primary Care: Better Outcomes, Lower Costs, Greater Equity,” Presentation to the Primary Care Roundtable: Strengthening Adult Primary Care: Models and Policy Options, October 3, 2006. Quality/Cost Impact

OECD = Organization for Economic Cooperation & DevelopmentPYLL = Potential years of life lost

HPPC Examined Health Care in the USA HPPC Examined Health Care in the USA and Systems in 12 Other Countriesand Systems in 12 Other Countries

LessonLesson: High performing systems encourage : High performing systems encourage patients to be prudent purchasers and engage in patients to be prudent purchasers and engage in
healthy behaviorshealthy behaviors
• Cost-sharing Cost-sharing with co-payment schedules based with co-payment schedules based on incomeon income can help restrain costs while assuring can help restrain costs while assuring that poorer individuals have access that poorer individuals have access
• Incentives to encourage personal responsibility Incentives to encourage personal responsibility can be effective in influencing healthy behaviors, can be effective in influencing healthy behaviors, improved health outcomes and responsible improved health outcomes and responsible utilization, without punishing people who fail to utilization, without punishing people who fail to adopt recommended behaviors or lifestyles adopt recommended behaviors or lifestyles
Belgium
France
Japan
New Zealand
Switzerland
Australia Belgium Japan
New Zealand Netherlands Switzerland
Taiwan

Lesson: Lesson: High performing systems High performing systems measure their own performancemeasure their own performance
• Performance measures, Performance measures, financial incentives linked to financial incentives linked to quality, and active monitoring quality, and active monitoring of performance are key of performance are key elements of high performing elements of high performing systemssystems
Australia
New Zealand
United Kingdom

LessonLesson: Primary care is : Primary care is thethe foundation foundation of high performing delivery systemsof high performing delivery systems
• Societal investment in medical education can Societal investment in medical education can help achieve a well-trained workforce with the help achieve a well-trained workforce with the right proportion of primary care physicians and right proportion of primary care physicians and specialists and is large enough to assure accessspecialists and is large enough to assure access
• Investment in primary and preventive care can Investment in primary and preventive care can result in better health outcomes, reduce costs, result in better health outcomes, reduce costs, and help assure an adequate supply of primary and help assure an adequate supply of primary care physicians care physicians
• These efforts can be enhanced by assuring that These efforts can be enhanced by assuring that all residents have equitable access to a personal all residents have equitable access to a personal physician through a patient-centered medical physician through a patient-centered medical home modelhome model
France Germany
United Kingdom
Australia, Canada, Denmark
France NetherlandsNew Zealand Switzerland
UK
Denmark

LessonLesson: The best payment systems : The best payment systems recognize the value of care coordinated by recognize the value of care coordinated by
primary care physiciansprimary care physicians• Effective payment systems:Effective payment systems:
– Provide adequate payment for primary Provide adequate payment for primary care servicescare services
– Create incentives for quality Create incentives for quality improvement and reporting improvement and reporting
– Recognize geographic or local payment Recognize geographic or local payment differencesdifferences
– Provide incentives for care coordination Provide incentives for care coordination
Canada Denmark Germany
United Kingdom
Belgium
United Kingdom
Denmark Netherlands

Lesson: Lesson: High performing systems invest in High performing systems invest in HIT, have uniform billing, and lower HIT, have uniform billing, and lower
administrative costsadministrative costs• Adoption of a uniform billing and Adoption of a uniform billing and
electronic processing of claims improves electronic processing of claims improves efficiency and reduces administrative efficiency and reduces administrative expensesexpenses
• An inter-operable health information An inter-operable health information infrastructure can enable physicians to infrastructure can enable physicians to obtain instantaneous information at the obtain instantaneous information at the point of medical decision-making and point of medical decision-making and enhance electronic communications enhance electronic communications among treating health professionals among treating health professionals
Germany
Canada
Taiwan
United Kingdom and most others
Denmark
Taiwan
Netherlands

Interest in Entering Primary Care has been Interest in Entering Primary Care has been Declining Among Graduating SeniorsDeclining Among Graduating Seniors
(Percentages 1999-2006)(Percentages 1999-2006)
0
2
4
6
8
10
12
14
1999 2000 2001 2002 2003 2004 2005 2006
GIMIM SSFPPED
Source: Association of American Medical School Graduation Questionnaires http://www.aamc.org/data/gq/allschoolsreports/2006.pdf

Bodenheimer, T. et. al. Ann Intern Med 2007;146:301-306
The Primary Care—Specialty Income Gap

Patient-Centered, Physician-Guided Care
Adapted from:Defining Primary Care: An Interim Report, Institute of Medicine 1994
Physician Patient
Practice Family Team
Integrated CommunityDeliverySystemorVirtualTeam
Core of Team-Based Care
NP/PARN/LPNMedical AssistantCare CoordinatorOffice StaffNutritionist/EducatorPharmacistBehavioral HealthCase ManagerCommunity resourcesDM companiesOthers…
Immediate familyExtended familyFriendsNeighbors

What must it provide/Joint Principles
patient centered
personal physician
team approach
whole person
• preventive/acute/chronic/end of life
longitudinal care
coordinated care
high quality and continuous quality improvement
navigation of a complex system

PCMH/Payment
1) “Bundled Care” Coordination Fee
▪ Physician/non-physician work outside of face-to-face visits (e.g. email, telephone/group visits
-Promoting efficiency rather than volume-based care
▪ System infrastructure (e.g. HIT)
-Encourage coordination of care
▪ Risk adjusted
-Remove incentives to avoid complex or costly patients

PCMH/Payment
2) Visit based fee-for-service
• Incentive to physician to see patients in office when appropriate
3) Performance based component
• Recognize achievement of quality and efficiency

Potential New Payment Codes
Care plan oversight for specified condition
• Communicate with provider of treatment
• On-going review of patients’ medical status/labs
• Care plan modification
Physician e-mail/telephonic consultations
Training and follow up of patient self management by physician/nurse

Health Care Utilization & Primary Care
• For population of 775,000, an increase from 35% to 40% primary care physicians could:– Reduce inpatient admissions by ~2500/year
• At approximately $9000/admission = $23M
– Reduce ED utilization by 15,000 visits/year– Reduce surgery by about 2500 cases/year
*Kravet, S et al: Health Care Utilization and the Proportion of Primary Care Physicians.
Amer J of Medicine, 2008; 121:142-148.

Three Commonly Posed Questions:
1. Why does the ACP, with nearly equal numbers of general internists and subspecialty internists members, advocate for a system that appears more beneficial to primary care physicians?
2. How will my practice and my patients' experiences change?
3. Why should subspecialists support this model?

Why is the ACP Advocating for Stronger Primary Care and the PCMH Model:
• Extensively reviewed data from this country and abroad
• Data compellingly suggest: Better outcomes and reduced costs by expanding primary care

How Might the PCMH Benefit Primary Care Physicians:
• Narrowing the earnings disparities– payment for care coordination – performance-based component to recognize
quality and efficiency – visit-based fee-for-service payment to incentivize
physicians to see patients in the office
• More time to spend with chronically ill patients

How Might the PCMH Benefit Patients:
• Innovative scheduling systems to minimize delays in getting appointments,
• Non-urgent medical advice by e-mail and telephone,
• Same-day care with PCMH-based non-physicians for less complex patient issues,
• Group teaching of patients with chronic diseases.

How Might the PCMH Benefit Patients:
• Time for coordinating care with family and other clinicians
• Evidenced-based point-of-care support tools, and
• Better health information technology (HIT) to efficiently coordinate all sources of the patient's care within the community and track quality and patient satisfaction measures to promote continuous improvement.

How Might the PCMH Benefit Subspecialists?
• May head a medical home
• New billing codes
• Fewer hassles
• Better referrals
• Improved quality of practice
• Efficient spending