0010 Pri
-
Upload
prashantkaushal2 -
Category
Documents
-
view
37 -
download
4
Transcript of 0010 Pri

Recent Patents on Anti-Infective Drug Discovery, 2012, 7, 73-89 73
2212-4071/12 $100.00+.00 © 2012 Bentham Science Publishers
Bacterial Efflux Pumps Involved in Multidrug Resistance and their Inhibi-
tors: Rejuvinating the Antimicrobial Chemotherapy
Ashima K. Bhardwaj* and Priyabrata Mohanty
Department of Human Health and Diseases, Indian Institute of Advanced Research, Koba Institutional Area, Gandhina-
gar 382 007, Gujarat, India
Received: January 23, 2012; Accepted: February 8, 2012; Revised: February 13, 2012
Abstract: Active efflux of antibiotics is one of the major mechanisms of drug resistance in bacteria. The efflux process is
mediated by membrane transporters with a large variety of unrelated compounds as their substrates. Though these pumps
are responsible for the low intrinsic resistance of a bacterium to a drug, their overexpression, accumulation of mutations in
these proteins and their synergy with other drug resistance mechanisms hampers effective antimicrobial treatment. As ef-
flux pumps have been reported to play vital roles in mediating multidrug resistance in clinical isolates from varied geo-
graphic locations and varied populations, the inhibition of efflux pumps appears to be an attractive approach to combat
the problem of drug resistance. Efflux pump inhibitors can be utilized for increasing the antibiotic concentration inside a
pathogenic cell making these drugs more effective, reduce the accumulation of other resistance mechanisms in a cell and
for diagnostic purposes to evaluate the presence and contribution of the efflux mechanism in a pathogen. A large number
of inhibitors have been discovered and patented in last two decades but the process of discovery, testing and commerciali-
zation is rather slow. Some of the important inhibitors include the energy decouplers, phenothiazines, analogs of popular
antibiotics, inhibitors of serotonin re-uptake, to name a few, that have been used as adjuvants in the antimicrobial chemo-
therapy to potentiate the activity of some important antimicrobials in deadly pathogens that have worried the mankind
since long. This review describes the role of efflux pumps in governing the resistance phenotype of a pathogen, efflux
pumps found in bacteria and the efflux pump inhibitors that have been studied and patented so far.
Keywords: Antibiotic analogs, efflux pumps, efflux pump inhibitors, energy decouplers, multidrug resistance, patents, pepti-domimetics, Pseudomonas aeruginosa, Staphylococcus aureus.
INTRODUCTION
Efflux pumps or multidrug resistance (MDR) pumps have been recognized as one of the major determinants of the concentration of an antibiotic inside a bacterial cell. Therefore, inhibition of the activity of these pumps with ef-flux pump inhibitors (EPIs) appears to be a promising ap-proach for restoring the activity of the drugs that are sub-strates for these efflux pumps. Since the field for develop-ment, testing and commercialization of various EPIs is still in its infancy, one must consider the factors that affect the efflux-mediated resistance in order to characterize the fully effective inhibitors. Three main factors that should be con-sidered for the development of EPIs are: the type of patho-genic bacteria to be targeted, the type of pump to be targeted for inhibition and lastly, the type of antibiotic that would be rendered effective clinically during the process. As one EPI could be used to target multiple efflux pumps, these EPIs could be used not only as adjuvants in antibiotic treatments but also as diagnostic tools for detection of antibiotic resis-tance by the process of drug efflux by these pumps [1, 2]. In addition to this, as the efflux pumps have been shown to be crucial for bacterial survival, virulence and pathogenicity, inhibition of these pumps is also expected to affect the bacte-rial pathogenicity in vivo [3, 4].
*Address correspondence to this author at the Department of Human Health
and Diseases, Indian Institute of Advanced Research, Koba Institutional Area, Gandhinagar 382 007, Gujarat, India; Tel: + 91 -079- 30514235;
Fax: + 91 -079-30514110; E mail: [email protected]
ANTIBIOTIC RESISTANCE AND ITS MECHANISMS
Antibiotic resistance is a phenomenon where the antibiot-ics used to treat a particular pathogen become useless as the bacterial cell evolves mechanisms to render these drugs inef-fective. With rise in the reports of pan- resistant Pseudo-monas aeruginosa, appearance of extensively drug resistant (XDR) strains of deadly pathogens that cause tuberculosis [5] and all other multiple drug resistant gram-positive and gram-negative pathogens, it is often speculated that we are at the end of the antibiotic era [6, 7]. In order to overcome this grave problem of multiple drug resistance that has wreaked havoc in clinical settings, it becomes imperative to under-stand the mechanisms of action of antibiotics and mecha-nisms of development of resistance against these wonderful drugs. Growing awareness and vigilance is an utmost re-quirement in order to maintain a stride ahead of these micro-bial pathogens that can only be treated by antibiotics. There are various ways in which a bacterium can develop resis-tance to an antibiotic [7]. These are: restricted access of anti-biotics to its target inside the bacterium, inactivation of the antibiotic, modification of the antibiotic target making it refractory to the antibiotic action and failure to activate the antibiotic. Restricted access could be achieved with the means of either porins that will reduce the antibiotic uptake or it could be achieved with the help of efflux pumps that would accelerate the loss of antibiotics thus making them ineffective [7].

74 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
EFFLUX PUMPS AND ANTIBIOTIC RESISTANCE
Efflux pumps operate by limiting the intracellular con-centration of antibiotics and have been described in both gram-positive as well as gram-negative bacteria. Since the first report of involvement of efflux pumps in determining the resistance towards tetracycline in1980s, there have been numerous reports describing the role of efflux pumps in ex-truding each class of antibiotics [3, 4, 8, 9]. Efflux pumps are present in bacteria for defense as they help in the extrusion of toxic substances outside the cell. The physiological roles of efflux pumps in the bacteria include bile tolerance of en-teric bacteria leading to colonization, invasion and survival in the host [3, 4, 10, 11]. It is very natural that efflux pumps predate the antibiotic era and play important roles in bacte-rial physiology, metabolism and pathogenicity as described above [3, 4, 10, 11]. Their importance for a cell is supported by the finding that the size of the genomes is directly propor-tional to the number of pump genes harboured by them [3, 4, 12]. Extrusion of antibiotics appears just a part of their func-tion in removing noxious chemicals from the bacteria. It is not difficult to envisage that antibiotics would also be the natural substrates of efflux pumps as these pumps would export the antibiotics outside the cell in the antibiotic-producing bacteria. While some efflux pumps like TetA and CmlA selectively extrude specific antibiotics like tetracy-cline and chloramphenicol, other efflux pumps like MexAB-OprM, NorA and BmrA are capable of expelling large num-ber of structurally unrelated compounds that have different modes of antibacterial action and therefore are called multidrug resistance (MDR) pumps capable of extruding antibiotics, disinfectants, dyes and detergents [3]. Most of these pumps are chromosome-borne and provide intrinsic resistance to bacteria. Some of these efflux pumps could also be located on mobile genetic elements like plasmids, trans-posons and integrons thus providing a means of transferable resistance [13]. For example, the transposon-encoded mac-rolide-specific pumps MefA and MefE have been reported [14, 15] and plasmids are known to carry efflux pump genes like tet, qepA, OqxAB and qac [13, 16, 17]. Given their physiological significance, though the efflux mechanisms would be operative in the pathogenic as well as non-pathogenic organisms, antibiotic-resistant as well as antibi-otic-susceptible organisms, it becomes relevant to under-stand their role in pathogenic organisms with an aim to com-bat the problem of multidrug resistance. Gram-negative bac-teria are more likely to become drug resistant due to their multilayered cell envelope which restricts the access of many drugs inside the cytoplasm; the drugs being expelled out either at the level of outer membrane, or through the perip-lasmic space or if it gains access to the interiors of the cell, through the tripartite efflux pumps that traverse the three envelope layers [3].
On experiencing the antibiotic pressure, there are two mechanisms by which efflux pumps would prepare to expel them. Either there is an overexpression of these efflux pumps to handle the increasing concentration of antibiotics inside the cell, or the pumps accumulate mutations for expelling the drug efficiently [3]. Some of the efflux pump genes require induction or mutations in the regulatory genes for their ex-
pression, while other efflux pump genes are expressed con-stitutively. This constitutive expression leads to a basal ef-flux activity in a cell contributing to intrinsic antibiotic resis-tance. Though efflux pumps are thought to confer low levels of protection against antibiotics due to intrinsic resistance, they work in synergy with many other mechanisms of resis-tance like mutations in topoisomerases, beta lactamases or presence of Quinolone-resistance (QNR) proteins to increase the level of resistance to a clinically significant end point. Overexpression of efflux pumps or simultaneous expression of many efflux pumps could also help to achieve the same effect clinically [18-21]. Though factors like extracellular polysaccharide matrix, higher bacterial cell density and slower bacterial growth all work together for antimicrobial resistance in biofilms, efflux pumps have also been impli-cated in increasing antibiotic resistance in biofilms [6].
TYPES OF EFFLUX PUMPS, THEIR STRUCTURE
AND REGULATION
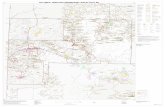
Resistance mediated through efflux pumps appears to be a very basic and general mechanism as compared to other mechanisms involving a particular class of antibiotics or a specific target. One efflux pump can recognize a variety of antimicrobials and one antimicrobial can be recognized by many different types of efflux pumps. For example, MATE family of transporters recognize various structurally unre-lated molecules like fluoroquinolones, aminoglycosides and a large number of cationic compounds. Also, tetracycline may be recognized by various pumps. The bacterial efflux pumps are generally divided into five classes: Small multidrug resistance (SMR) pumps of the drug/metabolite transporters (DMT) superfamily, ATP-binding cassette (ABC) transporters, Major facilitator superfamily (MFS), Resistance nodulation division (RND) superfamily and Multidrug and toxic compound extrusion (MATE) transport-ers of the multidrug/oligosaccharidyl-lipid/polysaccharide flippases (MOP) superfamily [3]. All these pumps, their sub-strate specificity and their energy sources have been depicted in Fig. (1) and important pumps from various bacteria have been described in Table 1. While RND, SMR and MFS util-ize the energy derived from proton gradients for the transport activity, MATE transporters utilize the energy from H
+ or
Na+ gradient and ABC pumps are driven by ATP hydrolysis
[3, 22-24]. Though ABC pumps have been implicated in drug resistance in eukaryotic cells, their role in prokaryotic drug resistance is not well characterised. P-glycoprotein 1 (P-gp, MDR1) is one of the well studied ABC transporter implicated in conferring resistance towards the compounds used for chemotherapy [25]. LmrA ABC efflux pump from Lactococcus lactis has been shown to confer MDR pheno-type [26]. Out of all the known transporters, MFS and RND pumps are the most common. NorA of Staphylococcos aureus, PmrA of Streptococcus pneumoniae and EmeA of Enterococcus faecalis are some of the well studied MFS pumps [27-29]. RND pumps have tripartite organization with three components: an outer membrane protein, a periplasmic channel protein and an inner membrane transporter protein [3]. The most well studied example for this kind of pump is the Mex system in P. aeruginosa and Acr system in Entero-bacteriaceae. Typically, the genes encoding these systems

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 75
Fig. (1). Efflux pumps found in prokaryotes. The five multidrug transporters have been depicted with their substrates and mechanisms of
transport. MATE: Multidrug And Toxic compound Extrusion; MFS: Major Facilitator Superfamily; SMR: Small multidrug resistance; RND:
Resistance nodulation division and ABC: ATP-Binding Cassette transporters.
Table 1. Kinds of efflux pumps found in prokaryotes.
S. No. Organism Pump Type of Pump Resistance Conferred Reference
Bacillus subtilis BmrA MFS
Fluoroquinolones, chloramphenicol, antiseptics, dyes,
disinfectants
[33]
NorA MFS Fluoroquinolones, chloramphenicol [34]
NorB MFS Fluoroquinolones, tetracycline, dyes, disinfectants [35]
Tet38 MFS Tetracycline [35]
MepA MATE Fluoroquinolones, biocides [36]
MsrA MFS Macrolides [37]
S. aureus
MdeA MFS Macrolides [38]
PmrA ABC Fluoroquinolones, EtBr, acriflavine [28]
MsrD ABC Macrolide, ketolide [39]
MefA MFS Macrolide [40]
MefE MFS Macrolide [40]
S. pneumoniae
Tet K-L MFS Tetracycline [13]
MexAB-OprM RND Tetracycline, chloramphenicol, fluoroquinolones,
glycylcyclines
[41] P. aeruginosa
PmpM MATE Fluoroquinolones [42]
Gram-negative Bacteria Tet A, Tet B, Tet
C
MFS Tetracycline [13, 43]

76 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
(Table 1) Contd....
S. No. Organism Pump Type of Pump Resistance Conferred Reference
Salmonella enterica serovar
typhimurium
AcrAB-TolC RND Tetracycline, nalidixic acid, chloramphenicol [44, 45]
Campylobacter jejuni CmeB RND Tetracycline, chloramphenicol, ciprofloxacin, am-
picillin
[46]
N. gonorrhoeae MtrCDE RND Tetracycline, macrolides, penicillins [47]
Bacteroides fragilis BmeB RND Fluoroquinolones, -lactams [48]
Bacteroides thetaiotaomicron BexA MATE Fluoroquinolones, chloramphenicol,
Ethidium bromide
[49]
HmrM MATE Fluoroquinolones [50]
TetB,K MFS Tetracycline [1]
H. influenzae
AcrAB-TolC RND Macrolide, trimethoprim [51]
MacAB-TolC ABC Macrolide [52]
YdhE MATE Fluoroquinolones, trimethoprim, chloramphenicol [30]
Bcr MFS Tetracycline, sulphamide [1]
Dep MFS Tetracycline [1]
ErmAB-TolC MFS Fluoroquinolones, tetracycline [1]
Fsr MFS Trimethoprim [1]
MdfA MFS Aminoglycoside, fluoroquinolones, macrolides, tetra-
cycline chloramphenicol
[24]
SetA MFS Aminoglycoside [1]
Tet A-E MFS Tetracycline [1]
Ycel MFS Fluoroquinolones [1]
YidY MFS Chloramphenicol [1]
YebQ MFS Trimethoprim [1]
AcrAB-TolC RND -Lactams, fluoroquinolones, macrolide, tetracycline,
trimethoprim, sulphamide
[53]
AcrAD-TolC RND Aminoglycoside [3]
AcrEF-TolC RND -Lactams, Fluoroquinolones, macrolides, tetracy-
cline, trimethoprim
[3]
YegN RND Fluoroquinolones [1]
E. coli
ErmE SMR Macrolides, tetracycline [1]
CmlB MFS Chloramphenicol [54]
AcrAB-TolC RND Fluoroquinolones, macrolide, tetracycline, chloram-
phenicol, licosamides
[53]
Enterobacter aerogenes
EefABC RND Fluoroquinolones, macrolides, tetracycline, chloram-
phenicol
[1]
VcrM MATE Fluoroquinolones, aminoglycosides,
ethidium bromide
[31] V. cholerae/
V. parahemolyticus
VcmA MATE Fluoroquinolones, aminoglycosides ethidium bro-
mide
[31]

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 77
(Table 1) Contd....
S. No. Organism Pump Type of Pump Resistance Conferred Reference
VcmB MATE Fluoroquinolones, aminoglycosides,
ethidium bromide
[31]
VcmD MATE Fluoroquinolones, aminoglycosides,
ethidium bromide
[31]
VcmH MATE Fluoroquinolones, aminoglycosides,
ethidium bromide
[31]
VcmN MATE Fluoroquinolones, aminoglycosides, ethidium bro-
mide
[31]
VmrA MATE Ethidium bromide [55]
NorM MATE Fluoroquinolones, aminoglycosides, ethidium bro-
mide, acriflavine
[30, 56]
VcaM ABC Tetracycline, fluoroquinolones [57]
VceCAB MFS Chloramphenicol, nalidixic acid [58]
Vex AB and
Vex CD
RND Detergents, novobiocin, aminoglycosides [59]
are organized as well regulated operons. The outer mem-brane proteins (OMPs) like TolC or OprM may or may not be co-located with other genes in the operons. ABC trans-porters have six transmembrane-spanning regions, MATE and RND have twelve and SMR has four such regions. While MFS are found both in gram-positive as well as gram-negative bacteria and are narrow-spectrum transporters, RND are exclusively found in the gram-negative bacteria due to their membrane architecture and are broad-spectrum transporters. MATE family pumps were first described from Vibrio parahaemolyticus [30]. Now these pumps have been described in many other bacteria and include VcrM, VcmA, VcmD from V. cholerae, HmrM from Haemophilus influen-zae, PmpM from P. aeruginosa [3, 31].
The complex regulatory operons/mechanisms control the expression of proteins that are responsible for the influx and efflux of the drugs thus maintaining the intracellular concen-tration of these compounds. MarA regulator controls the expression of porins and efflux pumps and the expression of this regulator is in turn controlled by some antibiotics. For example, imipenem that is not a substrate of an efflux pump in Enterobacter aerogenes results in expression of gene en-coding marA regulator and alters the permeability of the membrane for some other antibiotics thus leading to the in-creased resistance towards chloramphenicol, quinolones and tetarcyclines [32]. Therefore, even though marRA doesnot encode a multidrug efflux system/porin, the marRAB locus confers resistance to compounds like tetracycline, chloram-phenicol, fluoroquinolones, nalidixic acid and rifampin be-cause it controls the expression of other loci important in mediating drug resistance e.g. the porin OmpF and acrAB gene for AcrAB efflux pump [24]. Hence, the mar locus has been implicated in producing multiple antibiotic resistance (MAR) phenotype in E.coli by acquiring mutation. While the marR gene encodes a repressor for this operon and accumu-
lates mutations, the marA gene product is known to activate a plethora of genes related to antibiotic resistance and oxida-tive stress.
WELL STUDIED EFFLUX PUMPS
NorA of S. aureus, BmrA of B. subtilis, PmrA of P. aeruginosa, MexAB-OprM, MexCD-OprJ, MexEF-OprN, MexXY-OprM of P. aeruginosa, AcrAB-TolC of E. coli, AdeABC of Acinetobacter baumannii are some of the well studied pumps. Some of these pumps and their characteris-tics have been detailed in Table 1. The crystal structures have been solved for the RND pumps like AcrB and TolC in E. coli and MexA, MexB and OprM in P. aeruginosa [60-64]. The X-ray structure of NorM from V. cholerae has re-cently been solved to the resolution of 3.63 Å [65].
EFFLUX PUMP INHIBITORS (EPIs)
Deletion of an efflux pump from a bacterium has been shown to increase the susceptibility of this bacteria to many antibiotics. For example, disruption of the gene coding for MexB in P. aeruginosa led to a decrease in MIC for a wide range of drugs like aminoglycosides, chloramphenicol etc. These P. aeruginosa mutants have been used for screening of EPIs [66]. There is ample data which shows that efflux pumps are involved in determining the resistance phenotype of a pathogen and therefore pose a major threat for the effec-tive treatment of many gram-positive, gram-negative and opportunistic pathogens. This necessitates the development of inhibitors for these pumps that would circumvent the transporters to produce successful treatment regimens. In the next few sections of this review, various strategies to inhibit efflux pumps, various compounds that have been used as inhibitors and some recent patents describing these EPIs have been discussed. Some of the sections deal with the de-

78 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
scription of various advantages and disadvantages of using EPIs and about the alternatives to these compounds.
REQUISITES OF AN IDEAL INHIBITOR
Since a specific and truly effective EPI is required for potentiating the activity of antimicrobials thus circumventing the bacterial multidrug resistance, efforts should be directed towards the search for a compound which satisfies one or more of the following criteria:
1. The EPI should be free of any pharmacological activity on eukaryotic cells as this makes these EPIs unviable for use on eukaryotic cells. Some inhibitors like MC-207, 110, are not recognized by eukaryotic transporters which enhances their specificity and reduces the side effects arising due to inhibition of eukaryotic efflux pumps and their physiological functions [1].
2. Synthesis of biological inhibitors from natural products should not be time-consuming, expensive and difficult as these factors would make the products commercially unviable. For example, problems with isolation, purifi-cation, stability, solubility and potential toxicity of plant products like berberine have seriously hampered their development as EPIs.
3. The inhibitors should be proteolytically stable to ensure enhanced serum levels and cellular accumulation that potentiates their activity in intracellular infections.
4. They should have enhanced therapeutic index and pharmacokinetic profile to ensure maximum specificity and efficacy.
5. They should be devoid of antibacterial activity as this could lead to development of resistance mechanisms against these EPIs. Chemotypes of clinically used anti-biotics like aminoglycosides, tetracyclines and qui-nolones have been used as inhibitors with low intrinsic antibacterial effects [1].
6. EPIs should not be toxic for human use since they are used at high concentrations. As described later, some EPIs like reserpine are neurotoxic at the concentrations used to combat bacterial infections. Some of the EPIs are toxic due to their serotonin-agonist properties [1-3].
STRATEGIES FOR INHIBITION OF EFFLUX PUMPS
There could be many strategies for achieving the inhibi-tion of efflux pumps. These are:
1. Designing new antibiotics or changing the design of the existing antibiotics so that they are no longer recognized by the efflux pumps. This can help bypass the use of ef-flux pumps and hence inhibit the efflux pump. Examples include glycylcyclines and ketolides which have lower affinity for the specific efflux pumps. Tigecycline by-passes MFS pumps specific for tetracycline [67] and te-lithromycin bypasses MefA/E and AcrAB systems [53]. Among fluoroquinolones, levofloxacin, moxifloxacin and gatifloxacin are not affected by efflux pumps NorA and PmrA [68].
2. Interference with the assembly/functioning of efflux pumps. This is especially valid for the tripartite efflux
pump proteins like RND pumps found in gram-negative bacteria [69]. In case of these efflux pumps, blocking the outer membrane channel can also lead to the inhibi-tion of efflux pump activity [70].
3. Blocking the energy required by the efflux pumps to operate. Energy decouplers can be used as a general mechanism to dissipate the energy gradients driving the efflux pumps [1, 71]. These have been discussed in de-tail in next sections.
4. Interfering with the regulatory steps in the expression of the efflux pump genes so that the expression of the ef-flux pumps declines. As already discussed before, the membrane permeability of a bacterial cell is often under complex regulatory mechanisms that control the expres-sion of the porins and the efflux pumps simultaneously to achieve certain standards of permeability. These regu-lators termed as Mar regulators can be targeted to con-trol the efflux pump expression. For example, Mar A regulator that controls the membrane permeability in E. aerogenes regulates the expression of both the porins as well as AcrAB-TolC efflux pump, and can be affected by imipenem. Though this antibiotic is not a substrate for this efflux pump, in the presence of this drug, the bacterium becomes resistant to quinolones, tetracycline and chloramphenicol thus leading to cross resistance [32]. Mutations in Mar regulator often cause resistance to many classes of antibiotics [72]. Interference with these regulatory steps therefore could be used to de-crease the expression of efflux pumps thus restoring the antibiotic activity.
5. Competitive/non-competitive inhibition of efflux pumps. These inhibitors are beneficial in many ways clinically as they not only circumvent the problem of bacterial resistance to antibiotics by inhibiting efflux pumps, they also reverse the acquired resistance associ-ated with the overexpression of efflux pumps and sup-press the emergence of mutations leading to resistance [71, 73-76]. Example of competitive inhibitor is MC-207, 110, described later in the review in detail.
6. Blocking the efflux pump protein or gene. This falls under the category of biological inhibition of efflux pumps. The efflux pumps could be deactivated with the means of specific antibodies [70]. Alternatively, the genes encoding these pumps or their regulators could be blocked using the antisense strategies. The antisense ap-proach has been shown to work for AcrAB efflux pump in E. coli and has also been patented [77, 78].
TYPES OF EPIs
Efforts have been directed at identification of EPIs from natural sources, screening of libraries of chemical com-pounds and secondary evaluation of current therapeutics [1, 2]. Plants have evolved to produce both the antimicrobial compounds as well as their inhibitors [79-82]. There are dif-ferent kinds of inhibitors that work on various strategies de-scribed in the section above. It may be pertinent to state here that some of the inhibitors may fall under more than one category. Some of the important EPIs have been described in

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 79
Table 2 in context of the patents describing them. The differ-ent categories of EPIs are:
1. Energy decouplers: As most of the efflux pumps utilize the Proton Motive Force (PMF) as their energy source, any compound that dissipates this PMF will act as an inhibitor of the efflux pump [71, 83]. Examples include Carbonyl Cyanide m-ChloroPhenyl-hydrazone (CCCP), valinomycin and dinitrophenol (DNP). However, these compounds do not directly bind the efflux pumps to cause their inhibition. They dissipate the PMF by modi-fying the trans-membrane electrochemical potential. This class of molecules have not been used clinically or patented due to cytotoxicity issues [76].
2. Direct binding and inhibition of efflux pumps: These kind of EPIs can be further subdivided into many groups that are described below.
2a. Drugs used for therapeutic purposes other than in-fectious diseases: Reserpine, a plant alkaloid is known to bind directly to the efflux pump protein to effect its inhibition. It has been shown to directly interact with B. subtilis Bmr protein recognizing the amino acids phenylalanine 143, valine 286 and phenylalanine 306 [84]. This compound as well as verapamil have been shown to reverse the MDR phenomenon in B. subtilis and mammalian cells where it inhibits PgP pump [85]. Both reserpine and verapamil are used as antihypertensive drugs as they inhibit vesicular monoamine transporters and calcium channel antagonists respectively. Both the drugs are also used to detect the activity of efflux pumps in gram-positive bacteria [86]. In bacterial cells, reserpine inhibits NorA pump of S. aureus [87] and hence potentiates the activity of norflox-acin in this organism [34]. Verapamil inhibits MDR pumps of parasites and potentiates the activity of tobramycin [76, 86]. Verapamil also inhibits ABC pumps like LmrA from bacteria. Berberine and palmatine are the plant-derived antimicrobials with activity against S. aureus. These were identified on screening the S. aureus strain where NorA was dis-rupted [88, 89]. Plant extracts contain 5’-MHC (5’-methoxyhydnocarpin), an inhibitor of NorA, that potentiates the activity of berberine [80]. All these EPIs suffer from the problem of neurotoxicity at the concentrations used for combating bacterial infec-tions [76, 86, 90]. Omeprazole, an antiulcer agent, which acts by inhibiting proton pumps, also inhibits NorA of gram-positive bacteria but requires high dosages for inhibiting bacterial growth. 11 pyr-rolo[1,2-a] quinaxoline derivatives structurally analogous to omeprazole have also been shown to inhibit MDR S. aureus overexpressing NorA pump and restores the activity of norfloxacin [91]. Simi-larly, tricyclic neuroleptics like phenothiazines, used for treatment of mental disorders, have been shown to inhibit efflux pumps like BpeAB-OprB and AmrAB-OprA and potentiate the activities of aminoglycosides and macrolides in Burkholderia pseudomallei [92]. Promethazine, a phenothiazine, has been used in combination with penicillin G to
inhibit RND pumps in E. coli [93], inhibit ABC pumps in yeast [94], potentiate the activities of an-timicrobials in Mycobacterium tuberculosis [95] and reverse chloroquine resistance in Plasmodium falciparum [96]. Phenothiazines have also been shown to reverse MDR phenotypes of pathogenic bacteria like P. aeruginosa or S. typhimurium [97, 98]. They probably inhibit the PMF-driven pumps. The concentration of phenothiazines required to control bacterial infection are not clinically achiev-able and hence these compounds are not widely used [76].
Other therapeutic reagents used for treatment of condi-tions other than infectious diseases but can be used as EPIs are:
2a.1. Selective serotonin reuptake inhibitors: Paroxetine have shown activity against gram-positive bacteria. These com-pounds inhibit NorA and MepA of S. aureus and AcrAB-TolC pump of E. coli [99-101].
2a.2. Arylpiperazines and arylpiperidines: Arylpiperazines reverse MDR in bacteria overexpressing AcrAB and AcrEF pumps. NMP (1-naphthylmethyl-piperazine) is the most potent inhibitor that increases the intracellular concentra-tion of drugs like linezolid, chloram-phenicol, tertracycline, macrolides and fluoroquinolones but are likely to be toxic due to their serotonin agonist prop-erties [102]. Elongation of the spacer be-tween the benzene ring and the piperazine ring as well as the halogenic substitutions at the benzene ring have been shown to enhance the activity of these EPIs. Dihalogens among arylpiperidines have been shown to re-store the activity of linezolid in E. coli [103].
2b. Peptidomimetics: Dipeptide amide compounds INF271 and MC-207,110 (Phenylalanine Arginyl -Naphthylamide/PA N) fall under this category. As reserpine cannot be used with antibiotics for treat-ment of staphylococcal infections due to neurotox-icity problems [104], 9, 600 structurally diverse synthetic molecules were screened for enhancing the activity of ethidium bromide and ciprofloxacin using the strains of S. aureus, one of which overex-pressed NorA [105, 106]. For this screening, the compounds were used at lower concentrations than reserpine. The inhibitors belonged to four chemo-types: indoles, biphenyl ureas, aromatic amides and molecules bearing a trichloromethylaminal group [105-107]. Some putative inhibitors including INF55 (indole), INF271(urea) and INF240 (aro-matic amide), were obtained. Thus, the inhibitors had broad structural diversity and showed inhibitory activity for homologous transporters like BmrA from B. subtilis and PmrA of S. pneumoniae [106].

80 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
Similarly, a library of 200,000 synthetic compounds and natural products was screened with the aim of potentiating the activity of levofloxacin against P. aeruginosa [66, 89, 108-112]. MC-207,110 was identified as an inhibitor of Mex pumps. The crystal structure of E. coli AcrB has been solved in the presence of this drug and its binding to the pump has been proved [113]. This compound has been shown to decrease the frequency of the emergence of highly levofloxacin resistant P. aeruginosa strains and reduced the intrinsic resistance of the bug to levofloxacin 8-folds [66, 108, 109]. MC-207,110 is a competitive inhibitor of the efflux pumps and acts by binding to the same pocket or at a site closer to the antibiotic substrate binding site [71, 76]. The compound has not only restored the activity of levofloxacin but has also been found to potentiate the activity of other antibiotics like oxa-zolidinones, chloramphenicol, rifampicin, mac-roliodes/ketolides [2, 114]. Also, it has been shown to be effective not only for P. aeruginosa, but also for K. pneumoniae, C. jejuni, E. coli, S. typhimurium and E. aerogenes [83, 108, 115-117]. To summarise, PA N appears to be a promis-ing inhibitor with a broad host as well as antibiotic range and an effective mode of efflux pump inhibi-tion. The derivatives of PA N have been produced by substitution of amino acid or use of D-amino ac-ids [108, 118-120]. As their toxicity has limited their clinical applications, to circumvent this prob-lem, MC-04, 124 compound has been designed with lesser toxicity and higher stability [121].
2c. Quinolines: This class of compounds have been shown to restore the activity of various antibiotic classes like quinolones, cyclines and chlorampheni-col. These are now used as broad spectrum inhibi-tors for resistant E. aerogenes and K. pneumoniae to make them susceptible for the above mentioned class of antimicrobials [122]. The alkyl side chain linked to the heterocyclic moiety on alkylaminoqui-nolines and the connecting heteroatom and the posi-tion of substituted groups on ring have been shown to be important for the inhibitor activity [76]. These compounds need to be studied in more details in terms of their toxicity and pharmacodynamic pro-files.
3. Chemical modifications of substrates of efflux
pumps: Ofloxacin was modified by conjugating its core with bisaryl urea-based NorA inhibitor and this com-pound was found to inhibit NorA and MepA pumps in S. aureus [101].
4. Iron chelators: These compounds inhibit the pumps by chelating iron required for the pump activity. Nocar-damine has been shown to inhibit TetB and TetK pumps in S. aureus [123].
5. Inhibitors of eukaryotic efflux pumps: This class of molecules called piperidine-carboxylic acid derivatives were used and patented as inhibitors of mammalian P-glycoprotein and MRP-1and used as adjuvants in cancer treatment [124-127]. The advantage with these mole-
cules was their already established pharmacokinetic and toxicity profiles which facilitated their use as adjuvants in antibiotic treatments. Phenols epicatechin-gallate and epigallocatechingallate reverse tetracycline resistance in S. aureus overexpressing TetB or TetK [128]. They also enhance the norfloxacin activity against NorA overex-pressing strains [129]. GG918, biricodar (VX-710), tim-codar (VX-853) potentiate the activity of fluoroqui-nolones against E. coli or gram-positive bacteria like S. aureus, S. pneumoniae [129, 130].
6. Antibiotic analogs: The compounds in this category help in circumventing the efflux pumps thus increasing the susceptibility towards this antibiotic class. Analogs of tetracyclines, quinolones and aminoglycosides have been studied and patented so far. Tetracycline analogs have been designed to increase the susceptibility of S. aureus against tetracyclines [131-135]. Such com-pounds have now been tested with several pathogens and several antibiotics [132-134]. Since these com-pounds are structurally similar to the antibiotic, they suf-fer from the disadvantage of having antimicrobial activ-ity and hence selection of other resistance mechanisms against the same antibiotic. The analogs of aminoglyco-side paromomycin have been used as inhibitors of the efflux pumps using the bacterium H. influenzae [136]. These compounds have been shown to increase the sus-ceptibility of wild-type and clinical strains to gentamicin and tetracyclines. The fluoroquinolone analogs have been shown to be effective in increasing the potency of this class of antibiotics in both gram-positive as well as gram-negative bacteria overexpressing some of the ef-flux pumps. Some of these analogs have been able to re-store the activity of macrolides in Streptococci overex-pressing Mef pumps [137].
7. Antisense oligos/antibodies: This approach is based on the utilization of antisense oligonucleotides to inhibit the expression of target efflux pumps. AcrAB efflux pump was inhibited using this approach in E. coli and this strategy has been patented [77, 78]. A recent report has described the use of antisense phosphorothioate oli-gonucleotide encapsulated in a novel anion liposome to restore the activity of fluoroquinolones in E. coli [138]. This strategy could be utilized for a wide variety of pumps with known gene sequences. The strategy to use antibody or parts thereof has been patented for inhibition of MexAB-OprM pumps in P. aeruginosa [70].
IMPORTANT PATENTS DESCRIBING EPIS
Though most of the patents for EPIs have been summa-rized in Table 2 and some reviewed earlier [1, 2], the details regarding the strategy, the target pathogen and the target efflux pump have been presented in this section for some of the important patents.
Markham et al. 2002 [106]: This patent reported the enhancement of the antibacterial action of fluoroquinolone and antifungal action of azole in combination with an EPI. An array of powerful broad spectrum inhibitor compositions comprising indole, urea, quinoline or aromatic amide was described. These formulations were shown to be effective

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 81
Table 2. Details of the efflux pump inhibitors and the patents where these inhibitors are described.
Type of Inhibitor Structure of the Compound Substrate Reference
Substituted polyamines
Aminoglycosides
Polyamines
[142, 143]
Paratek Pharmaceuti-
cals, Inc.
Peptidomimetic
Quinolone Tetracycline
-lactam
Coumermycin
Chloranphenicol
Aminoglycoside
Macrolide
Rifamycin
Oxazolidonone
[144, 145]
Essential Therapeutics,
Inc.
Substituted Analogs
Fluoroquinolones rifampin
[78]
Trustees of Tufts Col-
lege
Substituted Analogs
Fluoroquinolones rifampin [106]
Influx, Inc.
Substituted Analogs
Quinolone tetracycline
-Lactam
Coumermycin
Chloramphenicol glycopeptide
Aminoglycoside
Macrolide
Rifamycin
Oxazolidonone
[112]
Microcide Pharmaceu-
ticals, Inc.

82 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
(Table 2) Contd....
Type of Inhibitor Structure of the Compound Substrate Reference
Efflux Pump inhibitor
All classes [146]
Daiichi Pharmaceuticals,
Co. Ltd,
Trine Pharmaceuticals, Inc.
Tetracyclines ana-
logues
Tetracycline [135]
President and Fellows of
Harvard College
Glycylcycline
Tigecycline [141]
Mpex Pharmaceuticals,
Inc.
Efflux Pump inhibitor
Quinolones
[139, 140]
Mpex Pharmaceuticals,
Inc.
Rempex Pharmaceuticals,
Inc.

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 83
(Table 2) Contd....
Type of Inhibitor Structure of the Compound Substrate Reference
Amino Acid Modifica-
tion
All classes [70]
Tokai University
particularly for gram-positive bacteria like Staphylococci, Streptococci and Enterococci when used in combination with ciprofloxacin which is less active against gram-positive pathogens. The inhibitors were shown to target efflux pumps like BmrA and NorA. The screening assays used by the in-ventors were quite simple to set up and perform. After ob-taining a suitable bacterial (standard) cell with an active ef-flux pump (NorA), an inhibitor (urea/indole/amide) was ad-ministered in the presence of transportable substance (ethid-ium bromide/fluoroquinolone). Inhibition of the transporter was measured by monitoring the growth. Potential inhibitors of transport were identified as those compounds that in-creased the bactericidal effect of ethidium bromide/ fluoro-quinolone.
Oethinger and Levy, 2011 [78]: AcrAB-like efflux pumps have been targeted in highly resistant microbes using antisense oligonucleotides or their modified forms. These antisense oligonucleotides hybridise with nucleic acids en-coding efflux pump AcrB or with nucleic acids regulating the expression of an efflux pump (marA, rob or soxS). Other EPIs included ribozymes directed against the above men-tioned genes or antibodies to the efflux pump or proteins that regulate the expression of this efflux pump. Methods of treating infection, screening inhibitors for these pumps and of enhancing antimicrobial activity of fluoroquinolones, ri-fampin or non-antibiotic agents like ticlosan is provided.
Bostian et al. 2011 [139, 140]: The patent described the use of pentamidine compositions as EPIs administered along with antimicrobials to treat infections caused by multidrug resistant gram-negative pathogens. The composition in-cluded a pharmaceutically acceptable carrier, an antimicro-bial agent and an EPI. The EPI is administered to the lungs as an aerosol to achieve an effective EPI concentration at the site of infection by inhalation. These EPIs have also been co-administered with antimicrobial agents for treatment of oph-thalmic or otic infections directly at the site of infection.
Glinka et al. 2011 [141]: This patent described the methods of treatment and pharmaceutical compositions for co-administering tigecycline with an EPI that increases the
potency of tigecycline. Tigecycline belongs to glycylcycline class of antibiotic analogs not susceptible to known resis-tance mechanisms affecting tetracyclines but there are some pumps known to efflux even this new compound. Tigecy-cline has been recently approved by the Food and Drug Ad-ministration. The EPI is a dipeptidic structure including a stereochemistry that supports reduced tissue accumulation and reduced toxicity of this formulation.
Yoshihara, 2011 [70]: This patent described a method to inhibit MexAB-OprM pump in multidrug resistant P. aeru-ginosa by modifying the amino acid sequence of OprM, an outer membrane subunit of this efflux pump Fig. (2A). The amino acids from positions 100-109 (designated E1) or 311 to 320 (designated E2), which lie in the extracellular domain 3 (ECD) of OprM comprising two loops each with ten amino acids, were modified for this work Fig. (2B). This invention was based on the fact that all three subunits of this pump are indispensable for the pump function. With inhibition of any of these units, the pump becomes non-functional. It was con-cluded that Arginine 311 and Aspartic acid 318 in mature OprM played an important role in the function of MexAB-OprM. Therefore, any agent specifically acting on these amino acids could inhibit the function of this efflux pump. A monoclonal antibody was synthesized and used to block this E2 loop of ECD. This antibody/its variant without Fc do-main/ humanized antibody were administered with the anti-biotic, and an increase in the efficacy of this antibiotic was observed. These formulations could also contain a pharma-ceutically acceptable carrier along with the antibiotic and the antibody and could be used to inhibit the OprM subunit in both MexAB-OprM and MexXY-OprM.
BACTERIAL STRAINS EMPLOYED FOR THE
STUDY OF EFFLUX PUMPS AND THEIR INHIBI-
TORS
Disruption of the efflux pump genes from a bacterial strain has provided an effective means to prove the involve-ment of these proteins in deciding the drug resistance pheno-type of that particular bacterium. For study of native or re-

84 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
combinant efflux pumps and the efficacy of various EPIs, bacterial strains have been constructed with the deletions of some major efflux pumps [30, 31, 66, 75, 88, 89]. These strains have been used as a sensitive tool for drug discovery [88]. For example P. aeruginosa PAO1 wild-type and its efflux mutants were constructed for such a study. Disruption of the gene coding for MexB in this pathogen led to the de-crease in MIC for a wide range of drugs like aminoglyco-sides, chloramphenicol etc. These efflux mutants have been used for identification and characterization of EPIs [66, 89]. Similarly, mutant strain 799/61 of P. aeruginosa which did not produce any measurable amount of efflux pumps were derived from the parent strain 799. These strains were 8- to 10-folds more susceptible to tetracycline and ciprofloxacin [144, 145]. Considering the devastating effect of multidrug resistant S. aureus (MRSA) in clinical settings, the search for inhibitors to restore the activity of antibiotics started with this deadly organism. A strain was constructed with NorA pump disrupted as a tool for drug discovery for screening of natural compounds [88]. Similarly, another strain E. coli
KAM32 has been constructed with the deletions in AcrAB and YdhE pumps for studying the role of efflux pumps from Vibrios when expressed in E. coli KAM32 [55] and has been used to study the functional expression of MATE pumps from V. cholerae when expressed in E. coli [30, 31].
BOTTLENECKS IN THE USE OF EPIS
For most of the EPIs, synthesis of their derivatives, their toxic properties, stability and solubility are some of the fac-tors that have affected their commercial viability [2, 105]. Toxicity problems in EPIs could be due to any of these rea-sons:
1. Compound-specific toxicity: Phototoxicity issues in case of MC-207,110 has led to the failure of this inhibitor in the market despite its potential to restore the activity of levofloxacin [66, 89].
2. The effect of EPIs on infectious bacteria as well as the human host: Efforts should be made to design inhibitors
Fig. (2). A: Tripartite RND pump MexAB-OprM found in P. aeruginosa and implicated in drug resistance phenotype of this pathogen.
MexB is located in the inner membrane, Mex A in the periplasmic space and OprM spans the outer membrane forming a pore through which
the drug is expelled. B: Secondary structure of OprM protein. This outer membrane protein consistes of three domains. Domain 1 is the larg-
est domain comprised of -helices and interacts with MexA and MexB, Domain 2 is a barrel-shaped structure comprised of -sheets and
spans the outer membrane and Domain 3 is the smallest domain comprising of extracellular loops E1 (aa 100-109) and E2 (aa 311-320), each
consisting of ten amino acid residues. Mutations in these two loops have been shown to be crucial for the functioning of OprM and hence the
whole MexAB-OprM pump [70].

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 85
specific for prokaryotic cells. Most of the inhibitors show strong pharmacological activities in eukaryotic hosts and therefore rendered useless in clinical practice. Toxicity problems associated with the use of reserpine, omeprazole and others have been described above.
USES OF EPIS
With the detailed discussion in the above sections per-taining to different EPIs, their advantages and disadvantages, it can be concluded that EPIs could be useful for aca-demic/research and therapeutic purposes for the following reasons:
1. They are used to detect and evaluate different efflux mechanisms in the host organism and can be used as di-agnostic tools [1]. CCCP and reserpine have been used by many groups for this purpose [30, 31, 86, 147, 148].
2. In case of bacteria displaying resistance due to efflux pump, EPIs help in increasing the intracellular drug concentration. This leads to a decrease in the problem of drug resistance by restoring or potentiating the activity of an antimicrobial. MC 04,124 has been shown to po-tentiate the activity of levofloxacin in a mouse model of P. aeruginosa infection and that of azithromycin in a mouse model of E. coli pyelonephritis [149].
3. EPIs lead to a decrease in the frequency of emergence of drug resistant strains. Selection of resistant mutants is reduced as demonstrated for reserpine and quinolones in S. aureus [150] and MC-207,110 and quinolones in P. aeruginosa [66, 89].
4. EPIs are not only useful for treating microbial infections by limiting the drug export, they also prevent the export of other virulence factors synthesized by the microbes thus inhibiting bacterial infections. For example, sidero-phores are needed for bacterial growth under iron starva-tion conditions in a bacterial infection. These are syn-thesized as important virulence factors in the cytoplasm and exported by the efflux pumps when the pathogen requires iron [144, 145]. Hence, the pathogenicity of the bacterium is reduced due to EPI interfering with the transport of siderophores and bacterial iron acquisition and also many other vital virulence factors.
5. EPIs are not only essential for treating the microbial infections when the drugs are clinically ineffective even at high doses, they also help in reducing the dosage of the antimicrobial when used in combination with EPI. This dramatically improves the efficacy of antimicrobi-als as the dosage required is well below the achievable tissue levels for effective treatment [144, 145].
OTHER ROADS THAT CAN BE TRAVERSED
The discussion in this review pertaining to the invention and use of EPIs has led us to believe that with these class of molecules, the existing antibiotics would be effectively used. Nevertheless, researchers and clinicians should be prepared to have alternate strategies in case of failure of EPIs because these EPIs could also suffer from the problem of develop-ment of drug resistance against them thus decreasing their
efficacy. This kind of phenomenon has been observed for reserpine [151]. Some of these have been discussed below:
Older drugs to be re-used: The antimicrobials that were abandoned by clinicians earlier should be re-tried in the clinical settings as there is a probability of reduced resistance towards them. For example, the use of polymyxins had de-clined earlier due to toxicity problems but recent studies have shown that they are still very effective against gram-negative bacteria and not as toxic as indicated earlier [1, 2, 152].
Newer drugs to be developed: There is a need to de-velop novel antibiotics against novel targets that can override the mechanism of resistance [152]. Though there will always be the possibility of developing resistance against these new drugs also, we need to have some new additions in our ar-mamentarium against the deadly pathogens that have tor-mented us in the past.
CURRENT & FUTURE DEVELOPMENTS
With the profligate use of antibiotics in human and vet-erinary medicine leading to a rise in the incidence of multidrug resistance, there is an urgent need to develop novel therapeutic agents to vanquish the threat of antibiotic resistance. The MDR pathogens are notoriously difficult to treat and have debilitating impact on social and economical development. In this review, the possibility of using EPIs as adjunctive therapy in combination with antibiotics has been discussed. In order to produce effective inhibitors, the phar-macodynamic characteristics and other kinetic parameters of EPIs should be studied carefully for their clinical applica-tions and there is a need to develop assay systems for meas-uring their efficacy. Since the inhibitors are used along with a specific antibiotic, the pharmacokinetic properties of both these compounds should be considered for the effective and synergistic use. Structural biology of the efflux pump pro-teins with and without the substrates/inhibitors could provide valuable information about the structure-activity relationship of these efflux pump proteins. Today, in the era of bioinfor-matics and molecular modeling, in silico studies carried out prior to the wet lab experiments can help narrow down the relevant molecules from a vast library of compounds and precise targets could be identified for the EPIs. These EPIs can then be evaluated for their efficacy. Also, the recombi-nant DNA technology allows a researcher to isolate a par-ticular efflux pump gene and express it in a suitable het-erologous host in optimum quantities if the recombinant pro-tein is assembled properly in lipid bilayer and shows activity. The purified recombinant membrane proteins can be studied in combination with the EPIs for the efficacy of the latter. In the current scenario of waning interest of pharmaceutical companies in the antibiotic development, the older/traditional antibiotics can be used in combination with these EPIs [153]. The other fields that would support the design of new EPIs are:
• Structural studies on pumps-substrate complexes
• 3D resolution of structures of efflux pumps
• Combinatorial chemistry and organic synthesis of new compounds/their libraries

86 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
• Molecular dynamics studies
• Rational drug design
• Quantitative structure-activity relationship (QSAR) analysis [154].
Through this review, bacterial multidrug efflux pumps and their inhibitors have been discussed in detail but the clinical significance of efflux-mediated resistance towards antifungal drugs like azole and the EPIs developed to over-come this problem can not be ignored and deserve to be mentioned. It has been shown that azole resistance in fungal infections can be overcome by inhibiting efflux pumps di-rectly and development of EPIs for increasing the potency of antifungals parallels the efforts made to develop inhibitors of human P-glycoprotein [155]. The modified strains of Sac-charomyces cerevisiae have been developed to study the expression of heterologously expressed ABC and MFS transporters like CaCdr1p and Mdr1p respectively from Candida albicans and for the screening of EPIs [155].
ACKNOWLEDGEMENTS
The authors thank the Department of Biotechnology (DBT), Ministry of Science and Technology, Government of India for the grants (BT/PR10304/GBD/27/95/2008 and BT/PR/11634/INF/22/104/2008).
The authors thankfully acknowledge the support from Puri Foundation for Education in India. Authors thank Mr. K Vinothkumar for critical reviewing of the manuscript.
CONFLICT OF INTEREST
There is no potential conflict of interest.
REFERENCES
[1] Van Bambeke F, Pages JM, Lee VJ. Inhibitors of bacterial efflux pumps as adjuvants in antibiotic treatments and diagnostic tools for
detection of resistance by efflux. Recent Pat Anti-Infect Drug Dis-cov 2006; 1: 157-75.
[2] Zechini B, Versace I. Inhibitors of multidrug resistant efflux sys-tems in bacteria. Recent Pat Anti-Infect Drug Discov 2009; 4: 37-
50. [3] Piddock LJ. Clinically relevant chromosomally encoded multidrug
resistance efflux pumps in bacteria. Clin Microbiol Rev 2006; 19: 382-402.
[4] Piddock LJ. Multidrug-resistance efflux pumps- not just for resis-tance. Nature Rev Microbiol 2006; 4: 629-36.
[5] Gothi D, Joshi JM. Resistant TB: Newer drugs and community approach. Recent Pat Anti-Infect Drug Discov 2011; 6: 27-37.
[6] Askoura M, Mottawea W, Abujamel T, Taher I. Efflux pump in-hibitors (EPIs) as new antimicrobial agents against Pseudomonas
aeruginosa. Libyan J Med 2011; 6: 5870 - DOI: 10.3402/ljm.v6i0.5870
[7] Salyers AA WD. Bacterial pathogenesis: A molecular approach. 2nd ed. Washington DC ASM; 2002.
[8] McMurry L, Petrucci RE, Jr., Levy SB. Active efflux of tetracy-cline encoded by four genetically different tetracycline resistance
determinants in Escherichia coli. Proc Natl Acad Sci USA 1980; 77: 3974-7.
[9] Poole K. Efflux-mediated antimicrobial resistance. J Antimicrob Chemother 2005; 56: 20-51.
[10] Bina JE, Mekalanos JJ. Vibrio cholerae to lC is required for bile resistance and colonization. Infect Immun 2001; 69: 4681-5.
[11] Bina XR, Provenzano D, Nguyen N, Bina JE. Vibrio cholerae RND family efflux systems are required for antimicrobial resistance, op-
timal virulence factor production, and colonization of the infant mouse small intestine. Infect Immun 2008; 76: 3595-605.
[12] Ren Q, Paulsen IT. Comparative analyses of fundamental differ-
ences in membrane transport capabilities in prokaryotes and eu-karyotes. PLoS Computational Biol 2005; 1: e27.
[13] Butaye P, Cloeckaert A, Schwarz S. Mobile genes coding for ef-flux-mediated antimicrobial resistance in Gram-positive and Gram-
negative bacteria. Int J Antimicrob Agents 2003; 22: 205-10. [14] Clancy J, Petitpas J, Dib-Hajj F, Yuan W, Cronan M, Kamath AV,
et al. Molecular cloning and functional analysis of a novel macrol-ide-resistance determinant, mefA, from Streptococcus pyogenes.
Mol Microbiol 1996; 22: 867-79. [15] Tait-Kamradt A, Clancy J, Cronan M, Dib-Hajj F, Wondrack L,
Yuan W, et al. mefE is necessary for the erythromycin-resistant M phenotype in Streptococcus pneumoniae. Antimicrob Agents Che-
mother 1997; 41: 2251-5. [16] Ma J, Zeng Z, Chen Z, Xu X, Wang X, Deng Y, et al. High preva-
lence of plasmid-mediated quinolone resistance determinants qnr, aac(6')-Ib-cr, and qepA among ceftiofur-resistant Enterobacte-
riaceae isolates from companion and food-producing animals. An-timicrob Agents Chemother 2009; 53: 519-24.
[17] Zhao J, Chen Z, Chen S, Deng Y, Liu Y, Tian W, et al. Prevalence and dissemination of OqxAB in Escherichia coli isolates from
animals, farmworkers and the environment. Antimicrob Agents Chemother 2010; 54: 4219-24.
[18] Mazzariol A, Cornaglia G, Nikaido H. Contributions of the AmpC beta-lactamase and the AcrAB multidrug efflux system in intrinsic
resistance of Escherichia coli K-12 to beta-lactams. Antimicrob Agents Chemother 2000; 44: 1387-90.
[19] Broskey J, Coleman K, Gwynn MN, McCloskey L, Traini C, Voel-ker L, et al. Efflux and target mutations as quinolone resistance
mechanisms in clinical isolates of Streptococcus pneumoniae. J Antimicrob Chemother 2000; 45 (Suppl 1): 95-9.
[20] Baranwal S, Dey K, Ramamurthy T, Nair GB, Kundu M. Role of active efflux in association with target gene mutations in fluoroqui-
nolone resistance in clinical isolates of Vibrio cholerae. Antimicrob Agents Chemother 2002; 46: 2676-8.
[21] Pazhani GP, Chakraborty S, Fujihara K, Yamasaki S, Ghosh A, Nair GB, et al. QRDR mutations, efflux system & antimicrobial re-
sistance genes in enterotoxigenic Escherichia coli isolated from an outbreak of diarrhoea in Ahmedabad, India. Indian J Med Res
2011; 134: 214-23. [22] Borges-Walmsley MI, McKeegan KS, Walmsley AR. Structure and
function of efflux pumps that confer resistance to drugs. Biochem J 2003; 376: 313-38.
[23] Paulsen IT. Multidrug efflux pumps and resistance: regulation and evolution. Curr Opin Microbiol 2003; 6: 446-51.
[24] Poole K. Efflux mediated antimicrobial resistance. J Antimicrob Chemother 2005; 56: 20-51.
[25] Lage H. ABC-transporters: Implications on drug resistance from microorganisms to human cancers. Int J Antimicrob Agents 2003;
22: 188-99. [26] Poelarends GJ, Mazurkiewicz P, Konings WN. Multidrug trans-
porters and antibiotic resistance in Lactococcus lactis. Biochim Biophys Acta 2002; 1555: 1-7.
[27] Yoshida H, Bogaki M, Nakamura S, Ubukata K, Konno M. Nu-cleotide sequence and characterization of the Staphylococcus
aureus norA gene, which confers resistance to quinolones. J Bacte-riol 1990; 172: 6942-9.
[28] Gill MJ, Brenwald NP, Wise R. Identification of an efflux pump gene, pmrA, associated with fluoroquinolone resistance in Strepto-
coccus pneumoniae. Antimicrob Agents Chemother 1999; 43: 187-9.
[29] Lee EW, Chen J, Huda MN, Kuroda T, Mizushima T, Tsuchiya T. Functional cloning and expression of emeA, and characterization of
EmeA, a multidrug efflux pump from Enterococcus faecalis. Biol Pharm Bull 2003; 26: 266-70.
[30] Morita Y, Kodama K, Shiota S, Mine T, Kataoka A, Mizushima T, et al. NorM, a putative multidrug efflux protein, of Vibrio para-
haemolyticus and its homolog in Escherichia coli. Antimicrob Agents Chemother 1998; 42: 1778-82.
[31] Begum A, Rahman MM, Ogawa W, Mizushima T, Kuroda T, Tsuchiya T. Gene cloning and characterization of four MATE fam-
ily multidrug efflux pumps from Vibrio cholerae non-O1. Micro-biol Immunol 2005; 49: 949-57.
[32] Bornet C, Chollet R, Mallea M, Chevalier J, Davin-Regli A, Pages JM, et al. Imipenem and expression of multidrug efflux pump in

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 87
Enterobacter aerogenes. Biochem Biophys Res Commun 2003;
301: 985-90. [33] Steinfels E, Orelle C, Fantino JR, Dalmas O, Rigaud JL, Denizot F,
et al. Characterization of YvcC (BmrA), a multidrug ABC trans-porter constitutively expressed in Bacillus subtilis. Biochemistry
2004; 43: 7491-502. [34] Kaatz GW, Seo SM. Inducible NorA-mediated multidrug resistance
in Staphylococcus aureus. Antimicrob Agents Chemother 1995; 39: 2650-5.
[35] Truong-Bolduc QC, Dunman PM, Strahilevitz J, Projan SJ, Hooper DC. MgrA is a multiple regulator of two new efflux pumps in
Staphylococcus aureus. J Bacteriol 2005; 187: 2395-405. [36] Kaatz GW, McAleese F, Seo SM. Multidrug resistance in Staphy-
lococcus aureus due to overexpression of a novel multidrug and toxin extrusion (MATE) transport protein. Antimicrob Agents
Chemother 2005; 49: 1857-64. [37] Reynolds E, Ross JI, Cove JH. Msr(A) and related macrol-
ide/streptogramin resistance determinants: incomplete transporters? Int J Antimicrob Agents 2003; 22: 228-36.
[38] Huang J, O'Toole PW, Shen W, Amrine-Madsen H, Jiang X, Lobo N, et al. Novel chromosomally encoded multidrug efflux trans-
porter MdeA in Staphylococcus aureus. Antimicrob Agents Che-mother 2004; 48: 909-17.
[39] Robertson GT, Doyle TB, Lynch AS. Use of an efflux-deficient Streptococcus pneumoniae strain panel to identify ABC-class
multidrug transporters involved in intrinsic resistance to antimicro-bial agents. Antimicrob Agents Chemother 2005; 49: 4781-3.
[40] Pozzi G, Iannelli F, Oggioni MR, Santagati M, Stefani S. Genetic elements carrying macrolide efflux genes in streptococci. Curr
Drug Targets Infect Disord 2004; 4: 203-6. [41] Dean CR, Visalli MA, Projan SJ, Sum PE, Bradford PA. Efflux-
mediated resistance to tigecycline (GAR-936) in Pseudomonas aeruginosa PAO1. Antimicrob Agents Chemother 2003; 47: 972-8.
[42] He GX, Kuroda T, Mima T, Morita Y, Mizushima T, Tsuchiya T. An H(+)-coupled multidrug efflux pump, PmpM, a member of the
MATE family of transporters, from Pseudomonas aeruginosa. J Bacteriol 2004; 186: 262-5.
[43] Poole K, Srikumar R. Multidrug efflux in Pseudomonas aerugi-nosa: Components, mechanisms and clinical significance. Curr Top
Med Chem 2001; 1: 59-71. [44] Eaves DJ, Ricci V, Piddock LJ. Expression of acrB, acrF, acrD,
marA, and soxS in Salmonella enterica, Serovar typhimurium: Role in multiple antibiotic resistance. Antimicrob Agents Chemother
2004; 48: 1145-50. [45] Nikaido H. Multidrug efflux pumps of gram-negative bacteria. J
Bacteriol 1996; 178: 5853-9. [46] Pumbwe L, Piddock LJ. Identification and molecular characterisa-
tion of CmeB, a Campylobacter jejuni multidrug efflux pump. FEMS Microbiol Lett 2002; 206: 185-9.
[47] Veal WL, Nicholas RA, Shafer WM. Overexpression of the MtrC-MtrD-MtrE efflux pump due to an mtrR mutation is required for
chromosomally mediated penicillin resistance in Neisseria gonor-rhoeae. J Bacteriol 2002; 184: 5619-24.
[48] Pumbwe L, Chang A, Smith RL, Wexler HM. Clinical significance of overexpression of multiple RND-family efflux pumps in Bacter-
oides fragilis isolates. J Antimicrob Chemother 2006; 58: 543-8. [49] Miyamae S, Ueda O, Yoshimura F, Hwang J, Tanaka Y, Nikaido
H. A MATE family multidrug efflux transporter pumps out fluoro-quinolones in Bacteroides thetaiotaomicron. Antimicrob Agents
Chemother 2001; 45: 3341-6. [50] Xu XJ, Su XZ, Morita Y, Kuroda T, Mizushima T, Tsuchiya T.
Molecular cloning and characterization of the HmrM multidrug ef-flux pump from Haemophilus influenzae Rd. Microbiol Immunol
2003; 47: 937-43. [51] Peric M, Bozdogan B, Jacobs MR, Appelbaum PC. Effects of an
efflux mechanism and ribosomal mutations on macrolide suscepti-bility of Haemophilus influenzae clinical isolates. Antimicrob
Agents Chemother 2003; 47: 1017-22. [52] Kobayashi N, Nishino K, Yamaguchi A. Novel macrolide-specific
ABC-type efflux transporter in Escherichia coli. J Bacteriol 2001; 183: 5639-44.
[53] Chollet R, Chevalier J, Bryskier A, Pages JM. The AcrAB-TolC pump is involved in macrolide resistance but not in telithromycin
efflux in Enterobacter aerogenes and Escherichia coli. Antimicrob Agents Chemother 2004; 48: 3621-4.
[54] Schwarz S, Kehrenberg C, Doublet B, Cloeckaert A. Molecular
basis of bacterial resistance to chloramphenicol and florfenicol. FEMS Microbiol Rev 2004; 28: 519-42.
[55] Chen J, Morita Y, Huda MN, Kuroda T, Mizushima T, Tsuchiya T. VmrA, a member of a novel class of Na(+)-coupled multidrug ef-
flux pumps from Vibrio parahaemolyticus. J Bacteriol 2002; 184: 572-6.
[56] Morita Y, Kataoka A, Shiota S, Mizushima T, Tsuchiya T. NorM of Vibrio parahaemolyticus is an Na(+)-driven multidrug efflux
pump. J Bacteriol 2000; 182: 6694-7. [57] Huda N, Lee EW, Chen J, Morita Y, Kuroda T, Mizushima T, et al.
Molecular cloning and characterization of an ABC multidrug efflux pump, VcaM, in Non-O1 Vibrio cholerae. Antimicrob Agents
Chemother 2003; 47: 2413-7. [58] Woolley RC, Vediyappan G, Anderson M, Lackey M, Rama-
subramanian B, Jiangping B, et al. Characterization of the Vibrio cholerae vceCAB multiple-drug resistance efflux operon in Es-
cherichia coli. J Bacteriol 2005; 187: 5500-3. [59] Bina JE, Provenzano D, Wang C, Bina XR, Mekalanos JJ. Charac-
terization of the Vibrio cholerae vexAB and vexCD efflux systems. Arch Microbiol 2006; 186: 171-81.
[60] Akama H, Kanemaki M, Yoshimura M, Tsukihara T, Kashiwagi T, Yoneyama H, et al. Crystal structure of the drug discharge outer
membrane protein, OprM, of Pseudomonas aeruginosa: Dual modes of membrane anchoring and occluded cavity end. J Biol
Chem 2004; 279: 52816-9. [61] Akama H, Matsuura T, Kashiwagi S, Yoneyama H, Narita S, Tsu-
kihara T, et al. Crystal structure of the membrane fusion protein, MexA, of the multidrug transporter in Pseudomonas aeruginosa. J
Biol Chem 2004; 279: 25939-42. [62] Higgins MK, Bokma E, Koronakis E, Hughes C, Koronakis V.
Structure of the periplasmic component of a bacterial drug efflux pump. Proc Natl Acad Sci USA 2004; 101: 9994-9.
[63] Koronakis V, Sharff A, Koronakis E, Luisi B, Hughes C. Crystal structure of the bacterial membrane protein TolC central to
multidrug efflux and protein export. Nature 2000; 405: 914-9. [64] Murakami S, Nakashima R, Yamashita E, Yamaguchi A. Crystal
structure of bacterial multidrug efflux transporter AcrB. Nature 2002; 419: 587-93.
[65] He X, Szewczyk P, Karyakin A, Evin M, Hong WX, Zhang Q, et al. Structure of a cation-bound multidrug and toxic compound
extrusion transporter. Nature 2010; 467: 991-4. [66] Lomovskaya O, Warren MS, Lee A, Galazzo J, Fronko R, Lee M,
et al. Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: Novel agents
for combination therapy. Antimicrob Agents Chemother 2001; 45: 105-16.
[67] Chopra I. New developments in tetracycline antibiotics: Glycylcy-clines and tetracycline efflux pump inhibitors. Drug Resist Updat
2002; 5: 119-25. [68] Hooper DC. Mechanisms of action and resistance of older and
newer fluoroquinolones. Clin Infect Dis 2000; 31 (Suppl 2): S24-8. [69] Zgurskaya HI, Nikaido H. Multidrug resistance mechanisms: Drug
efflux across two membranes. Mol Microbiol 2000; 37: 219-25. [70] Yoshihara, E., Inoko, H. Method or agent for inhibiting the func-
tion of efflux pump in Pseudomonas aeruginosa. US7985410B2 (2011).
[71] Pages JM, Masi M, Barbe J. Inhibitors of efflux pumps in Gram-negative bacteria. Trends Mol Med 2005; 11: 382-9.
[72] Kern WV, Oethinger M, Jellen-Ritter AS, Levy SB. Non-target gene mutations in the development of fluoroquinolone resistance in
Escherichia coli. Antimicrob Agents Chemother 2000; 44: 814-20. [73] Marquez B. Bacterial efflux systems and efflux pumps inhibitors.
Biochimie 2005; 87: 1137-47. [74] Lynch AS. Efflux systems in bacterial pathogens: An opportunity
for therapeutic intervention? An industry view. Biochem Pharma-col 2006; 71: 949-56.
[75] Lomovskaya O, Bostian KA. Practical applications and feasibility of efflux pump inhibitors in the clinic--a vision for applied use.
Biochem Pharmacol 2006; 71: 910-8. [76] Mahamoud A, Chevalier J, Alibert-Franco S, Kern WV, Pages JM.
Antibiotic efflux pumps in Gram-negative bacteria: The inhibitor response strategy. J Antimicrob Chemother 2007; 59: 1223-9.
[77] Oethinger, M., Levy, S.B. Methods of reducing microbial resis-tance to drugs. US6346391B1 (2002).

88 Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 Bhardwaj and Mohanty
[78] Oethinger, M., Levy S. B. Methods of screening for compounds
that reduce microbial resistance to fluoroquinolones. US8012711B2 (2011).
[79] Tegos G, Stermitz FR, Lomovskaya O, Lewis K. Multidrug pump inhibitors uncover remarkable activity of plant antimicrobials. An-
timicrob Agents Chemother 2002; 46: 3133-41. [80] Stermitz FR, Lorenz P, Tawara JN, Zenewicz LA, Lewis K. Syn-
ergy in a medicinal plant: antimicrobial action of berberine potenti-ated by 5'-methoxyhydnocarpin, a multidrug pump inhibitor. Proc
Natl Acad Sci USA 2000; 97: 1433-7. [81] Stermitz FR, Beeson TD, Mueller PJ, Hsiang J, Lewis K. Staphylo-
coccus aureus MDR efflux pump inhibitors from a Berberis and a Mahonia (Sensu strictu) species. Biochem Syst Ecol 2001; 29: 793-
98. [82] Stermitz FR, Scriven LN, Tegos G, Lewis K. Two flavonols from
Artemisa annua which potentiate the activity of berberine and nor-floxacin against a resistant strain of Staphylococcus aureus. Planta
medica 2002; 68: 1140-1. [83] Mallea M, Chevalier J, Eyraud A, Pages JM. Inhibitors of antibiotic
efflux pump in resistant Enterobacter aerogenes strains. Biochem Biophys Res Commun 2002; 293: 1370-3.
[84] Klyachko KA, Schuldiner S, Neyfakh AA. Mutations affecting substrate specificity of the Bacillus subtilis multidrug transporter
Bmr. J Bacteriol 1997; 179: 2189-93. [85] Neyfakh AA, Bidnenko VE, Chen LB. Efflux-mediated multidrug
resistance in Bacillus subtilis: Similarities and dissimilarities with the mammalian system. Proc Natl Acad Sci USA 1991; 88: 4781-5.
[86] Li XZ, Nikaido H. Efflux-mediated drug resistance in bacteria. Drugs 2004; 64: 159-204.
[87] Neyfakh AA, Borsch CM, Kaatz GW. Fluoroquinolone resistance protein NorA of Staphylococcus aureus is a multidrug efflux trans-
porter. Antimicrob Agents Chemother 1993; 37: 128-9. [88] Hsieh PC, Siegel SA, Rogers B, Davis D, Lewis K. Bacteria lack-
ing a multidrug pump: A sensitive tool for drug discovery. Proc Natl Acad Sci USA 1998; 95: 6602-6.
[89] Lomovskaya O, Watkins W. Inhibition of efflux pumps as a novel approach to combat drug resistance in bacteria. J Mol Microbiol
Biotechnol 2001; 3: 225-36. [90] Brenwald NP, Gill MJ, Wise R. The effect of reserpine, an inhibi-
tor of multi-drug efflux pumps, on the in vitro susceptibilities of fluoroquinolone-resistant strains of Streptococcus pneumoniae to
norfloxacin. J Antimicrob Chemother 1997; 40: 458-60. [91] Vidaillac C, Guillon J, Arpin C, Forfar-Bares I, Ba BB, Grellet J,
et al. Synthesis of omeprazole analogues and evaluation of these as potential inhibitors of the multidrug efflux pump NorA of Staphy-
lococcus aureus. Antimicrob Agents Chemother 2007; 51: 831-8. [92] Chan YY, Ong YM, Chua KL. Synergistic interaction between
phenothiazines and antimicrobial agents against Burkholderia pseudomallei. Antimicrob Agents Chemother 2007; 51: 623-30.
[93] Lehtinen J, Lilius EM. Promethazine renders Escherichia coli susceptible to penicillin G: real-time measurement of bacterial sus-
ceptibility by fluoro-luminometry. Int J Antimicrob Agents 2007; 30: 44-51.
[94] Kolaczkowski M, Michalak K, Motohashi N. Phenothiazines as potent modulators of yeast multidrug resistance. Int J Antimicrob
Agents 2003; 22: 279-83. [95] Viveiros M, Amaral L. Enhancement of antibiotic activity against
poly-drug resistant Mycobacterium tuberculosis by phenothiazines. Int J Antimicrob Agents 2001; 17: 225-8.
[96] Oduola AM, Sowunmi A, Milhous WK, Brewer TG, Kyle DE, Gerena L, et al. In vitro and in vivo reversal of chloroquine resis-
tance in Plasmodium falciparum with promethazine. Am J Trop Med Hyg 1998; 58: 625-9.
[97] Molnar J, Hever A, Fakla I, Fisher J, Ocsovski I, Aszalos A. Inhibi-tion of the transport function of membrane proteins by some substi-
tuted phenothiazines in Escherichia coli and multidrug resistant tumor cells. Anticancer Res 1997; 17: 481-486.
[98] Michalak K, Wesolowska O, Motohashi N, Molnar J, Hendrich AB. Interaction of phenothiazines with lipid bilayer and their role
in multidrug resistance reversal. Curr Drug Targets 2006; 7: 1095- 1105.
[99] Munoz-Bellido JL, Munoz-Criado S, Garcia-Rodriguez JA. Antim-icrobial activity of psychotropic drugs: Selective serotonin reuptake
inhibitors. Int J Antimicrob Agents 2000; 14: 177-80. [100] Kaatz GW, Moudgal VV, Seo SM, Hansen JB, Kristiansen JE.
Phenylpiperidine selective serotonin reuptake inhibitors interfere
with multidrug efflux pump activity in Staphylococcus aureus. Int J
Antimicrob Agents 2003; 22: 254-61. [101] German N, Kaatz GW, Kerns RJ. Synthesis and evaluation of
PSSRI-based inhibitors of Staphylococcus aureus multidrug efflux pumps. Bioorg Med Chem Lett 2008; 18: 1368-73.
[102] Kern WV, Steinke P, Schumacher A, Schuster S, von Baum H, Bohnert JA. Effect of 1-(1-naphthylmethyl)-piperazine, a novel pu-
tative efflux pump inhibitor, on antimicrobial drug susceptibility in clinical isolates of Escherichia coli. J Antimicrob Chemother 2006;
57: 339-43. [103] Thorarensen A, Presley-Bodnar AL, Marotti KR, Boyle TP,
Heckaman CL, Bohanon MJ, et al. 3-Arylpiperidines as potentia-tors of existing antibacterial agents. Bioorg Med Chem Lett 2001;
11: 1903-6. [104] Markham PN, Neyfakh AA. Inhibition of the multidrug transporter
NorA prevents emergence of norfloxacin resistance in Staphylo-coccus aureus. Antimicrob Agents Chemother 1996; 40: 2673-4.
[105] Markham PN, Westhaus E, Klyachko K, Johnson ME, Neyfakh AA. Multiple novel inhibitors of the NorA multidrug transporter of
Staphylococcus aureus. Antimicrob Agents Chemother 1999; 43: 2404-8.
[106] Markham, P.N., Mulhearn, D.C., Neyfakh, A.A., Crich, D., Jaber, M.-R., Johnson, M.E. Inhibitors of multidrug transporters.
US6362229B1 (2002). [107] Markham, P.N., Mulhearn, D.C., Neyfakh, A.A., Crich, D., Jaber,
M.-R., Johnson, M.E. WO0032196A2, WO0032196A3 (2000). [108] Renau TE, Leger R, Flamme EM, Sangalang J, She MW, Yen R,
et al. Inhibitors of efflux pumps in Pseudomonas aeruginosa poten-tiate the activity of the fluoroquinolone antibacterial levofloxacin. J
Med Chem 1999; 42: 4928-31. [109] Coban AY, Ekinci B, Durupinar B. A multidrug efflux pump in-
hibitor reduces fluoroquinolone resistance in Pseudomonas aerugi-nosa isolates. Chemotherapy 2004; 50: 22-6.
[110] Chamberland, S., Hecker, S.J., Lee, V.J., Trias, J. Efflux pump inhibitors. WO9633285A1 (1996).
[111] Chamberland S., Lee, M., Lee, V.J., Leger, R., Renau, T., She, M., Zhang, Z.J. Efflux pump inhibitors. WO9937667A1 (1999).
[112] Chamberland, S., Ishida, Y., Lee, V.J., Leger, R., Nakayama, K., Ohta, T., Ohtsuka, M., Renau, T.E., Watkins, W.J., Zhang, Z.J. Ef-
flux pump inhibitors. US6399629B1 (2002). [113] Yu EW, Aires JR, McDermott G, Nikaido H. A periplasmic drug-
binding site of the AcrB multidrug efflux pump: A crystallographic and site-directed mutagenesis study. J Bacteriol 2005; 187: 6804-
15. [114] Mamelli L, Amoros JP, Pages JM, Bolla JM. A phenylalanine-
arginine beta-naphthylamide sensitive multidrug efflux pump in-volved in intrinsic and acquired resistance of Campylobacter to
macrolides. Int J Antimicrob Agents 2003; 22: 237-41. [115] Hasdemir UO, Chevalier J, Nordmann P, Pages JM. Detection and
prevalence of active drug efflux mechanism in various multidrug-resistant Klebsiella pneumoniae strains from Turkey. J Clin Microb
2004; 42: 2701-6. [116] Mazzariol A, Tokue Y, Kanegawa TM, Cornaglia G, Nikaido H.
High-level fluoroquinolone-resistant clinical isolates of Es-cherichia coli overproduce multidrug efflux protein AcrA. Antimi-
crob Agents Chemother 2000; 44: 3441-3. [117] Baucheron S, Imberechts H, Chaslus-Dancla E, Cloeckaert A. The
AcrB multidrug transporter plays a major role in high-level fluoro-quinolone resistance in Salmonella enterica serovar typhimurium
phage type DT204. Microb Drug Resist 2002; 8: 281-9. [118] Renau TE, Leger R, Flamme EM, She MW, Gannon CL, Mathias
KM, et al. Addressing the stability of C-capped dipeptide efflux pump inhibitors that potentiate the activity of levofloxacin in Pseu-
domonas aeruginosa. Bioorg Med Chem Lett 2001; 11: 663-7. [119] Renau TE, Leger R, Yen R, She MW, Flamme EM, Sangalang J,
et al. Peptidomimetics of efflux pump inhibitors potentiate the ac-tivity of levofloxacin in Pseudomonas aeruginosa. Bioorg Med
Chem Lett 2002; 12: 763-6. [120] Renau TE, Leger R, Filonova L, Flamme EM, Wang M, Yen R,
et al. Conformationally-restricted analogues of efflux pump inhibi-tors that potentiate the activity of levofloxacin in Pseudomonas
aeruginosa. Bioorg Med Chem Lett 2003; 13: 2755-8. [121] Watkins WJ, Landaverry Y, Leger R, Litman R, Renau TE, Wil-
liams N, et al. The relationship between physicochemical proper-ties, in vitro activity and pharmacokinetic profiles of analogues of

Efflux Pump Inhibitors Restore and Potentiate the Activity of Antimicrobials Recent Patents on Anti-Infective Drug Discovery, 2012, Vol. 7, No. 1 89
diamine-containing efflux pump inhibitors. Bioorg Med Chem Lett
2003; 13: 4241-4. [122] Chevalier J, Bredin J, Mahamoud A, Mallea M, Barbe J, Pages JM.
Inhibitors of antibiotic efflux in resistant Enterobacter aerogenes and Klebsiella pneumoniae strains. Antimicrob Agents Chemother
2004; 48: 1043-6. [123] Rothstein DM, McGlynn M, Bernan V, McGahren J, Zaccardi J,
Cekleniak N, et al. Detection of tetracyclines and efflux pump in-hibitors. Antimicrob Agents Chemother 1993; 37: 1624-9.
[124] Armistead, D.M., Boger, J.S., Meyers, H.V., Saunders, J.O., Tung, R.D. Immunosuppressive compounds. US19945330993 (1994).
[125] Zelle, R.E., Harding, M.W. Amino acid derivatives with improved multi-drug resistance activity. US19965543423 (1996).
[126] Zelle RE, Harding, M.W. Tetralin compounds with improved MDR activity. US19985726184 (1998).
[127] Grossman TH. Compounds augmenting the activity of antibacterial agents. WO05007162A1 (2005).
[128] Sudano Roccaro A, Blanco AR, Giuliano F, Rusciano D, Enea V. Epigallocatechin-gallate enhances the activity of tetracycline in
Staphylococci by inhibiting its efflux from bacterial cells. Antimi-crob Agents Chemother 2004; 48:1968-73.
[129] Gibbons S, Oluwatuyi M, Kaatz GW. A novel inhibitor of multidrug efflux pumps in Staphylococcus aureus. J Antimicrob
Chemother 2003; 51: 13-7. [130] Mullin S, Mani N, Grossman TH. Inhibition of antibiotic efflux in
bacteria by the novel multidrug resistance inhibitors biricodar (VX-710) and timcodar (VX-853). Antimicrob Agents Chemother 2004;
48: 4171-6. [131] Levy, S.B. Reducing tetracycline resistance in living cells.
US19985811412 (1998). [132] Nelson ML, Park BH, Andrews JS, Georgian VA, Thomas RC,
Levy SB. Inhibition of the tetracycline efflux antiport protein by 13-thio-substituted 5-hydroxy-6- deoxytetracyclines. J Med Chem
1993; 36: 370-7. [133] Nelson ML, Park BH, Levy SB. Molecular requirements for the
inhibition of the tetracycline antiport protein and the effect of po-tent inhibitors on the growth of tetracycline-resistant bacteria. J
Med Chem 1994; 37: 1355-61. [134] Nelson ML, Levy SB. Reversal of tetracycline resistance mediated
by different bacterial tetracycline resistance determinants by an in-hibitor of the Tet(B) antiport protein. Antimicrob Agents Che-
mother 1999; 43: 1719-24. [135] Myers AG, Charest, M.G., Lerner, C.D., Brubaker, J.D., Siegel,
D.R. Synthesis of tetracyclines and analogues thereof. US7807842B2 (2010).
[136] Nelson, M.L., Alekshun, M.N. Substituted polyamines as inhibitors of bacterial efflux pumps. WO2004062674A2 (2004).
[137] De Souza, N., Patel, M.V., Gupte, S.V., Upadhyay, D.J., Shukla, M.C., Chaturvedi, N.C., Bhawsar, S.B., Nair, S.C., Jafri, M.A.,
Khorakiwala, H.F. Inhibitors of cellular efflux pumps of microbes. WO0209758A2 & WO0209758A3 (2002).
[138] Meng J, Bai H, Jia M, Ma X, Hou Z, Xue X, et al. Restoration of antibiotic susceptibility in fluoroquinolone-resistant Escherichia
coli by targeting acrB with antisense phosphorothioate oligonucleo-tide encapsulated in novel anion liposome. J Antibiot 2011; doi:
10.1038/ja.2011.125.
[139] Bostian, K., Glinka, T., Lomovskaya, O., Surber, M., Berkley, N.,
Griffith D. Bacterial efflux pump inhibitors for the treatment of ophthalmic and otic infections. US7994225B2 (2011).
[140] Bostian, K., Glinka, T., Lomovskaya, O., Surber, M. Use and ad-ministration of bacterial efflux pump inhibitors. US7947741B2
(2011). [141] Glinka, T., Bostian, K., Lomovskaya, O., Surber, M., Sun, D En-
hancement of tigecycline potency using efflux pump inhibitors US7879795B2 (2011).
[142] Nelson, M.L., Alekshun, M.N. Substituted polyamines as inhibitors of bacterial efflux pumps. US20110218168A1 (2011).
[143] Nelson, M.L., Alekshun, M.N. Substituted polyamines as inhibitors of bacterial efflux pumps. US7829543B2 (2010).
[144] Leger, R.L, Ving, J. She, M. Peptidomimetic efflux pump inhibi-tors. US6204279B1 (2001).
[145] Leger RL, Ving J. She, M. Peptidomimetic efflux pump inhibitors. US6436980B1 (2002).
[146] Nakayama, K., Ohtsuka, M., Kawato, H., Watkins, W., Zhang, J., Palme, M., Cho, A. Drug efflux pump inhibitor. US7056917B2
(2006). [147] Singh R, Rajpara N, Tak J, Patel A, Mohanty P, Vinothkumar K,
et al. Clinical isolates of Vibrio fluvialis from Kolkata, India, ob-tained during 2006: Plasmids, qnr and mutation in gyrase A as
mechanisms of multidrug resistance. J Med Microbiol 2011; [148] Srinivasan VB, Virk RK, Kaundal A, Chakraborty R, Datta B,
Ramamurthy T, et al. Mechanism of drug resistance in clonally re-lated clinical isolates of Vibrio fluvialis isolated in Kolkata, India.
Antimicrob Agents Chemother 2006; 50: 2428-32. [149] Griffith DC, Corcoran E, Sorensen K, Cho D, Lomovskaya O,
Dudley MN. Potentiation of levofloxacin and azithromycin by MC-04, 124, a broad spectrum efflux pump inhibitor, in mouse models
of infection due to strains of Pseudomonas aeruginosa and Es-cherichia coli expressing efflux pumps. 41st Interscience Confer-
ence on Antimicrobial Agents and Chemotherapy. Chicago, I11 (2001). F-340.
[150] Markham PN, Neyfakh AA. Inhibition of the multidrug transporter NorA prevents prevents emergence of norfloxacin resistance in
Staphylococcus aureus. Antimicrob Agents Chemother 1996; 40: 2673-4.
[151] Garvey MI, Piddock LSV. The efflux pump inhibitor reserpine selects multidrug resistant S. pneumoniae strains that overexpress
the ABC transporters PatA and PatB. Antimicrob Agents Che-mother 2008; 52: 1677-1685.
[152] Projan SJ. New (and not so new) antibacterial targets - from where and when will the novel drugs come? Curr Opin Pharmacol 2002;
2: 513-22. [153] Projan SJ. Why is big Pharma getting out of antibacterial drug
discovery? Curr Opin Microbiol 2003; 6: 427-30. [154] Nargotra A, Koul S, Sharma S, Khan IA, Kumar A, Thota N, et al.
Quantitative structure-activity relationship (QSAR) of aryl alkenyl amides/imines for bacterial efflux pump inhibitors. Eur J Med
Chem 2009; 44: 229-38. [155] Cannon RD, Lamping E, Holmes AR, Niimi K, Baret PV, Keniya
MV, et al. Efflux-mediated antifungal drug resistance. Clin Micro-biol Rev 2009; 22: 291-321.