archive.psnc.org.ukarchive.psnc.org.uk/services_db/docs/467/NHS_Dorset_NHS_Health... · Web...
Transcript of archive.psnc.org.ukarchive.psnc.org.uk/services_db/docs/467/NHS_Dorset_NHS_Health... · Web...
Local Enhanced Service for NHS Health Checks (Vascular)
Author(s): Rose Owens/Julia Booth
Issue Date: October 2010
Version no: 2
Status: FINAL
Review date: as required for service development
Agreed with LMCAgreed with LPC
Page 1 of 25
Specification: NHS Health Checks (Vascular)
1. INTRODUCTION
1.1. This specification sets out a joint Local Enhanced Service (LES) for GMS, PMS and Community Pharmacy contractors to provide NHS Health Checks (vascular risk assessment and management services).
1.2. All providers are expected to provide the full range of essential and those additional/advanced services as set out in their contracts. This enhanced service specification for the provision of a screening programme for NHS Health Checks (vascular) is designed to cover the enhanced aspects of the clinical care provided to the patient, all of which are beyond the scope of essential services. No part of the specification by commission, omission or implication defines or redefines essential or additional services.
1.3. With any provision of service, consideration must be given to addressing inequalities in health. This primary care service provides an opportunity to narrow the inequalities gap by providing services not only to the mainstream population but also to those in disadvantaged groups with poor health outcomes. As the service develops, ways of engaging people who do not normally access healthcare services will be explored.
1.4. The service will be introduced initially in early adopter sites which will be selected to ensure that the most disadvantaged groups in both a rural and urban setting can be targeted in the first instance. The service will be rolled out over a period of time across the remainder of the trust. The first phase of the programme will target those in the 40 to 74 age group who have an established or estimated CVD risk score of >20% over 10 years as identified by the Oberoi software, are recorded as current smokers (or who have no data regarding their smoking status) and are not already on any vascular disease register.
1.5. The LES will be comprised of two components –
Component A: The initial work required of GMS/PMS contractors to identify patients, set up call and recall systems, send invitations and record outcome data from all checks carried out in a timely and accurate way on the GP clinical system.
Component B: The process for GMS, PMS and community pharmacy contractors carrying out NHS Health Checks, as well as follow-up and referral pathways.
Page 2 of 25
2. BACKGROUND
2.1. Cardiovascular disease is a major cause of morbidity and mortality and is a significant contributory factor towards the current level of health inequalities in Dorset. 37.4% of deaths in 2005 (Office for National Statistics) were attributed to this, the highest cause of premature death. A structured approach to cardiovascular risk management for all people aged 40-74 years old, who are not already on any patient risk register, is expected to be established by 2012, with initial small scale early implementation in each PCT during 2009/10. The service is referred to as “NHS Health Checks”.
2.2. It is calculated that NHS Health Checks and appropriate management of risk could prevent 1,600 heart attacks and strokes a year nationally, and provide a real opportunity to tackle the gap in life expectancy between deprived and less deprived populations. Based on 2008 figures, the total population in NHS Dorset eligible for a Health Check will be 139,684 once the service is fully established.
2.3. In order to reduce risk and prevent development of diseases such as diabetes, the emphasis will be placed on encouraging people into lifestyle interventions to address the modifiable risk factors. Only once these interventions and lifestyle changes have been tried will treatments such as medication be considered unless there are clear overriding medical indications e.g. identification of diabetes, hypertension or familial hyperlipidaemia.
2.4. Patients must be offered a choice of venue (where available) at which the checks may be carried out.
3. SERVICE AIMS
3.1. To improve health outcomes and quality of life by enabling more people to be identified at an earlier stage of vascular change. This will give a better chance of putting in place positive ways to make substantial reductions in the risk of cardiovascular morbidity, premature death or disability.
3.2. To prevent the development of diabetes in many of those at increased risk of this disease.
3.3. To sustain the continuing increase in life expectancy and reduction in premature mortality that is under threat from the rise in obesity and sedentary living.
3.4. To make significant inroads into reducing health inequalities, including socio-economic, ethnic and gender inequalities.
3.5. To offer convenience and accessibility of testing facilities by providing a choice of location and extended hours of availability.
Page 3 of 25
SERVICE OUTLINE
This Local Enhanced Service will fund the following:
4. COMPONENT A (GMS AND PMS CONTRACTORS ONLY): PATIENT IDENTIFICATION, RECALL AND RECORDING
Identification of at risk patients
4.1. Practices will use the Oberoi software already installed on GP Clinical Systems to identify the patient cohort for the service. Eligible patients will be those who:
are aged between 40 and 74 years are recorded as a current smoker or have no smoking status recorded have an established or estimated CVD risk score of over 20% and are NOT on one of the following disease registers:
Diabetes CHD Heart Failure Atrial Fibrillation Hypertension Stroke/TIA Renal disease / CKD
(All the above disease registers can be filtered using the Oberoi software and a spreadsheet.)
Palliative Care (practices will manually identify and exclude those patients that are on the palliative care register)
Establishment of call and recall process
4.2. Practices will set up a call and recall process for this group of patients. Using the template provided (Appendix A) written invitations, including a copy of the Department of Health information leaflet, will be sent to all patients eligible to attend a health check. The letter must be presented at the time of the Health Check as proof of invitation. Invitations must include details of available choice of provider and venue where applicable.
4.3. Practices are required to record two attempts at contacting the patient. Where necessary, the second attempt may be by telephone or text message. It is recommended that the time between contact attempts is approximately one month.
4.4. All practices must order and maintain supplies of the DoH leaflets to send out with the letters of invitation. Orders are made directly from the DoH by following the link: http://www.orderline.dh.gov.uk/ecom_dh/public/home.jsf
Page 4 of 25
4.5. By 2012/13, the PCT will be required to ensure that 20% of the population is offered screening annually, with a 5 year call and recall system in place. The call and recall system will ultimately be a national arrangement, but until that is in place, local arrangements will need to be made.
Recording
4.6. GP practices will record in the patient’s clinical record the full data set (measurements, values, follow-up, referral and outcome) collected as a result of Health Checks carried out at any venue by any approved provider.
4.7. A clinical system template will be provided by the PCT to assist data entry (Appendix D). An electronic copy of this will be supplied to all pharmacy contractors to complete with a responsibility to ensure safe and timely transfer to the patient’s registered GP for entry into the patient record.
5. COMPONENT B (GMS, PMS AND COMMUNITY PHARMACY CONTRACTORS): “THE HEALTH CHECK”
5.1. The service to be provided will be underpinned by the values and principles detailed in the following documents:
Putting Prevention First (DOH, March 2008) The Handbook for Vascular Risk Assessment, Risk Reduction and Risk
Management (UK National Screening Committee, March 2008) Putting Prevention First – Best Practice Guidance (April 2009)
(http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_098410.pdf)
Be Active Be Healthy: (DOH, February 2009)
It is a requirement that best practice guidance is followed at all times.
Process
5.2. The service provider will ensure that people presenting for an NHS Health Check are informed about the process of the service and are given the opportunity to ask questions. The provider will seek consent for the assessment and the communication of results to their GP. Invitation letters will contain a clause stating that consent to share information with their GP is a requirement for having a Health Check. Persons who decline this consent should be refused a Health Check. Pharmacy contractors are required to record this on the monthly data submission form (Appendix F)
Page 5 of 25
5.3. The following information and measurements will be collected in order to establish the CVD risk over 10 years as well as the appropriate referrals or interventions required:
Age Gender Ethnicity Smoking status Physical activity Alcohol consumption level Family history of vascular disease Body Mass Index Random Cholesterol measurement (TC:HDL ratio) Blood pressure measurement
5.4. The service provider will calculate the estimated individual 10 year CVD risk using the Framingham or Q-Risk2 score tools (as per best practice guidance page 14). GP practices will have access to one or both of these tools. Pharmacies can access Framingham at http://cvrisk.mvm.ed.ac.uk/calculator/framingham.htmThe Q-risk calculator can be found athttp://www.qrisk.org
5.5. The risk assessment pathway is presented in detail in the DoH publication Putting Prevention First – Best Practice Guidance (April 2009). The diagrams in appendix B are taken from the guidance and describe the risk assessment pathway and diabetes filter. Some patients may need to return for a subsequent fasting blood glucose measurement or additional blood pressure measurements.
5.6. The service provider will document the measurements and assessed level of CVD risk using the data template provided (appendix D). In GP practices this will be entered directly on to the clinical system. In community pharmacies the template must be completed electronically and sent via secure NHS e-mail to the agreed e-mail address at the at the patient’s registered GP practice for entry by the practice on to the clinical system.
5.7. All data collected from NHS Health Checks carried out either in the GP practice or by a community pharmacy contractor will be recorded in a robust, accurate and timely way to enable effective monitoring.
5.8. The records in pharmacies must be kept securely for two years to enable audit and post payment verification. The records may be kept electronically or in paper form.
5.9. All persons undergoing a Health Check will be given a copy of their results.
5.10. The service provider will communicate the level of risk (high, moderate, low) to the person, and an individually tailored management programme, with appropriate advice, support and interventions depending on the level of risk identified, will be agreed as follows:
Page 6 of 25
5.11. Brief healthy lifestyle advice and support will be given to all people receiving the service to assist them with managing and / or reducing their risk.
5.12. People who are found to be at moderate risk will be offered, where appropriate, interventions such as stop smoking or weight management. Where these services are not available in house, appropriate referrals should be made.
5.13. In addition to the above, people who are found to be at high risk or where a pre-existing disease is suspected or identified (eg Diabetes), will be referred to their GP for further investigation and management. This includes instances where blood pressure measurement is ≥ 200/100 or total cholesterol is ≥ 7.5
5.14. The person will be actively involved in agreeing what advice and/or interventions they will follow. Any decisions must be made in partnership with the person and with their informed consent.
5.15. The service provider will be expected to demonstrate a clear understanding of the services available locally to individuals to support healthier lifestyles and communicate this information to the appropriate individuals.
5.16. The service provider will supply the individual with a pack of information, appropriate to their needs, as identified by the Health Check. PCT recommended resources are listed in appendix E. Providers will order these resources directly and maintain adequate supplies.
5.17. The service will be expected to be available at suitable times which maximise uptake in populations at highest risk. Providers will not be expected to offer the service outside their normal opening hours.
5.18. All service providers will attend clinical meetings to share best practice and discuss service development and improvements. Ideally these meetings will be organised on a locality or sub locality basis, but where this is not possible, a practice meeting will be held. The meetings will be multidisciplinary and include representation from both GP practices and community pharmacies.
Equipment
5.19. NHS Dorset will provide all equipment and consumables required if the service provider does not already have such equipment. Any equipment supplied by the PCT will remain the property of the PCT. All instructions for the equipment must be followed each time it is used. The following equipment will be required: Scales Height measurers Electronic blood pressure monitoring machine or sphygmomanometer Point of care testing devices for measuring cholesterol and blood glucose
5.20. The service provider will undertake external quality assurance tests for point of care testing equipment. All equipment used as part of the service must be cleaned, calibrated and serviced as advised by the manufacturer with appropriate protocols in place. Any problems or faults with NHS equipment must be reported to the PCT immediately.
Page 7 of 25
5.21. All providers must ensure that there are processes in place to ensure robust compliance with current infection control guidelines.
5.22. Each participating contractor will need to have access to a clinical waste disposal service. The contractor will allocate a safe place to store equipment required for the provision of the service and the resultant clinical waste. Contractors should ensure that all sharps and waste are disposed of appropriately, following their own Standard Operating Procedure (SOP).
5.23. The contractor must ensure that all staff are made aware of the risks associated with the handling of clinical waste and the correct procedures to be used to minimise those risks. SOPs for needle stick injury and the handling of clinical waste (including dealing with spillages) must be in place.
Accreditation and Eligibility to Provide the Service
Workforce requirements
5.24. The contractor will:
ensure that all staff involved meet the training, registration and competence requirements
be able to guarantee an adequate and stable workforce at all times to meet the potential demand
notify the PCT immediately if the service is not available due to workforce issues
demonstrate that the NHS Health Checks are performed by a suitably trained and competent healthcare professional who has completed the PCT training and accreditation programme
be expected to work in collaboration with NHS Dorset to ensure that this occurs in a timely manner and in accordance with guidelines
ensure that the Hepatitis B status of all staff involved in blood collection is recorded and uptake of immunisation is recommended if required in accordance with national guidance.
Training
5.25. All staff who are involved in the delivery of the screening programme will be expected to attend training provided by NHS Dorset.
5.26. The training requirements for GP practice and pharmacy staff are variable and the following options will be available:
Page 8 of 25
5.27. Pharmacy staff:
Completion of CPPE Vascular Risk Focal Point Learning Programme (only available to pharmacists and registered technicians)OR Attendance at one of the PCT organised “Putting Prevention First” training days covering the background to the programme, risk assessment and management
PLUSAttendance at a separate training evening to cover practical use of equipment and the details of the NHS Dorset Health Checks programme.
Each participating pharmacy must have pharmacist/s who have attended both elements of the training to take the clinical lead for the service and who must be present in the pharmacy when the service is being provided. All other members of staff involved in the delivery of the service must also complete both elements of the training.
5.28. GP practice staff
Clinical lead for the service within the practice and clinical staff involved in delivery of the service:
o Attendance at one of the PCT organised “Putting Prevention First” training days covering the background to the programme, risk assessment and management
o Specific training as required for Point of Care testing equipment
Practice manager and / or designated administrator for the service:
o Attendance at a PCT organised meeting to cover the details of the NHS Dorset Health Checks programme.
Service providers will be required to work with NHS Dorset to review progress and identify any further training needs.
Consultation Area in Community Pharmacies
5.29. A consultation area, at least at the level required for the provision of the Medicines Use Review service, which provides sufficient privacy (including visual privacy) and safety, must be used for provision of the service. Hand washing facilities will be required within the consultation area or nearby. The service provider must ensure that NHS infection control standards are complied with.
Duration of Service
5.30. This service is offered initially for the period from January 2010 to January 2011, to be extended with agreement between the PCT and the contractor thereafter. This early implementation phase of the programme will inform future developments and the detail of the service is likely to change over time.
Page 9 of 25
Termination
5.31. It is not envisaged that either party would give notice to terminate the Local Enhanced Agreement during this one year period. However, should this issue arise, NHS Dorset and the provider must jointly agree an appropriate strategy to manage existing services.
5.32. The contractor must advise NHS Dorset of its wish to opt out of the LES. NHS Dorset will seek to secure an alternative provider within a three month notification period.
5.33. This Local Enhanced Service may be suspended or terminated:
Immediately if the provider becomes bankrupt or insolvent;
If either party commits a fundamental breach of the terms of the agreement at any point during the period of agreement.
Pricing and Payment Mechanisms
5.34. Each practice or pharmacy contracted to provide this service will receive fees attached to the service components that they are contracted to provide.
Component A
5.35. For confirmation of participation in the scheme and agreement to deliver Component A, including provision of audit data as requested by the PCT: - A one-off payment based on the practice list size will be paid. This payment to be made upon receipt of approved sign-up form. (see back of this document)
The payment will be £250 for the average list size of 6,666. The minimum payment will be £125 for a list sized of 3,333 or less and the payment will be capped at £500 for practices with list sizes of 13,332 or above.
5.36. A payment of £1.00 will be made for each patient invited to attend for a Health Check in accordance with Oberoi data, when all the following criteria have been met –
Invitation sent and recorded Follow up invitation sent if required Data template completed for any Health Checks carried out by GP
Practice Data template completed for any Health Checks carried out by any other
provider Patients failing to attend after 3 month period to be exception reported as
non-responders.
Page 10 of 25
5.37. Claims to be made on the quarterly enhanced services claim form.
Component B
5.38. The fee for the Health Check will be £35. This will include follow up with further blood pressure measurements and a fasting blood glucose test where indicated. The fee will be kept under review.
5.39. This price is fully inclusive of attendance at training, administration costs and a professional fee relating to the carrying out of the health check.
5.40. PCT equipment, consumables, quality control, waste contract and Hepatitis B vaccination costs will be covered by NHS Dorset.
5.41. Equipment supplied by the PCT is and remains the property of the PCT.
5.42. No payments will be made for checks carried out on patients not included in the recall cohort patients who do not attend (DNAs) services that are outwith this specification and for which prior approval has not
been sought and granted checks carried out by pharmacy providers where consent to share information
has been refused.
5.43. The price will be uplifted annually in line with GMS/PMS enhanced services and Community Pharmacy services uplifts as determined by the PCT/Department of Health.
5.44. Providers will be paid on submission of a quarterly return to the PCT.
5.45. The GMS/PMS contractor return will be incorporated in the Enhanced Services quarterly claim form.
5.46. The community pharmacy contractor return will be as per the format in appendix F. Records of the Health Checks carried out and patient invitation letters collected must be retained in the pharmacy for the purpose of claim validation for 2 years.
5.47. Community pharmacy contractors must ensure that there are processes in place to ensure compliance with current information governance guidelines, especially in relation to the safe and secure storage of electronic clinical records.
Page 11 of 25
Monitoring and audit
5.48. All contractors will be required to have systems in place to ensure effective contract monitoring can take place.
5.49. Performance monitoring will involve the use of information collected from the GP clinical systems.
5.50. The PCT will require data from the Oberoi CVD risk management tool every three months to accompany the enhanced services quarterly claim. It will be the responsibility of the GP practice to provide this. The first collection date to be decided when a date for commencement of the Health Checks programme is agreed.
5.51. In addition to Oberoi quarterly data, reporting on additional information gathered in the Health Check template may be required, including numbers of referrals resulting from the checks and any new clinical diagnoses recorded.
5.52. All contractors must be able to demonstrate robust quality assurance for any processes or equipment used and must be able to provide evidence of the following:
The results of external quality assurance tests for point of care testing equipment. The results should fall within the acceptable range.
SOPs and the referral pathways for the service that are reviewed on an annual basis. The SOPs must specify which groups of staff can provide the individual elements of the service.
Staff involved in the provision of the service have undertaken CPD relevant to this service on at least an annual basis.
Appropriate NHS Dorset / DoH healthy lifestyle advice leaflets and other promotional materials are available and actively promoted and discussed with the client where appropriate.
All contractors will participate in an annual NHS Dorset organised audit of service provision and co-operate with any local assessment of service user experience. The detail and timing of these activities will be decided once the service is operational and feedback of processes can be assessed.
Page 12 of 25
6 COMPONENT C (GMS, PMS AND COMMUNITY PHARMACY CONTRACTORS)
IDENTIFICATION WITHIN THE COMMUNITY OF PEOPLE FROM GROUPS WITH THE HIGHEST RISK OF DYING PREMATURELY
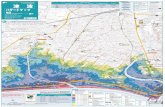
6.1 Component C complements the practice record-based approach described in paragraph 1.4 and in Component A. Opportunistic signposting to a GMS, PMS or community pharmacy contractor by means of an “NHS Dorset Health Check Passport” (see Fig. 1) will enable those potentially most at risk (NICE public health guidance 15), who may or may not be not be registered with a GP, to access the NHS Health Check.
Figure 1
6.2 As an alternative to the invitation to an NHS Health Check described in Component A, the “Passport Criteria” will be used to identify the patients who are eligible for the service.
6.3 Eligible patients in this case will be those who:
are aged between 50 and 74 years (please note the higher threshold for this group which enables more cost effective targeting (BMJ 2010; 340.c1693doc10.1136/bmjc1693)
are in receipt of income support, job seeker’s allowance, working tax credit or pension credit.
Page 13 of 25
GP practices
Handed out at events
Job centres
Citizens Advice Bureaux
Post offices
Pharmacies
Patient attends their chosen venue for an NHS Health Check
NHS Dorset Health Check
Passport
PharmacyPatient’s own GP practice
Report sent to patients GP or information provided to encourage registration
are residents of the Weymouth and Portland or North Dorset localities
and who state they are NOT already diagnosed and being treated for any of the following diseases -
Diabetes CHD Heart Failure Atrial Fibrillation Hypertension Stroke/TIA Renal disease / CKD Familial hypercholesterolemia Peripheral Arterial Disease (PAD) Receiving palliative care treatment
6.4 Patients, who have previously had an NHS Health Check, are not eligible for a further check within a five year period. No payment will be made for any Health Check under the NHS Dorset Passport scheme which is carried out on patients who are not eligible The “Blue Free NHS Health Check” strap line on the Passport and official NHS Health Check leaflet may help people who are unsure to recognise the service. GMS and PMS contractors must check the patient records to ascertain whether the patient has previously had an NHS Heath Check.
6.5 Patients who have previously received an invitation but have not responded are eligible to proceed via the passport system.
6.6 NHS Dorset Health Check Passports will be made available and promoted at the outlets listed in figure 1. The person will then present at their chosen venue to request a check. GMS and PMS contractors must ensure that patients are registered with the practice before undertaking an NHS Health Check
6.7 The provider must seek consent for the assessment. Persons (Fig.1) who are considering having an NHS Health Check must be offered an explanatory NHS Health Check leaflet (DH 291778). It is a requirement that adequate opportunity is given to proceed to an NHS Health Check from an informed position.
6.8 Before conducting an NHS Health Check the provider must ensure that the patient has signed the passport confirming eligibility as defined in 6.3 and 6.4. No payment will be made for any Health Check under the NHS Dorset Passport scheme which is carried out on patients who are not eligible. A copy of the signed passport must be securely stored by the GP practice or pharmacy and kept for audit purposes for a period of two years. Receipt of a signed passport will provide evidence of consent.
6.9 The provider must seek consent for communication of the results of the NHS Health Check to the patient’s registered GP. People who decline this consent should not be refused an NHS Health Check. However:
Page 14 of 25
People not already registered with a GP practice must be encouraged and given advice on how to register with a GP practice.
People who are registered with a GP practice must be encouraged strongly to reconsider and give consent at a future time.
6.10 This scenario should be the exception and the majority of patients should consent with the sharing of information. Pharmacy contractors are required to record this on the monthly data submission form (Appendix F). The results for those people not willing to consent to sharing results or not currently registered with a GP practice must be stored securely in the pharmacy until required. An anonymised copy of the results must be e-mailed to a designated nhs.net e-mail address at the PCT so that the results can be collated and used alongside the data from GP practice records.
6.11 The NHS number should be recorded by the pharmacy where possible. If the patient does not know their NHS number, this does not preclude them from having a check.
Once eligibility has been established and the patient wishes to proceed with an NHS Health Check the process continues as per paragraph 5 Component B “The NHS Health Check
Page 15 of 25
Appendix A
NHS Number –
Name
Address Line1
Address Line 2
Address Line 3
Dear Xxxx
We are inviting you to attend your free NHS Health Check
NHS Health Checks are being offered to people aged between 40 and 74 once every five years.
You have a choice where you wish to attend for your Health Check – in your area these are available at:-
Your GP Surgery (tel…………..)
Your local community pharmacy (Tel………………….)
Please contact your chosen venue to make an appointment.
PLEASE NOTE – YOU MUST PRESENT THIS INVITATION WHEN ATTENDING FOR YOUR CHECK.
The check is to assess your risk of developing heart disease, stroke, kidney disease or diabetes. If there are any warning signs, then together we can do something about it.
By taking early action, you can improve your health and prevent the onset of these conditions. There is good evidence for this.
The check should take about 20–30 minutes and is based on straightforward questions and measurements such as age, sex, family history, height, weight and blood pressure. There will also be a simple blood test to measure your cholesterol level.
Following the check, you will receive a copy of your results and free personalised advice about what you can do to stay healthy.
Please note that choosing to have a health check at your local pharmacy is dependent on your agreement to the information and results collected being shared with your GP.
Take a look at the enclosed leaflet for more information about the NHS Health Check and how it could benefit you.
Yours sincerely
xxxxxxxxxxxxxxxx
(Name of health care professional to go here)
PS. REMEMBER TO KEEP THIS INVITATION AS YOU WILL NEED TO TAKE IT WITH YOU WHEN ATTENDING FOR YOUR CHECK.
Page 16 of 25
Appendix C
REFERRAL AND FOLLOW UP:
Factor Threshold Action Referral or GP follow upCardiovascular risk assessment
CV risk is assessed as >20% over 10 years
Offer intensive lifestyle advice and refer to GP for follow up after 3 months
Management of risk and consideration of statin prescribing(if lifestyle advice has been attempted for 3 months)
Total Cholesterol TC is ≥ 7.5 Refer to GP To assess for possibility of familial hypercholesterolaemia
Hypertension risk assessment
BP is ≥ 140/90
BP is ≥ 200/100
Ask person to return for 2 more appointments * and check BP at least twice on each occasion. If the BP is still ≥ 140/90 refer to GP
Refer to GP immediately
Management for hypertension
Diabetes risk assessment
BMI is ≥27.5 in individuals from Indian, Pakistani, Bangladeshi, Other Asian and Chinese ethnicity categories
BMI is ≥ 30 in other ethnicity categories
BP is ≥ 140/90 (either measurement)
People with symptoms of diabetes must be referred immediately
People without symptoms requested to return to surgery/pharmacy for Fasting Plasma Glucose Test or HbA1c
If fasting plasma glucose ≥5.5mmol/l refer to GP
Follow up at GP practice with oral glucose tolerance test or repeat HbA1c as per diabetes filter to establish possible diagnosis of diabetes
Chronic kidney disease risk assessment (as for hypertension risk above)
BP is ≥ 140/90
BP is ≥ 200/100
Ask person to return for 2 more appointments * and check BP at least twice on each occasion. If the BP is still ≥ 140/90 refer to GP
Refer to GP immediately
Person requires assessment for CKD by GP
* Please see BNF for appropriate time periods between appointments
Page 18 of 25
Factor Threshold Action Referral or GP follow upSmoking status Smoker Ask and record smoking
status.Advise person of health benefits.Act on person`s response
Offer 1:1 SmokeStop support in surgery/pharmacy if available or referral to NHS Dorset SmokeStop service
Weight management
BMI is ≥ 28 Consider:Overall readiness to commit to making changesBarriers to changeSelf-esteemLife stageCultural preferences
Offer 1:1 weight / lifestyle management service in surgery/pharmacy if available or referral to Healthy Choices
Physical activity Activity levels are below the recommended levels of 30 minutes at least 5 times per week/less than active on GPPAQ**
Brief intervention in physical activityGoal settingInformation
Exercise on prescription if available locally
Alcohol Alcohol consumption is over recommended daily levels of 3-4 units for men and 2-3 units for women
Provide “know your limits”information and refer to GP if have concerns
Assessment and further referral if necessary
** GP Physical activity questionnaire can be accessed at http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_063812
Page 19 of 25
Appendix DVascular Risk Assessment
Place of Assessment: Date:
Name:
Date of birth: Age: Sex: M F
Address:
Postcode: Tel:
NHS Number: GP: Practice:
Ethnicity: Click here
BP1: Follow up:
BP2: Date:
BP3: Date: Ref to GP:
Advice on diet:
Smoking: Status Smoking advice: Ref to Smokestop:
Total Cholesterol: HDL cholesterol:
Total Cholesterol / HDL Cholesterol:
FH Diabetes in first degree relative: FH FH CVD in first degree male relative <55: FHFH CVD in first degree female relative <65 FH
Fasting Blood Glucose:
Alcohol: units/week Alcohol Advice: GPPAQ
Exercise grading Advice:
Framingham: Score: QRisk: Score: Reason for non assessment: Click here
Notes:
Page 20 of 25
Appendix E
RISK MANAGEMENT – LIFESTYLE INTERVENTIONS
NHS SMOKESTOP SERVICES REFERRAL:
There are 4 resources to be provided for those who wish to reduce their risk by stopping smoking:
1. Stop Smoking Start Living. Order No. 6000a Smokefree Guide. October 2008. DOH 291379.
2. Your Smokefree Road to Health. Order No. DH296847/0709/6000BR Ready Reckoner. July 2009.
3. The “Want to quit smoking?” Dorset SmokeStop card for those contemplating but not ready to give up.
4. The Dorset Smokefree referral card for those who are ready to stop smoking and wish to access this service.
ORDER 1 and 2 at: http://smokefree.nhs.uk/resources/ORDER 3 and 4 from: SmokeStop Administrator, NHS Dorset, Little Keep Gate Office, Bridport Road,Dorchester,DT1 1AH.Tel: 01305 361178Email: [email protected]: www.dorsetsmokestop.co.uk
PHYSICAL ACTIVITY:
DoH’s validated tool GPPAQ identifies individuals less than active:http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_063816.xls
Get Active Booklet: http://www.bhf.org.uk/publications/view_publication.aspx?ps=1000815
Alternatives for over 50`s 30 minutes a day, any way: The fit for life planhttp://www.bhf.org.uk/publications/view_publication.aspx?ps=1000953
Let’s get moving is a resource for an individual that has been recently produced through the NHS physical activity care pathway.http://www.info4local.gov.uk/documents/publications/1344663
Walking the way to health link to local health walks http://www.whi.org.uk/index.asp
Local resources:B-active in Dorset guidehttp://www.b-activeindorset.org/
Coming soon: website with physical exercise opportunities for 2012. Team Dorset Challenge supported by Active Dorset.
Page 21 of 25
EXERCISE ON PRESCRIPTION
Currently there is no central coordination of exercise referral across NHS Dorset.
Weymouth and Portland
Exercise referral happens in:• Budmouth Community Sports Centre 01305 830508• Portland Spa 01305 828245• Weymouth Swimming Pool 01305 774373
Osprey leisure centre is a private organisation which is a sports trust who offer services but who do not fit into the criteria for the exercise referral scheme as they don’t have exercise referral trained personnel there. Although it is not a recognized centre, they do have a trained nurse providing pre checks.
Cardio clubs operate already and have small capacity to expand for those with specific health needs. Contact: Healthy Living Wessex.
North Dorset
The North Dorset exercise referral scheme is administered by the North Dorset District Council. In the Sherborne area it is administered by the West Dorset District Council
A physical activity opportunities contact sheet for North Dorset is being circulated to service providers.
ALCOHOL
Advice sheet downloadable from the Health Professionals “Health Check” Zone of the NHS Dorset website.
Behaviour change tool: Mid-llfe LifeCheck: http://www.nhs.uk/LifeCheck/Pages/Mid-LifeLifeCheck.aspx
Page 22 of 25
WEIGHT MANAGEMENT:
Give lifestyle advice about healthy eating and physical activity.
If a person has a BMI of equal to or over 28, is not pregnant, and is ready to make lifestyle changes and has not attended a slimming group in the last three months, the person can be referred to healthy choices (commercial weight management programme). A referral form and flier for this service is available see below:
Raising the issue of weight with adults – information leaflet order from:http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4134408
For those with BMI >28 Your weight, provide “Your health” (a weight loss guide – booklet) and if individual willing, referral to Healthy Choices using word document attached (Available for download on NHS Health Check link within Health Professionals Zone of NHS Dorset Website).
For those who are overweight with BMI >25:Your weight, Your health (a weight loss guide – Booklet)http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4134408
For those where the individual’s weight status is not a risk factor, reinforcement of the benefits of healthy eating and being physically active can be provided using the following two publications:
Eatwell – 8 tips for making healthier choiceshttp://www.food.gov.uk/aboutus/publications/to order – 0845 6060667 or e-mail [email protected]
Get active - http://www.bhf.org.uk/publications/view_publication.aspx?ps=1000815
Advice and referral sheets to the Health Choices programme and IGT lifestyle management advice are downloadable from the Health Professionals “Health Check” Zone of the NHS Dorset website.
Health Professionals “Health Check” Zone of the NHS Dorset website.
http://www.dorset-pct.nhs.uk/health_professionals_zone/health_checks/main.asp
Username and password will be provided.
Page 23 of 25
Appendix F
NHS Health Check service – Community Pharmacy Claim Form
Pharmacy Name: Claim for months of:
Pharmacy Address: Date claim submitted:
Patient No
NHS Number Fasting blood glucose test required
Additional BP measurements required
Referral to GP
Number of patients who refused consent to share information with GP and therefore did not have a Health Check
I declare that the above information is a true record of the Health Checks conducted:Signed: Name:
Please return quarterly to the Medicines Management Team at the PCT
Page 24 of 25
NHS DORSETLOCAL ENHANCED SERVICE SPECIFICATION
NHS HEALTH CHECKSThis service specification has been produced by NHS Dorset
and has been discussed with the Local Pharmaceutical Committee.
1. The contract is made between NHS Dorset (the purchaser) and ……………………………………………… (the provider), the pharmacy authorised to supply this service.
2. The contact will commence on ……………………… and is subject to termination as in points 5 and 6 below.
3. The provider will ensure that the necessary documentation, as detailed in the service specification, is maintained and made available to the purchaser to enable the service to be monitored.
4. All equipment supplied by the PCT is loaned to the pharmacy and must be returned to the PCT on termination of the contract.
5. The first points of contact for enquiries about this service specification are: ………………………………………….. (the nominated contact manager for the provider) and ……Julia Booth ……... (the nominated contract manager for the purchaser).
6. This agreement shall be terminated:
by either party giving not less than three months notice in writing; if either party commits a breach of the terms and conditions of the contract
at any point during the period of the contract. The offended party may service notice in writing of not less than one month to the party in breach, terminating the contract on the expiry of the notice period
if the provider ceases to maintain the standards of the service specification.
The PCT must be informed in advance if there is a change in pharmacy staff that will affect the delivery of this service
7. The contract will be suspended pending the outcome of any investigation into alleged fraud.
8. The pharmacy must remain compliant with all the essential services under the Community Pharmacy Contractual Framework as part of this agreement.
9. In the event of a dispute remaining unresolved to the satisfaction of both parties, the issue shall be resolved by arbitration. Within one month of the required meeting between the contract manager for the purchaser and the contract manager for the provider, an arbitrator who is mutually acceptable to both parties shall be monitored. The decision of the arbitrator shall be binding upon both parties.
For the Primary Care Trust
Signed: Dated:
For the Pharmacy
Signed: Dated:
I understand that action may be taken against me if I make an incorrect claim. I consent to the disclosure of relevant information for the purposes of fraud prevention, detection and investigation
Page 25 of 25